Abstract
To assess the efficacy and short-term outcomes of adherence to statin therapy among coronary heart disease (CHD) patients following their hospital discharge, we enrolled 615 CHD patients who were prescribed statins from The First Affiliated Hospital of Chongqing Medical University in China between February 1st and October 31st of 2013. Statin adherence was evaluated by identifying the proportion of patients who remained adherent or became non-adherent to statin therapy over 4–8 months post-discharge from the hospital. The composite outcomes included all-cause mortality and re-hospitalization with cardiovascular disease. We found that 15.9% patients were non-adherent to their statin therapies and that coronary artery stenosis<75% (OR = 3.433, 95% CI: 2.191–5.380, p < 0.001) and adverse effects (OR = 2.542, 95% CI: 1.327–4.869, p = 0.005) both clearly contributed to poor adherence. The primary self-reported reasons for non-adherence included a lack of knowledge about the benefits of statin therapy (36.7%), the treatment being halted at the advice of their doctor (19.4%), and the difficulty in obtaining statins (12.2%). Non-adherence to statin therapy was significantly associated with an increased risk of cardiovascular events (OR = 1.741, 95% CI: 1.035–2.929, p = 0.037). In conclusion, CHD patients with moderate stenosis or adverse effects tended to have poor statin adherence, and this was significantly associated with increased cardiovascular events. We should strengthen education of the importance of statin therapy for both patients and doctors and facilitate the ability of patients to obtain their statin medication.
Clinical Study Register Code: ChiCTR-EPC-16007839.
Keywords: Adherence, Adverse effects, Cardiovascular events, Coronary heart disease, Statin
Abbreviations: CHD, coronary heart disease; LDL-C, low-density lipoprotein-cholesterol; MACE, major adverse cardiac events; PDC, proportion of days covered; BP, blood pressure; ULN, upper limits of normal; OR, odds ratio; HR, hazard ratio; CI, confidence interval; SD, standard deviation
Introduction
The 2013 American College of Cardiology and American Heart Association (ACC/AHA) guidelines for cholesterol management showed that statin treatment benefits patients with a low-density lipoprotein-cholesterol (LDL-C) level over 190 mg/dL and patients with arteriosclerotic cardiovascular disease who have acute coronary syndrome, a history of myocardial infarction, stable or unstable angina and have had a percutaneous coronary intervention.1 A previous study demonstrated that statin therapy had a significant beneficial effect in the secondary prevention of cardiovascular events in patients with coronary heart disease (CHD). The lowering of LDL-C by 1 mmol/L with statin therapy reduces the incidence of major adverse cardiac events (MACE; a composite of all cause death, non-fatal acute myocardial infarction, or target vessel revascularization) by approximately 20%.2 However, conversely, CHD patients with poor adherence to their statin therapy have a higher risk of MACE.
This poses a crucial problem because the use of statins for the secondary prevention of CHD is much lower in middle-income countries like China.3 Most studies in China emphasize the positive relationship between statin adherence and cardiovascular outcomes, yet little has been done to study effective measures to improve patient adherence to statin therapy. As a municipality directly under the Central Government, Chongqing is representative of the larger southwestern Chinese population. Therefore, our study assessed statin adherence rates in CHD patients from Chongqing city to elucidate factors that influence statin adherence to analyze the relationship between statin adherence and MACE and to evaluate measures to improve statin adherence in CHD patients.
Methods
Study design
We recruited patients diagnosed with CHD who were prescribed statins and collected basic information, such as the patients' habits in taking medicine, and we collected the patients' outcomes, which primarily consisted of a composite of all-cause mortality and re-hospitalization with MACE. The influencing factors of statin adherence and the relationship between adherence and the composite outcomes were directly explored in this study. The primary goal was non-adherence, and the secondary goal was risk factors of mortality. Adherence to statins was estimated by calculating the percentage of days a patient was prescribed statins from the day they were discharged to the day of their first re-hospitalization for MACE, the end of their follow-up period, or their death. Patients were then divided into two groups according to their proportion of days covered (PDC) level. PDC was defined as the total number of day's supply of medication divided by the total length of the interval, and multiplied by 100%. Adherent participants were defined as taking at least 80% of their current prescribed statin dose in the past studied period (PDC≥80%), whereas all other current statin users taking less than 80% of their prescribed statin dose were defined as non-adherent (PDC<80%).4, 5 This patient study conformed to the mandates set forth in the Declaration of Helsinki. Formal consent was not required for this study; however, we obtained informed consent from all participants. This study was approved by the Human Studies Committee of Chongqing Medical University.
Study population
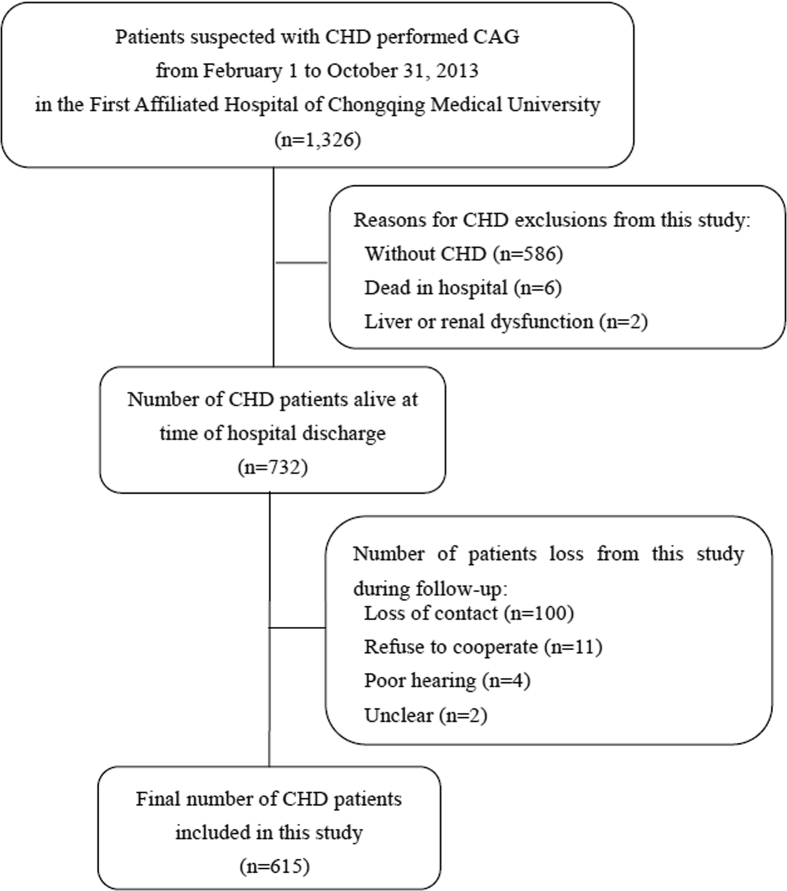
We enrolled 1326 patients who had undergone coronary angiography between February 1st and October 31st of 2013 at The First Affiliated Hospital of Chongqing Medical University in China into this retrospective cohort study. Patients were diagnosed as having CHD if catheterization demonstrated greater than 50% stenosis in one or more coronary vessels or if they had suffered from a previous acute myocardial infarction. A total of 594 patients without CHD who died in the hospital with liver or renal dysfunction were excluded. A total of 732 patients diagnosed with CHD and prescribed statins were identified for this study. All of these patients were followed up for a period of time between 4 and 8 months starting from their discharge date to the study end date on May 25, 2014 or to their end events if applicable. General information including age, sex, copayment proportion, blood pressure (BP), cholesterol level, degree of coronary artery stenosis, coronary heart disease type, comorbidities, and number of drugs prescribed for CHD were collected from the patients' medical records. Data regarding the patients' habits of taking statins, their occurrence of MACE, and their mortality were obtained by phone calls. Two to four phone calls were made for every subject to get as much detailed and accurate data as possible. The data regarding statin adherence and end-points were collected with a self-completed questionnaire. The part about drug adherence included statin type, dose, frequency and days of taking the drug post-discharge. The part about end-point data included time, location and causes of re-hospitalization for MACE or their death. A total of 117 patients were lost during the follow-up process due to loss of contact, refusal to cooperate, poor hearing, and ambiguity concerning their prescription. Thus, a total of 615 patients were analyzed in our study (Fig. 1).
Figure 1.
Study design and study population. The figure shows the criteria for including and excluding patients in our study. Abbreviations: CHD, coronary heart disease; CAG, coronary angiography.
Statistical analysis
We assessed the baseline characteristics of the patients for similarity between the two groups by using 2-sided unpaired Student's t-test or the Wilcoxon test for continuous variables and the Chi-square test for categorical variables. Multivariable logistic regression models with backward selection of all patients' characteristics with a significance of level of 0.20 were performed to screen for the risk factors of non-adherence to statin therapy during the follow-up. The adjusted odds ratio (OR) as well as the 95% confidence interval (CI) are presented. Reasons for non-adherence were compared by proportions. Univariate Cox regression analyses were first conducted for non-adherence and other factors associated with the composite outcome, followed by multivariate analysis with selection of the patients' characteristics with a significance at the 0.20 level in univariable analysis or with clinical significance as covariates for inclusion into the final model. Statin drug safety was assessed by examining the incidence of adverse events that appeared after initiating statin therapy. Lipid profiles were missing for 46 participants and were replaced with their median values. Two-tailed p-value<0.05 was considered statistically significant. All analyses were performed using SPSS 19.0 for Windows, version 19.0.
Results
Table 1 shows a comparison of the baseline and clinical characteristics between the adherence and non-adherence groups. The CHD was divided into two types, new-onset or previous myocardial infarctions. The comorbidities included hypertension, diabetes, cerebral infarction and/or peripheral arteriosclerosis. According to the 2013 ACC/AHA statin guideline, a high intensity correlates to an atorvastatin dose of 40–80 mg per day or a rosuvastatin dose of 20 mg per day while a medium-low intensity correlates to an atorvastatin dose of 10–20 mg per day, a rosuvastatin dose of 5–10 mg per day, a simvastatin dose of 10–40 mg per day, or a fluvastatin dose of 20–80 mg per day.1 Adverse effects from these statin treatments include adverse hepatic events, adverse muscular events, cognitive impairment, new-onset diabetes mellitus, and self-reported discomfort causing symptoms such as dizziness and fatigue. The number of drugs includes the number of aspirin/cilostazol, clopidogrel/ticagrelor, angiotensin conversion enzyme inhibitor/angiotensin receptor blocker, beta receptor blocker, and statins that a patient was prescribed.
Table 1.
Baseline characteristics of CHD patients in our study.
| Patient characteristics | PDC<80% | PDC≥80% | P value |
|---|---|---|---|
| No. Participants (%) | 98 (15.9) | 517 (84.1) | |
| Male, n (%) | 63 (69.4) | 359 (64.3) | 0.313 |
| Age, ≥65years, n (%) | 59 (60.2) | 281 (54.4) | 0.285 |
| Copayment proportion<50%, n (%) | 15 (15.3) | 65 (12.6) | 0.461 |
| Smoker, n (%) | 52 (53.1) | 297 (57.4) | 0.422 |
| Blood pressure (mean ± SD, mmHg) | |||
| Systolic blood pressure | 137.4 ± 20.1 | 135.3 ± 21.8 | 0.242 |
| Diastolic blood pressure | 80.3 ± 13.0 | 78.5 ± 13.9 | 0.116 |
| Cholesterol, (mean ± SD, mg/dL) | |||
| Total cholesterol | 175.8 ± 41.5 | 172.2 ± 47.6 | 0.131 |
| Total triglyceride | 149.2 ± 98.4 | 153.8 ± 120.9 | 0.494 |
| High density lipoprotein | 44.6 ± 12.1 | 44.7 ± 12.5 | 0.821 |
| Low density lipoprotein | 106.2 ± 34.0 | 102.0 ± 38.2 | 0.125 |
| Coronary heart disease type, n (%) | |||
| Myocardial infarction | 28 (28.6) | 175 (34.5) | 0.254 |
| Others | 70 (71.4) | 332 (65.5) | |
| Comorbidities, n (%) | 76 (77.6) | 404 (78.1) | 0.897 |
| Statin intensity, n (%) | |||
| High intensity | 16 (16.3) | 93 (18.0) | 0.693 |
| Medium-low intensity | 82 (83.7) | 424 (82.0) | |
| Statin, n (%) | |||
| atorvastatin | 58 (59.2) | 361 (69.8) | 0.074 |
| rosuvastatin | 34 (34.7) | 123 (23.8) | |
| other | 6 (6.1) | 33 (6.4) | |
| Adverse effects, n (%) | 16 (16.3) | 40 (7.8) | 0.007 |
| Number of drugs≥3, n (%) | 87 (88.8) | 500 (96.7) | 0.001 |
Abbreviations: CHD, coronary heart disease; PDC, proportion of days covered; SD, standard deviation.
We found that the division of patients into the non-adherent and adherent groups was 15.9% and 84.1%, respectively (Table 1). The baseline characteristics of all patients were evaluated between the non-adherent and adherent groups and were similar between the two cohorts. Sex, age, copayment proportion, smoking status, systolic BP, diastolic BP, CHD type, comorbidity, and statin intensity were also significantly different between the two groups. Non-adherent patients exhibited coronary artery stenosis were less likely to experience adverse effects with statin therapy, and took a smaller number of drugs to treat their disease.
Table 2 shows the adjusted OR and 95% CI of participant characteristics from multivariate logistic regression for non-adherence. Logistic regression was adopted to analyze the relationship between statin adherence and patient characteristics including diastolic BP, LDL-C, coronary artery stenosis, statin therapy, adverse effect and number of drugs. The results showed that CHD patients with less severe stenosis (OR: 3.433; 95% CI: 2.191–5.380; p < 0.001) or experienced adverse effects (OR: 2.542; 95% CI: 1.327–4.869; p = 0.005) tended to have poor adherence.
Table 2.
Predictors of adherence to statin therapy.
| Patient characteristics | OR (95% CI) | P value |
|---|---|---|
| Coronary artery stenosis | ||
| <75% | 3.433 (2.191,5.380) | <0.001a |
| ≥75% | 1.000 | |
| Adverse effects | ||
| With | 2.542 (1.327,4.869) | 0.005b |
| Without | 1.000 | |
Abbreviations: OR, odds ratio; CI, confidence interval.
Adjusted for diastolic blood pressure, low-density lipoprotein-cholesterol, statin, adverse effect, number of drugs.
Adjusted for diastolic blood pressure, low-density lipoprotein-cholesterol, coronary artery stenosis, statin, number of drugs.
Table 3 conveys the reasons for non-adherence to statins among patients with a PDC<80%. When we inquired into patient reasons for non-adherence to statins via phone calls, three main reasons were revealed, and these included a lack of knowledge (36.7%), doctor's advice (19.4%), and difficulty in obtaining statins (12.2%). A preference for traditional Chinese medicine over statins (9.2%), economics (6.1%) and adverse effects (5.1%) were less common reasons cited among these patients for non-adherence.
Table 3.
Reasons for non-adherence to statin therapy.
| Reasons | n (%) |
|---|---|
| Lack of knowledge about CHD | 36 (36.7) |
| Doctor's advice | 19 (19.4) |
| Difficulty in obtaining statins | 12 (12.2) |
| Traditional Chinese medicine | 9 (9.2) |
| Economics | 6 (6.1) |
| Adverse effects | 5 (5.1) |
| Others | 11 (11.2) |
| Total | 98 (100.0) |
Abbreviations: CHD, coronary heart disease.
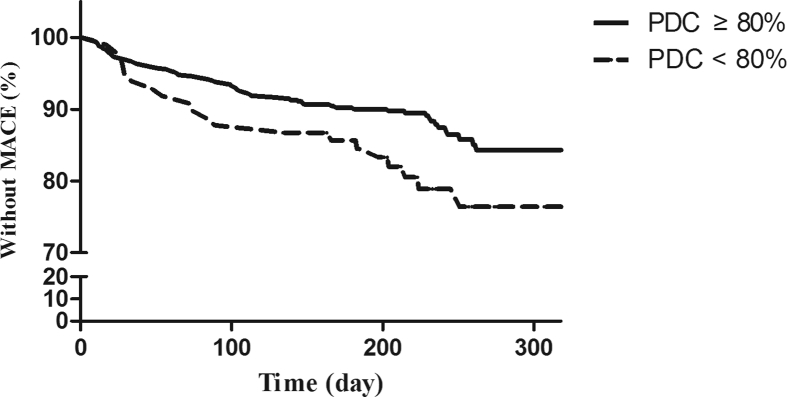
Fig. 2 shows, during a mean follow-up of 7 months (range, 0.13–12.7), 83 (13.5%) composite outcome events (7 death and 76 re-hospitalization) were observed, with 517 (84.1%) in the PDC≥80% group and 98 (15.9%) in the PDC<80% group. The mean time to occurrence of a composite outcome event following patient discharge was 105 ± 82.1 days (range: 4–348).
Figure 2.
The survival curves for people with PDC≥80% and with PDC<80%. The solid line stands for the percentage of PDC≥80% patients without end points over time, while the dotted line stands for the percentage of PDC<80% patients without end points over time. Patients with PDC≥80% were significantly longer-lived than those with PDC<80% (p < 0.05). Abbreviations: PDC, proportion of days covered; MACE, major adverse cardiac events.
Table 4 shows the risk factors associated with composite clinical events. Univariate cox regression analysis revealed that female patients with an age greater than 65 years and patients that had comorbidities and non-adherence (PDC<80%) were statistically associated with the composite clinical outcome. Non-adherence to statins was associated with a 78% increase in the probability of experiencing clinical outcomes, with an unadjusted hazard ratio of 1.780 (95% CI: 1.084–2.922). After adjustment for potential confounders, non-adherence to statins remained statistically significant and was shown to be a reliable independent predictor of clinical outcome (HR: 1.741; 95% CI: 1.035–2.929; p = 0.037). The adjusted confounders included being female (HR: 1.893; 95% CI: 1.218–2.944; p = 0.005), ≥65years of age (HR: 1.701; 95% CI: 1.055–2.743; p = 0.029), presentation with comorbidities (HR: 1.990; 95% CI: 1.022–3.878; p = 0.043), having a myocardial infarction (HR: 1.152; 95% CI: 0.703–1.888; p = 0.574) and the presence of coronary artery stenosis that was ≥75% (HR: 1.084; 95% CI: 0.644–1.823; p = 0.762). To further emphasize these findings, Fig. 2 shows survival between patients with a PDC≥80% and patients with a PDC<80%, which clearly shows that patients with a PDC<80% with a MACE survive for a shorter period of time.
Table 4.
Risk factors associated with composite clinical events.
| Variables | Univariate |
Multivariatea |
||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P value | HR | 95% CI | P value | |
| Sex, female | 2.094 | 1.360, 3.224 | 0.001 | 1.893 | 1.218, 2.944 | 0.005 |
| Age, ≥65years | 2.035 | 1.272, 3.254 | 0.003 | 1.701 | 1.055, 2.743 | 0.029 |
| Comorbidities | 2.149 | 1.110, 4.163 | 0.023 | 1.990 | 1.022, 3.878 | 0.043 |
| Coronary stenosis, ≥75% | 0.883 | 0.555, 1.404 | 0.598 | 1.084 | 0.644, 1.823 | 0.762 |
| Coronary heart disease type, Myocardial infarction | 0.984 | 0.624, 1.551 | 0.943 | 1.152 | 0.703, 1.888 | 0.574 |
| PDC, <80% | 1.780 | 1.084, 2.922 | 0.023 | 1.741 | 1.035, 2.929 | 0.037 |
Abbreviations: PDC, proportion of days covered; HR, hazard ratio; CI, confidence interval.
Adjusted for sex, age, coronary stenosis, coronary heart disease type, comorbidities, and PDC.
We examined the safety of statin therapy and the data are shown in Table 5. For hepatic adverse events, statistical indices indicate a stronger association with atorvastatin. The hepatic adverse events were defined as a hepatic enzyme level greater than the upper limits of normal (ULN) × 3. The muscular adverse events included in Table 5 include myalgia, myositis (muscle related symptoms and creatine kinase elevation > ULN × 10), and rhabdomyolysis. Cognitive impairment was defined as dementia, or the disturbance of perception or thought. New-onset diabetes mellitus was defined as an impaired fasting blood glucose level, abnormal glucose tolerance, or increased hemoglobin A1C after taking statins. Interestingly, we found that muscular adverse events and new-onset diabetes mellitus were more common in patients receiving rosuvastatin therapy. Furthermore, there was less cognitive impairment observed in patients on atorvastatin than compared with patients on rosuvastatin and simvastatin/pravastatin therapies.
Table 5.
Statin drug safety.
| Adverse events | Atorvastatin | Rosuvastatin | Simvastatin/pravastatin |
|---|---|---|---|
| Hepatic adverse events | 3.1% | 1.9% | 2.6% |
| Muscular adverse events | 3.1% | 3.8% | 2.6% |
| Cognitive impairment | 2.6% | 5.1% | 5.1% |
| New-onset diabetes mellitus | 0.0% | 0.6% | 0.0% |
Discussion
Adherence to statin therapy by CHD patients
In our study, 84.1% of CHD patients were adherent (PDC≥80%) to statin therapy during the follow-up, which was in accordance with Rasmussen JN et al but was quite improved when compared with adherence levels in multi-center studies reported previously from western countries.6 Since we carried out this project in a tertiary referral center, our population does not represent patient populations from other hospitals in China.
The benefits associated with statin treatment for the prevention of secondary CHD have been well-documented in studies such as LIPID, 4S, and CARE, and their results highlight a larger problem of general underuse of statins in CHD patients worldwide. Choudhry et al, found only 24.9% of CHD patients had good adherence to statins.7 In Finland, Upmeier et al, found only 28.1% of the patients with CHD had a good adherence to statins.8 Lemstra and Blackburn suggested that only 38.3% of CHD patients in Canada had good adherence to statins.9 On the other hand, Iqbal et al, reported that approximately 70% of CHD patients were adherent to statins following a percutaneous coronary intervention and coronary artery bypass graft and Rasmussen et al, observed a good adherence of 80.5% of participants in their studies.6, 10
Patients with moderate stenosis tended to be less adherent in our study, and this observation is supported by Choudhry et al, who showed that post-myocardial infarction revascularization was associated with an improved adherence to statins.7 We also observed lower adherence in patients with more adverse effects and this is in accordance with a study by Wei et al, that showed that statin-related muscle side effects contributed significantly to poor rates of adherence.5 We found that patients with a low copayment, of older age, of the female sex, with congestive heart failure, and co-diagnosed with diabetes were more adherent to statins and this has also been demonstrated in other studies.11, 12 Factors such as age, sex, and comorbidities, however, were not linked to adherence in our study. Our study also showed that non-adherence to statin therapy was associated with an increased incidence of clinical events, which has been shown previously.2
Methods to improve statin therapy adherence
Although numerous initiatives have been implemented and evaluated to improve the initiation of statin therapy in patients when they are discharged from the hospital, little has been done to improve long-term patient adherence to statin therapy after discharge. We found that coronary artery stenosis of less than 75% was an independent predictor of discontinuing statin therapy. Doctors should reinforce the benefits of statin therapy with their patients to improve statin adherence. Additionally, we found that self-reports of adverse effects were also predictive of discontinuing statin therapy. This is interesting because it is known that some of these self-reported adverse effects such as dizziness and fatigue are not actually caused by statins. Thus, we recommend that doctors should change the statin type in the patients with adverse effects to improve adherence.
As for the self-reported reasons of non-adherence, 36.7% of the patients discontinued statin therapy in our study due to a lack of knowledge about its benefits. Another 19.4% of the patients in our study were told to stop statin therapy by doctors at their local clinics. Thus, this demonstrates that it is urgent to strengthen the education of both patients and doctors about the importance and therapeutic benefits of statin therapy. Additionally, we found that 12.2% of the patients reported that it was difficult to obtain their statin therapy. To address this, easier ways for patients to receive their medications should be further explored in the future.
Limitations
This study had some limitations. First, information about some confounders affecting the associations between exposure and CHD might be lacking in this historical cohort study, thus they might affect the comparability of the two cohorts. Second, recall bias existed because the days of medicine taking in the past were collected by a questionnaire; thus, the PDC might not be precisely calculated. Third, all CHD patients in our study were diagnosed with CHD and prescribed statins in a tertiary hospital, so statin adherence in these patients was likely to be better than China's average. Thus, caution should be taken when extending the conclusions of this study to other populations. Elsewhere in China, the factors associated with poor adherence in our study probably exist as well, and therefore the results of our study should be further proven by conducting a Chinese multi-center study in future. Fourth, because the follow-up of our study was not long (4–8 months post-discharge), we might not have found some outcomes associated with poor statin adherence long-term, and thus a study with a much longer follow-up period should be conducted in the future.
Conclusions
CHD patients with moderate stenosis or adverse effects tend to have poor statin adherence. The primary self-reported reasons for non-adherence included a lack of knowledge about the benefits of statin therapy, the treatment being halted at the advice of their doctor, and the difficulty in obtaining statins. Furthermore, non-adherence to statin therapy was significantly associated with an increased risk of cardiovascular events. To improve the statin adherence in these CHD patients, we should strengthen the education of patients and doctors to convey the importance of statin therapy and additionally make it easier for patients to obtain their statin medication.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Acknowledgement
This work was supported by the National Natural Science Foundation (Grant number 81570212) and the National Key Clinical Specialties Construction Program of China (Grant number 2011-170).
Footnotes
Peer review under responsibility of Chongqing Medical University.
References
- 1.Andrus B., Lacaille D. 2013 ACC/AHA guideline on the assessment of cardiovascular risk. J Am Coll Cardiol. 2014;63(25 Pt A):2886. doi: 10.1016/j.jacc.2014.02.606. [DOI] [PubMed] [Google Scholar]
- 2.Bangalore S., Breazna A., DeMicco D.A., Wun C.C., Messerli F.H. Visit-to-visit low-density lipoprotein cholesterol variability and risk of cardiovascular outcomes: insights from the TNT trial. J Am Coll Cardiol. 2015;65(15):1539–1548. doi: 10.1016/j.jacc.2015.02.017. [DOI] [PubMed] [Google Scholar]
- 3.Wang Y., Fu R., Wang Z. Assessing the quality of care for patients with acute myocardial infarction in China. Clin Cardiol. 2015;38(6):327–332. doi: 10.1002/clc.22405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Osterberg L., Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 5.Wei M.Y., Ito M.K., Cohen J.D., Brinton E.A., Jacobson T.A. Predictors of statin adherence, switching, and discontinuation in the USAGE survey: understanding the use of statins in America and gaps in patient education. J Clin Lipidol. 2013;7(5):472–483. doi: 10.1016/j.jacl.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 6.Rasmussen J.N., Chong A., Alter D.A. Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA. 2007;297(2):177–186. doi: 10.1001/jama.297.2.177. [DOI] [PubMed] [Google Scholar]
- 7.Choudhry N.K., Glynn R.J., Avorn J. Untangling the relationship between medication adherence and post-myocardial infarction outcomes: medication adherence and clinical outcomes. Am Heart J. 2014;167(1):51–58 e5. doi: 10.1016/j.ahj.2013.09.014. [DOI] [PubMed] [Google Scholar]
- 8.Upmeier E., Korhonen M.J., Rikala M., Helin-Salmivaara A., Huupponen R. Older statin initiators in Finland - cardiovascular risk profiles and persistence of use. Cardiovasc Drugs Ther. 2014;28(3):263–272. doi: 10.1007/s10557-014-6517-x. [DOI] [PubMed] [Google Scholar]
- 9.Lemstra M., Blackburn D. Nonadherence to statin therapy: discontinuation after a single fill. Can J Cardiol. 2012;28(5):567–573. doi: 10.1016/j.cjca.2012.03.018. [DOI] [PubMed] [Google Scholar]
- 10.Iqbal J., Zhang Y.J., Holmes D.R. Optimal medical therapy improves clinical outcomes in patients undergoing revascularization with percutaneous coronary intervention or coronary artery bypass grafting: insights from the Synergy between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial at the 5-year follow-up. Circulation. 2015;131(14):1269–1277. doi: 10.1161/CIRCULATIONAHA.114.013042. [DOI] [PubMed] [Google Scholar]
- 11.Wei L., Fahey T., MacDonald T.M. Adherence to statin or aspirin or both in patients with established cardiovascular disease: exploring healthy behaviour vs. drug effects and 10-year follow-up of outcome. Br J Clin Pharmacol. 2008;66(1):110–116. doi: 10.1111/j.1365-2125.2008.03212.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ye X., Gross C.R., Schommer J., Cline R., St Peter W.L. Association between copayment and adherence to statin treatment initiated after coronary heart disease hospitalization: a longitudinal, retrospective, cohort study. Clin Therapeut. 2007;29(12):2748–2757. doi: 10.1016/j.clinthera.2007.12.022. [DOI] [PubMed] [Google Scholar]