Abstract
SIGNIFICANCE
This first report of the use of objective measures of disparity vergence as outcome measures for symptomatic convergence insufficiency in children provides additional information that is not accessible with clinical tests. The study results also demonstrate that objective measures of vergence could be used in future randomized clinical trials of binocular vision disorders with children.
PURPOSE
This study was designed to evaluate changes in objective measures of disparity vergence after office-based vergence/accommodative therapy (OBVAT) for convergence insufficiency in children 12 to 17 years old.
METHODS
In this prospective trial, we recruited 10 participants with normal binocular vision and 12 with convergence insufficiency. All participants with convergence insufficiency were treated with 12 weeks of OBVAT. The primary outcome measure was average peak velocity for 4° symmetrical convergence steps. Other objective outcome measures of disparity vergence included time to peak velocity, latency, and accuracy. Changes in clinical measures (near point of convergence, positive fusional vergence at near) and symptoms were evaluated.
RESULTS
There was a statistically significant increase in peak velocity and more accurate response amplitude to 4° symmetrical convergence step stimuli after OBVAT compared with baseline measurements. Near point of convergence, positive fusional vergence, and symptoms also statistically significantly improved after OBVAT. Ten of the 12 participants met clinical success criteria.
CONCLUSIONS
In this prospective study on the treatment of symptomatic convergence insufficiency in children in which both clinical and objective eye movement measurements were used to evaluate the results of treatment, significant changes were found in symptoms and both clinical and objective measures of disparity vergence after completion of OBVAT in children with symptomatic convergence insufficiency.
Convergence insufficiency is a common binocular vision disorder with an estimated prevalence between 4.2% and 17.6%,1–4 when defined as a condition in which there is a greater amount of exodeviation at near than at far, the near point of convergence is receded, and positive fusional vergence is below the expected level. Convergence insufficiency often results in visual symptoms including headaches, eyestrain, blurred vision, loss of place while reading, and diplopia during near visual activities.5,6 In two randomized clinical trials completed by the Convergence Insufficiency Treatment Trial Investigator Group, office-based vergence/accommodative vision therapy combined with home reinforcement was found to be the most effective treatment for symptomatic convergence insufficiency in children 9 to 17 years of age.7–9 The Convergence Insufficiency Treatment Trial Investigator Group studies used traditional clinical measures of vergence and accommodation, along with a validated symptom questionnaire score, as outcome measures. However, both the symptom questionnaire and clinical measures were subjective measurements that depend on the patient's ability to accurately report what he/she was experiencing and seeing. The use of objective measures of oculomotor function may provide additional valuable information about physiological changes in vergence function that cannot be determined clinically. In addition, objective measures may be useful in clinical trials because they are not prone to bias by either participants or examiners. There is a paucity of studies using objective eye movement recordings of vergence as outcome measures after treatment of vergence disorders,10–18 a smaller number that limited the study to only convergence insufficiency,11,12 and an even smaller number that studied only convergence insufficiency in the pediatric population.12
Thus, although there are some data available about the use of objective measures of vergence used as outcome measures, most of the studies have used adult subjects and have not limited the vergence disorder to convergence insufficiency. There is a need for additional research to evaluate the use of objective measures of vergence eye movements as outcome measures for the treatment of symptomatic convergence insufficiency in children. The primary objective of this study is to determine how office-based vergence/accommodative vision therapy affects various objective vergence parameters (i.e., peak velocity, latency, time to peak velocity, response amplitude, settling time). These five parameters were selected based on previous research suggesting that they may be abnormal in patients with impaired binocular vision.11–15,18 Secondary objectives are to gather preliminary information about the feasibility of using these measures as outcome measures in a future large-scale randomized clinical trial studying concussion-related convergence insufficiency in children and to produce pilot data about effect size and variability that can be used in future studies for sample size estimation.
METHODS
The tenets of the Declaration of Helsinki were followed throughout the study. The institutional review board of Salus University approved the protocol, and written informed consent and assent as well as Health Insurance Portability and Accountability Act authorization were obtained before participation. The trial is registered with clinicaltrials.gov (identifier, NCT03248336; date of registration, August 7, 2017).
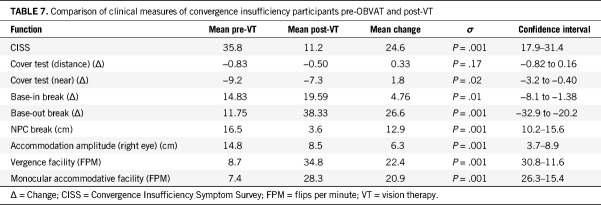
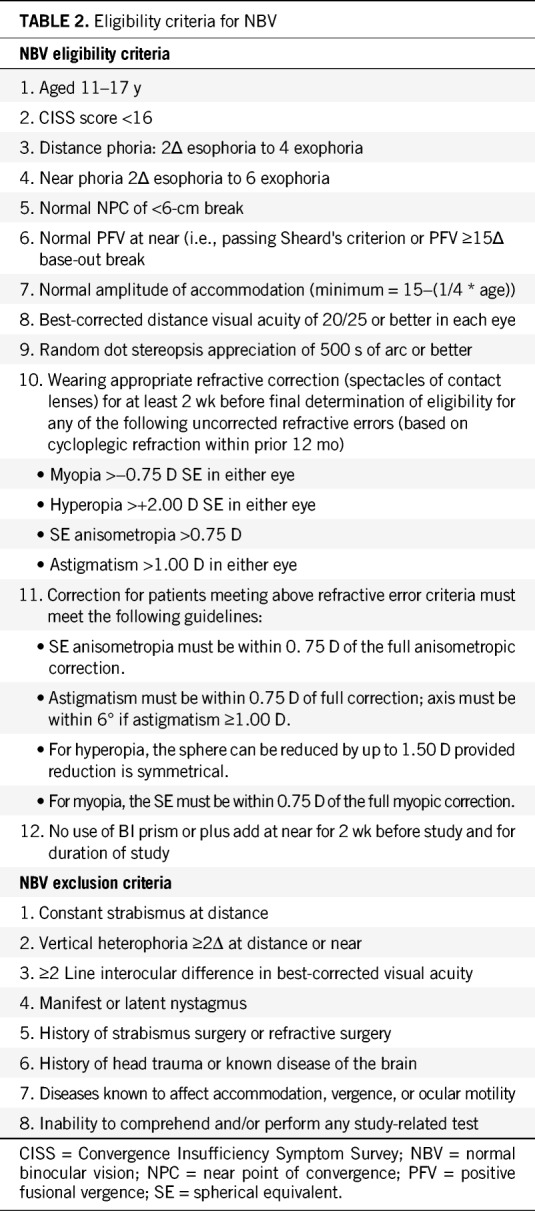
Patient Selection and Definitions of Convergence Insufficiency and Normal Binocular Vision
Patients were recruited from the Eye Institute of the Pennsylvania College of Optometry at Salus University and from the clinical practice of one of the authors (MS). All of the patients had a comprehensive eye examination before the baseline visit. To be eligible for the convergence insufficiency group, individuals had to be between 12 and 17 years old and have a diagnosis of symptomatic convergence insufficiency. Symptomatic convergence insufficiency was defined as (1) a score of 16 or higher on the Convergence Insufficiency Symptom Survey, (2) exophoria at near at least 4 prism diopters (Δ) greater than at distance, (3) a receded near point of convergence of 6 cm or greater break, and (4) insufficient positive fusional vergence (i.e., failing Sheard's criterion or positive fusional vergence ≤15Δ base out) at near. Participants were required to have 20/25 visual acuity or better with best refractive correction if needed. Participants with a previous history of vision therapy were excluded. The participants also were required to have stable general health, intact cognitive function, and no other neurological conditions. To be eligible for the normal binocular vision group, patients had to be between 12 and 17 years old and have Convergence Insufficiency Symptom Survey score of less than 16, 20/25 visual acuity or better with best correction, and normal binocular vision and accommodation. Eligibility criteria for both groups are listed in Tables 1 and 2.
TABLE 1.
Eligibility and exclusion criteria for symptomatic CI
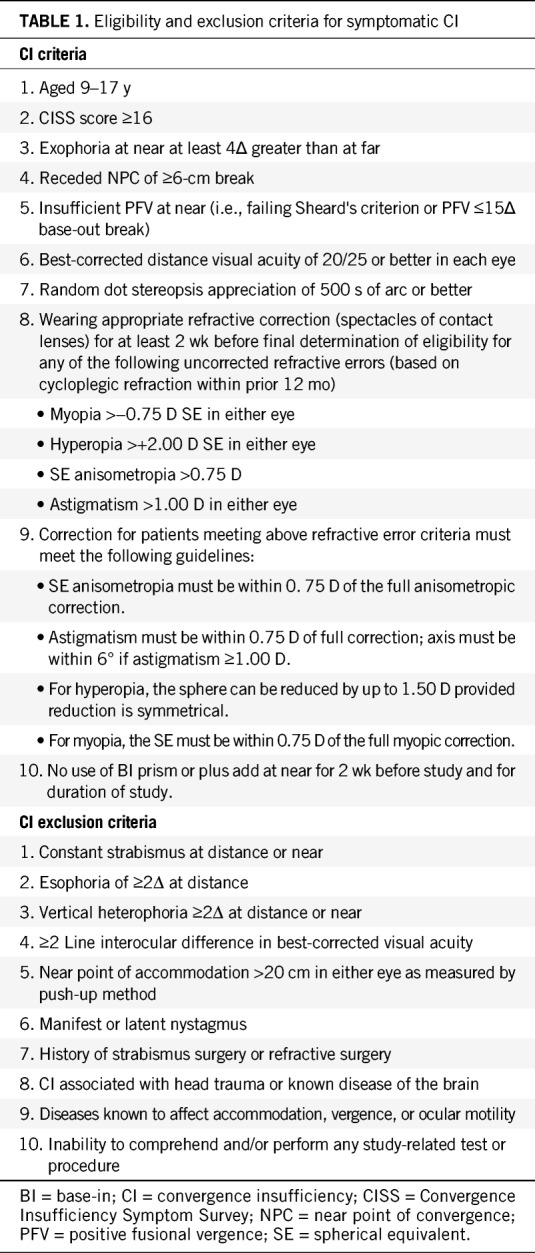
TABLE 2.
Eligibility criteria for NBV
Study Design
Clinical testing and objective eye movement recording were performed with both groups at baseline. After baseline measurements, participants in the convergence insufficiency group received twelve 1-hour visits of office-based vergence/accommodative therapy. At the completion of therapy, the baseline clinical testing was repeated for the participants in the convergence insufficiency group. For participants in the normal binocular vision group, the study ended after the baseline measurements.
Eligibility Examination/Baseline Clinical Convergence Insufficiency Testing for Enrollment
After obtaining written consent/assent, a vision examination was performed to determine if the patient was eligible for the study. Eligibility testing included administration of the Convergence Insufficiency Symptom Survey to identify whether or not the patient was symptomatic.19,20 Other eligibility tests included best-corrected visual acuity at distance and near, a sensorimotor examination (cover test at distance and near, near point of convergence [20/30 target and the Gulden near point rod], positive and negative fusional vergence at near [prism bar and a held 20/30 vertical line of letters as a target], vergence facility [12 base-out, 3 base-in prism] at distance and near, near stereoacuity [Randot stereotest], monocular accommodative amplitude [20/30 target and the Gulden near point rod], monocular accommodative facility [±2.00 flipper lenses and 20/30 vertical line of letters]) cycloplegic refraction, and an ocular health evaluation. This test battery was identical to that used in previous randomized clinical trials of symptomatic convergence insufficiency.7,8,21,22
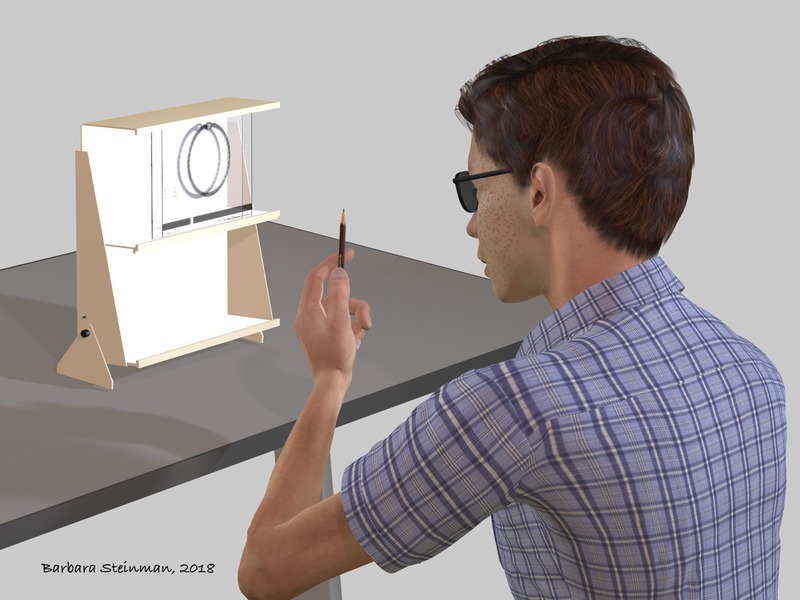
Objective Outcome Measures of Disparity Vergence: Instrumentation
The ISCAN RK-826PCI binocular tracking system (Burlington, MA) was used to objectively record horizontal vergence eye movements within a traditional haploscope (Fig. 1). This system uses an infrared emitter (940 nm) and two cameras to capture the eye movement data at 240 frames per second. The manufacturer reports an instrument resolution of 0.1°. We used the methods described by van Rijn et al.23 to study the variability of the steady state of the 4° symmetrical vergence eye movement responses. For the 10 binocularly normal controls, the standard deviation in the steady state was 0.24 ± 0.02°, and for the 12 convergence insufficiency subjects studied, the standard deviation was 0.28 ± 0.03°. The increase in the standard deviation for the convergence insufficiency participants may be owing to the greater fixation disparity reported to be observed in convergence insufficiency patients.24 Given our study was on latency, peak velocity, and response amplitude, our system has adequate resolution for this proposed research.
FIGURE 1.
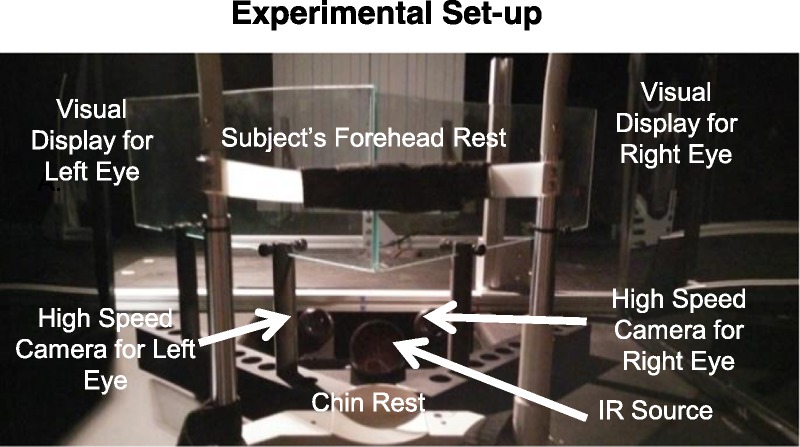
Experimental setup of haploscope used to record disparity vergence eye movements.
Stimuli Presentation, Data Collection, Calibration
It is well established that there is an interaction between the disparity and accommodative vergence systems.25–29 A vertically oriented difference of Gaussians was used to reduce accommodative vergence as the disparity vergence step stimuli were introduced using a haploscope. This visual target was designed to minimize blur cues and feedback to produce virtually accommodation open-loop conditions during the presentation of disparity vergence stimuli. Hence, the vergence response was primarily owing to the disparity vergence stimulus cue and had minimal accommodative vergence30 and is the same stimulus from the research of Schor and Kotulak.31 The following equation described by Schor and Kotulak31 was generated using MATLAB (Mathworks, Waltham, MA) to create the visual stimulus:
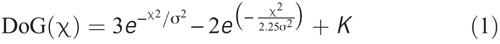
where DoG is difference of Gaussians, σ2 is the space constant, and K is the mean luminance. The target was 1 cm in width when measuring the nonblack background. The peak spatial frequency was 6.4 cycles per degree with a luminance of 10 cd/m2 and contrast of 100%, which was the same as that used by Schor and Kotulak,31 who objectively demonstrated that using this visual stimulus results in negligible stimulation to the accommodation system. The laboratory of one of the coauthors (TLA) contained a PlusOptix power refractor 3; the accommodative response from this difference of Gaussians stimulus was less than 0.2 D, suggesting the accommodative cue was minimal. This accommodation instrument was not available at the site where the data from this current study were collected. This study does not have quantitative data from the accommodation system, which was beyond the scope of this current study.
All experiments were conducted in the dark to reduce influence from proximal vergence. Hence, the major variable that changed within this study was disparity vergence.
Experimental Design Parameters
The use of 4° (~7Δ) and 6° (~11Δ) symmetrical disparity steps was chosen to maximize the ability to gather quality data for each observation. These disparities in binocularly normal controls are known to elicit fewer saccades compared with larger disparity movements such as those stimulated from 8° and 12° symmetrical vergence disparity steps. A number of previous studies used these parameters and found these values minimize the likelihood of loss of data because of inability to fuse the targets.11,32–37 Convergence and divergence step stimuli were presented at binocular vergence angles from 6 (~11Δ) to 12° (~21Δ) (referred to as near stimuli) and binocular vergence angles from 2 (~3.5Δ) to 8° (~14Δ) (referred to as far stimuli). Twelve observations of each of the visual stimuli were presented: 4° symmetrical disparity vergence steps from a vergence angle of 2 to 6°, 4 to 8°, 6 to 10°, and 8 to 12°, as well as 6° symmetrical disparity vergence steps from 6 to 12° and from 4 to 10°. This resulted in a total of 72 convergent movements. This protocol was used to reduce prediction, which is known to influence vergence eye movements.38 By using an experimental design that had a randomized visual stimulus latency (presented stimulus after a delay of 1 to 2 seconds) and a randomized magnitude (4° or 6°), subjects would have difficulty anticipating or predicting when a visual stimulus would be presented next or its size. The experiment was sequenced to begin with far disparity vergence stimuli, which was hypothesized to be easier for convergence insufficiency participants owing to their receded near point of convergence. An average interpupillary distance of 6 cm was assumed because we studied children 12 to 17 years of age. We report only the results for the 4° convergence data because the majority of the convergence insufficiency group participants had difficulty responding to the 6° convergence stimuli at baseline. Many of these responses to 6° stimuli had saccades within the transient period, or subjects could not fuse the visual stimulus, making it difficult to conduct a meaningful analysis. The divergence data will be presented in a separate article.
Calibration
The participant's head was restrained using a chin/head rest to minimize head movement and influence from the vestibular system. A midline adjustment procedure was performed to insure proper positioning within the chin/head rest. Two separate calibrations were performed for each experiment (vergence with a far initial vergence angles and vergence with a near vergence angle). Calibration for far vergence step responses consisted of a six-point monocular calibration (1°, 3°, and 5° monocular, corresponding to 2°, 6°, and 10° binocular vergence angle demand). Calibration for near vergence step responses consisted of a six-point monocular calibration (4°, 5°, and 6° monocular, corresponding to 8°, 10°, and 12° binocular vergence angle demand). These calibrations were performed before and after completion of each experimental group.
After the initial calibration was complete, the experiment began, and 12 disparity vergence step stimuli were presented (combination of convergence and divergence), followed by an opportunity to rest. This was repeated six times for a total of 72 pseudorandom convergent/divergent observations for the far disparity vergence experiment and 72 pseudorandom convergent/divergent observations for the near disparity vergence. Near dissociated phoria measurements were recorded, but the phoria was not neutralized within our experiment.
Eye Movement Analyses
All parameters described in this article refer to vergence eye movements. Eye movement data were processed and analyzed with a custom MATLAB program. All of the 4° step vergence data were merged for analysis, as were the 6° data. The eye movements were filtered with a fourth-order low-pass Butterworth filter, with a cutoff frequency of 40 Hz to eliminate instrumentation noise especially 60 Hz noise that is probably not physiological in nature. Based on previous research11,13 of changes in objective measures after vision therapy, we selected peak velocity as the primary outcome measure in this study. Velocity was computed by taking the derivative of the position response using a two-point central difference algorithm.39 Each individual left-eye and right-eye convergent movement response was manually inspected for the presence of any blink(s) or saccade(s) during any portion of the transient portion of the vergence eye movement. Saccades were easily identified because saccadic dynamics are an order of magnitude greater than vergence. Saccades that occurred during the transient portion of the vergence response were omitted from the peak velocity analysis because several studies suggest that saccades facilitate the maximum velocity of vergence.34,35,40
Other objective eye movement parameters assessed included time to peak velocity, latency, response amplitude, and settling time. These parameters are illustrated in Fig. 2. Peak velocity was defined as the maximum value within the transient portion of the vergence movement. Time to peak velocity was defined as the time when the movement reaches its peak velocity within the transient portion of the response (green line in Fig. 2) measured from target onset. Latency was defined as the time at which the average positional data deviated 5% from the stimulus amplitude and was measured from target onset. Hence, for our study, this threshold was at 0.2° away from the initial response position. An example of the response latency was illustrated by the purple arrow and lines in Fig. 2. The settling time was defined as the time when the response was within the 5% error band (black dashed lines in Fig. 2) of the stimulus target amplitude (red line in Fig. 2).
FIGURE 2.
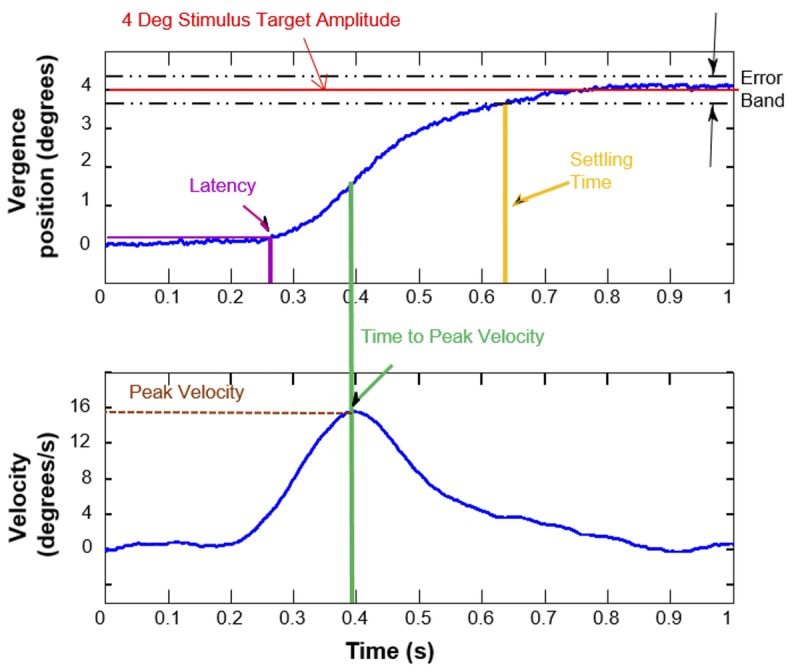
Data analysis of objective eye movements. The plot shows the temporal properties where the position is plotted as a function of time (upper plot) and the velocity is plotted as a function of time (lower plot).
Treatment
Office-based Vision Therapy with Home Reinforcement
Twelve, 60-minute, weekly visits of office-based vergence/accommodative therapy were administered by a trained therapist combined with procedures to practice at home (15 minutes, five times per week). This treatment sequence is a well-accepted approach for treatment of convergence insufficiency11 and has been successfully implemented in previous studies.7,8 Fifteen minutes of home-based therapy was prescribed to be performed 5 days per week, and compliance with home-based therapy was monitored at each visit by the therapist.
Follow-up Visit
All participants were reexamined after completion of 12 weeks of office-based vergence/accommodative therapy. Both the clinical testing and objective testing performed at enrollment were repeated at the outcome examination, which occurred between 12 and 14 weeks from baseline.
Determination of Treatment Outcome
To evaluate improvement in clinical measures and symptoms, we used the following criteria from the Convergence Insufficiency Treatment Trial Investigator Group studies.8,41 A successful outcome was a score of less than 16 on the Convergence Insufficiency Symptom Survey, a normal near point of convergence (i.e., less than 6 cm), and normal positive fusional vergence (i.e., greater than 15Δ and passing Sheard's criterion). Improved was defined as a score of less than 16 or a 10-point decrease in the Convergence Insufficiency Symptom Survey score, and at least one of the following: normal near point of convergence, an improvement in near point of convergence of more than 4 cm, normal positive fusional vergence, or an increase in positive fusional vergence of more than 10Δ. Patients who did not meet the criteria for successful or improved were considered nonresponders.
Statistical Analysis
All analyses were performed using SPSS version 24.0 (IBM Corp., Armonk, NY) with an α level of 0.05 used to determine statistical significance. Although we made multiple comparisons, we did not adjust the α level because our primary null hypothesis (i.e., there will be no change in the mean values for objective measures of disparity vergence after office-based vergence/accommodative therapy) involved only five comparisons (latency, peak velocity, time to peak velocity, response amplitude, and settling time). The remainder of the statistical testing was performed for hypothesis-generating purposes, and we therefore did not adjust α for these tests.
In regard to sample size calculations, there were no previous data in the literature with a pediatric population with the equipment used in this study. This was a pilot study with an objective of generating the data necessary to calculate sample size in future clinical studies using objective outcome measures.
Because a number of variables were not normally distributed, we used nonparametric statistical tests. Statistical significance of the changes in both clinical (near point of convergence, positive fusional vergence, and vergence facility) and objective findings (peak velocity, time to peak velocity, response amplitude, response latency, and settling time) after office-based vergence/accommodative therapy for the convergence insufficiency participants was tested using a Wilcoxon signed rank test. A Mann-Whitney U test was used to compare both the objective and clinical measures between the participants with normal binocular vision and those with convergence insufficiency at baseline and again after office-based vergence/accommodative therapy. Effect sizes were determined using the formula:  .
.
A Pearson product-moment correlation coefficient was calculated to evaluate the potential association between the change in the objective measures (peak velocity, time to peak velocity, response amplitude/accuracy, latency, settling time) and clinical measures (Convergence Insufficiency Symptom Survey, near point of convergence, positive fusional vergence at near, vergence facility, near point of accommodation, and accommodative facility) at baseline. The absolute values of each measurement were used for this analysis. Another analysis using the Pearson product-moment correlation coefficient was conducted using the outcome data after 12 weeks of office-based vergence/accommodative therapy.
RESULTS
We only report the results for the 4° convergence data because the majority of the convergence insufficiency group participants had difficulty responding to the 6° convergence stimuli at baseline. Many of these responses to 6° stimuli had saccades within the transient period or subjects could not fuse the visual stimulus, making it difficult to conduct a meaningful analysis.
Participant Characteristics
Twenty-two participants were recruited from the patient population at the Eye Institute (Salus University) between June 2014 and February 2016, 10 with normal binocular vision and 12 with symptomatic convergence insufficiency. Eight (67%) of these 12 convergence insufficiency participants were female with a mean age of 13.1 years (range, 12 to 17 years). Six (60%) of the 10 participants in the normal binocular vision group were female with a mean age of 14.2 years (range, 12 to 17 years).
Objective Disparity Vergence Measures—Overview and Visual Display of Data
Fig. 3 illustrates an ensemble plot of multiple convergence movements evoked from all symmetrical 4° vergence stimuli in a subject with normal binocular vision. The plot shows that there is very little variance in the responses, and the response amplitude closely matches the 4° symmetrical binocular visual stimulus when compared with the convergence insufficiency data.
FIGURE 3.
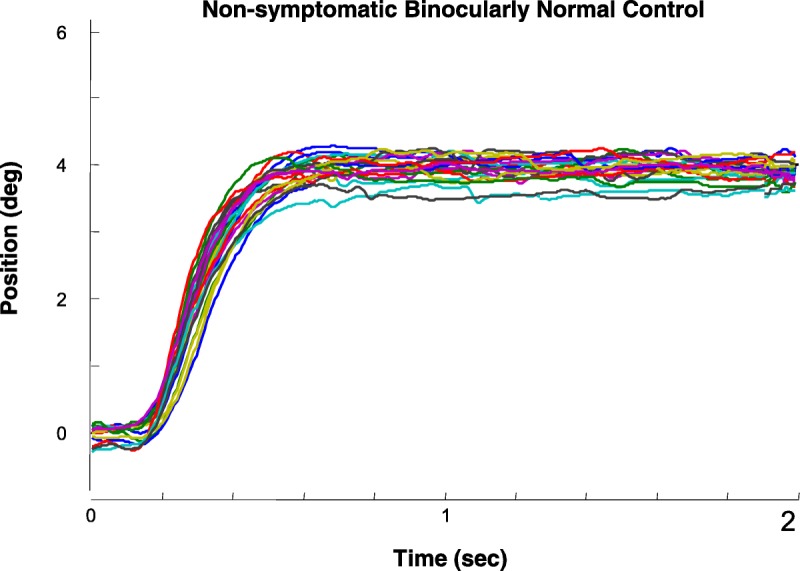
Each colored trace is an individual convergence eye movement response to a 4° symmetrical binocular disparity vergence step stimulus from a nonsymptomatic binocularly normal control participant.
In contrast, all of the convergence insufficiency participants have impaired convergence responses before office-based vergence/accommodative therapy. Fig. 4 represents an ensemble plot of all 4° vergence responses showing significant changes in the positional variance of convergence eye movements from 4° symmetrical vergence stimuli before (Figs. 4A, B, C) compared with after office-based vergence/accommodative therapy (Figs. 4D, E, F) for three participants. Figs. 4A and B show examples of two participants who exhibited substantial impairment of convergence and a more typical participant whose means are more similar to the group level means (Fig. 4C). In Fig. 4A, the convergence response within the steady state reaches approximately only 2.5° on average, and there is considerable variance in the convergence responses (from less than 2 to 4°) including one response in which it appears the participant loses convergence (loss of fusion) and then attempts to converge again. The second participant illustrated in Fig. 4B also demonstrates a high degree of variance in the convergence responses. In addition, one response suggests underconvergence followed by a second corrective convergence response after about 2 seconds. The participant illustrated in Fig. 4C is a more typical response in this sample showing variance but not as substantial as the variance observed within Figs. 4A and B. After therapy (Figs. 4D–F), the convergence response amplitudes are more accurate, and the maximum response is achieved in less than 1 second. The responses after office-based vergence/accommodative therapy look more similar to the participant with normal binocular vision (Fig. 3).
FIGURE 4.
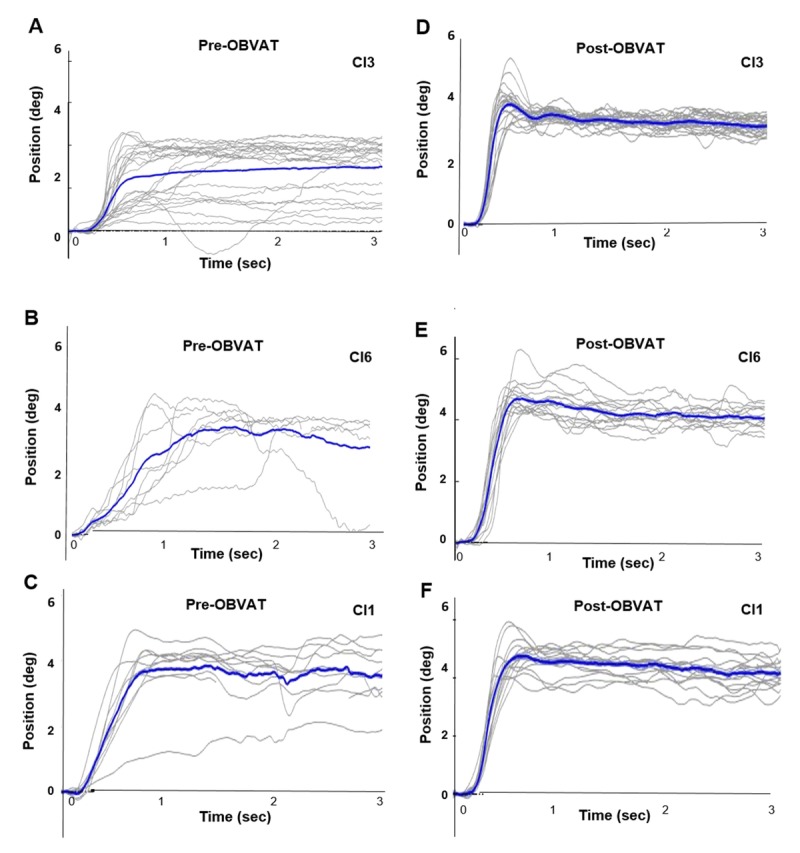
Each gray line is an individual eye movement response from a 4° symmetrical binocular disparity vergence step stimulus. The blue traces show the average position before office-based vergence/accommodative therapy (OBVAT) for participants 3 (A), 6 (B), and 1 (C). (D, E, F) The same data after OBVAT for participants 3, 6, and 1.
Fig. 5 represents averaged convergence data from the same two participants (CI3 and CI6) before and after office-based vergence/accommodative therapy. In these figures, eye movement responses are averaged to display the average eye position trace (solid lines) during the 3-second recording, as well as average velocity trace (dotted lines) on the same graph. One can observe changes in several of the response parameters such as peak velocity, time to peak velocity, and response accuracy.
FIGURE 5.
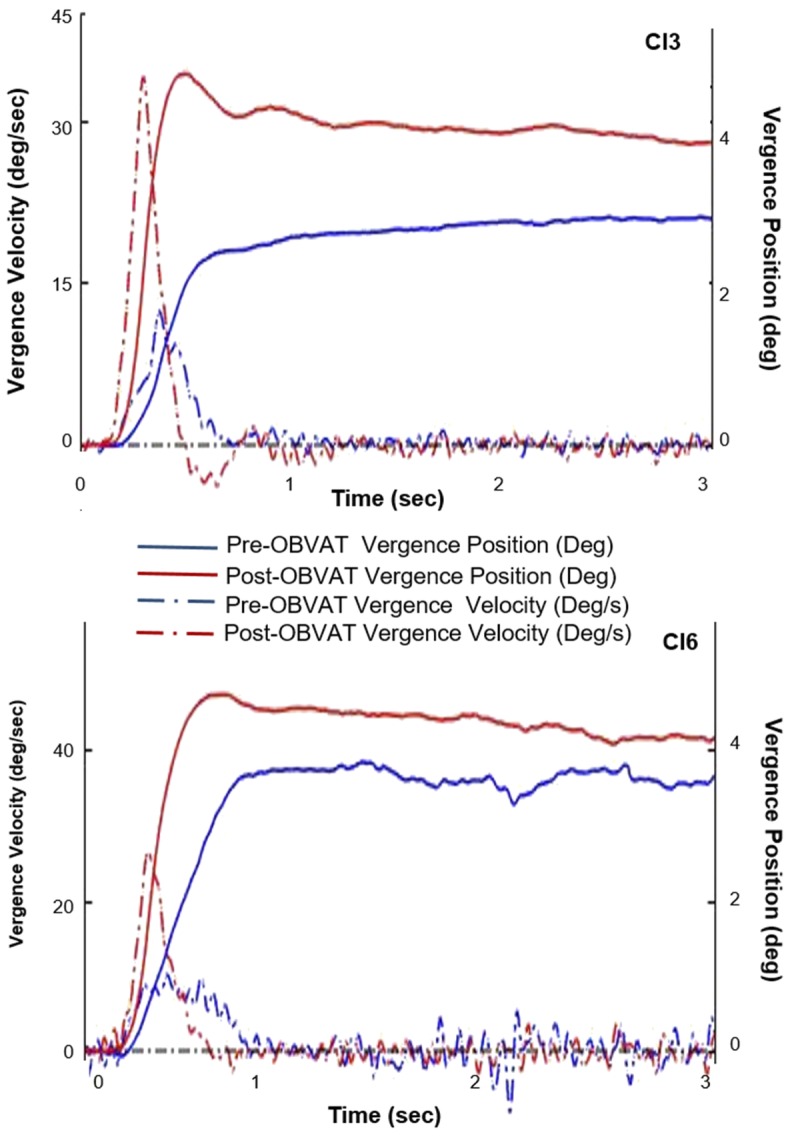
Typical convergence insufficiency participant's eye movement responses before and after office-based vergence/accommodative therapy (OBVAT). Position (solid) and velocity (dotted) as a function of time before (blue) and after (red) OBVAT for convergence in far space (upper plot) and convergence in far space (lower plot).
Objective Disparity Vergence Measures: Comparison of Data from Participants with Normal Binocular Vision with Convergence Insufficiency Participants
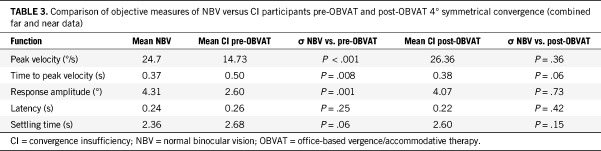
The Mann-Whitney U test was used to compare the normal binocular vision and convergence insufficiency post–office-based vergence/accommodative therapy group. These data (Table 3) indicate statistically significant differences for peak velocity, average time to peak velocity, and response amplitude for the combined far and near 4° convergence steps. A comparison of the normal binocular vision group with the convergence insufficiency group post–office-based vergence/accommodative therapy for 4° convergence steps (Table 3) indicates that peak velocity, average time to peak velocity, and response amplitude improved from baseline and were no longer statistically significant (P ≥ .05) from the normal binocular vision group values for 4° convergence steps.
TABLE 3.
Comparison of objective measures of NBV versus CI participants pre-OBVAT and post-OBVAT 4° symmetrical convergence (combined far and near data)
Objective Disparity Vergence Measures: Convergence Insufficiency Participants Pre–Office-based Vergence/Accommodative Vision Therapy and Post–Office-based Vergence/Accommodative Vision Therapy
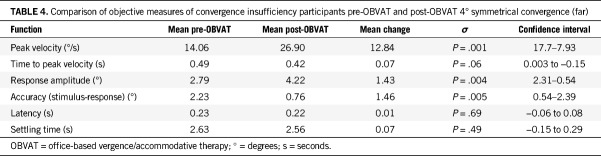
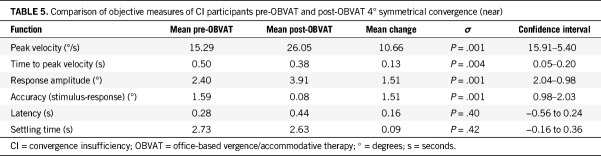
Tables 4 and 5 show that a Wilcoxon signed rank test revealed a statistically significant increase in average peak velocity after office-based vergence/accommodative therapy for both far and near 4° convergence steps (far, z = 3.06, P = .002, with a large effect size of r = 0.65; near, z = 2.98, P = .003, with a large effect size of r = 0.64). Statistically significant improvements in response amplitude were also found for far and near and a decrease in time to peak velocity for 4° convergence steps at near. Post–office-based vergence/accommodative therapy, several subjects adopted a neural control strategy of initially overshooting the visual stimulus before reaching the steady state, which from control engineering is an underdamped system. Specifically, 4 of 12 subjects and 5 of 12 subjects exhibited this behavior on average for the near and far 4° convergence steps, respectively. The individual participant data are shown in Figs. 6A and B (velocity) and Figs. 7A and B (response amplitude).
TABLE 4.
Comparison of objective measures of convergence insufficiency participants pre-OBVAT and post-OBVAT 4° symmetrical convergence (far)
TABLE 5.
Comparison of objective measures of CI participants pre-OBVAT and post-OBVAT 4° symmetrical convergence (near)
FIGURE 6.
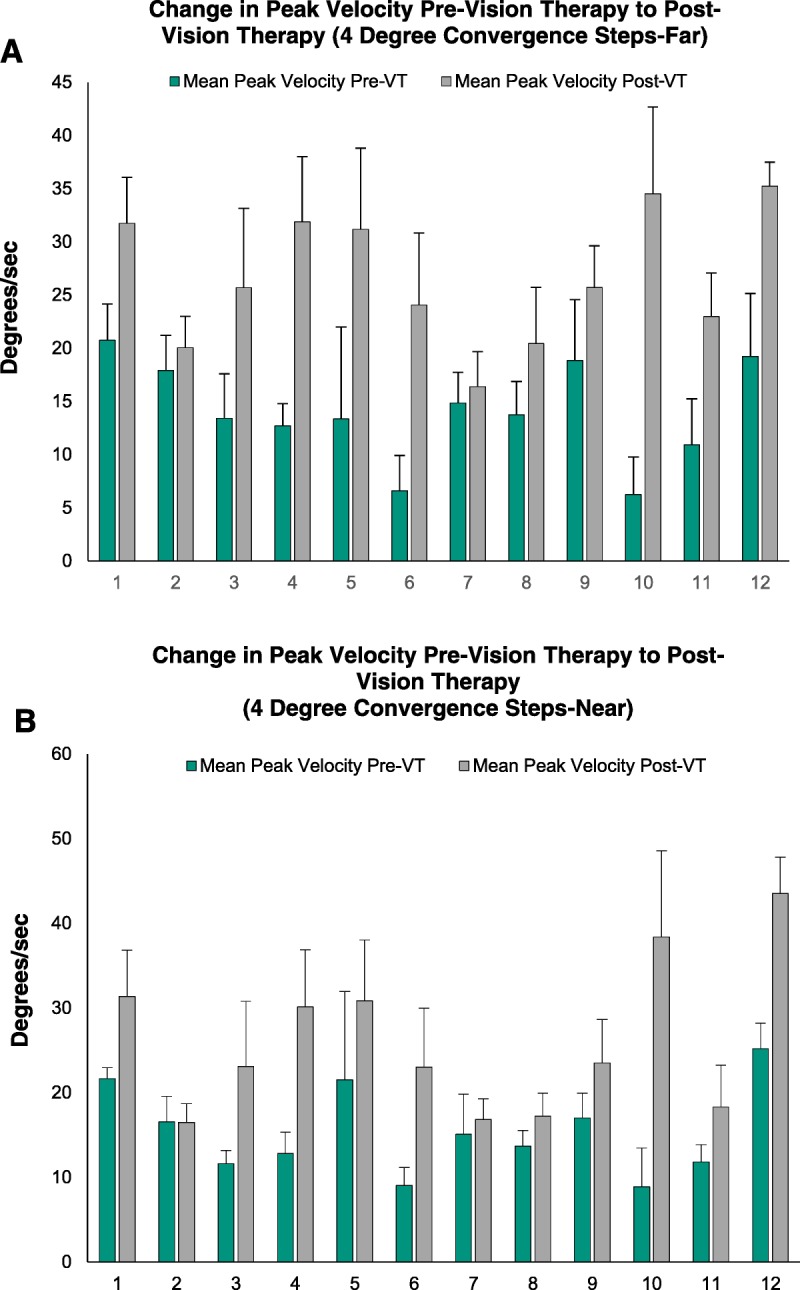
(A) The change in peak velocity pre–vision therapy (pre-VT) to post–vision therapy (post-VT) for 4° convergence steps at far. (B) The change in peak velocity pre–vision therapy to post–vision therapy for 4° convergence steps at near.
FIGURE 7.
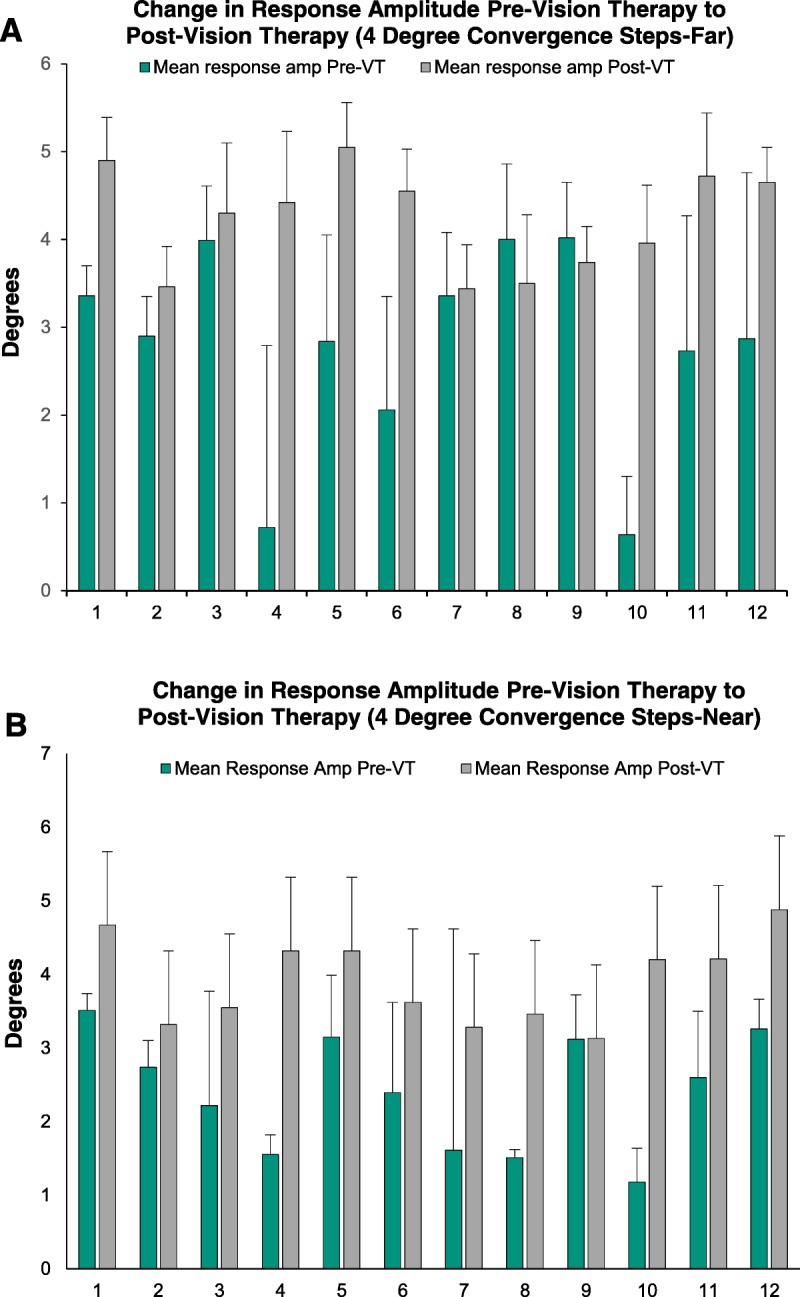
(A) The change in response amplitude pre–vision therapy (pre-VT) to post–vision therapy (post-VT) for 4° convergence steps at far. (B) The change in response amplitude pre–vision therapy to post–vision therapy for 4° convergence steps at near.
All of the statistically significant findings of mean change after office-based vergence/accommodative therapy have a medium to large effect size (>0.5), using Cohen criteria42 of 0.1, small effect; 0.3, medium effect; and 0.5, large effect, suggesting a high level of clinical significance.
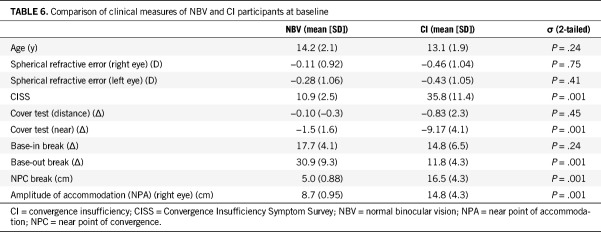
Clinical Measures
The Mann-Whitney U test was used to compare the normal binocular vision and convergence insufficiency pre–office-based vergence/accommodative therapy group. The group means of the clinical measures at baseline for both groups are shown in Table 6. For the normal binocular vision group, all measures fall within the expected range. As one would predict, all the clinical findings were statistically significantly different between the two groups at baseline except for the spherical refractive error, phoria at distance, and the base-in to break measures (Table 6). The mean Convergence Insufficiency Symptom Survey score is elevated with a mean score of 35.8 for convergence insufficiency compared with normal binocular vision groups. In addition, the three findings supporting a diagnosis of convergence insufficiency (phoria, near point of convergence, positive fusional vergence at near) all indicate that this population sample is consistent with a diagnosis of symptomatic convergence insufficiency.
TABLE 6.
Comparison of clinical measures of NBV and CI participants at baseline
Table 7 illustrates the changes that occurred in each clinical measure for the convergence insufficiency group from baseline to the outcome visit and showed statistically significant (P < .05) and clinically meaningful changes in all parameters except the cover test at distance. Although there was a statistically significant change in the near phoria, a 2Δ change is not considered clinically significant.
TABLE 7.
Comparison of clinical measures of convergence insufficiency participants pre-OBVAT and post-VT
Ten (83%) of the 12 participants in the convergence insufficiency group were categorized as successful based on these pre-determined composite criteria (Convergence Insufficiency Symptom Survey, near point of convergence, positive fusional vergence), and the remaining two (participants 6 and 12) were improved. Although these last two participants did not reach the required cutoff of less than 16 on the Convergence Insufficiency Symptom Survey, in both the Convergence Insufficiency Symptom Survey score decreased by 10 points or more (participant 6 by 19 points and participant 12 by 36 points). In addition, although participant 12 did not fully meet the criteria to be labeled successful, she did achieve the largest decrease in symptoms (36 points) of all the participants.
Relationship between Clinical Measures and Objective Measures Baseline Results
Because peak velocity and response accuracy were the two measures that showed statistically significant and clinically meaningful changes, these two parameters were used to look for correlations with clinical data at baseline. A Pearson product-moment correlation coefficient was computed to assess the relationship between peak velocity and six clinical measures. There was a positive correlation with two of the six clinical measures (positive fusional vergence at near, r = 0.45, n = 24, P = .03; vergence facility, r = 0.61, n = 18, P = .03). Overall, there was a moderate positive correlation with peak velocity and positive fusional vergence at near and vergence facility at baseline. Thus, lower positive fusional vergence at near and vergence facility findings were associated with slower peak velocity. The relationship between response accuracy and the six clinical measures was also assessed. There was a positive correlation between two of the six clinical measures (positive fusional vergence at near, r = 0.45, n = 24, P = .03; vergence facility, r = 0.65, n = 18, P = .004). Overall, there was a moderate positive correlation between response accuracy and both positive fusional vergence and vergence facility at baseline. Lower positive fusional vergence at near and vergence facility findings were associated with less accurate convergence responses.
Results After 12 Weeks of Office-based Vergence/Accommodative Vision Therapy
There was a positive correlation between change in three of the six clinical measures and change in peak velocity (vergence facility, r = 0.60, n = 24, P = .002; positive fusional vergence at near, r = 0.52, n = 24, P = .01; monocular accommodative facility, r = 0.45, n = 24, P = .03). Overall, there was a moderate positive correlation between change in peak velocity and positive fusional vergence at near, vergence facility, and monocular accommodative facility after 12 weeks of office-based vergence/accommodative therapy. The relationship between the change in response accuracy and the change in the six clinical measures was also assessed. There was a positive correlation between the change in positive fusional vergence at near and the change in response accuracy (r = 0.49, n = 24, P = .02). Overall, there was a moderate positive correlation between the change in response accuracy and the change in vergence facility after 12 weeks of office-based vergence/accommodative therapy. A smaller change in vergence facility was associated with less accurate convergence responses after 12 weeks of treatment.
DISCUSSION
In this study, significant changes were found in symptoms and both clinical and objective measures of disparity vergence after completion of office-based vergence/accommodative therapy in children with symptomatic convergence insufficiency. This is the first prospective study on the treatment of symptomatic convergence insufficiency in children in which both clinical and objective eye movement measurements have been used to evaluate the results of treatment. The changes in clinical measures observed after office-based vergence/accommodative therapy in this study are comparable with those reported in previous randomized clinical trials with children with symptomatic convergence insufficiency.8,41
The unique aspect of this study was the addition of objective measures of temporal (response latency, time of peak velocity, and settling time) and spatial measurements (peak velocity and response accuracy) of disparity vergence. The use of objective recording of vergence eye movements allows the investigator to access additional more subtle information about the physiology of these eye movements that is not available with traditional clinical testing. The study revealed statistically significant improvements in peak velocity, time to peak velocity, and response amplitude after 12 weeks of office-based vergence/accommodative therapy for 4° convergence steps. These findings are consistent with a previous study11 in pre-presbyopic adults with convergence insufficiency in which Alvarez et al.11 found a significant increase in convergence peak velocity. The results of other studies are available, but direct comparison is challenging because these authors did not limit their subject recruitment to convergence insufficiency.
In regard to clinical relevance of the study results, the strongest correlation between clinical and objective measures in this study was between changes in vergence facility and peak velocity. This is an important finding and suggests that vergence facility testing should be used as a standard assessment tool for the evaluation of binocular vision disorders.
Although not the primary aim of this study, an important secondary goal was to determine whether the use of objective eye movement recordings would be feasible in a large multicenter clinical trial with children. The previous Convergence Insufficiency Treatment Trial Investigator Group studies7,8,21,43 used well-accepted traditional clinical tests as outcome measures. These tests are sometimes referred to as objective clinical measures; however, they are actually subjective and rely upon the participant to tell the investigator what they are seeing. The possibility of adding a more objective measurement, less prone to bias, is a potentially valuable addition to future clinical trials. The key perceived concerns have been feasibility issues related to maintaining the equipment over a long period of time in good working condition, the length of the required testing session, the age at which participants would be able to be tested, and whether the proposed testing sequence would yield any significant physiological changes in vergence and version eye movements. The results of this study have answered all of these questions. Data gathering occurred over an 18-month period of time, and the system was stable with no downtime. Attempts were made to test children as young as 9 years old, but testing was not feasible until about the age of 12 years. Younger children were unable to maintain a stable head position for long-enough periods to gather meaningful data. The testing session lasted about 25 to 30 minutes, and all participants 12 years or older could be tested. Finally, significant changes were found in several physiological measures including peak velocity and response accuracy.
There are several study limitations. Although we demonstrated significant changes in some objective aspects of disparity vergence, we are unable to say with a high level of confidence that these findings normalized after office-based vergence/accommodative therapy. There are limited data available about expected findings for the five objective measures of disparity vergence used as outcome measures in this study. We enrolled 10 children with normal binocular vision and used their data as a reference point in this study. However, we recognize that this is a small sample size, and it would be desirable to develop expected findings for these measures in a much larger sample.
In addition, there was no placebo treatment group, and the examiners at the outcome visit were not masked, potentially introducing bias, particularly within the clinical testing. However, the advantage of using objective testing, the primary outcome in this study, is that these measures are unlikely to be susceptible to bias. Because of instrumentation limitations at the time of data collection, we were unable to simultaneously evaluate the vergence and accommodative systems. Finally, even though the subjects with normal binocular vision were not treated, it would have been informative to reevaluate the subjects after 12 weeks. This information would have revealed information about the repeatability of objective measurements of vergence. It also would have been interesting to see if there were changes to disparity vergence in the group with normal binocular vision after going through office-based vergence/accommodative therapy, even though they did not have convergence insufficiency.
This is the first report of the use of objective measures of disparity vergence as outcome measures for symptomatic convergence insufficiency in children after office-based vergence/accommodative therapy. These measures provide additional information that is not accessible with clinical tests. The study results also demonstrate that children 12 to 17 years of age can be successfully tested using a protocol that requires about 25 minutes and suggests that these measures could be used in future large-scale randomized clinical trials of binocular vision disorders.
Footnotes
Funding/Support: National Science Foundation (NSF MRI CBET 1428425; to TLA) and National Eye Institute (1R01EY023261; to TLA).
Conflict of Interest Disclosure: None of the authors have reported a financial conflict of interest.
Study Registration Information: Trial Registration: clinicaltrials.gov Identifier: NCT03248336 (date of registration August 7, 2017).
Author Contributions: Conceptualization: MS, TLA; Data Curation: MS; Formal Analysis: MS, HT, TLA; Funding Acquisition: TLA; Investigation: MS, TLA; Methodology: MS, TLA; Project Administration: MS, TLA; Software: HT, TLA; Supervision: TLA; Validation: MS; Visualization: MS; Writing – Original Draft: MS, TLA; Writing – Review & Editing: HT, TLA.
REFERENCES
- 1.Rouse MW, Borsting E, Hyman L, et al. Frequency of Convergence Insufficiency among Fifth and Sixth Graders. Optom Vis Sci 1999;76:643–9. [DOI] [PubMed] [Google Scholar]
- 2.Hussaindeen JR, Rakshit A, Singh NK, et al. Prevalence of Non-strabismic Anomalies of Binocular Vision in Tamil Nadu: Report 2 of Band Study. Clin Exp Optom 2017;100:642–8. [DOI] [PubMed] [Google Scholar]
- 3.Davis AL, Harvey EM, Twelker JD, et al. Convergence Insufficiency, Accommodative Insufficiency, Visual Symptoms, and Astigmatism in Tohono O'odham Students. J Ophthalmol 2016;2016:6963976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wajuihian SO, Hansraj R. Vergence Anomalies in a Sample of High School Students in South Africa. J Optom 2016;9:246–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Borsting E, Rouse MW, Deland PN, et al. Association of Symptoms and Convergence and Accommodative Insufficiency in School-age Children. Optometry 2003;74:25–34. [PubMed] [Google Scholar]
- 6.Barnhardt C, Cotter SA, Mitchell GL, et al. Symptoms in Children with Convergence Insufficiency: Before and After Treatment. Optom Vis Sci 2012;89:1512–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scheiman M, Mitchell GL, Cotter S, et al. A Randomized Clinical Trial of Treatments for Convergence Insufficiency in Children. Arch Ophthalmol 2005;123:14–24. [DOI] [PubMed] [Google Scholar]
- 8.Convergence Insufficiency Treatment Trial Investigator Group. Randomized Clinical Trial of Treatments for Symptomatic Convergence Insufficiency in Children. Arch Ophthalmol 2008;126:1336–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scheiman M, Gwiazda J, Li T. Non-surgical Interventions for Convergence Insufficiency. Cochrane Database Syst Rev 2011;CD006768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grisham JD, et al. Vergence Orthoptics: Validity and Persistence of the Training Effect. Optom Vis Sci 1991;68:441–51. [DOI] [PubMed] [Google Scholar]
- 11.Alvarez TL, Vicci VR, Alkan Y, et al. Vision Therapy in Adults with Convergence Insufficiency: Clinical and Functional Magnetic Resonance Imaging Measures. Optom Vis Sci 2010;87:985–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scheiman M, Ciuffreda KJ, Thiagarajan P, et al. Objective Assessment of Vergence and Accommodation After Vision Therapy for Convergence Insufficiency in a Child: A Case Report. Optom Vis Perf 2014;2:7–12. [Google Scholar]
- 13.Scheiman MM, Talasan H, Mitchell GL, et al. Objective Assessment of Vergence After Treatment of Concussion-related CI: A Pilot Study. Optom Vis Sci 2017;94:74–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bucci MP, Kapoula Z, Yang Q, et al. Speed-accuracy of Saccades, Vergence and Combined Eye Movements in Children with Vertigo. Exp Brain Res 2004;157:286–95. [DOI] [PubMed] [Google Scholar]
- 15.Jainta S, Bucci MP, Wiener-Vacher S, et al. Changes in Vergence Dynamics Due to Repetition. Vision Res 2011;51:1845–52. [DOI] [PubMed] [Google Scholar]
- 16.Morize A, Brémond-Gignac D, Daniel F, et al. Effects of Pure Vergence Training on Initiation and Binocular Coordination of Saccades. Invest Ophthalmol Vis Sci 2017;58:329–42. [DOI] [PubMed] [Google Scholar]
- 17.Daniel F, Morize A, Brémond-Gignac D, et al. Benefits from Vergence Rehabilitation: Evidence for Improvement of Reading Saccades and Fixations. Front Integr Neurosci 2016;10:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kapoula Z, Morize A, Daniel F, et al. Objective Evaluation of Vergence Disorders and a Research-based Novel Method for Vergence Rehabilitation. Transl Vis Sci Technol 2016;5:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rouse M, Borsting E, Mitchell GL, et al. Validity of the Convergence Insufficiency Symptom Survey: A Confirmatory Study. Optom Vis Sci 2009;86:357–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Borsting EJ, Rouse MW, Mitchell GL, et al. Validity and Reliability of the Revised Convergence Insufficiency Symptom Survey in Children Aged 9–18 Years. Optom Vis Sci 2003;80:832–8. [DOI] [PubMed] [Google Scholar]
- 21.Scheiman M, Cotter S, Rouse M, et al. Randomised Clinical Trial of the Effectiveness of Base-in Prism Reading Glasses Versus Placebo Reading Glasses for Symptomatic Convergence Insufficiency in Children. Br J Ophthalmol 2005;89:1318–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Convergence Insufficiency Treatment Trial Investigator Group. The Convergence Insufficiency Treatment Trial: Design, Methods, and Baseline Data. Ophthalmic Epidemiol 2008;15:24–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van Rijn LJ, van der Steen J, Collewijn H. Instability of Ocular Torsion during Fixation: Cyclovergence Is More Stable than Cycloversion. Vision Res 1994;34:1077–87. [DOI] [PubMed] [Google Scholar]
- 24.Saladin JJ. Convergence Insufficiency, Fixation Disparity, and Control Systems Analysis. Am J Optom Physiol Opt 1986;63:645–53. [DOI] [PubMed] [Google Scholar]
- 25.Hung GK, Semmlow JL. Static Behavior of Accommodation and Vergence: Computer Simulation of an Interactive Dual-feedback System. IEEE Trans Biomed Eng 1980;27:439–47. [DOI] [PubMed] [Google Scholar]
- 26.Semmlow JL, Hung GK. Binocular Interactions of Vergence Components. Am J Optom Physiol Opt 1980;57:559–65. [DOI] [PubMed] [Google Scholar]
- 27.Maxwell J, Tong J, Schor CM. Short-term Adaptation of Accommodation, Accommodative Vergence and Disparity Vergence Facility. Vision Res 2012;62:93–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schor CM. A Dynamic Model of Cross-coupling between Accommodation and Convergence: Simulations of Step and Frequency Responses. Optom Vis Sci 1992;69:258–69. [DOI] [PubMed] [Google Scholar]
- 29.Schor CM. Models of Mutual Interactions between Accommodation and Convergence. Am J Optom Physiol Opt 1985;62:369–74. [DOI] [PubMed] [Google Scholar]
- 30.Kotulak JC, Schor CM. The Effects of Optical Vergence, Contrast, and Luminance on the Accommodative Response to Spatially Bandpass Filtered Targets. Vision Res 1987;27:1797–806. [DOI] [PubMed] [Google Scholar]
- 31.Schor CM, Kotulak JC. Dynamic Interactions between Accommodation and Convergence Are Velocity Sensitive. Vision Res 1986;26:927–42. [DOI] [PubMed] [Google Scholar]
- 32.Kim EH, Granger-Donetti B, Vicci VR, et al. The Relationship between Phoria and the Ratio of Convergence Peak Velocity to Divergence Peak Velocity. Invest Ophthalmol Vis Sci 2010;51:4017–27. [DOI] [PubMed] [Google Scholar]
- 33.Kim E, Alvarez TL. The Frequency of Saccades Correlates to Peak Velocity in Symmetrical Disparity Vergence. Conf Proc IEEE Eng Med Biol Soc 2011;2011:1664–7. [DOI] [PubMed] [Google Scholar]
- 34.Kim EH, Alvarez TL. The Frequency of Horizontal Saccades in Near and Far Symmetrical Disparity Vergence. Vision Res 2012;63:9–19. [DOI] [PubMed] [Google Scholar]
- 35.Alvarez TL, Kim EH. Analysis of Saccades and Peak Velocity to Symmetrical Convergence Stimuli: Binocularly Normal Controls Compared to Convergence Insufficiency Patients. Invest Ophthalmol Vis Sci 2013;54:4122–35. [DOI] [PubMed] [Google Scholar]
- 36.Alvarez TL, Jaswal R, Gohel S, et al. Functional Activity within the Frontal Eye Fields, Posterior Parietal Cortex, and Cerebellar Vermis Significantly Correlates to Symmetrical Vergence Peak Velocity: An ROI-based, fMRI Study of Vergence Training. Front Integr Neurosci 2014;8:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Semmlow JL, Chen YF, Granger-Donetti B, et al. Correction of Saccade-induced Midline Errors in Responses to Pure Disparity Vergence Stimuli. J Eye Mov Res 2009;2:1–13.20664810 [Google Scholar]
- 38.Alvarez TL, Semmlow JL, Yuan W, et al. Comparison of Disparity Vergence System Responses to Predictable and Nonpredictable Stimulations. Curr Psychol Cogn 2002;21:243–61. [Google Scholar]
- 39.Bahill AT, Kallman JS, Lieberman JE. Frequency Limitations of the Two-point Central Difference Differentiation Algorithm. Biol Cybern 1982;45:1–4. [DOI] [PubMed] [Google Scholar]
- 40.Zee DS, Fitzgibbon EJ, Optican LM. Saccade-vergence Interactions in Humans. J Neurophysiol 1992;68:1624–41. [DOI] [PubMed] [Google Scholar]
- 41.Scheiman MM, Hertle RW, Beck RW, et al. Randomized Trial of Treatment of Amblyopia in Children Aged 7 to 17 Years. Arch Ophthalmol 2005;123:437–47. [DOI] [PubMed] [Google Scholar]
- 42.Cohen J. Statistical Power Analyses for the Behavioral Sciences, 2nd ed Hillsdale, NH: Earlbaum Associates; 1988. [Google Scholar]
- 43.Scheiman M, Mitchell GL, Cotter S, et al. A Randomized Clinical Trial of Vision Therapy/Orthoptics Versus Pencil Pushups for the Treatment of Convergence Insufficiency in Young Adults. Optom Vis Sci 2005;82:583–95. [DOI] [PubMed] [Google Scholar]