Abstract
Objective
To explore current practice and influencing factors on adoption of the opportunistic salpingectomy (OS), particularly regarding the decision making, to eventually enhance the development and implementation of clear guidelines.
Methods
This nationwide cross-sectional survey study was conducted in all hospitals in the Netherlands. An anonymous online survey was sent to gynecologists with special interest in gynecological oncology, gynecological endoscopy or urogynecology and all Dutch gynecology trainees. The survey mainly focused on current practice regarding OS and identification of influencing factors on the level of innovation, organization, healthcare professional and individual patient.
Results
The response rate was 348 out of 597 gynecologists (58.3%) and 142 out of 340 trainees (41.8%). Current practice of discussing and performing the OS varied widely, with ovarian cancer (OC) risk reduction as most important supportive factor on innovation level. Supportive factors on the level of organization and healthcare provider were; working in a non-training hospital, knowledge of current literature and extensive work experience (in years and annual number of hysterectomies). On individual patient level, a vaginal approach of hysterectomy, negative family history for OC and the presence of firm adhesions were suppressive factors for the OS.
Conclusion
In this study we evaluated the current practice regarding the opportunistic salpingectomy in the Netherlands and identified influencing factors on different levels to raise awareness and attribute to development of a targeted implementation strategy, on both national and international level.
Keywords: Salpingectomy, Ovarian Neoplasms, Primary Prevention, Risk Reduction
INTRODUCTION
Ovarian cancer (OC) is often detected at an advanced stage of disease, limiting 5-year survival to 30%–40%. The lifetime risk to develop OC varies from 1.3% in the general population up to 17%–44% in BRCA 1/2 germline mutation carriers [1]. High grade serous ovarian cancer (HGSC) accounts for 70% of all epithelial OCs [2]. As curative therapies are limited and effective screening methods are lacking, emphasis should be directed towards preventive measures. Therefore, BRCA 1/2 germline mutation carriers are currently recommended to remove both ovaries and fallopian tubes (salpingo-oophorectomy) around the age of 40, resulting in premature menopause.
In the wake of the discovery of the Serous Tubal Intraepithelial Carcinoma (STIC) in 2001, the fallopian tube has been shown to play an important role in HGSC pathogenesis [3]. This insight has provided new opportunities for OC risk reduction by performing a salpingectomy. In BRCA 1/2 germline mutation carriers this finding led to the initiation of several studies (NCT02321228) [4]. These studies compare early salpingectomy (after completion of childbearing) and delayed oophorectomy with the standard salpingo-oophorectomy to delay menopause and increase quality of life.
For the general population, opportunistic salpingectomy (OS) is defined as an additional salpingectomy during (benign) pelvic surgery and is currently a point of discussion among gynecologists [5]. According to a recent meta-analysis, opportunistic removal of the Fallopian tubes might decrease the overall incidence of OC up to 50% [6]. Some researchers suggest a risk reduction up to 70%, based on the assumption that OS will prevent all OCs of the serous subtype (HGSC) [5]. However, an OS has potential downsides; the Fallopian tube and ovary partially share their blood supply and thus, salpingectomy could diminish ovarian reserve. Several studies investigated this issue, with no difference in ovarian reserve after salpingectomy [7,8,9]. Furthermore, there is no evidence for an increased complication rate after OS [6,8] and literature on surgical time suggests a minor increase of 0–13 minutes, depending on surgical approach [8,10,11,12].
Currently there is no consensus regarding OS in the Netherlands, resulting in a large variety of practice, probably due to a lack of clear guidelines. According to previous research in other countries, 43%–77% of gynecologists discuss the possibility of an OS [13,14,15]. It is likely that the adoption rate is influenced by several factors, which can be found on different levels, such as the innovation itself (OS), the organization of care, healthcare professionals attitudes towards OS and characteristics of the individual patient [16].
In this study we aim to explore current practice and the influencing factors on OS adoption, particularly regarding the decision making, to eventually enhance the development of clear guidelines and subsequent implementation.
MATERIALS AND METHODS
1. Study design and population
This observational cross-sectional study among gynecologists and obstetrics and gynecology trainees was conducted between October and December 2017. The nationwide study sample consisted of 605 gynecologists (members of the Dutch Society of Obstetrics and Gynecology [NVOG]) with special interest in gynecological oncology, gynecological endoscopy or urogynecology and all 364 current Dutch gynecology trainees.
2. Setting
All gynecologists in the Netherlands are affiliated to the NVOG and benign pelvic surgery is solely performed in community hospitals with affiliations to all Dutch healthcare insurance companies. The surgeries investigated in this survey are performed in all 92 Dutch hospitals and is fully covered by the health insurance after paying a flat rate each year when using healthcare in general. The costs of all surgeries exceed this flat rate, which means an additional salpingectomy does not influence the individual patient's costs.
3. Development survey
The survey was developed by a team of researchers and clinicians (S.M., H.R.P.M.G., C.S.F.P.J. and D.H.J.A.) based on current literature and subsequently pilot-tested by A.J.W.M., V.L.L.A.M. and H.D. The survey consisted of four subsections with 44 questions in total. It included questions about demographics, current practice of OS and subsections to identify influencing factors on different levels as formulated by Grol et al. [16]. The survey focused particularly on the level of the innovation (OS), organization, healthcare professional and individual patient [16];
• The questions about baseline demographics for gynecologists contained information about the years of work experience, type of institution, special interest, number of (vaginal) hysterectomies performed annually and the knowledge of current literature. For trainees, the questions were about the year of residency, special interest, number of (vaginal) hysterectomies performed and also the knowledge of current literature. Knowledge of current literature was based on self-assessment of the respondents with three possible answers; 1) knowledge of current literature on the suggested influence of OS for OC risk reduction (hypothesis), 2) knowledge of the hypothesis but not the literature itself, or 3) no knowledge of the hypothesis at all.
• The current practice domain (12 questions) covered both how frequent patients were informed on the possibility of OS and how frequent the procedure was carried out.
• Potential supportive and suppressive influencing factors were identified from literature and could be stratified according to perceived importance. Most of the included potential influencing factors were on the level of the innovation itself. Respondents were asked to allocate a total of 100 points to different influencing factors, allocating the highest amount of points to the most important factor. Influencing factors not covered by the questionnaire could be reported in a free text field.
• To identify and stratify influencing factors on patient level, case-vignettes were designed. The vignettes consisted of a fictive case of a 40-year old women intending to undergo a hysterectomy for menstrual complaints with varying patient-specific factors such as surgical modality (abdominal, laparoscopic or vaginal approach), family history (no or one family member with OC) and presence of intra-abdominal adhesions (mild or firm). Prior to presentation of the case-vignette, respondents received a short overview of background information, consisting of the lifetime risk of OC in the general population (1.3%), in patients with one family member with OC (2.5%) and the estimated risk reduction attributed to OS (50%–70%). As this study focused on the general population, there was no vignette with more than one family member with OC. The section started out with a vignette of a patient in optimal circumstances to advise salpingectomy (abdominal approach, one family member with OC and no intra-abdominal adhesions). Further on, patient-specific factors got more complicated and the number of respondents willing and reluctant to advise OS due to a combination of factors were identified (15 questions).
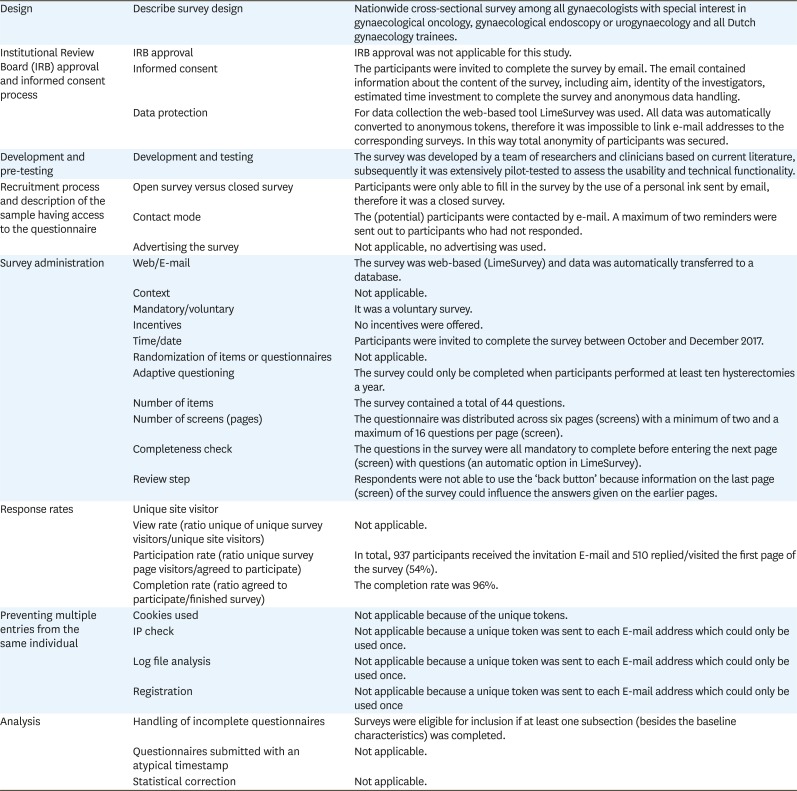
4. Data collection
A nationwide email-survey was sent out with an online computer programme using anonymous tokens so no identifiable information was collected. Due to the nature of the survey and anonymous collection of data, institutional review board approval was not required for this study. All fields in the questionnaire were set to be obligatory to answer in order to minimize missing data. It took approximately 10 minutes to complete the survey. A maximum of two reminders were sent out to non-responding participants. Surveys were eligible for inclusion if at least one subsection after baseline characteristics was completed. In the baseline characteristics section, gynecologists were asked to estimate the number of hysterectomies performed annually. If this number was below ten, the questionnaire could not be completed and ended after baseline characteristics. The Checklist for Reporting Results of Internet E-Surveys (CHERRIES) was followed (Appendix 1) [17].
5. Data analysis
Data was analyzed in SPSS (released 2013, IBM SPSS Statistics, version 22.0; IBM Corp., Chicago, IL, USA). Baseline characteristics of respondents, results on the current practice domain and the influencing factors on innovation and individual level were descriptively analyzed (median with interquartile range [IQR] and percentages). Influencing factors on organization and professional level were analyzed by the use of multivariate logistic regression analysis. As dependent variable, the current practice was converted to a bivariate variable (‘never,’ ‘rarely,’ ‘about half the time’ versus ‘usually,’ ‘always’) per type of surgery. The following baseline characteristics were used as independent variables among gynecologists; years of work experience, type of institution, special interest, number of (vaginal) hysterectomies performed annually and knowledge of current literature. Among trainees the imputed independent variables were; year of residency, number of (vaginal) hysterectomies performed with or without supervision and the knowledge of current literature. At first, univariate logistic regression analysis was performed and independent variables with a p-value ≤0.20 were analyzed in multivariate logistic regression analysis. The multivariate analysis was performed using backward-stepwise method and a p-value ≤0.05 was considered statistically significant.
RESULTS
1. Study population
In total, we received 510 responses, 20 of which were excluded because respondents did not fill out one complete domain, apart from baseline characteristics. The response rate was 348 out of 597 gynecologists (58.3%) and 142 out of 340 trainees (41.8%). A total of 47 gynecologists reported to perform less than ten hysterectomies per year, meaning that these surveys were not eligible for analysis. Ultimately, 443 surveys were included in the analysis, consisting of 68% gynecologists and 32% trainees.
The median duration of work experience among gynecologists was 12 years (IQR 7–19) and was over 25 years for 33 out of 301 (11%) gynecologists. Approximately two-thirds of the gynecologists (67.1%) worked in a (academic) training-hospital. Most respondents had special interest in benign gynecology/endoscopy and gynecologic oncology (70.2%). Out of 142 trainees, 49 were in the final two years of their training and started a subject of special interest (e.g., urogynecology, gynecologic oncology or benign gynecology). The most common subject of special interest was partially the same as among gynecologists (benign gynecology/endoscopy) (Table 1).
Table 1. Baseline characteristics of respondents.
| Baseline characteristics | Value | ||
|---|---|---|---|
| Gynecologists | 301 (67.9) | ||
| Work experience in years | 12 (7–19) | ||
| Type of institution | |||
| (Academic) Training hospital | 202 (67.1) | ||
| Non-academic non-training hospital | 99 (32.9) | ||
| Special interest | |||
| Urogynecology | 102 (23.0) | ||
| Benign gynecology/endoscopy | 191 (43.1) | ||
| Gynecologic oncology | 120 (27.1) | ||
| Other | 6 (2.0) | ||
| No. of hysterectomies per year | 30 (20–40) | ||
| No. of vaginal hysterectomies per year | 5 (0–12) | ||
| Knowledge of current literature | |||
| Knows current literature | 182 (60.5) | ||
| Knows hypothesis, not the literature | 119 (39.5) | ||
| Never heard of hypothesis | 0 (0.0) | ||
| Gynecology trainees | 142 (32.1) | ||
| Year of residency | |||
| 1 or 2 | 39 (27.5) | ||
| 3 or 4 | 54 (38.0) | ||
| 5 or 6 | 49 (34.5) | ||
| Special interest (residents in 5th or 6th year only) | |||
| Urogynecology | 2 (4.1) | ||
| Benign gynecology/endoscopy | 15 (30.6) | ||
| Gynecologic oncology | 9 (18.4) | ||
| Other/unknown | 23 (53.1) | ||
| No. of hysterectomies performed with or without supervision | 25 (10–50) | ||
| No. of vaginal hysterectomies performed with or without supervision | 8 (3–15) | ||
| Knowledge of current literature | |||
| Knows current literature | 57 (40.1) | ||
| Knows hypothesis, not the literature | 85 (59.9) | ||
| Never heard of hypothesis | 0 (0.0) | ||
Values are presented as number (%) or median (interquartile range).
2. Current practice of the opportunistic salpingectomy
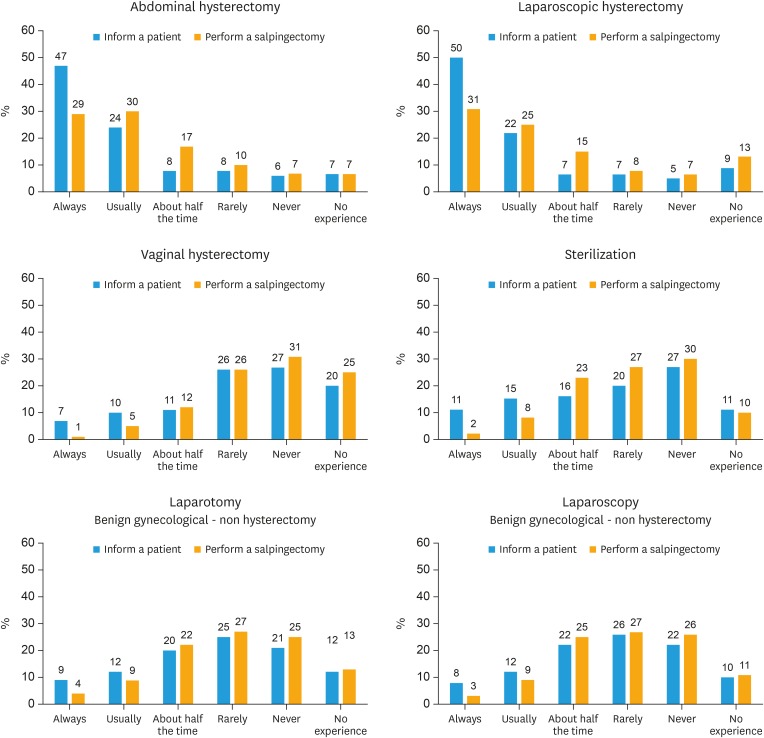
Out of 443 respondents, 71.3% said to always or in the majority of cases discuss OS when planning an abdominal hysterectomy; 58.7% said to always or in the majority of the cases perform an OS. In case of laparoscopic hysterectomy, the results were 71.3% and 56.2%, respectively. In the discussion of vaginal hysterectomy, the respondents indicated OS to be feasible in a median of five out of ten vaginal hysterectomies (IQR 2–7). Gynecologists who performed over 30 vaginal hysterectomies a year expected feasibility in eight out of ten vaginal hysterectomies (range 4–9). Furthermore, 6.7% reported to always or usually inform patients about OS prior to vaginal hysterectomy, 26.9% never discussed this possibility with patients. The actual performance rate was reported as always or usually by 6.3% of respondents. Approximately half of the respondents indicated to rarely or never discuss OS in case of a laparotomy (46.0%) or laparoscopy (48.5%), other than hysterectomy. In terms of permanent contraception, 47.2% said to never or rarely inform patients on the option of salpingectomy. Approximately one third of the respondents (33.0%) did perform salpingectomies as sterilization technique in at least half of the patients. The abovementioned results are summarized in Fig. 1.
Fig. 1. Current practice of gynecologists and trainees in The Netherlands.
3. Influencing factors related to the OS
Domain 1: influencing factors at innovation level
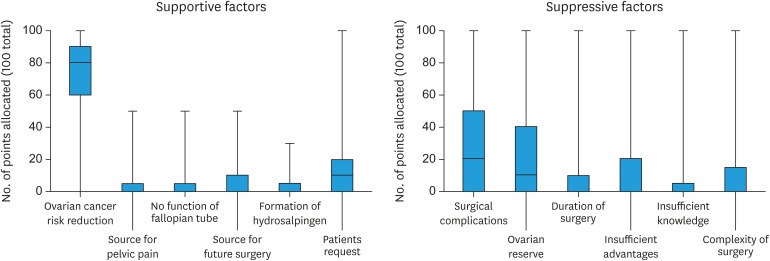
A total of 408 respondents completed this section (Fig. 2). Among the supportive factors, reduction of OC risk was the most important and heavy weighing (median of 80 points, IQR 60–90), followed by the explicit request from a patient (median of 10 points, IQR 0–20). Supportive factors mentioned in the free text field were the removal of sterilization devices (e.g., clips or rings) or a positive family history of OC.
Fig. 2. A forest plot of potential influencing factors and the distribution of allocated points.
The stratification of suppressive factors was more diverse, with an approximately equal rank for possible increased surgical risk (median of 20 points, IQR 0–50) and possible negative effect on ovarian reserve (median of 10 points, IQR 0–40). Other factors (suggested in free text fields) were complicated or difficult situations (for example due to adhesions), no consent from the patient and the lack of a Dutch guideline on OS.
Respondents were reluctant to recommend OS as definitive contraception technique because no options for re-fertilization are available (37.7%), insufficient proof of potential benefits (31.4%), possibly increased risk of complications (30.9%), possibly deleterious effects on ovarian reserve (25.7%) and prolonged duration of surgery (22.6%). Furthermore, 22 respondents commented that lack of consensus in the Netherlands formed the most important reason not to advise OS as method of sterilization.
Domain 2: influencing factors at organization and healthcare professional level
When counseling a patient for surgery, gynecologists with more knowledge of current literature were more likely to usually or always discuss OS, just as gynecologists working in a non-training hospital. Work experience, either in years or number of procedures a year, was also a factor in whether or not gynecologists discuss OS, especially in vaginal hysterectomies.
A higher performance rate was found among gynecologists from non-training hospitals. Another supportive factor was knowledge of current literature and not just the hypothesis. Furthermore, the amount of work experience in years was positively correlated with higher performance rate of OS. During laparotomy for benign gynecological disease or tubal sterilization, the subgroup of gynecologists with a special interest in oncology was more likely to perform OS compared to gynecologists with other interests.
For trainees, only the knowledge of current literature was a significant supportive factor for OS in laparotomy for benign gynecological disease. An overview of all statistically significant results is presented in Table 2.
Table 2. Multivariate analysis of influencing factors on organization and professional level.
| Variables | Never, rarely, half the time | Usually, always | Univariate analysis | Multivariate analysis | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | |||||||
| Gynecologists (n=301) | ||||||||||
| Discuss the OS in case of: | ||||||||||
| Abdominal hysterectomy | Type of institution | Non-training hospital | 14 | 83 | 1 | 1 | ||||
| Training hospital | 52 | 144 | 0.47 (0.24–0.89) | 0.02 | 0.43 (0.23–0.83) | 0.01 | ||||
| Knowledge of current literature, not just the hypothesis | No | 33 | 83 | 1 | 1 | |||||
| Yes | 33 | 144 | 1.74 (1.00–3.02) | 0.05 | 1.89 (1.08–3.33) | 0.03 | ||||
| Laparoscopic hysterectomy | Type of institution | Non-training hospital | 18 | 77 | 1 | 1 | ||||
| Training hospital | 76 | 119 | 0.37 (0.20–0.66) | 0.00 | 0.37 (0.20–0.66) | 0.00 | ||||
| Vaginal hysterectomy | Knowledge of current literature, not just the hypothesis | No | 90 | 19 | 1 | 1 | ||||
| Yes | 96 | 46 | 2.27 (1.24–4.17) | 0.01 | 2.07 (1.10–3.88) | 0.02 | ||||
| Work experience (yr) | 10 (6–16) | 17 (9–24) | 1.07 (1.03–1.11) | 0.00 | 1.08 (1.04–1.12) | 0.00 | ||||
| Vaginal hysterectomies a year | 8 (3–15) | 7 (2–10) | 0.97 (0.94–1.01) | 0.12 | 0.96 (0.93–0.99) | 0.04 | ||||
| Benign gynecological laparoscopy | No. of hysterectomies a year | 30 (20–40) | 30 (25–40) | 1.01 (1.00–1.02) | 0.15 | 1.01 (1.00–1.03) | 0.04 | |||
| Sterilization | Knowledge of current literature, not just the hypothesis | No | 94 | 21 | 1 | 1 | ||||
| Yes | 98 | 60 | 2.74 (1.55–4.86) | 0.00 | 2.74 (1.54–4.86) | 0.00 | ||||
| Perform the OS in case of: | ||||||||||
| Abdominal hysterectomy | Type of institution | Non-training hospital | 18 | 77 | 1 | 1 | ||||
| Training hospital | 76 | 119 | 0.37 (0.20–0.66) | 0.00 | 0.37 (0.20–0.66) | 0.00 | ||||
| Laparoscopic hysterectomy | Type of institution | Non-training hospital | 15 | 72 | 1 | 1 | ||||
| Training hospital | 66 | 112 | 0.35 (0.19–0.67) | 0.00 | 0.35 (0.19–0.67) | 0.00 | ||||
| Vaginal hysterectomy | Knowledge of current literature, not just the hypothesis | No | 90 | 19 | 1 | 1 | ||||
| Yes | 96 | 46 | 4.86 (1.61–14.64) | 0.01 | 4.30 (1.39–13.33) | 0.01 | ||||
| Work experience (yr) | 11 (6–18) | 20 (13–27) | 1.12 (1.06–1.18) | 0.00 | 1.11 (1.05–1.17) | 0.00 | ||||
| Benign gynecological laparotomy | Work experience (yr) | 11 (6–17) | 14.5 (8–24) | 1.12 (1.06–1.18) | 0.00 | 1.05 (1.01–1.10) | 0.01 | |||
| Special interest in oncology | No | 129 | 45 | 1 | 1 | |||||
| Yes | 71 | 33 | 2.40 (1.04–5.56) | 0.00 | 2.90 (1.52–5.54) | 0.00 | ||||
| Benign gynecological laparoscopy | Work experience (yr) | 11 (6–18) | 14 (9–24) | 1.05 (1.01–1.09) | 0.01 | 1.05 (1.01–1.09) | 0.02 | |||
| Knowledge of current literature, not just the hypothesis | No | 102 | 10 | 1 | 1 | |||||
| Yes | 132 | 34 | 2.55 (1.24–5.25) | 0.01 | 2.48 (1.16–5.28) | 0.02 | ||||
| Sterilization | Type of institution | Non-training hospital | 79 | 16 | 1 | 1 | ||||
| Training hospital | 160 | 18 | 0.56 (0.27–1.15) | 0.11 | 0.41 (0.19–0.89) | 0.02 | ||||
| Work experience (yr) | 10 (6–18) | 16 (8–25) | 1.07 (1.02–1.12) | 0.00 | 1.08 (1.03–1.12) | 0.00 | ||||
| Special interest in oncology | No | 161 | 15 | 1 | 1 | |||||
| Yes | 78 | 19 | 2.62 (1.26–5.42) | 0.01 | 2.87 (1.34–6.17) | 0.01 | ||||
| Gynecology trainees (n=142) | ||||||||||
| Discuss the OS in case of: | ||||||||||
| Benign gynecological laparotomy | Knowledge of current literature, not just the hypothesis | No | 59 | 6 | 1 | 1 | ||||
| Yes | 33 | 12 | 3.58 (1.23–10.41) | 0.02 | 3.58 (1.23–10.41) | 0.02 | ||||
Values are presented as number or median (interquartile range).
CI, confidence interval; OR odds ratio; OS, opportunistic salpingectomy.
Domain 3: influencing factors at individual patient level
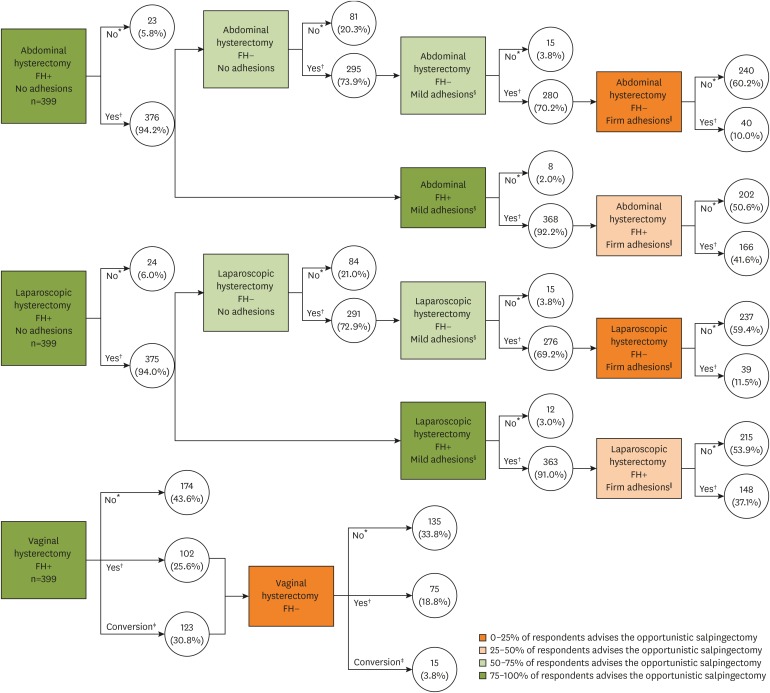
The recommendation on whether or not to perform OS based on patient characteristics, is represented in Fig. 3. In the optimal situation (e.g., abdominal or laparoscopic approach, one family member with OC and no intra-abdominal adhesions) 94% of the respondents would advise OS. For patients with a negative family history of OC, approximately 73% of the respondents would advise OS. Mild adhesions lead to a decline of approximately 3% while firm adhesions were a suppressive factor for an extra 50%–60% of the respondents, resulting in approximately 11% of respondents advising OS when combined with a negative family history. In case of one family member with OC, respondents were more willing to perform OS, with an additional 25.6%–31.6% of the respondents advising OS.
Fig. 3. Influencing factors on individual patient level.
FH+, one first-degree family member with ovarian cancer; FH−, no first-degree family member with ovarian cancer.
*Salpingectomy advised: no; †Salpingectomy advised: yes; ‡Advise to perform laparoscopic hysterectomy instead of the vaginal approach; §Mild adhesions are defined as easily to be removed, with minimal risk of damaging adjacent organs; ∥Firm adhesions are defined as difficult to remove, with risk of damaging adjacent organs.
In case of vaginal hysterectomy, 56.4% of the respondents reported to recommend OS to patients with a positive family history. Of these respondents, 54.6% advised a strategic conversion to laparoscopy to perform OS. In case of a negative family history, OS was recommended by 22.6% of the respondents and 3.8% advised the strategic conversion. The most important reason to strategically convert a vaginal hysterectomy to laparoscopy was to maximize the chances of a successful OS (76.6%). Other reasons were a possibly increased complication rate in case of a vaginal approach (50.8%) and technical difficulties (41.1%). An important consideration to persevere in the vaginal route was the preference for the vaginal approach according to the Dutch guideline (76.2%).
Respondents were also asked about their recommendations on OS as sterilization technique. A total of 84 (20.7%) respondents would advise OS to all patients, 101 (24.9%) respondents would recommend OS to patients with one family member with OC and a total of 221 (54.4%) would not recommend OS at all, but would advise other techniques instead (i.e., clips, rings).
DISCUSSION
In this nationwide study performed in the Netherlands, we assessed both the current practice and influencing factors on the level of innovation, organization, healthcare professional and individual patient characteristics. The diverse results in the current practice domain represent the lack of consensus in the Netherlands regarding OS. On the level of innovation, OC risk-reduction was considered to be the most influential factor. On organizational level, OS appeared to be more routinely implemented in non-training hospitals compared to training hospitals. On healthcare professional level, implementation was mainly dependent on the knowledge of current literature, years of work experience and annual number of (vaginal) hysterectomies performed. Among trainees, solely knowledge of current literature was associated with higher performance rate when discussing OS preceding laparotomy for benign gynecological disease. Strong influencing factors on individual patient level were vaginal approach of hysterectomy, negative family history of OC and presence of firm adhesions during surgery.
On innovation level, OC risk risk-reduction was by far the most influential factor in favor of OS. Intervention-related factors not to perform OS were possible effect on surgical risk and ovarian reserve. In addition, the absence of a Dutch guideline was perceived as a suppressive factor for OS. Previous research however, has not found evidence for an increased complication risk, estimated blood loss or duration of hospital stay [8,10,18]. Furthermore, studies on ovarian reserve after OS found no difference in ovarian function after hysterectomy with or without OS [8,10].
On organizational level, OS appeared to be better implemented in non-training hospitals when compared to training hospitals. This finding is in contrast with our expectations. The number of hysterectomies a gynecologist performs a year would have been a plausible explanation, yet in our cohort the number of hysterectomies per gynecologist was higher in training hospitals. Although unlikely, the lower implementation rate in training hospitals might be the result of reluctance to ‘complicate’ the procedure for trainees with an additional surgical step. Furthermore, several respondents commented on the absence of a univocal guideline in the Netherlands. Over the past few years several countries published statements and guidelines regarding OS. The general tendency of these papers is that in patients at population risk of OC, OS should be considered and discussed prior to hysterectomy (American College of Obstetricians and Gynecologists [ACOG], Arbeitsgemeinschaft Gynäkologische Onkologie [AGO], The Society of Gynecologic Oncology of Canada [GOC], Royal Australian and New Zealand College of Obstetricians and Gynaecologists [RANZCOG]) and other pelvic surgery (Royal College of Obstetricians and Gynecologists [RCOG], Society of Gynecologic Oncology [SGO]) [19,20,21,22]. Yet, the implementation of new innovations goes beyond guideline development and is in need of a specific implementation strategy to achieve the aimed change [16]. In Canada, efforts to increase the implementation of OS have increased the number of hysterectomies with OS from 5% to 35% in a few years' time [23].
On healthcare professional level, OS was more likely to be adopted by experienced gynecologists (either in years of work experience or amount of hysterectomies performed annually) and in case of knowledge of current literature. These insights create opportunities to improve OS adoption as increased surgical risk and possible decrease of ovarian reserve were most frequently mentioned as suppressive factor. Thus, improvement in knowledge of current literature might increase implementation rate. Despite our findings, Jones et al. [15] investigated the implementation of OS and found no association between practice patterns and physicians characteristics. This discrepancy could be explained by differences in the subset of analyzed characteristics or study population. Aside from our findings regarding professional experience, gynecological surgeries performed by high-volume surgeons are associated with lower conversion rates, decreased operative complication rates and shorter duration of hospital stay [24]. Moreover, for gynecological surgeons with advanced surgical skills, the addition of a surgical step is probably less challenging, with easier implementation of OS consequently.
On individual patient level, the most influencing factors were a vaginal approach of hysterectomy, negative family history of OC and presence of firm adhesions. The realization of OS is more challenging during vaginal hysterectomy when compared to a laparoscopic or abdominal approach. Therefore, a tailored approach to OS during this type of surgery is comprehensible. Previous research demonstrated OS to be feasible in 81%–88% of vaginal hysterectomies [12,25]. However, respondents in our cohort estimated OS to be feasible in approximately half of the cases. This difference could be explained by the type of gynecologists performing the hysterectomies in the feasibility studies. Furthermore, decreasing number of vaginal hysterectomies per gynecologist might lead to a loss of expertise and less gynecologists with sufficient experience to safely perform the intervention. In the study of Robert et al. [25] all hysterectomies were performed or supervised by two experienced vaginal surgeons and in the study of Antosh et al. [12] the type of gynecologists performing the surgeries were not specified. The more experienced gynecologists in the present study (performing over 30 vaginal hysterectomies annually) estimated the feasibility to be 80% [12,25].
Aside from feasibility of OS during vaginal hysterectomy, very few patient-specific factors have been investigated prior to this survey study on the overall implementation of OS. However, patient-specific factors are essential when aiming for a more widespread adoption of OS. A higher performance rate will result in OS implementation among an increased variety of circumstances, including difficult surgeries (in the case of firm adhesions for example). However, as OS is a preventive measure, it should not be carried out at all costs. Generally, the costs should always be weighed against the (potential) benefits; our respondents agree that firm adhesions appear to be a strong influencing factor.
There are several strengths and limitations in the present study. The nationwide character gives a representative view on different influencing factors. The influencing factors among OS have not been investigated before and therefore attribute to specific implementation strategies on both a national and international basis. Additionally, the use of a case-vignette provides results that give insight in daily practice and increases the accuracy of self-assessment of the respondents. On the contrary, the self-assessment of respondents is one of the possible limitations of the study as self-assessment is susceptible to recall bias. Moreover, less than 50% of the trainees (against almost 60% of the gynecologists) filled in the questionnaire and possibly our respondents are more prone to complete the questionnaire when interested in the OS. Therefore, non-responders might have an even lower rate of OS in the current practice. This is a potential source of selection bias in the results and therefore the results might not be applicable to all gynecologists and trainees in general. However, the representation of gynecologists from the various types of organizations in our study was similar to the current situation in the Netherlands, with approximately one-third of the gynecologists working in a non-training hospital [26]. Although extrapolation of results to gynecologists and trainees in other countries is complicated.
In this study we objectified the current care regarding OS in the Netherlands and identified influencing factors on different levels to raise awareness and attribute to development of a specific implementation strategy, on both national and international level. Future research should be focused on the presence of factors identified in this study in the actual clinical practice and the effect of specific implementation strategies.
ACKNOWLEDGEMENTS
We would like to thank Dana Huppelschoten (D.H.) for extensive pilot-testing of the questionnaire prior to this study and Steven Teerenstra for statistical support.
Appendix 1
CHERRIES checklist
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
- Conceptualization: S.M., H.R.P.M.G., D.H.J.A.
- Data curation: S.M., V.L.L.A.M., A.J.W.M., P.J.M.J., C.S.F.P.J., M.L.F.A.G., H.R.P.M.G., D.H.J.A.
- Formal analysis: S.M., V.L.L.A.M., H.R.P.M.G., D.H.J.A.
- Methodology: S.M., H.R.P.M.G., C.S.F.P.J., D.H.J.A.
- Software: S.M., H.R.P.M.G.
- Supervision: A.J.W.M., P.J.M.J., C.S.F.P.J., M.L.F.A.G., H.R.P.M.G., D.H.J.A.
- Validation: S.M., H.R.P.M.G., D.H.J.A.
- Visualization: S.M., V.L.L.A.M.
- Writing - original draft: S.M., V.L.L.A.M.
- Writing - review & editing: A.J.W.M., P.J.M.J., C.S.F.P.J., M.L.F.A.G., H.R.P.M.G., D.H.J.A.
References
- 1.Kuchenbaecker KB, Hopper JL, Barnes DR, Phillips KA, Mooij TM, Roos-Blom MJ, et al. Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA. 2017;317:2402–2416. doi: 10.1001/jama.2017.7112. [DOI] [PubMed] [Google Scholar]
- 2.McCluggage WG. Morphological subtypes of ovarian carcinoma: a review with emphasis on new developments and pathogenesis. Pathology. 2011;43:420–432. doi: 10.1097/PAT.0b013e328348a6e7. [DOI] [PubMed] [Google Scholar]
- 3.Piek JM, van Diest PJ, Zweemer RP, Jansen JW, Poort-Keesom RJ, Menko FH, et al. Dysplastic changes in prophylactically removed fallopian tubes of women predisposed to developing ovarian cancer. J Pathol. 2001;195:451–456. doi: 10.1002/path.1000. [DOI] [PubMed] [Google Scholar]
- 4.Harmsen MG, Arts-de Jong M, Hoogerbrugge N, Maas AH, Prins JB, Bulten J, et al. Early salpingectomy (TUbectomy) with delayed oophorectomy to improve quality of life as alternative for risk-reducing salpingo-oophorectomy in BRCA1/2 mutation carriers (TUBA study): a prospective non-randomised multicentre study. BMC Cancer. 2015;15:593. doi: 10.1186/s12885-015-1597-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dilley SE, Straughn JM. Leath CA. The evolution of and evidence for opportunistic salpingectomy. Obstet Gynecol. 2017;130:814–824. doi: 10.1097/AOG.0000000000002243. [DOI] [PubMed] [Google Scholar]
- 6.Yoon SH, Kim SN, Shim SH, Kang SB, Lee SJ. Bilateral salpingectomy can reduce the risk of ovarian cancer in the general population: a meta-analysis. Eur J Cancer. 2016;55:38–46. doi: 10.1016/j.ejca.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 7.Venturella R, Lico D, Borelli M, Imbrogno MG, Cevenini G, Zupi E, et al. 3 to 5 years later: long-term effects of prophylactic bilateral salpingectomy on ovarian function. J Minim Invasive Gynecol. 2017;24:145–150. doi: 10.1016/j.jmig.2016.08.833. [DOI] [PubMed] [Google Scholar]
- 8.Van Lieshout LA, Pijlman B, Vos MC, de Groot MJ, Houterman S, Coppus SF, et al. Opportunistic salpingectomy in women undergoing hysterectomy: results from the HYSTUB randomised controlled trial. Maturitas. 2018;107:1–6. doi: 10.1016/j.maturitas.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Song T, Kim MK, Kim ML, Jung YW, Yun BS, Seong SJ, et al. Impact of opportunistic salpingectomy on anti-Müllerian hormone in patients undergoing laparoscopic hysterectomy: a multicentre randomised controlled trial. BJOG. 2017;124:314–320. doi: 10.1111/1471-0528.14182. [DOI] [PubMed] [Google Scholar]
- 10.Song T, Lee SH, Kim WY, Heo EJ, Kim TJ. Opportunistic salpingectomy does not affect ovarian reserve or surgical outcomes in patients undergoing laparoscopic myomectomy. Gynecol Obstet Invest. 2017;82:468–474. doi: 10.1159/000452663. [DOI] [PubMed] [Google Scholar]
- 11.Ganer Herman H, Gluck O, Keidar R, Kerner R, Kovo M, Levran D, et al. Ovarian reserve following cesarean section with salpingectomy vs tubal ligation: a randomized trial. Am J Obstet Gynecol. 2017;217:472.e1–472.e6. doi: 10.1016/j.ajog.2017.04.028. [DOI] [PubMed] [Google Scholar]
- 12.Antosh DD, High R, Brown HW, Oliphant SS, Abed H, Philip N, et al. Feasibility of prophylactic salpingectomy during vaginal hysterectomy. Am J Obstet Gynecol. 2017;217:605.e1–605.e5. doi: 10.1016/j.ajog.2017.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gill SE, Mills BB. Physician opinions regarding elective bilateral salpingectomy with hysterectomy and for sterilization. J Minim Invasive Gynecol. 2013;20:517–521. doi: 10.1016/j.jmig.2013.02.010. [DOI] [PubMed] [Google Scholar]
- 14.Chene G, de Rochambeau B, Le Bail-Carval K, Beaufils E, Chabert P, Mellier G, et al. Current surgical practice of prophylactic and opportunistic salpingectomy in France. Gynecol Obstet Fertil. 2016;44:377–384. doi: 10.1016/j.gyobfe.2016.05.003. [DOI] [PubMed] [Google Scholar]
- 15.Jones NL, Schulkin J, Urban RR, Wright JD, Burke WM, Hou JY, et al. Physicians' perspectives and practice patterns toward opportunistic salpingectomy in high- and low-risk women. Cancer Invest. 2017;35:51–61. doi: 10.1080/07357907.2016.1242597. [DOI] [PubMed] [Google Scholar]
- 16.Grol R, Wensing M, Eccles M. Improving patient care: the implementation of change in clinical practice. Edinburgh/New York: Elsevier Butterworth Heinemann; 2005. [Google Scholar]
- 17.Eysenbach G. Improving the quality of web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) J Med Internet Res. 2004;6:e34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ghezzi F, Cromi A, Siesto G, Bergamini V, Zefiro F, Bolis P. Infectious morbidity after total laparoscopic hysterectomy: does concomitant salpingectomy make a difference? BJOG. 2009;116:589–593. doi: 10.1111/j.1471-0528.2008.02085.x. [DOI] [PubMed] [Google Scholar]
- 19.Pölcher M, Hauptmann S, Fotopoulou C, Schmalfeldt B, Meinhold-Heerlein I, Mustea A, et al. Opportunistic salpingectomies for the prevention of a high-grade serous carcinoma: a statement by the Kommission Ovar of the AGO. Arch Gynecol Obstet. 2015;292:231–234. doi: 10.1007/s00404-015-3697-y. [DOI] [PubMed] [Google Scholar]
- 20.Committee on Gynecologic Practice Committee opinion No. 620: salpingectomy for ovarian cancer prevention. Obstet Gynecol. 2015;125:279–281. doi: 10.1097/01.AOG.0000459871.88564.09. [DOI] [PubMed] [Google Scholar]
- 21.Salvador S, Scott S, Francis JA, Agrawal A, Giede C. No. 344-opportunistic salpingectomy and other methods of risk reduction for ovarian/fallopian tube/peritoneal cancer in the general population. J Obstet Gynaecol Can. 2017;39:480–493. doi: 10.1016/j.jogc.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 22.Royal College of Obstetricians & Gynaecologists. The distal fallopian tube as the origin of non-uterine pelvic high-grade serous carcinoma. Scientific impact paper No. 44. London: Royal College of Obstetricians & Gynaecologists; 2014. [Google Scholar]
- 23.McAlpine JN, Hanley GE, Woo MM, Tone AA, Rozenberg N, Swenerton KD, et al. Opportunistic salpingectomy: uptake, risks, and complications of a regional initiative for ovarian cancer prevention. Am J Obstet Gynecol. 2014;210:471.e1–471.11. doi: 10.1016/j.ajog.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 24.Worley MJ, Jr, Anwandter C, Sun CC, dos Reis R, Nick AM, Frumovitz M, et al. Impact of surgeon volume on patient safety in laparoscopic gynecologic surgery. Gynecol Oncol. 2012;125:241–244. doi: 10.1016/j.ygyno.2011.12.452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robert M, Cenaiko D, Sepandj J, Iwanicki S. Success and complications of salpingectomy at the time of vaginal hysterectomy. J Minim Invasive Gynecol. 2015;22:864–869. doi: 10.1016/j.jmig.2015.04.012. [DOI] [PubMed] [Google Scholar]
- 26.van der Velden LFJ, Hingstman L. Monitor arbeidsmarkt gynaecologen 2006. Utrecht: NIVEL; 2006. [Google Scholar]