ABSTRACT
Encephalitis, inflammation of the brain, is most commonly caused by a viral infection (especially herpes simplex virus [HSV] type 1 in the UK) although autoimmune causes, such as N-methyl D-aspartate receptor (NMDAR) antibody encephalitis, are increasingly recognised. Most patients present with a change in consciousness level and may have fever, seizures, movement disorder or focal neurological deficits. Diagnosis hinges crucially on lumbar puncture and cerebrospinal fluid (CSF) examination, but imaging and electroencephalography (EEG) may also be helpful. Treatment of HSV encephalitis with aciclovir dramatically improves outcome, but the optimal management of autoimmune encephalitis is still uncertain. Many patients with encephalitis are left with residual physical or neuropsychological deficits which require long-term multidisciplinary management. Here we review assessment of patients with suspected encephalitis, general aspects of management and areas of ongoing research.
KEYWORDS: encephalitis, encephalopathy, confusion, lumbar puncture, brain infection
Key points
Undertaking a lumbar puncture is vital to distinguish encephalitis from encephalopathy, and therefore to guide management
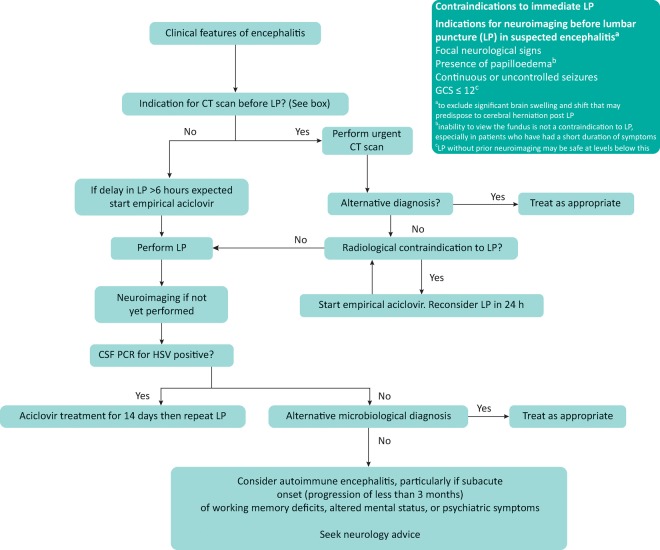
Imaging is not required before lumbar puncture unless a specific contraindication is present (see Fig 1)
Aciclovir is a time-critical life-saving treatment for HSV encephalitis and should be commenced before lumbar puncture if this is delayed for any reason
Investigation and management of suspected autoimmune encephalitis should be undertaken in consultation with a neurologist
Many patients with encephalitis will have residual physical and neuropsychological issues and require a multidisciplinary approach to their ongoing care
Fig 1.
Algorithm for basic management of acute encephalitis (based on UK guidelines).6 CSF = cerebrospinal fluid; GCS = Glasgow Coma Scale; HSV = herpes simplex virus; LP = lumbar puncture; VZV = varicella zoster virus
Introduction: definitions and importance
Acute encephalitis is a neurological emergency which can cause severe disability or death, but can often be treated if diagnosed promptly. Strictly, encephalitis is a pathological entity meaning inflammation of the brain, but this can be ascertained clinically by assessing proxy markers: cerebrospinal fluid (CSF) parameters, imaging or electroencephalogram (EEG) (Box 1). There are approximately 6000 cases of encephalitis in the UK annually,1 so most district general hospitals might expect several cases per year. However, unlike more common conditions such as stroke, which has dedicated units providing multifaceted management, patients with encephalitis are not usually looked after by specialist teams, presenting significant clinical challenges.
Box 1.
Definitions (as used in research studies)4
| Encephalopathy = (altered consciousness persisting for longer than 24 h, including lethargy, irritability or a change in personality or behaviour) |
Encephalitis = encephalopathy AND evidence of CNS inflammation, demonstrated by at least two of:
|
CNS = central nervous system; CSF = cerebrospinal fluid; EEG = electroencephalography
The typical patient presenting with encephalopathy is referred to the acute medicine team, but there are often significant delays in the suspicion of encephalitis being raised.2 The urgent tasks facing the assessing doctor are to stabilise the patient and to rule out potentially life-threatening diagnoses, including HSV type 1 encephalitis which can kill rapidly and needs urgent antiviral treatment. Making this diagnosis hinges crucially on lumbar puncture (LP), which in practice is often delayed.3 Once a treatable viral cause is excluded, autoimmune encephalitis may be considered, but tests for these conditions take longer to perform. Even with thorough investigation, between 37% and 62% of patients with encephalitis will have no identified cause,4,5 and the management of this group remains challenging.
This article aims to cover current practice in encephalitis in adults, from the front door of the emergency department to the point when a specialist referral to neurology or infectious diseases may be made.
Clinical assessment and investigations
Confusion is a common presentation to the acute medical unit and has a wide differential diagnosis (Box 2). The clinical challenge is distinguishing causes of encephalopathy, including septic, metabolic, toxic and others, from patients who have encephalitis and therefore need specific treatments. Initial history should identify clues as to possible causes, including a full collateral history if available, in order to ascertain the true duration of the problem. Evidence should be sought of a change in personality or behaviour, or periods of drowsiness or seizures (which may be subtle). A travel history should be obtained, including any contact with animals, fresh water, mosquito or tick bites, or exposure to illnesses in the community. Known immunocompromise or risk factors for HIV infection should be established. Examination should establish conscious level, any focal neurological deficit, seizure activity or movement disorder.
Box 2.
Most common causes and mimics of encephalitis in immunocompetent adults in the UK
| Causes: |
| Viral: Herpes simplex virus types 1 and 2, varicella zoster virus, enteroviruses, adenovirus, parechovirus, measles virus, HIV |
| Autoimmune (main tumour associations in brackets): Antibodies against neuronal surface antigens: NMDAR antibody encephalitis (ovarian teratoma), LGI-1 antibody encephalitis (thymoma), antibodies against intracellular antigens: anti-Hu (small cell lung tumour), anti-Ma (testicular tumours), anti-GAD, acute disseminated encephalomyelitis, Bickerstaff's encephalitis |
| Mimics: |
| Infective: Systemic sepsis with encephalopathy, bacterial meningitis, TB, opportunistic infections in immunocompromised patients (eg crytococcus, toxoplasma, cytomegalovirus) |
| Inflammatory: Vasculitis, systemic lupus erythematosus with CNS involvement, Behçet's disease, neurosarcoidosis |
| Metabolic: Hypoglycaemia, hyponatraemia, hepatic encephalopathy, toxins (drugs, alcohol) |
| Neoplastic: Primary brain tumour (particularly low grade glioma mimicking CNS inflammation), metastases |
| Others: Status epilepticus from other causes, haemorrhagic or ischaemic stroke, psychiatric disease |
CNS = central nervous system; GAD = glutamic acid decarboxylase; LGI-1 = leucin-rich glioma inactivated 1; NMDAR = N-methyl D-aspartate receptor; TB = tuberculosis
The key to establishing evidence of central nervous system (CNS) inflammation is the analysis of CSF. Lumbar puncture (LP) is often excessively delayed, primarily due to performing brain imaging to exclude raised intracranial pressure.3 Not all patients need imaging before LP, and consensus guidelines suggest a few clear indications for imaging (Fig 1).6–8 If these are present, then either a computed tomography (CT) scan or, ideally, magnetic resonance imaging (MRI) should be obtained urgently. Following this, if there are no radiological contraindications, LP should be performed as soon as possible. Brain imaging serves three purposes: to look for changes of encephalitis, to exclude alternative diagnoses, and to assess patency of the basal cisterns and an absence of mass effect so that LP can proceed.
The key tests that should be requested on CSF are outlined in Fig 1. In viral encephalitis there is typically a CSF pleocytosis (>5 white cells x 109/L), comprising predominantly lymphocytes. However, early in the illness neutrophils can predominate, or occasionally the white cell count may be normal.9 Protein is normal to moderately raised and glucose is normal. Polymerase chain reaction (PCR) for the most frequent viral causes should yield results within 24–48 hours from most laboratories. Cerebrospinal fluid PCR for HSV has a sensitivity and specificity of over 95% for HSV encephalitis in immunocompetent adults.10 In some cases where CSF is obtained very early in the disease course, PCR for HSV can be falsely negative. Therefore, if clinical suspicion of HSV remains, LP should be repeated and will often be positive, despite aciclovir treatment.11
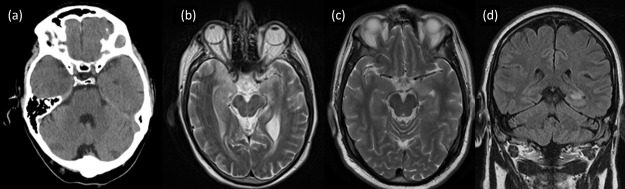
Magnetic resonance imaging is the gold standard technique for brain imaging in encephalitis,12 and is abnormal in 90% of cases of HSV encephalitis,4 but may be normal or subtly abnormal in autoimmune encephalitis (Fig 2).13 Further imaging techniques including ultrasonography, CT of the body and positron emission tomography (PET) imaging may be indicated if a paraneoplastic cause is suspected14 (for example in N-methyl D-aspartate receptor [NMDAR] antibody encephalitis, which may be associated with ovarian teratoma in young females).15 Electroencephalography is useful in identifying and monitoring seizure activity, but is non-specific and can be abnormal in a number of other causes of encephalopathy.
Fig 2.
Brain imaging in encephalitis. (a) CT scan of 69-year-old male with acute HSV-1 encephalitis showing low intensity area in right temporal lobe. (b) T2 weighted axial MRI from same patient showing bilateral asymmetrical signal abnormality in medial temporal lobes. (c) T2 weighted axial MRI of 55-year-old male with LGI-1 antibody encephalitis showing high signal in the left medial temporal lobe. (d) Coronal T2 FLAIR from same patient showing high signal in left medial temporal lobe. CT = computed tomography; FLAIR = fluid attenuation inversion recovery; HSV = herpes simplex virus; LGI-1 = leucin-rich glioma inactivated 1; MRI = magnetic resonance imaging
All patients with suspected brain infection should have an HIV test. Meningoencephalitis can occur at the time of HIV seroconversion16 and immunocompromise vastly alters the differential diagnosis. Since HIV serology may be negative at seroconversion, if there is clinical suspicion HIV RNA testing should be requested.17
If tests for an infective cause are negative, or if patients present with a recognisable phenotype of autoimmune encephalitis at the outset, then autoantibody testing should be considered.18 The number of antibodies associated with encephalitis is expanding rapidly, but the best recognised phenotypes are those of NMDAR antibody encephalitis and LGI-1 antibody encephalitis (a subunit of the voltage-gated potassium channel). The decision of which tests to send is best made in consultation with a neurologist.
The role of brain biopsy in the diagnosis of encephalitis has declined since the advent of PCR testing in CSF and it does not form part of the initial assessment. However, it still has a place for patients in whom diagnosis has not been obtained following extensive investigation, particularly if there are focal abnormalities on imaging.19
Key aspects of management
Intravenous aciclovir is a life-saving treatment in HSV encephalitis and has reduced mortality from above 70% to around 10–20%.20,21 It is relatively safe, although there is a small risk of renal impairment owing to a crystal nephropathy.22 Renal function should be monitored; in patients with known renal impairment the dose should be reduced.
Ideally, LP should be performed immediately in patients with suspected brain infection, and empirical treatment started immediately thereafter. However, if LP is delayed for more than 6 hours empirical aciclovir may be needed before LP.6 Patients with HSV encephalitis are likely to remain PCR positive in CSF for at least the first few days after commencing treatment, so LP should still be performed as soon as possible in patients who have commenced aciclovir. This will help to establish the diagnosis and therefore dictate the duration of treatment. The UK guidelines recommend that aciclovir should be continued for at least 2 weeks, at which point the LP should be repeated. If the HSV PCR is still positive, aciclovir should be continued with repeat LP every week until the PCR is negative.6 If the patient is completely well, some would suggest that repeat LP is not necessary.23
The management of autoimmune encephalitis with immune therapy is non-standardised and based on evidence from retrospective studies.24 For initial therapy, most neurologists use corticosteroids intravenously or orally. Intravenous immunoglobulin or plasma exchange are often also used, especially in those failing to improve. Patients should be investigated thoroughly for underlying malignancy, as a proportion of cases are paraneoplastic.25 The available evidence suggests that early treatment improves outcome, and that, if initial therapy is ineffective, second-line therapy with more potent agents is beneficial.26
Of patients with encephalitis, 50–60% have seizures in the acute phase, which may be clinically subtle,4,5,27 and seizure control is a key aspect of management.
The care of patients with encephalitis is challenging for nursing staff. Patients often have physical, neuropsychological and communication difficulties which make interaction with their environment and their relatives demanding. Most patients with encephalitis are left with some degree of neuropsychological impairment,28 and the prevalence of attentional, behavioural and emotional disorders in survivors remains high up to 3 years after diagnosis.29 Access to neuropsychology services can be invaluable in assisting with memory difficulties and other psychological changes in encephalitis.30 Patients and relatives often only hear about encephalitis for the first time when they are diagnosed, and giving them access to reliable information about the condition can be empowering (eg via the Encephalitis Society www.encephalitis.info).
New directions and areas of uncertainty
The advent of aciclovir therapy in the 1980s revolutionised the outcome of HSV encephalitis. However, patients are still dying of the condition and many survivors are left with debilitating sequelae. There is accumulating evidence that the pathogenesis of HSV encephalitis is intimately connected to the degree of host inflammatory response to the virus.31 For some years evidence from in vitro and animal models has suggested that the addition of corticosteroids to aciclovir for the treatment of HSV encephalitis may improve outcome.32–34 A multicentre trial is addressing this question (www.dexenceph.org.uk).
Autoimmune encephalitis mediated by antibodies directed against neuronal components has been newly described in the last decade, and the various antibody targets and clinical phenotypes are still being clarified, including the concept that in some cases autoimmune encephalitis may be triggered by a prior viral encephalitis.35 The optimal management of autoimmune encephalitis is still unclear.24 Key questions, such as whether intravenous immunoglobulin is beneficial as a first line therapy, remain to be clarified by randomised controlled trials.
Despite thorough investigation for infective and autoimmune causes, between 37 and 62% of patients with encephalitis do not have an aetiological cause established.4,5 Novel laboratory techniques, including proteomics, transcriptomics and metabolomics, offer the hope that immune responses in encephalitis will be elucidated, and this may help to stratify unknown patients into aetiological groups. In addition, the search for putative infective agents using next-generation sequencing, and novel antibodies using protein arrays and mass spectrometry, may provide a diagnosis for more patients in the future.
Funding
MAE is supported by the Association of British Neurologists through a Clinical Research Training Fellowship. Both authors are supported by the NIHR Health Protection Research Unit in Emerging and Zoonotic Infections, by the National Institute for Health Research Programme Grants for Applied Research Programme, (Understanding and improving the outcome of viral encephalitis, RP-PG-0108-10048) and the European Union's Horizon 2020 research and innovation program under grant agreement No. 734584, ZikaPLAN (Preparedness Latin America Network).
References
- 1.Granerod J. Cousens S. Davies NW. Crowcroft NS. Thomas SL. New estimates of incidence of encephalitis in England. Emerg Infect Dis. 2013;19:1455–62. doi: 10.3201/eid1909.130064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bell DJ. Suckling R. Rothburn MM, et al. Management of suspected herpes simplex virus encephalitis in adults in a UK teaching hospital. Clin Med. 2009;9:231–5. doi: 10.7861/clinmedicine.9-3-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Michael B. Menezes BF. Cunniffe J, et al. Effect of delayed lumbar punctures on the diagnosis of acute bacterial meningitis in adults. Emerg Med J. 2010;27:433–8. doi: 10.1136/emj.2009.075598. [DOI] [PubMed] [Google Scholar]
- 4.Granerod J. Ambrose HE. Davies NW, et al. Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis. 2010;10:835–44. doi: 10.1016/S1473-3099(10)70222-X. [DOI] [PubMed] [Google Scholar]
- 5.Glaser CA. Gilliam S. Schnurr D, et al. In search of encephalitis etiologies: diagnostic challenges in the California Encephalitis Project, 1998–2000. Clin Infect Dis. 2003;36:731–42. doi: 10.1086/367841. [DOI] [PubMed] [Google Scholar]
- 6.Solomon T. Michael BD. Smith PE, et al. Management of suspected viral encephalitis in adults – Association of British Neurologists and British Infection Association National Guidelines. J Infect. 2011;64:347–73. doi: 10.1016/j.jinf.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 7.Tunkel AR. Glaser CA. Bloch KC, et al. The management of encephalitis: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2008;47:303–27. doi: 10.1086/589747. [DOI] [PubMed] [Google Scholar]
- 8.McGill F. Heyderman RS. Michael BD, et al. The UK joint specialist societies guideline on the diagnosis and management of acute meningitis and meningococcal sepsis in immunocompetent adults. J Infect. 2016;72:405–38. doi: 10.1016/j.jinf.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 9.Saraya AW. Wacharapluesadee S. Petcharat S, et al. Normocellular CSF in herpes simplex encephalitis. BMC Res Notes. 2016;9:95. doi: 10.1186/s13104-016-1922-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cinque P. Cleator GM. Weber T, et al. The role of laboratory investigation in the diagnosis and management of patients with suspected herpes simplex encephalitis: a consensus report. The EU Concerted Action on Virus Meningitis and Encephalitis. J Neurol Neurosurg Psychiatry. 1996;61:339–45. doi: 10.1136/jnnp.61.4.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weil AA. Glaser CA. Amad Z. Forghani B. Patients with suspected herpes simplex encephalitis: rethinking an initial negative polymerase chain reaction result. Clin Infect Dis. 2002;34:1154–7. doi: 10.1086/339550. [DOI] [PubMed] [Google Scholar]
- 12.Bertrand A. Leclercq D. Martinez-Almoyna L, et al. MR imaging of adult acute infectious encephalitis. Med Mal Infect. 2017;47:195–205. doi: 10.1016/j.medmal.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 13.Baumgartner A. Rauer S. Mader I. Meyer PT. Cerebral FDG-PET and MRI findings in autoimmune limbic encephalitis: correlation with autoantibody types. J Neurol. 2013;260:2744–53. doi: 10.1007/s00415-013-7048-2. [DOI] [PubMed] [Google Scholar]
- 14.Hoftberger R. Rosenfeld MR. Dalmau J. Update on neurological paraneoplastic syndromes. Curr Opin Oncol. 2015;27:489–95. doi: 10.1097/CCO.0000000000000222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dalmau J. Tüzün E. Wu HY, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61:25–36. doi: 10.1002/ana.21050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.del Saz SV. Sued O. Falcó V, et al. Acute meningoencephalitis due to human immunodeficiency virus type 1 infection in 13 patients: clinical description and follow-up. J Neurovirol. 2008;14:474–9. doi: 10.1080/13550280802195367. [DOI] [PubMed] [Google Scholar]
- 17.Palfreeman A. Fisher M. Ong E, et al. Testing for HIV: concise guidance. Clin Med. 2009;9:471–6. doi: 10.7861/clinmedicine.9-5-471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Graus F. Titulaer MJ. Balu R, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016;15:391–404. doi: 10.1016/S1474-4422(15)00401-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong SH. Jenkinson MD. Faragher B, et al. Brain biopsy in the management of neurology patients. Eur Neurol. 2010;64:42–5. doi: 10.1159/000315032. [DOI] [PubMed] [Google Scholar]
- 20.Skoldenberg B. Forsgren M. Alestig K, et al. Acyclovir versus vidarabine in herpes simplex encephalitis. Randomised multicentre study in consecutive Swedish patients. Lancet. 1984;2:707–11. doi: 10.1016/s0140-6736(84)92623-0. [DOI] [PubMed] [Google Scholar]
- 21.Whitley RJ. Soong SJ. Dolin R, et al. Adenine arabinoside therapy of biopsy-proved herpes simplex encephalitis. National Institute of Allergy and Infectious Diseases collaborative antiviral study. N Engl J Med. 1977;297:289–94. doi: 10.1056/NEJM197708112970601. [DOI] [PubMed] [Google Scholar]
- 22.Yarlagadda SG. Perazella MA. Drug-induced crystal nephropathy: an update. Expert Opin Drug Saf. 2008;7:147–58. doi: 10.1517/14740338.7.2.147. [DOI] [PubMed] [Google Scholar]
- 23.Stahl JP. Azouvi P. Bruneel F, et al. Guidelines on the management of infectious encephalitis in adults. Med Mal Infect. 2017;47:179–94. doi: 10.1016/j.medmal.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 24.Nosadini M. Mohammad SS. Ramanathan S. Brilot F. Dale RC. Immune therapy in autoimmune encephalitis: a systematic review. Expert Rev Neurother. 2015;15:1391–419. doi: 10.1586/14737175.2015.1115720. [DOI] [PubMed] [Google Scholar]
- 25.Irani SR. Bera K. Waters P, et al. N-methyl-D-aspartate antibody encephalitis: temporal progression of clinical and paraclinical observations in a predominantly non-paraneoplastic disorder of both sexes. Brain. 2010;133:1655–67. doi: 10.1093/brain/awq113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Titulaer MJ. McCracken L. Gabilondo I, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol. 2013;12:157–65. doi: 10.1016/S1474-4422(12)70310-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Misra UK. Tan CT. Kalita J. Viral encephalitis and epilepsy. Epilepsia. 2008;49(Suppl 6):13–8. doi: 10.1111/j.1528-1167.2008.01751.x. [DOI] [PubMed] [Google Scholar]
- 28.Raschilas F. Wolff M. Delatour F, et al. Outcome of and prognostic factors for herpes simplex encephalitis in adult patients: results of a multicenter study. Clin Infect Dis. 2002;35:254–60. doi: 10.1086/341405. [DOI] [PubMed] [Google Scholar]
- 29.Mailles A. De Broucker T. Costanzo P, et al. Long-term outcome of patients presenting with acute infectious encephalitis of various causes in France. Clin Infect Dis. 2012;54:1455–64. doi: 10.1093/cid/cis226. [DOI] [PubMed] [Google Scholar]
- 30.Cooper J. Kierans C. Defres S, et al. Care beyond the hospital ward: understanding the socio-medical trajectory of herpes simplex virus encephalitis. BMC Health Serv Res. 2017;17:646. doi: 10.1186/s12913-017-2608-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Michael BD. Griffiths MJ. Granerod J, et al. The Interleukin-1 Balance During Encephalitis Is Associated With Clinical Severity, Blood-Brain Barrier Permeability, Neuroimaging Changes, and Disease Outcome. J Infect Dis. 2015;213:1651–60. doi: 10.1093/infdis/jiv771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Meyding-Lamade U. Seyfer S. Haas J, et al. Experimental herpes simplex virus encephalitis: inhibition of the expression of inducible nitric oxide synthase in mouse brain tissue. Neurosci Lett. 2002;318:21–4. doi: 10.1016/s0304-3940(01)02469-7. [DOI] [PubMed] [Google Scholar]
- 33.Meyding-Lamade UK. Oberlinner C. Rau PR, et al. Experimental herpes simplex virus encephalitis: a combination therapy of acyclovir and glucocorticoids reduces long-term magnetic resonance imaging abnormalities. J Neurovirol. 2003;9:118–25. doi: 10.1080/13550280390173373. [DOI] [PubMed] [Google Scholar]
- 34.Thompson KA. Blessing WW. Wesselingh SL. Herpes simplex replication and dissemination is not increased by corticosteroid treatment in a rat model of focal Herpes encephalitis. J Neurovirol. 2000;6:25–32. doi: 10.3109/13550280009006379. [DOI] [PubMed] [Google Scholar]
- 35.Armangue T. Moris G. Cantarín-Extremera V, et al. Autoimmune post-herpes simplex encephalitis of adults and teenagers. Neurology. 2015;85:1736–43. doi: 10.1212/WNL.0000000000002125. [DOI] [PMC free article] [PubMed] [Google Scholar]