Abstract
Methods
Two reviewers systematically searched multiple databases for articles published between January 2009 and June 2018. Both screened and selected studies based on the set inclusion criteria. Following quality assessments, data on study characteristics, process of data collection and analysis and findings reported were extracted. Extracted data were synthesised and presented in tables and charts. Narrative synthesis was used to summarise reported findings.
Results
15 studies met the inclusion criteria, with varying assessed quality: high (7 studies), medium (4 studies) and low (4 studies). 8 studies were conducted at a national level while 7 were sub-national. 8 studies focused on assessing Indicator 2, while the others assessed multiple EmOC indicators. Only about half of the studies presented details of analysis for assessing geographical distribution, provided a map and interpreted their findings. Similarly, half of the studies used geographic information systems (GIS) for analyses. Of these, GIS was used to map EmOC facilities or relate facility numbers to 500 000 population (3), estimate straight-line distances between facilities and residences of women (2) and model travel scenarios (3). EmOC facilities in SSA are concentrated in capitals, central and urban areas and at least a third of women in the region cannot reach their nearest EmOC facility within the recommended two-hour time-frame.
Conclusions
There is a limited number of studies that have assessed EmOC geographical distribution in SSA. When available, completeness and quality of analysis are questionable. Comprehensive assessments need to maximise recent advancements in mobile and GIS open-source technology to provide more realistic representation of EmOC access for service planners and policy-makers.
PROSPERO Registration
CRD42018099882
Despite global efforts aimed at maternal mortality reduction, 303 000 women still lose their lives due to complications of pregnancy and childbirth annually. Ninety-nine percent of these deaths occur in low- and middle-income countries (LMICs), with the sub-Saharan African region accounting for almost two-thirds of the recorded maternal deaths [1]. Similar to other regions, direct obstetric complications which usually present as emergencies such as haemorrhage, hypertension, sepsis, complications of obstructed labour, and unsafe abortion lead to more than three-quarters of these deaths in sub-Saharan Africa (SSA) [2]. It has long been established that three delays are associated with maternal deaths: delay in decision to seek care, delay in travel to an appropriate health facility, and delay in receiving appropriate care upon arrival at the facility [3]. When and if women arrive at health facilities, evidence suggests that provision of timely and quality emergency obstetric care (EmOC) significantly reduces maternal morbidity and mortality, that could otherwise occur [4]. EmOC can either be basic (comprising of seven care packages – injectable antibiotics, injectable oxytocics, injectable anticonvulsants, manual removal of placenta, removal of retained products, assisted vaginal delivery and basic neonatal resuscitation), or comprehensive – all basic EmOC packages plus blood transfusion and caesarean section) (Table 1) [5].
Table 1.
Emergency obstetric care (EmOC) signal functions*
| Signal functions | |
|---|---|
|
Basic emergency obstetric care (BEmOC) |
Comprehensive emergency obstetric care (CEmOC) |
| 1) Antibiotics (injectable) |
All Basic EmOC functions (1-7) plus |
| 2) Oxytocics (injectable) |
8) Caesarean |
| 3) Anticonvulsants (injectable) |
9) Blood transfusion |
| 4) Manual removal of placenta |
|
| 5) Removal of retained products |
|
| 6) Assisted vaginal delivery |
|
| 7) Basic neonatal resuscitation | |
*A BEmOC facility is one in which all functions 1-7 are performed. A CEmOC facility is one in which all functions 1-9 are performed.
In 2009, the World Health Organization (WHO) updated the guidelines for assessing the availability and quality of EmOC, recommending eight indicators, one of which included ‘geographical distribution of EmOC facilities’ (EmOC Indicator 2) [5]. The WHO recommended that as an acceptable minimum level for geographic distribution, “all subnational areas have at least five emergency obstetric care facilities (including at least one comprehensive facility) for every 500,000 population” [5]. In the guideline, the WHO also recommended that to assess the indicator, researchers should “calculate the distribution of EmOC facilities for subareas” and report the percentage of the subareas meeting the acceptable minimum levels. In addition, researchers could map the facilities in sub-areas and show roads as well as the general topography, using geographical information system (GIS) or similar mapping methods. This may be more useful for health system planners to “identify problems of access and show referral systems” [5]. While such additional analysis was recommended, no specific indicator was proposed to assess it [5].
For varied reasons in SSA urban and rural areas, geographical distribution and accessibility of EmOC facilities is particularly critical. In many urban areas in the region, there are high population densities mostly due to urbanization [6]. Additionally, roads, which make up the dominant mode of motorized transport in SSA, are mostly in poor conditions and therefore prone to severe traffic congestions [7]. In the rural areas, roads are in even poorer conditions, compounded by difficult terrain [8]. These factors limit access to EmOC facilities if women decide to seek care and may jeopardise pregnancy outcomes [9,10]. With the persistent high maternal mortality burden in SSA, it is critical to understand how geographical availability and access to EmOC facilities have been measured. Our objective in this systematic review was to explore studies published in the peer-review literature that assessed EmOC geographical distribution and accessibility in SSA.
METHODS
Search strategy
Using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) approach [11], PubMed, Scopus, Embase, CINAHL, Global Health and Directory of Open Access Journal (DOAJ) were searched for articles published between year 2009 (the publication year of the updated WHO handbook [5]) and June 2018 (The PRISMA Checklist is provided in Appendix S1 in Online Supplementary Document). The search terms used combined the care package (“Emergency Obstetric Care” OR “Emergency Obstetric and Newborn Care” OR EmOC OR EmONC) AND a word indicating assessment of the care package (Assess* OR evaluat* OR monitor* OR function* OR perform* OR effect*). Duplicates were identified and removed. Subsequently, a reference-list checking of the retrieved articles was conducted to identify any additional relevant articles that had been missed. The search was conducted by two authors (ABT and LC). Following title and abstract screening to confirm relevance of articles, ABT and LC independently read the articles to identify those that specifically assessed EmOC geographical distribution and accessibility in sub-Saharan African countries, as defined by the World Bank [12]. Both authors compared their retrieved records and agreed on final eligibility based on the agreed inclusion/exclusion criteria. Any disagreements were resolved through discussions with another author (KW).
Inclusion and exclusion criteria
Articles were included if they reported observational studies that assessed EmOC geographical distribution and accessibility and were published in the peer-reviewed literature from January 2009 to June 2018. Articles had to be published in English language and conducted in a sub-Saharan African country to be included. Commentaries, editorial letters, conference proceedings, other reviews and studies that solely focused on testing associations between travel/access to specific facility or facilities and dependent variables, were excluded.
Data extraction and synthesis
Articles that met the inclusion criteria were allocated unique identifiers for auditing. Article full-texts were subsequently reviewed, and data extracted using a pre-developed extraction sheet. Data collected included the author(s), publication year, study country, stated study objectives, scale of study (national, sub-national or facility level), indicators assessed, number of facilities included, percentage of all facilities surveyed, level of care (Basic Emergency Obstetric Care (BEmOC) or Comprehensive Emergency Obstetric Care (CEmOC)), type of facilities included (public or private), assessment model used (United Nations (UN) EmOC assessment model or others), data sources, methods used for collecting data to assess EmOC geographical distribution and accessibility, analytical approach utilised (None-GIS or GIS approach. If GIS was used, for what purpose?), key findings reported, and interpretation of geographical findings. Data synthesis involved consolidation of data extracted from the retrieved articles. A mix of summary tables and charts was used to present the aggregated data to show trends and patterns for distribution and characteristics of the included studies. As study findings were varied, narrative synthesis was used to analyse and interpret the findings [13,14].
Quality assessment
Building on a previous quality assessment framework proposed for EmOC indicators more broadly [15] and further guidance from the UN EmOC monitoring handbook [5], we developed a bespoke quality assessment framework for studies assessing EmOC geographical distribution and accessibility (Appendix S2 in Online Supplementary Document). A bespoke framework was required, as compared with the other 7 EmOC indicators, EmOC indicator 2, which focuses on EmOC geographical distribution and accessibility, requires unique methods for data collection and analysis [5]. This framework assessed the use of recent population figures, type of facilities included (public vs private), direct inspection for data collection, geo-referencing of EmOC facilities, information provided on methods used for assessment, mapping of EmOC facilities in relation to catchment population and identification of underserved areas. For scoring, 1 point was awarded for each achieved criterion and 0 point when not achieved or not particularly clear. Studies were assessed as high quality, if they achieved 75% or more of the criteria, medium quality for 50-74% or low quality for less than 50%.
RESULTS
Summary of results
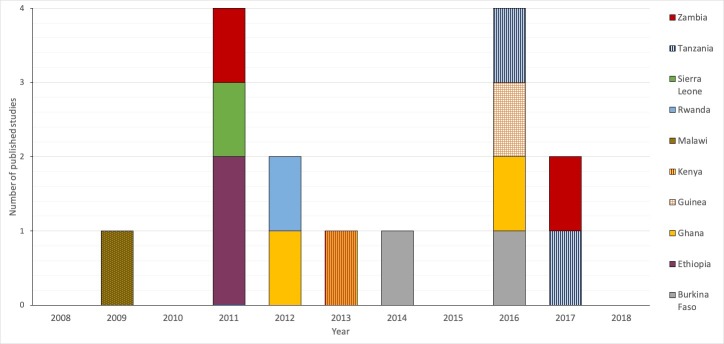
As shown in the PRISMA flow diagram, following removal of duplicates, we had 177 records from all databases combined. After abstract and full-text reading to specifically find articles that assessed EmOC geographical distribution and accessibility, 15 studies were found to meet the set inclusion criteria and were included for review (Figure 1).
Figure 1.
Flow diagram of the literature search process.
Quality assessment of studies
Of the 15 studies, seven were assessed to be of high quality [8,9,16-20], 4 were medium quality [21-24] and the remaining 4 studies were assessed as being of low quality [25-28] (See Quality assessment of studies in Appendix S2 in Online Supplementary Document).
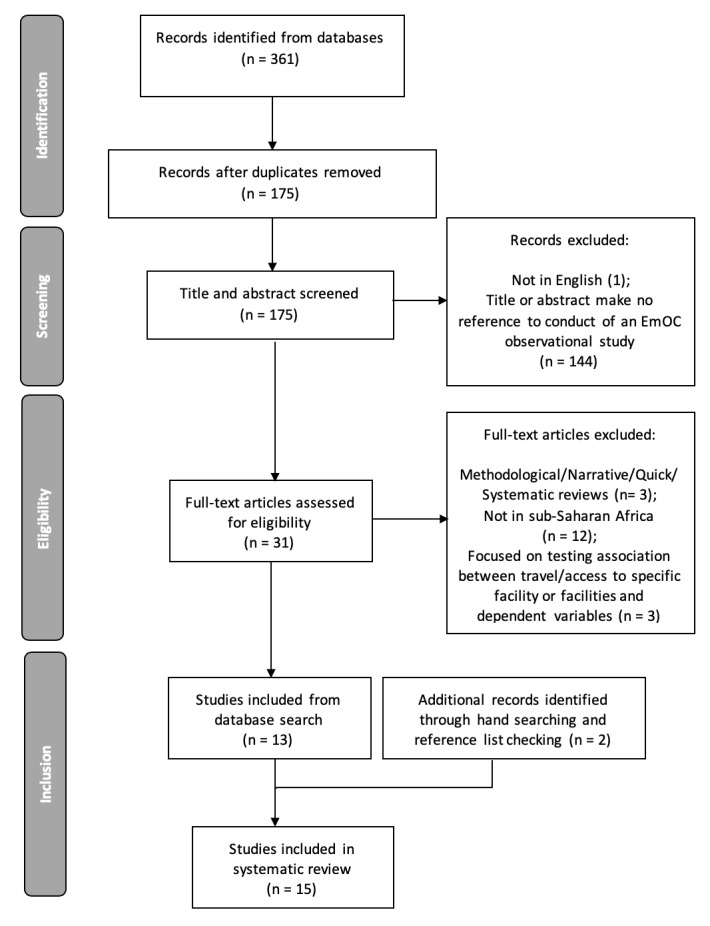
Distribution of included studies
Since 2009, there has been an average of about 1 study per year that assessed EmOC geographical distribution and accessibility in SSA published in the peer-reviewed literature (Figure 2). The peak publication year was in 2011 [8,22,24,25] and 2016 [16,17,21,27] when 4 articles were published in each year (Figure 2). 2 studies have each been published in Burkina-Faso [26,27], Ethiopia [8,25], Ghana [17,19], Tanzania [20,21] and Zambia [22,28]. Guinea [16], Kenya [18], Malawi [23], Sierra-Leone [24], Rwanda [9] each have 1 published study (Figure 2).
Figure 2.
Distribution of emergency obstetric care (EmOC) geographical distribution published peer-reviewed studies in sub-Saharan Africa.
Characteristics of included studies
8 of the 15 studies were conducted on a national scale [16,17,19,22,24-27], while the remaining 7 studies assessed sub-national levels – regions or districts [8,9,18,20,21,23,28] (Table 2).
Table 2.
Summary of study characteristics
| Study characteristics | No. of studies (n = 15) | % of total |
|---|---|---|
| Scale of study: | ||
| National | 8 | 53.3% |
| Sub-national |
7 |
46.7% |
| Indicators assessed: | ||
| Indicator 1 & 2 | 8 | 53.3% |
| Indicator 1 & 2 plus another | 1 | 6.7% |
| Five or more indicators |
6 |
40.0% |
| Assessment model | ||
| United Nations Emergency Obstetric Care assessment tool | 12 | 80.0% |
| United Nations Emergency Obstetric Care assessment tool + Geographic Information Systems |
3 |
20.0% |
| Level of care assessed: | ||
| Basic and Comprehensive Emergency Obstetric Care | 14 | 93.3% |
| Comprehensive Emergency Obstetric Care only |
1 |
6.7% |
| Type of facilities assessed: | ||
| Public facilities only | 1 | 6.7% |
| Public and private facilities only | 3 | 20.0% |
| Public, private and mission facilities | 9 | 60.0% |
| Could not tell type of facility classification |
2 |
13.3% |
| Data sources used indicator assessment: | ||
| Secondary population and primary facility data | 4 | 26.7% |
| Primary facility and geographical data | 1 | 6.7% |
| Secondary population, facility and geographical data | 4 | 26.7% |
| Secondary population, primary facility and primary geographical data |
6 |
40.0% |
| Geographical analysis and visualisation presented: | ||
| Yes | 9 | 60.0% |
| No |
6 |
40.0% |
| Use of Geographic Information Systems (GIS, n = 9): | ||
| Thematic mapping | 3 | 33.3% |
| Thematic mapping and spatial analysis | 3 | 33.3% |
| Thematic mapping and spatial modelling |
3 |
33.3% |
| Interpretation and implication of findings presented: | ||
| Yes | 8 | 53.3% |
| No | 7 | 46.7% |
8 articles focused on the UN EmOC indicator 1 and 2 (availability and geographical distribution) [8,9,17,19,20,22,26,28]. 1 study looked at both indicator 1 and 2 as well as indicator 5 [18], while the remaining 6 studies assessed 5 or more of the 8 EmOC indicators [16,21,23-25,27]. 12 studies used only the UN EmOC assessment guidelines as the basis for their analysis [8,16-18,21-28], while 3 studies used additional GIS frameworks not stipulated in the UN EmOC assessment handbook [8,19,20] (Table 2).
14 studies assessed both basic and comprehensive EmOC facilities [8,9,16-25,27,28], with 1 study focusing on only CEmOC facilities [26]. 9 studies assessed all types of facilities within the country or district (public, private and mission owned) [8,18,19,21-25,27]. 3 studies assessed public and private facilities [16,17,28] and 1 study assessed only public facilities [26]. EmOC classification of facilities could not be determined for 2 studies [9,20] (Table 2). 5 studies selected all possible facilities within their set geographical assessment area [9,16,18,19,23], while 3 studies selected all hospitals and randomly selected lower facilities like health centres [21,22,24]. Of the remaining studies, 4 sampled a proportion of the available facilities, ranging from 31% to 98.6% [8,17,25,27]. Proportion of hospitals sampled was not stated or could not be determined for 2 studies [20,28] (See data extraction sheet in Appendix S3 in Online supplementary document).
6 of the 15 studies used a combination of secondary population, primary facility and primary geographical data [8,9,22-25]. 4 used only secondary population and primary facility data [16,21,27,28] and another four studies used secondary population, facility and geographical data [17,19,20,22]. 1 study used primary facility and geographical data [26] (Table 2).
9 studies presented some information on their analytical framework for assessing EmOC geographical distribution and provided some visualisation in the form of a map [8,9,16-20,22,24]. The other 6 studies did not provide any detail and/or did not include a map [21,23,25-28] (Table 2).
In 6 studies, the authors simply counted number of facilities per district and estimated the locations of facilities on a map [21,23,25-28]. In 9 studies, the authors used a GIS software to aid analysis [8,9,16-20,22,24] (Table 2). For studies that used GIS, it was used for thematic mapping as either solely mapping locations of fully functioning facilities within districts in 1 study or to map fully functioning facilities and relate the output to the 500 000 population benchmark set by the UN [16,17,24]. In addition to mapping facilities, 3 studies used GIS for some form of spatial analysis, either to estimate straight-line distances between the facilities and place of residence of women while building concentric travel buffers (circles with a common centre) around the facilities [18,22] or relate spatial location of facilities to rate of EmOC service utilisation [9]. 3 studies used GIS for spatial modelling of various travel scenarios for women in need of EmOC within specified geographical areas [8,19,20] (Table 2). 8 of the 15 studies interpreted their findings within the discussion section and provided implication of their findings [8,9,18-20,22-24], while the remaining 7 studies did not provide any detailed interpretation of findings [16,17,21,25-28] (Table 2).
Findings reported
Most studies reported inequitable distribution of CEmOC and BEmOC facilities. The sub-national studies mainly reported that there was concentration of CEmOC facilities in urban areas [21-23] (Table 3). The national survey conducted in Zambia pointed that more than 75% of those who reside in rural areas lived more than 15 km of an EmOC facility [22] (Table 3). In the Ghana national survey, across board, 34% and 50% of women lived more than 2 hours away from the nearest partial or fully functional EmOC and specifically CEmOC facilities respectively [19]. Similarly, 32% of live-births occurred in places where it was impossible for women to reach with motorised means of transport within 2 hours [20]. In the most rural areas, the figures rose to 63% and 81% [19] (Table 3). Within rural areas of Rwanda, CEmOC rates were the lowest in the more remote parts and incidence or morbidities and mortalities associated with pregnancy complications was higher than in less remote rural parts [9] (Table 3). Other surveys highlighted that there were more fully functioning EmOC facilities in central areas of the country or district [18,25] or in the capital [16,21,24] (Table 3). In some countries, even when there is “good geographical distribution of hospitals”, very few are fully functional [26] (Table 3).
Table 3.
Summary table of key geographical findings
| Author(s) | Year | Country of study | Indicators assessed | Scale of study | Number of facilities studied | Percentage of total facilities surveyed | Type of facility studied | Key geographical findings presented |
|---|---|---|---|---|---|---|---|---|
| Kongnyuy et al [23] |
2009 |
Malawi |
Indicator 1-6 |
Sub-national |
73 |
100% of all facilities within the selected geographical area. |
Public, private and mission facilities |
There was no equitable distribution as some rural areas are not covered. Most of the Comprehensive EmOC* facilities were located in the central area of Lilongwe District and three were actually in or near the capital city. |
| Admasu, Haile-Mariam & Bailey [25] |
2011 |
Ethiopia |
All indicators |
National |
795 |
98.6% of all facilities within the selected geographical area. |
Public, private and mission facilities |
In Ethiopia, facilities were concentrated in the centre of the country, leaving peripheral areas underserved. Only 1 (Harari) of 11 regions met the goal of 5 per 500 000. The most populous regions of Oromiya, Amhara, and Southern Nations, Nationalities, and Peoples’ Region had only 0.4, 0.4, and 0.5 EmOC facilities per 500 000, respectively. |
| Bailey et al [8] |
2011 |
Ethiopia |
Indicator 1 & 2 |
Sub-national |
249 |
31% of all facilities within the selected geographical area. |
Public, private and mission facilities |
Approximately 70% of the population of Tigray and Amhara regions is served by facilities that are within a 2-h transfer time to a hospital with obstetric surgery. By adding vehicles and communication capability, this percentage increased to 83%. In a second scenario, upgrading 7 strategically located facilities changed the configuration of the referral networks, and the percentage increased to 80%. By combining the two strategies, 90% of the population would be served by midlevel facilities within 2 h of obstetric surgery. The mean travel time from midlevel facilities to surgical facilities would be reduced from 121 to 64 min in the scenario combining the 2 interventions. |
| Gabrysch et al [22] |
2011 |
Zambia |
Indicator 1 & 2 |
National |
1370 |
100% public hospitals. Percentage of private hospitals surveyed not reported. |
Public, private and mission facilities |
Geographic access to EmOC services in rural areas was low; in most provinces, less than 25% of the population lived within 15 km of an EmOC facility |
| Oyerinde et al [24] |
2011 |
Sierra Leone |
Indicator 1-6 |
National |
145 |
100% of all hospitals. 33% of community health clinics and four MCH posts per district. |
Public, private and mission facilities |
Eastern Province and Southern Province had the lowest coverage. There was an abundance of Comprehensive EmOC facilities in Western Area District (where the capital city, Freetown, is located). |
| Gething et al [19] |
2012 |
Ghana |
Indicator 1 & 2 |
National |
1864 |
100% of all facilities within the selected geographical area. |
Public, private and mission facilities |
A third of women (34%) in Ghana live beyond the clinically significant two-hour threshold from facilities likely to offer emergency obstetric and neonatal care (EmONC) classed at the ‘partial’ standard or better. Nearly half (45%) live that distance or further from ‘comprehensive’ EmONC facilities. In the most remote regions these figures rose to 63% and 81%, respectively. |
| Sudhof et l. [9] |
2012 |
Rwanda |
Indicator 1 & 2 |
Sub-national |
9 |
100% of all facilities within the selected geographical area. |
Could not tell |
The lowest Caesarean section rates were found in the more remote part of the hospital catchment area. |
| Echoka et al [18] |
2013 |
Kenya |
Indicator 1, 2 & 5 |
Sub-national |
40 |
100% of all facilities within the selected geographical area. |
Public, private and mission facilities |
All the three hospitals offering Comprehensive EmOC services and one of the two health centres offering BEmOC services were located in Malindi Division, the main urban centre in the district. The area is served by a relatively well functioning public transport system and adequate roads. The two vast and remote divisions, Langobaya and Marafa, were not served by any EmOC facility and are not connected to any major trunk road with regular public transport. Average distance to the nearest EmOC facility was 5kms and 30kms in the urban and rural areas respectively. |
| Compaoré et al [26] |
2014 |
Burkina Faso |
Indicator 1 & 2 |
National |
52 |
100% of public hospitals. No private hospitals included. |
Public hospitals only |
Map of georeferenced facilities shows a relatively good geographical distribution of both regional and district hospitals within the country, very few of which are ready to provide Comprehensive EmOC. |
| Bosomprah et al [17] |
2016 |
Ghana |
Indicator 1 & 2 |
National |
1159 |
91% of all facilities within the selected geographical area. |
Public and private facilities |
Greater Accra and Ashanti recorded a shortfall of 28 and 26 facilities, respectively, whereas Upper East and Upper West had a shortfall of only 7 and 3, respectively. Subnational analyses based on estimated total pregnancies in each district revealed a pattern of inequity in service provision across the country. |
| Baguiya et al [16] |
2016 |
Guinea |
All indicators |
National |
502 |
100% of all facilities within the selected geographical area. |
Public and private facilities |
There was a scarce and unequal distribution of such facilities. Fully functioning facilities were not equally distributed across regions. Boké and Conakry had four each, whereas Kindia and Mamou had none. |
| Kouanda et al [27] |
2016 |
Burkina Faso |
All indicators |
National |
1628 (2010) and 812 (2014) |
82% (2010) of facilities at national level. Not estimated in the 2014 survey. |
Public, private and mission facilities |
There was wide regional disparity in both 2010 and 2014 on the availability of functional EmONC health facilities. |
| Fakih et al [21] |
2016 |
Tanzania |
Indicator 1-7 |
Sub-national |
79 |
100% of all hospitals. 38% of Primary Health Care Units (PHCUs) across all districts. |
Public and private facilities |
The distribution of Basic EmOC and Comprehensive EmOC facilities varied across Zanzibar. Basic EmOC facilities were available in North Pemba and South Pemba regions, as well as West Urban regions. Comprehensive EmOC facilities were mainly concentrated in Urban West (Unguja); North Pemba and South Pemba regions. |
| Tembo et al [28] |
2017 |
Zambia |
Indicator 1 & 2 |
Sub-national |
35 |
Could not tell |
Public and private facilities |
18 Basic EmOC per 500 000 population; 5 Comprehensive EmOC per 500 000 population. |
| Chen et al [20] | 2017 | Tanzania | Indicator 1 & 2 | Sub-national | 127 | Could not tell | Could not tell | Of all live births in Kigoma Region, 13% occurred in areas where women can reach EmOC facilities within 2 h on foot, 33% in areas that can be reached within 2 h only by motorized vehicles, and 32% where it is impossible to reach EmOC facilities within 2 h. Over 50% of births in 3 of the 8 administrative councils had poor estimated access. In half the councils, births with poor access could be reduced to no higher than 12% if all female residents had access to motorized vehicles. |
EmOC – emergency obstetric care
DISCUSSION
Our findings showed that there are only a few studies assessing EmOC geographical distribution and accessibility in SSA published in the peer-review literature (15) [8,9,16-28]. Of the 46 sub-Saharan African countries [12], only 10 had peer-reviewed assessments. This is despite the huge burden of maternal deaths that can be addressed with improved EmOC access in the sub-region [2]. However, the finding of limited quantity of peer-reviewed studies is not surprising. A 2016 systematic review of peer-review literature showed that EmOC indicator 2 was 1 of the least studied EmOC indicator in LMICs [15].
In terms of quality of studies, evidence from our review suggests that studies that focused on indicator 1 and 2 only were of the highest quality [8,9,17-20]. These studies included more detail and better interpreted their findings. 4 of 6 studies judged to be of the highest quality were sub-national [8,9,18,20], and the other 2 were national studies [17,19]. A national and a sub-national study conducted by the same group of authors were assessed as low and high quality respectively [8,25]. Similarly, national studies conducted in Burkina-Faso and Guinea involving authors from the same institution were assessed as low and high quality respectively [16,27]. As such, it is difficult to conclude that study scope (national vs sub-national) influences quality of the study. The most prevalent reason for low-quality ratings in studies were authors not providing any detail of how they geo-referenced EmOC facilities and identified the catchment population for each assessed facility [9,21,23-28] and not mapping facilities in relation to population of the assessed district [23,25-28]. These criteria are recommendations in the UN assessment guidelines [5]. In our review, only about half of the studies presented details of analysis for assessing EmOC geographical distribution, provided a map [8,9,16-18,20,22,24] and interpreted their findings [8,9,18,20,22-24]. For the remaining studies [21,23-28], assessment of indicator 2 was essentially presented as an “add-on”, without going into any significant detail on assessment process or interpretation of findings. It was particularly surprising that no map was included in these studies, bearing in mind the strength of visualisation in strengthening an abstract indicator such as indicator 2 and the power of such tool for advocacy and planning [8].
A study included only public facilities [26], and in this study, this was the stated objective. No reason was given for the non-inclusion of private facilities. However, for some studies that included public and private facilities [16,17,28], it was not clear if inclusion of private facilities solely referred to “privately-owned” by an individual or if “mission-owned” facilities were also classified as private facilities. The WHO assessment guideline clearly identifies five categories of operating agencies – Government, private, nongovernmental organization, religious mission, and others [5]. In cases in which these operating agencies have not been included in the study, it is important that such non-inclusion is clearly stated within studies, as there might be implications for interpretation and comparison with similar studies. A statement showing the percentage distribution of EmOC facility types (public/private/non-governmental/faith-based), as was done by Baguiya et al [16], will make such distinctions clearer.
Only half of the reviewed studies used GIS for analyses [8,16-20,22,24]. Not just for EmOC assessments, but generally within maternal and newborn health (MNH), mapping and application of GIS has been lagging behind, despite its more robust and sophisticated application in many other health-related fields where it has proven to be a valuable tool for generating evidence to aid strategic decision-making [29]. A 2015 review found only 19 GIS applications in MNH, published in Africa [30]. In our review, we found that GIS application was mainly limited to simply mapping EmOC facilities or relating EmOC facility numbers to the 500 000-benchmark population recommended by WHO. However, focus on this benchmark only reflects EmOC service ‘provision’ at sub-national levels. While ‘provision’ is important, there is a critical need to demonstrate ‘access’ to and ‘utilisation’ of those facilities by women, which is only possible if more is done with GIS [8,30]. A more useful finding for EmOC service planners would be EmOC coverage, which can show for example that there are 2 comprehensive EmOC facilities available for a million population, and all women in the district can reach a facility within two hours, irrespective of their means of transport [20,22]. Only a third of the studies in our review provided such sophisticated yet critical level of analyses [8,18-20,22]. Clearly, there is scope for leveraging more of the potentials of GIS in producing for useful results for service planners.
For those who used GIS to assess travel to facilities, some estimated straight-line distances between facilities and residences of women [18,22]. While this may partly reflect access, estimating straight-line (Euclidean) distances do not demonstrate real-life travel experiences of women to EmOC facilities, since the route of travel may be convoluted, with poor conditions and different terrain barriers [18]. Therefore, interpretation of straight-line buffers can be complicated. Some women may fall within the buffer but may not be able to access facilities because geographical bodies such as mountains and rivers are located between their residence and the facilities. However, the accuracy derived from real-life travel estimates should always be juxtaposed with the associated cost and complexity of estimating Euclidean distances. In a study in Ghana, some authors showed that Euclidean distances can be reasonable proxies for the actual distance covered in LMICs [31]. More research is required in other LMICs to ascertain this finding. However, in the few studies that reported access and coverage, it appeared that generally about a third of women lived more than two hours away from functional EmOC facilities [19,20]. This is similar to conclusions made in a recent analysis of access to emergency hospital care provided by the public sector in SSA, in which the authors showed that 28.2% of women of reproductive age needed more than two hours to reach the nearest hospital [32]. When disaggregated, wider disparity to accessing EmOC was reported in rural areas in SSA, with rural women twice more likely to live more than two hours away from functioning EmOC facilities than urban women [19].
In our review, studies that used the UN EmOC assessment framework along with more elaborate GIS assessment framework appeared to provide more detailed analysis and interpretation of their findings [8,19,20]. There is a need to rethink the scope of the UN assessment framework for Indicator 2, so that more critical information, which had previously been labelled “supplementary” and “cumbersome to analyse” [5], can be generated. In other areas of health in which GIS has been applied without a specific framework for supporting assessments, authors have been able to detail more extensive analysis with useful information for service planners [33-36]. Additional data such as health worker density and hours of service should be considered for future assessments. This adds crucial information on functionality of facilities for service planners and indeed will highlight the fully functional EmOC facilities, which are expected to be open 24 hours a day, seven days a week [22]. Such complementary data can be collected using tools such as the Service Availability and Readiness Assessment (SARA) survey [37] and the Workload Indicators of Staffing Need (WISN) survey [38].
GIS clearly provides further insight for EmOC geographical distribution and accessibility. So, why is it not used in all studies? 1 study in our review stated this was because of the “non-availability of GIS software to analyse geographical data” [28]. It is not clear why this was the case for this study, more so in the post-2010 era of the GIS evolution, when GIS is described as being ubiquitous, even in SSA [39]. In a previous review, issues such as prohibitive cost of GIS assessments and need for advanced technical know-how have been attributed to its limited use in EmOC assessments [15]. However, recent mobile technological developments, availability of free population data and in some cases facility data bring new opportunities for scaling up GIS use for EmOC assessments in SSA [29].
Previously, data collection for EmOC indicator 2 assessment required use of handheld global positioning system (GPS) machines, which came at a cost to the researchers and required knowledge on how to import the geo-coordinates and post-process into specialized software after collection [15]. However, with the proliferation of smart mobile phones in many LMICs [40], free applications such as ‘Get Geo-Coordinates’ (Available in Android Play Store) and ‘Easy GPS’ (Available in Apple App Store) can be used to capture location data for assessments, without incurring significant costs aside from travel-related expenses. For researchers who are unable to travel to the EmOC facilities and/or residences of women, there are free websites, such as http://www.gps-coordinates.net/ and http://www.mygeoposition.com/ that can be assessed from office-based desktops, which provide x,y geo-coordinates for specific addresses/locations. No advanced technical know-how is required to use these applications or websites. However, ethical considerations regarding geo-referencing specific locations require researchers to randomly displace the coordinates to guarantee confidentiality. Similar random displacements are carried out in the conduct of the Demographic Health Surveys conducted in LMICs [41].
As with GIS for data collection, the basic analysis for geographic distribution of EmOC facilities can be easily done today. It involves simply geocoding the x,y coordinates that have been collected in data files known as shapefiles (which include a feature geometry file (.shp), positional index (.shx) and some attribute data (.dbf) [42]). Though availability of these shapefiles may be limited for some LMICs [43], there are growing databases online such as http://www.diva-gis.org/Data and http://www.gadm.org/, from which shapefiles at national and sub-national levels can be downloaded for free. The supplementary analyses suggested in extant literature can then be performed using these shapefiles with various attributes. Typically, these supplementary analyses need to be done within proprietary GIS software such as ArcGIS® (Environmental Systems Research Institute, Redlands CA, USA) or MapInfo® (Pitney Bowes, Stamford CT, USA). However, there are now free open-source alternatives such as GRASS GIS® (GRASS Development Team, Bonn, Germany), QGIS® (QGIS Development Team, Global) and AccessMod® (enviroSPACE Laboratory, Geneva, Sitzerland) that are increasingly becoming more user-friendly and designed to be used by non-specialists. If these tools appear complex, Google Maps® (Google, Mountain View CA, USA), a freely available tool used for everyday commuting, can be used to estimate travel time and distance. Google Maps® also has the capability to provide data on live and typical traffic behaviour.
To the best of our knowledge, this is the first systematic review that specifically explores assessment of EmOC geographical distribution and accessibility in SSA. In interpreting our findings, some limitations need to be kept in mind. First, our search is limited to peer-reviewed literature. There are published and unpublished assessments in the grey literature, which we have not included. In addition, we have only included studies published in English language.
CONCLUSION
Assessment of EmOC geographical distribution and accessibility is limited in SSA. With the advent of smarter mobile technology and explosion of innovative, user-friendly open-source GIS technologies, there is a unique opportunity for scaling-up quantity and quality of such assessments in the sub-region. Where skill gaps still exist, EmOC assessors and service planners should collaborate with GIS specialists. Furthermore, these assessments need to be able to provide answers to questions regarding service provision, access, coverage and identify priority areas for new or upscaled EmOC facilities [44]. These answers are critical components in the efforts to reduce maternal mortality in SSA.
Additional material
Acknowledgements
The authors would like to acknowledge the support of Dr Oluwasola Banke-Thomas in the writing-up of this manuscript.
Footnotes
Funding: None.
Authorship contributions: Concept and design of review: ABT and LC; Literature search, screening and data extraction: ABT, LC and KW; Quality assessment: ABT and KW; Data synthesis: ABT and KW; All authors were involved in writing the manuscript and approved the final version.
Competing interest: The authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare no conflict of interest.
REFERENCES
- 1.WHO, UNICEF, UNFPA, World Bank Group, The United Nations Population Division. Trends in Maternal Mortality: 1990 to 2015. Geneva: World Health Organization; 2015. Available: http://apps.who.int/iris/bitstream/handle/10665/194254/9789241565141_eng.pdf?sequence=1. Accessed: 28 November 2018.
- 2.Say L, Chou D, Gemmill A, Tunçalp Ö, Moller A-B, Daniels J, et al. Global causes of maternal death: A WHO systematic analysis. Lancet Glob Health. 2014;2:e323–33. doi: 10.1016/S2214-109X(14)70227-X. [DOI] [PubMed] [Google Scholar]
- 3.Thaddeus S, Maine D. Too far to walk: Maternal mortality in context. Soc Sci Med. 1994;38:1091–110. doi: 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- 4.Paxton A, Maine D, Freedman L. The evidence for emergency obstetric care. Int J Gynaecol Obstet. 2005;88:181–93. doi: 10.1016/j.ijgo.2004.11.026. [DOI] [PubMed] [Google Scholar]
- 5.WHO. UNFPA, UNICEF, AMDD. Monitoring emergency obstetric care: a handbook. Geneva, Switzerland: WHO Press; 2009. [Google Scholar]
- 6.Cohen B. Urbanization in developing countries: Current trends, future projections, and key challenges for sustainability. Technol Soc. 2006;28:63–80. doi: 10.1016/j.techsoc.2005.10.005. [DOI] [Google Scholar]
- 7.Kumar A, Barrett F. Stuck in traffic: urban transport in Africa. Washington D.C.; 2008. Available: http://documents.worldbank.org/curated/en/671081468008449140/pdf/0Urban1Trans1FINAL1with0cover.pdf. Accessed: 28 November 2018.
- 8.Bailey PE, Keyes EB, Parker C, Abdullah M, Kebede H, Freedman L. Using a GIS to model interventions to strengthen the emergency referral system for maternal and newborn health in Ethiopia. Int J Gynaecol Obstet. 2011;115:300–9. doi: 10.1016/j.ijgo.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 9.Sudhof L, Amoroso C, Barebwanuwe P, Munyaneza F, Karamaga A, Zambotti G, et al. Local use of geographic information systems to improve data utilisation and health services: mapping caesarean section coverage in rural Rwanda. Trop Med Int Health. 2013;18:18–26. doi: 10.1111/tmi.12016. [DOI] [PubMed] [Google Scholar]
- 10.Niyitegeka J, Nshimirimana G, Silverstein A, Odhiambo J, Lin Y, Nkurunziza T, et al. Longer travel time to district hospital worsens neonatal outcomes: a retrospective cross-sectional study of the effect of delays in receiving emergency cesarean section in Rwanda. BMC Pregnancy Childbirth. 2017;17:242. doi: 10.1186/s12884-017-1426-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Bank. Sub-Saharan Africa. Data. 2018. Available: https://data.worldbank.org/region/sub-saharan-africa. Accessed: 8 October 2018.
- 13.Thomas J, Harden A, Newman M. Synthesis: Combining results systematically and appropriately. In: Gough D, Oliver S, Thomas J, editors. An introduction to systematic reviews. London: SAGE Publications Inc.; 2012. p. 179–226. [Google Scholar]
- 14.Snilstveit B, Oliver S, Vojtkova M. Narrative approaches to systematic review and synthesis of evidence for international development policy and practice. J Dev Effect. 2012;4:409–29. doi: 10.1080/19439342.2012.710641. [DOI] [Google Scholar]
- 15.Banke-Thomas A, Wright K, Sonoiki O, Banke-Thomas O, Ajayi B, Ilozumba O, et al. Assessing emergency obstetric care provision in low- and middle-income countries: a systematic review of the application of global guidelines. Glob Health Action. 2016;9:31880. doi: 10.3402/gha.v9.31880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baguiya A, Meda IB, Millogo T, Kourouma M, Mouniri H, Kouanda S. Availability and utilization of obstetric and newborn care in Guinea: A national needs assessment. Int J Gynaecol Obstet. 2016;135:S2–6. doi: 10.1016/j.ijgo.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 17.Bosomprah S, Tatem AJ, Dotse-Gborgbortsi W, Aboagye P, Matthews Z. Spatial distribution of emergency obstetric and newborn care services in Ghana: Using the evidence to plan interventions. Int J Gynaecol Obstet. 2016;132:130–4. doi: 10.1016/j.ijgo.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 18.Echoka E, Kombe Y, Dubourg D, Makokha A, Evjen-Olsen B, Mwangi M, et al. Existence and functionality of emergency obstetric care services at district level in Kenya: theoretical coverage versus reality. BMC Health Serv Res. 2013;13:113. doi: 10.1186/1472-6963-13-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gething PW, Johnson FA, Frempong-Ainguah F, Nyarko P, Baschieri A, Aboagye P, et al. Geographical access to care at birth in Ghana: a barrier to safe motherhood. BMC Public Health. 2012;12:991. doi: 10.1186/1471-2458-12-991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen YN, Schmitz MM, Serbanescu F, Dynes MM, Maro G, Kramer MR. Geographic Access Modeling of Emergency Obstetric and Neonatal Care in Kigoma Region, Tanzania: Transportation Schemes and Programmatic Implications. Glob Health Sci Pract. 2017;5:430–45. doi: 10.9745/GHSP-D-17-00110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fakih B, Nofly AAS, Ali AO, Mkopi A, Hassan A, Ali AM, et al. The status of maternal and newborn health care services in Zanzibar. BMC Pregnancy Childbirth. 2016;16:134. doi: 10.1186/s12884-016-0928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gabrysch S, Simushi V, Campbell OMR. Availability and distribution of, and geographic access to emergency obstetric care in Zambia. Int J Gynaecol Obstet. 2011;114:174–9. doi: 10.1016/j.ijgo.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 23.Kongnyuy EJ, Hofman J, Mlava G, Mhango C, van den Broek N. Availability, utilisation and quality of basic and comprehensive emergency obstetric care services in Malawi. Matern Child Health J. 2009;13:687–94. doi: 10.1007/s10995-008-0380-y. [DOI] [PubMed] [Google Scholar]
- 24.Oyerinde K, Harding Y, Amara P, Kanu R, Shoo R, Daoh K. The status of maternal and newborn care services in Sierra Leone 8 years after ceasefire. Int J Gynaecol Obstet. 2011;114:168–73. doi: 10.1016/j.ijgo.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 25.Admasu K, Haile-Mariam A, Bailey P. Indicators for availability, utilization, and quality of emergency obstetric care in Ethiopia, 2008. Int J Gynaecol Obstet. 2011;115:101–5. doi: 10.1016/j.ijgo.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 26.Compaoré GD, Sombié I, Ganaba R, Hounton S, Meda N, De Brouwere V, et al. Readiness of district and regional hospitals in Burkina Faso to provide caesarean section and blood transfusion services: a cross-sectional study. BMC Pregnancy Childbirth. 2014;14:158. doi: 10.1186/1471-2393-14-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kouanda S, Ouédraogo AM, Ouédraogo GH, Sanon D, Belemviré S, Ouédraogo L. Emergency obstetric and neonatal care needs assessment: Results of the 2010 and 2014 surveys in Burkina Faso. Int J Gynaecol Obstet. 2016;135:S11–5. doi: 10.1016/j.ijgo.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 28.Tembo T, Chongwe G, Vwalika B, Sitali L. Signal functions for emergency obstetric care as an intervention for reducing maternal mortality: a survey of public and private health facilities in Lusaka District, Zambia. BMC Pregnancy Childbirth. 2017;17:288. doi: 10.1186/s12884-017-1451-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tatem AJ, Campbell J, Guerra-Arias M, de Bernis L, Moran A, Matthews Z. Mapping for maternal and newborn health: the distributions of women of childbearing age, pregnancies and births. Int J Health Geogr. 2014;13:2. doi: 10.1186/1476-072X-13-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ebener S, Guerra-Arias M, Campbell J, Tatem AJ, Moran AC, Amoako Johnson F, et al. The geography of maternal and newborn health: the state of the art. Int J Health Geogr. 2015;14:19. doi: 10.1186/s12942-015-0012-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nesbitt RC, Gabrysch S, Laub A, Soremekun S, Manu A, Kirkwood BR, et al. Methods to measure potential spatial access to delivery care in low- and middle-income countries: a case study in rural Ghana. Int J Health Geogr. 2014;13:25. doi: 10.1186/1476-072X-13-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ouma PO, Maina J, Thuranira PN, Macharia PM, Alegana VA, English M, et al. Access to emergency hospital care provided by the public sector in sub-Saharan Africa in 2015: a geocoded inventory and spatial analysis. Lancet Glob Health. 2018;6:e342–50. doi: 10.1016/S2214-109X(17)30488-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Huerta Munoz U, Källestĺl C. Geographical accessibility and spatial coverage modeling of the primary health care network in the Western Province of Rwanda. Int J Health Geogr. 2012;11:40. doi: 10.1186/1476-072X-11-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alegana VA, Wright JA, Pentrina U, Noor AM, Snow RW, Atkinson PM. Spatial modelling of healthcare utilisation for treatment of fever in Namibia. Int J Health Geogr. 2012;11:6. doi: 10.1186/1476-072X-11-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Blanford JI, Kumar S, Luo W, MacEachren AM. It’s a long, long walk: accessibility to hospitals, maternity and integrated health centers in Niger. Int J Health Geogr. 2012;11:24. doi: 10.1186/1476-072X-11-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Macharia PM, Ouma PO, Gogo EG, Snow RW, Noor AM. Spatial accessibility to basic public health services in South Sudan. Geospat Health. 2017;12:510. doi: 10.4081/gh.2017.510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O’Neill K, Takane M, Sheffel A, Abou-Zahr C, Boerma T. Monitoring service delivery for universal health coverage: the Service Availability and Readiness Assessment. Bull World Health Organ. 2013;91:923–31. doi: 10.2471/BLT.12.116798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.WHO. Workload Indicators of Staffing Need: User’s Manual. Geneva, Switzerland: World Health Organization; 2010. 1-56 p. Available: http://www.who.int/hrh/resources/WISN_Eng_UsersManual.pdf Accessed: 28 November 2018.
- 39.Maliene V, Grigonis V, Palevičius V, Griffiths S. Geographic information system: Old principles with new capabilities. URBAN Des Int. 2011;16:1–6. doi: 10.1057/udi.2010.25. [DOI] [Google Scholar]
- 40.International Telecommunication Union. ICT facts and figures: the world in 2015. Geneva; 2015. Available: https://www.itu.int/en/ITU-D/Statistics/Documents/facts/ICTFactsFigures2015.pdf. Accessed: 28 November 2018.
- 41.Burgert CR, Colston J, Roy T, Zachary B. Geographic Displacement Procedure and Georeferenced Data Release Policy for the Demographic and Health Surveys. Calverton, Maryland, USA; 2013. (DHS Spatial Analysis Reports). Report No.: 7.
- 42.ESRI. ESRI shapefile technical description. California; 1998. (ESRI White Paer). Available: https://www.esri.com/library/whitepapers/pdfs/shapefile.pdf. Accessed: 28 November 2018.
- 43.Makanga PT, Schuurman N, von Dadelszen P, Firoz T. A scoping review of geographic information systems in maternal health. Int J Gynaecol Obstet. 2016;134:13–7. doi: 10.1016/j.ijgo.2015.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Salehi F, Ahmadian L. The application of geographic information systems (GIS) in identifying the priority areas for maternal care and services. BMC Health Serv Res. 2017;17:482. doi: 10.1186/s12913-017-2423-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.