Abstract
Background
The beneficial effects of atrial septal defect (ASD) device closure on electrical cardiac remodeling are well established. The timing at which these effects starts to take place has yet to be determined.
Objectives
To determine the immediate and short term effects of ASD device closure on cardiac electric remodeling in children.
Methods
30 pediatric patients were subjected to 12 lead Electrocardiogram immediately before ASD device closure, 24 h post procedure, 1 and 6 months after. The maximum and minimum P wave and QT durations in any of the 12 leads were recorded and P wave and QT dispersions were calculated and compared using paired T test.
Results
The immediate 24 h follow up electrocardiogram showed significant decrease in P maximum (140.2 ± 6 versus 130.67 ± 5.4 ms), P dispersion (49.73 ± 9.01 versus 41.43 ± 7.65 ms), PR interval (188.7 ± 6.06 ms versus 182.73 ± 5.8 ms), QRS duration (134.4 ± 4.97 ms versus 127.87 ± 4.44), QT maximum (619.07 ± 15.73 ms versus 613.43 ± 11.87), and QT dispersion (67.6 ± 5.31 versus 62.6 ± 4.68 ms) (P = 0.001). After 1 month all the parameters measured showed further significant decrease with P dispersion reaching 32.13 ± 6 (P = 0.001) and QT dispersion reaching 55.0 ± 4.76 (P = 0.001). These effects were maintained 6 months post device closure.
Conclusion
Percutaneous ASD device closure can reverse electrical changes in atrial and ventricular myocardium as early as the first 24 h post device closure.
Keywords: ASD, Device closure, Electric remodeling, Dispersion
1. Introduction
Atrial septal defect (ASD) accounts for 7–10% of all forms of congenital heart diseases and is the most common form observed in adults.1. Although a significant number of patients with ASD remain asymptomatic until adult age, early diagnosis and treatment of this disease is crucial because of potential complications such as pulmonary hypertension, right-sided heart failure, and atrial arrhythmias.2 Major problems encountered with ASD patients are arrhythmias and primarily atrial fibrillation. Previous studies have demonstrated that P maximum and P dispersion times (the predictors of atrial arrhythmias) are prolonged with ASD patients.3, 4, 5
One reason for recommending early Closure of secundum ASD in children is to prevent the future development of atrial arrhythmias.6 As a result of ASD correction, the right heart is protected from volume load, leading to reductions in both pulmonary artery pressure and right heart cavity dimensions. Thus, significant symptomatic improvement with a decrease in arrhythmic events is observed in these patients.2
The timing of improved electric remodeling and whether this improvement is related to the age of the patient at time of closure represents an area of active research. We sought to record the earliest evidence of improvement of this electric remodeling after ASD device closure in children and to study the longitudinal trend data of electric remodeling using both P wave and QT dispersion in a prospective observational study focusing on measuring these markers before, immediately after, one month and 6 month after device closure in a group of children undergoing ASD device closure.
2. Methods
The study was approved by our institutional review board and informed consent was obtained from all patients or there guardians enrolled in the study.
This was a prospective observational study which included all patients in the pediatric age group who were referred for elective ASD device closure in our center over a period of 6 months. The inclusion criteria for patients to complete the study included children with isolated Secundum ASD with adequate rims deemed suitable for device closure by transthoracic echocardiogram and confirmed by transoesophogeal echocardiogram at time of scheduled closure and who underwent successful ASD device closure.
The following patients were excluded from the study: (i) patients with sinus venosus or primum type ASD, (ii) patients with inadequate rims, (iii) patients with any type of arrhythmia or receiving antiarrhythmic drugs, (iv) presence of contraindications to undergo ASD device closure under general anesthesia.
A custom made sheet was done to include demographic data of each patient as well as echocardiographic assessment of the ASD and its hemodynamic effect before device closure. All patients underwent ASD device closure using the Amplatzer septal occluder (AGA Medical Corporation, now part of St Jude Medical Inc. MN, USA). Device size selection was based on either the balloon waist diameter in case balloon sizing was used or the maximum diameter of the ASD measured by TEE +20% in cases were balloon sizing was not used. Clinical outcome post procedure as well as any related morbidity at follow up was also recorded.
2.1. Electrocardiographic findings
A standard 12-lead electrocardiogram (ECG) was recorded at a rate of 50 mm/s and a calibration of 1mv/cm for all the patients at baseline before the procedure. The P wave, PR interval, and QRS and QT dispersion times were measured as follows:4, 7
P wave: the distance between the points of the earliest and latest P wave activity was recorded as P wave duration. The longest P wave measurement was noted as P maximum (P max) and the shortest measurement as P minimum (P min). A P wave dispersion (P dis = P max–P min) was calculated using these values. PR interval: defined as the interval between the beginning of the P wave and the beginning of the QRS complex.
QRS duration: defined as the maximum QRS duration in any lead from the first to the last sharp vector crossing the isoelectric line. QT interval: defined as the interval between the beginning of the QRS complex and the end of the T wave. The QT dispersion was defined as the difference between the maximum and the minimum of QT intervals that could be measured in any of the 12 ECG leads.
Ten randomly chosen ECGs were reevaluated by the same and another observer to calculate intra- and inter observer variability.
2.2. Follow up evaluation
All patients underwent full transthoracic echocardiogram and 12 lead surface ECG 24 h post ASD device closure and after 1 and 6 months post procedure. Our patients did not experience any significant arrhythmias before ASD closure, neither there were clinically relevant arrhythmias reported or detected in any of the ECGs done at follow up and hence no further evaluations (e.g. 24-h ECG monitoring) were performed.
The same ECG parameters recorded before the procedure (P max, P min, P dis, PR interval, QRS duration, QT interval and QT dis) were recorded by the same observer at 24 h, I month and 6 month post procedure. The single observer reading the ECG data was blinded to the patients’ condition and follow-up details.
2.3. Statistical analysis
All data were collected, tabulated and statistically analyzed using the PC computer. The data were entered to the Statistical Package for Social Science Program (SPSS) version 16. The quantitative data were presented as mean and SD for the parametric data and as median and inter quartile ranges for the non parametric data while the qualitative data was presented as numbers and their related percentage. Chi square test was used to compare between two groups with qualitative data while, paired sample t-test was used to compare between two paired groups with quantitative data. A P value was considered significant if less than 0.05. The Bland-Altman method and coefficient of variation6 were used to evaluate inter and intra observer variability of ECG measurements.
3. Results
This was a prospective observational study which initially included all the 48 patients referred for possible elective trans-catheter ASD closure in our center over the study period. 18 patients were deemed unsuitable for device closure and thus were excluded from the study. The clinical and demographic characteristic of the 30 patients who completed the study are enlisted in Table 1. All the patients studied had successful ASD device closure with the exception of 2 patients who had trivial residual shunting (6.6%) which disappeared after 1 month. Intra- and inter observer variability of both pre- and post procedural measurements was acceptable.
Table 1.
Clinical and demographic characteristics of the study group.
| Characteristics | Findings |
|---|---|
| Gender (M/F) | 16/14 |
| Median age (range) in yrs | 6 (2.5–17) |
| Mean of BSA (range) in m2 | 1.02 (0.6–1.47) |
| ASD diameter by TTE in mm | 16.13 ± 6.51 |
| ASD diameter by TEE in mm | 18.67 ± 6.63 |
| Balloon sizing (Yes/No) | 18/12 |
| Balloon stretched diameter | 18.78 ± 6.38 |
| Qp/Qs | 1.75 ± 0.09 |
| Procedural time in minutes | 37 ± 6.64 |
| Fluoroscopy time in minutes | 16.17 ± 3.64 |
| MPAP at baseline in mmHg | 16.97 ± 3.37 |
| RVSP at baseline in mmHg | 30.77 ± 4.69 |
| MPAP 24 h post procedure in mmHg | 13.33 ± 3.20 |
| RVSP 24 h post procedure in mmHg | 24.70 ± 3.35 |
BSA = body surface area, ASD = atrial septal defect, MPAP = mean pulmonary artery pressure, RVSP = right ventricular systolic pressure.
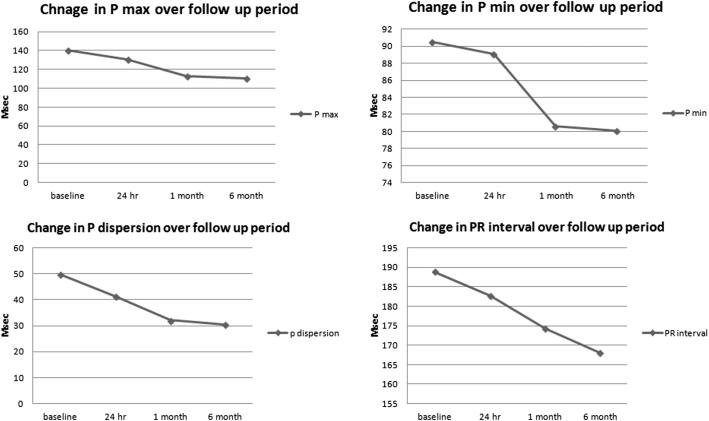
Paired T test was used to compare baseline ECG and the follow up ECG done 24 h after closure; before closure the P maximum ranged from 129 ms to 158 ms with mean 140.2 ± 6.04 ms and at follow up it ranged from 119 ms to 140 ms with mean 130.67 ± 5.40 ms (P value = 0.001). The P minimum before closure ranged from 76 ms to 114 ms with mean 90.47 ± 9.44 ms while after closure ranged from 75 ms to 112 ms with mean 89.1 ± 8.96 ms (P value = 0.072). The P dispersion before closure ranged from 26 ms to 69 ms with mean 49.73 ± 9.01 ms where after closure it ranged from 26 ms to 57 ms with mean 41.43 ± 7.65 ms (P value = 0.001). The PR interval ranged before closure from 174 ms to 200 ms with mean 188.87 ± 6.06 ms while after closure it ranged from 170 ms to 193 ms with mean 182.73 ± 5.80 ms (P value = 0.001) (Fig. 1).
Fig. 1.
Line graph displaying trend over time for P max, P min, PR interval and P wave dispersion of the study group over a follow up period of 6 months.
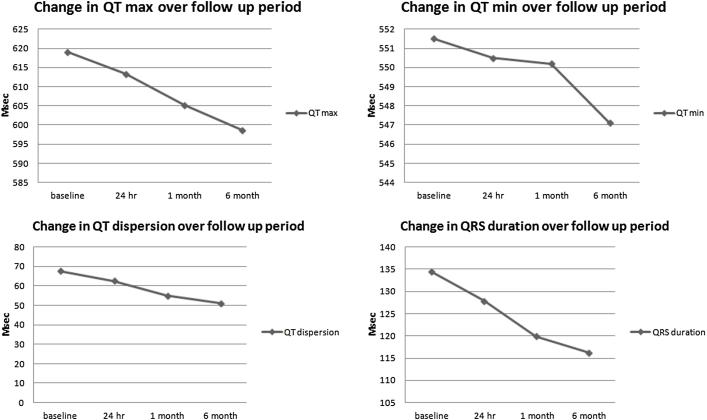
The baseline QRS interval ranged from 122 ms to 141 ms with mean 134.40 ± 4.97 ms and after closure it ranged from 119 ms to 136 ms with mean 127.87 ± 4.44 ms (P value = 0.001). Baseline QT maximum ranged from 596 ms to 662 ms with mean 619.07 ± 15.73 while after closure it ranged from 591 ms to 645 ms with mean 613.43 ± 11.87 ms (P value = 0.001); QT minimum before closure ranged from 530 ms to 589 ms with mean 551.47 ± 13.93 ms while after closure it ranged from 531 ms to 580 ms with mean 550.50 ± 12.00 ms (P value = 0.145); QT dispersion before closure ranged from 59 ms to 75 ms with mean 67.60 ± 5.31 ms while after closure it ranged from 51 ms to 69 ms with mean 62.60 ± 4.68 ms (P value = 0.001) (Fig. 2).
Fig. 2.
Line graph displaying trend over time for QT max, QT min, QRS duration and QT dispersion of the study group over a follow up period of 6 months.
There was a highly significant reduction in the values of P maximum, P dispersion, QT maximum, QT dispersion, QRS interval and PR interval at 24 h post ASD device closure while there was no significant reduction in the P minimum and the QT minimum (Table 2).
Table 2.
Comparison between ECG variables measured at baseline before ASD device closure and those measured after 24 h, at 1 month and 6 month post procedure using paired T test.
| ECG variables | Study Group |
Paired T test |
||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 24 h | 1 month | 6 month | P1 | P2 | P3 | P4 | |
| P max | 140.2 ± 6.0 | 130.7 ± 5.4 | 113.2 ± 5.93 | 110.7 ± 5.2 | 0.001 | 0.001 | 0.001 | 0.004 |
| P min | 90.47 ± 9.4 | 89.1 ± 9.0 | 80.6 ± 4.46 | 80.1 ± 4.9 | 0.072 | 0.004 | 0.002 | 0.004 |
| P dispersion | 49.73 ± 9.0 | 41.4 ± 7.6 | 32.1 ± 6.00 | 30.5 ± 5.1 | 0.001 | 0.001 | 0.001 | 0.004 |
| PR interval | 188.8 ± 6.1 | 182.7 ± 5.8 | 174.3 ± 6.76 | 168.0 ± 6.2 | 0.001 | 0.002 | 0.001 | 0.002 |
| QRS duration | 134.4 ± 5.0 | 127.9 ± 4.4 | 119.9 ± 4.12 | 116.2 ± 3.5 | 0.001 | 0.003 | 0.001 | 0.002 |
| QT max | 619.1 ± 15.7 | 613.4 ± 11.9 | 605.3 ± 13.57 | 598.7 ± 13.3 | 0.001 | 0.001 | 0.001 | 0.002 |
| QT min | 551.5 ± 14.0 | 550.5 ± 12.0 | 550.2 ± 13.00 | 547.1 ± 12.2 | 0.145 | 0.237 | 0.668 | 0.004 |
| QT dispersion | 67.60 ± 5.3 | 62.6 ± 4.7 | 55.0 ± 4.76 | 51.1 ± 5.7 | 0.001 | 0.001 | 0.002 | 0.003 |
P1: between baseline and 24 h, P2: between baseline and 1 month post procedure, P3: between 24 h and 1 month post procedure, P4: between 24 h and 6 month post procedure.
At 1 month follow up all ECG parameters continued to show significant reduction compared to baseline with the exception of QT minimum. The P maximum ranged from 102 ms to 124 ms with mean 113.20 ± 5.93 ms (P value = 0.001); the P minimum ranged from 73 ms to 91 ms with mean 80.57 ± 4.46 ms (P value = 0.004). The P dispersion ranged from 24 ms to 44 ms with mean 32.13 ± 6.00 ms (P value = 0.001). The PR interval ranged from 166 ms to 191 ms with mean 174.27 ± 6.76 ms (P value = 0.002) while the QRS interval ranged from 113 ms to 128 ms with mean 119.87 ± 4.12 ms (P value = 0.003). The QT maximum ranged from 588 ms to 641 ms with mean 605.27 ± 13.57 ms (P value = 0.001); QT minimum ranged from 532 ms to 581 ms with mean 550.17 ± 13.00 ms (P value = 0.237); QT dispersion ranged from 48 ms to 67 ms with mean 55.00 ± 4.76 ms (P value = 0.001) (Table 2).
Comparing the ECG parameters measured 24 h and 1 month post device closure; there was highly significant reduction in the values of P maximum, P minimum, P dispersion, QT maximum, QT dispersion, QRS interval and the PR interval while there was no statistically significant reduction in the QT minimum. This significant reduction was maintained at 6 month follow up and involved the QT minimum as well (Figs. 1 and 2).
4. Discussion
A number of ECG parameters have recently been proposed as a substrate for future development of atrial arrhythmia8 Right sided volume overload and hence atrial arrhythmia are well known long term sequelae of ASD.9 A number of studies emerged to prove the protective effect of either surgical or device ASD closure against these long term sequelae. The majority of these studies involved either adult patients or a mixed group of children and adults and determining the time onset of improvement in electrical remodeling was not the primary focus of these studies.7, 10, 11 We sought not only to determine the protective effect of device closure in an isolated group of children undergoing elective ASD device closure through a prospective study of these electrical substrates but also to detect the onset of improvement in these ECG parameters through recording these ECG changes as early as 24 h post ASD device closure.
In the current study we used P wave duration and P wave dispersion as a substrate for electrical atrial remodeling; this was in agreement with earlier studies which showed a significant increase in these parameters in patients with ASD compared to control groups and suggested a relation between volume overload and ASD size and these electrical substrates.12, 13 Also QT dispersion measured in the current study was previously used as an indicator of electrical remodeling by Kaya et al.7 and Santoro et al.10 in earlier studies.
In the current study 12 lead ECG for 30 patients in the pediatric age group were evaluated before ASD device closure and at 24 h, 1 month and 6 month follow up for P wave duration and dispersion as well as QT duration and dispersion.
There was a significant decrease in P max and P dispersion as early as 24 h post procedure compared to baseline. This decrease was sustained over a follow up period of 6 month. Fang et al.14 demonstrated a significant decrease in P wave dispersion at 3 month follow up post ASD device closure. Santoro et al.9 showed a significant decrease in P wave dispersion post ASD device closure in a small group of adult patients undergoing ASD device closure at follow up period of 6 month despite significant increase in both P max and P min.
There was a significant sustained decrease in QT dispersion and QRS duration over 6 month follow up period, this was in agreement with Santoro et al.10 who showed significant decrease in QT dispersion at 1 month follow up. Kaya et al.7 showed a significant reduction in P min, P max, P dispersion, QRS duration and QT duration over a follow up period of 2 years in a mixed group of adults and children undergoing ASD device closure. However Kaya et al.7 unlike our study showed no significant decrease in the PR interval among their study group.
Although a number of earlier studies sought to study these electrical substrates only few studies applied these measurements in children undergoing ASD closure.11, 15, 16 In contrast to our prospective study, Girgnani et al.11 retrospectively reviewed ECG recordings of their patient. Our follow up started as early as 24 h post ASD device closure to document the earliest change in these electrical parameters while Girgnani et al.11 earliest follow up was 1 week post device closure. Baspinar et al.15 did not study the immediate effect of ASD device closure on P wave dispersion in their study group of 31 children. This study also failed to show a statistically significant reduction in P wave dispersion over a follow up period of 1 year although the values were reduced compared to baseline measurements.
Ozylimaz et al.16 in agreement with our results showed a slight decrease in P wave maximum duration and P wave dispersion as early as 24 h post device closure. However unlike our results this decrease was not statistically significant and the authors did not trace these changes over the follow up period but instead used Holter monitoring to document presence or absence of arrhythmia in the study group at follow up. Also unlike the few studies involving electrical remodeling in children undergoing ASD device closure, the current study included the analysis of not only atrial but also ventricular electrical activity in contrast to studying only P wave duration and P wave dispersion in these studies.
To the best of our knowledge one more study examined the effect of ASD device closure on P wave dispersion one day after the procedure.17 However, Pac et al.17 study had major differences in contrast to the current study, the earlier was a retrospective study involving adult patients undergoing ASD device closure using two different devices and even showed an increase in P max and P wave dispersion immediately post device closure and again like the study of Ozylimaz et al.16 did not follow up these patients to determine the final status of the P max and P wave dispersion over a suitable period of time. Kaya et al.7 although did not study the immediate follow up post device closure postulated that the initial increase in P max and P dispersion suggested by these studies might be due to overstretch of the septum by the effect of the occluder device acting as a foreign body. We used a strict sizing protocol during deployment of the devices in our study group to avoid over sizing and thus decrease the risk of using unnecessary larger devices in our group of children. This protocol might explain why we had a statistically significant decrease in P max and P dispersion as early as 24 h post device closure unlike earlier studies.
Our findings of prolonged QT intervals are frequently observed in children before ASD closure as stated in the literature.18 We confirmed that QT intervals shorten significantly after ASD trans-catheter closure in childhood. This phenomenon might reflect a mechanoelectrical feedback associated with RV volume overload, which has already been mentioned previously in several differently designed studies.19, 20 We assume that with the regression of RV volumes to normal values at longer term follow up this prolongation in QT intervals is going to normalize.
The early significant decrease in the ECG parameters at 1 day follow up in the current study despite the fact that reverse electrical remodeling is supposedly a slow process particularly at the level of the ventricles following hemodynamic changes should be put in the context of our study group. The median age of the study group was 6 years and thus most of our patients were not subjected to RV volume overload for long duration and had significant reduction in this volume overload at follow up which was reflected in the significant reduction in the ECG parameters studied.
4.1. Study limitations and recommendations
The current study focused on the immediate and short term effect of ASD device closure in children on the reversed electrical remodeling in this age group. Similar study involving ASD closure in adults to determine the time onset of improvement in this electrical remodeling should be considered to determine whether delayed ASD closure delay the improvement in electrical remodeling in older patients or not. Long term sequelae of the reversal of electrical remodeling post ASD device closure on the development of atrial arrhythmia through a longer follow up period should also be considered. The aim of these studies should be directed toward establishment of the ideal age for ASD device closure that would achieve best follow up results and least morbidity over longer follow up periods post ASD device closure.
Although none of our patients had abnormal heart rate neither at baseline nor during follow up and we measured QT values without heart rate correction in accordance to earlier studies,7, 10 this led to difficulty in comparing our data concerning the QT measurements with other studies which used heart rate correction especially in older subjects.
The current study could establish that reversed electrical remodeling start as early as one day post procedure. A larger perhaps multi-center study including hundreds of patients of different age groups, different devices and a wide range of ASD sizes should be considered to determine predictors of reversed electrical remodeling with suitable follow up period to determine which patients are going to show normalized values and when this normalization is going to occur.
5. Conclusions
Improvement in electrical remodeling in children under going ASD device closure occurs as early as 24 h post ASD closure. There is also a progressive and sustained improvement in P wave duration, P wave dispersion, QT duration and QT dispersion over short term follow up period of 6 months and thus ASD closure in the pediatric age group is sought to have a protective role against future development of atrial arrhythmias through the reversal of the electrical remodeling associated with the presence of ASD.
Disclosures
The authors of this manuscript have nothing to disclose related to this research. This research was not funded by any funding organization.
Conflict of interest
All the authors of this manuscript have no related conflict of interest to disclose regarding this research.
Footnotes
Peer review under responsibility of Egyptian Society of Cardiology.
References
- 1.Samánek M., Slavík Z., Zborilová B., Hrobonová V., Vorísková M., Skovránek J. Prevalence, treatment, and outcome of heart disease in live-born children: a prospective analysis of 91,823 live-born children. Pediatr Cardiol. 1989;10:205–211. doi: 10.1007/BF02083294. [DOI] [PubMed] [Google Scholar]
- 2.Pascotto M., Santoro G., Cerrato F. Time course of cardiac remodeling following transcatheter closure of atrial septal defect. Int J Cardiol. 2006;112:348–352. doi: 10.1016/j.ijcard.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 3.Ho T.F., Chia E.L., Yip W.C., Chan K.Y. Analysis of P wave and P dispersion in children with secundum atrial septal defect. Ann Noninvasive Electrocardiol. 2001;6:305–309. doi: 10.1111/j.1542-474X.2001.tb00123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guray U., Guray Y., Mecit B., Yilmaz M.B., Sasmaz H., Korkmaz S. Maximum p wave duration and p wave dispersion in adult patients with secundum atrial septal defect: the impact of surgical repair. Ann Noninvasive Electrocardiol. 2004;9:136–141. doi: 10.1111/j.1542-474X.2004.92532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yavuz T., Nisli K., Oner N. The effects of surgical repair on P-wave dispersion in children with secundum atrial septal defect. Adv Ther. 2008;25:795–800. doi: 10.1007/s12325-008-0081-3. [DOI] [PubMed] [Google Scholar]
- 6.Roos-Hesselink J.W., Meijboom F.J., Spitaels S.E. Excellent survival and low incidence of arrhythmias, stroke and heart failure long-term after surgical ASD closure at young age. A prospective follow-up study of 21–33 years. Eur Heart J. 2003;24:190–197. doi: 10.1016/s0195-668x(02)00383-4. [DOI] [PubMed] [Google Scholar]
- 7.Kaya M.G., Baykan A., Dogan A. Intermediate-term effects of transcatheter secundum atrial septal defect closure on cardiac remodeling in children and adults. Pediatr Cardiol. 2010;31(4):474–482. doi: 10.1007/s00246-009-9623-y. [DOI] [PubMed] [Google Scholar]
- 8.Guray U., Guray Y., Yýlmaz M.B. Evaluation of P wave duration and P wave dispersion in adult patients with secundum atrial septal defect during normal sinus rhythm. Int J Cardiol. 2003;91:75–79. doi: 10.1016/s0167-5273(02)00598-3. [DOI] [PubMed] [Google Scholar]
- 9.Santoro G., Pascotto M., Caputo S. Short-term electrogeometric atrial remodelling after percutaneous atrial septal defect closure. J Cardiovascular Med. 2008;9:789–793. doi: 10.2459/JCM.0b013e3282f4c87b. [DOI] [PubMed] [Google Scholar]
- 10.Santoro G., Pascotto M., Sarubbi B. Early electrical and geometric changes after percutaneous closure of large atrial septal defect. Am J Cardiol. 2004;93:876–880. doi: 10.1016/j.amjcard.2003.12.027. [DOI] [PubMed] [Google Scholar]
- 11.Grignani R.T., Tolentino K.M., Rajgor D.D., Quek S.C. Longitudinal evaluation of P-wave dispersion and P-wave maximum in children after transcatheter device closure of secundum atrial septal defect. Pediatr Cardiol. 2015;36:1050–1056. doi: 10.1007/s00246-015-1119-3. [DOI] [PubMed] [Google Scholar]
- 12.Guray U., Guray Y., Mecit B., Yilmaz B., Sasmaz H., Korkmaz S. Maximum P wave duration and P wave dispersion in adult patients with secundum atrial septal defect: the impact of surgical repair. Ann Noninvasive Electrocardiol. 2004;9:136–141. doi: 10.1111/j.1542-474X.2004.92532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fei Ho T., Chia E.L., Chin-Ling W., Chan K.Y. Analysis of P wave and p dispersion in children with secundum atrial septa1 defect. Ann Noninvasive Electrocardiol. 2001;6:305–309. doi: 10.1111/j.1542-474X.2001.tb00123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fang F., Luo X., Lin Q. Characterization of mid-term atrial geometrical and electrical remodeling following device closure of atrial septal defects in adults. Int J Cardiol. 2013;168:467–471. doi: 10.1016/j.ijcard.2012.09.119. [DOI] [PubMed] [Google Scholar]
- 15.Baspinar O., Kervancioglu M., Koruk S., Kilinc M., Irdem A. Follow-up of P dispersion after transcatheter closure of an atrial septal defect in children. J Pak Med Assoc. 2014;64:546–548. [PubMed] [Google Scholar]
- 16.Ozyilmaz I., Ozyilmaz S., Tola H.T. Holter electrocardiography findings and P-wave dispersion in pediatric patients with transcatheter closure of atrial septal defects. Ann Noninvasive Electrocardiol. 2014;19:174–181. doi: 10.1111/anec.12104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pac F.A., Balli S., Topaloglu S., Ece I., Oflaz M.B. Analysis of maximum P-wave duration and dispersion after percutaneous closure of atrial septal defects: comparison of two septal occluders. Anadolu Kardiyol Derg. 2012;12:249–254. doi: 10.5152/akd.2012.069. [DOI] [PubMed] [Google Scholar]
- 18.Rucklova K., Koubsky K., Tomek V., Kubus P., Janousek J. Prolonged repolarization in atrial septal defect: an example of mechanoelectrical feedback due to right ventricular volume overload. Heart Rhythm. 2016;13(6):1303–1308. doi: 10.1016/j.hrthm.2016.01.032. [DOI] [PubMed] [Google Scholar]
- 19.Lab M.J. Mechanoelectric feedback (transduction) in heart: concepts and implications. Cardio Vasc Res. 1996;32:3–14. [PubMed] [Google Scholar]
- 20.Eckhardt L., Kirchhof P., Breithardt G., Haverkamp W. Load-induced changes in repolarization: evidence from experimental and clinical data. Basic Res Cardiol. 2001;96:369–380. doi: 10.1007/s003950170045. [DOI] [PubMed] [Google Scholar]