Abstract
Background
Adult obesity is globally recognized as a public health concern. As adults spend most of their weekdays at work, worksite wellness programs may include topics of nutrition education and physical activity to improve an employee's body composition. However, results are inconsistent with the impact they have on employees' body composition.
Objective
The purpose of this systematic review was to evaluate worksite wellness nutrition and physical activity programs and their subsequent impact on participants' body composition.
Methods
Extraction of articles was completed through 4 databases: PubMed, CINAHL, SCOPUS, and PsycINFO using keywords such as “nutrition and physical activity interventions/programs” and “weight.” A 9-point inclusion criterion was established. Evaluation of the articles was assessed using the Academy of Nutrition and Dietetics Evidence-Based Manual.
Results
A total of 962 articles were identified. Twenty-three met the inclusion criterion. Seventeen studies resulted in a change in body composition (e.g., decreased BMI (kg/m2), waist circumference, and body fat percentage), and six studies did not show any changes. Programs that had professionals frequently interact with participants, regardless if the interactions were done daily, weekly, or monthly, led to a change in body composition. Additionally, programs that incorporated a motivation theory and provided content relevant to participants' needs resulted in a change in body composition.
Conclusion
Evidence supports that future worksite wellness programs that are designed using a motivational theory and content that is created relevant to participants' needs and that has frequent interactions with participants may result in a change in body composition.
1. Introduction
The global rise in obesity has deemed it a public health crisis. In 2016, the World Health Organization reported that globally over 1.9 billion adults, aged 18 and older, (39% of men and 40% of women), were considered overweight (BMI 25–29.9 kg/m2). Of those, 650 million (11% of men and 15% of women) were considered obese (BMI ≥ 30 kg/m2) [1]. Adult obesity contributes to 7 out of 10 deaths per year [2–4] and leads to several chronic health conditions such as cardiovascular disease (hypertension, stroke, and atherosclerosis), certain types of cancers (breast, colon, and prostate), and type II diabetes [2–9].
Adult obesity rates continue to rise for a number of reasons such as adults consuming less than the required amounts of whole grains, fresh fruits, and vegetables while increasing their consumption of high saturated fat and sodium foods [10–12] and reducing their physical activity [2, 4, 13–15]. Considering that employees spend an average of 8.0 hours working at their jobs compared to an average of 3.1 hours working at home [16], a worksite wellness program may be an ideal strategy to combat this rise in obesity.
Since the 1630s, organizations have implemented occupational programs for a variety of reasons such as for the prevention of injuries or to enhance employee performance [17–19]. In the mid-1970s, worksite wellness programs emerged to focus on the health of the employees [18, 19]. These worksite wellness programs are critical to have in place as employers are combating the number of sick days and productivity lost to employees who have chronic conditions such as obesity [14, 15, 18]. Healthcare costs associated with obesity are estimated to be about 190.2 billion dollars per year [20] with employers spending about 4.3 billion dollars per year due to employee-related absenteeism [20, 21] and another 506 million dollars per year due to lost productivity [22]. A 2013 report indicated that more than 50% of organizations are offering worksite wellness programs to enhance employees' health. These programs may include nutrition education, fitness, and weight management practices [23].
For worksite wellness programs to be effective in reducing the prevalence of obesity, physical activity and nutrition education should be incorporated within these programs [15, 24, 25]. Evidence has shown that regular physical activity (150 minutes per week) and consuming a nutritious diet (e.g., whole grains, fresh fruits, and vegetables) aid in weight reduction [26–29]. Therefore, common components included within these programs are health/risk assessments, exercising, and educational sessions geared toward nutrition and overall wellness [30–34]. Results from studies demonstrated that participants achieved program goals such as changing their body composition (e.g., decreasing body fat percentage and body mass index (BMI kg/m2)) [35–37]. Beyond the incorporation of physical activity and nutrition education, other factors included in the design of these programs that led to a change in body composition were the inclusion of a motivational theory, length of the program, and intensity of interaction. For instance, programs that were 12 months or longer resulted in decreased body weight. This may be because a change in behavior takes at least six months for it to be sustained [38]. An individual is less likely to carry on with a behavior change if they do not have ample opportunities within an extended period of time to restructure choices in regard to physical activity and eating nutritiously throughout daily living [27, 29, 39]. Plus, if one is motivated either internally or externally, this could help to integrate the program goals into everyday practice [39–42] to potentially change his or her body composition. However, results from worksite wellness programs that incorporated these components were inconsistent with changes in an individual's body composition [32, 43, 44]. Therefore, the purpose of this systematic review was to evaluate worksite wellness nutrition and physical activity programs and their subsequent impact on participants' body composition.
2. Materials and Methods
2.1. Search Strategy
This review was conducted by two independent researchers from Eastern Illinois University using the Preferred Reporting Items for Systematic review and Meta-analysis (PRISMA) [45]. Identification of studies followed a three-step process: (i) search, (ii) distillation, and (iii) independent review [46]. To assess the quality of the identified articles, the researchers used the Quality Criteria Checklist from the Academy of Nutrition and Dietetics (AND) Evidence Analysis Manual [46, 47]. No IRB approval was acquired as no humans or animals were involved in this study.
In the first phase, search, the researchers used four databases: PubaMed, CINAHL, SCOPUS, and PsycINFO to identify these articles [46]. The key search terms, in various combinations, were used to identify articles: “adults, 18 years and older,” “worksite wellness/employee wellness/organization,” “nutrition/dietary/nutritious,” “physical activity/exercise,” “interventions/programs,” “overweight/obesity,” “body composition/weight percentage,” and “body fat/weight/weight loss.” A language restriction was applied to include publications written in English. Also, a time restriction for the literature published between January 1, 1980, and November 1, 2017, was applied. The reference list of the retrieved articles was searched to identify other relevant manuscripts for this review. Literature searches were combined into EPPI-Reviewer 4 [48], a software to assist in screening and removing duplicate articles [46].
2.2. Article Screening
The second phase of the systematic review process was the distillation phase. This involved one researcher reading through the titles and abstracts to identify articles that met the following nine inclusion criterion [46]: studies (1) were published peer-reviewed; (2) were published between January 1, 1980 to November 1, 2017; (3) included experimental studies; (4) included participants over 18 years of age; (5) included participants that were overweight (BMI ≥ 25 kg/m2) and/or obese (BMI ≥ 30 kg/m2); (6) took place at a worksite; (7) had intervention components that included physical activity and nutrition education; (8) involved interventions that lasted 12 months or longer and (9) had outcome measurements that included body composition (BMI (kg/m2), waist circumference, and weight). Articles were excluded if they did not meet the above nine criteria.
The third phase of the systematic review process was the independent review of articles. In this phase, the two researchers independently read all remaining articles to determine the ones that met the inclusion criterion. After each reviewer independently identified the articles to keep, if discrepancies existed, a discussion took place until reviewers were satisfied with including or excluding the articles [46]. After this third phase, the remaining articles were critically evaluated for relevance and validity via the Quality Criteria Checklist from the Academy of Nutrition and Dietetics (AND) Evidence Analysis Manual [47]. Relevance determines a study's usefulness to the nutrition profession and is defined by four questions. If responses to all four questions were yes, the reviewers then proceeded to the validation questions; otherwise, the article was removed from this systematic review.
For validity, 10 criteria questions were used to determine the quality of these studies; a thorough discussion of each criterion is found within the AND Evidence Analysis Manual [47]. Each component within the validity portion of the analysis manual was answered with a yes, no, unclear, or not applicable. An article was determined of high quality (+) if responses to validity criterion 2, 3, 6, and 7 were yes with an additional yes from another criterion. An article was determined low quality (−) and subsequently removed from further analysis if the responses to criterion 2, 3, 6, and 7 and two additional criterion were no. An article was determined neutral (Ө) if responses to the validity criteria 2, 3, 6, and 7 was no or unclear.
After the two researchers independently evaluated the quality of the articles, interrater reliability was determined using quadratic weighted Cohen's kappa statistic [46, 49]. A quadratic weighted Cohen's kappa was selected to account for the degree of disagreement among the reviewers [46]. Kappa results were interpreted as follows: values ≤0 indicate no agreement, 0.01–0.20 indicates none to a slight agreement, 0.21–0.40 indicates fair agreement, 0.41–0.60 indicates moderate agreement, 0.61–0.80 indicates substantial agreement, and 0.81–1.00 indicates almost perfect agreement [46, 49].
2.3. Data Extraction
Table 1 was constructed and organized by the researchers to compare the data extracted from each article to be included in this systematic review. The data extracted included the first author's last name, publication date, location, research design, study duration, participants, design/intervention groups, theory/framework, intervention description, evaluation measures, and findings (Table 1).
Table 1.
Summary of articles included within the systematic review (n=23).
| Author (year) | Location | Design/duration | Population/groups | Theory/wellness intervention | Evaluation measures | Measurement techniques | Results |
|---|---|---|---|---|---|---|---|
| Allen et al. (2012) [43] | USA | RCT1,12 months | Total n=55 Intervention n=26 Control n=29 |
No specific theory Intervention: monthly education sessions and pedometers Control: no intervention |
BMI2, BF%3, WC4 | Weight: calibrated electronic scale Height: stadiometer BF: BIA5 WC: tape measurer No further specifications |
Intervention: insignificant decrease in BMI, BF%, or WC (p > 0.05) Control: WC increased (p < 0.05) |
|
| |||||||
| Almeida et al. (2015) [10] | USA | RCT,12 months | Total n=1,790 Intervention n=1001 Control n=789 |
No specific theory Intervention: daily email, incentives, education website Control: quarterly newsletter and 1-hour resource session |
BW6, BMI | Weight: calibrated electronic scale Height: stadiometer No further specifications |
Intervention: BW and BMI decreased (p < 0.05) |
|
| |||||||
| Baker Parker et al. (2010) [50] | USA | Quasi-experimental: 3 groups, 24 months | Total n=2,431 Intense n=1,520 Moderate n=382 Control n=529 |
No specific theory Intense intervention: health goals, prompts, and messages Moderate intervention: prompts and messages Control: no intervention |
BMI | Weight and height were measured, but no further specifications | An insignificant decrease in BMI (p > 0.05) |
|
| |||||||
| Barham et al. (2011) [36] | USA | RCT,12 months | Total n=45 Intervention n=21 Control n=24 |
No specific theory Intervention: 12 1-hour weekly sessions; 1-hour monthly sessions Control: 3-month delay of intervention |
BMI, WC | Weight: calibrated electronic scale Height: stadiometer WC: tape measurer. Measurements were taken by trained professionals, no further specifications |
Intervention: decreased BMI (p < 0.001) and WC (p=0.004) in the first three months |
|
| |||||||
| Campbell et al. (2002) [51] | USA | RCT,18 months | Total n=660 Intervention n=362 Control n=298 |
Social cognitive theory, Stages of Change Trans-Theoretical framework, social support model Intervention: two personalized tailored “magazines,” Natural helpers Control: after 6 months, 1 magazine was provided |
BMI | Weight: calibrated scale Height: tape measure Weight and height measured without shoes |
No changes in BMI |
|
| |||||||
| Christensen et al. (2012) [31] | Denmark | RCT,12 months | Total n=98 Intervention n=54 Control n=44 |
Cognitive behavioral training Intervention: 1-hour weekly educational sessions Control: monthly 2-hour oral presentations |
BW, BMI, BF% | Weight: calibrated scale. Measurements taken without socks and shoes, light clothing, 1 kg subtracted to compensate for clothing. Height: stadiometer Measurements taken without shoes BF: BIA. Measured by “standard” body frame and participant's age, height, and gender BF: tape measurer. Waist circumference measured over umbilicus. Hip circumference measured on the hip part that gave the greatest circumference |
Intervention: BW decreased by 6 kg (p < 0.001) BMI decreased by 2.2 kg/m2 (p < 0.001) BF% decreased by 2.8% (p < 0.001) |
|
| |||||||
| Fernandez et al. (2015) [52] | USA | RCT: 10 groups,24 months | Total n=2,996 Intervention n=1,882 Control n=1,114 |
No specific theory Intervention: marketing at workplace, newsletters, interactive website Control: no intervention |
BMI | Weight: calibrated electronic scale Height: stadiometer Measurements were taken in street clothes and without shoes |
Intervention: BMI decreased by 0.54 kg/m2 (p=0.02) Control: BMI decreased by 0.12 kg/m2 (p=0.73) |
| French et al. (2010) [53] | USA | RCT, 18 months |
Total n=696 | No specific theory Intervention: healthy vending machine options, fitness facility, self-weighing competition, 2-day long health expos, monthly farmers markets Control: quarterly advisory group |
BMI | Weight: calibrated electronic scale Height: stadiometer Measurements taken in street clothes and without shoes; 2 separate measurements taken and then averaged the values |
Intervention: BMI decreased by −0.14 kg/m2 (p < 0.005) |
|
| |||||||
| Goetzel et al. (2014) [54] | USA | 1 cohort group, 12 months |
Total n=2,458 | No specific theory Intervention: 15-minute individual telephone health coaching and online interactive wellness tools |
BMI | Self-reported weight and height No specifications on how they trained participants to take these measurements |
BMI decreased by 2.0 kg/m2 (p < 0.001) |
|
| |||||||
| Hochart et al. (2011) [32] | USA | Pretest, posttest: 13 groups, 36 months |
Total n=8,030 Intervention n=4,230 Control n=3,800 |
No specific theory Intervention: telephone coaching, worksite or webinar education classes, online resources, and behavior change support tools Control: no intervention |
BW, BMI | Weight and height measured, but no specifications on how these measurement techniques were taken | Intervention: Insignificant decreases in BW and BMI (p > 0.05) |
|
| |||||||
| LeCheminant et al. (2012) [55] | USA | 1 cohort group 24 months |
Total n=174 | Behavioral change framework Intervention: 6, 3- to 8-week intervention campaigns |
BMI | Weight and height measured, but no specifications on how these measurement techniques were taken | BMI increased (p < 0.05) |
|
| |||||||
| Lemon et al. (2014) [56] | USA | RCT, 24 months |
Total n=782 Intervention n=446 Control n=336 |
Social ecological model Intervention: fitness facilities, healthy lunchroom options, elimination of SSB7, healthy prompts, print, and web-based materials Control: print and web-based materials only |
BMI | Weight: calibrated electronic scale. Measured by trained staff, readings to the nearest 2/10th pound Height: stadiometer. Measured by trained staff, readings to the nearest 1/8th inch |
Decreased BMI -0.48 kg/m2 (p=0.05) |
|
| |||||||
| Leyk et al. (2014) [57] | Germany | Pretest, posttest: 3 groups, 12 months |
Total n=474 Nonactive n=129 Not very active n=209 Very active n=136 |
No specific theory Intervention: voluntary sport participation, sports-medicine exam, monthly lectures |
BW, BMI, BF%, WC | Weight: calibrated electronic scale Height: stadiometer BF: caliper WC: tape measurer Sports-medicine specialist took the measurements, no specifications of how measurements were taken |
Decrease in BW (p=0.002), BMI (p < 0.001), and WC (p=0.001) among men No significant differences among women |
|
| |||||||
| Linde et al. (2012) [44] | USA | RCT, 24 months |
Total n=1,406 Intervention n=611 Control n=795 |
No specific theory Intervention: education classes Control: no intervention |
BW, BMI | Weight: calibrated electronic scale. Trained team specialists measured to the nearest 0.1 kg wore light street clothes without shoes Height: stadiometer Trained team specialists measured to the nearest 0.1 cm |
Intervention: no changes in BW and BMI |
| Mache et al. (2015) [34] | Germany | RCT, 12 months |
Total n=675 Intervention n=377 Control n=298 |
No specific theory Intervention: weekly 30–60 minutes training sessions, healthy food and exercise demonstrations, and activities Control: no intervention |
BMI | Weight and height measured but no further specifications | No changes in BMI |
|
| |||||||
| MacKinnon et al. (2010) [58] | USA | RCT: 3 groups, 48 months |
Total n=599 MI n=202 TEAM n=234 Control n=163 |
No specific theory TEAM: 11–45 minute sessions in the first year and 6 booster sessions in the second year MI: 4 1-hour individual motivational interviewing sessions in the first year, and 2 meetings with a counselor and optional additional 6 hours of in-person or phone contact in the second year Control: no intervention |
BMI | Weight and height measured but no further specifications | Decreased BMI for TEAM intervention at 1 year (p=0.06) |
|
| |||||||
| Merrill et al. (2014) [59] | USA | 1 cohort group, 48 months |
Year 1 n=1,814 Year 2 n=2,777 Year 3 n=2,739 Year 4 n=3,012 |
Motivational interviewing theory Intervention: monetary incentives, monthly newsletter, individual health coaching |
BMI, BF% | BMI: weight and height measured but no further specifications BF%: body fat analyzer, but no further specifications |
Over the 4-year period, decreased BMI (p < 0.05) |
|
| |||||||
| Merrill et al. (2010) [60] | USA | 1 cohort group, 12 months |
Total n=6,128 | Healthy belief model, Trans-theoretical model of change, motivational interviewing Intervention: telephonic health coaching |
BMI | Weight and height measured but no further specifications | Decreased BMI (p < 0.001) |
|
| |||||||
| Muto et al. (2001) [37] | Japan | RCT, 18 months |
Total n=302 Intervention n=152 Control n=150 |
No specific theory Intervention: 4-day education program, individual counseling, group discussions Control: no intervention |
BMI | Weight and height measured but no further specifications | Intervention: decreased BMI by 0.5 kg/m2 (p < 0.05) |
|
| |||||||
| Neville et al. (2011) [33] | USA | Quasi-experimental: 3 groups, 96 months |
Total n=365 Group 1 n=108 Group 2 n=106 Group 3 n=151 |
No specific theory Intervention: monthly education sessions, incentives, health screenings Control: no intervention |
BW, BMI, BF% | Weight: calibrated electronic scale Height: stadiometer BF: BIA Trained health educator staff members took measurements, but no further specifications |
Decreased BMI for the highest risk group (group #1) (p < 0.05) |
|
| |||||||
| Poole et al. (2001) [61] | USA | 1 cohort group, 48 months |
Total n=304 | No specific theory Intervention: annual health assessment, incentive system |
BF% | Skinfold calipers. Measurements were taken at the chest, abdomen, and thigh for men and triceps, supra-ilium, and thigh for females | Decreased BF% (p < 0.05) |
|
| |||||||
| Robroek et al. (2012) [62] | Netherlands | RCT, 24 months |
Total n=924 Intervention n=465 Control n=459 |
Social cognitive theory Intervention: physical health check, face-to-face advice, personal feedback, monthly emails Control: no intervention |
BMI | Weight and height measured, no further specifications. In the follow-up measurement, height and weight were self-reported | No decreases in BMI (p > 0.05) |
| Salinardi et al. (2013) [35] | USA | RCT, 12 months |
Total n=133 Intervention n=94 Control n=39 |
Social ecological model Intervention: 19 1-hour long education sessions Control: no intervention |
BW | Weight: calibrated electronic scale Measurements were taken with light indoor clothing and measured to 0.05 kg Height: stadiometer, no further specifications |
BW decreased by an average of 8 kg (p < 0.05) |
Note. 1 = randomized control trial, 2 = body mass index, 3 = body fat percentage, 4 = waist circumference, 5 = bioelectrical impedance analyzer, 6 = body weight, and 7 = sugar-sweetened beverages.
3. Results
3.1. Article Selection
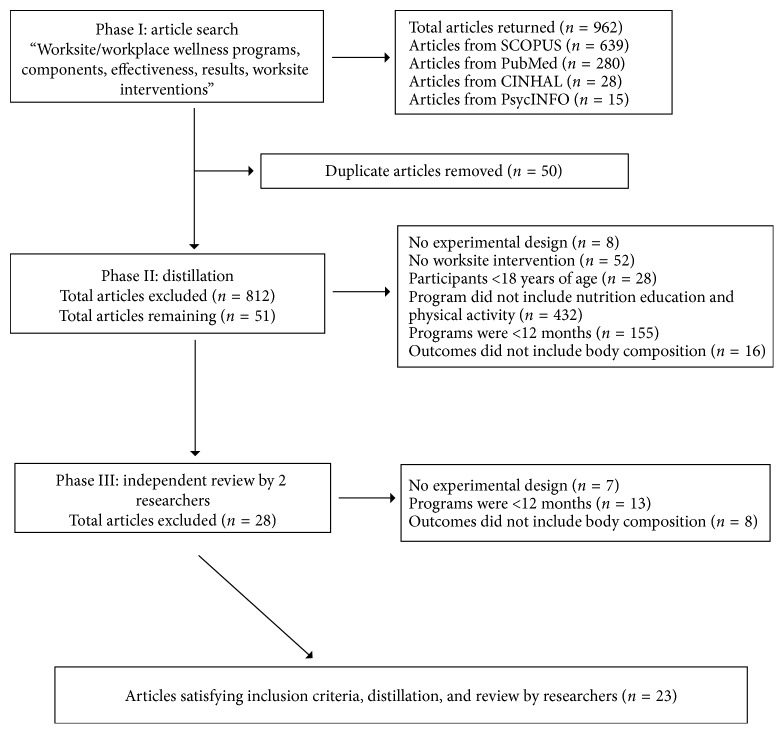
A total of 962 articles were identified from the first search phase: PubMed (n=280), CINAHL (n=28), SCOPUS (n=639), and PsycINFO (n=15) databases. In the second, or distillation phase, 150 articles were found to be duplicates and therefore removed. Then, using a 9-point inclusion checklist, one researcher reviewed the remaining 812 articles. From this initial review, 761 articles were removed because they did not have an experimental design (n=78), did not include a worksite program (n=52), included participants younger than 18 years of age (n=28), did not include nutrition education and physical activity components (n=432), were less than twelve months in duration (n=155), and outcomes did not include an aspect of body composition (n=16). After phase two, 51 articles remained and were independently reviewed by two researchers. In this final phase, 28 articles were excluded because they did not have an experimental design (n=7), were less than twelve months in duration (n=13), and outcomes did not include an aspect of body composition (n=8) (Figure 1).
Figure 1.
Article extraction.
From the 23 articles that remained, the researchers assessed their quality. These studies were deemed high quality. None of the studies was rated as low quality. Unbiased endpoint assessment (i.e., not clearly stating if researchers were blinded), calculation of outside factors that could impact the results (i.e., dietary intake and physical activity behaviors in the home), variability in measurement techniques of body composition, and lost to follow-up received the lowest ratings across all items irrespective of study design. The overall kappa score from the researchers was 0.76, which demonstrates substantial agreement [49] (Table 2).
Table 2.
Quality of studies within the systematic review (n=23).
| Author (Year) | Quality rating | Research question stated | Clear of selection bias | Comparable study groups | Withdraws discussed | Blinding use | Intervention described | Outcomes defined | Appropriate statistical analyses | Results support conclusions | No potential for funding bias |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Allen et al. (2012) [43] | + | Y | Y | Y | N | N | Y | Y | Y | Y | Y |
| Almeida et al. (2015) [10] | + | Y | Y | Y | N | N | N | Y | Y | Y | Y |
| Baker Parker et al. (2010) [50] | + | Y | Y | Y | N | N | Y | Y | Y | Y | Y |
| Barham et al. (2011) [36] | + | Y | Y | Y | N | N | Y | Y | Y | Y | Y |
| Campbell et al. (2002) [51] | + | Y | Y | Y | N | N | Y | Y | Y | Y | Y |
| Christensen et al. (2012) [31] | + | Y | Y | Y | N | Y | Y | Y | Y | Y | Y |
| Fernandez et al. (2015) [52] | + | Y | Y | Y | N | N | Y | Y | Y | Y | Y |
| French et al. (2010) [53] | + | Y | Y | Y | N | N | Y | Y | Y | Y | Y |
| Goetzel et al. (2015) [54] | + | Y | Y | Y | N | N | Y | Y | Y | Y | Y |
| Hochart et al. (2011) [32] | + | Y | Y | Y | N | N | Y | Y | Y | Y | Y |
| LeCheminant et al. (2012) LeCheminant | + | Y | N | N/A | N | N | Y | Y | Y | Y | Y |
| Lemon et al. (2014) [56] | + | Y | Y | Y | N | N | Y | Y | Y | Y | Y |
| Leyk et al. (2014) [57] | + | Y | N | Y | Y | N | Y | Y | Y | Y | Y |
| Linde et al. (2012) [44] | + | Y | Y | Y | N | Y | Y | Y | Y | Y | Y |
| Mache et al. (2015) [34] | + | Y | Y | Y | N | N | Y | Y | Y | Y | Y |
| MacKinnon et al. (2010) [58] | + | Y | Y | Y | N | N | Y | Y | Y | Y | Y |
| Merrill et al. (2014) [59] | + | Y | Y | Y | N | N | Y | Y | Y | Y | Y |
| Merrill et al. (2010) [60] | + | Y | Y | Y | N | N | Y | Y | Y | Y | Y |
| Muto et al. (2001) [37] | + | Y | Y | Y | N | N | Y | Y | Y | Y | Y |
| Neville et al. (2011) [33] | + | Y | Y | N/A | Y | N | Y | Y | Y | Y | Y |
| Poole et al. (2001) [61] | + | Y | Y | Y | N | N | Y | Y | Y | Y | Y |
| Robroek et al. (2012) [62] | + | Y | Y | Y | N | Y | Y | Y | Y | Y | Y |
| Salinardi et al. (2013) [35] | + | Y | Y | Y | Y | N | Y | Y | Y | Y | Y |
Note. Quality ratings: (+) = positive.
3.2. Study Range and Characteristics
The twenty-three studies included a total of 41,867 participants, ranging between 45 and 8,030 participants, with a mean of 1,819 participants [10, 31–37, 43, 44, 50–62]. Four studies did not report the age range of participants, but three studies included participants aged 18 years and older [10, 30, 50] and one study included participants aged 21 years and older [53]. The designs of these studies were randomized controlled trials (n=14) [10, 31, 34–37, 43, 44, 51–53, 56, 58, 62], prospective cohorts (n=5) [54, 55, 59–61], pretest/posttest (n=2) [32, 57], and quasi-experimental design (n=2) [33, 50]. The shortest duration of the interventions lasted one year [31, 35, 36, 43, 54, 56, 57, 60, 63], and the longest intervention lasted eight years [33].
3.3. Synthesis of the Intervention Results
Of the twenty-three studies, six studies offered monthly educational sessions [33, 35, 43, 55, 57, 58], three offered weekly educational sessions [31, 34, 36], two offered a one-time educational session [37, 62], and two offered an unspecified amount of educational sessions [32, 44]. These educational sessions included topics such as nutrition, physical activity, and health behaviors. Studies offered telephone health coaching throughout the intervention (n=3) [32, 54, 60] or in-person health coaching (n=1) [59], health screenings (n=5) [33, 51, 57, 61, 62], and provided magazines (n=1) [51] or posters (n=5) [32, 50, 52, 53, 56].
Specific physical activity components offered within some of the interventions aside from physical activity education, training, and encouragement included pedometer step counting [43], voluntary participation in sports [57], and on-site fitness facilities for employees [34, 53, 56].
Of the twenty-three studies, four of them incorporated incentives into the intervention [10, 33, 59, 61]. Incentives included being entered into a $250 cash prize lottery for completing a health screening [63] and redeeming healthy behavior points for cash prizes for logging behaviors such as exercising, being a nonsmoker or quitting, reducing or maintaining optimal blood pressure, cholesterol, and/or body fat levels, having routine preventative exams, and engaging in various educational activities on healthy lifestyle topics [33, 61].
Additionally, studies included some form of a theory or framework to guide the intervention. These included a social-based theory: Social Cognitive theory (n=1) [62] or Social Ecological Model (n=2) [35, 37]; a self-driving theory: Motivational Interviewing (n=1) [59]; a behavioral change theory: Cognitive Behavioral Training (n=1) [31] and Behavioral Change Framework (n=1) [55]; or a combination of theories: Social Support Model, Social Cognitive Theory, and Stages of Change Trans-Theoretical [51] and the Health Belief Model, Motivational Interviewing, and Stages of Change Trans-Theoretical [60]. Fifteen of the articles did not specify a certain theory but included elements such as a voluntary participation and incentives to encourage a self-motivation component within the intervention.
Studies varied in the measurement techniques for determining body composition. For determination of BMI, calibrated electronic/digital scales and a stadiometer were used (n=12) [10, 31, 33, 35, 36, 43, 44, 51–53, 56, 57] or had participants self-report their height and weight (n=1) [54]. For determination of body fat, a bioelectrical impedance analyzer (n=4) [31, 33, 43, 59] or skinfold calipers (n=2) were used [57, 61]. For determination of waist circumference, flexible tape measures were used (n=4) [31, 36, 43, 57]. However, there were research studies that indicated biometric measurements such as weight and height were taken, but did not report the device(s) used (n=8) [32, 34, 37, 50, 55, 58, 59, 62]. Seven studies provided specifics on measurements [31, 35, 44, 51–53, 56, 61]. Measurements were primarily taken at baseline and postintervention with a few measurements taken at certain time points of the intervention (e.g., baseline, 12 months, and 24 months) [32, 33, 37, 44, 50, 52, 55, 56, 58, 59, 61, 62].
Results from studies showed statistically significant changes in body composition (e.g., decreased BMI, body fat percentage, and waist circumference) [10, 33, 35–37, 52, 54, 56–61]. Even though body composition changed in other studies, these findings were not statistically significant [31, 50, 53]. Six of the interventions did not show any changes in body composition [32, 34, 43, 44, 51, 62], and one showed an increase in BMI [55].
4. Discussion
Twenty-three studies were included in this systematic review to evaluate worksite wellness nutrition and physical activity programs and their subsequent impact on participants' body composition. Overall, results from this systematic review showed inconsistencies with the effect worksite wellness programs had on participants' body composition. In which, 13 studies resulted in significant changes in body composition (e.g., decreased BMI (kg/m2), body fat percentage, and waist circumference), three resulted in nonsignificant changes in body composition (e.g., slightly decreased BMI (kg/m2), body fat percentage, and waist circumference), six resulted in no changes in body composition and one showed an increase in BMI. Interventions that lasted for 48 or 96 months consistently demonstrated significant changes in body composition compared to those interventions that lasted between 12 and 36 months. Furthermore, regardless of the length of the intervention, participants who were able to interact with others on a consistent basis (e.g., interactive websites, group discussions, or one-on-one health coaching) were more likely to change their body composition (e.g., decreased BMI (kg/m2), body fat percentage, and waist circumference). However, there were inconsistencies with the incorporation of physical activity and change in participants' body composition as well as measurement techniques to analyze body composition.
Further analysis of these programs showed those that used a self-motivation theory (Motivational Interviewing) resulted in a greater change in body composition (e.g., decreased BMI (kg/m2), body fat percentage, and waist circumference) compared to those programs that did not use this type of theory. Motivational Interviewing is described as a direct, client-centered counseling style to initiate or derive a behavior change by means of aiding individuals and educating to resolve uncertainty [64]. Two of the studies within the review specifically utilized Motivational Interviewing as the framework for the interventions [59, 61]. Merrill and Merill [59] conducted a 4-year workplace program that was designed based on Motivational Interviewing and included health courses and personal telephone coaching. Participants (n=10,342) were split into 4 groups: year 1 (n=1,814), year 2 (n=2,777), year 3 (n=2,739), and year 4 (n=3,012). Results showed that all groups were successful in decreasing BMI and body fat percentage. Conclusions indicated that engaging and motivating participants to change their behaviors led to positive weight outcomes. In accordance with this study, several other studies demonstrated that Motivational Interviewing engages participants and ultimately changes aspects of their behaviors to improve health outcomes [65–67]. Kouwenhoven-Pasmooij and colleagues (2018) [67] showed that by incorporating Motivational Interviewing within a health-risk assessment class, participants (n=274) were more motivated and engaged and increased their participation in health-promotion activities compared to those participants (n=217) that were not. The researchers concluded that Motivational Interviewing should be incorporated into classes to further engage participants in health-promoting activities. Even though modest changes in body composition were seen in the studies that directly used a theory, the design, methods, and frequency of providing information to participants may have also led to changes in body composition.
The educational content presented in these interventions focused on increasing healthy eating habits, physical activity, and healthy behaviors presented in a variety of methods such as emails, face to face, telephone calls, interactive websites, newsletters, posters, or a combination of methods. Participants had a reduction in body composition if the educational content was based on their knowledge or the content's messaging was tailored to their knowledge level. Designing content that is tailored to an individual's knowledge and attitudes may increase his or her self-motivation to change health behaviors [68, 69]. However, results from a few studies, in which tailored messaging were incorporated within the interventions, did not show a change in body composition [32, 51, 70]. This may be because the messages were not designed based on participants' knowledge and attitudes, participants were not motivated, or it is not known whether the frequency of these messages was conveyed to the participants. The frequency of researchers interacting with participants ranged from daily [63] to monthly [33, 43, 57, 59, 70] and for a minimum interaction time of 15 minutes [54] to a maximum of one hour [31, 34–36, 58]. If participants received frequent interaction, regardless of the length of time and the method, there were changes in the participants' body composition. Other studies, including systematic reviews, reported that participants who had frequent interactions with health professionals reduced their body weight significantly more compared to those who had limited or no interactions [71–75]. Receiving continuous feedback or support from health professionals may enhance participants' motivation and vigilance to maintain their lifestyle behaviors. However, this is not always the case as a study [34] showed. Participants in the intervention group (n=377) were exposed to weekly 30- or 60-minute nutrition educational sessions over 12 months. However, there were no changes in BMI compared to the control group. This may have been because participants were not motivated or provided with sufficient support. Thus, future worksite wellness programs should consider the depth of the educational content and the frequency of interaction for participants to remain motivated to adhere to the program and ultimately affect their body composition.
Furthermore, there were inconsistencies with the impact physical activity had on participants' body composition. Studies used various devices such as pedometers and accelerometers to increase physical activity among participants in these worksite interventions [31, 43, 55]. Pedometers measure steps and total physical activity but not intensity, while accelerometers measure frequency but not the type of exercise [76]. Neither can provide adequate information on the duration, frequency, and intensity of the activity, which would provide a more reliable measure of energy expenditure [77]. Aparicio-Ugarriza and colleagues [77] conducted a review of the literature to identify a method to better assist with tracking physical activity. Results showed that all measurement devices developed for tracking physical activity in the field contained limitations such as the inability to measure intensity, frequency, and type of physical activity. To fully understand the impact physical activity has on body composition, further development needs to be conducted on these devices that can obtain information on intensity, duration, and frequency.
The main outcomes of this review showed a change in participants' body composition; however, the tools used to measure body composition fluctuated. Moreover, these studies used simple, quick, and noninvasive tools to measure body composition due to the number of participants and the location of these studies (e.g., businesses). Twelve studies indicated the use of a calibrated scale to measure body weight and a stadiometer to measure height to determine participants' BMI. Only six of those studies indicated the techniques used to take these measurements (e.g., no socks or shoes, measured to the nearest kg). The accuracy of these scales, though, may not have been adequate. A report that evaluated 223 scales in health-care clinics and fitness and weight loss centers showed that increased weight led to decreased precision. Moreover, more than 25% of the scales were off by more than 0.9 kg, and 15% were off by more than 2 kg [78]. Additionally, the condition of the scales, surface (e.g., rug and concrete), and calibration history was not reported, which may have led to imprecise body weight. Furthermore, one study collected weight and height based on self-reported data, which may have been inaccurate as participants may have underreported their weight and over reported their height or had recall bias [79–81]. Additionally, the weight of the individual cannot determine the percentage of body fat or muscle mass, which may produce erroneous classifications of BMI, thus reporting BMI should be with caution [82]. For example, a bodybuilder with 12% body fat may potentially be characterized as overweight due to his weight compared to his height. Therefore, using other tools to define body composition may be more effective. Four studies used a bioelectrical impedance analyzer (BIA), and two studies used skinfold calipers to measure body fat. The studies which measured body fat with a BIA did not specify the body parts measured (e.g., hand to hand, foot to foot, or hand to foot), the conditions (e.g., fasting/hydration status, exercise status, and phase of menstrual cycle), nor the calibration techniques, which may have affected the measurement accuracy [83–85]. Also, BIAs are more accurate in a BMI range of 17–34 kg/m2, and in the included studies, some participants had a BMI > 34 kg/m2 [85, 86]. Congruent with BIA measurement issues, skinfold measurements may also be inaccurate due to age, gender, and variability of fat distribution [87, 88]. Additionally, limited information was provided about calibration and the number of times measurements were repeated [89]. Finally, four studies used a tape measurer for determination of waist circumference. As with the other measurement tools, limited information was provided about the methods used to obtain the measurements (e.g., relax stance, normal expiration, and repeated measures). In addition, inaccuracies of measurements may have been obtained especially if the tape could not lay flat against the skin due to deposits of fat or the marked curvature near the iliac crest [90, 91]. From the 23 studies, six used a variety of body composition measurement tools and techniques to reduce measurement inaccuracies from using only one tool. Therefore, future studies should include the exact techniques they are using to measure one's weight as well as consider multiple tools to reduce any potential measurement inaccuracies.
4.1. Limitation
A limitation of this systematic review was that the search focused on nutrition education and physical activity in worksite programs that were long-term, thus limiting the potential number of articles. Second, while some of the studies reviewed showed positive results, the methods of collecting body composition data were inconsistent. The methods to measure body composition included body fat percentage calculation, body weight measurement, BMI calculation, and waist circumference measurement. To improve this limitation, inclusion criteria could have specified body measurement techniques. This would have created consistencies across the studies but would have also potentially limited the number of studies that would have been able to be included within the review. Another limitation was that the studies did not specifically measure baseline diet quality and did not keep adequate records of food intake throughout the studies. This could have caused variation in findings between participants. To better analyze the diet quality, the researchers could have included a quality analysis of diet at baseline as well as assigned a diet recall for participants to record throughout the studies. It is known that physical activity can be effective for reducing weight, but the combination of both diet and exercise has been proven to be the most effective means of weight loss [92, 93]. Because of this, it would have been beneficial to take a closer look at the dietary behaviors of participants. If participants were practicing nutritious eating behaviors while also increasing physical activity, weight loss would be more likely to occur [94].
5. Conclusion
Worksite wellness programs that were designed using motivational theories, content was created based on participants' needs and participants had frequent interactions with health professionals, resulted in a change in participants' body composition. Future research would be beneficial for the continued analysis of worksite wellness program components. Breaking programs apart into the basic components could help to identify what is effective in not only changing body composition but also decreasing risk factors for chronic diseases such as type 2 diabetes and heart disease. While self-motivation theories and intensive educational sessions have been identified as effective components, there are more elements of programs to explore such as health assessments, health marketing, and health campaigns. If the most effective and beneficial components of worksite programs could be identified, all future worksite wellness programs could be modeled using only favorable elements to warrant positive results.
Disclosure
The results of this study were presented at a poster session at the annual Society for Nutrition Education and Behavior conference in July 2018.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.World Health Organization. Obesity and Overweight. Geneva, Switzerland: WHO; 2018. http://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. [Google Scholar]
- 2.Benjamin E. J., Blaha M. J., Chiuve S. E., et al. Heart disease and stroke Statistics’2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ogden C. L., Carroll M. D., Fryar C. D., Flegal K. M. Prevalence of Obesity Among Adults and Youth: United States, 2011–2014, NCHS Data Brief, No. 219. Hyattsville, MD, USA: National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- 4.Flegal K. M., Kruszon-Moran D., Carroll M. D., Fryar C. D., Ogden C. L. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016;315(21):2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trembling P. M., Apostolidou S., Gentry-Maharaj A., et al. Risk of chronic liver disease in post-menopausal women due to body mass index, alcohol and their interaction: a prospective nested cohort study within the United Kingdom Collaborative Trial of Ovarian Cancer Screening (UKCTOCS) BMC Public Health. 2017;17(1):p. 603. doi: 10.1186/s12889-017-4518-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gregg E. W., Shaw J. E. Global health effects of overweight and obesity. New England Journal of Medicine. 2017;377(1):80–81. doi: 10.1056/NEJMe1706095. [DOI] [PubMed] [Google Scholar]
- 7.Shirakami Y., Ohnishi M., Sakai H., Tanaka T., Shimizu M. Prevention of colorectal cancer by targeting obesity-related disorders and inflammation. International Journal of Molecular Sciences. 2017;18(5):p. 908. doi: 10.3390/ijms18050908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kovesdy C. P., susan F., ZoCCali C. Obesity and kidney disease: hidden consequences of the epidemic Obesidad y enfermedad renal: las consecuencias ocultas de una epidemia. Revista Medica de Chile. 2017;145:281–291. doi: 10.4067/S0034-98872017000300001. [DOI] [PubMed] [Google Scholar]
- 9.Rubinow K. B., Rubinow D. R. In immune defense: redefining the role of the immune system in chronic disease. Dialogues in Clinical Neuroscience. 2017;19(1):19–26. doi: 10.31887/DCNS.2017.19.1/drubinow. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Almeida F. A., You W., Harden S. M., et al. Effectiveness of a worksite-based weight loss randomized controlled trial: the worksite study. Obesity. 2015;23(4):737–745. doi: 10.1002/oby.20899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moore L. V., Dodd K. W., Thompson F. E., Grimm K. A., Kim S. A., Scanlon K. S. Using behavioral risk factor surveillance system data to estimate the percentage of the population meeting US department of agriculture food patterns fruit and vegetable intake recommendations. American Journal of Epidemiology. 2015;181(12):979–988. doi: 10.1093/aje/kwu461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee-Kwan S. H., Moore L. V., Blanck H. M., Harris D. M., Galuska D. Disparities in state-specific adult fruit and vegetable consumption—United States, 2015. MMWR. Morbidity and Mortality Weekly Report. 2017;66(45):1241–1247. doi: 10.15585/mmwr.mm6645a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ammendolia C., Côté P., Cancelliere C., et al. Healthy and productive workers: using intervention mapping to design a workplace health promotion and wellness program to improve presenteeism. BMC Public Health. 2016;16:p. 1190. doi: 10.1186/s12889-016-3843-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Asay G. R. B., Roy K., Lang J. E., Payne R. L., Howard D. H. Absenteeism and employer costs associated with chronic diseases and health risk factors in the US workforce. Preventing Chronic Disease. 2016;13:p. e141. doi: 10.5888/pcd13.150503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bauer U. E., Briss P. A., Goodman R. A., Bowman B. A. Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA. The Lancet. 2014;384(9937):45–52. doi: 10.1016/S0140-6736(14)60648-6. [DOI] [PubMed] [Google Scholar]
- 16.United States Department of Labor. American Time Use Survey-2017 Results. Washington, DC, USA: United States Department of Labor; 2018. https://www.bls.gov/news.release/pdf/atus.pdf. [Google Scholar]
- 17.Gainer R. D. History of ergonomics and occupational therapy. Work. 2008;31(1):5–9. [PubMed] [Google Scholar]
- 18.Chenoweth D. Worksite Health Promotion. 3rd. Champaign, IL, USA: Kinetics; 2011. [Google Scholar]
- 19.Sparling P. B. Preventing chronic disease. Preventing Chronic Disease. 2010;77(11) [Google Scholar]
- 20.Cawley J., Meyerhoefer C. The medical care costs of obesity: an instrumental variables approach. Journal of Health Economics. 2012;31(1):219–230. doi: 10.1016/j.jhealeco.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 21.Cawley J., Rizzo J. A., Haas K. Occupation-specific absenteeism costs associated with obesity and morbid obesity. Journal of Occupational and Environmental Medicine. 2007;49(12):1317–1324. doi: 10.1097/JOM.0b013e31815b56a0. [DOI] [PubMed] [Google Scholar]
- 22.Gates D. M., Succop P., Brehm B. J., Gillespie G. L., Sommers B. D. Obesity and presenteeism: the impact of body mass index on workplace productivity. Journal of Occupational and Environmental Medicine. 2008;50(1):39–45. doi: 10.1097/JOM.0b013e31815d8db2. [DOI] [PubMed] [Google Scholar]
- 23.Guardian. The 2014 Workplace Benefits Study. New York, NY, USA: Guardian; 2014. [Google Scholar]
- 24.Kruseman M., Schmutz N., Carrard I. Long-term weight maintenance strategies are experienced as a burden by persons who have lost weight compared to persons with a lifetime normal, stable eight. Obesity Facts. 2017;10(4):373–385. doi: 10.1159/000478096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McLoughlin R. F., McDonald V. M., Gibson P. G., et al. The impact of a weight loss intervention on diet quality and eating behaviours in people with obesity and COPD. Nutrients. 2017;9(1147):1–14. doi: 10.3390/nu9101147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Villareal D. T., Aguirre L., Gurney A. B., et al. Aerobic or resistance exercise, or both, in dieting obese older adults. New England Journal of Medicine. 2017;376:1943–1955. doi: 10.1056/NEJMoa1616338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kelley C. P., Sbrocco G., Sbrocco T. Behavioral modification for the management of obesity. Primary Care: Clinics in Office Practice. 2016;43(1):159–175. doi: 10.1016/j.pop.2015.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Francois M. E., Gillen J. B., Little J. P. Carbohydrate-restriction with high-intensity interval training: an optimal combination for treating metabolic diseases? Frontiers in Nutrition. 2017;4 doi: 10.3389/fnut.2017.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.den Braver N. R., de Vet E., Duijzer G., et al. Determinants of lifestyle behavior change to prevent type 2 diabetes in high-risk individuals. International Journal of Behavioral Nutrition and Physical Activity. 2017;14(1):p. 78. doi: 10.1186/s12966-017-0532-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mattke S., Liu H., Caloyeras J., et al. Workplace wellness programs study: final report. Rand Health Quarterly. 2013;3(2):p. 7. [PMC free article] [PubMed] [Google Scholar]
- 31.Christensen J. R., Overgaard K., Carneiro I. G., Holtermann A., Søgaard K. Weight loss among female health care workers- a 1-year workplace based randomized controlled trial in the FINALE-health study. BMC Public Health. 2012;12(1):p. 625. doi: 10.1186/1471-2458-12-625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hochart C., Lang M. Impact of a comprehensive worksite wellness program on health risk, utilization, and health care costs. Population Health Management. 2011;14(3):111–116. doi: 10.1089/pop.2010.0009. [DOI] [PubMed] [Google Scholar]
- 33.Neville B. H., Merrill R. M., Kumpfer K. L. Longitudinal outcomes of a comprehensive, incentivized worksite wellness program. Evaluation and the Health Professions. 2011;34(1):103–123. doi: 10.1177/0163278710379222. [DOI] [PubMed] [Google Scholar]
- 34.Mache S., Jensen S., Linnig S., et al. Do overweight workers profit by workplace health promotion, more than their normal-weight peers? Evaluation of a worksite intervention. Journal of Occupational Medicine and Toxicology. 2015;10(1):p. 28. doi: 10.1186/s12995-015-0068-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Salinardi T. C., Batra P., Roberts S. B., et al. Lifestyle intervention reduces body weight and improves cardiometabolic risk factors in worksites. American Journal of Clinical Nutrition. 2013;97(4):667–676. doi: 10.3945/ajcn.112.046995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barham K., West S., Trief P., Morrow C., Wade M., Weinstock R. S. Diabetes prevention and control in the workplace: a pilot project for county employees. Journal of Public Health Management and Practice. 2011;17(3):223–241. doi: 10.1097/PHH.0b013e3181fd4cf6. [DOI] [PubMed] [Google Scholar]
- 37.Muto T., Yamauchi K. Evaluation of a multicomponent workplace health promotion program conducted in Japan for improving employees’ cardiovascular disease risk factors. Preventive Medicine. 2001;33(6):571–577. doi: 10.1006/pmed.2001.0923. [DOI] [PubMed] [Google Scholar]
- 38.Prochaska J. O. Transtheoretical therapy: toward a more integrative model of change. Psychotherapy: Theory, Research & Practice. 1982;19(3):p. 276. doi: 10.1037/h0088437. [DOI] [Google Scholar]
- 39.Kwasnicka D., Dombrowski S. U., White M., Sniehotta F. Theoretical explanations for maintenance of behaviour change: a systematic review of behaviour theories. Health Psychology Review. 2016;10(3):277–296. doi: 10.1080/17437199.2016.1151372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cook D. A., Artino A. R. Motivation to learn: an overview of contemporary theories. Medical Education. 2016;50(10):997–1014. doi: 10.1111/medu.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Castelnuovo G., Pietrabissa G., Manzoni G. M., et al. Cognitive behavioral therapy to aid weight loss in obese patients: current perspectives. Psychology Research and Behavior Management. 2017;2017(10):165–173. doi: 10.2147/PRBM.S113278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Quinton T. S., Brunton J. A. Implicit processes, self-regulation, and interventions for behavior change. Frontiers in Psychology. 2017;8:p. 346. doi: 10.3389/fpsyg.2017.00346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Allen J., Lewis J., Tagliaferro A. Cost-effectiveness of health risk reduction after lifestyle education in the small workplace. Preventing Chronic Disease. 2012;9:p. e96. doi: 10.5888/pcd9.110169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Linde J. A., Nygaard K. E., MacLehose R. F., et al. HealthWorks: results of a multi-component group-randomized worksite environmental intervention trial for weight gain prevention. International Journal of Behavioral Nutrition and Physical Activity. 2012;9:p. 14. doi: 10.1186/1479-5868-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shamseer L., Moher D., Clarke M., et al. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015: elaboration and explanation. BMJ. 2015;349(1) doi: 10.1136/bmj.g7647.g7647 [DOI] [PubMed] [Google Scholar]
- 46.Andrade J., Lotton J., Andrade J. Systematic review: frameworks used in school-based interventions, the impact on hispanic children’s obesity-related outcomes. Journal of School Health. 2018;88(11):847–858. doi: 10.1111/josh.12693. [DOI] [PubMed] [Google Scholar]
- 47.Academy of Nutrition and Dietetics. Evidence Analysis Manual: Steps in the Academy Evidence Analysis Process Academy of Nutrition and Dietetics Evidence Analysis Library. Chicago, IL, USA: Academy of Nutrition and Dietetics; 2016. https://www.andeal.org/vault/2440/web/files/2016_april_ea_manual.pdf. [Google Scholar]
- 48.Thomas J., Brunton J., Graziosi S. EPPI-Reviewer 4.0: Software for Research Synthesis. London, UK: EPPI; 2010. [Google Scholar]
- 49.Landis J. R., Koch G. G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 50.Parker K. B., Dejoy D. M., Wilson M. G., Bowen H. M., Goetzel R. Z. Application of the environmental assessment tool (EAT) as a process measure for a worksite weight management intervention. Journal of Occupational and Environmental Medicine. 2010;52(1):s42–s51. doi: 10.1097/JOM.0b013e3181ca3b37. [DOI] [PubMed] [Google Scholar]
- 51.Campbell M. K., Tessaro I., De Vellis B., et al. Effects of a tailored health promotion program for female blue-collar workers: health works for women. Preventive Medicine. 2002;34(3):313–323. doi: 10.1006/pmed.2001.0988. [DOI] [PubMed] [Google Scholar]
- 52.Fernandez I. D., Chin N. P., Devine C. M., et al. Images of a healthy worksite: a group-randomized trial for worksite weight gain prevention with employee participation in intervention design. American Journal of Public Health. 2015;105(10):2167–2174. doi: 10.2105/AJPH.2014.302397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.French S. A., Harnack L. J., Hannan P. J., Mitchell N. R., Gerlach A. F., Toomey T. L. Worksite environment intervention to prevent obesity among metropolitan transit workers. Preventive Medicine. 2010;50(4):180–185. doi: 10.1016/j.ypmed.2010.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Goetzel R. Z., Tabrizi M., Henke R. M., et al. Estimating the return on investment from a health risk management program offered to small Colorado-based employers. Journal of Occupational and Environmental Medicine. 2014;56(5):554–560. doi: 10.1097/JOM.0000000000000152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.LeCheminant J. D., Merrill R. M. Improved health behaviors persist over two years for employees in a worksite wellness program. Population Health Management. 2012;15(5):261–266. doi: 10.1089/pop.2011.0083. [DOI] [PubMed] [Google Scholar]
- 56.Lemon S. C., Wang M. L., Wedick N. M., et al. Weight gain prevention in the school worksite setting: results of a multi-level cluster randomized trial. Preventive Medicine. 2014;60:41–47. doi: 10.1016/j.ypmed.2013.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Leyk D., Rohde U., Hartmann N. D., Preuß P. A., Sievert A., Witzki A. Ergebnisse einer betrieblichen gesundheitskampagne: Wie viel kann man erreichen? Deutsches Aerzteblatt Online. 2014;111:320–327. doi: 10.3238/arztebl.2014.0320. [DOI] [Google Scholar]
- 58.MacKinnon D. P., Elliot D. L., Thoemmes F., et al. Long-term effects of a worksite health promotion program for firefighters. American Journal of Health Behavior. 2010;34(6):695–706. doi: 10.5993/ajhb.34.6.6. [DOI] [PubMed] [Google Scholar]
- 59.Merrill R. M., Merrill J. G. An evaluation of a comprehensive, incentivized worksite health promotion program with a health coaching component. International Journal of Workplace Health Management. 2014;7(2):74–88. doi: 10.1108/IJWHM-10-2012-0027. [DOI] [Google Scholar]
- 60.Merrill R. M., Bowden D. E., Aldana S. G. Factors associated with attrition and success in a worksite wellness telephonic health coaching program. Education for Health Change in Learning & Practice. 2010;23(3):p. 385. [PubMed] [Google Scholar]
- 61.Poole K., Kumpfer K., Pett M. The impact of an incentive-based worksite health promotion program on modifiable health risk factors. American Journal of Health Promotion. 2001;16(1):21–26. doi: 10.4278/0890-1171-16.1.21. [DOI] [PubMed] [Google Scholar]
- 62.Robroek S. J. W., Polinder S., Bredt F. J., Burdorf A. Cost-effectiveness of a long-term internet-delivered worksite health promotion programme on physical activity and nutrition: a cluster randomized controlled trial. Health Education Research. 2012;27(3):399–410. doi: 10.1093/her/cys015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Almeida F. A., Wall S. S., You W., et al. The association between worksite physical environment and employee nutrition, and physical activity behavior and weight status. Journal of Occupational and Environmental Medicine. 2014;56(7):779–784. doi: 10.1097/JOM.0000000000000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hollon S. D., Beck A. T. Cognitive and cognitive-behavioral therapies. In: Bergin A. E., Garfield S. L., editors. Handbook of Psychotherapy and Behavior Change. New York, NY, USA: Wiley; 1994. pp. 428–466. [Google Scholar]
- 65.Boerger N. L., Barleen N. A., Marzec M. L., Moloney D. P., Dobro J. The impact of specialized telephonic guides on employee engagement in corporate well-being programs. Population Health Management. 2018;21(1) doi: 10.1089/pop.2017.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kolbe-Alexander T. L., Proper K. I., Lambert E. V., et al. Working on wellness (WOW): a worksite health promotion intervention programme. BMC Public Health. 2012;12(1):p. 372. doi: 10.1186/1471-2458-12-372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kouwenhoven-Pasmooij T. A., Robroek S. J., Nieboer D., et al. Quality of motivational interviewing matters: the effect on participation in health-promotion activities in a cluster randomized controlled trial. Scandinavian Journal of Work, Environment & Health. 2018;44(4):414–422. doi: 10.5271/sjweh.3716. [DOI] [PubMed] [Google Scholar]
- 68.Lustria M. L. A., Cortese J., Noar S. M., Glueckauf R. L. Computer-tailored health interventions delivered over the web: review and analysis of key components. Patient Education and Counseling. 2009;74(2):156–173. doi: 10.1016/j.pec.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 69.Kreuter M. W., Bull F. C., Clark E. M., Oswald D. L. Understanding how people process health information: a comparison of tailored and untailored weight loss materials. Health Psychology. 1999;18(5):1–8. doi: 10.1037//0278-6133.18.5.487. [DOI] [PubMed] [Google Scholar]
- 70.Robroek S. J. W., Bredt F. J., Burdorf A. The (cost-)effectiveness of an individually tailored long-term worksite health promotion programme on physical activity and nutrition: design of a pragmatic cluster randomise controlled trial. BMC Public Health. 2007;7(259):1–11. doi: 10.1186/1471-2458-7-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Svetkey L. P., Stevens V. J., Brantley P. J., et al. Comparison of strategies for sustaining weight loss. JAMA. 2008;299(10):1139–1148. doi: 10.1001/jama.299.10.1139. [DOI] [PubMed] [Google Scholar]
- 72.Marchesini G., Montesi L., Ghoch M. E., Brodosi L., Calugi S., Dalle Grave R. Long-term weight loss maintenance for obesity: a multidisciplinary approach. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. 2016;9:p. 37. doi: 10.2147/DMSO.S89836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wadden T. A. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity. 2014;22(1):5–13. doi: 10.1002/oby.20662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.LeBlanc E., O’Connor E., Whitlock E., Patnode C., Kapka T. Effectiveness of primary care–relevant treatments for obesity in adults: a systematic evidence review for the U.S. preventive services task force. Annals of Internal Medicine. 2011;155(7):434–447. doi: 10.7326/0003-4819-155-7-201110040-00006. [DOI] [PubMed] [Google Scholar]
- 75.United States Department of Health & Human Services. Managing Overweight and Obesity in Adults. Washington, DC, USA: US Government Printing Office; 2013. [Google Scholar]
- 76.Blackford K., Jancey J., Howat P., Ledger M., Lee A. H. Office-based physical activity and nutrition intervention: barriers, enablers, and preferred strategies for workplace obesity prevention, Perth, Western Australia. Preventing Chronic Disease. 2012;10:p. e154. doi: 10.5888/pcd10.130029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Aparicio-Ugarriza R., Mielgo-Ayuso J., Benito P. J., Pedrero-Chamizo R., Ara I., González-Gross M. Physical activity assessment in the general population; Instrumental methods and new technologies. Nutrición Hospitalaria. 2015;31(s3):219–226. doi: 10.3305/nh.2015.31.sup3.8769. [DOI] [PubMed] [Google Scholar]
- 78.Stein R. J., Haddock C. K., Poston W. S. C., Catanese D., Spertus J. A. Precision in weighing : a comparison of scales found in physician offices, fitness centers, and weight loss centers. Public Health Reports. 2005;120:266–270. doi: 10.1177/003335490512000308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gorber S. C., Tremblay M., Moher D., Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index : a systematic review. Obesity Reviews. 2007;8:307–326. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- 80.Gokler M. E., Bugrul N., Sarı A. O., Metintas S. The validity of self-reported vs. measured body weight and height and the effect of self-perception. Archives of Medical Science. 2018;14(1):174–181. doi: 10.5114/aoms.2016.61401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yorkin M., Spaccarotella K., Martin-biggers J., Quick V., Byrd-bredbenner C. Accuracy and consistency of weights provided by home bathroom scales. BMC Public Health. 2013;13(1194):1–5. doi: 10.1186/1471-2458-13-1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Centers for Disease Control. Body Mass Index: Considerations for Practitioners. Washington, DC, USA: CDC; 2011. https://www.cdc.gov/obesity/downloads/BMIforPactitioners.pdf. [Google Scholar]
- 83.Dehghan M., Merchant A. T. Is bioelectrical impedance accurate for use in large epidemiological studies? Nutrition Journal. 2008;7(1):1–7. doi: 10.1186/1475-2891-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lee S. Y., Gallagher D. Assessment methods in human body composition. Current Opinion in Clinical Nutrition and Metabolic Care. 2008;11(5):566–572. doi: 10.1097/mco.0b013e32830b5f23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kyle U. G., Bosaeus I., De Lorenzo A. D., et al. Bioelectrical impedance analysis - Part II: utilization in clinical practice. Clinical Nutrition. 2004;23(6):1430–1453. doi: 10.1016/j.clnu.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 86.Lloret Linares C., Ciangura C., Bouillot J. L., et al. Validity of leg-to-leg bioelectrical impedance analysis to estimate body fat in obesity. Obesity Surgery. 2011;21(7):917–923. doi: 10.1007/s11695-010-0296-7. [DOI] [PubMed] [Google Scholar]
- 87.Wagner D. R., Heyward V. H. Techniques of body composition assessment: a review of laboratory and field methods. Research Quarterly for Exercise and Sport. 1999;70(2):135–149. doi: 10.1080/02701367.1999.10608031. [DOI] [PubMed] [Google Scholar]
- 88.McRae M. P. Male and female differences in variability with estimating body fat composition using skinfold calipers. Journal of Chiropractic Medicine. 2010;9(4):157–161. doi: 10.1016/j.jcm.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rutherford W. J. J., Gary A. Comparison of bioelectrical impedance and skinfolds with hydrodensitometry in the assessment of body composition in healthy young adults. Journal of Research. 2010;6(2):56–60. [Google Scholar]
- 90.Ketel I. J. G., Volman M. N. M., Seidell J. C., Stehouwer C. D. A., Twisk J. W., Lambalk C. B. Superiority of skinfold measurements and waist over waist-to-hip ratio for determination of body fat distribution in a population-based cohort of Caucasian Dutch adults. European Journal of Endocrinology. 2007;156(6):655–661. doi: 10.1530/EJE-06-0730. [DOI] [PubMed] [Google Scholar]
- 91.Mason C., Katzmarzyk P. T. Variability in waist circumference measurements according to anatomic measurement site. Obesity. 2009;17(9):1789–1795. doi: 10.1038/oby.2009.87. [DOI] [PubMed] [Google Scholar]
- 92.Johns D. J., Hartmann-Boyce J., Jebb S. A., Aveyard P. Diet or exercise interventions vs combined behavioral weight management programs: a systematic review and meta-analysis of directcom parisons. Journal of the Academy of Nutrition and Dietetics. 2014;114(10):1557–1568. doi: 10.1016/j.jand.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Anderson L. M., Quinn T. A., Glanz K., et al. The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity. A systematic review. American Journal of Preventive Medicine. 2009;37(4):340–357. doi: 10.1016/j.amepre.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 94.Balk E. M., Earley A., Raman G., Avendano E. A., Pittas A. G., Remington P. L. Combined diet and physical activity promotion programs to prevent type 2 diabetes among persons at increased risk: a systematic review for the community preventive services task force. Annals of Internal Medicine. 2015;163(6):437–451. doi: 10.7326/M15-0452. [DOI] [PMC free article] [PubMed] [Google Scholar]