Abstract
Objective:
Few studies have reported blood lead levels (BLLs) in Haitian children, despite the known presence of lead from environmental factors such as soil, water, leaded paint and gasoline, improperly discarded batteries, and earthquakes. We sought to determine the prevalence of elevated blood lead levels (EBLLs) among healthy Haitian children.
Methods:
We enrolled children aged 9 months to 6 years from 3 geographic areas in Haiti (coastal, urban, and mountain) from March 1 through June 30, 2015. We obtained anthropometric measurements, household income, potential sources of lead exposure, and fingerstick BLLs from 273 children at 6 churches in Haiti. We considered a BLL ≥5 μg/dL to be elevated.
Results:
Of 273 children enrolled in the study, 95 were from the coastal area, 78 from the urban area, and 100 from the mountain area. The median BLL was 5.8 μg/dL, with higher levels in the mountain area than in the other areas (P < .001). BLLs were elevated in 180 (65.9%) children. The prevalence of EBLL was significantly higher in the mountain area (82 of 100, 82.0%; P < .001) than in the urban area (42 of 78, 53.8%) and the coastal area (56 of 95, 58.9%; P < .001). Twenty-eight (10.3%) children had EBLLs ≥10 μg/dL and 3 (1.1%) children had EBLLs ≥20 μg/dL. Exposure to improperly discarded batteries (P = .006) and living in the mountain area (P < .001) were significant risk factors for EBLLs.
Conclusions:
More than half of Haitian children in our study had EBLLs. Public health interventions are warranted to protect children in Haiti against lead poisoning.
Keywords: lead, global health, child health, pediatrics, environmental exposures
Lead is ubiquitous in the environment and comprises a small proportion of the Earth’s crust.1–4 Human exposure to lead increases when the earth’s floor is disrupted by events such as volcanic eruptions, earthquakes, or mining.1–4 However, most human exposure to lead is associated with industrialization and the use of products as varied as soldered pipes, pigments in paint, leaded gasoline, batteries, ammunition, and traditional medicines.5–14
Lead is a highly toxic metal, environmental contaminant, and neurotoxin that can impair human development. Lead poisoning can cause anemia, impaired hearing, delayed puberty, nephrotoxicity, convulsions, coma, and death.15–23 Low levels of lead can cause hypertension and affect the immune system.24–28 Perhaps the most profound consequence of lead exposure, which can occur at any level, is its impact on the central nervous system. Lead exposure is associated with hyperactivity, behavioral disorders, reduced intelligence, and impaired cognitive and neuromotor function.29–38 A population’s mean intelligence quotient is estimated to decrease by 1 point for every 0.3 μg/dL (range, 0.2-1.4 μg/dL) increase in blood lead levels (BLLs).26 These deleterious effects have important economic consequences related to health, crime, and lost earnings, and the largest burden is on low- and middle-income countries.39–42
Lead is insidious and causes subtle and potentially unnoticeable effects in children.43–45 Children also absorb more lead than do adults, and exposure to equivalent levels of lead has disproportionate effects on their developing nervous systems.34,44,46,47 Recognizing that no BLL is safe, in 2012, the Centers for Disease Control and Prevention (CDC) reduced the actionable level to 5 μg/dL, the 97.5th percentile among US children aged 1-5 years (meaning that only 2.5% of US children have a BLL >5 μg/dL).48
In response to research in other countries, Haiti phased out its use of leaded gasoline in 1998.49 However, the effects of lead exposure on Haitian children had not been determined, and it was unknown whether these children had been exposed to lead through other environmental factors, such as soil, paint, or improperly discarded batteries. Accordingly, we measured BLLs in otherwise healthy Haitian children and determined the proportion of children with elevated blood lead levels (EBLLs).
Methods
Setting and Participants
We conducted this cross-sectional study of Haitian infants and young children aged 9 months to 6 years from March 1 through June 30, 2015, in 3 diverse geographical departments of Haiti: an urban area in the Haitian capital (Port-au-Prince) in the Nord-Ouest Department (an administrative region in Haiti), a coastal area in the Artibonite Department, and a mountain area in the Centre Department. The urban area is a densely populated industrialized city that had a devastating earthquake in 2010. The coastal area is less densely populated but is a hub for commercial transport by land and sea. The mountain area is more rural and agrarian than the other 2 areas.
We studied a convenience sample of children who were simultaneously being tested for vitamin D deficiency at churches and represented approximately 0.3%, 0.5%, and 0.6% of children living in the coastal, urban, and mountain areas, respectively. Eligible children were enrolled from 2 churches in each area on consecutive days. We selected churches as recruitment sites because most Haitians are Christian. Selecting churches gave us access to children with varying socioeconomic status and minimized any bias toward sicker children, which may have occurred at clinics or hospitals. We contacted pastors from 6 large churches that did not cater to expatriate (ie, wealthy) clientele before the study and received permission from all churches to conduct testing. The pastors assisted with notifying their congregations of the study. All infants and children aged 9 months to 6 years were eligible for the study. Only 1 child per household could be enrolled in the study. We excluded children who had a chronic medical condition (except malnutrition and sickle-cell disease) and who had lived outside of Haiti for longer than 6 months. We excluded children with chronic medical conditions because their medical management had the potential to introduce confounding factors not typical for groups of healthy children.
We obtained institutional review board approval from Boston Children’s Hospital and the Haitian National Bioethics Committee. Children were voluntarily enrolled after we obtained written informed consent from the children’s parent or guardian, after the study was verbally explained in Haitian Creole. We informed parents of the benefit of knowing their child’s BLL and advised them on how to minimize exposure to lead. If parents or guardians were not literate, we obtained verbal consent in the presence of a witness. Participants received no financial incentives for participating in the study.
Anthropometric Measurements
We obtained anthropometric data from each child, including weight, height for children aged ≥2 years and length for children aged <2 years, and mid-upper-arm circumference. We weighed infants who were unable to stand on the Redmon Precision Digital Baby Scale (W.C. Redmon Company, Peru, Indiana), and we weighed children who could stand on a Detecto 337 Eye Level Physician Scale (Dectecto, Webb City, Missouri). We obtained measurements of length and height using the Seca 210 Mobile Measuring Mat for Babies and Toddlers and the Seca 213 Portable Stadiometer Height Rod for all other children (Seca, Hamburg, Germany). We assessed nutritional status by using z-scores from the World Health Organization Child Growth Standards, and we categorized children as having “normal” nutrition (ie, no malnutrition or stunting) or “poor” nutrition (ie, malnutrition only, stunting only, or malnutrition and stunting).50 The cutoff for malnutrition was a weight ≥2 standard deviations below the mean, and the cutoff for stunting was a length or height for age ≥2 standard deviations below the mean.
Lead Exposure and BLLs
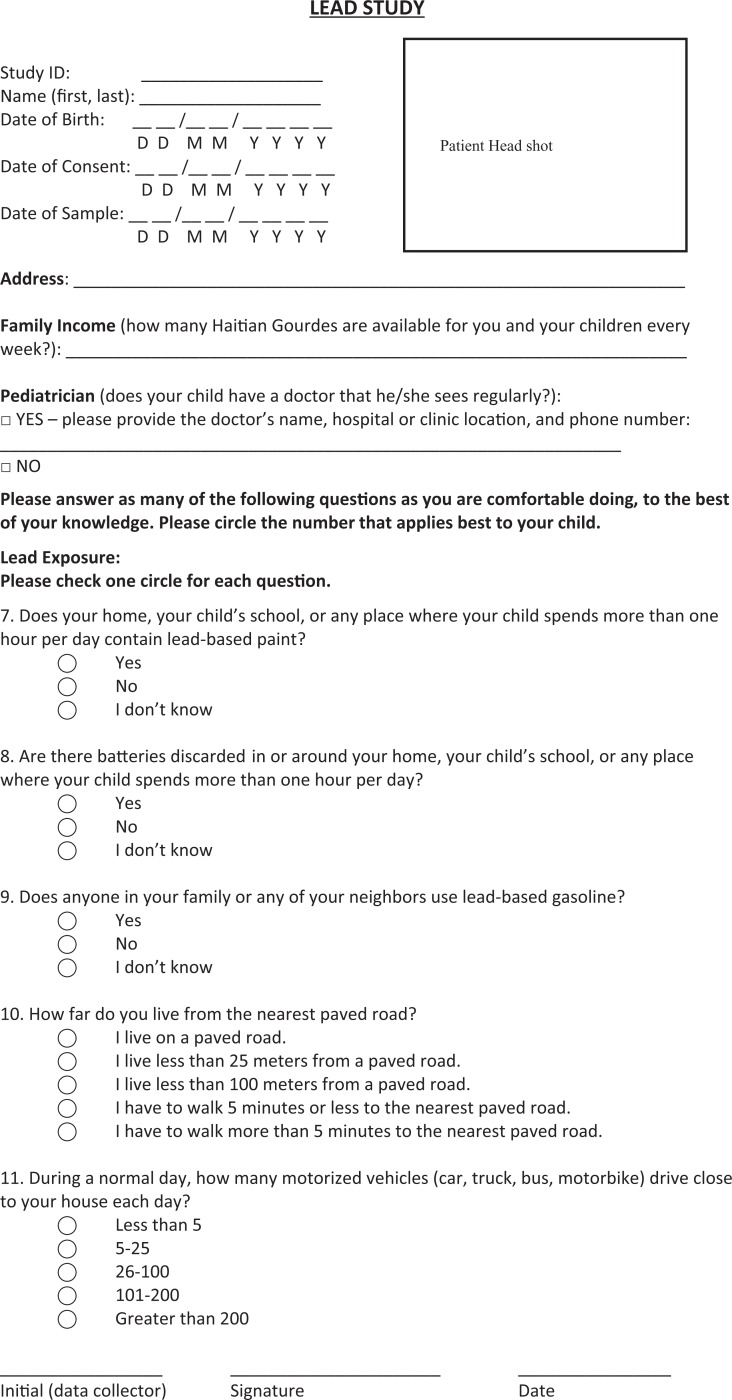
Each child’s parent or guardian answered questions about household income and potential environmental exposure to lead, such as exposure to improperly discarded car batteries or household batteries, the number of vehicles that passed by their home on a daily basis, and exposure to leaded paint and gasoline (Figure). Trained study personnel administered questionnaires verbally in Haitian Creole in an area of the church that was separate from the testing area. The portion of the questionnaire that asked about lead exposures comprised 7 questions and was typically completed in 5 minutes.
Figure.
Questionnaire used to determine lead exposure characteristics of a convenience sample of children aged 9 months to 6 years (n = 273) who were tested for blood lead level at 6 churches in Haiti, March 1 through June 30, 2015.
We sampled capillary blood by standard procedures, and we measured BLLs with the LeadCare II Blood Lead Analyzer (Magellan Diagnostics Inc, North Billerica, MA) point-of-care test machine. A nurse cleaned each participant’s finger with water and then with alcohol. The nurse then collected 50 μL of blood in a heparinized capillary tube using aseptic technique, immediately mixed the blood with reagent, and then tested per the LeadCare II Blood Lead Analyzer User’s Guide and CDC guidelines for collecting and handling blood lead samples.51–53 The reportable range for the LeadCare II Blood Lead Analyzer is 3.3-65.0 μg/dL, and reports are measured in increments of 0.1 μg/dL.52 We recorded BLLs of <3.3 μg/dL as 0 for data analysis. Before analyzing each batch of samples, we calibrated the analyzer as per the manufacturer’s recommendations to ensure precise results.53 We conducted all testing in an environment with consistent temperature, humidity, and sun exposure. We considered BLLs ≥5 μg/dL to be elevated, as per the CDC definition.48
Result Reporting
All parents and guardians received the results of their children’s tests and appropriate education and preventive counseling on the same day of the study visit. All children with BLLs ranging from 10-20 μg/dL received follow-up testing after 3 months. We retested children with BLLs ranging from 21-45 μg/dL 1 week later and completed a thorough evaluation by a physician if the level stayed in this range. Any child with a BLL >45 μg/dL was to receive a complete evaluation and be removed from their home to undergo chelation therapy; however, we identified no children in this range. At the time of repeat testing, we visited the homes of all children with BLLs ≥10 μg/dL and again advised parents on how to prevent lead exposure.
Statistical Methods
Study data were collected and managed using REDCap (Research Electronic Data Capture) electronic data capture tools.54 We analyzed characteristics of the study population as numbers and percentages, except for income and serum lead levels, which we reported as medians and interquartile ranges (IQRs). We stratified characteristics and analyzed them for differences across the 3 geographic areas by using the Pearson χ2 test; we compared median incomes and serum lead levels by using the nonparametric Kruskal-Wallis test.
We determined the prevalence of EBLLs by demographic and potential lead exposure characteristics, and we calculated the prevalence ratios (PRs) of EBLLs by selected risk factors, with a predetermined reference category (in general, the category with the lowest prevalence of EBLLs). We tabulated PRs with 95% confidence intervals (CIs), and we considered P < .05 to be significant.
We also calculated PRs to determine the attributable risk of exposure to improperly discarded batteries in each geographic area because exposure to improperly discarded batteries was so common. We derived PRs to compare the prevalence of EBLLs in children with and without exposure to improperly discarded batteries. We analyzed data by using Stata release 14.55 All tests of significance were 2-tailed.
Results
Baseline Characteristics
Of the 273 children enrolled in the study, 95 were from the coastal area, 78 were from the urban area, and 100 were from the mountain area (Table 1). Age, sex, and income were similar across all 3 areas. Forty-eight (17.6%) children had poor nutrition; children in the mountain area had a significantly higher prevalence of poor nutrition (27.0%) than children in the urban area (14.1%) and coastal area (10.5%; P = .007).
Table 1.
Demographic and lead-exposure characteristics of a convenience sample of children aged 9 months to 6 years (n = 273) tested for blood lead levels, by geographic area, Haiti, 2015a
| Characteristic | Total (N = 273) | Coastal Areab (n = 95) | Urban Areac (n = 78) | Mountain Aread (n = 100) | P Valuee |
|---|---|---|---|---|---|
| Age, y, No. (%) | .39 | ||||
| <2 | 67 (24.5) | 29 (30.5) | 16 (20.5) | 22 (22.0) | |
| 2 | 55 (20.1) | 17 (17.9) | 14 (17.9) | 24 (24.0) | |
| ≥3 | 151 (55.3) | 49 (51.6) | 48 (61.5) | 54 (54.0) | |
| Female, No. (%) | 138 (50.5) | 47 (49.5) | 37 (47.4) | 54 (54.0) | .66 |
| Weekly income, median (IQR), US $ | 1500 (1000-2500) | 1500 (1000-2500) | 1500 (1000-2500) | 1500 (840-2500) | .43f |
| Poor nutrition, No. (%) | 48 (17.6) | 10 (10.5) | 11 (14.1) | 27 (27.0) | .007 |
| Lead exposure, No. (%) | |||||
| Paint | <.001 | ||||
| Present | 31 (11.4) | 4 (4.2) | 15 (19.2) | 12 (12.0) | |
| Absent | 115 (42.1) | 14 (14.7) | 40 (51.3) | 61 (61.0) | |
| Unknown | 127 (46.5) | 77 (81.1) | 23 (29.5) | 27 (27.0) | |
| Improperly discarded batteries (n = 272) | .82 | ||||
| Present | 132 (48.0) | 46 (48.4) | 35 (44.9) | 51 (51.0) | |
| Absent | 126 (46.2) | 44 (46.3) | 40 (51.3) | 42 (42.0) | |
| Unknown | 14 (5.1) | 5 (5.2) | 3 (3.8) | 6 (6.0) | |
| Gasoline (n = 272) | <.001 | ||||
| Present | 77 (28.2) | 41 (43.2) | 15 (19.2) | 21 (21.0) | |
| Absent | 109 (39.9) | 21 (22.1) | 38 (48.7) | 50 (50.0) | |
| Unknown | 86 (31.5) | 33 (34.7) | 25 (32.1) | 28 (28.0) | |
| Daily exposure to vehicles, No. (%) | .001 | ||||
| <5 vehicles | 49 (17.9) | 16 (16.8) | 7 (9.0) | 26 (26.0) | |
| 5-25 vehicles | 72 (26.4) | 29 (30.5) | 22 (28.2) | 21 (21.0) | |
| 26-100 vehicles | 66 (24.2) | 28 (29.5) | 11 (14.1) | 27 (27.0) | |
| 101-200 vehicles | 22 (8.1) | 6 (6.3) | 7 (9.0) | 9 (9.0) | |
| >200 vehicles | 64 (23.4) | 16 (16.8) | 31 (39.7) | 17 (17.0) | |
| Serum BLL, median (IQR)g | 5.8 (4.5-7.7) | 5.2 (4.2-6.8) | 5.1 (4.2-6.9) | 6.9 (5.5-8.4) | .001f |
| BLL 5 to <10 μg/dL, No. (%) | 180 (65.9) | 56 (58.9) | 42 (53.8) | 82 (82.0) | <.001 |
| BLL 10 to <20 μg/dL, No. (%) | 28 (10.3) | 7 (7.4) | 7 (9.0) | 14 (14.0) | .31 |
| BLL ≥20 μg/dL, No. (%) | 3 (1.1) | 2 (2.1) | 1 (1.3) | 0 | .39h |
Abbreviations: BLL, blood lead level; IQR, interquartile range.
a Data collected at 6 churches in Haiti from March 1 through June 30, 2015.
b Artibonite Department.
c Nord-Ouest Department.
d Centre Department.
e All P values were calculated using the Pearson χ2 test unless otherwise indicated; P < .05 was considered significant.
f Using the Kruskal-Wallis test; P < .05 was considered significant.
g BLLs ≥5 μg/dL were considered to be elevated.48
h Using the Fisher exact text; P < .05 was considered significant.
Lead Exposure and BLLs
BLLs ranged from <3.3-33.2 μg/dL, with a median (IQR) of 5.8 (4.5-7.7) μg/dL. Median (IQR) levels were significantly higher in the mountain area (6.9 [5.5-8.4] μg/dL) than in the urban area (5.1 [4.2-6.9] μg/dL) and coastal area (5.2 [4.2-6.8] μg/dL; P = .04). Lead exposure varied by geographic area but not consistently so; children had higher exposures to leaded paint in the urban area, higher exposures to leaded gasoline in the coastal area, and no differences in exposure to improperly discarded batteries across the 3 areas. Children in the urban area were exposed to a greater volume of vehicle traffic than children in the mountain or coastal area.
We found EBLLs >5 μg/dL in 180 (65.9%) children and BLLs <3.3 μg/dL in 13 (4.8%) children. The percentage of children with EBLLs was significantly higher in the mountain area (82.0%; P < .001) than in the urban area (53.8%) and coastal area (58.9%; P < .001; Table 2). Twenty-eight (10.3%) children had EBLLs ≥10 μg/dL, and 3 (1.1%) children had EBBLs ≥20 μg/dL, but the differences were not significant across the 3 areas.
Table 2.
Prevalence of elevated blood lead levels (≥5 μg/dL) among a convenience sample of children aged 9 months to 6 years (n = 273), by selected risk factors, Haiti, 2015a
| Risk Factor | Total No. of Children (N = 273) | Children With Elevated Blood Lead Levels (≥5 μg/dL), No. (%) (n = 180) | Prevalence Ratio (95% CI) | P Valueb |
|---|---|---|---|---|
| Age, y | ||||
| <2 | 67 | 44 (65.7) | 1.00 (0.81-1.23) | .99 |
| 2 | 55 | 37 (67.3) | 1.03 (0.83-1.28) | .82 |
| ≥3 | 151 | 99 (65.6) | 1.00 (Reference) | |
| Sex | ||||
| Female | 138 | 91 (65.9) | 1.00 (0.84-1.19) | .99 |
| Male | 135 | 89 (65.9) | 1.00 (Reference) | |
| Area | ||||
| Mountainc | 100 | 82 (82.0) | 1.52 (1.22-1.91) | <.001 |
| Coastald | 95 | 56 (58.9) | 1.09 (0.84-1.43) | .50 |
| Urbane | 78 | 42 (53.8) | 1.00 (Reference) | |
| Nutritional status | ||||
| Poor nutrition | 48 | 34 (70.8) | 1.09 (0.89-1.34) | .43 |
| Normal | 225 | 146 (64.9) | 1.00 (Reference) | |
| Exposure to leaded paintf | ||||
| Yes | 31 | 15 (48.4) | 0.73 (0.50-1.08) | .07 |
| No | 115 | 76 (66.1) | 1.00 (Reference) | |
| Exposure to improperly discarded batteriesf | ||||
| Yes | 132 | 97 (73.5) | 1.29 (1.07-1.54) | .006 |
| No | 126 | 72 (57.1) | 1.00 (Reference) | |
| Exposure to leaded gasolinef | ||||
| Yes | 77 | 55 (71.4) | 1.14 (0.93-1.40) | .20 |
| No | 109 | 68 (62.4) | 1.00 (Reference) | |
| No. of motorized vehicles per day | ||||
| >200 | 64 | 45 (70.3) | 1.11 (0.85-1.45) | .43 |
| 101-200 | 22 | 12 (54.5) | 0.86 (0.56-1.33) | .49 |
| 26-100 | 66 | 48 (72.7) | 1.15 (0.89-1.49) | .28 |
| 5-25 | 72 | 44 (61.1) | 0.97 (0.73-1.28) | .81 |
| <5 | 49 | 31 (63.3) | 1.00 (Reference) |
a Data collected at 6 churches in Haiti from March 1 through June 30, 2015.
b Calculated using the Pearson χ2 test, with P < .05 considered significant.
c Artibonite Department.
d Nord-Ouest Department.
e Centre Department.
f Parents were asked if there were improperly discarded batteries at home, at school, or in play areas. The number does not include “unknown” responses: paint (n = 127), battery (n = 14), gasoline (n = 86), and item not checked on questionnaire (n = 2).
Children exposed to improperly discarded batteries, compared with children not exposed, had a 29% higher risk of EBLLs (73.5% vs 57.1%; PR = 1.29; P = .006).
We also calculated PRs for EBLLs between children exposed and unexposed to batteries in each area separately. By geographic area, only children exposed to improperly discarded batteries in the mountain area had a significantly higher prevalence of EBLLs (P = .004; Table 3).
Table 3.
Exposure to lead from improperly discarded batteriesa among a convenience sample of children aged 9 months to 6 years (n = 258), by geographic area, Haiti, 2015b
| Location | Total No. of Children | Children With Elevated Blood Lead Levels, No. (%) | Attributable Risk, %c | Prevalence Ratio (95% CI) | P Valued |
|---|---|---|---|---|---|
| Mountain areae | |||||
| Exposed | 51 | 47 (92.2) | 23 | 1.34 (1.07-1.66) | .004 |
| Unexposed | 42 | 29 (69.0) | |||
| Urban areaf | |||||
| Exposed | 35 | 20 (57.1) | 4 | 1.09 (0.72-1.64) | .69 |
| Unexposed | 40 | 21 (52.5) | |||
| Coastal areag | |||||
| Exposed | 46 | 30 (65.2) | 15 | 1.30 (0.91-1.88) | .14 |
| Unexposed | 44 | 22 (50.0) | |||
a Parents were asked if there were improperly discarded batteries at home, at school, or in play areas.
b Data collected at 6 churches in Haiti from March 1 through June 30, 2015.
c The risk difference between exposed and unexposed children.
d Calculated using the Pearson χ2 test, with P < .05 considered significant.
e Artibonite Department.
f Nord-Ouest Department.
g Centre Department.
Parents and guardians had limited knowledge of their children’s exposure to leaded paint (n = 127, 46.5%) and leaded gasoline (n = 86, 31.5%), but only a few (n = 14, 5.1%) did not know whether their child had been exposed to improperly discarded batteries.
Discussion
More than half of the Haitian children we studied had an EBLL >5 μg/dL, and the highest prevalence of EBLLs was among children in the mountain area. Children exposed to improperly discarded batteries, compared with children not exposed, were also significantly more likely to have EBLLs. Although we primarily analyzed and reported our data using nonparametric measures, the median BLL we observed (5.8 μg/dL) was similar to the geometric mean of these BLLs (5.5 μg/dL) when we replaced those levels that were undetectable (and counted as 0 μg/dL when calculating the median, n = 13) with a value of 0.5 μg/dL to calculate a geometric mean. By comparison, recent studies reported geometric mean BLLs of 2.8 μg/dL among children aged 2-8 years in Jamaica,56 1.57 μg/dL among children aged 0-6 years in Puerto Rico,57 1.96 μg/dL among children aged 0-6 years in Shanghai, China,58 and 0.76 μg/dL among children aged 1-5 years in the United States.59 In contrast, a study in Jakarta, Indonesia, reported a geometric mean BLL of 8.6 μg/dL among children aged 6-12 years.60
Despite identifying no children as having a life-threatening BLL requiring chelation, we found a high prevalence of EBLLs in Haiti. The CDC’s actionable BLL, which encompasses 2.5% of US children, could potentially include 66% of all Haitian children and more than 80% of children in some areas of Haiti. These percentages, which are 10 times higher than in the 2014 outbreak of EBLLs in Flint, Michigan, far exceed acceptable childhood population BLLs and are a major public health concern.12
Among the risk factors studied, exposure to improperly discarded car and household batteries was a significant and modifiable risk factor for EBLLs in Haitian children, a finding consistent with the findings of studies in other countries.10,61,62 After batteries expire in Haiti, they may be stored in the yard, burned with other garbage, or thrown in a local natural water source. With nearly half the children in our study reporting exposure to improperly discarded batteries near their home or school, providing ways to safely discard batteries could be one way to decrease EBLLs in Haiti.
We did not find that exposure to leaded paint predicted EBLLs in children, despite ample literature documenting this association.63,64 However, nearly half of the parents and guardians we interviewed were unaware of their child’s exposure to lead-based paint, and, thus, we could not draw a definitive conclusion about this important potential risk factor. Future studies should investigate the lead content of the paint commonly used in residences in Haiti, and appropriate parental and community education campaigns should ensue.
Potential sources of lead exposure in Haiti are not well studied. A small 2013 study found no detectable levels of lead in the soil of a commune in Ouest (from which our urban sample was drawn).65 However, the sample was obtained from an area with little human activity and, thus, may not be representative of the rest of the country. Another study in the urban area found that groundwater had lead levels in excess of the US Environmental Protection Agency’s actionable level.66,67 Interventions to improve access to potable water after the 2010 cholera epidemic may have decreased the population’s exposure to contaminated drinking water from rivers or wells, but water in certain areas could potentially remain a source of lead exposure. Finally, manioc, a root vegetable that is a staple food in Haiti, could be a source of lead and warrants investigation. Consumption of manioc has been implicated in EBLLs in pregnant women in Guyana, possibly from manioc being grown in contaminated soil or from lead contamination that occurs during cooking of this vegetable on lead-containing hotplates.68
The strongest independent predictor of EBLLs in our study was residing in the mountain area of the Centre Department rather than the urban or coastal areas. This relationship cannot be explained by exposure to improperly discarded batteries, because this exposure did not differ across areas; however, exposure to lead from improperly discarded batteries accounted for 23% of the attributable risk (ie, risk difference between exposed and unexposed children) of battery exposure in the mountain area, 4% of the attributable risk of battery exposure in the urban area, and 15% of the attributable risk of battery exposure in the coastal area. This finding could be explained by the likelihood that children in the mountain area were less likely than children living in urban and coastal areas to have high levels of exposure to vehicles, thus distributing the risk of having an EBLL more evenly. However, this explanation does not clarify why children living in the mountain area were independently at higher risk of having EBLLs than children living in other areas, even when we adjusted the data for other exposures.
Interestingly, the percentage of children with EBLLs in the urban area was not substantially higher than the percentage of children with EBLLs in the mountain and coastal areas, although the urban area we studied was closer than the other 2 areas to the epicenter of the 2010 earthquake, which caused substantial dust accumulation in the city. In addition to a country-wide investigation into environmental contamination of soil and water, other potential exposures, such as local staple foods and their processing methods and locally produced healing remedies, medicines, and paint (which may be produced in lead-based receptacles), should be evaluated to better understand the geographic differences in the prevalence of EBLLs.
Children of low socioeconomic status are at increased risk of having EBLLs in several countries, including the United States, South Africa, China, and Mexico69–72; however, we did not find this association in Haiti. We evaluated socioeconomic status by reported household income, but we did not relate this amount to the number of people living in the home, nor did we investigate other markers of socioeconomic status. Although we may have underestimated differences in socioeconomic status among children, the high rates of poverty throughout the population would make this potential relationship difficult to appreciate.
The relationship between poor nutrition and BLLs in children is not well understood; several studies reported that EBLLs are associated with both underweight and obese children.73–76 In our study, although a higher percentage of children in the mountain area compared with the coastal and urban areas had both poor nutrition and EBLLs, poor nutrition did not predict EBLLs. However, an association between poor nutrition and high BLLs may have been masked, given the overall high rates of malnutrition and stunting we observed.
Limitations
This study had several limitations. Although we found many children with EBLLs in this initial cross-sectional study, our investigation into potential sources of lead exposure in the environment was exploratory. One major limitation was the reliance on parental reporting of environmental lead hazards, which may have introduced recall, social desirability, or acquiescence bias. Our questionnaire also asked only about the presence or absence of certain exposures. Although we were able to identify improperly discarded batteries as one source of lead exposure, additional questionnaire details such as information on manioc consumption, lead-containing paint or pottery, household dust, plaster, and dirt may have allowed for identification of additional potential sources of lead exposure in the child’s home environment. Likewise, we were unable to take into account exposures outside of the home, such as in schools. As such, we likely underestimated the contributing sources for lead exposure. Further studies that measure BLLs of children from all geographic areas of Haiti and that cover more risk factors than we covered in the home evaluation would provide a more comprehensive description of the extent of EBLLs in Haiti.
Our study may also have been biased by our use of a convenience sample. Although we chose to recruit children from churches within each area because of the high rate of Christianity across all socioeconomic levels in Haiti, we did not include in our sample children whose parents were not Christian or who were Christian but did not attend church. As such, we could not determine whether exposures among these excluded children were different from exposures among the children in our sample.
Conclusions
More than half of the Haitian children in our study had EBLLs, especially children in the mountain area. Exposure to improperly discarded batteries was a significant, modifiable risk factor. Comprehensive investigations into other environmental sources of lead exposure, particularly emphasizing mountain areas, will be important to mitigate this preventable epidemic among Haitian children. Public health interventions are warranted to protect children in Haiti against lead poisoning. These data will be shared with the Ministry of Population and Public Health, and we will advocate for a sustained public health screening program for Haitian children.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: All phases of this study were supported by the Kay Mackenson Center, which receives support from the Goldsmith Foundation. In-kind donation provided by Magellan Diagnostics Inc, Billerica, Massachusetts (LeadCare2® equipment and supplies).
References
- 1. Belin B, Yaçin T, Suner F, Bozkurtoğlu E, Gelir A, Güven H. Earthquake-related chemical and radioactivity changes of thermal water in Kuzuluk-Adapazan, Turkey. J Environ Radioact. 2002;63(3):239–249. [DOI] [PubMed] [Google Scholar]
- 2. Rodriguez-Espinosa PF, Jonathan MP, Morales-García SS, et al. Metal enrichment of soils following the April 2012-2013 eruptive activity of the Popocatépetl volcano, Puebla, Mexico. Environ Monit Assess. 2015;187(11):717. [DOI] [PubMed] [Google Scholar]
- 3. World Health Organization, International Agency for Research on Cancer. Inorganic and organic lead compounds: summary of data reported and evaluation. Vol 87 2006. http://www.inchem.org/documents/iarc/vol87/volume87.pdf. Accessed August 29, 2016. [Google Scholar]
- 4. Lo YC, Dooyema CA, Neri A, et al. Childhood lead poisoning associated with gold ore processing: a village-level investigation—Zamfara State, Nigeria, October–November 2010. Environ Health Perspect. 2012;120(10):1450–1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nasidi A, Karwowski M, Woolf A, et al. Infant lead poisoning associated with use of tiro, an eye cosmetic from Nigeria—Boston, Massachusetts, 2011. MMRW Morb Mortal Wkly Rep. 2012;61(30):574–576. [PubMed] [Google Scholar]
- 6. US Environmental Protection Agency. Latest Findings on National Air Quality: 2002 Status and Trends. Research Triangle Park, NC: US Environmental Protection Agency, Office of Air Quality Planning and Standards, Emissions, Monitoring, and Analysis Division; 2003. [Google Scholar]
- 7. VanArsdale JL, Horowitz BZ, Merritt TA, et al. Brief report: lead poisoning from ingestion of a toy necklace—Oregon, 2003. MMWR Morb Mortal Wkly Rep. 2004;53(23):509–511. [PubMed] [Google Scholar]
- 8. Lin Z, Comet B, Qvarfort U, Herbert R. The chemical and mineralogical behaviour of Pb in shooting range soils from central Sweden. Environ Pollut. 1995;89(3):303–309. [DOI] [PubMed] [Google Scholar]
- 9. Bourne IB. Epidemic lead poisoning in children from storage battery casings. J Natl Med Assoc. 1944;36(6):187–193. [PMC free article] [PubMed] [Google Scholar]
- 10. Matte TD, Figueroa JP, Ostrowski S, et al. Lead poisoning among household members exposed to lead-acid battery repair shops in Kingston, Jamaica. Int J Epidemiol. 1989;18(4):874–881. [DOI] [PubMed] [Google Scholar]
- 11. McCord CP. Lead and lead poisoning in early America: the lead pipe period. Ind Med Surg. 1954;23(1):27–31. [PubMed] [Google Scholar]
- 12. Hanna-Attisha M, LaChance J, Sadler RC, Champney Schnepp A. Elevated blood lead levels in children associated with the Flint drinking water crisis: a spatial analysis of risk and public health response. Am J Public Health. 2016;106(2):283–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bartleman EL, Dukes C. Chronic lead poisoning due to grease paint. Br Med J. 1936;1(3923):528–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Millichap JG, Llewellin KR, Roxburgh RC. Lead paint: a hazard to children. Lancet. 1952;2(6730):360–362. [DOI] [PubMed] [Google Scholar]
- 15. Boucher O, Jacobson SW, Plusquellec P, et al. Prenatal methylmercury, postnatal lead exposure, and evidence of attention deficit/hyperactivity disorder among Inuit children in Arctic Quebec. Environ Health Perspect. 2012;120(10):1456–1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Abdel Rasoul GM, Al-Batanony MA, Mahrous OA, Abo-Salem ME, Gabr HM. Environmental lead exposure among primary school children in Shebin El-Kom District, Menoufiya Governorate, Egypt. Int J Occup Environ Med. 2012;3(4):186–194. [PubMed] [Google Scholar]
- 17. Garçon G, Leleu B, Zerimech F, et al. Biologic markers of oxidative stress and nephrotoxicity as studied in biomonitoring of adverse effects of occupational exposure to lead and cadmium. J Occup Environ Med. 2004;46(11):1180–1186. [DOI] [PubMed] [Google Scholar]
- 18. Gonick HC. Nephrotoxicity of cadmium & lead. Indian J Med Res. 2008;128(4):335–352. [PubMed] [Google Scholar]
- 19. Mortada WI, Sobh MA, El-Defrawy MM, Farahat SE. Study of lead exposure from automobile exhaust as a risk for nephrotoxicity among traffic policemen. Am J Nephrol. 2001;21(4):274–279. [DOI] [PubMed] [Google Scholar]
- 20. Sabolić I. Common mechanisms in nephropathy induced by toxic metals. Nephron Physiol. 2006;104(3):107–114. [DOI] [PubMed] [Google Scholar]
- 21. Schwartz J, Landrigan PJ, Baker EL, Jr, Orenstein WA, Von Lindern IH. Lead-induced anemia: dose-response relationships and evidence for a threshold. Am J Public Health. 1990;80(2):165–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Selevan SG, Rice DC, Hogan KA, Euling SY, Pfahles-Hutchens A, Bethel J. Blood lead concentration and delayed puberty in girls. N Engl J Med. 2003;348(16):1527–1536. [DOI] [PubMed] [Google Scholar]
- 23. Wu T, Buck GM, Mendola P. Blood lead levels and sexual maturation in U.S. girls: the Third National Health and Nutrition Examination Survey, 1988-1994. Environ Health Perspect. 2003;111(5):737–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cheng Y, Schwartz J, Sparrow D, Aro A, Weiss ST, Hu H. Bone lead and blood lead levels in relation to baseline blood pressure and the prospective development of hypertension: the Normative Aging Study. Am J Epidemiol. 2001;153(2):164–171. [DOI] [PubMed] [Google Scholar]
- 25. Navas-Acien A, Guallar E, Silbergeld EK, Rothenberg SJ. Lead exposure and cardiovascular disease—a systematic review. Environ Health Perspect. 2007;115(3):472–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Government of British Colombia. Proposed toxicological reference values for lead (Pb). 2012. https://www2.gov.bc.ca/assets/gov/environment/air-land-water/site-remediation/docs/policies-and-standards/toxicological_reference_values_for_lead_tg7.pdf. Accessed August 28, 2016.
- 27. Lutz PM, Wilson TJ, Ireland J, et al. Elevated immunoglobulin E (IgE) levels in children with exposure to environmental lead. Toxicology. 1999;134(1):63–78. [DOI] [PubMed] [Google Scholar]
- 28. Karmaus W, Brooks KR, Nebe T, Witten J, Obi-Osius N, Kruse H. Immune function biomarkers in children exposed to lead and organochlorine compounds: a cross-sectional study. Environ Health. 2005;4(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kim S, Arora M, Fernandez C, Landero J, Caruso J, Chen A. Lead, mercury, and cadmium exposure and attention deficit hyperactivity disorder in children. Environ Res. 2013;126:105–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chiodo LM, Jacobson SW, Jacobson JL. Neurodevelopmental effects of postnatal lead exposure at very low levels. Neurotoxicol Teratol. 2004;26(3):359–371. [DOI] [PubMed] [Google Scholar]
- 31. Braun JM, Froehlich TE, Daniels JL, et al. Association of environmental toxicants and conduct disorder in U.S. children: NHANES 2001-2004. Environ Health Perspect. 2008;116(7):956–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Canfield RL, Henderson CR, Jr, Cory-Slechta DA, Cox C, Jusko TA, Lanphear BP. Intellectual impairment in children with blood lead concentrations below 10 microg per deciliter. N Engl J Med. 2003;348(16):1517–1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jusko TA, Henderson CR, Lanphear BP, Cory-Slechta DA, Parsons PJ, Canfield RL. Blood lead concentrations < 10 microg/dL and child intelligence at 6 years of age. Environ Health Perspect. 2008;116(2):243–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bellinger DC, Stiles KM, Needleman HL. Low-level lead exposure, intelligence and academic achievement: a long-term follow-up study. Pediatrics. 1992;90(6):855–861. [PubMed] [Google Scholar]
- 35. Eden AN. Intellectual impairment and blood lead levels. N Engl J Med. 2003;349(5):500–502. [PubMed] [Google Scholar]
- 36. Caravanos J, Chatham-Stephens K, Ericson B, Landrigan PJ, Fuller R. The burden of disease from pediatric lead exposure at hazardous waste sites in 7 Asian countries. Environ Res. 2013;120:119–125. [DOI] [PubMed] [Google Scholar]
- 37. Surkan PJ, Zhang A, Trachtenberg F, Daniel DB, McKinlay S, Bellinger DC. Neuropsychological function in children with blood lead levels <10 microg/dL. Neurotoxicology. 2007;28(6):1170–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Despres C, Beuter A, Richer F, et al. Neuromotor functions in Inuit preschool children exposed to Pb, PCBs, and Hg. Neurotoxicol Teratol. 2005;27(2):245–257. [DOI] [PubMed] [Google Scholar]
- 39. Attina TM, Trasande L. Economic costs of childhood lead exposure in low- and middle-income countries. Environ Health Perspect. 2013;121(9):1097–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gould E. Childhood lead poisoning: conservative estimates of the social and economic benefits of lead hazard control. Environ Health Perspect. 2009;117(7):1162–1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Grosse SD, Matte TD, Schwartz J, Jackson RJ. Economic gains resulting from the reduction in children’s exposure to lead in the United States. Environ Health Perspect. 2002;110(6):563–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Schwartz J. Societal benefits of reducing lead exposure. Environ Res. 1994;66(1):105–124. [DOI] [PubMed] [Google Scholar]
- 43. Etzel RA, Balk SJ, eds. Pediatric Environmental Health. 3rd ed Elk Grove Village, IL: American Academy of Pediatrics Council on Environmental Health; 2011. [Google Scholar]
- 44. Lanphear BP. Childhood lead poisoning prevention [published correction appears in JAMA. 2005;294(7):794]. JAMA. 2005;293(18):2274–2276. [DOI] [PubMed] [Google Scholar]
- 45. Mahaffey KR. Nutrition and lead: strategies for public health. Environ Health Perspect. 1995;103(suppl 6):191–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Dietert RR, Piepenbrink MS. Perinatal immunotoxicity: why adult exposure assessment fails to predict risk. Environ Health Perspect. 2006;114(4):477–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Needleman HL, Schell A, Bellinger D, Leviton A, Allred EN. The long-term effects of exposure to low doses of lead in childhood. An 11-year follow-up report. N Engl J Med. 1990;322(2):83–88. [DOI] [PubMed] [Google Scholar]
- 48. Advisory Committee on Childhood Lead Poisoning Prevention, Centers for Disease Control and Prevention Low Level Lead Exposure Harms Children: A Renewed Call for Primary Prevention. Atlanta, GA: Centers for Disease Control and Prevention; 2012. http://www.cdc.gov/nceh/lead/ACCLPP/Final_Document_030712.pdf. Accessed April 6, 2016. [Google Scholar]
- 49. US Department of State. Haiti: international religious freedom report 2003. https://www.state.gov/j/drl/rls/irf/2003/24496.htm. Accessed April 8, 2016.
- 50. World Health Organization. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development. Geneva, Switzerland: World Health Organization; 2006. http://www.who.int/entity/childgrowth/standards/Technical_report.pdf?ua=1. Accessed August 28, 2016. [Google Scholar]
- 51. Magellan Diagnostics. LeadCare II Blood Lead Analyzer user’s guide. http://www.leadcare2.com/getmedia/73ac501b-35e3-4d74-b6a9-9e7fc51adef0/70-6551_Rev_07_User-s_Guide,_LeadCare_II_(PRINT)-1.pdf.aspx. Published 2015. Accessed September 11, 2018.
- 52. Advisory Committee on Childhood Lead Poisoning Prevention, Centers for Disease Control and Prevention. Guidelines for measuring lead in blood using point of care instruments. https://www.cdc.gov/nceh/lead/acclpp/20131024_pocguidelines_final.pdf. Published 2013. Accessed April 8, 2016.
- 53. Magellan Diagnostics. LeadCare II Blood Lead Analyzer package insert. 2016. http://www.leadcare2.com/getmedia/dba92d69-a213-45ed-9699-771f899c5920/70-6869-Package-Insert,-LeadCare-II-v1-05-Rev-03.pdf.aspx. Accessed September 21, 2018.
- 54. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. StataCorp. Stata Release 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 56. Rahbar MH, Samms-Vaughan M, Dickerson AS, et al. Blood lead concentrations in Jamaican children with and without autism spectrum disorder. Int J Environ Res Public Health. 2015;12(1):83–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Dignam T, Rivera Garcia B, De León M, et al. Prevalence of elevated blood lead levels and risk factors among residents younger than 6 years, Puerto Rico—2010. J Public Health Manag Pract. 2016;22(1):E22–E35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Cao J, Li M, Wang Y, Yu G, Yan C. Environmental lead exposure among preschool children in Shanghai, China: blood lead levels and risk factors. PLoS One. 2014;9(12):e113297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Caldwell KL, Cheng PY, Jarrett JM, et al. Measurement challenges at low blood lead levels. Pediatrics. 2017;140(2):e20170272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Albalak R, Noonan G, Buchanan S, et al. Blood lead levels and risk factors for lead poisoning among children in Jakarta, Indonesia. Sci Total Environ. 2003;301(1-3):75–85. [DOI] [PubMed] [Google Scholar]
- 61. Haefliger P, Mathieu-Nolf M, Lociciro S, et al. Mass lead intoxication from informal used lead-acid battery recycling in Dakar, Senegal. Environ Health Perspect. 2009;117(10):1535–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kaul B, Sandhu RS, Depratt C, Reyes F. Follow-up screening of lead-poisoned children near an auto battery recycling plant, Haina, Dominican Republic. Environ Health Perspect. 1999;107(11):917–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Kuruvilla A, Pillay VV, Venkatesh T, et al. Portable lead analyzer to locate source of lead. Indian J Pediatr. 2004;71(6):495–499. [DOI] [PubMed] [Google Scholar]
- 64. World Health Organization, United Nations Environment Programme. Background information in relation to the emerging policy issue of lead in paint. https://digitallibrary.un.org/record/736352/files/SAICM_ICCM.2_INF_38-EN.pdf. Published 2009. Accessed September 11, 2018.
- 65. Fifi U, Winiarski T, Emmanuel E. Assessing the mobility of lead, copper and cadmium in a calcareous soil of Port-au-Prince, Haiti. Int J Environ Res Public Health. 2013;10(11):5830–5843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Emmanuel E, Pierre MG, Perrodin Y. Groundwater contamination by microbiological and chemical substances released from hospital wastewater: health risk assessment for drinking water consumers. Environ Int. 2009;35(4):718–726. [DOI] [PubMed] [Google Scholar]
- 67. Emmanuel E, Perrodin Y, Fanfan PN, Vermande P. Impacts of hospital wastewater on groundwater quality in Port-au-Prince and human health risk assessment for drinking water consumers. Presented at: Aquatech Amsterdam; November 1-4, 2011; Amsterdam.
- 68. Rimbaud D, Restrepo M, Louison A, et al. Blood lead levels and risk factors for lead exposure among pregnant women in western French Guiana: the role of manioc consumption. J Toxicol Environ Health A. 2017;80(6):382–393. [DOI] [PubMed] [Google Scholar]
- 69. World Health Organization. Exposure to lead: a major public health concern. http://www.who.int/ipcs/features/lead.pdf?ua=1. Published 2010. Accessed April 7, 2016.
- 70. McClure LF, Niles JK, Kaufman HW. Blood lead levels in young children: US, 2009-2015. J Pediatr. 2016;175:173–181. [DOI] [PubMed] [Google Scholar]
- 71. Naicker N, Mathee A, Barnes B. A follow-up cross-sectional study of environmental lead exposure in early childhood in urban South Africa. S Afr Med J. 2013;103(12):935–938. [DOI] [PubMed] [Google Scholar]
- 72. Rothenberg SJ, Schnaas-Arrieta L, Pérez-Guerrero IA, Hernández-Cervantes R, Martínez-Medina S, Perroni-Hernández E. Factors related to the blood lead level in children 6 to 30 months old in the Prospective Lead Study in Mexico City [in Spanish]. Salud Pública Méx. 1993;35(6):592–598. [PubMed] [Google Scholar]
- 73. Wang N, Chen C, Nie X, et al. Blood lead level and its association with body mass index and obesity in China—results from SPECT-China study. Sci Rep. 2015;5:18299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Kim R, Hu H, Rotnitzky A, Bellinger D, Needleman H. A longitudinal study of chronic lead exposure and physical growth in Boston children. Environ Health Perspect. 1995;103(10):952–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Scinicariello F, Buser MC, Mevissen M, Portier CJ. Blood lead level association with lower body weight in NHANES 1999-2006. Toxicol Appl Pharmacol. 2013;273(3):516–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Bithoney WG. Elevated lead levels in children with nonorganic failure to thrive. Pediatrics. 1986;78(5):891–895. [PubMed] [Google Scholar]