Abstract
The recent discovery of the plasmid-mediated mcr-1 gene conferring resistance to colistin is of clinical concern. The worldwide screening of this resistance mechanism among samples of different origins has highlighted the urgent need to improve the detection of colistin-resistant isolates in clinical microbiology laboratories. Currently, phenotypic methods used to detect colistin resistance are not necessarily suitable as the main characteristic of the mcr genes is the low level of resistance that they confer, close to the clinical breakpoint recommended jointly by the CLSI and EUCAST expert systems (S ≤ 2 mg/L and R > 2 mg/L). In this context, susceptibility testing recommendations for polymyxins have evolved and are becoming difficult to implement in routine laboratory work. The large number of mechanisms and genes involved in colistin resistance limits the access to rapid detection by molecular biology. It is therefore necessary to implement well-defined protocols using specific tools to detect all colistin-resistant bacteria. This review aims to summarize the current clinical microbiology diagnosis techniques and their ability to detect all colistin resistance mechanisms and describe new tools specifically developed to assess plasmid-mediated colistin resistance. Phenotyping, susceptibility testing, and genotyping methods are presented, including an update on recent studies related to the development of specific techniques.
1. Introduction
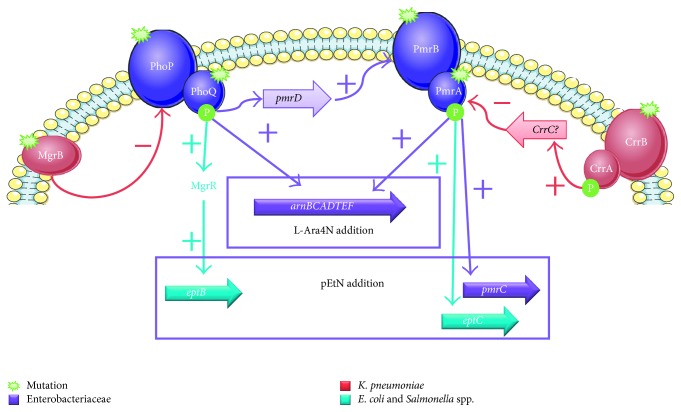
Multidrug-resistant (MDR) bacteria are of a global concern, notably with the description of carbapenemase-producing Enterobacteriaceae [1]. Colistin is an old antibiotic that regained popularity as a last resort treatment to face the worldwide emergence of these pathogens [2]. Colistin is a polycationic and bactericidal drug that targets the lipid A moiety of lipopolysaccharide (LPS), moving its cationic charges, leading to cell wall lysis and bacterial death [3]. The increasing use of colistin has led to emerging resistance, a phenomenon that represents a clinical source of worry [4]. Enterobacteriaceae are Gram-negative bacteria that are often described as the pathogens responsible for human infectious diseases, particularly the Escherichia coli and Klebsiella pneumoniae species. Until recently, all mechanisms described were of chromosomal origin, mostly mediated by the two-component systems PmrAB and PhoPQ, leading to the addition of positively charged carbohydrates on the negatively charged lipid A (Figure 1), a phosphoethanolamine by a phosphoethanolamine transferase or a 4-amino-4-arabinose by surexpression of arnBCADTEF operon, leading to the loss of polymyxin affinity for the LPS [5]. In November 2015, Liu et al. reported the first plasmid-mediated gene which they named mcr-1 [6], which encodes for a phosphoethanolamine transferase, and this was followed by the description of variants (mcr-1.2, mcr-1.3,…) and the genes mcr-2, mcr-3, mcr-4, mcr-5, mcr-6, mcr-7, and mcr-8 [7–15]. This recent discovery raised concern about the increase and spread of resistance among the Enterobacteriaceae [16] and led to new recommendations for laboratory diagnosis and clinicians [17]. Specifically, the majority of these mcr-1 strains exhibited a low minimal inhibitory concentration (MIC) of colistin, around 4 µg/ml [6], which is close to the MIC breakpoint according to the EUCAST guidelines (susceptibility ≤ 2 µg/ml and resistance > 2 µg/ml) (http://www.eucast.org). Moreover, several studies have reported the detection of the mcr-1 gene in carbapenemase-producing Enterobacteriaceae strains, describing coproduction with other plasmid-mediated genes (bla NDM-1, bla NDM-5, bla NDM-9, bla KPC-2, bla KPC-3, bla OXA-48, and bla OXA-181) [18–24].
Figure 1.
Molecular mechanisms of acquired resistance to polymyxins. L-Ara4N: 4-amino-4-arabinose; pEtN: phosphoethanolamine.
The emergence of antibiotic resistance of clinical interest usually conduces to the development of new tools in clinical microbiology laboratories [25]. Currently, the detection of carbapenemase-producing bacteria is well determined, combining specific culture media, phenotyping testing, antibiotic susceptibility testing, and molecular biology [26–28]. As colistin resistance is a recent global phenomenon, the implementation of rapid and reliable screening tools to detect and analyze colistin-resistant pathogens in such a way as to isolate the patient and adapt the treatment is a necessary approach [29]. Moreover, heteroresistance to colistin is a common phenomenon that is widely underestimated, requiring specific methods [30–32]. Here, we propose an overview of all the screening and analysis methods developed to assess colistin resistance among bacterial pathogens causing infectious diseases in hospitalized patients. This review summarizes the current clinical microbiology diagnosis techniques and their ability to detect all colistin resistance mechanisms, and describes new tools specifically developed to assess plasmid-mediated colistin resistance [33].
Phenotyping, susceptibility testing, and genotyping methods are presented, including an update on recent studies related to the development of specific techniques.
2. Phenotypic Detection Methods
2.1. Selective Culture Media
Culture remains the benchmark method for isolating pathogens within clinical samples, and selective media are continuously developed to isolate specific bacteria [25]. Until recently, there was no specific culture medium for the detection of colistin-resistant strains, and current polymyxin-containing culture media were not able to detect low-level resistant strains because the concentrations of polymyxin in their composition are too high or because they contain other antimicrobial drugs [34–61] (Table 1). Therefore, some in-house media have been developed for colistin-resistant strain screening studies, including strains carrying the mcr genes (Supplementary Table S1). These selective culture media were developed by adding low concentrations of colistin (2 or 4 mg/L) to LB nonselective agar or a MacConkey medium, which is selective of Gram-positive contaminants [62, 63]. The chromogenic and nonselective CHROMagar Orientation medium (Biomérieux, Marcy l'Étoile, France) was also used with 4 mg/ml of colistin [64]. They were used in studies to detect the growth of colistin-resistant isolates by directly culturing samples [65–67] or following an enrichment step [68] which could also be selective with the addition of 2 mg/L of colistin to the broth medium [62, 64, 69]. Other anti-infective drugs could be added to avoid contaminants: vancomycin for Gram-positive contaminants [64, 66, 68] and/or amphotericin B for fungal pathogens [67, 68]. For some other studies, such media were developed to screen colistin resistance in bacterial isolates by subculturing them on agar with 2 mg/L of colistin: MH agar [9], COS medium [70], or MacConkey medium [65]. Wong et al. named their medium MHC1 for Mueller–Hinton colistin 1 [71]. Lastly, the selective CNA medium (colistin and nalidixic acid-containing agar), containing 10 mg/L of colistin, could detect mcr-1-positive isolates, one E. coli [72] and one K. pneumoniae [73], and was also used with CLED (cysteine lactose electrolyte deficient) medium (BioMérieux, Marcy l'Étoile, France) for screening samples that had or had not been precultured on Trypticase Soy Broth ±2 mg/L of colistin [74].
Table 1.
Composition of polymyxin-containing agar.
| Targeted bacteria | Culture medium | Antibiotics (µg/mL) targeting | References | |||
|---|---|---|---|---|---|---|
| Gram-negative strains | Gram-positive strains | Yeast | ||||
| Polymyxins | Others | |||||
| Colistin-resistant Gram-negative strains | LBJMRa | 4 (C) | Vancomycin 50 | |||
| VancoR Gram-positive strains | ||||||
| Gram-negative strains | ||||||
| Colistin-resistant | SuperPolymyxin | 3.5 (C) | Daptomycin 10 BM 65 Éosine 400 |
5 (AB) | [75] | |
| Neisseria sp. | Martin–Lewis agar | 7.5 (C) | 5 (T) | Vancomycin 4 | 20 (A) | [34] |
| Thayer–Martin agar | 7.5 (C) | Vancomycin 3 | 2.57 (N) | [35] | ||
| MTMb agar | 7.5 (C) | 5 (T) | Vancomycin 3 | 2.57 (N) | [36] | |
| NYCc agar | 7.5 (C) | 3 (T) | Vancomycin 2 | 20 (A) | [37] | |
| Burkholderia cepacia | Cepacia medium | 30 (B) | Ticarcillin 100 | [38] | ||
| OFPBLd agar | 30 (B) | Bacitracin 3 | [39] | |||
| Burkholderia cepacia agar | 17.8 (B) | 5 (GEN) | Ticarcillin 100 | [38] | ||
| Burkholderia cepacia selective agar | 71.4 (B) | 10 (GEN) | Vancomycin 2.5 | [40] | ||
| Legionella sp. | BCYEe selective agar with | |||||
| GVPCf | 9.4 (B) | Glycine 3000 | Vancomycin 1 | 80 (CH) | [41] | |
| CCVCg | 16 (C) | Vancomycin 0.5 Cefalotin 4 |
80 (CH) | [42] | ||
| GPVAh | 11.9 (B) | Glycine 3000 | Vancomycin 1 | 80 (A) | [43] | |
| PAVi | 4.76 (B) | Vancomycin 0.5 | 80 (A) | [44] | ||
| PACj | 9.52 (B) | Cefamandole 2 | 80 (A) | [45] | ||
| DGVPk | 8 (B) | Glycine 3000 | Vancomycin 1 | [46] | ||
| Campylobacter sp. | Campylobacter agar | |||||
| Butzler | 0.33 (C) | Bacitracin 338 | Novobiocin 5 Cefazolin 15 |
50 (CH) | [47] | |
| Skirrow | 0.25 (B) | 2.5 (T) | Vancomycin 5 | [48] | ||
| Blaser–Wang | 0.125 (B) | 2.5 (T) | Vancomycin 5 Cefalotin 15 |
2 (AB) | [49] | |
| Preston | 0.125 (B) | 5 (T) | Rifampicin 5 | 50 (CH) | [50] | |
| Brucella spp. | Brucella selective medium | 1 (B) | Bacitracin 500 | 100 (CH) | [51] | |
| Vibrio sp. | CPCl | 66.34 (C) 11.9 (B) |
[52] | |||
| Gram-positive strains | ||||||
| Streptococcus sp. and Gram-positive strains | ANCm | 10 (C) | Nalidixic acid 10 | [53] | ||
| Listeria monocytogenes | Oxford medium | 20 (C) | Fosfomycin 10 | Cefotetan 2 Acriflavine 5 |
400 (CH) | [54] |
| Modified Oxford | 10 (C) | Moxalactam 15 | [55] | |||
| Listeria spp. | PALCAMn | 10 (B) | Ceftazidime 8 Acriflavine 5 |
[56] | ||
| Bacillus cereus | MYPo | 10 (B) | [57] | |||
| Mycobacteriaceae | Middlebrook 7H11 | 25 (B) | 20 (T) | Carbenicillin 50 | 10 (AB) | [58] |
| Clostridium perfringens | SPSp agar | 10 (B) | Sulfadiazine 120 | [59] | ||
| TSNq agar | 20 (B) | Neomycin 50 | [60] | |||
| SFPr agar | 3.57 (B) | Kanamycin 12 | [61] | |||
B: polymyxin B; C: colistin; AB: amphotericin B; A: anisomycin; CH: cycloheximide; MB: methylene blue; N: nystatin; GEN: gentamicin; T: trimethoprim. aLBJMR: Lucie Bardet–Jean-Marc Rolain; bMTM: modified Thayer–Martin; cNYC: New York City; dOFPBL: oxidation/fermentation, polymyxin B, bacitracin, and lactose; eBCYE: buffered charcoal and yeast extract; fGPVC: glycine, polymyxin B, vancomycin, and cycloheximide; gCCVC: cefalotin, colistin, vancomycin, and cycloheximide; hGPVA: glycine, polymyxin B, vancomycin, and anisomycin; iPAV: polymyxin B, anisomycin, and vancomycin; jPAC: polymyxin B, anisomycin, and cefamandole; kDGVP: dyes, glycine, vancomycin, and polymyxin B; lCPC: cellobiose, polymyxin B, and colistin; mCNA: colistin and nalidixic acid; nPALCAM: polymyxin B, acriflavine, lithium, ceftazidime, esculin, and mannitol; oMYP: mannitol, egg yolk, and polymyxin B; pSPS: sulfite, polymyxin B, and sulfadiazine, qTSN: trypticase, sulfite, and neomycin; rSFP: Shahidi-Ferguson perfringens.
More specifically, the SuperPolymyxin medium (Elitech Microbio, Signes, France) was developed and intended to specifically detect colistin-resistant strains, including those with a low MIC of colistin and harboring the mcr-1 gene [75]. The SuperPolymyxin medium has the advantage of facilitating the visualization of E. coli strains because it is composed of EMB agar, meaning that they exhibit a metallic green reflect. Its specificity is enabled by 3.5 µg/ml of colistin, 10 µg/ml of daptomycin, and 5 µg/ml of amphotericin B in its composition.
The CHROMagar COL-APSE medium was also developed to detect colistin-resistant strains and was compared to the SuperPolymyxin [76]. Its composition is not precisely described, based on commercial CHROMagar compounds containing colistin sulfate and oxazolidonone antibiotics. The CHROMagar COL-APSE medium presents the advantage to be chromogenic, with the capacity to differentiate colistin-resistant nonfermentative Gram-negative strains as well as Enterobacteriaceae.
The LBJMR medium was also developed to detect all the colistin-resistant bacteria, including those harboring mcr-1 genes [77]. The LBJMR medium presents the advantage of being versatile, combining colistin-resistant and vancomycin-resistant bacteria screening tools, conferred by 4 µg/ml of colistin sulfate and 50 µg/ml of vancomycin. In particular, the LBJMR medium can be used to detect vancomycin-resistant enterococci (VRE), which represents another emerging field of clinical concern. Both colistin-resistant Enterobacteriaceae and VRE strains are easy to detect on the LBJMR medium with the presence of bromocresol purple and glucose: fermentative strains exhibit yellow colonies on a purple agar. Lastly, it can be used to specifically detect pathogens that are often diagnosed in cystic fibrosis patient samples.
The sensitivities of these three media were excellent to detect colistin-resistant strains.
2.2. Qualitative Detection of Colistin Resistance with Phenotypic Tests
2.2.1. Rapid NP Polymyxin Test for Enterobacteriaceae
The rapid polymyxin NP test (Elitech, Signes, France) is based on a simple pH test, and detection of colistin resistance is obtained by a color change within 2 hours [78, 79]. The test was evaluated on 200 isolates of Enterobacteriaceae and can be used directly on blood samples [80]. A recent review proposed a diagnosis plan integrating this phenotypic test to confirm colistin resistance of Enterobacteriaceae strains after their growth on a selective medium [29], and its reliability is discussed in several studies [81, 82]. Compared to the broth microdilution (BMD) susceptibility testing method, agreements were excellent to detect mcr-1 and mcr-2 strains [83, 84]. The rapid polymyxin test has a good sensitivity to detect Hafnia sp. colistin-resistant isolates [79] but failed to detect Enterobacter sp. isolates, surely due to their heteroresistance to colistin [85]. This test has to be evaluated with nonfermentative colistin-resistant strains, such as Acinetobacter baumannii and Pseudomonas aeruginosa.
2.2.2. Micromax Assay for A. baumannii
The Micromax assay (Halotech DNA SL, Madrid, Spain) is based on the detection of DNA fragmentation and cell wall damage in the presence of colistin [86]. Bacteria are incubated for 60 min with 0.5 µg/ml of colistin, trapped in a microgel, and then incubated with a lysis solution to remove weakened cell walls. The presence of DNA fragments is detected after staining by SYBR Gold fluorochrome and observed by fluorescence microscopy. Resistance corresponds to ≤11% of bacteria with cell wall damage. This method is rapid (3 h 30 min) and showed an excellent sensitivity for the detection of colistin resistance on the 70 A. baumannii tested isolates (50 susceptible and 20 resistant), but it is not specific for determining the resistance type.
2.3. Specific Phenotypic Screening Methods for the Detection of MCR-1
2.3.1. Matrix-Assisted Laser Desorption-Ionization Time-of-Flight Mass Spectrometry (MALDI-TOF MS)
The detection of polymyxin-resistant bacteria by MALDI-TOF is a promising and costless approach, as the majority of clinical microbiology laboratories own the required equipment to routinely identify clinical isolates [87]. Currently, the use of MALDI-TOF for detecting the carbapenemase-producing bacteria is described, with the detection of carbapenem hydrolysis [88–90]. As a specific peak was described for lipid A at 1796.2 m/z [91], the MALDI-TOF could be used for the detection of lipid A modifications [92]. Very recently, the MALDIxin test was developed for E. coli strains, based on the detection of phosphoethanolamine addition on lipid A, and could specifically detect the mcr-positive isolates [93]. Indeed, an additional peak at 1919.2 m/z was observed for all polymyxin-resistant strains, and a second additional peak at 1821.2 m/z was observed for all the mcr-positives. The MALDIxin test could detect polymyxin-resistant E. coli and also differentiate the chromosome- and plasmid-encoded resistance in 15 minutes, and should be evaluated on other species for which phosphoethanolamine addition is involved in polymyxin resistance.
2.3.2. Inhibition of MCR-1 Activity
Several studies on the structure of the catalytic domain of the MCR-1 protein have demonstrated that the phosphoethanolamine transferase is a zinc metalloprotein [94–96], and that zinc deprivation could reduce the colistin MIC in E. coli isolates [97]. Screening tests were developed to specifically detect MCR-1, based on the difference of colistin susceptibility obtained in the presence or absence of chelators of zinc ion.
The colistin-MAC test consists of the addition of dipicolinic acid (DPA) in the BMD method, leading to a colistin MIC reduction of ≥ 8-fold in case of MCR-1-positive strain [98]. 74 colistin-resistant Enterobacteriaceae strains were tested, and 59 of the 61 strains carrying mcr-1-like genes were detected by the colistin-MAC test, while the 13 mcr-negative strains exhibited discrepancy in results (increase, maintain, or slow decrease) giving a sensitivity of 96.7% and specificity of 100%. Interestingly, the two mcr-1 strains that were negative with the colistin-MAC test were K. pneumoniae strains.
More recently, four assays were tested, based on inhibition by EDTA [99]. The specific detection of MCR-1 was assessed with the following tests: combined-disk method with diameter differences ≥3 mm, BMD with a reduction of colistin MIC of ≥4-fold, modified rapid polymyxin NP test with the absence of color change, and the alteration of zeta potential R ZP ≥ 2.5. These assays were performed on 109 Enterobacteriaceae including 59 mcr-1-positive E. coli and one mcr-1-positive K. pneumoniae. The modified rapid NP test and zeta potential methods showed excellent sensitivity and specificity and could be inexpensive and simple methods to detect the presence of the mcr-1 gene.
These tests should be performed on other species harboring the mcr-1 gene, in particular K. pneumoniae, and also on strains harboring other mcr genes, to validate their ability.
3. New Recommendations on Polymyxins Susceptibility Testing
Polymyxin susceptibility testing is challenging, as these large and cationic molecules poorly diffuse into the reference cation-enriched Mueller-Hinton (MH2) agar, giving discrepant results, and much more since the description of the mcr genes that confer low MICs. Moreover, even in MH2 broth medium, the concentration of cation could largely influence the polymyxin MIC results [64], notably by interacting with the acquired resistance mechanisms of the tested isolates. Defining a reference method for colistin susceptibility testing is a priority, along with the increasing use of polymyxin as last-line therapies.
3.1. Reference Method
Broth microdilution (BMD) is the only approved method for colistin MIC determination by both the European Committee on Antibiotic Susceptibility Testing (EUCAST) and the Clinical and Laboratory Standards Institute (CLSI) [100, 101]. BMD has to be performed with colistin sulfate in untreated polystyrene plates without addition of any surfactant (polysorbate 80) (Table 2). The Mueller–Hinton broth medium has to be cation-adjusted, with a final composition of 20–25 mg/L of calcium and 10–12.5 mg/L of magnesium [102]. EUCAST and CLSI joined their recommendations on the polymyxin breakpoint for MIC of Enterobacteriaceae, P. aeruginosa and Acinetobacter spp. isolates: susceptible (S) if ≤2 µg/ml and resistant (R) if >2 µg/ml [100, 103]. In 2017, EUCAST added a new quality control (QC) strain that has to be used to control the performances of a colistin susceptibility method: E. coli NCTC 18853 that harbors the mcr-1 gene, in addition to E. coli ATCC 25922 and P. aeruginosa ATCC 27853 [104] (Table 2).
Table 2.
Joint EUCAST-CLSI recommendations on colistin susceptibility testing.
| Reference method | Broth microdilution | ||
|---|---|---|---|
| Preparation according to ISO 20776-1 standard [102] | (i) Cation-adjusted Mueller-Hinton medium (MH2) | ||
| (ii) Colistin sulfate | |||
| (iii) Polystyrene trays without pretreatment | |||
| (iv) Absence of polysorbate 80 or any surfactant | |||
|
| |||
| MIC breakpoint (µg/ml) | Enterobacteriaceae | P. aeruginosa | Acinetobacter spp. |
| EUCAST [100] | S ≤ 2 and R > 2 | S ≤ 2 and R > 2 | S ≤ 2 and R > 2 |
| CLSI [103] | ECV∗: WT ≤ 2 and NWT ≥4 | S ≤ 2 and R ≥ 4 | S ≤ 2 and R ≥ 4 |
|
| |||
| Quality control [104] (µg/ml) | E. coli ATCC 25922 | P. aeruginosa ATCC 27853 | E. coli (mcr-1) NCTC 18853# |
| Target | 0.5–1 | 1–2 | 4 |
| Range | 0.25–2 | 0.5–4 | 2–8 |
∗Epidemiological cutoff values: clinical data and PK/PD are not sufficient to evaluate a clinical breakpoint for the following species: E. aerogenes, E. cloacae, E. coli, K. pneumoniae, and R. ornithinolytica. WT: wild type; NWT: non-wild type. #Recommended by EUCAST; MIC must be 4 µg/ml and only occasionally 2 or 8 µg/ml.
Dilution methods consist of adding colistin to the culture medium in such a way as to obtain twofold dilutions and are prepared according to the CLSI guide M07-A10 [101] and ISO 20776-1 standard (International Standard Organization). Broth macrodilution is performed in tubes when reference broth microdilution (BMD) is performed in 96-well trays. Only colistin sulfate can be used and particular care is required, as the powder is expressed in IU/mg, meaning that the concentrations need to be adjusted according to the CLSI M100 and the manufacturer's instructions [103]. The antibiotic is suspended in sterile water and then diluted in MH2 broth medium before its distribution into 96-well trays. The final bacterial inoculum is 5 × 105 CFU/ml (colony-forming unit) or 5 × 104 CFU/well for the BMD method, prepared using the 0.5 McFarland standard (corresponding to approximately 1 to 2 × 108 CFU/ml) [101]. Trays are then incubated at 35 ± 1°C for 18 ± 2 hours [100, 102]. Results are read visually or with a spectrophotometer.
Broth microdilution is a time-consuming and fastidious way to assess MIC in clinical routines [105, 106]. Many errors can occur, such as an incorrect colistin concentration or dilution. This technique is not well suited to clinical microbiology routines and needs to be automated. Moreover, this method exhibits limitations for assessing heteroresistance. Indeed, the presence of resistant subpopulations can give uninterpretable results due to the presence of skipped wells and has been described for the Enterobacter species, as presented in a study of 114 Enterobacter cloacae [107]. Population analysis profiling is recommended to confirm heteroresistance [108]. For now, heteroresistance to polymyxins is not correlated with the presence of mcr genes.
3.2. Comparative Evaluations of Polymyxin Susceptibility Testing Methods
Evaluating antimicrobial susceptibility testing (AST) methods is performed using a comparison with the reference method, as per the ISO 20776-2 standard [109]: a categorical agreement (CA) is obtained when the strain is in the same clinical category (R, I, S), and an essential agreement (EA) is obtained when the MIC is within plus or minus one doubling dilution from the reference MIC. A very major error (VME) corresponds to a false susceptibility result and is calculated using the resistant strains tested, and a major error (ME), in the case of false resistance, is calculated on the number of susceptible strains. Finally, a minor error (MiE) occurs when a strain is classified as Intermediate (I) instead of S or R, or S or R instead of I. A reliable method will obtain the following scores: CA ≥ 90%, EA ≥ 90%, VME ≤ 3%, and ME ≤ 3% [109]. The results of all the comparative studies performed on colistin susceptibility testing are summarized in Table 3 (in Table S2 for polymyxin B). MIC50 and MIC90 correspond to the MIC that inhibits 50 or 90%, respectively, of the tested strains of the same species.
Table 3.
Comparison of different colistin susceptibility testing methods to detect colistin resistance in Gram-negative clinical isolates.
| Bacterial species | Reference method | MIC breakpoint | MIC range; % resistant | MIC50 (µg/ml) | MIC90 (µg/ml) | Methods | CA ≥ 90% | EA ≥ 90% | ME ≤ 3% | VME ≤3% | MiE | References |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 42 A. baumannii isolates | BMD | S ≤ 2 µg/ml | 0.5–4 µg/ml | 1 µg/ml | 2 µg/ml | BMD in glass-coated plates | 92.8 | 100 | 0 | 100 | [114] | |
| AD | 78.5 | 92.8 | 15.4 | 100 | ||||||||
| R > 2 µg/ml | 0.07% | E-test | 92.8 | 16.6 | 0 | 100 | ||||||
| Vitek 22 AST-N2812 | 92.8 | 61.9 | 0 | 100 | ||||||||
|
| ||||||||||||
| 353 isolates | BMD | S ≤ 2 µg/ml | ND | ND | ND | Sensitest | 98.9 | 96 | 1.46 | 0.93 | [146] | |
| (83 mcr-1) | R > 2 µg/ml | 38.8% | ||||||||||
|
| ||||||||||||
| 219 isolates | S ≤ 2 µg/ml | ND | ND | ND | Phoenix 1003 NMIC-417 | 96.8 | ND | 0.6 | 10 | [146] | ||
| R > 2 µg/ml | 27.4% | |||||||||||
|
| ||||||||||||
| 14 E. coli isolates | BMD | S ≤ 2 µg/ml | 0.25–128 µg/ml; 48% | 2 | 16 | Sensititre1 SEMPA1 | 94.7 | 96 | 10.2 | 0 | [143] | |
| 18 K. pneumoniae isolates | R > 2 µg/ml | Micronaut-S | 89.3 | 96 | 15.4 | 5.6 | ||||||
| 21 P. aeruginosa isolates | Micronaut-MIC | 90.7 | 99 | 12.8 | 5.6 | |||||||
| 22 Acinetobacter spp. isolates | Etest, Oxoid MH | 81.3 | 71 | 5.1 | 33.3 | |||||||
| Etest, BBL MH | 78.7 | 43 | 2.6 | 41.7 | ||||||||
| Etest, MHE | 85.3 | 47 | 5.1 | 25 | ||||||||
| MTS, Oxoid MH | 78.7 | 40 | 0 | 44.4 | ||||||||
| MTS, BBL MH | 76 | 49 | 0 | 50 | ||||||||
| Sensitest | 89.3 | 88 | 17.9 | 2.8 | ||||||||
| UMIC | 92 | 82 | 7.7 | 8.3 | ||||||||
|
| ||||||||||||
| 117 A. baumannii isolates | BMD | S ≤ 2 µg/ml | ≤0.5–≥16 µg/ml; 24.8% | ≤0.5 | 8 | Vitek 2 AST-XN05 | 89.7 | 88.9 | 1.1 | 37.9 | [129] | |
| R > 2 µg/ml | Phoenix 100 NMIC/ID-96 | 88.9 | 91.5 | 1.1 | 41.4 | |||||||
| AD | 87.2 | 93.2 | 15.9 | 3.4 | ||||||||
|
| ||||||||||||
| 123 Enterobacteriaceae isolates (14 mcr-1 and 1 mcr-2) | BMD | S ≤ 2 µg/ml | 0.12–128 µg/ml; 67.5% | Phoenix 100 NMIC-93 | 91.8 | ND | 0 | 12.1 | [83] | |||
| R > 2 µg/ml | Rapid NP | 98.3 | NA | 2.5 | 1.2 | |||||||
|
| ||||||||||||
| 15 Hafnia alvei isolates | BMD | S ≤ 2 µg/ml | 0.125–32 µg/ml; 96% | 8 | 16 | DD | 4 | NA | 0 | 100 | [79] | |
| 10 Hafnia paralvei isolates | R >2 µg/ml | 8 | 8 | Etest | 76 | 32 | 0 | 25 | ||||
| Phoenix NMIC-93 | 100 | NA | 0 | 0 | ||||||||
| Rapid NP | 100 | NA | 0 | 0 | ||||||||
|
| ||||||||||||
| 76 Enterobacteriaceae isolates (21 mcr-1) | BMD | S ≤ 2 µg/ml | 0.06–>64 µg/ml; 32.9% | 0.25 | 16 | Vitek 2 AST N315 | 88.2 | 93.9 | 0 | 36 | [147] | |
| R >2 µg/ml | 2 (4) | 8 (8) | Sensititre GNX3F | 90.1 | 89.5 | 11.8 | 4 | |||||
| 0.12 | 0.5 | Etest | 92.1 | 75 | 5.9 | 12 | ||||||
| MicroScan4 NM44 | 88.2 | NA | 15.8 | 4 | ||||||||
|
| ||||||||||||
| 246 isolates (absence of mcr genes) | Broth macrodilution | S ≤ 2 µg/ml | ≤0.5–>8 µg/ml; 12.6% | ≤0.5 | 8 | Etest | 95.1 | 92.3 | 0.4 | 35.5 | [160] | |
| R >2 µg/ml | ||||||||||||
|
| ||||||||||||
| 41 K. pneumoniae isolates | BMD | S ≤ 2 µg/ml | 2–>128 µg/ml; 95.1% | 8 | 32 | BMD-P80 | 82 | 95.1 | 0 | 18.9 | NA | [110] |
| 20 A. baumannii isolates | R > 2µg/ml | 8 | 32 | AD | 91.8 | 55.7 | 100 | 3.4 | ||||
| Etest | 59 | 50.8 | 33.3 | 39.3 | ||||||||
| MTS | 67.2 | 65.6 | 33.3 | 41.4 | ||||||||
| Vitek 2 AST EXN8 | 96.7 | 70 | 66.6 | 0 | ||||||||
|
| ||||||||||||
| 290 A. baumannii isolates | BMD | S ≤ 2 µg/ml | 1–128 µg/ml; 9.3% | 2 | 2 | DD 10 µg (9–12 mm) | 94.8 | NA | 0 | 0 | 5.2 | [136] |
| R > 2 µg/ml | Etest S ≤ 2; R > 4 | 94.5 | 2.1 | 0 | 55.5 | 0 | ||||||
| Etest S ≤ 0.5; R > 2 | 99.3 | ≡ | 0 | 0 | 5.5 | |||||||
| Vitek 2 AST-N136 | 94.1 | 44.8 | 0.38 | 59.2 | ||||||||
|
| ||||||||||||
| 213 Acinetobacter sp. isolates | AD | S ≤ 2 µg/ml | ≤0.5–≥32 µg/ml; 6.1% | 1 | 2 | Vitek 2 AST-N132 | 99.1 | ND | 0 | 15.4 | [115] | |
| R >2 µg/ml | Etest | 87.3 | 1 | 0 | ||||||||
| MicroScan panel type 42 | 99.1 | 12.5 | 15.4 | |||||||||
|
| ||||||||||||
| 60 P. aeruginosa isolates | BMD-P80 | S ≤ 2 µg/ml | ≤0.12–≥8 µg/ml; 17.8% | Broth macrodilution | 98 | 83 | 2.3 | 0 | [128] | |||
| 20 K. pneumoniae isolates | R >2 µg/ml | >8 | Etest | 91 | 61 | 4.5 | 31.6 | |||||
| 27 A. baumannii isolates | >8 | |||||||||||
|
| ||||||||||||
| 11 A. baumannii isolates | BMD-P80 | S ≤ 2 µg/ml | ≤0.12–≥8 µg/ml; 20% | >8 | BMD | 88 | 34∗ | 12.5 | 10 | [128] | ||
| 15 K. pneumoniae isolates | R >2 µg/ml | >8 | AD | 94 | 80 | 7.5 | 0 | |||||
| 24 P. aeruginosa isolates | Sensititre GNXF | 96 | 62∗ | 5 | 0 | |||||||
|
| ||||||||||||
| 11 A. baumannii isolates | BMD-P80 | S ≤ 2 µg/ml | ≤0.12–≥8 µg/ml; 30% | Etest, BBL MH | 78 | 46 | 5.7 | 47 | [128] | |||
| 15 K. pneumoniae isolates | R > 2 µg/ml | Etest, Hardy MH | 78 | 64 | 2.8 | 53 | ||||||
| 24 P. aeruginosa isolates | >8 | Etest, Remel MH | 84 | 68 | 2.8 | 47 | ||||||
|
| ||||||||||||
| 109 P. aeruginosa isolates | BMD | S ≤ 2 µg/ml | 0% | Phoenix NMIC/ID-76 | 100 | 99.1 | 0 | 0 | [149] | |||
| R >2 µg/ml | ||||||||||||
|
| ||||||||||||
| 63 E. coli isolates | BMD | S ≤ 2 µg/ml | 0.12–16 µg/ml; 18.6% | 1 | BMD-P80 | 99.2 | 41.3 | 0 | 43.5 | [112] | ||
| 61 K. pneumoniae isolates | R >2 µg/ml | 0.5 | ||||||||||
| 60 Acinetobacter spp. isolates | 2 | |||||||||||
| 63 P. aeruginosa isolates | 2 | |||||||||||
|
| ||||||||||||
| 200 Enterobacteriaceae isolates | AD | S ≤ 2 µg/ml | 0.128–>128 µg/ml; 28.5% | DD 50 µg; R < 15 mm | 96.5 | NA | 0 | 12.3 | [116] | |||
| 82 K. pneumoniae isolates | R > 2 µg/ml | 0.5 | 128 | DD 10 µg; R ≤ 8; S ≥ 11 mm | 93 | NA | 0 | 8.8 | 4.5 | |||
| 51 E. coli isolates | 0.5 | 0.5 | DD 10 µg; R ≤ 11; S ≥ 14 mm | 99.5 | NA | 0 | 1.7 | 26.5 | ||||
| 67 E. cloacae isolates | 0.5 | 2 | Etest | 100 | 52 | 0 | 0 | 0 | ||||
|
| ||||||||||||
| 25 P. aeruginosa isolates | AD | S ≤ 2 µg/ml | 0.25–≥256 µg/ml; 57.1% | 2 | >256 | BMD | 81.1 | 40.5 | 0 | 25 | 5.4 | [120] |
| 12 S. maltophilia isolates | R > 4 µg/ml | >256 | >256 | Etest | 74.3 | 56.7 | 0 | 35 | 11.4 | |||
| DD 10 µg; R ≤ 10; S ≥ 11 mm | 82.8 | NA | 0 | 35 | 2.9 | |||||||
|
| ||||||||||||
| 157 E. coli isolates | AD | S ≤ 2 µg/ml | 0.25–32 µg/ml; 9.6% | 0.5 | 2 | DD 150 µg; R < 16; S ≥ 20 mm | 46.5 | NA | 1.4 | 20 | 49.7 | [123] |
| R >4 µg/ml | DD 10 µg; 2 + 18H∗ (10–15) | 96.8 | NA | 0.7 | 13.3 | 1.9 | ||||||
| Etest | 96.8 | 81.5 | 0.7 | 0 | 0.6 | |||||||
|
| ||||||||||||
| 78 P. aeruginosa isolates | BMD | S ≤ 2 µg/ml | <0.25–2 µg/ml; 0 | 1 | 1 | Etest | 100 | 79.5 | 0 | 0 | 6.4 | [135] |
| R > 4 µg/ml | DD 10 µg | 100 | NA | |||||||||
|
| ||||||||||||
| 100 A. baumannii isolates | Phoenix | S ≤ 2 µg/ml | 0.5 | 0.5 | DD 10 µg; R ≤ 8; S ≥ 11 mm | 100 | NA | 0 | 0 | [137] | ||
| R > 4 µg/ml | Etest | 100 | NA | 0 | 0 | |||||||
|
| ||||||||||||
| 154 Acinetobacter spp. isolates | AD | S ≤ 2 µg/ml | ≤0.064–≥32; 11.7% | NA | NA | Etest | 98.7 | 88 | 0.7 | 5.6 | [124] | |
| R ≥ 4 µg/ml | ||||||||||||
|
| ||||||||||||
| 170 Gram-negative isolates | AD | S ≤ 4 µg/ml | 0.25–128; 31.2% | Etest | 100 | 91.2 | 0 | 0 | [126] | |||
| R > 4 µg/ml | ||||||||||||
|
| ||||||||||||
| 102 Gram-negative isolates | BMD | S ≤ 2 µg/ml | <0.5–>64 µg/ml; 50% | NA | NA | AD, Oxoid MH | ND | 96.8 | [31] | |||
| R > 4 µg/ml | AD, Oxoid Iso-Sensitest | 97.9 | ||||||||||
| Etest, MH | 72.6 | |||||||||||
| Etest, ISO | 64.2 | |||||||||||
| Vitek 2 AST N038 | 93.1 | |||||||||||
| DD 10 µg; R ≤ 10; S ≥ 13 mm | NA | |||||||||||
|
| ||||||||||||
| 44 Acinetobacter spp. isolates | AD | S ≤ 2 µg/ml | 1-2 µg/ml; 0 | 1 | 2 | Vitek 2 AST-N032 | 100 | ND | 0 | NA | NA | [118] |
| R > 2 µg/ml | ||||||||||||
|
| ||||||||||||
| 172 Gram-negative isolates | AD | S ≤ 2 µg/ml | 0.5–64; 31.4% | Vitek 22 AST-N032 (n = 32) | 82 | 75.2 | 0 | 57.4 | [32] | |||
| R > 2 µg/ml | Etest (n = 137) | 86.6 | 75.0 | 6.8 | 27.8 | |||||||
|
| ||||||||||||
| 115 A. baumannii isolates | BMD | S ≤ 2 µg/ml | ≤0.06–512 µg/ml; 19.1% | ≤0.06 | 32 | Etest | 98.2 | 16.5 | 0 | 1.7 | [138] | |
| R > 2 µg/ml | ||||||||||||
|
| ||||||||||||
| 501 P. aeruginosa isolates (401 CF) | AD | S ≤ 4 µg/ml | ≤0.5–≥16 µg/ml; 17.8% | 2 | 4 | BMD 24 h | 96 | 1.2 | 26.5 | [121] | ||
| 50 A. xylosoxidans isolates | R >4 µg/ml | 4 | ≥16 | BMD 48 h | 93.6 | 3.9 | 18.0 | |||||
| 50 S. maltophilia isolates | 8 | ≥16 | ||||||||||
|
| ||||||||||||
| 70 S. maltophilia | AD | S ≤ 2 µg/ml | 0.12–32 µg/ml; 24.3% | 2 | 4 | DD 10 µg; R ≤ 8; S ≥ 11 mm | 71.2 | NA | 0 | 93.7 | 5.7 | [125] |
| R > 2 µg/ml | Etest | 86.4 | 96.7 | 5.6 | 37.5 | NA | ||||||
|
| ||||||||||||
| 200 Gram-negative isolates | BMD | S ≤ 2 µg/ml | ≤1–>128 µg/ml; 15% | DD 10 µg; R ≤ 10; S ≥ 14 mm | 94 | NA | 0 | 21.8 | 1.5 | [127] | ||
| (i) 60 A. baumannii isolates | R > 2 µg/ml | ≤1 | 2 | DD 10 µg; R ≤ 8; S ≥ 11 mm | 95 | 0 | 31.2 | 1 | ||||
| (ii) 80 P. aeruginosa isolates | ≤1 | ≤1 | ||||||||||
| (iii) 12 S. maltophilia isolates | ≤1 | 32 | ||||||||||
|
| ||||||||||||
| 35 representatives | BMD | S ≤ 2 µg/ml | ≤1–≥128 µg/ml; 40% | AD | 97.1 | 91.4 | 47.6 | 0 | [127] | |||
| R > 2 µg/ml | ||||||||||||
CA: categorical agreement; EA: essential agreement; VME: very major error; ME: major error; MiE: minor error; AD: agar dilution; BMD: broth microdilution; DD: disk diffusion; MH: Mueller-Hinton. Italic values indicate the number of errors and not the percentage when a too few number of strains tested, where R for VME or S for ME. 1Sensititre panels: ≤0.25–>4 µg/ml except for SEMPA1. 2Vitek 2 reagent cards: ≤0.5–≥16 µg/ml except for AST-N038 (≤2, 4, and >4 µg/ml) and AST-N032 (1–4 µg/ml). 3Phoenix 100 cards: ≤1–>4 µg/ml. 4MicroScan-dried Gram-negative breakpoint combo panel type 42 ≤2 and >4 µg/ml. ∗Prediffusion test: discs were removed after 2 h of incubation.
The surfactant polysorbate 80 was previously added to trays to limit polymyxin adherence to polystyrene and is not yet recommended; however, it could induce VME and mcr strains might not be detected [31, 110–112]. Albur et al. demonstrated that the polystyrene trays used also have an influence: using tissue-culture-coated round-bottom trays gave a 5.3-fold increase in MIC values compared to noncoated V-bottom trays [113], for the material used [106] (Table S3). A very recent study compared polystyrene coated trays to glass coated trays and also showed very few differences (Table 3) [114].
Until 2013, many comparative studies used agar dilution (AD) as the reference method for polymyxins susceptibility testing, a method that differs from the BMD only because the polymyxins are added to a solid MH2 medium [31, 32, 115–126]. Compared to BMD, agar dilution generally gave concordant results for colistin and polymyxin B [31, 110, 127, 128]. VMEs were very uncommon with AD, and this pointed to the AD's potential role in screening, as it presents the advantage to test several strains on the same plates [117, 129]. A recent study compared agar dilution to broth macro- and microdilution on 8 strains and concluded that agar dilution was the most reproducible method, with an excellent distribution of colistin in agar, but that colistin-containing agar plates could be only stored for 7 days [130].
Diffusion methods based on the antibiotic diffusion in agar, whether with the Kirby–Bauer disk diffusion [131] or with the gradient strips, are not reliable for polymyxin testing and should not be used as a large number of studies have obtained high rates of VMEs or poor EA [32, 120, 125, 128, 132–135]. Some studies showed good results but contained only susceptible strains [136–138]. The influence of MH2 agar composition was assessed: agreement was not affected with agar dilution, but important differences were highlighted with Etest (BioMérieux, Marcy l'Étoile, France) [31, 139]. The advantage of the agar diffusion method is the detection of heteroresistance: colonies present within the inhibition zone correspond to resistant subpopulations [140]. One study compared disc diffusion to Etest method, and a large rate of minor errors occurred [141]. The ColiSpot test consists of replacing the disk of colistin by a drop of a calibrated colistin solution (8 µg/ml). Colistin resistance is revealed in the absence of the inhibition zone. This technique was evaluated with 89 colistin-resistant and 52 colistin-susceptible strains and was developed for veterinarian laboratories [142].
3.3. Commercial Devices Based on Broth Microdilution Reference Method
Several commercial devices based on BMD reference methods were developed to easily assess the reference method by offering ready-to-use systems. Their advantage is the elimination of critical preparation steps of MH2 medium and antibiotic dilutions. These systems were used to detect mcr-1 strains and were evaluated by EUCAST, giving correct results, with essential agreement ranging from 82% to 96%, and few MEs or VMEs (http://www.eucast.org/ast_of_bacteria/warnings/) [143].
3.3.1. UMIC Colistine (Biocentric, Bandol, France)
UMIC colistine consists of unitary tests composed of 12-well polystyrene strips, one for growth control and 11 containing dehydrated colistin, with concentrations ranging from 0.06 to 64 µg/ml, provided with unitary MH2 tubes. Inoculation is performed simply, after diluting the 0.5 McFarland suspension by 200-fold into the MH2 tubes, by distributing 100 µL of this diluted suspension into the 12 wells of the strip, leading to the rehydration of the antibiotic. The strips are then incubated at 35 ± 1°C using the UMIC box to avoid any desiccation. One comparative evaluation on 71 A. baumannii isolates and one on 92 Gram-negative isolates including 76 Enterobacteriaceae highlighted the reliability of the UMIC colistine kit [144, 145].
3.3.2. MIC Strip Colistin (MERLIN Diagnostika Bornheim-Hersel, Germany)
MIC Strip Colistin also consists in unitary 12-well strips with concentrations of dehydrated colistin ranging from 0.06 to 64 µg/mL, and Micronaut-S is a panel composed of different antibiotics on standard 96-well trays. Those systems can be automated with Micronaut ASTroID that concomitantly performs dilution for antimicrobial susceptibility testing (AST) and deposits on the MALDI-TOF target, simultaneously identifying the same colony being tested.
3.3.3. Sensitest Colistin (Liofilchem, Roseto degli Abruzzi, Italy)
It consists of a compact panel of 4 tests containing 7 twofold dilutions of dehydrated colistin (0.25–16 µg/ml). It showed excellent correlation with BMD when tested on 353 isolates, including 259 Enterobacteriaceae, 83 harboring the mcr-1 gene [146]. Recently, a combined Sentitest colistin/piperacillin-tazobactam was developed, with the same design, providing a unitary test for testing both antibiotics, with colistin concentrations ranging from 0.008 to 128 µg/ml.
3.3.4. The Sensititre System (Thermo Fisher Scientific, Waltham, MA, USA)
It presents different antibiotics on 96-well trays with a customizable plate layout. Inoculation, incubation, and reading (based on fluorescence) steps can be automated. Chew et al. [147] recently evaluated a Sensititre GNX3F panel containing both polymyxin B and colistin (0.25–4 mg/L) and presented a sensitivity of 95.2% and 100% in detecting the 21 mcr-1 isolates tested, respectively.
3.4. Automated Systems
Automated systems were developed to shorten result timeframes by increasing sensitivity, and also to avoid manipulation bias [148], with incubation and real-time reading. However, by combining several antibiotics, the number of concentrations tested is limited, and they cannot give a real MIC (Table 3).
3.4.1. MicroScan WalkAway (Beckman Coulter, San Diego, CA, USA)
It uses standard trays that are manually inoculated, and reading is based on fluorometry, with results obtained in 3.5–7H. It is not available on polymyxin B, and essential agreement cannot be evaluated between techniques as the NM44 panel proposes only ≤4 and ≥4 µg/ml for colistin. In the recent study of Chew et al., this panel was able to detect all mcr-1 tested isolates and presented only one VME on 76 Enterobacteriaceae isolates tested. It also evaluated 213 Acinetobacter species and presented 99.1 % categorical agreement against the agar dilution method [115].
3.4.2. Vitek 2 (BioMérieux, Marcy l'Étoile, France)
It is a semiautomated system that uses reagent cards containing dehydrated antibiotics and other reagents in a 64-well format. It combines rapid identification and AST using an extrapolated growth algorithm. Various comparative studies performed to evaluate Vitek 2 have returned discrepant results with high rates of VME. In their recent evaluation, Chew et al. [147] demonstrated the efficacy of Vitek 2 in assessing both polymyxin B and colistin MIC with only one VME for each and 96.1% and 93.9% EA, respectively, but it was only able to detect mcr-1 strains with polymyxin B.
3.4.3. BD Phoenix™ (Becton Dickinson, Le Pont de Claix, France)
It performs identification and AST in parallel in 84-well specific plates. Reading is based on an oxidation-reduction indicator in 6–16 hours. One study showed excellent agreement on 109 P. aeruginosa strains, but only colistin-susceptible strains were tested [149]. Vourli et al. [129] have shown concerning results testing Acinetobacter baumannii strains with very high VME rates (41.4%) despite the study including 24.8% of colistin-resistant strains. This was explained by the majority of errors occurring near the breakpoint (2 instead of 4 µg/ml). Lastly, in the study by Jayol et al. [83], the Phoenix system was able to detect all mcr-carrying bacteria, even those with a colistin MIC of 4 µg/ml, but the high rates of VMEs obtained prove its inability to assess heteroresistance.
4. Genotyping and Molecular Screening
4.1. PCR Amplification and Sequencing to Detect Gene Mutations
Molecular biology methods are the most sensitive for determining antibiotic resistance by assessing the presence of resistance genes or mutations conferring resistance. These methods are complementary to the phenotypic techniques and confirm the resistant status of bacterial isolates. The main mutations for Enterobacteriaceae species are located on genes coding the two-component systems PmrA/PmrB and PhoP/PhoQ (Figure 1). Specifically, mutations in the mgrB gene—the negative feedback regulator of PhoPQ—notably with the presence of insertional sequences, appeared to be the main resistance mechanism observed in K. pneumoniae strains. These colistin resistances are not based on drug-modifying enzymes or the acquisition of a resistance gene which could be easily detected. Screening of potential mutations on these chromosomal genes is done by amplification and sequencing, takes 3 days, and requires that all genes are tested. Sequenced amplicons are then compared by the BLAST tool against the NCBI database to screen possible mutations compared to wild-type genes.
4.2. Real-Time qPCR to Detect the Presence of mcr Genes
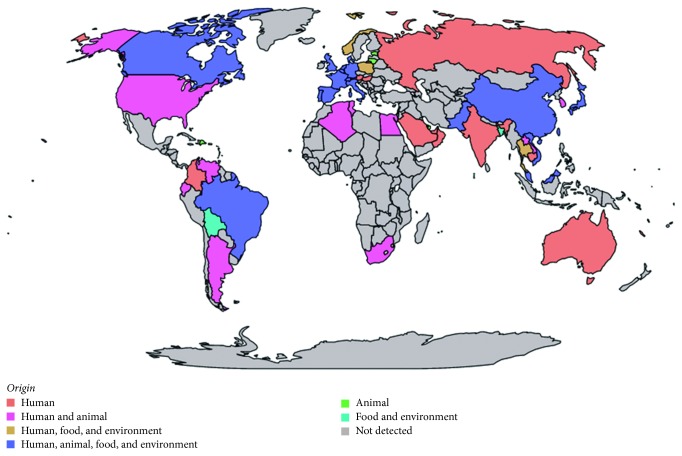
The discovery of the acquired gene mcr-1 justifies the use of molecular detection with RT-PCR, a rapid quantitative technique to detect the presence of the gene. A systematic screening of the gene in colistin-resistant strains was performed [150] (Figure 2). For such purposes, scientists have used the primers of the original study [6], or have designed their own primers for standard PCR [132, 151–160] or RT-PCR, based on SYBR Green assays [64, 151, 161], TaqMan probe [66, 72, 152, 162], or other FAM-labelled probe [9, 71, 163, 164] or HEX-labelled probe [165] (Table 4).
Figure 2.
Worldwide dissemination of the mcr-1 gene. The map was performed with Magrit mapping application (http://magrit.cnrs.fr).
Table 4.
List of primers designed to detect mcr genes by PCR.
| Targeted genes | Analyze | Method | Primer sequences | Cycle (nb: steps) | Product (bp) | Study |
|---|---|---|---|---|---|---|
| mcr-1 | Original study | Std | CLR F: 5′-CGGTCAGTCCGTTTGTTC-3′ | 25: 94°C, 30 s; 58°C, 90 s; 72°C, 60 s | 309 | [6] |
| CLR R: 5′-CTTGGTCGGTCTGTAGGG-3′ | ||||||
| 105 colistin-resistant strains | Std | mcr-1_F: 5′-TGTGGTACCGACGCTCGGTCAG-3′ | [152] | |||
| mcr-1_R: 5′-TCAGCGGATGAATGCGGTGC-3′ | ||||||
| 45 colistin-resistant strains in 2 spiked stools | HotStarTaqMasterMix | mcr-1_s: 5′-ATGGCACGGTCTATGATA-3′ | 45: 95°C, 30 s; 55°C, 30 s; 72°C, 30 s | 155 | [160] | |
| Mcr-1_FAM-BHQ: 5′-CTACAGACCGACCAAGCCGA-3′ | mcr-1_as: 5′-CGGATAATCCACCTTAACA-3′ | |||||
| In silico study | Pr 5 = -HEX-C | mcr-1-286F: 5′-ACTTATGGCACGGTCTATGA-3′ | 40: 95°C, 10 s; −56°C, 40 s | [162] | ||
| CAAGCCGA-ZEN-GACCAAGGATC-3IABkFQ-3 | mcr-1-401R: 5′-ACACCCAAACCAATGATACG-3′ | |||||
| 20 strains in 3 spiked stools | SYBR Green | mcr-1-qF1: 5′-ACACTTATGGCACGGTCTATG-3′ | 40: 95°C, 3 s; 60°C, 20 s; 72°C, 7 s | 120 | [148] | |
| mcr-1-qR1: 5′-GCACACCCAAACCAATGATAC-3′ | ||||||
| mcr-1-qF2: 5′-TGGCGTTCAGCAGTCATTAT-3′ | [165] | |||||
| mcr-1-qR2: 5′-AGCTTACCCACCGAGTAGAT-3′ | ||||||
| 2046 strains | Std | mcr-1-F: 5′-ATGATGCAGCATACTTCTGTGTG-3′ | 1646 | [148] | ||
| mcr-1-R: 5′-TCAGCGGATGAATGCGGTGC-3′ | ||||||
| Wastewater samples | SYBR Green | mcr-1-F1: 5′-TGTTCTTGTGGCGAGTGTTG-3′ | 40: 95°C, 15 s; 60°C, 30 s | [158] | ||
| mcr-1-R1: 5′-CGCGCCCATGATTAATAGCA-3′ | ||||||
| 78 stool | SYBR Green | mcr-1-FW: 5′-ACGCCATCTGCAACACCAA-3′ | 30/40: 95°C, 15 s; −63°C, 10 s; −72°C, 10 s | 59 | [61] | |
| mcr-1-RV: 5′-GCCAACGAGCATACCGACAT-3′ | ||||||
| 100 strains: 18 colistin-resistant strains in 833 faecal samples | TaqMan probe: 6 FAM–GACCGCGACCGCCAATCTTACC-TAMRA | F1: GCAGCATACTTCTGTGTGGTAC | 35: 95°C, 30 s; −60°C, 1 min | 145 | [149] | |
| R1: ACAAAGCCGAGATTGTCCGCG | ||||||
| Std | F1: GCAGCATACTTCTGTGTGGTAC | 554 | ||||
| R3: TATGCACGCGAAAGAAACTGGC | ||||||
| 1495 E. coli strains and 571 KP strains | Std | Mcr-1-forward: 5ʹ-GCTCGGTCAGTCCGTTTG-3ʹ | [150] | |||
| Mcr-1-reverse: 5ʹ-GAATGCGGTGCGGTCTTT-3′ | ||||||
| 51 strains | FastStart Universal Probe Master kit | M-F: CATCGCGGACAATCTCGG | 40: 95°C, 15 s; −60°C, 1 min | 116 | [161] | |
| 18 samples | FAM-AACAGCGTGGTGATCAGTAGCAT-BHQ | M-R: AAATCAACACAGGCTTTAGCAC | ||||
| 241 isolates | Std | MCR-1-F2: 5′-CTCATGATGCAGCATACTTC-3′ | Entire gene | [151] | ||
| MCR-1-R2: 5′-CGAATGGAGTGTGCGGTG-3′ | ||||||
| Clinical E. coli isolates | TaqMan Fast Advanced Master Mix | MCR-1F: 5′-CATCGCTCAAAGTATCCAGTGG-3′ | [69] | |||
| 5′-Cy5-TGCAGACGCACAGCAATGCCTATGAT-TAO-3′ | MCR-1R: 5′-CCATGTAGATAGACACCGTTCTCAC-3′ | |||||
| 10,609 E. coli isolates (505R) | TaqMan RT-mcr-1_Probe | RT-mcr-1_F: TGGCGTTCAGCAGTCATTAT | 30°C–95°C, 15 s; −60°C, 1 min | [159] | ||
| Cy5-AGTTTCTTTCGCGTGCATAAGCCG-BBQ-650 | RT-mcr-1_R: AGCTTACCCACCGAGTAGAT | |||||
| 62 isolates | MCR1_22,763_Pb1 FAM-TGGTCTCGG/ZEN/CTTGGTCGGTCTGTAGGGC-3IABkFQ | MCR1_22,697_F1: 5′-CACTTATGGCACGGTCTATGA-3′ | [68] | |||
| MCR1_22,810_R1: 5′-CCCAAACCAATGATACGCAT-3′ | ||||||
| 31 colistin-resistant isolates | Std | mcr-1_F: 5′-ATGATGCAGCATACTTCTGTGTGG-3′ | [157] | |||
| mcr- 1_R: 5′-GTGCGGTCTTTGACTTTGTCC-3′ | ||||||
| 122 faecal samples | TaqMan probe: 5′-TTGACCGCGACCGCCAATCTTA-3′ FAM | [6] | 45: 15 s, 95°C; −1 min, −60°C | 309 | [63] | |
| 48 E. coli and 27 KP strains | mcr-1-F1: 5′-ATGATGCAGCATACTTCTGTG-3′ | [153, 155] | ||||
| mcr-1-R1: 5′-TCAGCGGATGAATGCGGTG-3′ | ||||||
| CLR5-F1: 5′-ATGATGCAGCATACTTCTGTGTGG-3′ | [156] | |||||
| CLR5-R1: 5′-TCAGCGGATGAATGCGGTGC-3′ | ||||||
| CLR5-F: 5′-CGGTCAGTCCGTTTGTTC-3′ | [176] | |||||
| Mcr1-Rv2: 5′-CCAGCGTATCCAGCACATTT-3′ | ||||||
|
| ||||||
| mcr-2 | 136 colistin-resistant isolates | Std | MCR2-IF: 5′-TGTTGCTTGTGCCGATTGGA-3′ | 33: 95°C, 3 min; 65°C, 30 s; 72°C, 1 min | 567 | [7] |
| 31 coli-resistant isolates | MCR2-IR: 5′-AGATGGTATTGTTGGTTGCTG-3′ | [157] | ||||
| 1200 isolates | [163] | |||||
| 6 isolates | Std | MCR-2-F(EcoRI): 5′-AACCGAATTCATGACATCACATCACTCTTG-3′ | [164] | |||
| MCR-2-R (SalI): 5′-CCGGTCGACTTACTGGATAAATGCCGCGC-3′ | ||||||
| 2396 strains | Std | Mcr-2 full Fw: 5′-ATGACATCACATCACTCTTGG-3′ | 34: 95°C, 1 min; 52°C, 30 s; 72°C, 1 min | [165] | ||
| 1144 samples | Mcr-2 full Rv: 5′-TTACTGGATAAATGCCGCGC-3′ | [65, 166] | ||||
| 436 cultures | TaqMan mcr-2_Probe | Mcr-2_fwd: TTGTCGTGCTGTTATCCTATCG | 30: 95°C, 15 s; −60°C, 1 min | [167] | ||
| ROX-ACTGATTATGGGTGCGGTGACGAG-BHQ-2 | Mcr-2_rev: CCGTGCCATAAGTATCGGTAAA | |||||
|
| ||||||
| mcr-1 and mcr-2 | 1200 isolates | Std | mcr1-2 universal F: ACTTATGGCACGGTCTATGATAC | 30: 94°C, 30 s; 58°C, 30 s; 72°C, 2 min | 1311 | [163] |
| mcr1-2 universal R: CCGCGGTGACATCAAACA | ||||||
| Std | MCR-1/2-Fw: 5′-TAT CGC TAT GTG CTA AAG CC-3′ | 715 bp | [168] | |||
| MCR-1/2-Rv: 5′-TCT TGG TAT TTG GCG GTA TC-3′ | ||||||
| 621 faecal samples | Mcr-generic probe TATCACGCCACAAGATAC | Mcr-generic fw: GCCAAATACCAAGAAAATG | 98 bp | [71] | ||
| Mcr-generic rev: TTATCCATCACGCCTTTT | ||||||
|
| ||||||
| mcr-3 | 580 E. coli strains | Std | MCR3-F: 5′-TTGGCACTGTATTTTGCATTT-3′ | 30: 95°C, 30 s; 50°C, 30 s; 72°C, 45 s | 542 | [10] |
| MCR3-R: 5′-TTAACGAAATTGGCTGGAACA-3′ | ||||||
|
| ||||||
| mcr-1, mcr-2, and mcr-3 | 25 isolates: 17 mcr-1 and 8 mcr-3 20 samples | SYBR Green | mcr1-qf: AAAGACGCGGTACAAGCAAC MCR-1 | 40: 95°C, 30 s; 60°C, 30 s; 72°C, 30 s | 213 | [169] |
| mcr1-qr: GCTGAACATACACGGCACAG | 92 | |||||
| mcr2-qf: CGACCAAGCCGAGTCTAAGG MCR-2 | 169 | |||||
| mcr2-qr: CAACTGCGACCAACACACTT | ||||||
| mcr3-qf: ACCTCCAGCGTGAGATTGTTCCA MCR-3 | ||||||
| mcr3-qr: GCGGTTTCACCAACGACCAGAA | ||||||
|
| ||||||
| mcr-4 | 125 isolates | Std | Mcr-4 FW: ATTGGGATAGTCGCCTTTTT | 487 | [11] | |
| Mcr-4 RV: TTACAGCCAGAATCATTATCA | ||||||
|
| ||||||
| mcr-5 | 12 Salmonella paratyphi B isolates | Std | MCR5_fw: 5′-ATGCGGTTGTCTGCATTTATC-30′ | 30: 95°C, 30 s; 50°C, 95 s; 72°C, 95 s | 1644 | [12] |
| MCR5_rev: 5′-TCATTGTGGTTGTCCTTTTCTG-3′ | ||||||
|
| ||||||
| mcr-1, mcr-2, mcr-3, mcr-4 and mcr-5 | 49 E. coli and Salmonella isolates | Std | mcr1_fw: AGTCCGTTTGTTCTTGTGGC | 25: 94°C, 30s; 58°C, 90s; 72°C, 60s | 320 | [170] |
| mcr1_rev: AGATCCTTGGTCTCGGCTTG | ||||||
| mcr2_fw: CAAGTGTGTTGGTCGCAGTT | 715 | |||||
| mcr2_rev: TCTAGCCCGACAAGCATACC | ||||||
| mcr3_fw: AAATAAAAATTGTTCCGCTTATG | 929 | |||||
| mcr3_rev: AATGGAGATCCCCGTTTTT | ||||||
| mcr4_fw: TCACTTTCATCACTGCGTTG | 1116 | |||||
| mcr4_rev: TTGGTCCATGACTACCAATG | ||||||
| mcr5_fw: ATGCGGTTGTCTGCATTTATC | 1644 | |||||
| mcr5_rev: TCATTGTGGTTGTCCTTTTCTG | ||||||
Std: standard; KP: K. pneumoniae.
Xavier et al. designed primers to screen mcr-2 [7], giving a 567 bp product [166]. Some designed their own primers for standard PCR [167–169], and one study developed a TaqMan assay for qPCR [170]. Interestingly, three studies went further by designing a universal primer to detect both mcr-1 and mcr-2 genes by standard PCR [166, 171] and a generic primer and a probe to detect them by qPCR [74], but these have not yet been tested on other mcr genes. Lastly, primers were designed for detecting mcr-3 [10], mcr-4 [11], and mcr-5 genes [12] by standard PCR (Table 4). A recent study described a multiplex SYBR Green real-time PCR assay for the simultaneous detection of mcr-1, mcr-2, and mcr-3 genes [172]. Finally, a multiplex PCR assay for detection of the five mcr genes: mcr-1, mcr-2, mcr-3, mcr-4, and mcr-5, was developed in order to obtain sequential amplicons with a size difference of 200 bp, allowing their fast and simultaneous detection on agarose gels [173].
4.3. PCR to Detect Plasmid Carrying mcr Genes
mcr-1 is a 1626-base pair-long gene located on a 2607 bp common region flanked on both ends by an ISApl1 insertion sequence (IS) in some plasmids [174]. This sequence may form a composite transposon that can potentially move as one complete unit [155, 175, 176]. This insertion sequence appears to be a key component of the mobilome, and its presence is not systematic. Furthermore, only the upstream region can contain ISApl1 [165]. Li et al. identified the ability of the Tn6330 transposon (ISApl1-mcr-1-orf-ISApl1) to generate circular ISApl1-mcr-1-orf [177]. Specific primers were developed to screen the upstream presence of this IS transposon by PCR and Sanger sequencing [178–180]. Others have also designed their own system to directly screen on plasmid carrying mcr-gene type IncX4 [9, 181], but these methods also exhibit limitations, as a wide distribution has been observed for mcr-1 among different plasmids (IncI2, IncX4, IncHI2, IncY, IncF, IncP, IncH1, and IncX3), demonstrating the great ability of mcr genes to spread.
4.4. Microarray
Microarray technology allows scientists to analyze dozens of genes at the same time. The Check-MDR CT103 microarray system (Check-Points, Wageningen, the Netherlands) was developed to screen the presence of extended-spectrum beta-lactamase (ESBL) genes (TEM and SHV) and carbapenemase genes (OXA-48, KPC, NDM…) in the same assay and can assay 24 samples at the same time, with an effective detection in 6.5 hours. Recently, a study evaluated this assay for detecting mcr genes: sensitivity and specificity were excellent for mcr-1 and its variants (from mcr-1.2 to mcr-1.7 and mcr-2 genes), but it was not able to detect the new gene mcr-3 [182]. mcr-4 has not been assayed yet.
4.5. Loop-Mediated Isothermal Amplification (LAMP)
The Eazyplex SuperBug mcr-1 kit (Amplex Biosystems Gmbh, Giessen, Germany) was developed to assess the presence of the mcr-1 gene within 20 minutes [183]. It was effective on 104 microbial strains but needs to be assayed directly on clinical samples. As it was developed before the description of the other mcr genes, it can only detect the mcr-1 gene and the mcr-1.2 variant.
More recently, another LAMP-based assay was developed to detect mcr-1 gene and evaluated as a screening tool on 556 multidrug-resistant Enterobacteriaceae [184]. Seven isolates were positive by both standard PCR and LAMP-based assay (6 E. coli and 1 K. pneumoniae). The results can be assessed by chromogenic visualization. This test constitutes a rapid, specific, and cost-effective tool that exhibits a higher sensitivity than PCR (10-fold). It has to be assayed on clinical samples; as for now, only spiked tools were used.
4.6. Novel Approach with Direct Resistome Analysis
Genomic screening is an alternative approach for studying resistance and providing a better understanding of the behavior of bacterial isolates [185]. The development of next-generation sequencing has led to lower costs, reduced screening delay, and increased sequencing speeds combined with updated databases providing access to a large amount of information. The mcr-1 gene was initially discovered by whole genome sequencing during an active livestock monitoring program in China [6]. A considerable number of retrospective studies analyzing previously recorded genomic sequences have since been carried out, showing the global dispersion of the gene [9, 10, 20, 23, 24, 72, 74, 157, 158, 174, 177, 180, 186–204] (Figure 2).
The technologies used to completely sequence the bacterial genome are Illumina (Illumina Inc., San Diego, CA, USA), which produces short sequences (300 bp) and requires several days, and PacBio RS II (Pacific Biosciences, Menlo Park, CA, USA), which produces a single real-time molecule producing long sequences (60kb) in a few hours [205]. The use of Illumina sequencers is not suitable for covering bacterial genomes with multiple repetitive elements because too many sequence pieces are obtained after assembly, whereas PacBio RS II delivers a single sequence without missing regions [174]. Sekizuka et al. performed a hybrid analysis using the two technologies to analyze three Inc2 plasmids and found that they were highly conserved with the exception of the shufflon region, meaning that the combination of the two methods enables to analyze rearragements in highly recombinant regions [174].
The sequences obtained are assembled, the genome is annotated, and then a mapping is carried out against a reference plasmid, in general pHNSHP45 for mcr-1 [6]. The aligned sequences are then compared to one of the resistance gene databases: Antibiotic Resistance Gene-Annotation [206], ResFinder [207], Comprehensive Antibiotic Resistance Database [208], and Antibiotic Resistance Genes Database [209]. They could also be compared to the plasmid genome, with GenEpid-J [210] or PlasmidFinder, which enabled the discovery of the mcr-4 gene [11] and presents the advantage of screening multiple genes and detecting the coexistence of several genes including carbapenemases. Lindsey et al. proposed a whole protocol for plasmid sequencing [211]. More specifically, PointFinder was developed to detect chromosomal point mutations associated with antimicrobial resistance [212].
Whole genome sequencing combined with new bioinformatic tools improves our ability to detect several resistance genes at the same time [186, 205] but presents the same limitations than PCR: new genes are not recognized by these techniques, which require the continuous updating of databases [175, 213] that should be merged into a single reference database [213].
5. Conclusion
The recent description of plasmid-mediated colistin-resistant genes has generated concern among the global scientific community about the lack of new antibiotics to treat infections caused by multidrug-resistant pathogens. This concern was raised by the worldwide screening that demonstrated the global spread of bacterial strains harboring the mcr-1 gene from diverse human and animal origins. Thus, it is necessary to implement an adapted protocol to effectively detect colistin-resistant strains in clinical microbiology laboratories.
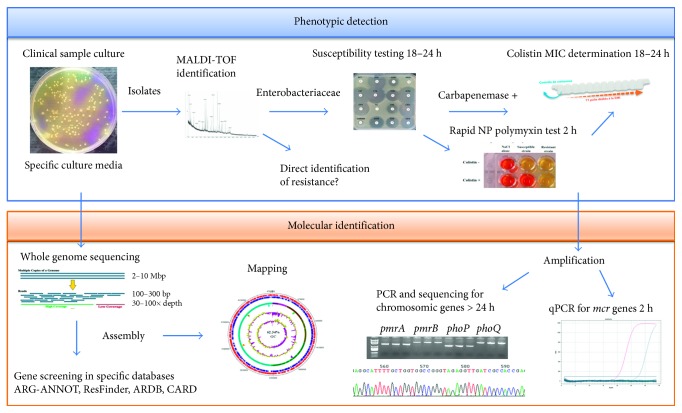
Phenotypic methods indicate to the microbiologist the presence of polymyxin-resistant strains but do not define the mechanism involved and the risk of transmission. Molecular methods are rapid and more sensitive but are specific to the resistance genes examined and faced with the large number of molecular mechanisms conferring resistance to polymyxins, should only be used to screen mcr genes in clinical microbiology laboratories. Genomic analysis enables the complete screening of resistance genes in genetically identified bacteria from clinical samples but remains an in silico study which enables predictions but not resistance observation, as the presence of a resistance gene in a genome does not mean that the corresponding isolate is resistant, supported by studies that identified polymyxin-susceptible bacteria carrying the mcr-1 gene [92, 165, 213]. Thus, phenotypic and molecular methods are complementary in detecting colistin-resistant pathogens in order to analyze the behavior of the clinical isolate, and it is important to carry them out in parallel [148] (Figure 3). All these techniques and their detection characteristics are summarized in Table 5.
Figure 3.
Complementarity of phenotypic and genotypic methods in detection and analysis of colistin-resistant bacteria.
Table 5.
Comparison of detection methods for polymyxin resistance.
| Method | Principle | Time | Manual (M); automated (A) | Detection | |||
|---|---|---|---|---|---|---|---|
| ColR | mcr | HR | MIC | ||||
| Phenotypic | |||||||
| Selective agar | Selective growth | 18 h | M | + | − | + | − |
| Rapid polymyxin NP | pH change | 4 h | M | + | − | − | − |
| Micromax | Cell wall lysis detection by fluorescence | 3 h | M/A | + | − | − | − |
| MALDI-TOF MS | Specific peak detection | 1 h | A | + | + | − | − |
| MCR-1 inhibition | Chelation with | 18 h | M | + | + | ± | + |
| Colistin MAC | Dipicolinic acid | ||||||
| EDTA assays | EDTA | ||||||
|
| |||||||
| AST | |||||||
| BMD (UMIC, Micronaut-MIC, Sensitest, Micronaut-S, and Sensititre) | Growth inhibition | 18 h | M/A | + | − | ± | + |
| Agar diffusion | Measure of growth inhibition zone | 18 h | M | ||||
| Disk diffusion | − | − | + | − | |||
| Gradient strip | − | − | + | + | |||
| ColiSpot | + | − | ND | − | |||
| Agar dilution | Growth inhibition | 18 h | M | − | − | + | + |
| Automatized system | Growth detection | ||||||
| MicroScan | Fluorimetry | 3.5–7 h | A | + | − | − | − |
| Vitek 2 | Algorithm | 4–10 h | A | + | − | − | − |
| Phoenix | Oxidoreduction | 6–16 h | A | + | − | − | − |
|
| |||||||
| Genotypic | |||||||
| Standard PCR | Amplification | 3 h | A | + | + | − | − |
| RT-PCR | Amplification | 1 h | A | + | + | − | − |
| LAMP (Eazyplex, etc.) | Amplification | 20 min | A | + | − | − | − |
| Microarray | DNA hybridization | 6.5 h | A | + | − | − | − |
| NGS | Whole-genome sequencing | ||||||
| Illumina | 4–56 h | A | + | + | − | − | |
| PacBio RS II | 0.5–3 h | A | + | + | − | − | |
ColR: colistin resistance; HR: heteroresistance; +: yes; −: no; ±: sometimes.
In conclusion, these new techniques need to be combined for a complete understanding of colistin resistance, in particular for strains carrying mcr genes, so clinicians can rapidly adapt treatments or isolate the carrier patient in the hospital.
Acknowledgments
This work was supported by the French Government under the “Investissements d'avenir” (Investments for the Future) program managed by the Agence Nationale de la Recherche (ANR, fr: National Agency for Research) (reference: Méditerranée Infection 10-IAHU-03).
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Supplementary Materials
Table S1: home-made polymyxin-containing agar. Table S2: comparison of different polymyxin B susceptibility testing methods to detect polymyxin B resistance in Gram-negative clinical isolates. Table S3: other comparative AST methods.
References
- 1.Jeannot K., Bolard A., Plésiat P. Resistance to polymyxins in Gram-negative organisms. International Journal of Antimicrobial Agents. 2017;49(5):526–535. doi: 10.1016/j.ijantimicag.2016.11.029. [DOI] [PubMed] [Google Scholar]
- 2.Biswas S., Brunel J. M., Dubus J. C., Reynaud-Gaubert M., Rolain J. M. Colistin: an update on the antibiotic of the 21st century. Expert Review of Anti-infective Therapy. 2012;10(8):917–934. doi: 10.1586/eri.12.78. [DOI] [PubMed] [Google Scholar]
- 3.Hancock R. E., Chapple D. S. Peptide antibiotics. Antimicrob Agents Chemother. 1999;43(6):1317–1323. doi: 10.1128/aac.43.6.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Olaitan A. O., Li J. Emergence of polymyxin resistance in Gram-negative bacteria. International Journal of Antimicrobial Agents. 2016;48(6):581–582. doi: 10.1016/j.ijantimicag.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 5.Olaitan A. O., Morand S., Rolain J. M. Mechanisms of polymyxin resistance: acquired and intrinsic resistance in bacteria. Frontiers in Microbiology. 2014;5:p. 643. doi: 10.3389/fmicb.2014.00643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu Y. Y., Wang Y., Walsh T. R., et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infectious Diseases. 2016;16(2):161–168. doi: 10.1016/S1473-3099(15)00424-7. [DOI] [PubMed] [Google Scholar]
- 7.Xavier B. B., Lammens C., Ruhal R., et al. Identification of a novel plasmid-mediated colistin-resistance gene, mcr-2, in Escherichia coli, Belgium, June 2016. Eurosurveillance. 2016;21(27):6–11. doi: 10.2807/1560-7917.es.2016.21.27.30280. [DOI] [PubMed] [Google Scholar]
- 8.Di Pilato V., Arena F., Tascini C., et al. mcr-1.2, a new mcr variant carried on a transferable plasmid from a colistin-resistant KPC carbapenemase-producing Klebsiella pneumoniae strain of sequence type 512. Antimicrobial Agents and Chemotherapy. 2016;60(9):5612–5615. doi: 10.1128/AAC.01075-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yang Y. Q., Li Y. X., Song T., et al. Colistin resistance gene mcr-1 and its variant in Escherichia coli isolates from chickens in China. Antimicrobial Agents and Chemotherapy. 2017;61(5):e01204–e01216. doi: 10.1128/AAC.01204-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yin W., Li H., Shen Y., et al. Novel plasmid-mediated colistin resistance gene mcr-3 in Escherichia coli . MBio. 2017;8(3) doi: 10.1128/mBio.00543-17.e00543-17-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carattoli A., Villa L., Feudi C., et al. Novel plasmid-mediated colistin resistance mcr-4 gene in Salmonella and Escherichia coli, Italy 2013, Spain and Belgium, 2015 to 2016. Eurosurveillance. 2017;22(31):p. 30589. doi: 10.2807/1560-7917.es.2017.22.31.30589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borowiak M., Fischer J., Hammerl J. A., Hendriksen R. S., Szabo I., Malorny B. Identification of a novel transposon-associated phosphoethanolamine transferase gene, mcr-5, conferring colistin resistance in d-tartrate fermenting Salmonella enterica subsp. enterica serovar Paratyphi B. Journal of Antimicrobial Chemotherapya. 2017;72(12):3317–3324. doi: 10.1093/jac/dkx327. [DOI] [PubMed] [Google Scholar]
- 13.AbuOun M., Stubberfield E. J., Duggett N. A., et al. mcr-1 and mcr-2 (mcr-6.1) variant genes identified in Moraxella species isolated from pigs in Great Britain from 2014 to 2015. Journal of Antimicrobial Chemotherapy. 2017;72(10):2745–2749. doi: 10.1093/jac/dky272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang Y.-Q., Li Y.-X., Lei C.-W., Zhang A.-Y., Wang H.-N. Novel plasmid-mediated colistin resistance gene mcr-7.1 in Klebsiella pneumoniae. Journal of Antimicrobial Chemotherapy. 2018;73(7):1791–1795. doi: 10.1093/jac/dky111. [DOI] [PubMed] [Google Scholar]
- 15.Wang X., Wang Y., Zhou Y., et al. Emergence of a novel mobile colistin resistance gene, mcr-8, in NDM-producing Klebsiella pneumoniae. Emerging Microbes and Infections. 2018;7(1) doi: 10.1038/s41426-018-0124-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rolain J. M., Olaitan A. O. Plasmid-mediated colistin resistance: the final blow to colistin? International Journal of Antimicrobial Agents. 2016;47(1):4–5. doi: 10.1016/j.ijantimicag.2015.11.010. [DOI] [PubMed] [Google Scholar]
- 17.Ministère de la santé. Recommandations pour la prévention de la transmission croisée des bactéries hautement résistantes aux antibiotiques émergentes. 2014. [Google Scholar]
- 18.Sun J., Yang R. S., Zhang Q., et al. Co-transfer of bla NDM-5 and mcr-1 by an IncX3-X4 hybrid plasmid in Escherichia coli . Nature Microbiology. 2016;1:p. 16176. doi: 10.1038/nmicrobiol.2016.176. [DOI] [PubMed] [Google Scholar]
- 19.Lai C. C., Chuang Y. C., Chen C. C., Tang H. J. Coexistence of MCR-1 and NDM-9 in a clinical carbapenem-resistant Escherichia coli isolate. International Journal of Antimicrobial Agents. 2017;49(4) doi: 10.1016/j.ijantimicag.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 20.Delgado-Blas J. F., Ovejero C. M., Abadia-Patino L., Gonzalez-Zorn B. Coexistence of mcr-1 and blaNDM-1 in Escherichia coli from Venezuela. Antimicrobial Agents and Chemotherapy. 2016;60(10):6356–6358. doi: 10.1128/AAC.01319-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Conceição-Neto O. C., Aires C. A. M., Pereira N. F., et al. Detection of the plasmid-mediated mcr-1 gene in clinical KPC-2-producing Escherichia coli isolates in Brazil. International Journal of Antimicrobial Agents. 2017;50:282–284. doi: 10.1016/j.ijantimicag.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 22.Tacão M., Tavares S. R., Teixeira P., et al. mcr-1 and bla KPC-3 in Escherichia coli sequence type 744 after meropenem and colistin therapy, Portugal. Emerging Infectious Diseases. 2017;23(8):1419–1421. doi: 10.3201/eid2308.170162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beyrouthy R., Robin F., Lessene A., et al. MCR-1 and OXA-48 in vivo acquisition in KPC-producing Escherichia coli after colistin treatment. Antimicrobial Agents and Chemotherapy. 2017;61(8) doi: 10.1128/AAC.02540-16.e02540-16-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pulss S., Semmler T., Prenger-Berninghoff E., Bauerfeind R., Ewers C. First report of an Escherichia coli strain from swine carrying an OXA-181 carbapenemase and the colistin resistance determinant MCR-1. International Journal of Antimicrobial Agents. 2017;50(2):232–236. doi: 10.1016/j.ijantimicag.2017.03.014. [DOI] [PubMed] [Google Scholar]
- 25.Perry J. D. A decade of development of chromogenic culture media for clinical microbiology in an era of molecular diagnostics. Clinical Microbiology Reviews. 2017;30(2):449–479. doi: 10.1128/CMR.00097-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nordmann P., Poirel L. Strategies for identification of carbapenemase-producing Enterobacteriaceae. Journal of Antimicrobial Chemotherapy. 2013;68(3):487–489. doi: 10.1093/jac/dks426. [DOI] [PubMed] [Google Scholar]
- 27.Dortet L., Bréchard L., Poirel L., Nordmann P. Rapid detection of carbapenemase-producing Enterobacteriaceae from blood cultures. Clinical Microbiology and Infection. 2013;20(4):340–344. doi: 10.1128/jcm.00918-16. [DOI] [PubMed] [Google Scholar]
- 28.Nordmann P., Poirel L., Carrër A., Toleman M. A., Walsh T. R. How to detect NDM-1 producers. Journal of Clinical Microbiology. 2011;49(2):718–721. doi: 10.1128/jcm.01773-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Caniaux I., van Belkum A., Zambardi G., Poirel L., Gros M. F. MCR: modern colistin resistance. European Journal of Clinical Microbiology & Infectious Diseases. 2017;36(3):415–420. doi: 10.1007/s10096-016-2846-y. [DOI] [PubMed] [Google Scholar]
- 30.Falagas M. E., Makris G. C., Dimopoulos G., Matthaiou D. K. Heteroresistance: a concern of increasing clinical significance? Clinical Microbiology and Infection. 2008;14(2):101–104. doi: 10.1111/j.1469-0691.2007.01912.x. [DOI] [PubMed] [Google Scholar]
- 31.Lo-Ten-Foe J. R., de Smet A. M. G. A., Diederen B. M. W., Kluytmans J. A. J. W., van Keulen P. H. J. Comparative evaluation of the VITEK 2, disk diffusion, etest, broth microdilution, and agar dilution susceptibility testing methods for colistin in clinical isolates, including heteroresistant Enterobacter cloacae and Acinetobacter baumannii . Antimicrobial Agents and Chemotherapy. 2007;51(10):3726–3730. doi: 10.1128/aac.01406-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tan T. Y., Ng S. Y. Comparison of Etest, Vitek and agar dilution for susceptibility testing of colistin. Clinical Microbiology and Infection. 2007;13(5):541–544. doi: 10.1111/j.1469-0691.2007.01708.x. [DOI] [PubMed] [Google Scholar]
- 33.Bardet L. Development of New Tools for Detection of Colistin-Resistant Gram-Negative Bacteria. Marseille, France: Aix-Marseille Université; 2017. [Google Scholar]
- 34.Martin J. E., Lewis J. S. Selective culture screening for penicillinase-producing Neisseria gonorrhoeae . The Lancet. 1977;2(8038):605–606. doi: 10.1016/s0140-6736(77)91448-9. [DOI] [PubMed] [Google Scholar]
- 35.Thayer J. D., Martin J. E. Improved medium selective for cultivation of N. gonorrhoeae and N. meningitidis . Public Heal Reports. 1966;81(6):559–562. [PMC free article] [PubMed] [Google Scholar]
- 36.Martin J. E., Lester A. Transgrow, a medium for transport and growth of Neisseria gonorrhoeae and Neisseria meningitidis . HSMHA Health Reports. 1971;86(1):30–33. doi: 10.2307/4594086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Faur Y. C., Weisburd M. H., Wilson M. E., May P. S. A new medium for the isolation of pathogenic Neisseria (NYC medium). I. Formulation and comparisons with standard media. Health Laboratory Science. 1973;10(2):44–54. [PubMed] [Google Scholar]
- 38.Gilligan P. H., Gage P. A., Bradshaw L. M., Schidlow D. V., DeCicco B. T. Isolation medium for the recovery of Pseudomonas cepacia from respiratory secretions of patients with cystic fibrosis. Journal of Clinical Microbiology. 1985;22(1):5–8. doi: 10.1128/jcm.22.1.5-8.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Welch D. F., Muszynski M. J., Pai C. H., et al. Selective and differential medium for recovery of Pseudomonas cepacia from the respiratory tracts of patients with cystic fibrosis. Journal of Clinical Microbiology. 1987;25(9):1730–1734. doi: 10.1128/jcm.25.9.1730-1734.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Henry D. A., Campbell M. E., LiPuma J. J., Speert D. P. Identification of Burkholderia cepacia isolates from patients with cystic fibrosis and use of a simple new selective medium. Journal of Clinical Microbiology. 1997;35(3):614–619. doi: 10.1128/jcm.35.3.614-619.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dennis P. J. L., Bartlett C. L. R., Wright A. E. Comparison of isolation methods for Legionella spp.. Proceedings of the 2nd International Symposium; 1984; Washington, DC, USA. American Society; pp. 294–296. [Google Scholar]
- 42.Bopp C. A., Sumner J. W., Morris G. K., Wells J. G. Isolation of Legionella spp. from environmental water samples by low-pH treatment and use of a selective medium. Journal of Clinical Microbiology. 1981;13(4):714–719. doi: 10.1128/jcm.13.4.714-719.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ta A., Stout J., Yu V., Wagener M. Comparison of culture methods for monitoring Legionella species in hospital potable water systems and recommendations for standardization of such methods. Journal of Clinical Microbiology. 1995;33(8):2118–2123. doi: 10.1128/jcm.33.8.2118-2123.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stout J., Yu V. L., Vickers R. M., Shonnard J. Potable water supply as the hospital reservoir for Pittsburgh pneumonia agent. The Lancet. 1982;1(8270):471–472. doi: 10.1016/s0140-6736(82)91449-0. [DOI] [PubMed] [Google Scholar]
- 45.Edelstein P. H. Manual of Clinical Microbiology. 9th. Washington, DC, USA: American Society for Microbiology; 2007. Legionella ; pp. 835–849. [Google Scholar]
- 46.Murray P. R., Baron E., Jorgensen J. H., Landry M. L., Pfaller M. A. Manual of Clinical Microbiology. 9th. Washington, DC, USA: American Society for Microbiology; 2007. [Google Scholar]
- 47.Butzler J. P., Dekeyser P., Detrain M., Dehaen F. Related vibrio in stools. Journal of Pediatrics. 1973;82(3):493–495. doi: 10.1016/S0022-3476(73)80131-3. [DOI] [PubMed] [Google Scholar]
- 48.Skirrow M. B. Campylobacter enteritis: a “new” disease. British Medical Journal. 1977;2(6078):9–11. doi: 10.1136/bmj.2.6078.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang W. L., Blaser M., Cravens J. Isolation of Campylobacter . British Medical Journal. 1978;2(6129):p. 57. doi: 10.1136/bmj.2.6129.57-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bolton F. J., Robertson L. A selective medium for isolating Campylobacter jejuni/coli . Journal of Clinical Pathology. 1982;35(4):462–467. doi: 10.1136/jcp.35.4.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jones L. M., Morgan W. J. B. A preliminary report on a selective medium for the culture of Brucella, including fastidious types. Bulletin of the World Health Organization. 1958;19(1):200–203. [PMC free article] [PubMed] [Google Scholar]
- 52.Vanderzant C., Splittstoesser D. F. Compendium of Methods for the Microbiological Examination of Foods. Washington, DC, USA: American Public Health Association; 1992. [Google Scholar]
- 53.Ellner P. D., Stoessel C. J., Drakeford E., Vasi F. A new culture medium for medical bacteriology. American Journal of Clinical Pathology. 1966;45(4):502–504. doi: 10.1093/ajcp/45.4_ts.502. [DOI] [PubMed] [Google Scholar]
- 54.Curtis G. D. W., Nichols W. W., Falla T. J. Selective agents for Listeria can inhibit their growth. Letters in Applied Microbiology. 1989;8(5):169–172. doi: 10.1111/j.1472-765X.1989.tb00240.x. [DOI] [Google Scholar]
- 55.Lee W. H., McClain D. Improved Listeria monocytogenes selective agar. Applied and Environmental Microbiology. 1986;52(5):1215–1217. doi: 10.1128/aem.52.5.1215-1217.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.van Netten P., Perales I., van de Moosdijk A., Curtis G. D. W., Mossel D. A. A. Liquid and solid selective differential media for the detection and enumeration of L. monocytogenes and other Listeria spp. International Journal of Food Microbiology. 1989;8(4):299–316. doi: 10.1016/0168-1605(89)90001-9. [DOI] [PubMed] [Google Scholar]
- 57.Mossel D. A., Koopman M. J., Jongerius E. Enumeration of Bacillus cereus in foods. Applied Microbiology. 1967;15(3):650–653. doi: 10.1128/am.15.3.650-653.1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cohn M. L., Waggoner R. F., McClatchy J. K. The 7H11 medium for the cultivation of mycobacteria. American Review of Respiratory Disease. 1968;98(2):295–296. doi: 10.1164/arrd.1968.98.2.295. [DOI] [PubMed] [Google Scholar]
- 59.Angelotti R., Hall H. E., Foter M., Lewis K. M. Quantification of Clostridium perfringens in foods. Applied Microbiology. 1962;10(3):193–199. doi: 10.1128/am.10.3.193-199.1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Marshall R. Rapid technique for the enumeration of Clostridium perfringens . Applied Microbiology. 1965;13(4):559–563. doi: 10.1128/am.13.4.559-563.1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shahidi S. A., Ferguson A. R. New quantitative, qualitative, and confirmatory media for rapid analysis of food for Clostridium perfringens . Applied Microbiology. 1971;21(3):500–506. doi: 10.1128/am.21.3.500-506.1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Meinersmann R. J., Ladely S. R., Plumblee J. R., et al. Colistin resistance mcr-1-gene-bearing Escherichia coli strain from the United States. Genome Announcements. 2016;4(5):p. e00898-16. doi: 10.1128/genomeA.00898-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fernandes M. R., Moura Q., Sartori L., et al. Silent dissemination of colistin-resistant Escherichia coli in South America could contribute to the global spread of the mcr-1 gene. Eurosurveillance. 2016;21(17):1–6. doi: 10.2807/1560-7917.ES.2016.21.17.30214. [DOI] [PubMed] [Google Scholar]
- 64.Donà V., Bernasconi O. J., Kasraian S., Tinguely R., Endimiani A. A SYBR® green-based real-time PCR method for improved detection of mcr-1-mediated colistin resistance in human stool samples. Journal of Global Antimicrobial Resistance. 2017;9:57–60. doi: 10.1016/j.jgar.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 65.Monte D. F., Mem A., Fernandes M. R., et al. Chicken meat as a reservoir of colistin-resistant Escherichia coli strains carrying mcr-1 genes in South America. Antimicrobial Agents and Chemotherapy. 2017;61(5):p. e02718-16. doi: 10.1128/AAC.02718-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.von Wintersdorff C. J. H., Wolffs P. F. G., van Niekerk J. M., et al. Detection of the plasmid-mediated colistin-resistance gene mcr-1 in faecal metagenomes of Dutch travellers. Journal of Antimicrobial Chemotherapy. 2016;71(12):3416–3419. doi: 10.1093/jac/dkw328. [DOI] [PubMed] [Google Scholar]
- 67.Buess S., Nüesch-Inderbinen M., Stephan R., Zurfluh K. Assessment of animals as a reservoir for colistin resistance: no MCR-1/MCR-2-producing Enterobacteriaceae detected in Swiss livestock. Journal of Global Antimicrobial Resistance. 2017;8:33–34. doi: 10.1016/j.jgar.2016.11.001. [DOI] [PubMed] [Google Scholar]
- 68.Zurfluh K., Stephan R., Widmer A., et al. Screening for fecal carriage of MCR-producing Enterobacteriaceae in healthy humans and primary care patients. Antimicrobial Resistance & Infection Control. 2017;6(1):p. 28. doi: 10.1186/s13756-017-0186-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hu Y., Wang Y., Sun Q., et al. Colistin-resistance gene mcr-1 in children’s gut flora. International Journal of Antimicrobial Agents. 2017;50(4):593–597. doi: 10.1016/j.ijantimicag.2017.06.011. [DOI] [PubMed] [Google Scholar]
- 70.Wang Y., Tian G. B., Zhang R., et al. Prevalence, risk factors, outcomes, and molecular epidemiology of mcr-1-positive Enterobacteriaceae in patients and healthy adults from China: an epidemiological and clinical study. Lancet Infectious Diseases. 2017;17(4):390–399. doi: 10.1016/S1473-3099(16)30527-8. [DOI] [PubMed] [Google Scholar]
- 71.Wong S. C. Y., Tse H., Chen J. H. K., Cheng V. C. C., Ho P. L., Yuen K. Y. Colistin-resistant Enterobacteriaceae carrying the mcr-1 gene among patients in Hong Kong. Emerging Infectious Diseases. 2016;22(9):1667–1669. doi: 10.3201/eid2209.160091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Payne M., Croxen M. A., Lee T. D., et al. mcr-1-positive colistin-resistant Escherichia coli in traveler returning to Canada from China. Emerging Infectious Diseases. 2016;22(9):1673–1675. doi: 10.3201/eid2209.160177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Caspar Y., Maillet M., Pavese P., et al. mcr-1 colistin resistance in ESBL-producing Klebsiella pneumoniae, France. Emerging Infectious Diseases. 2017;23(5):874–876. doi: 10.3201/eid2305.161942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Terveer E. M., Nijhuis R. H. T., Crobach M. J. T., et al. Prevalence of colistin resistance gene (mcr-1) containing Enterobacteriaceae in feces of patients attending a tertiary care hospital and detection of a mcr-1 containing, colistin susceptible E. coli . PLoS One. 2017;12(6) doi: 10.1371/journal.pone.0178598.e0178598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nordmann P., Jayol A., Poirel L. A universal culture medium for screening polymyxin-resistant Gram-negative isolates. Journal of Clinical Microbiology. 2016;54(5):1395–1399. doi: 10.1128/JCM.00446-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Abdul Momin M. H. F., Bean D. C., Hendriksen R. S., Haenni M., Phee L. M., Wareham D. W. CHROMagar COL-APSE: a selective bacterial culture medium for the isolation and differentiation of colistin-resistant Gram-negative pathogens. Journal of Medical Microbiology. 2017;66(11):1554–1561. doi: 10.1099/jmm.0.000602. [DOI] [PubMed] [Google Scholar]
- 77.Bardet L., Le Page S., Leangapichart T., Rolain J. M. LBJMR medium: a new polyvalent culture medium for isolating and selecting vancomycin and colistin-resistant bacteria. BMC Microbiology. 2017;17(1):1–10. doi: 10.1186/s12866-017-1128-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nordmann P., Jayol A., Poirel L. Rapid detection of polymyxin resistance in Enterobacteriaceae. Emerging Infectious Diseases. 2016;22(6):1038–1043. doi: 10.3201/eid2206.151840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jayol A., Saly M., Nordmann P., Ménard A., Poirel L., Dubois V. Hafnia, an enterobacterial genus naturally resistant to colistin revealed by three susceptibility testing methods. Journal of Antimicrobial Chemotherapy. 2017;72(9):1–5. doi: 10.1093/jac/dkx154. [DOI] [PubMed] [Google Scholar]
- 80.Jayol A., Dubois V., Poirel L., Nordmann P. Rapid detection of polymyxin-resistant Enterobacteriaceae from blood cultures. Journal of Clinical Microbiology. 2016;54(9):2273–2277. doi: 10.1128/JCM.00918-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Bakthavatchalam Y. D., Veeraraghavan B. Challenges, issues and warnings from CLSI and EUCAST working group on polymyxin susceptibility testing. Journal of Clinical and Diagnostic Research. 2017;11:DL03–DL04. doi: 10.7860/JCDR/2017/27182.10375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Giske C. G., Kahlmeter G. Colistin antimicrobial susceptibility testing—can the slow and challenging be replaced by the rapid and convenient? Clinical Microbiology and Infection. 2017;24(2):93–94. doi: 10.1016/j.cmi.2017.10.007. [DOI] [PubMed] [Google Scholar]
- 83.Jayol A., Nordmann P., Lehours P., et al. Comparison of methods for detection of plasmid-mediated and chromosomally encoded colistin resistance in Enterobacteriaceae. Clinical Microbiology and Infection. 2017;51(2):3726–3730. doi: 10.1016/j.cmi.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 84.Poirel L., Larpin Y., Dobias J., et al. Rapid polymyxin NP test for the detection of polymyxin resistance mediated by the mcr-1/mcr-2 genes. Diagnostic Microbiology and Infectious Disease. 2017;90(1):7–10. doi: 10.1016/j.diagmicrobio.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 85.Simar S., Sibley D., Ashcraft D., Pankey G. Evaluation of the rapid polymyxin NP test for polymyxin B resistance detection using Enterobacter cloacae and Enterobacter aerogenes isolates. Journal of Clinical Microbiology. 2017;55(10):3016–3020. doi: 10.1128/JCM.00934-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tamayo M., Santiso R., Otero F., et al. Rapid determination of colistin resistance in clinical strains of Acinetobacter baumannii by use of the Micromax assay. Journal of Clinical Microbiology. 2013;51(11):3675–3682. doi: 10.1128/JCM.01787-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Osei Sekyere J., Govinden U., Essack S. Y. Review of established and innovative detection methods for carbapenemase-producing Gram-negative bacteria. Journal of Applied Microbiology. 2015;119(5):1219–1233. doi: 10.1111/jam.12918. [DOI] [PubMed] [Google Scholar]
- 88.Ghebremedhin B., Halstenbach A., Smiljanic M., Kaase M., Ahmad-Nejad P. MALDI-TOF MS based carbapenemase detection from culture isolates and from positive blood culture vials. Annals of Clinical Microbiology and Antimicrobials. 2016;15(1):p. 5. doi: 10.1186/s12941-016-0120-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hrabák J., Chudáčková E., Papagiannitsis C. C. Detection of carbapenemases in Enterobacteriaceae: a challenge for diagnostic microbiological laboratories. Clinical Microbiology and Infection. 2014;20(9):839–853. doi: 10.1111/1469-0691.12678. [DOI] [PubMed] [Google Scholar]
- 90.Seng P., Drancourt M., Gouriet F., et al. Ongoing revolution in bacteriology: routine identification of bacteria by matrix-assisted laser desorption ionization time-of-flight mass spectrometry. Clinical Infectious Diseases. 2009;49(4):543–551. doi: 10.1086/600885. [DOI] [PubMed] [Google Scholar]
- 91.Larrouy-Maumus G., Clements A., Filloux A., McCarthy R. R., Mostowy S. Direct detection of lipid A on intact Gram-negative bacteria by MALDI-TOF mass spectrometry. Journal of Microbiological Methods. 2016;120:68–71. doi: 10.1016/j.mimet.2015.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sekyere J. O., Govinden U., Bester L. A., Essack S. Y. Colistin and tigecycline resistance in carbapenemase-producing Gram-negative bacteria: emerging resistance mechanisms and detection methods. Journal of Applied Microbiology. 2016;121(3):601–617. doi: 10.1111/jam.13169. [DOI] [PubMed] [Google Scholar]
- 93.Dortet L., Bonnin R. A., Pennisi I., et al. Rapid detection and discrimination of chromosome- and MCR-plasmid-mediated resistance to polymyxins by MALDI-TOF MS in Escherichia coli: the MALDIxin test. Journal of Antimicrobial Chemotherapy. 2018:1–9. doi: 10.1093/jac/dky330. In press. [DOI] [PubMed] [Google Scholar]
- 94.Stojanoski V., Sankaran B., Prasad B. V. V., Poirel L., Nordmann P., Palzkill T. Structure of the catalytic domain of the colistin resistance enzyme MCR-1. BMC Biology. 2016;14(1):p. 81. doi: 10.1186/s12915-016-0303-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hu M., Guo J., Cheng Q., et al. Crystal structure of Escherichia coli originated MCR-1, a phosphoethanolamine transferase for colistin resistance. Scientific Reports. 2016;6(1):p. 38793. doi: 10.1038/srep38793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ma G., Zhu Y., Yu Z., Ahmad A., Zhang H. High resolution crystal structure of the catalytic domain of MCR-1. Scientific Reports. 2016;6(1):p. 39540. doi: 10.1038/srep39540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hinchliffe P., Yang Q. E., Portal E., et al. Insights into the mechanistic basis of plasmid-mediated colistin resistance from crystal structures of the catalytic domain of MCR-1. Scientific Reports. 2017;7:p. 39392. doi: 10.1038/srep39392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Coppi M., Cannatelli A., Antonelli A., et al. A simple phenotypic method for screening of MCR-1-mediated colistin resistance. Clinical Microbiology and Infection. 2017;24(2):201.e1–201.e3. doi: 10.1016/j.cmi.2017.08.011. [DOI] [PubMed] [Google Scholar]
- 99.Esposito F., Fernandes M. R., Lopes R., et al. Detection of colistin-resistant mcr-1-positive Escherichia coli by use of assays based on inhibition by EDTA and zeta potential. Journal of Clinical Microbiology. 2017;55(12):3454–3465. doi: 10.1128/JCM.00835-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.European Committee on Antimicrobial Susceptibility Testing (EUCAST) Breakpoint Tables for Interpretation of MICs and Zone Diameters. Vol. 8. Växjö, Sweden: EUCAST; 2018. [Google Scholar]
- 101.CLSI, Clinical and Laboratory Standards Institute. M07–A10: Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically; Approved Standard. 10th. Vol. 35. Wayne, PA, USA: CLSI; 2015. [Google Scholar]
- 102.ISO 20776-1:2006. Clinical Laboratory Testing and In Vitro Diagnostic Test Systems–Susceptibility Testing of Infectious Agents and Evaluation of Performance of Antimicrobial Susceptibility Test Devices–Part 1: Reference Method for Testing the In Vitro Activity of Antimicrobial Agents against Rapidly Growing Aerobic Bacteria Involved in Infectious Diseases n.d. https://www.iso.org/standard/41630.html. [Google Scholar]
- 103.Clinical and Laboratory Standards. M100–S27: Performance Standards for Antimicrobial Susceptibility Testing. Wayne, PA, USA: Clinical and Laboratory Standards; 2017. [Google Scholar]
- 104.European Committee on Antimicrobial Susceptibility Testing (EUCAST) Routine and Extended Internal Quality Control for Mic Determination and Disk Diffusion as Recommended by EUCAST. Vol. 8. Växjö, Sweden: EUCAST; 2018. [Google Scholar]
- 105.Jerke K. H., Lee M. J., Humphries R. M. Polymyxin susceptibility testing: a cold case reopened. Clinical Microbiology Newsletter. 2016;38(9):69–77. doi: 10.1016/j.clinmicnews.2016.04.003. [DOI] [Google Scholar]
- 106.Humphries R. M. Susceptibility testing of the polymyxins: where are we now? Pharmacotherapy. 2015;35(1):22–27. doi: 10.1002/phar.1505. [DOI] [PubMed] [Google Scholar]
- 107.Landman D., Salamera J., Quale J. Irreproducible and uninterpretable polymyxin B MICs for Enterobacter cloacae and Enterobacter aerogenes . Journal of Clinical Microbiology. 2013;51(12):4106–4111. doi: 10.1128/JCM.02129-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Poudyal A., Howden B. P., Bell J. M., et al. In vitro pharmacodynamics of colistin against multidrug-resistant Klebsiella pneumoniae . Journal of Antimicrobial Chemotherapy. 2008;62(6):1311–1318. doi: 10.1093/jac/dkn425. [DOI] [PubMed] [Google Scholar]
- 109.ISO 20776-2:2007. Clinical Laboratory Testing and In Vitro Diagnostic Test Systems–Susceptibility Testing of Infectious Agents and Evaluation of Performance of Antimicrobial Susceptibility Test Devices–Part 2: Evaluation of Performance of Antimicrobial Susceptibility Test Devices n.d. 2018. https://www.iso.org/standard/41631.html. [Google Scholar]
- 110.Dafopoulou K., Zarkotou O., Dimitroulia E., et al. Comparative evaluation of colistin susceptibility testing methods among carbapenem-nonsusceptible Klebsiella pneumoniae and Acinetobacter baumannii clinical isolates. Antimicrobial Agents and Chemotherapy. 2015;59(8):4625–4630. doi: 10.1128/AAC.00868-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Sutherland C. A., Nicolau D. P. To add or not to add polysorbate 80: impact on colistin MICs for clinical strains of Enterobacteriaceae and Pseudomonas aeruginosa and quality controls. Journal of Clinical Microbiology. 2014;52(10):p. 3810. doi: 10.1128/JCM.01454-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sader H. S., Rhomberg P. R., Flamm R. K., Jones R. N. Use of a surfactant (polysorbate 80) to improve MIC susceptibility testing results for polymyxin B and colistin. Diagnostic Microbiology and Infectious Disease. 2012;74(4):412–414. doi: 10.1016/j.diagmicrobio.2012.08.025. [DOI] [PubMed] [Google Scholar]
- 113.Albur M., Noel A., Bowker K., MacGowan A. Colistin susceptibility testing: time for a review. Journal of Antimicrobial Chemotherapy. 2014;69(5):1432–1434. doi: 10.1093/jac/dkt503. [DOI] [PubMed] [Google Scholar]
- 114.Singhal L., Sharma M., Verma S., et al. Comparative Evaluation of Broth Microdilution with Polystyrene and Glass-Coated Plates, Agar Dilution, E-Test, Vitek, and Disk Diffusion for Susceptibility Testing of Colistin and Polymyxin B on Carbapenem-Resistant Clinical Isolates of Acinetobacter baum. Microbial Drug Resistance. 2018 doi: 10.1089/mdr.2017.0251. [DOI] [PubMed] [Google Scholar]
- 115.Lee S. Y., Shin J. H., Lee K., et al. Comparison of the Vitek 2, MicroScan, and Etest methods with the agar dilution method in assessing colistin susceptibility of bloodstream isolates of Acinetobacter species from a Korean University Hospital. Journal of Clinical Microbiology. 2013;51(6):1924–1926. doi: 10.1128/JCM.00427-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Maalej S. M., Meziou M. R., Rhimi F. M., Hammami A. Comparison of disc diffusion, Etest and agar dilution for susceptibility testing of colistin against Enterobacteriaceae. Letters in Applied Microbiology. 2011;53(5):546–551. doi: 10.1111/j.1472-765X.2011.03145.x. [DOI] [PubMed] [Google Scholar]
- 117.Behera B., Mathur P., Das A., et al. Evaluation of susceptibility testing methods for polymyxin. International Journal of Infectious Diseases. 2010;14(7):e596–e601. doi: 10.1016/j.ijid.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 118.Tan T. Y., Ng L. S. Y., Poh K. Susceptibility testing of unconventional antibiotics against multiresistant Acinetobacter spp. by agar dilution and Vitek 2. Diagnostic Microbiology and Infectious Disease. 2007;58(3):357–361. doi: 10.1016/j.diagmicrobio.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 119.Tan T. Y. Comparison of three standardized disc susceptibility testing methods for colistin. Journal of Antimicrobial Chemotherapy. 2006;58(4):864–867. doi: 10.1093/jac/dkl330. [DOI] [PubMed] [Google Scholar]
- 120.Moskowitz S. M., Garber E., Chen Y., et al. Colistin susceptibility testing: evaluation of reliability for cystic fibrosis isolates of Pseudomonas aeruginosa and Stenotrophomonas maltophilia . Journal of Antimicrobial Chemotherapy. 2010;65(7):1416–1423. doi: 10.1093/jac/dkq131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hogardt M., Schmoldt S., Götzfried M., Adler K., Heesemann J. Pitfalls of polymyxin antimicrobial susceptibility testing of Pseudomonas aeruginosa isolated from cystic fibrosis patients. Journal of Antimicrobial Chemotherapy. 2004;54(6):1057–1061. doi: 10.1093/jac/dkh470. [DOI] [PubMed] [Google Scholar]
- 122.Richter M., Rosselló-Móra R. Shifting the genomic gold standard for the prokaryotic species definition. Proceedings of the National Academy of Sciences of the United States of America. 2009;106(45):19126–19131. doi: 10.1073/pnas.0906412106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Boyen F., Vangroenweghe F., Butaye P., et al. Disk prediffusion is a reliable method for testing colistin susceptibility in porcine E. coli strains. Veterinary Microbiology. 2010;144(3-4):359–362. doi: 10.1016/j.vetmic.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 124.Nemec A., Dijkshoorn L. Variations in colistin susceptibility among different species of the genus Acinetobacter . Journal of Antimicrobial Chemotherapy. 2010;65(2):367–369. doi: 10.1093/jac/dkp440. [DOI] [PubMed] [Google Scholar]
- 125.Nicodemo A. C., Araujo M. R. E., Ruiz A. S., Gales A. C. In vitro susceptibility of Stenotrophomonas maltophilia isolates: comparison of disc diffusion, Etest and agar dilution methods. Journal of Antimicrobial Chemotherapy. 2004;53(4):604–608. doi: 10.1093/jac/dkh128. [DOI] [PubMed] [Google Scholar]
- 126.Goldstein F. W., Ly A., Kitzis M. D. Comparison of Etest with agar dilution for testing the susceptibility of Pseudomonas aeruginosa and other multidrug-resistant bacteria to colistin. Journal of Antimicrobial Chemotherapy. 2007;59(5):1039–1040. doi: 10.1093/jac/dkm046. [DOI] [PubMed] [Google Scholar]
- 127.Gales A. C., Reis A. O., Jones R. N. Contemporary assessment of antimicrobial susceptibility testing methods for polymyxin B and colistin: review of available interpretative criteria and quality control guidelines. Journal of Clinical Microbiology. 2001;39(1):183–190. doi: 10.1128/JCM.39.1.183-190.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hindler J. A., Humphries R. M. Colistin MIC variability by method for contemporary clinical isolates of multidrug-resistant Gram-negative bacilli. Journal of Clinical Microbiology. 2013;51(6):1678–1684. doi: 10.1128/JCM.03385-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Vourli S., Dafopoulou K., Vrioni G., Tsakris A., Pournaras S. Evaluation of two automated systems for colistin susceptibility testing of carbapenem-resistant Acinetobacter baumannii clinical isolates. Journal of Antimicrobial Chemotherapy. 2017;72(9):2528–2530. doi: 10.1093/jac/dkx186. [DOI] [PubMed] [Google Scholar]
- 130.Turlej-Rogacka A., Xavier B. B., Janssens L., et al. Evaluation of colistin stability in agar and comparison of four methods for MIC testing of colistin. European Journal of Clinical Microbiology & Infectious Diseases. 2017;37(2):345–353. doi: 10.1007/s10096-017-3140-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Bauer A. W., Kirby W. M., Sherris J. C., Turck M. Antibiotic susceptibility testing by a standardized single disk method. American Journal of Clinical Pathology. 1966;45(4):493–496. [PubMed] [Google Scholar]
- 132.Rojas L. J., Salim M., Cober E., et al. Colistin resistance in carbapenem-resistant Klebsiella pneumoniae: laboratory detection and impact on mortality. Clinical Infectious Diseases. 2016;314:p. ciw805. doi: 10.1093/cid/ciw805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Perez L. R. R. Evaluation of polymyxin susceptibility profile among KPC-producing Klebsiella pneumoniae using Etest and MicroScan WalkAway automated system. APMIS. 2015;123(11):951–954. doi: 10.1111/apm.12438. [DOI] [PubMed] [Google Scholar]
- 134.Lat A., Clock S. A., Wu F., et al. Comparison of polymyxin B, tigecycline, cefepime, and meropenem MICs for KPC-producing Klebsiella pneumoniae by broth microdilution, Vitek 2, and Etest. Journal of Clinical Microbiology. 2011;49(5):1795–1798. doi: 10.1128/JCM.02534-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.van der Heijden I. M., Levin A. S., De Pedri E. H., et al. Comparison of disc diffusion, Etest and broth microdilution for testing susceptibility of carbapenem-resistant P. aeruginosa to polymyxins. Annals of Clinical Microbiology and Antimicrobials. 2007;6(1):p. 8. doi: 10.1186/1476-0711-6-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Piewngam P., Kiratisin P. Comparative assessment of antimicrobial susceptibility testing for tigecycline and colistin against Acinetobacter baumannii clinical isolates, including multidrug-resistant isolates. International Journal of Antimicrobial Agents. 2014;44(5):396–401. doi: 10.1016/j.ijantimicag.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 137.Sinirtaş M., Akalin H., Gedikoğlu S. Investigation of colistin sensitivity via three different methods in Acinetobacter baumannii isolates with multiple antibiotic resistance. International Journal of Infectious Diseases. 2009;13(5):e217–e220. doi: 10.1016/j.ijid.2008.12.012. [DOI] [PubMed] [Google Scholar]
- 138.Arroyo L. A., Garcia-Curiel A., Pachón-Ibáñez M. E., et al. Reliability of the E-test method for detection of colistin resistance in clinical isolates of Acinetobacter baumannii . Journal of Clinical Microbiology. 2005;43(2):903–905. doi: 10.1128/jcm.43.2.903-905.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Girardello R., Bispo P. J. M., Yamanaka T. M., Gales A. C. Cation concentration variability of four distinct Mueller-Hinton agar brands influences polymyxin B susceptibility results. Journal of Clinical Microbiology. 2012;50(7):2414–2418. doi: 10.1128/JCM.06686-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Bardet L., Baron S., Leangapichart T., Okdah L., Diene S. M., Rolain J. M. Deciphering heteroresistance to colistin in a Klebsiella pneumoniae isolate from Marseille, France. Antimicrobial Agents and Chemotherapy. 2017;61(6):p. e00356-17. doi: 10.1128/AAC.00356-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Galani I., Kontopidou F., Souli M., et al. Colistin susceptibility testing by Etest and disk diffusion methods. International Journal of Antimicrobial Agents. 2008;31(5):434–439. doi: 10.1016/j.ijantimicag.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 142.Jouy E., Haenni M., Le Devendec L., et al. Improvement in routine detection of colistin resistance in E. coli isolated in veterinary diagnostic laboratories. Journal of Microbiological Methods. 2017;132:125–127. doi: 10.1016/j.mimet.2016.11.017. [DOI] [PubMed] [Google Scholar]
- 143.Matuschek E., Åhman J., Webster C., Kahlmeter G. Antimicrobial susceptibility testing of colistin–evaluation of seven commercial MIC products against standard broth microdilution for Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Acinetobacter spp. Clinical Microbiology and Infection. 2017 doi: 10.1016/j.cmi.2017.11.020. [DOI] [PubMed] [Google Scholar]
- 144.Plésiat P., Jeannot K., Triponney P. Évaluation comparative de la détermination du test de sensibilité à la colistine UMIC (Biocentric) chez Pseudomonas aeruginosa. Proceedings of the 36ème Réunion Interdiscip. Chim. Anti-Infectieuse; December 2016; Paris, France. [Google Scholar]
- 145.Bardet L., Okdah L., Baron S., Le Page S., Rolain J. Évaluation du test UMIC Colistine de détermination de la CMI. Proceedings of the 37ème Réunion Interdiscip. Chim. Anti-Infectieuse; December 2017; Paris, France. [Google Scholar]
- 146.Carretto E., Brovarone F., Russello G., et al. Clinical validation of the Sensitest Colistin, a broth microdilution based method to evaluate colistin MICs. Journal of Clinical Microbiology. 2018;56(4) doi: 10.1128/JCM.01523-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Chew K. L., La M. V., Lin R. T. P., Teo J. W. P. Colistin and polymyxin B susceptibility testing for carbapenem-resistant and mcr-positive Enterobacteriaceae: comparison of Sensititre, MicroScan, Vitek 2, and Etest with broth microdilution. Journal of Clinical Microbiology. 2017;55(9):2609–2616. doi: 10.1128/JCM.00268-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Cimmino T., Le Page S., Raoult D., Rolain J. M. Contemporary challenges and opportunities in the diagnosis and outbreak detection of multidrug-resistant infectious disease. Expert Review of Molecular Diagnostics. 2016;16(11):1163–1175. doi: 10.1080/14737159.2016.1244005. [DOI] [PubMed] [Google Scholar]
- 149.Giani T., Morosini M. I., D’Andrea M. M., García-Castillo M., Rossolini G. M., Cantón R. Assessment of the PhoenixTM automated system and EUCAST breakpoints for antimicrobial susceptibility testing against isolates expressing clinically relevant resistance mechanisms. Clinical Microbiology and Infection. 2012;18(11):E452–E458. doi: 10.1111/j.1469-0691.2012.03980.x. [DOI] [PubMed] [Google Scholar]
- 150.Skov R. L., Monnet D. L. Plasmid-mediated colistin resistance (mcr-1 gene): three months later, the story unfolds. Eurosurveillance. 2016;21(9):p. 30155. doi: 10.2807/1560-7917.es.2016.21.9.30155. [DOI] [PubMed] [Google Scholar]
- 151.Bontron S., Poirel L., Nordmann P. Real-time PCR for detection of plasmid-mediated polymyxin resistance (mcr-1) from cultured bacteria and stools. Journal of Antimicrobial Chemotherapy. 2016;71(8):2318–2320. doi: 10.1093/jac/dkw139. [DOI] [PubMed] [Google Scholar]
- 152.Chabou S., Leangapichart T., Okdah L., Le Page S., Hadjadj L., Rolain J. M. M. Real-time quantitative PCR assay with Taqman® probe for rapid detection of MCR-1 plasmid-mediated colistin resistance. New Microbes and New Infections. 2016;13:71–74. doi: 10.1016/j.nmni.2016.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Quan J., Li X., Chen Y. Prevalence of mcr-1 in Escherichia coli and Klebsiella pneumoniae recovered from bloodstream infections in China: a multicentre longitudinal study. The Lancet Infectious Diseases. 2017;17(4):400–410. doi: 10.1016/S1473-3099(16)30528-X. [DOI] [PubMed] [Google Scholar]
- 154.Elnahriry S. S., Khalifa H. O., Soliman A. M., et al. Emergence of plasmid-mediated colistin resistance gene mcr-1 in a clinical Escherichia coli isolate from Egypt. Antimicrobial Agents and Chemotherapy. 2016;60(5):3249–3250. doi: 10.1128/AAC.00269-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Falgenhauer L., Waezsada S. E., Yao Y., et al. Colistin resistance gene mcr-1 in extended-spectrum beta-lactamase-producing and carbapenemase-producing Gram-negative bacteria in Germany. Lancet Infectious Diseases. 2016;16(3):282–283. doi: 10.1016/S1473-3099(16)00009-8. [DOI] [PubMed] [Google Scholar]
- 156.Ye H., Li Y., Li Z., et al. Diversified mcr-1-harbouring plasmid reservoirs confer resistance to colistin in human gut microbiota. mBio. 2016;7(2):p. e00177-16. doi: 10.1128/mBio.00177-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Walkty A., Karlowsky J. A., Adam H. J., et al. Frequency of MCR-1-mediated colistin resistance among Escherichia coli clinical isolates obtained from patients in Canadian hospitals (CANWARD 2008–2015) CMAJ Open. 2016;4(4):E641–E645. doi: 10.9778/cmajo.20160080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Gao R., Hu Y., Li Z., et al. Dissemination and mechanism for the MCR-1 colistin resistance. PLoS Pathogens. 2016;12(11):p. e1005957. doi: 10.1371/journal.ppat.1005957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Cannatelli A., Giani T., Antonelli A., Principe L., Luzzaro F., Rossolini G. M. First detection of the mcr-1 colistin resistance gene in Escherichia coli in Italy. Antimicrobial Agents and Chemotherapy. 2016;60(5):3257–3258. doi: 10.1128/AAC.00246-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Wright G. D. Antibiotic resistance in the environment: a link to the clinic? Current Opinion in Microbiology. 2010;13(5):589–594. doi: 10.1016/j.mib.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 161.Lekunberri I., Balcázar J. L., Borrego C. M. Detection and quantification of the plasmid-mediated mcr-1 gene conferring colistin resistance in wastewater. International Journal of Antimicrobial Agents. 2017;50(6):734–736. doi: 10.1016/j.ijantimicag.2017.08.018. [DOI] [PubMed] [Google Scholar]
- 162.Irrgang A., Roschanski N., Tenhagen B. A., et al. Prevalence of mcr-1 in E. coli from livestock and food in Germany, 2010–2015. PLoS One. 2016;11(7) doi: 10.1371/journal.pone.0159863.e0159863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Nijhuis R. H. T., Veldman K. T., Schelfaut J., et al. Detection of the plasmid-mediated colistin-resistance gene mcr-1 in clinical isolates and stool specimens obtained from hospitalized patients using a newly developed real-time PCR assay. Journal of Antimicrobial Chemotherapy. 2016;71(8):2344–2346. doi: 10.1093/jac/dkw192. [DOI] [PubMed] [Google Scholar]
- 164.Yang D., Qiu Z., Shen Z., et al. The occurrence of the colistin resistance gene mcr-1 in the Haihe River (China) International Journal of Environmental Research and Public Health. 2017;14(6):p. 576. doi: 10.3390/ijerph14060576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Snesrud E., Ong A. C., Corey B. Analysis of serial isolates of mcr-1-positive Escherichia coli reveals a highly active IS Apl1 transposon. Antimicrobial Agents and Chemotherapy. 2017;61(5):p. e00056-17. doi: 10.1128/AAC.00056-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Lima Barbieri N., Nielsen D. W., Wannemuehler Y., et al. mcr-1 identified in avian pathogenic Escherichia coli (APEC) PLoS One. 2017;12(3) doi: 10.1371/journal.pone.0172997.e0172997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Sun J., Xu Y., Gao R., et al. Deciphering MCR-2 colistin resistance. mBio. 2017;8(3):p. e00625-17. doi: 10.1128/mBio.00625-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Liassine N., Assouvie L., Descombes M. C., et al. Very low prevalence of MCR-1/MCR-2 plasmid-mediated colistin resistance in urinary tract Enterobacteriaceae in Switzerland. International Journal of Infectious Diseases. 2016;51:4–5. doi: 10.1016/j.ijid.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 169.Simmen S., Zurfluh K., Nüesch-Inderbinen M., Schmitt S. Investigation for the colistin resistance genes mcr-1 and mcr-2 in clinical Enterobacteriaceae isolates from cats and dogs in Switzerland. ARC Journal of Animal and Veterinary Sciences. 2016;2(4):26–29. doi: 10.20431/2455-2518.0204004. [DOI] [Google Scholar]
- 170.Roschanski N., Falgenhauer L., Grobbel M., et al. Retrospective survey of mcr-1 and mcr-2 in German pig-fattening farms, 2011-2012. International Journal of Antimicrobial Agents. 2017;50(2):266–271. doi: 10.1016/j.ijantimicag.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 171.Poirel L., Jayol A., Nordmann P. Polymyxins: antibacterial activity, susceptibility testing, and resistance mechanisms encoded by plasmids or chromosomes. Clinical Microbiology Reviews. 2017;30(2):557–596. doi: 10.1128/CMR.00064-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Li J., Shi X., Yin W., et al. A multiplex SYBR Green real-time PCR assay for the detection of three colistin resistance genes from cultured bacteria, feces, and environment samples. Frontiers in Microbiology. 2017;8:1–5. doi: 10.3389/fmicb.2017.02078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Rita Rebelo A., Bortolaia V., Kjeldgaard J. S., et al. Multiplex PCR for detection of plasmid-mediated colistin resistance determinants, mcr-1, mcr-2, mcr-3, mcr-4 and mcr-5 for surveillance purposes. Eurosurveillance. 2018;23(6) doi: 10.2807/1560-7917.ES.2018.23.6.17-00672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Sekizuka T., Kawanishi M., Ohnishi M., et al. Elucidation of quantitative structural diversity of remarkable rearrangement regions, shufflons, in IncI2 plasmids. Scientific Reports. 2017;7(1):p. 928. doi: 10.1038/s41598-017-01082-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Doumith M., Godbole G., Ashton P., et al. Detection of the plasmid-mediated mcr-1 gene conferring colistin resistance in human and food isolates of Salmonella enterica and Escherichia coli in England and Wales. Journal of Antimicrobial Chemotherapy. 2016;71(8):2300–2305. doi: 10.1093/jac/dkw093. [DOI] [PubMed] [Google Scholar]
- 176.Stoesser N., Mathers A. J., Moore C. E., Day N. P. J., Crook D. W. Colistin resistance gene mcr-1 and pHNSHP45 plasmid in human isolates of Escherichia coli and Klebsiella pneumoniae . Lancet Infectious Diseases. 2016;16(3):285–286. doi: 10.1016/S1473-3099(16)00010-4. [DOI] [PubMed] [Google Scholar]
- 177.Li R., Xie M., Lv J., Wai-Chi Chan E., Chen S. Complete genetic analysis of plasmids carrying mcr-1 and other resistance genes in an Escherichia coli isolate of animal origin. Journal of Antimicrobial Chemotherapy. 2017;72(3):696–699. doi: 10.1093/jac/dkw509. [DOI] [PubMed] [Google Scholar]
- 178.Veldman K., van Essen-Zandbergen A., Rapallini M., et al. Location of colistin resistance gene mcr-1 in Enterobacteriaceae from livestock and meat. Journal of Antimicrobial Chemotherapy. 2016;71(8):2340–2342. doi: 10.1093/jac/dkw181. [DOI] [PubMed] [Google Scholar]
- 179.Campos J., Cristino L., Peixe L., Antunes P. MCR-1 in multidrug-resistant and copper-tolerant clinically relevant Salmonella 1,4,[5],12:i:- and S. Rissen clones in Portugal, 2011 to 2015. Eurosurveillance. 2016;21(26):p. 30270. doi: 10.2807/1560-7917.ES.2016.21.26.30270. [DOI] [PubMed] [Google Scholar]
- 180.Anjum M. F., Duggett N. A., AbuOun M., et al. Colistin resistance in Salmonella and Escherichia coli isolates from a pig farm in Great Britain. Journal of Antimicrobial Chemotherapy. 2016;71(8):2306–2313. doi: 10.1093/jac/dkw149. [DOI] [PubMed] [Google Scholar]
- 181.Poirel L., Kieffer N., Brink A., Coetze J., Jayol A., Nordmann P. Genetic features of MCR-1-producing colistin-resistant Escherichia coli isolates in South Africa. Antimicrobial Agents and Chemotherapy. 2016;60(7):4394–4397. doi: 10.1128/AAC.00444-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Bernasconi O. J., Principe L., Tinguely R., et al. Evaluation of a new commercial microarray platform for the simultaneous detection of β-lactamase and Mcr-1/-2 genes in Enterobacteriaceae. Journal of Clinical Microbiology. 2017;55(10):3138–3141. doi: 10.1128/JCM.01056-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Imirzalioglu C., Falgenhauer L., Schmiedel J., et al. Evaluation of a LAMP-based assay for the rapid detection of plasmid-encoded colistin resistance gene mcr-1 in Enterobacteriaceae isolates. Antimicrobial Agents and Chemotherapy. 2017;61(4):p. e02326-16. doi: 10.1128/AAC.02326-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Zou D., Huang S., Lei H., et al. Sensitive and rapid detection of the plasmid-encoded colistin-resistance Gene mcr-1 in Enterobacteriaceae isolates by loop-mediated isothermal amplification. Frontiers in Microbiology. 2017;8:1–7. doi: 10.3389/fmicb.2017.02356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Martinez J. L., Coque T. M., Baquero F. What is a resistance gene? Ranking risk in resistomes. Nature Reviews Microbiology. 2015;13(2):116–123. doi: 10.1038/nrmicro3399. [DOI] [PubMed] [Google Scholar]
- 186.Wang Y., Zhang R., Li J., et al. Comprehensive resistome analysis reveals the prevalence of NDM and MCR-1 in Chinese poultry production. Nature Microbiology. 2017;2:p. 16260. doi: 10.1038/nmicrobiol.2016.260. [DOI] [PubMed] [Google Scholar]
- 187.Gundogdu A., Nalbantoglu O. U. Humans as a source of colistin resistance: in silico analysis of public metagenomes for the mcr-1 gene in the gut microbiome. Erciyes Medical Journal. 2016;38(2):59–61. doi: 10.5152/etd.2016.0012. [DOI] [Google Scholar]
- 188.Thanh D. P., Tuyen H. T., Nguyen T. N. T., et al. Inducible colistin resistance via a disrupted plasmid-borne mcr-1 gene in a 2008 Vietnamese Shigella sonnei isolate. Journal of Antimicrobial Chemotherapy. 2016;71(8):2314–2317. doi: 10.1093/jac/dkw173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Meinersmann R. J., Ladely S. R., Bono J. L., et al. Complete genome sequence of a colistin resistance gene (mcr-1)-bearing isolate of Escherichia coli from the United States. Genome Announcements. 2016;4(6):p. e01283-16. doi: 10.1128/genomeA.01283-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Kluytmans-van den Bergh M. F., Huizinga P., Bonten M. J., et al. Presence of mcr-1-positive Enterobacteriaceae in retail chicken meat but not in humans in the Netherlands since 2009. Eurosurveillance. 2016;21(9):p. 30149. doi: 10.2807/1560-7917.ES.2016.21.9.30149. [DOI] [PubMed] [Google Scholar]
- 191.Malhotra-Kumar S., Xavier B. B., Das A. J., et al. Colistin-resistant Escherichia coli harbouring mcr-1 isolated from food animals in Hanoi, Vietnam. Lancet Infectious Diseases. 2016;16(3):286–287. doi: 10.1016/S1473-3099(16)00014-1. [DOI] [PubMed] [Google Scholar]
- 192.McGann P., Snesrud E., Maybank R., et al. Escherichia coli harboring mcr-1 and bla CTX-M on a novel IncF plasmid: first report of mcr-1 in the USA. Antimicrobial Agents and Chemotherapy. 2016;60(7):4420–4421. doi: 10.1128/AAC.01103-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Bernasconi O. J., Kuenzli E., Pires J., et al. Travelers can import colistin-resistant Enterobacteriaceae, including those possessing the plasmid-mediated mcr-1 gene. Antimicrobial Agents and Chemotherapy. 2016;60(8):5080–5084. doi: 10.1128/AAC.00731-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Fernandes M. R., McCulloch J. A., Vianello M. A., et al. First report of the globally disseminated IncX4 plasmid carrying the mcr-1 gene in a colistin-resistant Escherichia coli sequence type 101 isolate from a human infection in Brazil. Antimicrobial Agents and Chemotherapy. 2016;60(10):6415–6417. doi: 10.1128/AAC.01325-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Corbella M., Mariani B., Ferrari C., et al. Three cases of mcr-1-positive colistin-resistant Escherichia coli bloodstream infections in Italy, August 2016 to January 2017. Eurosurveillance. 2017;22(16):p. 30517. doi: 10.2807/1560-7917.es.2017.22.16.30517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Guenther S., Falgenhauer L., Semmler T., et al. Environmental emission of multiresistant Escherichia coli carrying the colistin resistance gene mcr-1 from German swine farms. Journal of Antimicrobial Chemotherapy. 2017;72:1289–1292. doi: 10.1093/jac/dkw585. [DOI] [PubMed] [Google Scholar]
- 197.Fritzenwanker M., Imirzalioglu C., Gentil K., Falgenhauer L., Wagenlehner F. M., Chakraborty T. Incidental detection of a urinary Escherichia coli isolate harbouring mcr-1 of a patient with no history of colistin treatment. Clinical Microbiology and Infection. 2016;22(11):954–955. doi: 10.1016/j.cmi.2016.08.027. [DOI] [PubMed] [Google Scholar]
- 198.Ellem J. A., Ginn A. N., Chen S. C. A., Ferguson J., Partridge S. R., Iredell J. R. Locally acquired mcr-1 in Escherichia coli, Australia, 2011 and 2013. Emerging Infectious Diseases. 2017;23(7):1160–1163. doi: 10.3201/eid2307.161638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Qian Y., Bulitta J. B., Peloquin C. A., Holden P. N. Crossm Polymyxin Combinations Combat Era. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Jørgensen S. B., Søraas A., Arnesen L. S., Leegaard T., Sundsfjord A., Jenum P. A. First environmental sample containing plasmid-mediated colistin-resistant ESBL-producing Escherichia coli detected in Norway. APMIS. 2017;125(9):10–12. doi: 10.1111/apm.12720. [DOI] [PubMed] [Google Scholar]
- 201.He T., Wei R., Zhang L., et al. Characterization of NDM-5-positive extensively resistant Escherichia coli isolates from dairy cows. Veterinary Microbiology. 2017;207:153–158. doi: 10.1016/j.vetmic.2017.06.010. [DOI] [PubMed] [Google Scholar]
- 202.Rutherford K., Parkhill J., Crook J., et al. Artemis: sequence visualization and annotation. 2000;16(10):944–945. doi: 10.1093/bioinformatics/16.10.944. [DOI] [PubMed] [Google Scholar]
- 203.Olaitan A. O., Chabou S., Okdah L., Morand S., Rolain J. M. Dissemination of the mcr-1 colistin resistance gene. Lancet Infectious Diseases. 2016;16(2):p. 147. doi: 10.1016/S1473-3099(15)00540-X. [DOI] [PubMed] [Google Scholar]
- 204.Zhang Y., Liao K., Gao H., et al. Decreased fitness and virulence in ST10 Escherichia coli harboring bla NDM-5 and mcr-1 against a ST4981 strain with bla NDM-5 . Frontiers in Cellular and Infection Microbiology. 2017;7:p. 242. doi: 10.3389/fcimb.2017.00242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Schürch A. C., van Schaik W. Challenges and opportunities for whole-genome sequencing-based surveillance of antibiotic resistance. Annals of the New York Academy of Sciences. 2017;1388(1):108–120. doi: 10.1111/nyas.13310. [DOI] [PubMed] [Google Scholar]
- 206.Gupta S. K., Padmanabhan B. R., Diene S. M., et al. ARG-ANNOT, a new bioinformatic tool to discover antibiotic resistance genes in bacterial genomes. Antimicrobial Agents and Chemotherapy. 2014;58(1):212–220. doi: 10.1128/AAC.01310-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Zankari E., Hasman H., Cosentino S., et al. Identification of acquired antimicrobial resistance genes. Journal of Antimicrobial Chemotherapy. 2012;67(11):2640–2644. doi: 10.1093/jac/dks261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.McArthur A. G., Waglechner N., Nizam F., et al. The comprehensive antibiotic resistance database. Antimicrobial Agents and Chemotherapy. 2013;57(7):3348–3357. doi: 10.1128/AAC.00419-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Liu B., Pop M. ARDB-antibiotic resistance genes database. Nucleic Acids Research. 2009;37:443–447. doi: 10.1093/nar/gkn656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Suzuki S., Ohnishi M., Kawanishi M., Akiba M., Kuroda M. Investigation of a plasmid genome database for colistin-resistance gene mcr-1 . Lancet Infectious Diseases. 2016;16(3):284–285. doi: 10.1016/S1473-3099(16)00008-6. [DOI] [PubMed] [Google Scholar]
- 211.Lindsey R. L., Batra D., Rowe L., et al. High-quality genome sequence of an Escherichia coli o157 strain carrying an mcr-1 resistance gene isolated from a patient in the United States. Genome Announcements. 2017;5(11):p. e01725-16. doi: 10.1128/genomeA.01725-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Zankari E., Allesøe R., Joensen K. G., Cavaco L. M., Lund O., Aarestrup F. M. PointFinder: a novel web tool for WGS-based detection of antimicrobial resistance associated with chromosomal point mutations in bacterial pathogens. Journal of Antimicrobial Chemotherapy. 2017;72(10):2764–2768. doi: 10.1093/jac/dkx217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Ellington M. J., Ekelund O., Aarestrup F. M., et al. The role of whole genome sequencing in antimicrobial susceptibility testing of bacteria: report from the EUCAST Subcommittee. Clinical Microbiology and Infection. 2017;23(1):2–22. doi: 10.1016/j.cmi.2016.11.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: home-made polymyxin-containing agar. Table S2: comparison of different polymyxin B susceptibility testing methods to detect polymyxin B resistance in Gram-negative clinical isolates. Table S3: other comparative AST methods.