Summary
Background
The injection of mixture of plain bupivacaine and triamcinolone acetonide into the sacroiliac joint (SIJ) to relieve chronic low back pain is uncommon in the West African sub-region. The objective of this study was to demonstrate the efficacy or otherwise of fluoroscopic-guided SI joint injection in the management of chronic axial low back pain in Nigeria.
Design
This was a prospective observational interventional study
Setting
The study was carried out at a tertiary hospital in Nigeria
Participants
Twenty-six patients with SI joint pain, based on IASP diagnostic criteria, who presented to our unit over 36 months from March 2012 to March 2015 and.
Interventions
Fluoroscopic-guided injections of 5mls mixture of bupivacaine and triamcinolone acetonide into the sacro-iliac (SI) joints of 26 patients with SI joint pain out of 116 patients who were offered different interventions for chronic low back pain. The patients were followed up for year and pain intensity and functional status were assessed at 3-, 6- and 12 months post-intervention.
Main outcome measures
Pain relief and functional improvement were the main outcome measures.
Results
The mean numeric rating score (NRS) and Oswestry Disability index (ODI) score in 14 (53.9%) patients at 12 months post-interventions were significantly lower compared with baseline values; 3.19 ± 1.10 vs 8.54 ±1.14 p=0.000 and 25.35 ± 5.40 vs 37.54 ±8.41, p=0.000 respectively.
Conclusion
Fluoroscopic-guided steroid injection into the SI joint resulted into reduction in pain intensity and improved physical function in the majority of patients with SI joint pain.
Funding
Not declared
Keywords: Axial low back pain, sacroiliac joint, steroid injection, fluoroscopy, pain relief
Introduction
Sacro-iliac (SI) joint is an important source of chronic axial low back pain;1, 2 with frequency of its occurrence increasing with age.2 The joint derives its innervations mainly from the dorsal rami of sacral nerves. Pain originating from the SIJ can be intra-articular, extra-articular or unknown. Intra-articular causes include infection, arthritis, spondyloarthropathies and malignancies while enthesopathy, fractures, ligamentous injuries and myofascial pain constitute the extra-articular causes of SI joint pain.3 Based on the proposed criteria by the International Association for the Study of Pain (IASP), SIJ pain is defined as pain localized in the region of the SI joint, reproducible by stress and provocation tests of SI joint, and reliably relieved by elective infiltration of the joint with local anaesthetic.4
Conservative treatment of SIJ pain with analgesics, as usually the case with other specific causes of chronic low back pain, are ineffective. Consequently, patients continue to experience severe pain, impaired function and associated psychiatric co-morbidities leading to decrease in quality of life. Interventional pain management techniques for specific sub-diagnosis of causes of back pain based on evidence-based practice guidelines have been shown to improve the chances of successful treatment outcome.3
Evidence-based treatments of SI joint pain such as SIJ blocks, radiofrequency denervation's (traditional and cooled), and fusion of the joint, especially following failed conservative management, can ameliorate pain and enhanced function in patients with SIJ-induced pain of diverse aetiologic causes. Availability of such services in health facilities in Sub-Sahara Africa was virtually non-existent until recently.5
Thus, assessing the benefits of SIJ block in patients with SIJ pain would broaden the existing treatment options for chronic low back pain and open new frontiers for research in the management of chronic low back pain in the region. This prospective observational study was conducted over a 3-year period (March 2012–March 2015) to determine the efficacy, safety and acceptability of image-guided sacroiliac joint injections in the management of chronic axial low back pain secondary to SIJ pain among patients with chronic low back pain that presented to our centre.
Methods
After approval from the Ethical Review Committee of University of Ilorin Teaching Hospital, Ilorin (ERCPAN/2014/03/1285), this prospective observational study was carried out in a tertiary health institution in Nigeria, from March 2012 to March 2015, on 26 consecutive patients who met the specific diagnostic criteria of SIJ pain.
Patients enrolled into the study had low back pain that included the region of the sacral sulcus with or without hip or leg symptoms; axial pain of more than 3 months duration; numerical rating scale (NRS) score of 5 at presentation, positive response to at least three widely accepted provocative maneuvers typically used to diagnose SIJ pain, such as the Patrick's test, Gaenslen's test, side-lying iliac compression test, midline sacral thrust, and pressure application to the sacral sulcus while in the prone position; and failure of pain to respond to nonsteroidal anti-inflammatory medications. Pregnancy, systemic infection or localized infection at anticipated point of needle entry, patient's refusal to participate in the study, patients with depression or communication barrier that impedes ability to fulfill study end points, patients with spinal pathology such as scoliosis or spondylolisthesis at L5/S1, symptomatic moderate or severe foraminal or central canal stenosis constituted the exclusion criteria in this study. Under fluoroscopy, 5mls mixture of plain bupivacaine and triamcinolone acetonide was injected into sacro-iliac (SI) joints of all the participants.
Description of the procedure
In the procedure room, patient was connected to a multi-parameter patient monitor to obtain baseline vital signs and periodic cardio-respiratory parameters and venous access was secured.
With patient in the prone position, the C-arm fluoroscope was placed in antero-posterior (AP) position to visualize the L5–S1 disc space at L5–S1 interspace. The widest space at the most inferior aspect of SI joint was identified and the C-arm was angled in cephalad (200) direction until the lines of anterior and posterior aspects of the joint overlapped.
The needle entry point was at the inferior edge (distal 1cm) of the joint and mixture of 1.0 mL of triamcinolone acetonide (6mg/mL) and 3mL of 0.25% plain bupivacaine and 1% of lidocaine hydrochloride was injected intra-articularly into the SI joint under fluoroscopic guidance. Patients were subsequently sent for physiotherapy session, consisting of lumbar stabilization techniques and reconditioning. An additional therapeutic injection was scheduled for each patient. The additional therapeutic injection was nullified if patients admitted to at least an 80% symptom relief 2 weeks after the initial injection. Patients were re-evaluated 2 weeks after the first or second therapeutic injection. Failure to achieve pain relief after two therapeutic injections ruled out another scheduled injection.
Outcome measures
At presentation and before fluoroscopic-guided SIJ block, a baseline numeric rating score (NRS) and Oswestry disability index (ODI) scores were assessed and recorded for each patient. At 3-, 6- and 12 months follow up visits, NRS and ODI were evaluated and the scores were compared with the baseline values. In this study, clinically relevant treatment success was deemed to have been achieved when patients reported a drop in the NRS score ≥2.5 or a reduction in the ODI score of 10 or greater.6,7 The impression of the patients about the treatment was assessed using patients global impression of change (PGIC) according to the following grading: very much improved, much improved, minimally improved and not improved.8
Statistical analysis
The data obtained were analyzed with the Statistical Package for the Social Sciences (SPSS) version 20.0 (SPSS Inc., Chic., Ill.). Means and standard deviations were calculated for continuous variables that described outcomes in the treated patients at baseline, 3, 6, and 12 months. Statistical significance: P < 0.05 using student's paired t-test. Results for proportions are reported as percentages, followed by confidence intervals calculation at the 95% level.
Results
Of the total 116 patients assessed for chronic low back pain, transformational epidural steroid injections, medial branch blocks or both were offered to 96 patients and only 26 met the diagnostic criteria for sacro-iliac joint pain, putting the incidence at 22.4% (26/116) in our centre. The male to female (M:F) ratio was 1.6:1, the age ranged from 42 to 78 years with a mean age of 57.50±10.1. Civil servants, retirees, self-employed, traders, and farmers constituted 50% (13), 19.2% (5), 15.4% (4), 11.5% (2) and 3.9% (1) respectively of the patients who received the intervention. The left SIJ was more affected than the right in more than 70% (19) of the patients; duration of low back pain was greater than 6 months in 76.9% (20) of the patients and the pain was localized in the gluteal region in 69.2% (18) of the patients, Table 1.
Table 1.
Patients baseline characteristics and sites of pain
| Variables | Mean (SD) | Min-Max | N (%) |
| Duration of LBP (years) | 2.62 (1.39) | 1–3 | |
|
Mean pain intensity (NRS) |
8.54 (1.14) | 6–10 | |
| Disability | |||
| Oswestry Disability Index % (SD) |
37.5 (8.4) | 25–56 | |
| Analgesic use | |||
| PCM+NSAIDs | 22 (84.6) | ||
| PCM | 2 ()7.7 | ||
| Opioids | 2 (7.7) | ||
| Pain site | |||
| Right SIJ | 7 (26.9) | ||
| Left SIJ | 19 (73.1) |
NRS, Numeric rating scale; LBP, low back pain; ODI, oswestry disability index; PCM, paracetamol
More than two-thirds of the patients, 22 (84.6%), were placed on oral paracetamol and non-steroidal anti-inflammatory drugs (NSAIDs) without desirable pain control and functionality, Table 1. At presentation, the mean pain intensity and functional disability scores, assessed by NRS and ODI, were 8.54±1.14 and 37.34±8.44 respectively, Table 1.
The mean baseline values and mean 6 months values of NRS and ODI were 8.54 ± 1.14 and 37.5 ± 8.4 versus 4.15 ± 1.1 and 27.4 ± 7.8 respectively. The mean 6 months changes in NRS and ODI from the baseline values were 4.4 ± 1.2 and 10.1 ± 5.0, and this indicated significant reductions in the mean NRS pain intensity and mean ODI score at 6 months follow up after the interventions. Similarly, the mean baseline values and mean 12 months values of NRS and ODI were 8.54 ± 1.14 and 37.5 ± 8.4 versus 3.19 ± 1.1 and 25.0 ± 5.4 respectively.
However, only the difference in the mean ODI score reached statistical significance when the parameters were compared at 3- and 12 months post-treatment; 4.4 ± 5.3 versus 25 ± 5.4, p=0.000.
Mean NRS pain intensity scores declined by 5.9±1.6, 4.4±1.2 and 5.4±1.5 points from baseline in 20 (77%), 16 (62%) and 14 (54%) of the patients respectively at 3-, 6-, and 12 months after interventions. Similarly, functional status of patients improved significantly with mean ODI scores changes of 13.2±7.0, 10.1±4.9 and 12.2±6.1 at 3-, 6-, and 12 months post intervention respectively. At the end of 12 month follow up, 22 (84.6%) of the patients were very satisfied with the treatment and the PGIC in the same percentage of patients was much improved on the patients global impression of change (PGIC) assessment scale.
Discussion
The findings demonstrated that fluoroscopic-guided sacroiliac joint injections with local anaesthetic and corticosteroid are effective and safe in the treatment of patients with SIJ-induced chronic axial low back pain.
Majority of the patients achieved statistically significant and clinically relevant pain control and improved function (mean NRS and ODI changes at 12 months from the baseline values were 5.4 and 12.2 respectively, p<0.05.
Outcome measures are deemed clinically relevant when a study established an 18 to 19mm reduction in visual analog scale (VAS)-based pain score or a 10-point improvement in the ODI6 in the setting of chronic pain setting; whereas a 3.5 to 4.7 point reduction in pain should be achieved in the setting of acute pain.7 Recommended management approach for SI joint pain are conservative treatments such as analgesics, cognitive-behavioural therapy, exercise therapy rehabilitation, and when indicated, psychiatric assessment as well as interventional pain techniques.3
Intra-articular SIJ injection and radiofrequency neurotomy of nerves that supply the joint are the appropriate pain techniques when conservative management failed or only produced short term pain relief. Cooled radio-frequency treatment of the lateral branches of S1 to S3 (S4) should precede pulsed RF procedures which target L5 dorsal ramus and lateral branches of S1 to S3.3,9 In accordance with the recommended treatment guidelines, this study explored the efficacy and safety of intra-articular SI joint injections in 26 patients with diagnosed chronic low back pain secondary to SI joint pain.
The results of this study are consistent with the outcomes of similar controlled studies 10,11 that established the beneficial effects of intra- and extra- articular injections. Luukainen and co-workers10 observed significant reduction in pain intensity in patients who were treated with intra-articular local anaesthestic and corticosteroid compared with the local anaesthetic and saline group one month after intervention. This study and Luukainen's work delivered the local anaesthetic and corticosteroid into the SIJ intra-articluarly with similar satisfactory pain relief in the enrolled patients.
Unlike Luukainen's work however, this study lacked a control group and the patients were followed up for up to a year. Similarly, Maugars and co-workers11 reported pain reduction of >70% in 5 of the 6 SI joints one month after intra-articular corticosteroid injection; whereas no benefit was observed in the placebo group (7 SI joints) injected with normal saline. The follow ups in the Maugars and group's study and the present study were of equal duration and the intervention produced comparable pain control in nearly equal number of patients in the two studies at the end of 6-month pain evaluation, 58% vs 54%.
Though we delivered the medications intra-articularly, two double-blind studies have demonstrated the effectiveness of peri-articular infiltrations to provide shortterm pain relief.12,13 Therefore, peri-articular infiltration of approach can be used in case of difficult intra-articular injection due to severe sacroilitis or presence of extra-articular causes of SI join pain.10,14 As noted in the previous studies cited above, there was no observed or reported major complication (s) such as intravascular uptake of the medications after the intervention apart from discomfort at the point of needle entry.
Sacroiliac joint injection is effective and safe in patients with chronic axial low back pain secondary to sacroiliac joint pathology; and this study has proven the clinical benefit of the procedure due to the prolonged duration of pain relief in 50% of the patients at the end of 12-month post-intervention. The impressions of the patients about the offered treatment was evaluated using PGIC and the responses were similar to the results obtained in a previous case report15 that examined the clinical benefits and hindrances of facet radiofrequency procedure for chronic low back pain carried.
The observed good impression of responses in the patients can be used as a surrogate to measure the acceptability of the intervention.
Conclusion
Overall, good pain control, improved physical functioning and reduction in analgesic consumptions were achieved in (14) 54% of the patients at the end of one year follow up. The discomfort of frequent ingestions of analgesics was reduced and compliance with medications enhanced. Attempting to use analgesics such as NSAIDs to achieve pain control for the same duration as offered by SIJ block in this study may increase the tendency to develop NSAIDs toxicity, especially in the elderly patients on steroid or those with co-morbid medical conditions like peptic ulcer disease. Fluoroscopic-guided SI joint injection is an effective, safe and acceptable treatment modality in patients with low back pain emanating from sacroiliac joint after failed conservative management.
The limitations of this study included small sample size, lack of control group and failure to do diagnostic intra-articular sacroiliac joint block before the therapeutic injections with local anaesthetic and corticosteroid.
Figure 1.
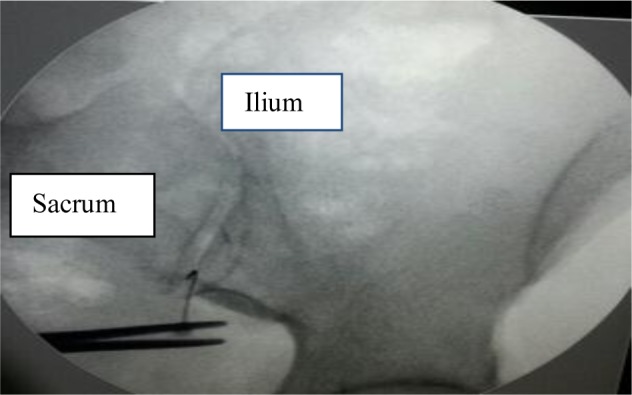
Sacroiliac joint injection (PA view), needle is positioned at the inferior margin of the joint
Figure 2.
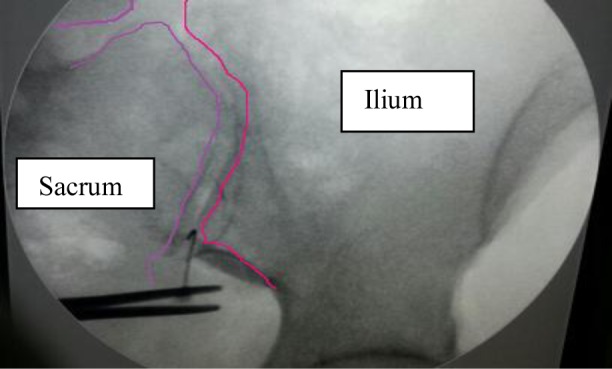
The medial edge of ilium and lateral edge of sacrum are outlined in pink and purple respectively
References
- 1.Yin W, Willard F, Carreiro J, Dreyfuss P. Sensory stimulation-guided sacroiliac joint radiofrequency neurotomy: technique based on neuroanatomy of the dorsal sacral plexus. Spine. 2003;28:2419–2425. doi: 10.1097/01.BRS.0000085360.03758.C3. [DOI] [PubMed] [Google Scholar]
- 2.DePalma MJ, Ketchum JM, Saullo T. What is the source of chronic low back pain and does the age play a role? Pain Med. 2011;12:224–233. doi: 10.1111/j.1526-4637.2010.01045.x. [DOI] [PubMed] [Google Scholar]
- 3.Van Kleef M, Mekhail N, van Zundert J. Evidence-based guidelines for interventional pain medicine according to clinical diagnoses. Pain Pract. 2009;9:470–478. doi: 10.1111/j.1533-2500.2009.00297.x. [DOI] [PubMed] [Google Scholar]
- 4.Cohen SP. Epidemics, evolution and sacroiliac joint pain. Reg Anesth Pain Med. 2007;32:3–6. doi: 10.1016/j.rapm.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 5.Suleiman Z, Burton AW. Introducing interventional pain services in a large African teaching hospital: challenges and opportunities. Pain Pract. 2013;13(8):663–666. doi: 10.1111/papr.12032. [DOI] [PubMed] [Google Scholar]
- 6.van der Roer N, Ostelo RW, Bekkering GE, van Tulder MW, de Vet HC. Minimal clinically important change for pain intensity, functional status, and general health status in patients with nonspecific low back pain. Spine. 2006;31:578–582. doi: 10.1097/01.brs.0000201293.57439.47. [DOI] [PubMed] [Google Scholar]
- 7.Hagg O, Fritzell P, Nordwall A, Swedish Lumbar Spine Study Group The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12:12–20. doi: 10.1007/s00586-002-0464-0. [DOI] [PubMed] [Google Scholar]
- 8.Dworkin RH, Turk DC, Farrar JT, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113:9–19. doi: 10.1016/j.pain.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Patel N. Twelve-month follow-up of a randomized trial assessing cooled radiofrequency denervation as a treatment for sacroiliac region pain. Pain Pract. 2016;16(2):154–167. doi: 10.1111/papr.12269. [DOI] [PubMed] [Google Scholar]
- 10.Luukkainene R, Wennerstrand PV, Kautianinen HH, Sanila MT, Asikainen EL. Efficacy of periarticular corticosteroid treatment of the sacroiliac joint in non-spondyloarthropathic patients with chronic low back pain in the region of the sacroiliac joint. Clin Exp Rheumatol. 2002;20:52–54. [PubMed] [Google Scholar]
- 11.Maugars Y, Mathis C, Berthellot JM, Charlier C, Prost A. Assessment of the efficacy of sacro-iliac corticosteroid injections in spondyloarthropathies: a double-blind study. Br J Rheumatol. 1996;35:767–770. doi: 10.1093/rheumatology/35.8.767. [DOI] [PubMed] [Google Scholar]
- 12.Manchikanti L, Singh V, Pampati V, Damron KS, Barnhill RC, Beyer C, et al. Evaluation of the relative contributions of various structures in chronic low back pain. Pain Physician. 2001;4:308–316. [PubMed] [Google Scholar]
- 13.Van der Wurff P, Buijs EJ, Groen GJ. Intensity mapping of pain referral areas in sacroiliac joint pain patients. J Manipulative Physiol Ther. 2006;29:190–195. doi: 10.1016/j.jmpt.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 14.Borowsky CD, Fagen G. Sources of sacroiliac region pain: insights gained from a study comparing standard intra-articular injection with a technique combining intra- and peri-articular injection. Arch Phys Med Rehab. 2008;89:2048–2056. doi: 10.1016/j.apmr.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 15.Suleiman ZA, Kolawole IK, Bolaji BO, Soyannwo OA, Burton AW. Clinical benefits and hindrances of Facet Radiofrequency procedure for chronic low back pain. A report of two cases. NJOT. 2013;12(2):124–127. [Google Scholar]


