Abstract
Background
Postradiation nasopharyngeal necrosis (PRNN) is a severe complication after radiotherapy in patients with nasopharyngeal carcinoma (NPC), which can severely affect the quality of life and threaten the patient’s life. Only 13.4%–28.6% of patients can be cured by traditional repeated endoscopic debridement. Here, we introduced an innovative curative-intent endoscopic surgery for PRNN patients and evaluated its clinical efficacy.
Methods
Clinical data of 72 PRNN patients who underwent radical endoscopic necrectomy, followed by reconstruction using a posterior pedicle nasal septum and floor mucoperiosteum flap were analyzed to determine the efficacy of this surgery. The endpoints were complete re-epithelialization of the nasopharyngeal defect, relief of headache, and overall survival (OS).
Results
All surgeries were successfully performed without any severe postoperative complications or death. The median value of numeric rating scales of pain decreased from 8 before surgery to 0 after surgery (P < 0.001). Fifty-one patients (70.8%) achieved complete re-epithelialization of the nasopharyngeal defect. The number of cycles of radiotherapy (odds ratio [OR], 7.254; 95% confidence interval [CI] 1.035–50.821; P = 0.046), postoperative pathological result (OR, 34.087; 95% CI 3.168–366.746; P = 0.004), and survival status of flap (OR, 261.179; 95% CI 17.176–3971.599; P < 0.001) were independent risk factors of re-epithelialization of the nasopharyngeal defects. Postoperative pathological result (hazard ratio [HR], 5.018; 95% CI 1.970–12.782; P = 0.001) was an independent prognostic factor for OS. The 2-year OS rate of the entire cohort was 77.9%.
Conclusion
Curative-intent endoscopic necrectomy followed by construction using the posterior pedicle nasal septum and floor mucoperiosteum flap is a novel, safe, and effective treatment of PRNN in patients with NPC.
Keywords: Nasopharyngeal carcinoma, Postradiation, Necrosis, Endoscopy, Necrectomy, Flap, Reconstruction, Re-epithelialization
Background
Nasopharyngeal carcinoma (NPC) is a common malignancy in Southeast Asia, particularly in the Guangdong province of China [1–3]. Radiotherapy is a fundamental treatment of NPC, with an observed 5-year overall survival (OS) rate of 68.2%–87.4% for patients with non-metastatic NPC [4–7]. However, radiotherapy may cause acute and chronic adverse effects on the normal tissues and bones surrounding the nasopharynx. As a severe adverse event after radiotherapy, postradiation nasopharyngeal necrosis (PRNN) can be observed in NPC patients after receiving high-dose irradiation [8–10]. It is commonly accompanied by a severe headache, foul odor, and epistaxis, which severely affect the patients’ quality of life [8, 9, 11]. Moreover, PRNN has been observed to contribute to 41.8%–42.9% of NPC patients’ death and to increase the risk of death by 69.2%–72.7% when the internal carotid artery (ICA) is exposed in the PRNN lesions [11, 12]. As such, ICA exposure has been found as an independent prognostic factor for patients with PRNN [8, 9, 11, 12]. Although repeated endoscopic debridement was reported as an effective traditional treatment of PRNN, only 13.4%–28.6% of these patients could be cured [11, 12], reflecting the possibility that the necrotic tissue could not be completely removed with or without efficient re-epithelialization of the nasopharyngeal defect.
Recently, we developed a new reconstruction technique using the posterior pedicle nasal septum and floor mucoperiosteum flap based on the posterior nasal septal artery to treat the nasopharyngeal defect, which has shown to promote wound healing and successfully resurface fresh, clean wounds after endoscopic nasopharyngectomy for patients with locally recurrent NPC [13]. However, whether this technique would be effective in treating old and infected PRNN wounds remains unclear. Thus, in this present study, we aimed to investigate and evaluate the clinical efficacy of a novel curative-intent endoscopic surgery comprising of radical endoscopic necrectomy and reconstruction of the nasopharyngeal defect using the nasal septum and floor mucoperiosteum flap to treat the PRNN lesions of NPC patients.
Patients and methods
Patient selection
From July 2010 to January 2017, NPC patients who had radical endoscopic necrectomy followed by reconstruction using a nasal septum and floor mucoperiosteum flap at the Sun Yat-sen University Cancer Center were selected for enrollment. This study was approved by the ethical committee of Sun Yat-sen University Cancer Center. Written informed consents were obtained from all patients.
The selection criteria were as follows: (1) a definitive history of radiotherapy, (2) diagnosed with PRNN based on clinical symptoms, imaging examinations, and preoperative biopsy, (3) their PRNN lesion was limited to a resectable region (i.e., the ICA was located at the outside margin of the lesion, the upper bound of the lesion consisted of the roof of the sphenoid sinus and ethmoid sinus, the posterior boundary of the lesion did not exceed the clivus, and the lower edge of axis was located at the lower bound of the lesion) so that the necrotic tissue could be completely removed with curative-intent.
The exclusion criteria for this study were as follows: (1) broad osteoradionecrosis of the skull base exceeding out of the resectable region (e.g. the lower edge of the axis) which would render the removal with curative-intent difficult and risky, (2) pathologically confirmed local recurrence with or without distant metastases before surgery, and (3) physical conditions unsuitable for surgery, such as heart failure, severe cardiac tamponade, unstable hemodynamics, severe nervous system abnormalities, clinically apparent malperfusion including lower limb, cerebral, coronary and renal malperfusion, and visceral ischemia or severe hepatic and renal abnormalities.
Surgery
Prior to surgery, a bacterial cultivation for purulent nasopharyngeal secretions and drug sensitivity assays were performed to identify sensitive antibiotics to be used postoperatively. For patients with ICA exposure in the PRNN lesions, a balloon occlusion test (BOT) was conducted to determine if the ICA could be safely occluded without causing cerebral ischemia [14, 15], and endovascular coiling embolization was required for some patients who suffered from vascular wall trauma or pseudoaneurysm, in order to avoid sudden fatal nasopharyngeal hemorrhage during surgery.
Radical endoscopic necrectomy was performed under general anesthesia using the endoscopic endonasal approach. The nasopharyngeal necrotic soft tissue (Figs. 1a, 2a) was completely removed using the XPS 3000 powered ENT system (Medtronic, Minneapolis, MN, USA) until a slight bleeding was observed (Fig. 1b), thereby exposing the underlying normal fresh tissue. Electrocoagulation was then performed to remove tough connective tissues surrounding the fresh tissues using a long head electrotome (Covidien, Saint Louis, MO, USA). If the skull base bone and anterior arch of atlas were observed to be necrotized, they were removed using a high-speed electric micro-drill (Stryker, Kalamazoo, MI, USA). Surgical specimens from the lateral and basal surgical margins, any tissue suspected to be a recurrent tumor, and the necrotic tissues removed were sent for pathological examination. One side flap, typically the ipsilateral side, was harvested after complete radical endoscopic necrectomy, as reported in our previous study [13]. According to the area of the nasopharyngeal defect, except for a narrow posterior pedicle above the nasal lumen, the flap which contained the posterior nasal septal artery was partially or completely separated and gently rotated backward to cover the defect (Figs. 1c, 2b). If the one-side flap was not large enough to cover the entire defect, the flap on the opposite side of the nasal septum was also simultaneously harvested with the inferior turbinate mucoperiosteum being separated to cover the oropharyngeal defect, especially when the necrotic anterior arch of the atlas was removed. Subsequently, an absorbable gelatin sponge was gently placed into the nasopharyngeal cavity to support the flap. A Rapid Rhino Nasal Pac with Gel Knit (Applied Therapeutics, Tampa, FL, USA) was used to hold up the absorbable gelatin sponge from the nasal cavity to avoid it falling into the oropharyngeal cavity. If the flap necrotized after being harvested, the flap on the opposite side of nasal septum was harvested as a remedial measure. If the flap with two bared sides of the nasal septum were harvested, the nasal septum bone would be removed.
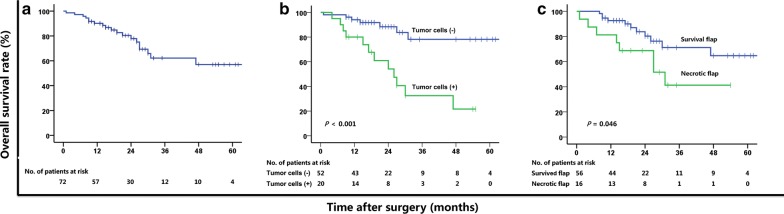
Fig. 1.
The radical endoscopic necrectomy followed by reconstruction using a posterior pedicle nasal septum and floor mucoperiosteum flap to resurface the nasopharyngeal defects in a 62-year-old man with post-radiation nasopharyngeal necrosis (PRNN). a–d display the anterior views of the nasal and nasopharyngeal cavity. a After full exposure of the nasopharyngeal cavity, the PRNN (indicated by the red arrow) in the roof of the posterior wall of the nasopharyngeal cavity was observed after removing purulent nasopharyngeal secretions using a steel suction apparatus. b After radical endoscopic necrectomy, the skull base (indicated by the blue arrow) and normal tissues were exposed. c In the ipsilateral nasal cavity, the flap (indicated by the yellow arrow) re-covered the nasopharyngeal defect. d Eight weeks after surgery, the NSFF completely relined the nasopharyngeal mucosa. ET eustachian tube, NSFF posterior pedicle nasal septum, and floor mucoperiosteum flap
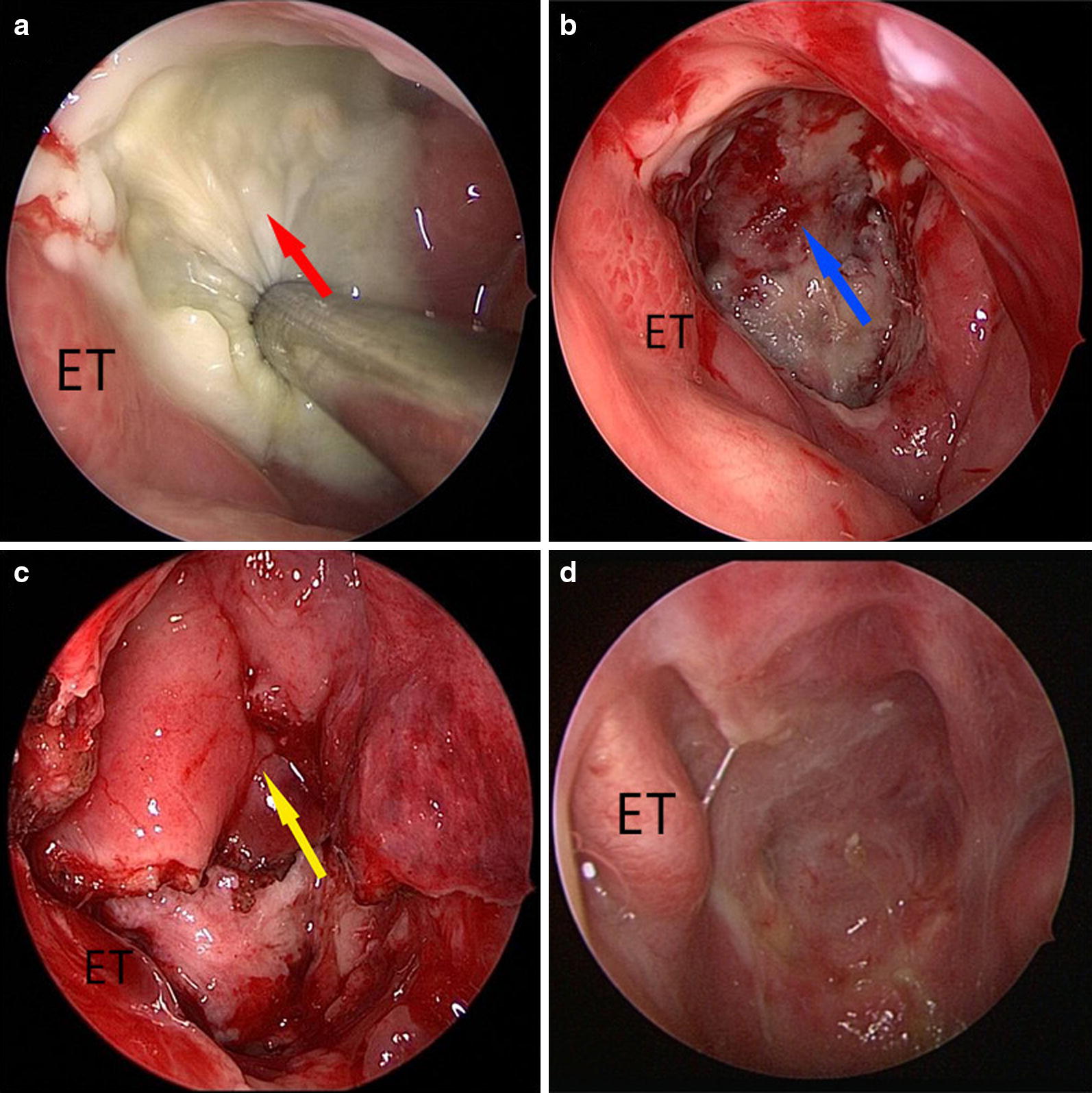
Fig. 2.
Contrast-enhanced sagittal magnetic resonance imaging (MRI) of the head and neck of a patient before and after surgery. a PRNN (indicated by the red arrow) was located in the roof of the posterior wall of the nasopharyngeal cavity and oral pharynx as shown on the preoperative MRI. b The flap (indicated by the blue arrow) re-surfaced the defect after radical endoscopic necrectomy, with good blood supply at 2 weeks after surgery. c The flap completely relined the nasopharyngeal mucosa at 8 weeks after surgery
Antibiotic therapy based on the result of bacterial cultivation before the surgery was administered for 5–7 days after surgery. Magnetic resonance imaging (MRI) of the nasopharynx was performed within 2 weeks after the operation to evaluate the flap blood supply (Fig. 2b). When signs of poor blood supply were observed on the MRI, balloon outgassing was performed to relieve the flap compression, and additional treatment with vasoactive drugs was prescribed. After removing the nasal packing on the 7th postoperative day, the patients were prescribed regional perfusion with recombinant human epidermal growth factor derivative liquid (Watsin Genetech Ltd, Shenzhen, Guangdong, P.R. China) to keep the wound humid, and endoscopic nasal cleanup was performed every 2–4 weeks until the flap was completely epithelialized and the entire defect was relined (Figs. 1d, 2c).
Evaluation of treatment efficacy
Locoregional recurrence in this study was defined as tumor recurrence identified in the PRNN lesion with positive pathology at the time of surgery or if the PRNN lesion had negative pathology at the time of surgery but the patient developed recurrence during follow-up examinations.
The primary endpoint of this study was the relining of the nasopharyngeal defect which was defined as the complete re-epithelialization of the nasopharyngeal cavity, upon nasal endoscopic examination, and the mucosa; upon MRI examination [8]. The observed changes in headache episodes and OS were defined as the secondary endpoints. The Numeric Rating Scales (NRS) of pain was used to evaluate headaches level before and within 3 months after surgery. The patients were requested to rate their level of headache on a scale from 0 to 10, with 0 being none and 10 being unbearable. OS was calculated from the date of PRNN surgery till the date of last follow-up (September 20, 2017) or death.
Follow-up
All patients were followed-up to assess the surgical outcomes, disease status, and performance status every 3 months in the first 3 years after the operation, every 6 months in the fourth and fifth years, and annually thereafter. Follow-up examinations included complete physical examinations, chest X-ray, abdominal ultrasonography, MRI of the head and neck, and/or whole-body bone scan.
Statistical analysis
For all cohorts, categorical data were described as numbers and percentages, and continuous data are presented as medians. Categorical data were analyzed using the Chi-square test or Chi-square test with continuity correction. Wilcoxon rank-sum test was conducted for ranked data. Univariate logistic regression was used to determine the associations between clinicopathological characteristics and complete re-epithelialization of the nasopharyngeal defect. Variables associated with severe necrosis (P < 0.1) in univariate logistic regression analysis were included in multivariate logistic regression models to adjust for confounding effects. Survival results were calculated using the Kaplan–Meier method, and their differences were compared using the log-rank test. Covariates significantly associated with prognosis detected in univariate analysis (P < 0.1) were included in a multivariate Cox proportional hazards model to identify independent prognostic factors. All analyses were performed using the SPSS software (version 16.0, SPSS, Chicago, IL, USA), and a two-tailed P value less than 0.05 was considered as statistically significant.
Results
Patient characteristics and surgical outcomes
Clinical records of 72 NPC patients, including 52 males and 20 females, with a median age of 51 years (range, 32–73 years) were selected. PRNN was diagnosed after one cycle of irradiation in 50 patients, with a median interval of 8 months (range, 1–240 months), and after two cycles of irradiation in 22 patients, with a median interval of 3.5 months (range, 0–103 months). PRNN was observed to occur within 3 months after radiotherapy (acute necrosis) in 17 patients and after 3 months (chronic necrosis) in 55 patients. Fifty-one patients presented with osteoradionecrosis, which included 5 patients who had combined necrosis of the anterior arch of the atlas. Fourteen patients presented with radiation-induced encephalopathy or temporal lobe necrosis with a median interval of 8 months (range, 2–150 months). Among the 25 patients whose ICA was exposed in their necrotic lesion, 24 had BOT intervention, and the remaining 1 patient rejected the BOT intervention. Among the 24 patients who underwent the BOT intervention, 14 of them underwent endovascular coiling embolization after the BOT.
Endoscopic necrectomy followed by reconstruction using the nasal septum and floor mucoperiosteum flap was successfully performed in all patients without any severe postoperative complications or death. The median surgical time was 110 min (range, 50–180 min) with little blood loss (median, 50 mL; range, 10–300 mL). Two patients had their flaps simultaneously harvested from both sides of the nasal septum in one operation. One patient underwent a repeated operation to harvest the flap on the opposite side of the nasal septum because the one-side flap necrotized 1 week after the surgery. Six patients had their inferior turbinate mucoperiosteum combined with the flap. Overall, the flap survived in 56 (77.8%) patients, and for the remaining 16 (22.2%) patients, their flaps became necrotic due to ischemia (Table 1). No clinical characteristic was significantly associated with the status of the flap (Table 2). Twenty patients were diagnosed with recurrent undifferentiated non-keratinizing carcinoma according to the findings of postoperative pathological assessments for deep surgical margins (Table 1).
Table 1.
Associations between the clinical characteristics and the re-epithelialization of the nasopharyngeal defects for patients with postradiation nasopharyngeal necrosis who underwent radical necrectomy followed by reconstruction using posterior pedicle nasal septum and floor mucoperiosteum flap (NSFF)
| Clinical characteristic | Total [cases (%)] | Re-epithelialization [cases (%)] | Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|---|---|---|
| Survived | Necrotized | P value | OR (95% CI) | P value | OR (95% CI) | ||
| Total | 72 | 51 (70.8) | 21 (29.2) | ||||
| Gender | |||||||
| Female | 20 (27.8) | 11 (21.6) | 9 (42.9) | ||||
| Male | 52 (72.2) | 40 (78.4) | 12 (57.1) | 0.072 | 2.727 (0.915–8.127) | 0.778 | 1.328 (0.185–9.533) |
| Age (years) | |||||||
| < 51 | 32 (44.4) | 21 (41.2) | 11 (52.4) | ||||
| ≥ 51 | 40 (55.6) | 30 (58.8) | 10 (47.6) | 0.386 | 0.636 (0.229–1.768) | ||
| Cycles of radiotherapy | |||||||
| One | 50 (69.4) | 40 (78.4) | 10 (47.6) | ||||
| Two | 22 (30.6) | 11 (21.6) | 11 (52.4) | 0.012 | 4.000 (1.351–11.845) | 0.046 | 7.254 (1.035–50.821) |
| Necrosis-free interval | |||||||
| Acute necrosis | 17 (23.6) | 14 (27.5) | 3 (14.3) | ||||
| Chronic necrosis | 55 (76.4) | 37 (72.5) | 18 (85.7) | 0.240 | 2.270 (0.578–8.919) | ||
| Carotid artery exposure | |||||||
| Yes | 25 (34.7) | 19 (37.3) | 6 (28.6) | ||||
| No | 47 (65.3) | 32 (62.7) | 15 (71.4) | 0.483 | 0.674 (0.223–2.032) | ||
| Osteoradionecrosis | |||||||
| Yes | 51 (70.8) | 35 (68.6) | 16 (76.2) | ||||
| No | 21 (29.2) | 16 (31.4) | 5 (23.8) | 0.522 | 1.463 (0.456–4.692) | ||
| Postoperative pathological result | |||||||
| Negative | 52 (72.2) | 42 (82.4) | 10 (47.6) | ||||
| Positive | 20 (27.8) | 9 (17.6) | 11 (52.4) | 0.004 | 5.133 (1.677–15.714) | 0.004 | 34.087 (3.168–366.746) |
| Status of the NSFF flap | |||||||
| Survived | 56 (77.8) | 49 (96.1) | 7 (33.3) | ||||
| Necrotized | 16 (22.2) | 2 (3.9) | 14 (66.7) | < 0.001 | 49.000 (9.133–262.904) | < 0.001 | 261.179 (17.176–3971.599) |
OR odds ratio, CI confidence interval, NSFF posterior pedicle nasal septum, and floor mucoperiosteum flap
Table 2.
Associations between clinical characteristics and the status of posterior pedicle nasal septum and the floor mucoperiosteum flap
| Characteristic | Status of the flap [cases (%)] | P value | |
|---|---|---|---|
| Survived | Necrotized | ||
| Total | 56 | 16 | |
| Gender | 0.193* | ||
| Female | 13 (23.2) | 7 (43.8) | |
| Male | 43 (76.8) | 9 (56.2) | |
| Age (years) | 0.949 | ||
| < 51 | 25 (44.6) | 7 (43.8) | |
| ≥ 51 | 31 (55.4) | 9 (56.2) | |
| Cycles of radiotherapy | 0.321* | ||
| One | 41 (73.2) | 9 (56.2) | |
| Two | 15 (26.8) | 7 (43.8) | |
| Necrosis-free interval | 0.394* | ||
| Acute necrosis | 15 (26.8) | 2 (12.5) | |
| Chronic necrosis | 41 (73.2) | 14 (87.5) | |
| Carotid artery exposure | 0.741 | ||
| Yes | 20 (35.7) | 5 (31.2) | |
| No | 36 (64.3) | 11 (68.8) | |
| Osteoradionecrosis | 0.177* | ||
| Yes | 37 (66.1) | 14 (87.5) | |
| No | 19 (33.9) | 2 (12.5) | |
| Postoperative pathological result | 0.972* | ||
| Negative | 41 (73.2) | 11 (68.8) | |
| Positive | 15 (26.8) | 5 (31.2) | |
* P values were calculated using the Chi square test with continuity correction
Treatment efficacy
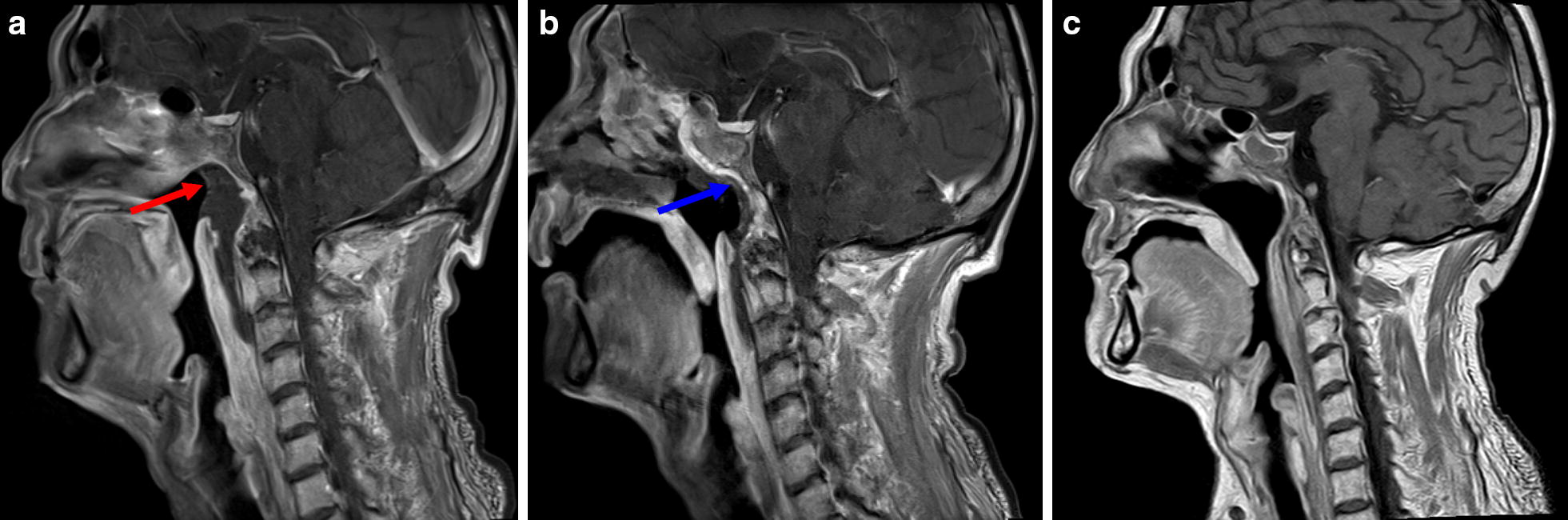
During the follow-up period (median, 20 months; range, 1.0–77.0 months), the nasopharyngeal defects were completely re-epithelialized in 51 (70.8%) patients, and the median time to re-epithelialization was 2.0 months (range, 1.1–3.3 months). The flaps did not show favorable re-epithelialization in the remaining 21 (29.2%) patients. Among the 50 patients who were receiving 1 course of radiotherapy, the nasopharyngeal defects were completely re-epithelialized in 40 (80.0%) patients, and the median time to re-epithelialization was 2.0 months (range, 1.3–26.0 months). Among the 22 patients who were receiving 2 courses of radiotherapy, the nasopharyngeal defects were completely re-epithelialized in 11 (50.0%) patients, and the median time to re-epithelialization was 1.9 months (range, 1.1–3.0 months). The median value of NRS of headache was 8 before surgery and decreased to 0 within 3 months after surgery (P < 0.001) (Table 3). Among the enrolled 72 patients, 19 (26.4%) died: 13 (18.1%) due to locoregional recurrence, metastases to distant organs, or both, 2 (2.7%) died from intracranial infection, 3 (4.2%) from nasopharyngeal hemorrhage, and 1 (1.4%) from aspiration pneumonia. Among the 20 patients who were diagnosed with necrosis combined with locoregional recurrence, 12 (60.0%) died: 10 (50.0%) due to locoregional recurrence, metastases to distant organs, or both, one (5.0%) died of intracranial infection and 1 (5.0%) of nasopharyngeal hemorrhage. The 2-year OS rate of the entire cohort was 77.9% (Fig. 3a).
Table 3.
Distribution of the headache levels measured using the numeric rating scales (NRS) among the patients with postradiation nasopharyngeal necrosis who underwent radical necrectomy followed by reconstruction
| Level of NRS | Time point (cases) | |
|---|---|---|
| Before surgery | Within 3 months after surgery | |
| 0 | 8 | 49 |
| 1 | 0 | 2 |
| 2 | 1 | 1 |
| 3 | 3 | 2 |
| 4 | 1 | 0 |
| 5 | 4 | 0 |
| 6 | 7 | 0 |
| 7 | 8 | 4 |
| 8 | 13 | 1 |
| 9 | 10 | 3 |
| 10 | 17 | 10 |
Fig. 3.
Kaplan–Meier curves illustrating the overall survival (OS) of a all patients, b patients stratified by their postoperative pathological result, and c patients stratified by the status of the flap. (+) positive, (−) negative, Path pathology
Among the 25 patients whose ICA was found to be exposed in the necrotic lesion, 19 patients had favorable re-epithelialization with no recorded death, and 6 patients showed did not show favorable re-epithelialization, which comprised of 1 died due to tumor progression, 1 from intracranial infection, 1 from aspiration pneumonia, and 3 were still alive at the last follow-up.
Independent risk factors for the re-epithelialization and survival
From the univariate logistic regression analysis, cycles of radiotherapy (P = 0.012), postoperative pathological result (P = 0.004), and survival status of the posterior pedicle nasal septum and floor mucoperiosteum flap (P < 0.001) were found to be significantly associated with the re-epithelialization of nasopharyngeal defects. Multivariable logistic regression analysis indicated that these three clinicopathological characteristics were also independent predictors of re-epithelialization (Table 1). Next, we further analyzed the predictors of nasopharyngeal defect re-epithelialization in the 52 PRNN patients with negative pathology at the time of surgery and as shown in Table 4, the number of cycles of radiotherapy (P = 0.022) and the status of the flap (P < 0.001) were significantly associated with the re-epithelialization.
Table 4.
Predictors of nasopharyngeal defect re-epithelialization of patients with postradiation nasopharyngeal necrosis but with negative pathology for tumor recurrence at the time of surgery
| Clinical characteristic | Total [cases (%)] | Status of the re-epithelialization [cases (%)] | Univariate logistic regression analysis | ||
|---|---|---|---|---|---|
| Survived | Necrotized | P-value | OR (95% CI) | ||
| Gender | 0.232 | 2.444 (0.565–10.570) | |||
| Female | 13 (25.0) | 9 (21.4) | 4 (40) | ||
| Male | 39 (75.0) | 33 (78.6) | 6 (60) | ||
| Age (years) | 0.405 | 0.551 (0.135–2.241) | |||
| < 51 | 25 (48.1) | 19 (45.2) | 6 (60) | ||
| ≥ 51 | 27 (51.9) | 23 (54.8) | 4 (40) | ||
| Cycles of radiotherapy | 0.022 | 5.500 (1.272–23.782) | |||
| One | 37 (71.2) | 33 (78.6) | 4 (40) | ||
| Two | 15 (28.8) | 9 (21.4) | 6 (60) | ||
| Necrosis-free interval | 0.296 | 3.194 (0.362–28.180) | |||
| Acute necrosis | 12 (23.1) | 11 (26.2) | 1 (10) | ||
| Chronic necrosis | 40 (76.9) | 31 (73.8) | 9 (90) | ||
| Carotid artery exposure | 0.978 | 0.980 (0.240–4.004) | |||
| Yes | 31 (56.9) | 25 (59.5) | 6 (60) | ||
| No | 21 (40.4) | 17 (40.5) | 4 (40) | ||
| Osteoradionecrosis | 0.173 | 4.500 (0.517–39.149) | |||
| Yes | 37 (71.2) | 28 (66.7) | 9 (90) | ||
| No | 15 (28.8) | 14 (33.3) | 1 (10) | ||
| Status of the flap | < 0.001 | 180.000 (14.672–2208.254) | |||
| Survived | 41 (78.8) | 40 (95.2) | 1 (10) | ||
| Necrotized | 11 (21.2) | 2 (4.8) | 9 (90) | ||
OR odds ratio, CI confidence interval
The 2-year OS rate observed in patients with negative postoperative pathology was higher than that in patients with positive postoperative pathology (88.4% vs. 54.2%, P < 0.001; Fig. 3b). For patients with surviving flap, their 2-year OS rate was higher than that in patients with a necrotic flap (80.3% vs. 68.8%, P = 0.046; Fig. 3c). In addition, postoperative pathological result (hazard ratio [HR], 5.018; 95% CI 1.970–12.782; P = 0.001) was an independent prognostic factor for OS in the multivariate Cox model (Table 5). For patients with negative pathology of tumor recurrence in their PRNN lesion at the time of surgery, the 2-year OS rate of those with survived flap was significantly higher than those with necrotic flap (90.1% vs. 81.8%, P = 0.043) (Table 6).
Table 5.
Cox univariate and multivariate analyses of the prognostic factors related to overall survival (OS) for the patients with postradiation nasopharyngeal necrosis
| Clinical characteristic | 2-year OS rate (%) | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|---|
| P value | HR (95% CI) | P value | HR (95% CI) | ||
| Gender | 0.601 | 1.295 (0.491–3.412) | |||
| Female | 84.0 | ||||
| Male | 76.0 | ||||
| Age (years) | 0.331 | 1.589 (0.625–4.039) | |||
| < 51 | 84.7 | ||||
| ≥ 51 | 72.7 | ||||
| Cycles of radiotherapy | 0.717 | 1.197 (0.453–3.163) | |||
| One | 80.8 | ||||
| Two | 71.9 | ||||
| Necrosis-free interval | 0.617 | 1.372 (0.397–4.737) | |||
| Acute necrosis | 86.3 | ||||
| Chronic necrosis | 75.7 | ||||
| Carotid artery exposure | 0.817 | 1.122 (0.423–2.975) | |||
| Yes | 68.6 | ||||
| No | 82.1 | ||||
| Osteoradionecrosis | 0.607 | 0.782 (0.308–1.991) | |||
| Yes | 81.2 | ||||
| No | 71.4 | ||||
| Postoperative pathological result | 0.001 | 5.026 (1.974–12.799) | 0.001 | 5.018 (1.970–12.782) | |
| Negative | 88.4 | ||||
| Positive | 54.2 | ||||
| Status of the flap | 0.055 | 2.467 (0.982–6.195) | 0.056 | 2.442 (0.978–6.099) | |
| Survived | 80.3 | ||||
| Necrotized | 68.8 | ||||
OS overall survival, HR hazard ratio, CI confidence interval
Table 6.
The prognostic factors for overall survival (OS) for the patients with postradiation nasopharyngeal necrosis with negative pathology at the time of surgery
| Clinical characteristic | 2-year OS rate (%) | P-value |
|---|---|---|
| Gender | ||
| Female | 100 | |
| Male | 84.9 | 0.613 |
| Age (years) | ||
| < 51 | 96 | |
| ≥ 51 | 81.6 | 0.295 |
| Cycles of radiotherapy | ||
| One | 86.5 | |
| Two | 93.3 | 1.000 |
| Necrosis-free interval | ||
| Acute necrosis | 91.7 | |
| Chronic necrosis | 87.7 | 0.443 |
| Carotid artery exposure | ||
| Yes | 75 | |
| No | 96.8 | 0.219 |
| Osteoradionecrosis | ||
| Yes | 93.9 | |
| No | 73.8 | 0.374 |
| Status of the NSFF flap | ||
| Survived | 90.1 | |
| Necrotized | 81.8 | 0.043 |
| All patients | 88.4 | |
NSFF posterior pedicle nasal septum, and floor mucoperiosteum flap
Discussion
Postradiation nasopharyngeal necrosis has a significant impact on patients’ quality of life and contributes to a high mortality rate [10–12]. Little is known about the best therapeutic management of PRNN. In the present study, we have designed a curative-intent endoscopic surgery comprising of radical endoscopic necrectomy and reconstruction of the nasopharyngeal defect using the nasal septum and floor mucoperiosteum flap and analyzed the treatment outcomes in a cohort of 72 NPC patients. All patients had successful surgical reconstruction of their infected PRNN wounds without any severe postoperative complications or death, of which fifty-one patients (70.8%) achieved successful complete re-epithelialization of their nasopharyngeal defect. The median value of NRS for headache was observed to decrease from a scale of 8 before surgery to scale 0 within 3 months after surgery (P < 0.001). The 2-year OS rate of the entire cohort was 77.9%. These results indicated that the proposed surgery could completely remove necrotic tissues, efficiently re-epithelialize nasopharyngeal defects, effectively relieve headache, and increase the OS rate of NPC patients with PRNN lesions, as compared to the results in previously published studies for which the risk of death ranged between 41.8% and 42.9% [9, 11, 12].
Since June 2006, we performed repeated endoscopic debridement of the nasopharyngeal necrotic tissues to obtain fresh wounds, which was helpful to control infections, inhibit necrosis, and relieve symptoms of headache and foul odor [11, 12, 16]. However, these procedures were lengthy and required multiple surgeries. Furthermore, most patients could not achieve complete re-epithelialization of the nasopharyngeal defect. Also, considering that when the ICA is exposed to the PRNN lesions, any aggressive endoscopic debridement is not advocated to prevent the ICA rupture and severe massive bleeding. As such, an efficient technique to remove the necrotic lesion, and to safely and completely re-epithelialize the defect had to be developed as a key step for successful treatment of PRNN lesions.
Endoscopic endonasal approaches have been rapidly developed in recent years. Chen et al. [17, 18]. reported that en-bloc excision of nasopharyngeal tumor lesions could be successfully achieved with endoscopic nasopharyngectomy through endoscopic endonasal approaches for recurrent NPC. Therefore, we thought of applying a similar technique to completely remove the PRNN lesions [17–21]. As such, we designed a novel radical endoscopic necrectomy with curative intent, in which we observed that the 72 patients who underwent this procedure had no severe postoperative complications or death. Moreover, preoperative BOT was used to determine whether the ICA could be safely occluded without cerebral ischemia when the ICA was exposed to the PRNN lesions. Furthermore, endovascular coiling embolization was performed for patients suffering from vascular wall trauma or pseudoaneurysm when the result of BOT was negative. These methods successfully solved the issues regarding intraoperative or postoperative sudden rupture and fatal nasopharyngeal hemorrhage of the ICA and could be additionally helpful to give surgeons enough confidence for the removal of necrotic tissues even they are close to the ICA [14, 15]. Even if the patient had intraoperative or postoperative sudden rupture or even massive nasopharyngeal hemorrhage of the ICA when the BOT result was negative, they could be rescued by endovascular coiling embolization.
In addition, how to effectively and promptly re-epithelialize the nasopharyngeal defect after radical endoscopic debridement is another key issue in treating PRNN. Cornes et al. [22] reported that the use of locoregional pedicle flaps could increase the wound healing rate by 12%–46% as compared with those not using pedicle flaps in the treatment of neck necrosis in patients with head and neck squamous cell carcinoma which was followed by brachytherapy. Hao et al. [23] proposed that healthy vascularized pedicle tissues should be used in reconstruction as this could bring new blood flow and nutrition to assist wound healing and tissue regeneration for the treatment of osteoradionecrosis at the head and neck area. Open salvage surgery following vascularized flap was also reported as an effective treatment for tissue necrosis after irradiation for head and neck cancers [24, 25]. However, until now, there have been no published studies regarding the treatment of PRNN using vascularized free flap in NPC patients.
Vascularized free flap is often used in open surgeries because ample open space is required to insert the micro-vascularized free flap into the nasopharyngeal cavity. However, this type of flap is obviously not suitable for endoscopic endonasal approaches because of the narrow surgical field [13, 26]. We had previously successfully applied nasal septum and floor mucoperiosteum flap to resurface fresh and clean nasopharyngeal defects to promote wound healing in recurrent NPC patients [13]. However, whether the flap would be effective in repairing old and infected necrotic wounds in PRNN remained unknown, until the results of this present study where we demonstrated that the nasal septum and floor mucoperiosteum flap could be useful to repair infected necrotic wounds. Further, we speculated that the survival flap could serve as a barrier to efficiently protect the ICA and as our data demonstrated, the survival flap was a protective factor for the re-epithelialization of the nasopharyngeal defect. We also found that larger number cycles of radiotherapy was an adverse independent predictor of re-epithelialization, and we believe that the reason for this might be because radiotherapy often leads to insufficient local tissue blood flow, oxygen supply, and microcirculation dysfunction; as this was particularly obvious in patients who received two cycles of radiotherapy [8, 23]. Moreover, patients who received two cycles of irradiation developed PRNN faster than those who received one cycle of irradiation (median time to develop PRNN after: one cycle vs. two cycles of irradiation, 8 months vs. 3.5 months, respectively). This suggests that oncologists should be more careful in choosing re-irradiation for recurrent NPC.
During radical endoscopic debridement, we found that some patients presented with recurrent cancer lesion in the deep surgical margins after surgery, despite that these individuals had no signs of recurrence prior to surgery. This finding suggests that superficial histopathological examination may not be sufficient to identify deeply located recurrent lesion, and this phenomenon has not yet been reported in previous studies. Moreover, the postoperative pathologic result was observed to be an independent prognostic factor for OS and a predictor of curing PRNN. For those patients suffering from PRNN combined with recurrent tumor, the treatment strategy would be much more difficult, whereby both the anti-cancer treatment and anti-necrosis treatment would be simultaneously equally important. Therefore, how to differentiate the PRNN from cancerous ulcer is very important. Unfortunately, these lesions are difficult to differentiate solely based on the current imaging techniques, such as MRI and positron emission tomography–computed tomography (PET/CT). In contrast, as demonstrated by our pathological results, we suggest that deep biopsy and/or radical endoscopic surgery might be a better alternative to identify such deeply located recurrence and relieve associated headaches. Based on these findings, we recommend radical endoscopic surgery for patients with PRNN, whether combined with or without deeply recurrent tumor.
Despite the promising results of this present study, there are several potential limitations worth mentioning. First, the data of this study were retrospectively analyzed, and prospective studies with a larger cohort are required to validate these results. Second, the number of patients was limited, and all of them were treated at a single cancer center. Third, the median follow-up time was relatively short (20 months), and we expect future studies to have a longer follow-up time.
Conclusions
Curative-intent endoscopic necrectomy followed by reconstruction using the posterior pedicle nasal septum and floor mucoperiosteum flap is a novel, safe, and effective treatment of PRNN in patients with NPC. However, it should be further validated with a long follow-up period.
Authors’ contributions
Ming-Yuan Chen, Xiong Zou, Shun-Lan Wang, and You-Ping Liu conceptualized and designed the study, conducted data analysis, and interpreted the data. All authors participated in drafting the manuscript and revising it critically. All authors read and approved the final manuscript.
Acknowledgements and funding
This work was supported by the National Natural Science Foundation of China (Nos. 81572912, 81772895, and 81572848), Guangdong Public Welfare Research and Capacity Building Projects (2014B020212005), the Program of Sun Yat-Sen University for Clinical Research 5010 Program (No. 201310 and No. 2015011), the Major Project of Sun Yat-Sen University for the New Cross Subject, the Special Support Program for High-level Talents in Sun Yat-Sen University Cancer Center (2015076316), and the National Key Research and Development Program of China (2016YFC0905000), Guangdong Province Science and Technology Development Special Funds (Frontier and Key Technology Innovation Direction—Major Science and Technology Project, 703040078088) and Guangzhou Science and Technology Planning Project—Production and Research Collaborative Innovation Major Project (201604020182).
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All patients in the study were treated in Sun Yat-Sen University Cancer Center, the data and material were reliable. The raw data of this article have been uploaded onto the Research Data Deposit (RDD) with an RDD number of RDDA2018000865.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by the ethical committee of Sun Yat-Sen University Cancer Center.
Abbreviations
- PRNN
postradiation nasopharyngeal necrosis
- NPC
nasopharyngeal carcinoma
- OS
overall survival
- OR
odds ratio
- CI
confidence interval
- HR
hazard ratio
- ICA
internal carotid artery
- BOT
balloon occlusion test
- MRI
magnetic resonance imaging
- NRS
numeric rating scales
- PET/CT
positron emission tomography–computed tomography
- ET
eustachian tube
- NSFF
posterior pedicle nasal septum, and floor mucoperiosteum flap
Contributor Information
Xiong Zou, Email: zouxiong@sysucc.org.cn.
Shun-Lan Wang, Email: 8520226@qq.com.
You-Ping Liu, Email: liuyoup@sysucc.org.cn.
Yan-Ling Liu, Email: liuyl@sysucc.org.cn.
Ru-Hai Zou, Email: zourh@sysucc.org.cn.
Yi-Nuan Zhang, Email: zhangyin@sysucc.org.cn.
Rui You, Email: yourui@sysucc.org.cn.
Qi Yang, Email: yangqi@sysucc.org.cn.
Yu-Long Xie, Email: xieyl1@sysucc.org.cn.
Mei Lin, Email: linmei@sysucc.org.cn.
Pei-Yu Huang, Email: huangpy@sysucc.org.cn.
Rou Jiang, Email: jiangrou@sysucc.org.cn.
Meng-Xia Zhang, Email: 18898534045@163.com.
Chao-Nan Qian, Email: qianchn@sysucc.org.cn.
Hai-Qiang Mai, Email: maihq@sysucc.org.cn.
Ling Guo, Email: guoling@sysucc.org.cn.
Ming-Huang Hong, Email: hongmh@sysucc.org.cn.
Ming-Yuan Chen, Phone: +86-20-8734-3361, Email: chmingy@mail.sysu.edu.cn.
References
- 1.Chua ML, Wee JT, Hui EP, Chan AT. Nasopharyngeal carcinoma. Lancet. 2016;387(10022):1012–1024. doi: 10.1016/S0140-6736(15)00055-0. [DOI] [PubMed] [Google Scholar]
- 2.Yu MC, Yuan JM. Epidemiology of nasopharyngeal carcinoma. Semin Cancer Biol. 2002;12(6):421–429. doi: 10.1016/S1044579X02000858. [DOI] [PubMed] [Google Scholar]
- 3.Zhang LF, Li YH, Xie SH, Ling W, Chen SH, Liu Q, et al. Incidence trend of nasopharyngeal carcinoma from 1987 to 2011 in Sihui County, Guangdong Province, South China: an age-period-cohort analysis. Chin J Cancer. 2015;34(8):350–357. doi: 10.1186/s40880-015-0018-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang MX, Li J, Shen GP, Zou X, Xu JJ, Jiang R, et al. Intensity-modulated radiotherapy prolongs the survival of patients with nasopharyngeal carcinoma compared with conventional two-dimensional radiotherapy: a 10-year experience with a large cohort and long follow-up. Eur J Cancer. 2015;51(17):2587–2595. doi: 10.1016/j.ejca.2015.08.006. [DOI] [PubMed] [Google Scholar]
- 5.Zhang W, Dou H, Lam C, Liu J, Zhou J, Liu Y, et al. Concurrent chemoradiotherapy with or without adjuvant chemotherapy in intermediate and locoregionally advanced nasopharyngeal carcinoma. Tumour Biol. 2013;34(3):1729–1736. doi: 10.1007/s13277-013-0710-6. [DOI] [PubMed] [Google Scholar]
- 6.Tsai WL, Chien CY, Huang HY, Liao KC, Fang FM. Prognostic value of quality of life measured after treatment on subsequent survival in patients with nasopharyngeal carcinoma. Qual Life Res. 2013;22(4):715–723. doi: 10.1007/s11136-012-0213-8. [DOI] [PubMed] [Google Scholar]
- 7.Mao YP, Tang LL, Chen L, Sun Y, Qi ZY, Zhou GQ, et al. Prognostic factors and failure patterns in non-metastatic nasopharyngeal carcinoma after intensity-modulated radiotherapy. Chin J Cancer. 2016;35(1):103. doi: 10.1186/s40880-016-0167-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang KP, Tsang NM, Chen CY, Su JL, Hao SP. Endoscopic management of skull base osteoradionecrosis. Laryngoscope. 2000;110(7):1162–1165. doi: 10.1097/00005537-200007000-00018. [DOI] [PubMed] [Google Scholar]
- 9.Huang XM, Zheng YQ, Zhang XM, Mai HQ, Zeng L, Liu X, et al. Diagnosis and management of skull base osteoradionecrosis after radiotherapy for nasopharyngeal carcinoma. Laryngoscope. 2006;116(9):1626–1631. doi: 10.1097/01.mlg.0000230435.71328.b9. [DOI] [PubMed] [Google Scholar]
- 10.Yu YH, Xia WX, Shi JL, Ma WJ, Li Y, Ye YF, et al. A model to predict the risk of lethal nasopharyngeal necrosis after re-irradiation with intensity-modulated radiotherapy in nasopharyngeal carcinoma patients. Chin J Cancer. 2016;35(1):59. doi: 10.1186/s40880-016-0124-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hua YJ, Chen MY, Qian CN, Hong MH, Zhao C, Guo L, et al. Postradiation nasopharyngeal necrosis in the patients with nasopharyngeal carcinoma. Head Neck. 2009;31(6):807–812. doi: 10.1002/hed.21036. [DOI] [PubMed] [Google Scholar]
- 12.Chen MY, Mai HQ, Sun R, Guo X, Zhao C, Hong MH, et al. Clinical findings and imaging features of 67 nasopharyngeal carcinoma patients with postradiation nasopharyngeal necrosis. Chin J Cancer. 2013;32(10):533–538. doi: 10.5732/cjc.012.10252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen MY, Wang SL, Zhu YL, Shen GP, Qiu F, Luo DH, et al. Use of a posterior pedicle nasal septum and floor mucoperiosteum flap to resurface the nasopharynx after endoscopic nasopharyngectomy for recurrent nasopharyngeal carcinoma. Head Neck. 2012;34(10):1383–1388. doi: 10.1002/hed.21928. [DOI] [PubMed] [Google Scholar]
- 14.Linskey ME, Jungreis CA, Yonas H, Hirsch WL, Jr, Sekhar LN, Horton JA, et al. Stroke risk after abrupt internal carotid artery sacrifice: accuracy of preoperative assessment with balloon test occlusion and stable xenon-enhanced CT. AJNR Am J Neuroradiol. 1994;15(5):829–843. [PMC free article] [PubMed] [Google Scholar]
- 15.Asai K, Imamura H, Mineharu Y, Tani S, Adachi H, Narumi O, et al. X-ray angiography perfusion analysis for the balloon occlusion test of the internal carotid artery. J Stroke Cerebrovasc Dis. 2015;24(7):1506–1512. doi: 10.1016/j.jstrokecerebrovasdis.2015.03.012. [DOI] [PubMed] [Google Scholar]
- 16.Hua YJ, Chen MY, Hong MH, Zhao C, Guo L, Han F, et al. Short-term efficacy of endoscopy-guided debridement on radiation-related nasopharyngeal necrosis in 20 nasopharyngeal carcinoma patients after radiotherapy. Aizheng. 2008;27(7):729–733. [PubMed] [Google Scholar]
- 17.Chen MY, Wen WP, Guo X, Yang AK, Qian CN, Hua YJ, et al. Endoscopic nasopharyngectomy for locally recurrent nasopharyngeal carcinoma. Laryngoscope. 2009;119(3):516–522. doi: 10.1002/lary.20133. [DOI] [PubMed] [Google Scholar]
- 18.Chen MY, Guo X, Wen WP, Hua YJ, Guo L, Li NW, et al. Salvage surgical operation via endoscopic transnasal approach for local persistent or recurrent nasopharyngeal carcinoma. Aizheng. 2007;26(7):673–678. [PubMed] [Google Scholar]
- 19.You R, Zou X, Hua YJ, Han F, Li L, Zhao C, et al. Salvage endoscopic nasopharyngectomy is superior to intensity-modulated radiation therapy for local recurrence of selected T1-T3 nasopharyngeal carcinoma—a case-matched comparison. Radiother Oncol. 2015;115(3):399–406. doi: 10.1016/j.radonc.2015.04.024. [DOI] [PubMed] [Google Scholar]
- 20.You R, Zou X, Wang SL, Jiang R, Tang LQ, Zhang WD, et al. New surgical staging system for patients with recurrent nasopharyngeal carcinoma based on the AJCC/UICC rTNM classification system. Eur J Cancer. 2015;51(13):1771–1779. doi: 10.1016/j.ejca.2015.05.014. [DOI] [PubMed] [Google Scholar]
- 21.Zou X, Han F, Ma WJ, Deng MQ, Jiang R, Guo L, et al. Salvage endoscopic nasopharyngectomy and intensity-modulated radiotherapy versus conventional radiotherapy in treating locally recurrent nasopharyngeal carcinoma. Head Neck. 2015;37(8):1108–1115. doi: 10.1002/hed.23719. [DOI] [PubMed] [Google Scholar]
- 22.Cornes PG, Cox HJ, Rhys-Evans PR, Breach NM, Henk JM. Salvage treatment for inoperable neck nodes in head and neck cancer using combined iridium-192 brachytherapy and surgical reconstruction. Br J Surg. 1996;83(11):1620–1622. doi: 10.1002/bjs.1800831141. [DOI] [PubMed] [Google Scholar]
- 23.Hao SP, Chen HC, Wei FC, Chen CY, Yeh AR, Su JL. Systematic management of osteoradionecrosis in the head and neck. Laryngoscope. 1999;109(8):1324–1327. doi: 10.1097/00005537-199908000-00027. [DOI] [PubMed] [Google Scholar]
- 24.Gordin EA, Ducic Y. Microvascular free tissue reconstruction in the patient with multiple courses of radiation. Laryngoscope. 2014;124(10):2252–2256. doi: 10.1002/lary.24681. [DOI] [PubMed] [Google Scholar]
- 25.Onoda S, Kimata Y, Sugiyama N, Onoda T, Mizukawa N. Effects of radiation therapy on postoperative complications and adverse events in patients with head and neck reconstruction with flaps. Microsurgery. 2014;34(7):516–521. doi: 10.1002/micr.22275. [DOI] [PubMed] [Google Scholar]
- 26.Song M, Chen WK, Zhang Q, Chen SW, Zhuang SM, Yang AK. Irradiation of the recipient site does not adversely affect successful free flap transfer in the repair of head and neck defects after salvage surgery for recurrent nasopharyngeal carcinoma originally treated with radiotherapy. J Plastic Surg Hand Surg. 2013;47(1):40–45. doi: 10.3109/2000656X.2012.729510. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All patients in the study were treated in Sun Yat-Sen University Cancer Center, the data and material were reliable. The raw data of this article have been uploaded onto the Research Data Deposit (RDD) with an RDD number of RDDA2018000865.