Abstract
Background
The internal jugular vein is one of the major vessels of the neck. The anatomy of this vessel is considered to be relatively stable. It is an important landmark for head and neck surgeons as well as the anaesthetists for both diagnostic and therapeutic purposes.
Methods
We present two case reports of the posterior tributary of the internal jugular vein and review the surgical literature regarding anatomical variations of the vein.
Findings
A total of 1197 patients from 27 published papers were included in this review. Of these patients, 99.6% had neck surgery and the rest were cadaveric dissections. Anatomical variations of the internal jugular vein were found in 2% of the patient cohort (n = 40). The majority of these patients had either bifurcation or fenestration of the vein. The posterior tributary of the internal jugular vein is unusual and is scarcely reported in the literature (three cases).
Knowledge of variations in the anatomy of the internal jugular vein assists surgeons in avoiding complications during neck surgery and preventing morbidity. Two rare cases of posterior branching of the internal jugular vein and experience of other surgeons are demonstrated in this extensive review.
Keywords: surgical variations, Internal Jugular Vein, Anatomical variations
Introduction
The vasculature of the head and neck is complex. A number of blood vessels traverse this region, which supply important and vital structures. Knowledge of the anatomy of the neck is particularly relevant to head and neck oncology and reconstructive surgeons and trainees, together with anaesthetists and intensivists.
Anatomical variations of the internal jugular vein (IJV) are uncommonly reported. Most of these reports are from anaesthetists and are based on evaluation of imaging for central venous access. The ‘surgical literature’ is solely based on the anatomical variations noted by the surgeons or anatomists during neck surgeries and teaching dissections. The anatomical features of the IJV are shown in Table 1.
Table 1.
Anatomical features of internal jugular vein.
| Feature | Description |
| Embryology | Derivatives of the right and left anterior cardinal veins (week 8 of intrauterine life)1 |
| Formation | Direct continuation of sigmoid sinus |
| Course | After exiting the jugular foramen, the IJV descends downwards in close proximity to the internal/common carotid arteries and the vagus nerve in the carotid sheath |
| Structure | Two dilated bulbs containing valves – superior (after exiting jugular foramen) and inferior (just before joining the subclavian vein is seen with its tributaries |
| Termination | Behind the sternal end of clavicle, the IJV joins the subclavian vein to form the brachiocephalic vein |
| Tributaries (all anterior) | 1. Inferior petrosal sinus |
| 2. Pharyngeal vein | |
| 3. Common facial vein | |
| 4. Lingual vein | |
| 5. Superior thyroid vein | |
| 6. Middle thyroid vein | |
| Surface landmarks | Band joining ear lobe to sternoclavicular joint |
Literature review
An extensive literature search to study the various anatomical variations of IJV as noted by surgeons and anatomists was conducted using electronic databases such as Medline, EMBASE and Google Scholar. A total of 124 papers were found, of which 27 were relevant (Table 2). A total of 40 anatomical variations were noted from a cohort of 1197 patients included in these 27 papers (Table 3).
Table 2.
Review of the surgical literature.
| No. | Paper | Year | Modality | Cohort | Feature | |
| Variation | Cases | |||||
| 1 | Deepak et al4 | 2015 | Surgical | 3 | Bifurcation | 1 |
| Trifurcation | 1 | |||||
| Posterior tributary | 1 | |||||
| 2 | Sankar et al5 | 2011 | Cadaveric | 1 | Fenestration | 1 |
| 3 | Contrera et al6 | 2016 | Surgical | 295 | Bifurcation | 1 |
| Fenestration | 1 | |||||
| Duplication | 1 | |||||
| 4 | Hashimoto et al7 | 2012 | Surgical | 123 | Fenestration | 4 |
| 5 | Prades et al8 | 2002 | Surgical | 750 | Duplication | 3 |
| 6 | Micozkadioglu et al9 | 2011 | Surgical | 1 | Posterior tributary | 1 |
| 7 | Moreno-Sánchez et al10 | 2015 | Surgical | 1 | Fenestration | 1 |
| 8 | Pegot et al11 | 2015 | Surgical | 1 | Fenestration | 1 |
| 9 | Downie et al12 | 2007 | Surgical | 1 | Duplication | 2 |
| 10 | Gardiner et al13 | 2002 | Surgical | 1 | Bifurcation | 1 |
| 11 | Nayak et al14 | 2006 | Surgical | 1 | Duplication | 1 |
| 12 | Turan-Ozdemir et al15 | 2004 | Surgical | 1 | Duplication | 1 |
| 13 | Ozturk et al16 | 2010 | Surgical | 1 | Fenestration | 1 |
| 14 | Ibrahim et al17 | 2016 | Surgical | 2 | Fenestration | 2 |
| 15 | Bacchoo et al18 | 2014 | Surgical | 1 | Duplication | 1 |
| 16 | Sidana et al19 | 2014 | Surgical | 1 | Duplication | 1 |
| 17 | Dogan et al20 | 2010 | Cadaveric | 1 | Duplication | 1 |
| 18 | Kapre et al21 | 2012 | Surgical | 1 | Duplication | 1 |
| 19 | Thakur et al22 | 2011 | Surgical | 1 | Fenestration | 1 |
| 20 | Wong et al23 | 2010 | Surgical | 1 | Duplication | 1 |
| 21 | Paolo et al24 | 2008 | Surgical | 1 | Fenestration | 1 |
| 22 | Nayak et al25 | 2017 | Cadaveric | 1 | Bifurcation | 1 |
| 23 | Bathala et al26 | 2015 | Surgical | 1 | Duplication | 1 |
| 24 | Cvetko27 | 2015 | Cadaveric | 1 | Fenestration | 1 |
| 25 | Cvetko et al28 | 2017 | Cadaveric | 1 | Fenestration | 1 |
| 26 | Anehosur et al29 | 2016 | Surgical | 1 | Posterior tributary | 1 |
| 27 | This paper | 2018 | Surgical | 2 | Posterior tributary | 2 |
Table 3.
Anatomical variations (from n = 1197 cases).
| Variation | Incidence (n) |
| Bifurcation | 4 |
| Duplication | 14 |
| Fenestration | 16 |
| Trifurcation | 1 |
| Posterior tributary | 5 |
| Total | 40 |
Methods
Case history: patient A
A 72-year-old man presented with a T1N0M0 squamous cell carcinoma of the right posterior buccal mucosa/retromolar region. He underwent prophylactic selective neck dissection (level 1–4) of the right neck as part of ablative and reconstructive surgery for this cancer. During the level 2–4 neck dissection, a posterior tributary was seen draining into the IJV from the medial aspect of sternocleidomastoid muscle (SCM) going antero-inferiorly joining the lower third of the IJV (Fig 1).
Figure 1.
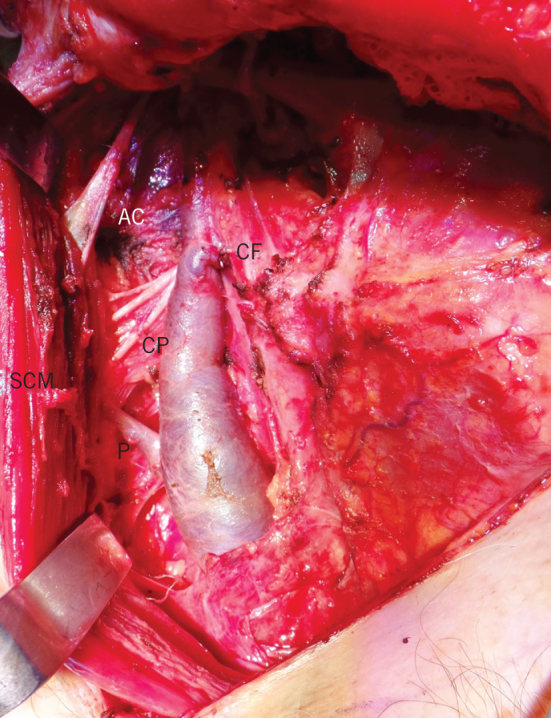
Posterior tributary of right internal jugular vein; AC – accessory nerve, CF – common facial vein (ligated), CP – cervical plexus, SCM – sternocleidomastoid, P – posterior tributary.
Case history: patient B
A 74-year-old woman presented with a lump in the right neck of four weeks’ duration. She had previously had squamous cell carcinoma of the left floor of the mouth and underwent ablative and reconstructive surgery, including neck dissection of the left side, 10 years ago. Ultrasound and fine-needle aspiration of this lump revealed a diagnosis of metastatic squamous cell carcinoma. As a consequence, the patient had selective neck dissection (level 1–4) of the right hand side on this occasion. A posterior tributary was seen draining the IJV arising from under the SCM joining the antero-inferior aspect of the lower-third of the IJV (Fig 2).
Figure 2.
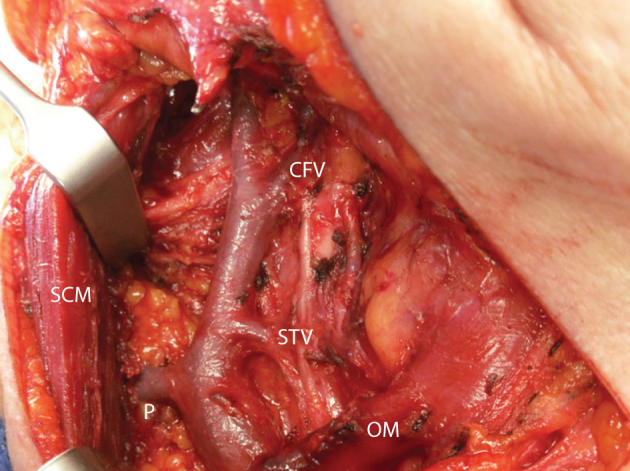
Posterior tributary of right internal jugular vein; CF – common facial vein, SCM – sternocleidomastoid, OM – omohyoid muscle, P – posterior tributary.
Findings
The paired jugular veins and the carotid arteries form the major vasculature of the head and neck region. Head and neck surgeons frequently perform neck dissections or cervical lymphadenectomy in a prophylactic and therapeutic role for patients with oral cancer. Anaesthetists and intensivists perform central venous access in patients who need central venous pressure monitoring, drug administration and volume resuscitation.1
Different variations reported in the surgical literature are presented (Fig 3). A predominance of duplication and fenestration was noted (31 of 40 cases). There is some ambiguity in terms of what surgeons considered as bifurcation as opposed to duplication. To ensure that a standardised approach is followed, the authors recommend using the level where the omohyoid muscle crosses the IJV as standard to discriminate between the two terms. If the IJV splits at or above the level of the omohyoid muscle, the terminology ‘bifurcation’ should be used. If the split occurs inferior to the level of omohyoid muscle the term ‘duplication’ should be used (Fig 4).
Figure 3.
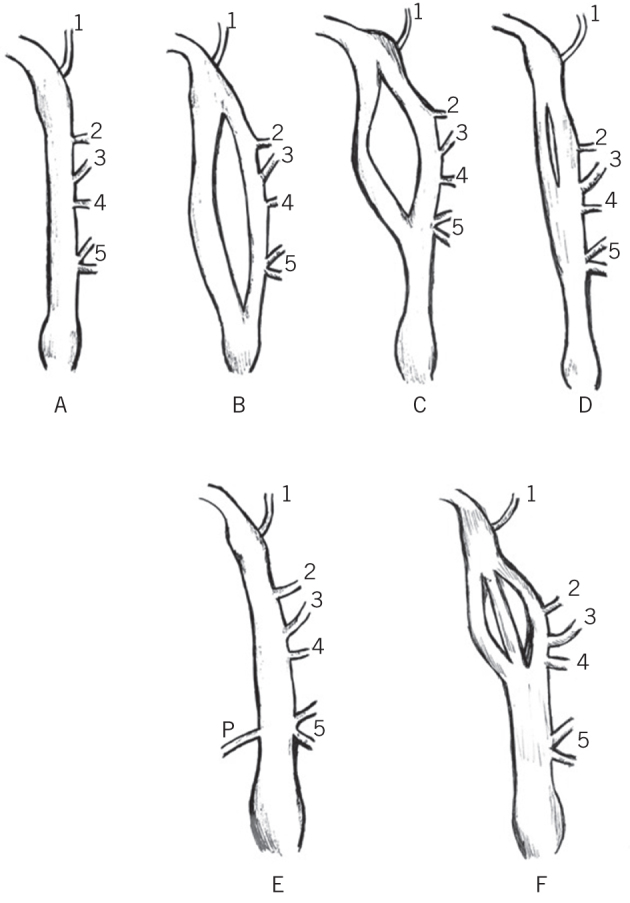
Anatomical variations of the internal jugular vein. A) Normal. B) Duplication. C) Bifurcation. D) Fenestration. E) Posterior tributary. F) Trifurcation. (1. inferior petrosal sinus; 2. pharyngeal vein; 3. common facial vein; 4. lingual vein; 5. thyroid veins; 6. posterior tributary).
Figure 4.
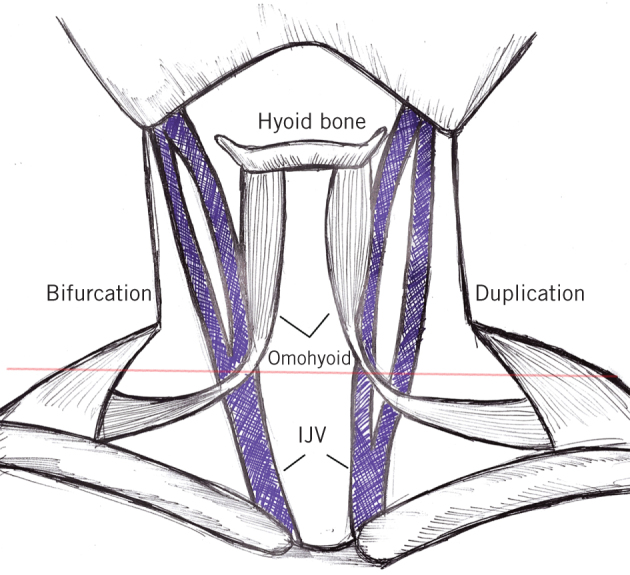
Diagrammatic representation of the relationship between the internal jugular vein (IJV) variations and the omohyoid muscle. The recommended definition of bifurcation (superior to the level of omohyoid) and duplication (inferior to the omohyoid) are shown (red line indicates the level where the omohyoid muscle crosses the IJV).
In more than two-third of the patients, these variations were noted to occur on the left side (Table 4). There is evidence to suggest that the right IJV is slightly larger and thicker in dimension compared with the left.2 Additionally, it is common knowledge that the ease of access and relatively less intimate carotid artery makes the right IJV a popular venous access site.
Table 4.
Laterality of anatomical variations.
| Laterality | Bifurcation | Duplication | Fenestration | Trifurcation | Posterior Tributary | Total (%) |
| Right | 1 | 3 | 5 | 0 | 3 | 12 (30) |
| Left | 3 | 11 | 10 | 1 | 2 | 28 (70) |
The posterior tributary has been reported in only five patients (including our cases) so far. Anehosur et al noted that the posterior tributary was actually a communication from the external jugular vein, which normally drains directly into the subclavian vein.3 Further dissection to assess this posterior tributary was not carried out in our case, as it was deemed unnecessary for satisfactory completion of the planned procedure.
Conclusions
Anatomical knowledge is one of the basic tenets of surgery. Variations in anatomy are well known amongst both anatomists and surgeons. Surgeons from different fields such as oral and maxillofacial surgery, otolaryngology, vascular, plastic and general surgery frequently operate in the head and neck region. We have endeavoured to improve knowledge, prevent morbidity and promote further understanding regarding these variations.
References
- 1.Collins P. Embryology and development. : Williams PL, Bannister LH, Berry MM, et al. (). Gray’s Anatomy: The Anatomical Basis of Medicine and Surgery. 38th ed Edinburgh: Churchill Livingston; 1995. p 327. [Google Scholar]
- 2.Saiki K, Tsurumoto T, Okamoto K et al. . Relation between bilateral differences in internal jugular vein caliber and flow patterns of dural venous sinuses. Anat Sci Int 2013; : 141–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith RN, Nolan JP. Central venous catheters. BMJ 2013; : f6570. [DOI] [PubMed] [Google Scholar]
- 4.Deepak CA, Sarvadnya JJ, Sabitha KS. Variant anatomy of internal jugular vein branching. Ann Maxillofac Surg 2015; : 284–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sankar KD, Bhanu PS. Variant anatomy of fenestrated internal jugular vein with unusual retromandibular and facial vein. Int J Anat Var 2011; : 144–148. [Google Scholar]
- 6.Contrera KJ, Aygun N, Ward BK et al. . Internal jugular vein duplication and fenestration: case series and literature review. Laryngoscope 2016; (7): 1,585–1,588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hashimoto Y, Otsuki N, Morimoto K et al. . Four cases of spinal accessory nerve passing through the fenestrated internal jugular vein. Surg Radiol Anat 2012; : 373–375. [DOI] [PubMed] [Google Scholar]
- 8.Prades JM, Timoshenko A, Dumollard JM et al. . High duplication of the internal jugular vein: clinical incidence in the adult and surgical consequences, a report of three clinical cases. Surg Radiol Anat 2002; : 129–132. [DOI] [PubMed] [Google Scholar]
- 9.Micozkadioglu SD, Erkan AN. Internal jugular vein anomaly: a lateral branch of the internal jugular vein in the neck. EJENTAS 2011; : 77–79. [Google Scholar]
- 10.Moreno-Sánchez M, Hernández Vila C, González-García R, Monje F. Fenestrated internal jugular vein: a rare finding in neck dissection. Int J Oral Maxillofac Surg 2015; (9): 1,086–1,087. [DOI] [PubMed] [Google Scholar]
- 11.Pegot A, Guichard B, Peron J-M, Trost O. Empty fenestration of the internal jugular vein: a rare phenomenon. Br J Oral Maxillofac Surg 2015; (1): 78–80. [DOI] [PubMed] [Google Scholar]
- 12.Downie SA, Schalop L, Mazurek JN et al. . Bilateral duplicated internal jugular veins: case study and literature review. Clin Anat 2007; : 260–266. [DOI] [PubMed] [Google Scholar]
- 13.Gardiner KJ, Irvine BW, Murray A. Anomalous relationship of the spinal accessory nerve to the internal jugular vein. Clin Anat 2002; : 62–63. [DOI] [PubMed] [Google Scholar]
- 14.Nayak BS. Surgically important variations of the jugular veins. Clin Anat 2006; : 544–546. [DOI] [PubMed] [Google Scholar]
- 15.Turan-Ozdemir S, Coskun H, Balban M. Phlebectasia of the external jugular vein associated with duplication of the internal jugular vein. Clin Anat 2004; : 522–525. [DOI] [PubMed] [Google Scholar]
- 16.Oztürk NC, Talas DÜ. Fenestration of internal jugular vein and relation to spinal accessory nerve: case report and review of the literature. Clin Anat 2010; (8): 883–884. [DOI] [PubMed] [Google Scholar]
- 17.Ibrahim B, Berania I, Moubayed SP et al. . Internal jugular vein duplication: anatomic relationship with the spinal accessory nerve. J Oral Maxillofac Surg 2016; : 1502.e1–1502.e4. [DOI] [PubMed] [Google Scholar]
- 18.Bachoo I, Evans B. Duplication of the lower third of the internal jugular vein – case report and surgical implications. Br J Oral Maxillofacial Surg 2014; (5): 461–463. [DOI] [PubMed] [Google Scholar]
- 19.Sidana S, Ahuja S. Empty fenestration of the internal jugular vein: a rare phenomenon. Br J Oral Maxillofacial Surg 2016; (4): 477–477. [DOI] [PubMed] [Google Scholar]
- 20.Dogan NU, Cicekcibasi AE, Fazliogullari Z et al. . Unilateral variations of vessels and nerves in the neck. Int J Morphol 2010; (3): 963–966. [Google Scholar]
- 21.Kapre M, Mangalgiri AS. Clinical importance of duplication of internal jugular vein. Indian J Otolaryngol Head Neck Surg 2012; (4): 386–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thakur JS, Sharma DR, Mohindroo NK. Double fenestration of the internal jugular vein: a rare anatomic variant. Ear Nose Throat J 2012; (10): 420, 427. [PubMed] [Google Scholar]
- 23.Wong B, Strachan D, Loney E. Duplication of internal jugular veins: case report. J Laryngol Otol 2010; (3): 341–344. [DOI] [PubMed] [Google Scholar]
- 24.Paolo B, Giuseppe C, Giulio G et al. . Internal jugular vein duplication. Indian J Plast Surg 2009; (2): 273–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nayak SB. Split internal jugular vein: surgical and radiological implications. Br J Oral Maxillofac Surg 2017; (8): 870–871. [DOI] [PubMed] [Google Scholar]
- 26.Bathala S, Makura ZG. Duplication of the right internal jugular vein: a case report. Ear Nose Throat J 2015; (6): 236–237. [DOI] [PubMed] [Google Scholar]
- 27.Cvetko E. Unilateral fenestration of the internal jugular vein: a case report. Surg Radiol Anat 2015; (7): 875–877. [DOI] [PubMed] [Google Scholar]
- 28.Cvetko E, Meznarič M. Concomitant fenestration and phlebectasia of the right internal jugular vein: a unique finding in anatomical dissection. Folia Morphol (Warsz) 2017; (3): 519–522. [DOI] [PubMed] [Google Scholar]
- 29.Anehosur V, Rajendiran S, Jayade GR, Kumar N. An unusual observation during neck dissection. J Maxillofac Oral Surg 2016; (Suppl 2): 306–308. [DOI] [PMC free article] [PubMed] [Google Scholar]


