Abstract
Background and Objectives:
Biologic and resorbable synthetic materials are used commonly for crural repair reinforcement during laparoscopic hiatal herniorrhaphy. Recently, an ovine polymer-reinforced bioscaffold (OPRBS) has been developed for reinforcement of abdominal wall and hiatal herniorrhaphies. This is the first reported series on use of OPRBS in hiatal hernia repairs.
Methods:
A retrospective chart review was conducted for consecutive series of patients (n = 25) undergoing laparoscopic or open hiatal herniorrhaphy between August 2016 and May 2017. Data collected included demographics, comorbidities and symptoms, details of operation, complications, and postoperative followup.
Results:
Laparoscopic repair was completed in 23 of 24 patients. Reinforcement with OPRBS was accomplished in all cases. Fundoplication was constructed in 24 of 25 patients (96%). Mean followup was 14.2 months. Good-to-excellent symptom control or resolution has been achieved for heartburn (95%), dysphagia (94.7%), regurgitation (100%), nausea and vomiting (100%), dyspnea (100%), and chest pain or discomfort (85.7%). Postoperative esophagogastroduodenoscopy with dilation resulted in resolution of persistent postoperative dysphagia in two patients (8%). To date there have been no clinical recurrences of hiatal hernia.
Conclusion:
OPRBS in hiatal hernia repair have been associated with excellent early patient outcomes in this study. OPRBS represent a new paradigm in hernia repair, as it is the first clinically available biological repair material reinforced with embroidered resorbable or permanent synthetic polymer. Relative weaknesses of the current study include the small sample size (n = 25), and short-term (mean = 14.2 months) followup. Long-term followup and additional studies will be required to confirm these findings.
Keywords: Hiatal hernia, Laparoscopy, Ovine polymer-reinforced bioscaffold (OPRBS)
INTRODUCTION
Hiatal hernia is defined as the temporal or permanent migration of a portion or all of the stomach, or other viscera, into the mediastinum via a defect in the diaphragmatic crura, which normally define the esophageal hiatus.1 This is a very common clinical problem, affecting up to 60% of the adult population.2 Following encouraging early reports, laparoscopic repair of symptomatic hiatal hernias became the standard of surgical care and is associated with reduced rates of perioperative morbidity and shorter hospital stays in comparison to open surgical procedures.3,4 Minimally invasive techniques afford patients several benefits including less pain, faster recovery time, and increased safety.4 The use of surgical mesh to reinforce the hernia repair has become an increasingly common practice in hiatal hernia surgery. Meta-analysis of 11 studies (randomized and nonrandomized) comparing mesh (n = 719) to suture-only (n = 755) repairs demonstrated that mesh augmented repairs were associated with a reduced overall recurrence rate compared to suture repair alone (2.6% vs 9.4%) over follow-up periods ranging from 6 to 58 months. The use of mesh did not lead to a significant difference in reported complications. A meta-analysis suggests quality of life improvements as measured by SF-36 or Health-Related Quality of Life (HRQOL) to be greater following biologic mesh-augmentationas compared to repairs with sutures only.5
The use of permanent synthetic meshes can lead to erosion of the mesh through the esophagus and other organs, a rare but serious complication.6–8 For this reason, either biologic or synthetic resorbable meshes are preferred for this indication. The handling characteristics and costs of these implants vary, as do the reported recurrence rates following their use.
MATERIALS AND METHODS
Recently, a novel implant intended for hiatal hernia repair was introduced. U.S. Food & Drug Administration (FDA) clearance for clinical use in soft-tissue reinforcement was received in early 2016. This is the first series to assess its utility in the repair of hiatal hernias. Ovine polymer-reinforced bioscaffold (OPRBS; OviTex) is a reinforced bioscaffold constructed from layers of ovine extracellular matrix, embroidered with a resorbable or permanent synthetic polymer. Available in 4, 6, and 8 layers, these extracellular matrix constructs are sewn together with monofilament polypropylene, or multifilament polygycolic acid. Nonhuman primate studies have shown that following implantation OPRBS rapidly repopulates with cells and new blood vessels, and subsequently remodels into a morphologically functional collagen layer. The implant does not cause a chronic inflammatory response.9,10 In this study, only bioscaffolds with resorbable polymer were used due to placement adjacent to the esophagus and stomach.
The aim of this retrospective study is to document the initial clinical experience of one surgeon at a single site with OPRBS in the augmentation of surgical repair of symptomatic hiatal hernias, with emphasis on intra-operative handling and early complications and outcomes.
Following Institutional Review Board approval, a retrospective chart review was conducted on a consecutive series of patients undergoing laparoscopic or open hiatal hernia repair utilizing OviTex, a novel OPRBS (n = 25), between August 2016 and May 2017. Preoperative assessment commenced with a complete clinical history documenting the type, severity, and duration of symptomatology referable to the hiatal hernia, along with physical examination. Patients who were considered appropriate candidates for surgery to correct the hiatal hernia underwent selective preoperative endoscopic, radiologic, and physiologic evaluation. Esophagogastroduodenoscopy with biopsies was completed in 24 patients (96%). Fluoroscopic upper gastrointestinal (GI) series was done in 14 patients (56%). A preoperative computerized tomography (CT) scan of the abdomen and pelvis was done in 5 patients (20%). Twenty-four-hour pH testing was utilized in 3 patients (12%). Esophageal manometry was completed in 13 patients (52%). An additional 4 patients either refused or could not complete manometric testing due to discomfort (16%). Laryngoscopy had been done in 2 patients who were referred by otolaryngologists (8%). Reflux laryngitis and pharyngitis was reported in both of the studies. Gastric emptying studies were completed in 2 patients with significant preoperative symptoms of nausea (8%). Both of these studies were normal.
A standardized technique was utilized for all laparoscopic hiatal hernia repairs. Following access to the abdominal cavity, the hernias were reduced. The hernia sacs were resected and the diaphragmatic crura were approximated with 2-0 polyester suture. The crural repair was reinforced using a rectangular piece of 4- or 6-layer OPRBS that was trimmed into a U-shaped implant. The pretrimmed dimensions of the implants that were used in this series were 4 × 8 cm core (4-layer), 4 × 8 cm 1S (6-layer), 10 × 12 cm 1S (6-layer) and 10 × 16 cm 1S (6-layer). The implants were fixed either with sutures, fibrin glue, or a combination of these. The procedure was completed with the creation of a fundoplication in 24 of the 25 cases. All fundoplications were constructed over a 52 Fr. or 56 Fr. esophageal bougie.
Patient demographics including body mass index (BMI) and comorbidities were collected. Operative data including hernia, OPRBS types and manner of fixation were recorded. Follow-up data were reviewed to identify symptom resolution, or improvement and postoperative complications.
RESULTS
Twenty-five patients underwent laparoscopic or open hiatal hernia repair utilizing OPRBS. There were 18 female (72%) and 7 male (28%) patients (Table 1). The mean age was 59.76 years (±14.79 years) with a median of 64 years and a range of 23–85 years. The mean BMI was 29.56 kg/m2 (±7.3 kg/m2) with a median of 28 kg/m2 and a range of 20–48 kg/m2. Comorbidities present with an incidence greater than 10% of the patient population include hypertension (n = 16; 64%), obesity (n = 11; 44%), hyperlipidemia (n = 8; 32%), diabetes (n = 5; 20%), obstructive sleep apnea (n = 5; 20%), chronic obstructive pulmonary disease (COPD)/asthma (n = 5; 20%), coronary artery disease (n = 4; 16%), and prior myocardial infarction (n = 3; 12%). The most common preoperative symptoms included heartburn (n = 21; 84%), dysphagia (n = 19; 76%), regurgitation (n = 10; 40%) and chest discomfort/pain (n = 7; 28%).
Table 1.
Demographic Data and Preoperative Symptoms
| Sex | Female (n = 18; 72%) | Male (n = 7; 28%) | ||
|---|---|---|---|---|
| Age | Mean 59.76 ± 14.79 | Median 64 | Range 23–85 | |
| BMI | Mean 29.56 ± 7.3 | Median 28 | Range 20–48 | |
| Comorbidities | DM (n = 5, 20%) Prior MI (n = 3, 12%) | HTN (n = 16, 64%) OSA (n = 5, 20%) | Hyperlipid. (n = 8, 32%) Obesity (n = 11, 44%) | CAD (n = 4, 16%) COPD/asthma (n = 5, 20%) |
| Preop. Symptoms/Findings | Heartburn (n = 21, 84%) Dyspnea (n = 4, 16%) Barrett esophagus (n = 2, 8%) | Dysphagia (n = 19, 76%) Chest discomfort/pain (n = 7, 28%) | Regurgitation (n = 10, 40%) Bloating (n = 1, 4%) | Nausea/vomiting (n = 3, 12%) Esoph. stricture (n = 2, 8%) |
BMI = Body mass index; CAD = Coronary artery disease; COPD = Chronic obstructive pulmonary disease; DM = Diabetes mellitus; HTN = Hypertension; Prior MI = Prior myocardial infarction; OSA = Obstructive sleep apnea.
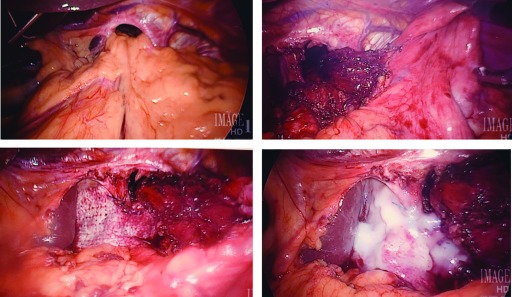
Each of the 4 hiatal hernia types were represented. Type I hernias were present in 11 patients, (44%). A Type II hiatal hernia was found in one (4%). Type III hiatal hernia was the pathology in 10 patients (40%). Three patients (12%) had a Type IV hiatal hernia (Table 2). Figure 1 and Figure 2 show OPRBS in the repair of Type III and Type I hiatal hernias. In most cases, the hiatal hernia was primary (n = 22; 88%). The operation was planned to be performed laparoscopically in 24 of 25 patients (96%). All patients except one underwent a fundoplication; Toupet (n = 16; 64%) and Nissen (n = 6; 24%) were the most common techniques used. The patient who did not undergo fundoplication had presented urgently with gastric organoaxial volvulus and esophageal obstruction. Multiple OPRBS types were used, with a 8 × 4 cm core (4 ply) being the most frequently used in 84% of procedures. The OPRBS fixation used was suture alone in 2 (8%), fibrin glue alone in 17 (68%) and suture plus fibrin glue in 6 (24%) procedures (Figures 1 and 2).
Table 2.
Operative Data
| Hernia Type | I (n = 11; 44%) | II (n = 1; 4%) | III (n = 10; 40%) | IV (n = 3; 12%) |
|---|---|---|---|---|
| Primary vs recurrent | primary (n = 22, 88%) | recurrent (n = 3, 12%) | ||
| Completed laparoscopically* | 23/24 (95.8%) | |||
| Intraoperative complications | 0 (0%) | |||
| OPBRS type | 8 × 4 cm core (4 ply) (n = 21; 84%) | 8 × 4 cm 1S (6 ply) (n = 2; 8%) | ||
| 10 × 12 cm 1S (6 ply) (n = 1; 4%) | 10 × 16 cm 1S (6 ply) (n = 1; 4%) | |||
| Fixation method for OPBRS | S (n = 2; 8%) | F (n = 17; 68%) | SF (n = 6; 24%) | |
| Fundoplication | Nissen (n = 6; 24%) | Toupet (n = 16; 64%) | D'Or (n = 2; 8%) | None (n = 1; 4%) |
*Twenty-three cases were completed laparoscopically. One case was straight open due to strangulation and perforation of a Type IV hiatal hernia with spillage of gastric contents into the right hemithorax. One case was converted to open due to extensive adhesions and a finding of synthetic mesh from a previous incisional herniorrhaphy eroding into the transverse colon requiring transverse colectomy.
#The reinforcing polymer for all core and 1S OPRBS used for crural repair is polyglycolic acid.
S = Suture alone; F = Fibrin glue alone; SF = Suture plus fibrin glue.
Figure 1.
OPRBS in repair of Type III hiatal hernia.
Figure 2.
OPRBS in repair of Type I hiatal hernia.
In one patient, a 74-year-old female, an open approach was necessary due to strangulation and perforation of a Type IV hiatal hernia with spillage of gastric contents into the right hemithorax. This had been recognized on a preoperative CT scan of the chest, abdomen, and pelvis performed in the emergency department. In another patient, a laparoscopic procedure was converted to an open procedure due to a finding of polypropylene-based synthetic mesh eroding into the transverse colon. This had been placed at a previous incisional herniorrhaphy in an upper vertical midline abdominal incision. In this patient, a concurrent transverse colectomy and resection of the indwelling polypropylene-based synthetic mesh were performed, in addition to the hiatal hernia repair. This was the only patient requiring conversion from laparoscopic to open surgery (4.2%). One patient died on postoperative day 16 due to severe pneumonia and hypoxemia leading to cardiac arrest. This was an 85-year-old woman with severe debility who presented with a giant paraesophageal hernia, organoaxial gastric volvulus, obstruction, and malnutrition. These complications stemmed from the pre-existing pathology and were not related to the hernia repair itself, or the implant.
Follow-up data have been recorded with mean time of 14.2 months (±4.7 months), with a median of 15 months and a range of 1 to 20 months. (Table 3). No clinical recurrence has been observed. In two patients with persistent dysphagia beyond 3 months of postoperative followup, an esophagogastroduodenoscopy (EGD) with dilation was associated with resolution of symptoms. Both of these patients had Type III paraesophageal hiatal hernias, with dysphagia as a prominent feature of their preoperative symptom complex. One of these patients had repair of a recurrent hernia. In both of these patients, the OPRBS was fixed in place with fibrin glue alone.
Table 3.
Follow-up Data
| Months of Follow up | Mean 14.2 ± 4.7 median | Median 15 | Range 1–20 |
|---|---|---|---|
| Clinical recurrence | 0 (0%) | ||
| Symptom control/resolution | Heartburn (n = 20/21, 95%) | Dysphagia (n = 18/19, 94.7%) | Regurgitation (n = 10/10, 100%) |
| Nausea/vomiting (n = 3/3, 100%) | Dyspnea (n = 4/4, 100%) | Chest discomfort/pain (n = 6/7, 85.7%) | |
| Bloating (n = 0/1, 0%) | |||
| Mortality | 1 (4%) | ||
| Additional Interventions | EGD with dilation (n = 2, 8%) | Dysphagia resolved in both cases |
Most preoperative symptoms resolved or were significantly improved, specifically heartburn in 20 of 21 (95%) patients, dysphagia in 18 of 19 (94.7%) patients, and regurgitation in all 10 (100%) patients.
DISCUSSION
The aging population and an increase in obesity are expected to lead to an increased incidence of hiatal hernia, and hence also of surgical repairs. Recurrence rates following repair remain high; 3 randomized clinical trials reporting the outcomes of 267 patients showed recurrence rate of 24.3% after primary hiatoplasty.11 These data demonstrates that there is a need for further clinical improvements. The reinforcement of the traditional suture repair with mesh implants has been shown to decrease the recurrence rate as high as 4-fold.11,12 Regarding the type of implant, biologic and resorbable mesh scaffolds are preferred to avoid the risk of erosion which has been reported for permanent synthetic meshes.8
Currently, a number of mesh products for use in hiatal hernia repair are available. Dermis based biologics are used, but these can be difficult to shape, handle, and fixate. The same is true for some of the resorbable synthetic meshes. This is the first reported case series describing the use of a new product, OPRBS, in hiatal hernia repair. OPRBS combines biologic and resorbable synthetic components in a novel manner which affords good intracorporeal handling characteristics. OPRBS is reconstituted in saline for 5 minutes prior to deployment. It becomes pliable, and conforms very well to the crural repair. Suture passes through the material readily. Suturing tended to bunch the material up slightly, resulting in less than optimal conformation to the repair. Because of this, a decision was made to alter fixation technique.
After the first 2 cases, a combination of suturing and augmented fixation with application of fibrin glue was chosen. Due to the excellent adherence afforded by the fibrin glue and previous evidence showing reliability in this as sole fixation method, suturing was abandoned and fibrin glue was used as the sole fixation method in the last 17 cases. Use of fibrin glue alone for prosthetic fixation at the hiatus has previously been reported. In a series of 70 patients, Powell and colleagues applied fibrin glue as the sole fixation modality for reinforcement of their crural repairs with a bioabsorbable prosthesis.13 The authors touted the short time required to place the mesh with this method of approximately 5 minutes. They also reported no short-term complications nor negative sequelae referable to the prosthesis or the fixation method.13 In a porcine hiatal hernia model, Krpata and associates described using fibrin sealant for biologic mesh fixation at the hiatus.14 This was a 30-day survival study. Twenty animals were randomized to suture (n = 10) or fibrin sealant (n = 10) fixation. At completion of the study, diaphragms were harvested. Results included a statistically significantly shorter operative time for the fibrin sealant group. Mean peel force did not differ between the groups, and there were no instances of mesh migration.14
A total of 4 cc of fibrin glue was typically used. A small amount, usually less than 1 cc, is sprayed between the posterior aspect of the OPRBS and the surface of the diaphragmatic crura. The OPRBS is held in place for several seconds as the fibrin glue cures. The remainder is applied to the anterior surface of the OPRBS, especially at the perimeter of the construct and its interface to the more lateral aspects of the crura. To date, there is no evidence that application of the fibrin glue by itself is directly associated with dysphagia, nor any deleterious anatomic or physiologic effects at the esophagogastric junction. However, the fact that the 2 patients who developed dysphagia requiring esophageal dilation underwent OPRBS fixation with fibrin glue alone requires further monitoring.
In this series, OPRBS has been used in repair of Types I, II, III, and IV hiatal hernias, and for the reinforcement of both primary and recurrent hiatal repairs. Both 4- and 6-layer constructs were used. This was not based on any specific clinical evidence, and was based on material availability. In most the repairs, an 4 × 8 cm OPRBS was used. The 10 × 12 and 6 × 10 cm 6-layer constructs were used for augmentation of the repairs of larger defects associated with Type IV paraesophageal hiatal hernias. In both of these patients, the transverse diameter of the hiatal defect was greater than 8 cm, and cruroplasty was used to facilitate repair. Larger pieces of OPRBS were chosen to augment the site of the cruroplasty as well. Technical application in these 25 patients suggests that in the short term, OPRBS is associated with ease of intracorporeal handling and fixation, as well as excellent conformation to the anatomical contours of the final repair.15
Most patients (64%) in this study underwent construction of a partial posterior (Toupet) fundoplication. This decision was made most commonly on the basis of esophageal hypomotility found at manometry testing, or the lack of manometric data due to patient's refusal of the study. In other cases, the presence of a large paraesophageal hiatal hernia and significant associated preoperative dysphagia prompted this decision.
The choice of a Nissen fundoplication versus Toupet fundoplication remains a controversial topic. However, several series have demonstrated good results with a posterior partial fundoplication. Almond and Wadley published the results of a 5-year prospective review of Toupet fundoplication in the management of gastroesophageal reflux disease.16 In their series of 101 patients, 4.9% of patients have prolonged dysphagia beyond 3 months of followup. Mild prolonged gas bloat was found in 7.9%. Only one patient had recurrence of reflux (1%) and underwent redo laparoscopic surgery.16 A meta-analysis of 9 randomized controlled trials, 8 prospective cohort trials and 15 retrospective trials compared Nissen and Toupet fundoplications.17 No differences were found in patient satisfaction, perioperative complications, postoperative heartburn, reflux recurrence, nor reoperation rates. In contrast, postoperative dysphagia, gas-bloat syndrome, the inability to belch, and the need for postoperative esophageal dilation were more common after Nissen fundoplication.17
In this study, good to excellent relief of symptoms was achieved in all but one patient, who reported persistent abdominal bloating which was also present preoperatively. The rate of symptomatic control achieved in this series is consistent with a recent meta-analysis of laparoscopic hiatal hernia repair using mesh reinforcement.5 There were no intraoperative complications and specifically no complications attributable to the use of OPRBS. At up to 20 months of followup, there have been no clinical hernia recurrences. There were no routine radiographic or endoscopic follow-up examinations in this study to date. All postoperative assessments have been based mainly on clinical office follow-up visits. These patients will be followed long term to assure durability of these repairs. Recurrence of symptoms will prompt appropriate endoscopic and radiologic evaluations, as was done in the patients with long-term postoperative dysphagia. Our initial experience demonstrates that OPRBS is easy to shape, handle, and fixate. Although the material sutures easily, we now use primarily fibrin glue for fixation of the implant as described above. Early clinical results are encouraging. However, it must be emphasized that the study population is small (n = 25), and followup has been relatively short (mean, 14.2 months). These factors preclude any statements about long-term durability and generalized usage at this time. Additional studies of OviTex in hiatal hernia repair with larger sample sizes and lengthier followup are needed to confirm these results.
References:
- 1. Apaydin N, Uz A, Evirgen O, Loukas M, Tubbs RS, Elhan A. The phrenico-esophageal ligament: An anatomical study. Surg Radiol Anat. 2008;30(1):29–36. [DOI] [PubMed] [Google Scholar]
- 2. Dean C, Etienne D, Carpentier B, Gielecki J, Tubbs RS, Loukas M. Hiatal hernias. Surg Radiol Anat. 2012;34(4):291–299. [DOI] [PubMed] [Google Scholar]
- 3. Müller-Stich BP, Kenngott HG, Gondan M, et al. Use of mesh in laparoscopic paraesophageal hernia repair: A meta-analysis and risk-benefit analysis. PLoS ONE 2015;10(10):e0139547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kohn GP, Price RR, DeMeester SR, et al. Guidelines for the management of hiatal hernia. Surg Endosc. 2013;27(12):4409–4428. [DOI] [PubMed] [Google Scholar]
- 5. Zhang C, Liu D, Li F, et al. Systematic review and meta-analysis of laparoscopic mesh versus suture repair of hiatus hernia: Objective and subjective outcomes. Surg Endosc. 2017;31(12):4913–4922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schneider R, Herrington JL, Jr, Granda AM. Marlex mesh in repair of a diaphragmatic defect later eroding into the distal esophagus and stomach. Am Surg. 1979;45(5):337–339. [PubMed] [Google Scholar]
- 7. Hazebroek EJ, Leibman S, Smith GS. Erosion of a composite PTFE/ePTFE mesh after hiatal hernia repair. Surg Laparosc Endosc Percutan Tech. 2009;19(2):175–177. [DOI] [PubMed] [Google Scholar]
- 8. Stadlhuber RJ, Sherif AE, Mittal SK, et al. Mesh complications after prosthetic reinforcement of hiatal closure: A 28-case series. Surg Endosc. 2009;23(6):1219–1226. [DOI] [PubMed] [Google Scholar]
- 9. Ferzoco S. Novel reinforced bioscaffolds in a non-human primate abdominal wall repair model. Poster Presentation, 8th Annual Abdominal Wall Reconstruction Conference; 2016 Jun 9–11; Washington, DC 2016. [Google Scholar]
- 10. Ferzoco S. Long-Term Results with Various Hernia Repair Materials in Non-Human Primates. Poster Presentation, 8th Annual Abdominal Wall Reconstruction Conference; 2016 Jun 9–11; Washington, DC. [Google Scholar]
- 11. Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA. Lower recurrence rates after mesh-reinforced versus simple hiatal hernia repair: A meta-analysis of randomized trials. Surg Laparosc Endosc Percutan Tech. 2012;22(6):498–502. [DOI] [PubMed] [Google Scholar]
- 12. Johnson JM, Carbonell AM, Carmody BJ, et al. Laparoscopic mesh hiatoplasty for paraesophageal hernias and fundoplications: A critical analysis of the available literature. Surg Endosc. 2006;20(3):362–366. [DOI] [PubMed] [Google Scholar]
- 13. Powell BS, Wandrey D, Voeller GR. A technique for placement of a bioabsorbable prosthesis with fibrin glue fixation for reinforcement of the crural closure during hiatal hernia repair. Hernia. 2013;17(1):81–84. [DOI] [PubMed] [Google Scholar]
- 14. Krpata DM, Blatnik JA, Harth KC, Phillips MS, Novitsky YW, Rosen MJ. Evaluation of fibrin sealant for biologic mesh fixation at the hiatus in a porcine model. Surg Endosc. 2012;26(11)3120–3126. [DOI] [PubMed] [Google Scholar]
- 15. Persenaire M. Surgeon feedback on initial clinical experience with OviTexTM reinforced bioscaffolds in a wide range of hernia patients. Poster presentation Abdominal Wall Reconstruction Conference; 2017 Jun 8–10; Washington, DC. [Google Scholar]
- 16. Almond LM, Wadley MS. A 5-year prospective review of posterior partial fundoplication in the management of gastroesophageal reflux disease. Int J Surg. 2010;8(3):239–242. [DOI] [PubMed] [Google Scholar]
- 17. Shan CX, Zhang W, Zheng XM, Jiang DZ, Liu S, Qiu M. Evidence-based appraisal in laparoscopic Nissen and Toupet fundoplications for gastroesophageal reflux disease. World J Gastroenterol. 2010;16(24):3063–3071. [DOI] [PMC free article] [PubMed] [Google Scholar]