Abstract
Objectives
In recent years, Bangladesh has made remarkable advances in health outcomes; however, the benefits of these gains are unequally shared among citizens and population groups. Dalits (jaat sweepers), a marginalised traditional working community, have relatively poor access to healthcare services. This study sought to explore the sociopolitical and cultural factors associated with health inequalities among Dalits in an urban setting.
Design
An exploratory qualitative study design was adopted. Fourteen in-depth interviews, five focus group discussions and seven key informant interviews were conducted. The acquired data were analysed using an iterative approach which incorporated deductive and inductive methods in identifying codes and themes.
Settings
This study was conducted in two sweeper communities in Dhaka city.
Participants
Participants were Dalit men and women (in-depth interviews, mean age±SD 30±10; and focus group discussions), and the community leaders and non-governmental organisation workers (key informant interviews).
Results
The health status of members of these Dalit groups is determined by an array of social, economic and political factors. Dalits (untouchables) are typically considered to fall outside the caste-based social structure and existing vulnerabilities are embedded and reinforced by this identity. Dalits’ experience of precarious access to healthcare or poor healthcare is an important manifestation of these inequalities and has implications for the economic and social life of Dalit populations living together in geographically constrained spaces.
Conclusions
The provision of clinical healthcare services alone is insufficient to mitigate the negative effects of discriminations and to improve the health status of Dalits. A better understanding of the precise influences of sociocultural determinants of health inequalities is needed, together with the identification of the strategies and programmes needed to address these determinants with the aim of developing more inclusive health service delivery systems.
Keywords: caste, Dalit, qualitative method, sociocultural determinants, health inequalities, untouchability
Strengths and limitations of this study.
This study used the ‘Commission on Social Determinants of Health Conceptual Framework’ proposed by the WHO which allows us to investigate how a set of social, cultural, economic and political elements interacts and plays a determining role in shaping Dalits’ health status.
To the best of our knowledge this is the first study that comprehensively examines how sociocultural and political elements are interconnected, and how they produce, sustain and reinforce health inequality among the Dalit population in Bangladesh.
To analyse the qualitative data we used an iterative approach which blended deductive and inductive methods to identify and generate codes and themes.
The main limitation is that the sample size is unavoidably small; therefore, the generalisability of the findings to other areas might be limited due to the contextual characteristics. Nonetheless, considering the data collected, we believe that this study provides an in-depth understanding of the determinants of health inequalities among Dalit population in Bangladesh.
Background
In recent years, Bangladesh has achieved remarkable progress in terms of health targets, with declining maternal and neonatal mortality rates, increased immunisation coverage, greater life expectancy at birth and increased vitamin A supplementation.1 2 However, these advances are experienced unequally across the population, often leaving behind individuals and communities that are economically marginalised and socially excluded. Improved health services, especially those provided by the state, are not yet effectively distributed to all individuals and groups, and frequently fail to reach ethnic minorities, people living in remote areas, extremely poor individuals, slum and pavement dwellers and other marginalised groups.3 This paper focuses on analysing the healthcare barriers experienced by one marginalised group, the Dalits, the untouchables.
Clifford4 explains that the word ‘Dalit’ comes from the Marathi language and means suppressed, ‘broken up’, downtrodden or oppressed, and the term was first used by Dr BR Amdedkar during the late period of British colonial rule. The Dalits of Bangladesh are a marginalised group whose identity is often characterised by the manual and low-status nature of their occupations. This identity and social status are strongly associated with their ancestral occupations, which were typically considered unclean and impure. In the 1872 census conducted in Bengal, the majority of Dalits were referred to by the term Chandala, a Sanskrit word for someone who deals with the disposal of corpses, a Hindu outcaste. In 2017 they are often called Harijan, a term coined by Mahatma Gandhi meaning ‘children of God’, or more commonly referred to by their occupation, family descent, ethnicity or derogatory terms. The Dalits often engage in sweeping activities, such as cleaning latrines, removing rubbish, skinning cattle and sweeping streets and houses. They scavenge in Bangladesh’s cities and towns, and are designated as ‘untouchable’ within the caste system of the Indian subcontinent.5 6
Healthcare issues of the Dalit population in Bangladesh remain largely neglected in the national government’s development agenda,7 8 despite its strong constitutional commitment to ‘not discriminate against any citizen on grounds only of religion, race, caste, sex or place of birth’ (The Bangladesh Constitution of 1972, Article 28 (1)). Although available literature9–11 (ie, Bangladesh Demographic and Health Survey, Bangladesh Urban Health Survey) does not present nationally representative demographic and survey data to demonstrate how extensively the healthcare access, and health and nutritional outcomes differ statistically between Dalit and other non-Dalit population in Dhaka city, some study reports indicate that Dalits have poor health outcome across the population in slum and other settings.12–15 For example, Nagorik Uddyog (Bangladesh Dalit and Excluded Rights Movement) notes:
Health surveys and research programmes undertaken with respect to the ‘public health situation’ in the country do not pay special attention to the child and maternal health conditions in the colonies and settlements where Dalit communities live. Because of this non-attention to their specific health situation, their suffering and specific requirements to access non-discriminatory and affordable health care remain unreported and unattended to.15
Chowdhury reported that Dalits are generally afflicted by skin diseases, diarrhoea, tuberculosis and pneumonia at a higher level than the non-Dalit population.13 Islam and Parvez14 reported that waterborne diseases are highly prevalent among Dalit population as water and sanitation facilities are scarce in the slum—with reports of nearly 12 000 Dalits sharing two water points in Dhaka, and nearly 58% of Dalits have no access to sanitary latrine.13 A study conducted outside the capital city found that in a Dalit community in Jessore city around half of preschool children were suffering from chronic stunted (58%) and underweight (45%), while nationally the corresponding figure is 36% and 33%.12 16 While no precise official statistics are available regarding the number of Dalits, various sources estimate the population at around 5.5 million,17 approximately 3%–4% of Bangladesh’s total population. The lack of official data on this population group indicates the lack of political will to recognise Dalits and the existence of these communities in Bangladesh.
Prior studies indicate that health inequalities are determined by broader societal factors, such as socioeconomic position, housing conditions, working environment, poverty, access to and control of resources, education and employment.18–22 A firm understanding of sociocultural determinants of health inequalities, and also of the factors which restrict access to health services, is critical to improving the health outcomes of marginalised communities.23 Several studies in Bangladesh have highlighted the socioeconomic issues and discrimination encountered by the Dalit population; however, the sociopolitical and cultural factors that contribute to generating severe health inequalities remain largely unexplored.
This present study therefore explores the political, social, economic and cultural determinants of health inequalities experienced by the majority of the Dalit population. We examine how caste-based positions generate and reinforce social stratification in society, and determine health inequities within two Dalit population groups in Bangladesh. We argue that health inequalities need to be viewed from a holistic perspective, keeping in mind the intersecting social, political and structural factors.
Materials and methods
Conceptual framework
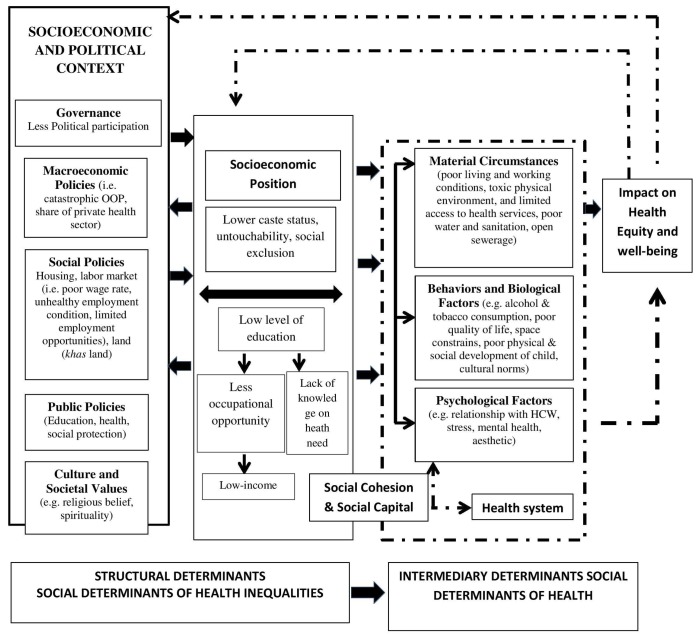
Our research was shaped by the ‘Commission on Social Determinants of Health (CSDH) Conceptual Framework’ proposed by the WHO in 2010.24 This framework offers a dynamic analytical configuration of the key social institutions and political structures that affect and shape the health of a population. It explains health status as a social phenomenon that is produced, configured and sustained through a complex and dynamic interplay of a set of context-embedded factors. Importantly, it also emphasises the need to distinguish the mechanisms that generate and reproduce social hierarchies and their multiple manifestations. The conceptual framework includes three interactive levels of dynamic influences: the wider sociopolitical context, individual socioeconomic position and intermediary socioeconomic influences.
The first level, the sociopolitical context, focuses on the social relationships within a society which organise and configure hierarchies and social stratification by defining individual positions and roles. This includes the labour market, the educational system and political institutions. The second level considers individual or groups of individuals’ positionality in relation to these macrostructures and mechanisms. It understands individual socioeconomic position as a function of the degree of exposure to health risks and vulnerabilities that result in differential health outcomes for an individual and/or a population. Key individual socioeconomic characteristics include income, education, occupation, level of knowledge and information. Combined with structural elements, these form what is referred to as ‘structural determinant’. Thus, structural determinants shape patterns of access to resources (eg, health services) and are rooted in socioeconomic institutions, policies and political context that construct, reinforce and maintain social hierarchies in various social systems, institutions, policies and sociocultural values.
The intermediary socioeconomic context refers to a circumstance where an individual and/or group have a distinct experience of materials, behavioural options, psychological supports and healthcare facilities that consecutively shape specific determinants of health status (intermediary determinants). Therefore, this framework summarises and synthesises the view that social determinants of health inequality are constructed, functioning and sustained through the act of long causal interceding factors (figure 1).
Figure 1.
Commission on Social Determinants of Health (CSDH) Conceptual Framework (adapted from the WHO (2010)) (to be placed). HCW, healthcare worker; OOP, out-of-pocket.
Although other frameworks have been developed to understand the social determinants of health, we found this conceptual framework particularly useful for exploring the dynamic relationships between social structures and political determinants of health inequalities. Several contemporary models, for example, the psychosocial, social production of diseases/political economy of health, and the ecosocial models, tend to explain disease distribution rather than focusing on the mechanism of disease causation.25–28 Therefore, in contrast to the WHO model, these frameworks leave contextual and sociopolitical aspects of health inequalities largely unexplored. The results presented in this paper are provided together with an exploration of the socioeconomic settings following the CSDH Conceptual Framework.
Study population and settings
This study was conducted in two sweeper communities in Dhaka city: the Agargaon Public Works Department Sweeper Colony, which is located adjacent to Dhaka Orthopaedic Hospital, and the Ganaktuli sweeper colony located in the city’s Hazaribagh area. Commonly, the sweepers in Agargaon and Ganaktuli are known as Telegu and Kanpuri, respectively. There are no official statistics providing precise population figures for these colonies, although secondary sources indicate that each includes approximately 1000 families.17
Sampling strategy
Between August and October 2014 the first author conducted interviews and focus group discussions (FGD, henceforth) with members of these Dalit colonies. We applied an inclusion criterion—that participants were aged 18 and above and volunteered to participate—and purposively recruited the study participants to address the research objectives. In this process, we invited individuals who showed a proactive interest to share their experiences, opinions and time. Using several data collection tools, we purposefully collected data from participants with various backgrounds (eg, different age groups, occupations, genders, position within the households, status within the community (leaders) and members of non-governmental organisations (NGO), henceforth). In this process, we achieved maximum variation among the participants.29
We conducted 14 in-depth interviews (IDI, henceforth) with household members from the Dalit community who had sought healthcare in different public and private facilities. We invited individuals to open group discussions on health status and health-seeking behaviour, and invited those individuals who showed a proactive interest in the study for interviews (IDIs, FGDs). The context in which the research was conducted required a high degree of iteration and flexibility in order to build coherence and maximise the validity of the data collected. For example, as part of the sampling strategy, a subtype of purposive sampling known as snowballing or chain sampling30 was used to select individuals who had experienced discrimination of a specific nature or means.
We also conducted seven key informant interviews (KII, henceforth) with community and religious leaders, and also NGO workers, in order to better understand the exclusion process experienced by Dalits in these specific locations. Finally, we conducted five FGDs to help understand communal perceptions and attitudes regarding entitlement to access basic public services. We have selected the key informants on the basis of two criteria—information depth (who have rich/depth information about the Dalit health aspect), and voluntary participation (who are willing to participate in the interview voluntarily). In case of selecting FGD participant we considered age, gender, occupation and volunteer participation. In addition, the authors used participant observations and informal conversations with some non-Dalit (converted Muslim) individuals who lived in the area to further understand the dynamics at play. Many of these informants operated small businesses (eg, tea stall, plastic shop, video game shop, and so on) within and around the sweeper colonies. Finally, we revisited the participant groups to triangulate the emerging themes and cross-check the accuracy of the data collected. The data collection process ceased when the authors reached a suitable understanding of the key specific historical, sociocultural belief systems influencing the process of discrimination, marginalisation and stigmatisation.31 32
Data collection procedure
In order to gather information in a semistructured and systematic manner, we developed an interview schedule. This document was used to guide conversations around key dimensions relevant to our research questions and objectives, including socioeconomic, demographic and political issues that impact on health conditions among the Dalit population and/or individuals. Interviews were semistructured in order to create a friendly rapport with respondents and leave sufficient space for other themes to emerge. Open-ended questions were used to explore the sociopolitical and economic factors affecting their health services. For example, we wanted to learn more about participants’ healthcare-seeking behaviours, experiences when attempting to access healthcare facilities, health information and interactions with healthcare workers.
We conducted all except one of the interviews and FGDs in Bengali, a language spoken by the researchers (first author) and most of the participants, while an interpreter was used to interview elderly Dalit men and women who only spoke Telegu and Hindi. On average, IDIs lasted 45–60 min and FGDs between 90 and 120 min. After obtaining the participants’ consent, IDIs and FGDs were electronically recorded, before being transcribed verbatim and subsequently translated into English. In some cases, several follow-up visits were made to obtain missing information, as well as to enable further probing of some issues. In addition, the authors took detailed field notes during the conversations.
Data analysis
To analyse the qualitative data we used an iterative approach which blended deductive and inductive methods to identify and generate codes and themes. Initially, a deductive approach was used through the use of interview guides, which provided a primary template for the framework of data coding. The researchers independently read and reread a few transcripts and identified codes which were incorporated into the coding framework in an inductive form which mirrored the ideas, perceptions, practices and concepts, concentrating on the health and health services of the participants. After coding all of the interviews we looked for clusters of several codes, which were termed ‘themes’ or ‘concepts’. Focusing on rigour-related criteria in qualitative research, such as credibility, transferability, dependability and conformability, a consensus was established by resolving coding differences after discussions among the research team. Throughout the analysis, systematically examined meaningful statements were assigned to the relevant code, and the relationship between the themes was then examined.33 The analysis process was adequately accomplished by the team of researchers, who have different educational backgrounds and training, through regular collaboration and discussions, self-reflexivity and triangulation of method and context (field sites), ensuring that no one researcher’s view was predominant.
Patient and public involvement
In this study we did not involve any patients. The participants were not directly involved in the design and conception of the study. However, we have plans to disseminate the results of this study with the study participants.
Ethical considerations
The study protocol was approved and ethical approval was obtained from the ‘ethics review committee’ at Dhaka University, Bangladesh. Written informed consent was taken and documented via audio recording. Before obtaining consent the research objectives were explained, together with the importance of the study, confidentiality rules, possible harms and benefits and the participants’ right to withdraw from the interviews at any stage during the conversation. Personal and household information, including age, sex, education, occupation, marital status, family composition and religion, was collected; however, the confidentiality of the personal identification (ID) of all participants was strictly maintained, with these details only being used by the researchers. Data were analysed using the participant ID number only and these ID numbers were removed prior to reporting the findings.
Results
Characteristics of the participants
We first describe the sociodemographic characteristics of the participants before presenting our results. Table 1 shows the characteristics of the study participants, who ranged in age from 22 to 64, and had a mean age of 30 (SD±10) years. More than half of the participants (9 out of 14) had received no formal schooling, which is far below the national level of over 60%. Overall, participants had received a mean of 2.9 (SD±1.3) years of schooling, and only three had received any education above the primary level.
Table 1.
Sociodemographic backgrounds of the in-depth interview participants (n=14)
| Characteristics | Study area | Combined | |
| Agargaon | Ganaktuli | ||
| Age in years (mean±SD) | 27±8 | 3±9 | 30±10 |
| Education | |||
| 1–5 years (n) | 1 | 2 | 3 |
| 6–10 years (n) | 0 | 2 | 2 |
| No formal schooling (n) | 5 | 4 | 9 |
| Schooling in years (mean±SD) | 2.6±1.2 | 3.4±1.4 | 2.9±1.3 |
| Occupation (n) | |||
| Cleaning | 3 | 5 | 8 |
| Housewife | 2 | 1 | 3 |
| Others | 1 | 2 | 3 |
| Sex (n) | |||
| Male | 4 | 4 | 8 |
| Female | 2 | 4 | 6 |
| Marital status (n) | |||
| Married | 4 | 5 | 9 |
| Unmarried | 2 | 2 | 4 |
| Divorced | 0 | 1 | 1 |
| Family type (n) | |||
| Extended | 4 | 6 | 10 |
| Nuclear | 2 | 2 | 4 |
| Religion (n) | |||
| Hindu | 5 | 8 | 13 |
| Converted Christian | 1 | 0 | 1 |
The majority of the participants were engaged in cleaning activities for Dhaka City Corporation and private organisations, while the remainder were employed in household activities, as day labourers, or in garment factories. More than half of the participants (10 out of 14) lived with their extended family, and almost all (13 out of 14) were Hindu, with just one participant having converted to Christianity.
Table 2 presents the key demographic characteristics of the FGD participants. Five FGDs were conducted: (1) among six Agargaon Dalit men (mean age 28, SD±8 years); (2) among seven Agargaon Dalit women (mean age 32, SD±7 years); (3) among six Ganaktuli Dalit men (mean age 39, SD±7 years); (4) among eight female Ganaktuli Dalit women (mean age 24, SD±5 years); and (5) among nine Ganaktuli Dalit men (mean age 35, SD±6 years).
Table 2.
Sociodemographic backgrounds of participants in the focus group discussions (n=36)
| Focus group discussion | Age of the participants in years (mean±SD) | Location | Participants (n) | Gender |
| I | 28±8 | Agargaon | 6 | Male |
| II | 32±7 | Agargaon | 7 | Female |
| III | 39±7 | Ganaktuli | 6 | Male |
| IV | 24±5 | Ganaktuli | 8 | Female |
| V | 35±6 | Ganaktuli | 9 | Male |
The dominant recurring themes were organised into categories reflecting the majority of interactive elements of the ‘social determinants of health’ framework (ie, socioeconomic and political context (including governance, macroeconomic policies, social and public policies, culture and societal values, untouchability, caste-based discrimination and social exclusion), socioeconomic position and intermediary determinants).
Space and power
In an attempt to contextualise our findings within the wider socioeconomic and political context, this section starts by providing a brief overview of the political history of the Dalit population. Accounts of the sociopolitical and economic dimensions of Dalit livelihoods help in understanding structural determinants of their health.
In Bangladesh, the majority of untouchable Hindu Dalits have Indian origins. In Bangladesh, as in India and Nepal, untouchable Hindus belong to the lowest social position at the base of the Varna system.6 During the reign of the Mughals, Dhaka was established as the commercial capital of the Bengal Subah by Subahdar (viceroy) Islam Khan in 1608. As the city grew to become one of the wealthiest and most prosperous cities in the South Asian region, the Mughal administrator appointed sweepers to maintain sanitation and cleaning activities.5 In the 1620s there was a large-scale migration of Dalit from India to Dhaka, which was precipitated by massacres by Burmese pirates in 1624–1626: they were required to remove dead bodies from the city.8 It is commonly believed that a large number of Dalits were brought to the city by British colonial administrators after Dhaka gained municipality status, to provide menial services.8 During the period of British colonial rule (1757–1947), Dalits (Telegu-speaking and Kanpuri sweepers) were brought to East Bengal (now Bangladesh) from the Indian states of Uttar Pradesh, Bihar, Andhra Pradesh and many other areas, including Bhagalpur, Motihari, Baliha, Patna, Maddaparpur, Uriya, Gorakhpur and Chapra.5 13 As the English administration rapidly developed townships and local municipalities, these populations were moved to meet the increasing need for sanitation workers.
The social position and status of Dalits are associated with their ancestral occupations, which were regarded as impure. Dalits are mostly employed by public and private organisations for sweeping activities, cleaning latrines, removing filth, skinning cattle, sweeping streets and houses. Despite the lack of official data on the economic condition of Dalits, some secondary sources claim that Dalits are engaged in low-paid manual work under severe discriminatory terms,13 and consequently earn much less than national average, with one source claiming that their income lies between BDT3000 and BDT5000 (considering BDT78=US$1) while the national average is BDT7203.13 Processes of occupational discrimination and unfair payment contribute to excluding the population from secure and safe dwellings. Dalit populations usually reside in unhygienic environments characterised by poor quality, insufficient and irregular water, electricity and gas provision. Overcrowded dwellings, narrow walkways and inadequate basic facilities, such as toilets and water taps, represent significant everyday challenges that become causes of further stigmatisation and marginalisation. Dalit populations often have to rely for access to these services on middlemen and informal brokers, called mastan (local thugs); they often rely on violence and illegal deals to negotiate access to resources. The interlacing of social structures and political processes shape the Dalits’ common everyday experiences of poverty and constitute their shared identity.
The material circumstances of the Dalit group in Dhaka city were identified as major intermediary determinants of their health status. Data from all this study’s sources (eg, IDIs, FGDs and KIIs) reported poor living conditions, their concentration in government-established slums, or so-called ‘colonies’, and their highly unsafe housing characterised by poor drainage, sanitation and water supply. Houses in government colonies had brick walls and corrugated iron sheet roofs, while those in private slums were constructed from bamboo, tin and wood. The sweeper slums were very overcrowded, with most respondents reporting that one small room housed 6–10 family members spanning three generations. The environment was also highly polluted, leading to extremely unsafe living conditions.
Sweeper slums also reported extremely unhygienic and inadequate sanitation conditions.14 Bacteria, parasites and disease vectors breed faster when sanitation and drainage systems are poor and when warmer and wetter conditions are prevalent all year round. Such poor living conditions are likely to increase the incidence of vectorborne/waterborne diseases and infections.13 34 For example, diarrhoea and respiratory infections, such as pneumonia, were commonly reported as the most frequent diseases among children aged less than 5 years old.13 In addition, malaria, dengue fever and kala-azar (visceral leishmaniasis) were reported to be prevalent among all age groups.
The wider sociopolitical context influences the effects of these material circumstances and has multiple behavioural implications. The data collected from KIIs, IDIs and FGDs clearly indicate that health policies largely ignore the specific needs of Dalits. For example, policies concerning housing, the labour market and land emerged as restricting factors for health. Over centuries, Dalit populations have been allocated space in designated colonies, and Dalit families have shared very small living spaces from generation to generation. Data from all the sources reflected that, despite the potential for promoting basic housing facilities within the government-owned land, effective initiatives were never taken due to the lack of policy support. The respondents related that government policy favoured congregating Dalits in such designated colonies, rather than facilitating actions for housing supply and availability, and improving quality. One participant reported:
Government policy has never allowed any action that facilitates housing facilities for Dalit. They are living like this in colonies for generations; but, neither own nor improve its quality. (A key informant in Ganaktuli)
Although the government has issued policy statements and strategies for the redistribution of non-agriculture and agricultural khas land (government-owned fallow land) to landless people since the early 1980s, Dalits have not been considered as a potential beneficiary group. More than half of the participants reported that Dalits lack political power to influence the policy aspects in this regard. One of the participants stated:
You will see very minimal or no action taken from the govt to solve the housing problem of Dalit. I understand govt can take necessary initiatives easily but it does not take so. Why? I believe, Dalit has no power to influence govt policy aspects. (A 46-year-old man in Ganaktuli)
Therefore, the scope for improving health outcomes through facilitating housing conditions for Dalits in allocated khas land is constrained by government land policy. One respondent stated:
Landlessness is the first and foremost problem that impacts the overall wellbeing of Dalit. Dalit living conditions are beyond description. But it can be improved through distributing khas land to Dalit as it is provided to landless people. But, it is a matter of fact that Dalit cannot fill in the inclusion criteria set by the policy. (A key informant in Agargaon)
Furthermore, the participants, especially the community leaders and NGO workers, believed that the lack of government interventions restricted the potential for improving living conditions, which also affected the health status of the population.
Education and labour
An individual’s place in a given society can be described by the concept of ‘social position’, as proposed by Evans et al,35 which is generated and maintained under a broader social context. The social position of an individual is dynamically created by a number of elements, such as caste, religion or gender, which transmit intergenerational discriminations and inequalities. Similar to what Evans et al argue, when interviewing the participants we found that Dalits’ health can be seen as an outcome that is generated from social position, where an individual and/or group are unable to fully participate in society because of their sociocultural identity. The socioeconomic context has shaped Dalits’ engagement with educational institutions; Dalits face discrimination and are often deprived of education through various means. Our data found that less than 30% of Dalits had received formal schooling, compared with more than 65% of the national population. This figure tends to be even lower outside Dhaka city, as one respondent reported:
In Dhaka city you will find higher number of Dalit who have schooling especially among the younger generation. But, the figure will drastically fall if you consider among the whole number of Dalit across the country. (A Dalit activist and key informant from Ganaktuli)
Respondents reported that their children faced discrimination by educational institutions, for example, being denied admission to private schools, rejection and teasing by teachers or students. The school enrolment of Dalit girls has also decreased due to the practice of child marriage, which subsequently affected sexual and reproductive health. The very low literacy rate among Dalits resulted in little or no access to health information. One of the key informants reported:
Education is vital for improving health and general well-being. When an individual lacks education, he/she eventually will be in a worse position to negotiate access to services and information such as nutrition. Low literacy amongst the Dalit, in turn, affects their health and overall well-being negatively. (A key informant in Ganaktuli)
The participants further reported that the low level of education nurtured significant information asymmetries, which cause health-related misinformation, and limited occupational and income-earning opportunities. Participants reported that, due to their being excluded from mainstream society, Dalits were perceived to have poor levels of infant and child feeding, breast feeding practices, immunisation take-up and personal and family hygiene, with an unhealthy consumption of tobacco and alcohol, and so on. One participant stated that:
I have little or no educational background. It might diminish my understanding of things like whether and what extent things such as smoking bad for health? …what and how infant and young child should be fed? …what are good practices for washing hands? (A 56-year-old woman in Ganaktuli)
The data also revealed that little and/or no education narrows the occupational opportunities, and subsequently results in low incomes. In addition to poor educational quality, Dalit occupational opportunities are determined by other factors such as caste-based identities and heredity, and together with poor education this reduces their chance of improving their health status.
The data analysis also showed how the wider structural determinants interact with and influence the status of Dalits and their material circumstances. We found that the labour market both dynamically excludes and adversely includes Dalits by restricting their social and occupational mobility. The data gathered from community participants and key informants strongly suggest that Dalit ancestral occupations have limited their skill sets and continue to force them to expose themselves to high health risks and to rely on very low wages.
Exposure to a toxic physical environment while at work was commonly reported in the interviews and group discussions. Dalits are traditionally linked to their ancestral occupations, which were passed down from generation to generation. Consequently, the majority of Dalits are engaged in sweeping and cleaning activities, manually handling waste material and garbage while using no personal protective equipment. This exposes them to large amounts of dust, bioaerosols, volatile organic matter, airborne particulates, bacteria, noise and ergonomic stress. Multiple participants reported that sweepers frequently experience infections. As one participant explained:
Dalit always carry health risk with them at workplaces as they are dealing with very serious issues such as dumping garbage or removing dirt. But, they do not use protective equipment. […] We are more likely than non-Dalit to experience physical injuries or develop infections. (A 29-year-old cleaner in Agargaon)
Similarly, another participant noted:
Dalit sweepers don’t take any dust protective measure; therefore, they inhale it… I witnessed my colleagues develop respiratory infections and other airborne diseases. (A street sweeper in Ganaktuli)
Nonetheless, Dalit participants were not inclined to look for alternative occupations, as they said there was no scope for them to work outside of these historical, marginalised social spaces. Participants were highly aware of their role in the history of the country, and explained that they would face significant resistance if they tried to access occupations that did not conform to their low social and political status. Occupation-based discrimination, lingering poverty and social stigmatisation reduced their opportunities to participate in the labour market on equal terms (in relation to non-Dalits) and to engage with activities that were not considered ‘impure’. One FGD participant talked about how the lack of skills combined with long-established social norms strongly discourages Dalits from engaging differently with the labour market:
We are traditionally engaged in sweeping, as my ancestors did. I have no other skill except this. How can I do [anything else], for example, pulling a rickshaw or running a business? Similarly, people will not come and take a cup of tea if I operate a tea stall. (A 37-year-old cleaner in Agargaon)
This particular barrier is becoming increasingly problematic, as over 70% of the respondents reported that their access to sweeping jobs had become highly insecure and precarious; although initially the nature of their recruitment in sweeping activities was permanent, Dalits had more recently had to compete for their occupation with non-traditional Muslim sweepers. Although the city corporation’s sweeper recruitment policy states that the Dalits are given a quota, the authorities have not adhered to this system in recent years. The frequent recruitment of non-traditional sweepers by different government organisations and NGOs has considerably narrowed Dalits’ employment options, leading to financial hardship:
Some proportion of sweeping is reserved in government offices. However, non-Dalit sweepers are getting these jobs through bribes to political leaders and government officials. Where will we go for work? We will likely have to resort to unsocial and illegal activities to survive if this situation is not improved. (A housewife in Agargaon)
The lack of a sufficient and regular income limited Dalit participants’ capacity to afford basic necessities, including food, healthcare (particularly from private facilities) and education fees. Their average monthly household income ranged from BDT5850 to BDT8970 (considering BDT78=US$1), which was insufficient to buy three nutritious meals per day for an extended family.
Politics and relationships
Our data have identified a set of social and political factors in the given political and governance system that impact on the Dalit health status through stratifying individual positions on the basis of hierarchies of power and prestige, and access to resources. Due to their weak socioeconomic position, caste-based identity and discrimination, Dalits in the studied areas generally have a weak power of participation in political processes, both at the national and community levels. One of the participants from Ganaktuli reported:
Our sweeping identity shapes our world—our work, our rights, our opportunities, our limitations, it shapes everything. Hundreds of years we are living a confined life in a sense that the mainstream society maintains a greater distance as we belong to such a low caste. Where are we? …In education, in health, in politics? …nowhere. (Add details)
The lack of political participation generated by a lack of consideration and discrimination by other powerful groups limited Dalits’ opportunity to voice their needs and impeded their capacity to exercise other constitutional and human rights. Making a direct connection between political engagement and health, one participant voiced:
To my knowledge, no one from the Dalit community has appeared as a candidate in any election at national or community level. Even, they are likely to be less concerned about this. Such an absence in political process diminishes our capacity to protect communal interest concerning health. (A 34-year-old Dalit in Agargaon)
Data from interviews with key informants and group discussants indicated that factors relating to macroeconomic policies influenced the health of Dalits. Macrolevel policies were considered to be having a negative impact on their health status and health-seeking capacity, and public allocations for social protection and healthcare schemes continued to exclude people living in urban settings. One of the key informants reflected on the situation:
Government policy only provides safety-net support for poor in the rural setting. However, the Dalit are concentrated on the big cities and smaller towns. …therefore we are not eligible for that. (A key informant in Agargaon)
This policy significantly affected Dalits’ capacity to seek and afford treatment in settings where they were exposed to regular health shocks and hazards. For example, in the existing health policy, two-thirds of healthcare costs are financed via an out-of-pocket mechanism,36 and the urban poor experience limited or no healthcare support. Participants reported that having no social protection schemes meant that they had to rely on considerable out-of-pocket healthcare expenditure in order to access healthcare from both public and private facilities. The low income-earning capacity of Dalits interacted directly with their individual socioeconomic condition, particularly for those suffering from chronic health conditions that required prolonged and continuous care and medication. The inability to afford treatment was frequently reported as an important barrier to better health by respondents suffering from cardiac issues, diabetes and renal disease due to out-of-pocket costs. One of them said:
I have been suffering from diabetes for the past years. The doctor prescribed several drugs that I imperatively need to continue taking to control my sugar levels. I cannot afford such drug for rest of my life […] you will never expect to get diabetic drug free of cost. (A street sweeper in Ganaktuli)
Some participants highlighted the heavy reliance on expensive private health service providers as a significant determinant of bad health. They indicated that an individual’s health status tended to deteriorate when they needed to access healthcare services from a local private institution. A key informant in Ganaktuli explained that local private healthcare facilities generally tended to be better equipped than local government facilities, and increasingly played a ‘vital role in healthcare services delivery.’ However, he noted:
If the problem is not minimal and, you must seek consultant at private facilities this involves huge expenses that are most likely beyond the capacity of Dalit. …I know a few individuals who have been suffering from chronic disease but fail to take care from private clinics due to the cost incurred. (A key informant in Ganaktuli)
Beyond the costs incurred by care, participants also identified the behaviour of healthcare professionals in public and private facilities as barriers to their accessing better health. Respondents shared experiences of entrenched stigmatisation and discrimination that hampered their willingness and motivation to see a doctor, thereby generating a process of self-exclusion from these facilities.
The Dalit identity generates considerable caste-based discrimination, enhancing exclusion, broadening inequalities and restricting them from accessing healthcare. Dalit people, considered untouchable due to their traditional employment that brings them into contact with human excreta, dirt, garbage, bad odours, dead bodies and other elements, are defined by others by their impurity. One participant described how mainstream society perceives the Dalit, and the following quote denotes how societal perceptions have been internalised by Dalits themselves:
We are methar [a Bangla colloquial term signifying degradation, disgust], nothing more than that. Our position can be nowhere else but at the bottom of the society. (A 34-year-old scavenger in Agargaon)
These socioeconomic mechanisms and Dalits’ identity interact with other factors to create psychosocial factors that determine their health status. Due to social discrimination and exclusion, Dalits often lose their self-worth and experience depression and shame. Such feelings in turn lead to social isolation and further narrow individual and/or community participation in health programmes. The participants further stated that Dalits could not fully participate in community-based health programmes focusing on child and maternal health, the promotion of nutrition, immunisation, sanitation and hygiene. One participant explained the situation as follows:
Dalit are social excluded and discriminated in many ways. Due to such discrimination and exclusion, they might lose self-esteem to be open-minded in participation of community-led health programmes. (A 34-year-old cleaner in Agargaon)
Prejudices against the Dalits are also reproduced by healthcare workers. Most respondents reported that healthcare workers were more likely to consider their health problems to be less serious than those of non-Dalits in order to limit the amount of time spent with them and their exposure to ‘impurity’. In small townships and localities outside Dhaka city, for example, in primary-level healthcare facilities where Dalits are easily identified by locals, they reported being more likely to face such prejudice and discrimination from healthcare workers. Multiple participants echoed the following experience of visiting a health facility:
Sometimes we do not disclose our identity to avoid neglect and unpleasant situations. … I can tell you a tragic story about the hospital admission of a Dalit woman. She was denied to get hospital admission and was kept lying on the floor of the balcony because she was a Dalit. Meanwhile, she developed additional problems—common cold, fever and breathing difficulties in such cold weather. Only later, when we put the issue forward the hospital authority admitted her and provided a bed. (A 51-year-old Dalit rights activist in Ganaktuli)
Several participants described a lack of attention from healthcare workers, and difficulties in obtaining adequate information regarding their health problems and required treatments. The following excerpt reflects this situation:
Doctors/nurses are unwilling to discuss details regarding any health information or health intervention in the facilities. They just provide minimal medicine and maintain indifference when asked about a health-related problem. (A 55-year-old leather worker in Ganaktuli)
Such negligent and discriminatory behaviour on the part of healthcare providers made Dalits hesitant to participate in health promotion activities to enhance their own health, and even influenced their decisions to delay seeking treatment for infectious diseases. One of the key informants explained how the sociopolitical position of the Dalit community impacted on the care-seeking behaviour of Dalits:
The Dalit live as a minority within the mainstream. All aspects of their lives—such as profession, access to services, rights and obligations, decisions, and so on—are determined and ascribed by these social and political contexts. (An NGO worker in Ganaktuli)
Denied access to formal and informal safety nets, this marginalisation is reinforced by idiosyncratic forms of discrimination based on class, gender, physical ability and age in particular. Undernutrition of low-income (often extreme poor) adolescent girls, pregnant mothers and elderly widows was found to be particularly severe. Health inequalities experienced by Dalits were also influenced by the manner in which policies are developed and translated into practice. One key informant stated:
The state did not consider that context-specific healthcare provision might be effective for providing services to this kind of disadvantaged group of people. We need the formulation of policies that cover the delivery of health services to the Dalit and other groups of people who are in an unfavourable position to seek care. (A Dalit rights activist in Agargaon)
In addition, some respondents reported that being a Dalit was associated with behaviours that negatively affected their health. Many respondents claimed that male Dalits were likely to consume high quantities of low-quality alcohol and tobacco, noting that this behaviour can be explained by the difficult occupations and psychosocial pressure they experienced. Exposure to bad odours, dirt and dead organisms can induce vomiting and appetite loss, and according to some respondents consuming alcohol and cigarettes mitigated the negative psychological and physical effects of this type of work. Historically, Dalits have been characterised by such depictions and so this is not new; it is beyond the scope of this research to assess the veracity of such claims. However, what is noteworthy is how such claims serve to further stigmatise members of this population group, who according to some respondents, are ‘habituated to consume alcohol and tobacco products’ as they believe it is ‘a habit rooted in their occupational roles and psychosocial identity’ (a 23-year-old scavenger in Agargaon). Our data suggest that Dalit children living in marginalised settlements suffer from stigmatisation and are therefore constrained in their physical mobility and social interactions. Although it was not possible to measure the physical growth of children due to the nature of this study, participants reported that children, particularly those aged under 5 years, were likely to be undernourished. Poverty, low health information and awareness, and physical environment were reported as the most likely causal factors for such poor physical and social development of young children.
As a response to the hostile wider sociopolitical context and challenging material circumstances, traditional health practices and rituals are widely practised within the Dalit community. Religious beliefs and spirituality influence their health status and attitudes towards seeking treatment. It was, for example, found that low-income Dalits adhering to strict religious beliefs were more likely to rely on faith-based healing for sexual and reproductive health, pregnancy care and infant and child feeding practices.
Discussion
To the best of our knowledge this is the first study aimed at understanding the sociocultural and economic determinants of health inequalities in the Dalit population in Bangladesh, and it applies the CSDH Conceptual Framework developed by the WHO. Our analysis suggested that the mechanisms of social and economic discrimination that result in severe health inequalities (as claimed by the participants) for Dalits are supported and reinforced by an array of interconnected structural factors, including geographic marginalisation, poor living conditions, low formal education, little political representation, poor access to resources, limited labour market engagement and stigmatisation. Stigmatisation was found to be pervasive, and to directly shape relational and structural determinants of health.
Dalits’ occupation-based identity determines their ability to interact with non-Dalits and with the state, and their stigmatisation as an impure, unhygienic, uneducated population group reinforces these processes and worsens their material and psychosocial circumstances. These are identified as significant intermediary determinants of their health status within this specific urban context.37 Our findings confirm that health inequalities are rooted in the social process, where structural, contextual and interpersonal factors intersect and influence each other38–40 and build on these to show how pervasive identity-based discrimination perpetuates the causes and effects of health inequalities.
Untouchability and caste-based discrimination perpetuate an exclusionary process that results in this population belonging to a lower caste status with limited or no access to or participation in healthcare services or health-seeking behaviours, and has been similarly noted by studies conducted in Indian societies.41–45 Broadly, these socioculturally constructed exclusionary processes restrict Dalits’ economic, political, social and cultural participation, which in turn negatively impacts on their health and well-being at the individual, communal, regional and global levels. These observations are also in line with a prior report of the Social Exclusion Knowledge Network to the World Health CSDH, which stated that sociocultural exclusion is a dynamic and multidimensional process driven by unequal power relations.39 42 46
Our results also highlight power differentials between Dalit individuals and healthcare professionals, which enhance health inequities and further victimise Dalits, and are in line with the results of another study in India.47 These power differentials further repress the social, political and economic participation of Dalits, leading to the unequal and unjust distribution of resources and access to services. Overall, sociocultural exclusionary processes generate, preserve and reproduce inequalities regarding participating in, accessing and using health services, which perpetuate intergenerational deprivation and discrimination. Other studies have demonstrated that caste-based exclusion, deprivation and discrimination have been practised on the Indian subcontinent for thousands of years.5 47
The socioeconomic and political context, together with macropolicies, facilitates the exclusionary process where Dalit people have limited opportunities for livelihood development and to improve their economic condition, consequently reducing their income opportunities and trapping them in poverty. This trap is sustained and enhanced through intergenerational transmission. Income is strongly associated with health and influences a range of material circumstances that directly impact health. Economic exclusion also determines access to and utilisation of health services, while economic marginalisation appears to limit the provision of healthcare, health-seeking behaviours and access to other basic services provided by members of society and the state.35 48 In addition, social and public policies narrow healthcare utilisation and healthcare seeking, for example, catastrophic out-of-pocket costs and the shrunken delivery of healthcare by public health facilities. The literature shows that over the recent years out-of-pocket costs are gradually increasing due to the steady expansion of private healthcare services36 49 and this affects healthcare seeking and utilisation. The wider structural factors facilitate the Dalits’ compromised material circumstances, unhealthy lifestyle and social isolation. As noted by other studies,34 50 51 our findings show that poor living and working conditions, limited healthcare access and support, poor state of water and sanitation, habit of tobacco consumption, stress and isolation from health services negatively impact on health status and healthcare seeking. A lower social background was observed by Desai and Dubey52 to contribute to weakening social networks that perpetuate poor healthcare access and healthcare seeking. Furthermore, the health system itself influences the health of Dalits as it presents Dalits with greater financial costs when accessing or seeking healthcare, as noted in other studies.36 53 Moreover, access to and acceptance by healthcare providers is determined by the social position of individuals and groups; Dalits’ low social position restricts their access to healthcare professionals, as had been previously reported in many regions across the world.50 54 55 Our findings suggest that the health status of the Dalit community is not shaped solely by clinical issues but also by a range of sociocultural determinants, as proposed in several other studies.14 56 For disadvantaged, marginalised and socioculturally excluded individuals or groups like Dalits, health outcome improvement is closely linked to public policies and actions that address sociocultural determinants of health inequities, with the government playing a central role.57
Limitations of the study
We think the limitations of this study warrant comments. First, due to unavailability (we approached some other groups to participate in the interviews but they could not participate because either they had other commitments in the study time or did not show interest to participate), and resource and time limitation, this study did not include the entire groups and/or stakeholders, such as state officials, employers of Dalit population and government healthcare providers, which might have provided alternative source of information to obtain greater level of trustworthiness. However, we maintained a greater level of trustworthiness by applying four principles—credibility, transferability, conformability and dependability. Furthermore, intercoder or synchronic reliability referring the amount of agreement between independent coders of the data, and triangulation between methods, and participants were used to avoid biases in this study. Second, some participants might have been dominating in the group discussions which caused other participants to feel uncomfortable sharing their own opinions and experiences honestly. However, this limitation was mitigated by the experienced facilitators who built good rapports and enable each person’s voice to be heard by elaborating, clarifying, agreeing or disagreeing, querying and explaining of the topic of discussion. Third, the qualitative strand of this study was geographically limited to an urban setting (Dhaka city); therefore, the results may not easily be transferable across populations and places; for example, a small Bangladeshi town. Nonetheless, considering the data collected, we believe that this study provides an in-depth understanding of a set of social, cultural, economic and political factors that strongly determine the health outcomes of Dalits population.
Conclusions and implication for the study
Although this subject has previously been sporadically discussed in newspaper reports, NGO reports and media reports, this paper is one of the first qualitative studies to explore a vast array of factors that determine health inequalities in urban Dalit populations in Bangladesh. This study is expected to contribute to knowledge by investigating how these elements interact and play a determining role in shaping Dalits’ health status. This study supports the view that Dalit health inequalities are largely affected by a wide range of sociocultural factors which can be observed in societies across many regions of South Asia.
Importantly, we argue for the need to recognise the significant intermediary effects of everyday discrimination and stigmatisation, perpetuated by socioeconomic structures, on educational achievement, political participation, occupations and health behaviours. Dalits’ social and political history shapes their social position in society today by limiting their power relative to non-Dalits in key social structures, including the labour market and health institutions. These mechanisms enhance exclusionary processes through mutually reinforcing sets of sociocultural and economic dynamics, and these generate, sustain, deepen, reinforce and reproduce inequalities in the health of Dalit populations. Therefore, it is unlikely that the health status of Dalit populations will be improved through the better clinical performance of existing healthcare providers alone. Recognition of the hostility of existing institutions and addressing entrenched exclusionary processes (including self-exclusion) and adverse inclusion is needed, together with research on the potential benefits of developing state-initiated social protection schemes focusing on deepening the social inclusion agenda.
Supplementary Material
Acknowledgments
The authors extend their gratitude to the Department of Anthropology, Dhaka University, for their approval of this study. The authors are also grateful to the members of the two Dalit communities, and NGO workers who participated in the interviews and group discussions.
Footnotes
Patient consent for publication: Not required.
Contributors: AK, AA and BC conceptualised the study. AK, MRLM and NF performed the analysis. AK developed interview guidelines, interviewed participants, and transcribed and translated interviews. AK, AA, NF and MRLM drafted the initial manuscript with substantial support from BC. All authors substantially contributed to critically revising further version of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Ethics approval: Ethics review committee at Dhaka University, Bangladesh.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: As we informed the participants during the consent process that data would only be shared within the research team, then the data cannot be made available publicly. However, we shared the interview and discussion guidelines under ‘additional supporting files.’ Interested parties may contact Mr Md Shahin Chowdhury (anthro.du@yahoo.com), Senior Administrative Assistant, Department of Anthropology, Dhaka University, for further inquiries in this regard.
References
- 1. El Arifeen S, Christou A, Reichenbach L, et al. Community-based approaches and partnerships: innovations in health-service delivery in Bangladesh. Lancet 2013;382:2012–26. 10.1016/S0140-6736(13)62149-2 [DOI] [PubMed] [Google Scholar]
- 2. Chowdhury AM, Bhuiya A, Chowdhury ME, et al. The Bangladesh paradox: exceptional health achievement despite economic poverty. Lancet 2013;382:1734–45. 10.1016/S0140-6736(13)62148-0 [DOI] [PubMed] [Google Scholar]
- 3. GoB M. Health population and nutrition sector strategic plan (HPNSSP): 2011-2016. 3rd ed Dhaka: Planning Wing, Ministry of Health and Family Welfare, Government of the People’s Republic of Bangladesh, 2010. [Google Scholar]
- 4. Clifford B. Dalit Rights are human rights: caste discrimination, international activism, and theconstruction of a new human rights issue. Human Rights Quarterly 2007;29:167–93. [Google Scholar]
- 5. Asaduzzaman A. The “Pariah” people: an ethnography of the urban sweepers in Bangladesh. The University Press 2001. [Google Scholar]
- 6. Sultana H, Subedi DB. Caste system and resistance: the case of untouchable hindu sweepers in Bangladesh. Int J Polit Cult Soc 2015:1–14. [Google Scholar]
- 7. International Dalit Solidarity Network (IDSN). Working globally against discrimination based on work and descent. IDSN: Copenhagen, 2013:1–51. [Google Scholar]
- 8. Islam F. political participation of Dalit women in Dhaka city, Bangladesh. Dhaka 2007. [Google Scholar]
- 9. National Institute of Population Research and Training (NIPORT), Mitra and Asscociates. Bangladesh Demographic and Health Survey 2014: Full Report. Dhaka, Bangladesh and Rockville, Maryland, USA, 2016:1–354. Ref Type: Report. [Google Scholar]
- 10. National Institute of Population Research and Training (NIPORT). Bangladesh Urban Health Survey 2013: Final Report. Dhaka, Bangladesh and Rockville, Maryland, USA, 2014. Ref Type: Report. [Google Scholar]
- 11. Govindaraj R, Raju D, Secci F, et al. Health and Nutrition in Urban Bangladesh: Social Determinants and Health Sector Governance. The World Bank 2018. [Google Scholar]
- 12. Roy RK. Assessment of Nutritional Status and Its Determinants Among Pre-School Children Within Dalit Communities of Jessore City in Bangladesh: A Cross-Sectional Study. Age 2018;24:43. [Google Scholar]
- 13. Chowdhury IU. Caste-based Discrimination in South Asia: a study of Bangladesh. New Delhi: Indian Institute of Dalit Studies, 2009. [Google Scholar]
- 14. Islam M, Parvez A. Dalit Initiatives in Bangladesh. Dhaka: Nagorik Uddyog & Bangladesh Dalit and Excluded Rights Movement, 2013. [Google Scholar]
- 15. Social. Economic and cultural status of dalit community in Bangladesh. Ref Type: Report, 2018. [Google Scholar]
- 16. National Institute of Population Research and Training (NIPORT). Mitra and Associates, ICF International Bangladesh Demographic and Health Survey. 66 Dhaka, Bangladesh, 2014. Ref Type: Report. [Google Scholar]
- 17. (Dalit). The Life and Days of (Dalit) Sweepers in Bangladesh. The Daily Star 2006. [Google Scholar]
- 18. Lundberg O. Causal explanations for class inequality in health--an empirical analysis. Soc Sci Med 1991;32:385–93. 10.1016/0277-9536(91)90339-E [DOI] [PubMed] [Google Scholar]
- 19. Davidson R, Mitchell R, Hunt K. Location, location, location: the role of experience of disadvantage in lay perceptions of area inequalities in health. Health Place 2008;14:167–81. 10.1016/j.healthplace.2007.05.008 [DOI] [PubMed] [Google Scholar]
- 20. Gwatkin DR, Bhuiya A, Victora CG. Making health systems more equitable. Lancet 2004;364:1273–80. 10.1016/S0140-6736(04)17145-6 [DOI] [PubMed] [Google Scholar]
- 21. Graham H. Social determinants and their unequal distribution:clarifying policy understanding. The Maibank Quarterly 2004;82:101–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Davidson R, Kitzinger J, Hunt K. The wealthy get healthy, the poor get poorly? Lay perceptions of health inequalities. Soc Sci Med 2006;62:2171–82. 10.1016/j.socscimed.2005.10.010 [DOI] [PubMed] [Google Scholar]
- 23. Ahmed SM, Adams AM, Chowdhury M, et al. Gender, socioeconomic development and health-seeking behaviour in Bangladesh. Soc Sci Med 2000;51:361–71. 10.1016/S0277-9536(99)00461-X [DOI] [PubMed] [Google Scholar]
- 24. Solar O, Irwin A. A conceptual framework for action on the social determinants of health: Social Determinants of Health Discussion Paper 2 (Policy and Practice. Geneva Switzerland: World Health Organization [WHO], 2007. [Google Scholar]
- 25. Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol 2001;30:668–77. [DOI] [PubMed] [Google Scholar]
- 26. Marmot M, Wilkinson RG. Psychosocial and material pathways in the relation between income and health: a response to Lynch et al. BMJ 2001;322:1233–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Smith GD, Egger M. Commentary: understanding it all--health, meta-theories, and mortality trends. BMJ 1996;313:1584–5. 10.1136/bmj.313.7072.1584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wilkinson RG, Pickett KE. Income inequality and population health: a review and explanation of the evidence. Soc Sci Med 2006;62:1768–84. 10.1016/j.socscimed.2005.08.036 [DOI] [PubMed] [Google Scholar]
- 29. Anderson C. Presenting and evaluating qualitative research. Am J Pharm Educ 2010;74:141 10.5688/aj7408141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Patton MQ. Qualitative research and evaluation methods, 209-339. Thousand Oaks, CA: Sage: Un estudio cualitativo, 2002. [Google Scholar]
- 31. Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods 2006;18:59–82. [Google Scholar]
- 32. Abbas T, Charles T. Handbook of mixed methods in social & behavioral research. Sage Publications, Thousand Oaks 2003. [Google Scholar]
- 33. Miles MB, Huberman AM. Qualitative data analysis: a sourcebook. Beverly Hills: Sage Publications, 1994. [Google Scholar]
- 34. Kumar Saha C. Dynamics of risk determinants regarding diarrhea affected slum children in urban dhaka: a dysfunctional health care system. Current Research Journal of Social Sciences 2012;4:304–13. [Google Scholar]
- 35. Evans T, Whitehead M, Diderichsen F, et al. Challenging Inequities in Health: From Ethics to Action. Oxford UP 2001. [Google Scholar]
- 36. Islam A, Biswas T. Health system in Bangladesh: Challenges and opportunities. American Journal of Health Research 2014;2:366–74. [Google Scholar]
- 37. Hankivsky O. Intersectionality 101. The Institute for Intersectionality Research & Policy, SFU 2014. [Google Scholar]
- 38. Cairney J, Veldhuizen S, Vigod S, et al. Exploring the social determinants of mental health service use using intersectionality theory and CART analysis. J Epidemiol Community Health 2014;68:145–50. 10.1136/jech-2013-203120 [DOI] [PubMed] [Google Scholar]
- 39. Patil RR. Caste-, work-, and descent-based discrimination as a determinant of health in social epidemiology. Soc Work Public Health 2014;29:342–9. 10.1080/19371918.2013.821363 [DOI] [PubMed] [Google Scholar]
- 40. Seng JS, Lopez WD, Sperlich M, et al. Marginalized identities, discrimination burden, and mental health: empirical exploration of an interpersonal-level approach to modeling intersectionality. Soc Sci Med 2012;75:2437–45. 10.1016/j.socscimed.2012.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Mohindra KS, Haddad S, Narayana D. Women’s health in a rural community in Kerala, India: do caste and socioeconomic position matter? J Epidemiol Community Health 2006;60:1020–6. 10.1136/jech.2006.047647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Nayar KR, Social exclusion caste. & health: a review based on the social determinants framework. Indian J Med Res 2007;126:355–63. [PubMed] [Google Scholar]
- 43. Agarwal S, Srivastava A. Social determinants of children’s health in urban areas in India. J Health Care Poor Underserved 2009;20:68–89. 10.1353/hpu.0.0232 [DOI] [PubMed] [Google Scholar]
- 44. Vart P, Jaglan A, Shafique K. Caste-based social inequalities and childhood anemia in India: results from the National Family Health Survey (NFHS) 2005-2006. BMC Public Health 2015;15:537 10.1186/s12889-015-1881-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Baral SC, Karki DK, Newell JN. Causes of stigma and discrimination associated with tuberculosis in Nepal: a qualitative study. BMC Public Health 2007;7:211 10.1186/1471-2458-7-211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kurian NJ. Widening economic & social disparities: implications for India. Indian J Med Res 2007;126:374–80. [PubMed] [Google Scholar]
- 47. Sabharwal SN, Sharma S, Diwakar GD, et al. Caste discrimination as a factor in poor access to public health service system: a case study of janani suraksha yojana scheme. Journal of Social Inclusion Studies 2014;1:148–68. [Google Scholar]
- 48. WHO. A Conceptual framework for action on the social determinants of health: discussion paper for the commission on social determinants of health: DRAFT, 2007. [Google Scholar]
- 49. Soors W, De Man J, Ndiaye P, et al. ; Towards universal coverage in the majority world: Transversal findings & lessons learnt, a summary. Antwerp, Belgium: ITG, 2015. [Google Scholar]
- 50. Kabir A, Farhana N, Akter F, et al. Sweeping practices, perceptions and knowledge about occupational safety and health hazards of street sweepers in Dhaka city, Bangladesh: a qualitative inquiry. Int J Community Med Public Health 2015;2:237–43. [Google Scholar]
- 51. Bambra C, Gibson M, Sowden A, et al. Tackling the wider social determinants of health and health inequalities: evidence from systematic reviews. J Epidemiol Community Health 2010;64:284–91. 10.1136/jech.2008.082743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Desai S, Dubey A. Caste in 21st Century India: competing narratives. Econ Polit Wkly 2012;46:40–9. [PMC free article] [PubMed] [Google Scholar]
- 53. Health System of Bangladesh. Online resource. 2014. http://www.bangladesh.gov.bd/?q=en/health-care-systems-bangladesh (cited 2014 May 23).
- 54. Wilkinson RG. Socioeconomic determinants of health. Health inequalities: relative or absolute material standards? BMJ 1997;314:591–5. 10.1136/bmj.314.7080.591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Borooah VK. Inequality in health outcomes in India: the role of caste and religion. 2010.
- 56. Sen G, Iyar A, George A. Systematic hierarchies and Systemic failures: Gender and Health Inequities in Koppal District. 2006.
- 57. Johnston HB. Addressing social exclusion: analyses from South Asia and southern Africa. J Health Popul Nutr 2009;27:423–5. 10.3329/jhpn.v27i4.3386 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.