This scoping study found 13 theories or models that offer guidance on adapting evidence-based programs. Eleven common steps in the adaptation process were identified.
Keywords: Evidence-based interventions, Program adaptation, Dissemination, Implementation, Frameworks, Public health
Abstract
Evidence-based public health translation of research to practice is essential to improve the public’s health. Dissemination and implementation researchers have explored what happens once practitioners adopt evidence-based interventions (EBIs) and have developed models and frameworks to describe the adaptation process. This scoping study identified and summarized adaptation frameworks in published reports and grey literature. We followed the recommended steps of a scoping study: (a) identifying the research question; (b) identifying relevant studies; (c) selecting studies; (d) charting the data; (e) collating, summarizing, and reporting the results; and (f) consulting with experts. We searched PubMed, PsycINFO, PsycNET, and CINAHL databases for articles referencing adaptation frameworks for public health interventions in the published and gray literature, and from reference lists of framework articles. Two reviewers independently coded the frameworks and their steps and identified common steps. We found 13 adaptation frameworks with 11 program adaptation steps: (a) assess community, (b) understand the EBI(s), (c) select the EBI, (d) consult with experts, (e) consult with stakeholders, (f) decide on needed adaptations, (g) adapt the original EBI, (h) train staff, (i) test the adapted materials, (j) implement the adapted EBI, and (k) evaluate. Eight of these steps were recommended by more than five frameworks: #1–3, 6–7, and 9–11. This study is the first to systematically identify, review, describe, and summarize frameworks for adapting EBIs. It contributes to the literature by consolidating key steps in program adaptation of EBIs and describing the associated tasks in each step.
Implications
Practice: These frameworks can offer guidance for steps in the adaptation process for evidence-based interventions (EBIs).
Policy: Funders or agencies that recommend the use of EBIs should encourage organizations implementing them to report on any adaptation and the steps taken for the modifications.
Research: Future research should examine the use of these frameworks in adaptations of EBIs in the field and their impacts on health.
INTRODUCTION
Dissemination and implementation (D&I) researchers focusing on the process in which new evidence-based interventions (EBIs) are integrated into clinical and community practice have found that organizations often make changes to fit the needs of their community and the capacity of their organization [1–4]. Despite the continuing debate about the relative importance of fidelity (delivery as originally designed) versus adaptation, some level of adaptation typically occurs [1]. Adaptation typically happens at the T3 stage of research when EBIs are scaled into everyday practice, after the efficacy (T1) and effectiveness studies (T2) [5, 6], although some adaptation occurs after T1 in advance of T2. Adaptations may be made to the original program’s content, delivery, logistics, training, and evaluation [4, 7]. Some researchers say that adaptations are an essential and natural step in the implementation process; others express concern that any modification to the original EBI could reduce the EBI’s efficacy or effectiveness [2, 8, 9]. Programs delivered with high fidelity have reported better outcomes than those of programs implemented with lower fidelity [10–12].
The research on program adaptation of EBIs is fairly new. Some recent efforts have been made to understand its use in practice. Stirman et al. [4] presented common types of modifications which include adding, lengthening, shortening, substituting, removing, or re-ordering program components; integrating another approach or intervention; loosening structure; or departing from the intervention (i.e., program stopped). Other taxonomies for types, reasons for making adaptations [13, 14], timing of the adaptation (proactive vs. reactive) and valence of change [13], and modifications made (additions/change/deletion) [14] have been developed. Chambers and Norton have proposed the adaptome model to synthesize knowledge about program adaptation and their impacts on implementation and outcomes and call for further research on components of adaptation including the process of modification, by whom, and context of the adaptation [15].
This tension between fidelity and adaptation gave rise to adaptation frameworks, suggesting steps that organizations could take to select, adapt, and implement EBIs in order to make the program fit the new context better while minimizing changes that could negatively affect the EBI effectiveness [8, 16]. Taken together and distilling common elements, these frameworks could inform a systematic process for program adaptation for the field. Using theories, frameworks, and models within dissemination and implementation research improves EBI implementation and sustainability, and the use of adaptation frameworks to increase acceptability, fit, and effectiveness is no exception [17,18].
Both researchers and practitioners have recommended frameworks to guide adaptation of effective interventions [19,20]. Other D&I models and frameworks have been compiled and summarized with the goal of improving practice [18, 21, 22]. No review of adaptation frameworks exists in the peer-reviewed scientific literature other than Krivitsky and colleagues’ book chapter summarizing several common frameworks [8] and Bartholomew Eldredge and associates’ more recent summary in their chapter on adaptation [7]. The absence of a comprehensive review of adaptation processes and practices in the literature prompted this scoping study [7].
Scoping studies differ from systematic reviews in their focus on comprehensive coverage rather than quality of evidence and map key concepts in an area of research, with analytic reinterpretation of the literature [23]. They overcome challenges associated with literature reviews, such as lack of consistent terms in the field of interest [23,24]. We selected a scoping study as a suitable approach to review and summarize program adaptation frameworks in both the published and grey literature to retrieve frameworks employed in research and practice.
Our purpose is to provide a summary of adaptation frameworks for public health interventions used in research and practice and key adaptation tasks, including the common steps the frameworks recommend. The study answers the following questions: (a) What adaptation frameworks to adapt public health EBIs have been described in published reports and gray literature? and (b) What are the common adaptation steps suggested across the adaptation frameworks? We also provide a chronology of the publication of the frameworks and associated sentinel events to provide context for the development of the adaptation frameworks. This review of known adaptation frameworks offers researchers and practitioners a valuable resource of frameworks and key steps for adaptation. This knowledge can facilitate proper program adaptation, thereby improving adoption, use, maintenance, and effectiveness of evidence-based public health interventions.
METHODS
The scoping study typically occurs in five steps, as outlined by Arksey and O’Malley [23], plus a sixth step that has recently been identified as an essential component of scoping study methods [25]. These steps include: (a) identifying the research question; (b) identifying relevant studies (frameworks); (c) study/framework selection; (d) charting the data; (e) collating, summarizing, and reporting the results; and (f) consultation with external experts or stakeholders.
Step 1: Identifying the research question
This scoping study was guided by the following questions: (a) What adaptation frameworks to adapt public health EBIs are found in published reports and gray literature? and (b) What are the common adaptation steps suggested across the adaptation frameworks?
Step 2: Identifying potentially relevant frameworks
We identified articles describing the use of adaptation frameworks using three methods. (a) We searched the “gray literature,” including book chapters, books, conference abstracts, dissertations, and other published and unpublished materials not normally identifiable through bibliographic [26,27]. We searched Google Scholar with keywords “program adaptation” alone and with the addition of “evidence-based” in May 2016. (b) We drew on a literature review for an associated systematic review of program adaptations of evidence-based interventions that had searched PubMed, PsycINFO, PsycNET, and CINAHL via OVID interface in December 2014 to June 2016 [28]. We discussed search criteria and databases with the consultation of a health sciences librarian. These searches used both MeSH (Medical Subject Headings) and general terms for PubMed and adapted terms for the other databases that included the concepts of adaptation, evidence-based programs/interventions, and behavioral and public health practice. (Specific search terms available from the first author.) (c) We also searched the bibliographies of framework articles from the gray literature and articles selected for the systematic review.
The first two searches yielded 543 article abstracts after the removing duplicates. From these, we selected articles published in English after January 1, 1995 that described the methods or process of adapting an evidence-based intervention, including programs and policies, or best practices, models, or outcomes of adapted interventions. (We excluded articles in other languages because of search team language limitations and the possible difficulty in accessing journals in other languages.) This review resulted in 60 full text articles that were deemed potentially relevant. We added further criteria to select original adaptation frameworks in Step 3 below.
Step 3: Study (framework) selection
We then focused on selecting articles that described a program adaptation framework or the author’s description of systematic steps in adaptation (not attributed to a previous framework) used to adapt public health EBIs produced originally in the USA. We excluded those that focused on clinical interventions or protocols. Each candidate study abstract or document and full article was reviewed independently by two individuals for inclusion (C.E. and H.U.). We excluded studies that applied an adaptation framework described elsewhere (e.g., Tortolero et al. [29] and Highfield et al. [30]).
Step 4: Charting the data
According to Arksey and O’Malley [23], charting is a technique to sort through the data for synthesis and interpretation. Using a descriptive analytic method, we analyzed and sorted the articles according to the adaptation framework and steps described in each. We charted each framework and its respective steps into a “data charting form” using Excel [23]. The data included columns with each framework and then rows with the steps, using the exact language described in the framework. We identified commonalities among the frameworks, and provided standardized names for similar adaptation steps. One researcher (C.E.) reviewed the steps described in each article and listed a suggested step name and its descriptions in a table. A second researcher (H.U.) independently reviewed this table and, using a consensus process, both created names for the final included steps (e.g., assess the community).
Step 5: Collating, summarizing, and reporting the results
We structured the results according to categories of common program adaptation steps across the adaptation frameworks. First, we summarized the authors’ description of each step and tallied the frequency of the step’s inclusion in the reviewed frameworks (Supplemental Table 1). Two researchers (E.B. and H.U.) performed a cross walk of the steps descriptions for each framework and developed a final matrix that was verified by a third reviewer (C.E.). Step descriptions and frequencies are reported by step name and article or document author. To identify more commonly used frameworks, we used PubMed, Web of Science, and Google Scholar to identify the number of citations for each adaptation framework. We calculated the total citations for each scientific article using Scopus and Web of Science, with duplicates removed. We employed Google Scholar for citations in the gray literature.
Step 6: Consultation with stakeholders or experts
The protocol and methods for this scoping study were developed in collaboration with researchers who are considered experts on adaptation and translation from the University of Texas (UT) School of Public Health. UTSPH implementation researchers working in the area of program adaptation reviewed the definitions and final steps for construct (face validity). They have experience in adapting interventions and increasing use of EBIs with an emphasis on adaptation [31,32].
RESULTS
Overview and relations among the frameworks
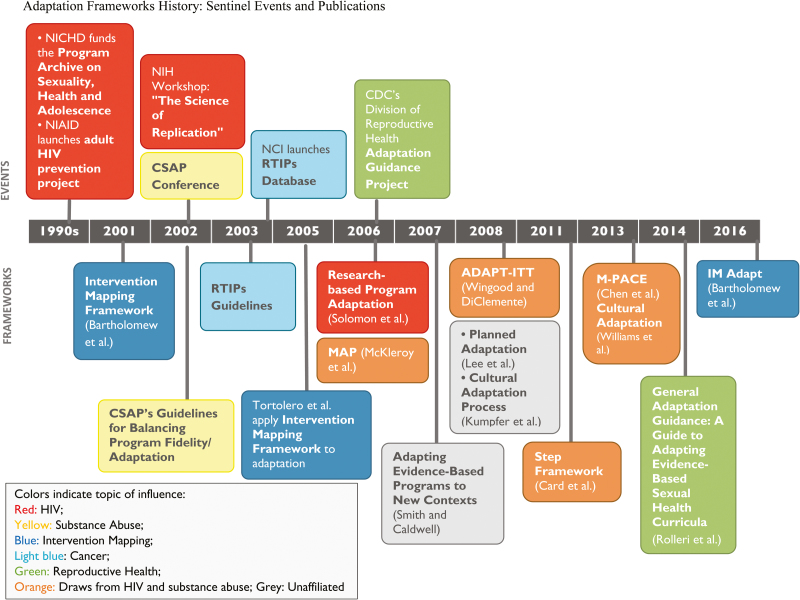
We identified 13 frameworks that presented adaptation steps—three from the gray literature (The National Cancer Institute (NCI) website Guidelines for Choosing and Adapting Programs [33], Finding the Balance: Program Fidelity and Adaptation in Substance Abuse Prevention [34]), and IM (Intervention Mapping) Adapt [7, 35, 36] and 10 from the published literature [16, 19, 20, 37–43]. These reports can be characterized generally as a dialectic, with mutual citation and acknowledgement and positioning of new frameworks as building on previous work (Figure 1).
Fig. 1.
| Adaptation frameworks history: sentinel events and publications.
To illustrate this interconnectedness of the frameworks, we present a chronology of sentinel events leading to the frameworks to follow. Framework development was largely supported by four U.S. governmental agencies: (a) the National Institute for Child Health and Human Development (NICHD), (b) National Institute of Allergy and Infectious Diseases (NIAID), (c) Center for Substance Abuse Prevention (CSAP) in the Substance Abuse and Mental Health Services Administration, and (d) Centers for Disease Control and Prevention (CDC). The first three sponsored seminal conferences in 2002, with CDC’s participation.
The National Institutes of Health (NIH) workshop, The Science of Replication, sponsored by NICHD and the NIAID, focused on HIV interventions and the translation from efficacy to dissemination. Solomon and associates’ framework [39] was based on a paper presented at the workshop, a compilation of principles and processes for adapting HIV prevention programs based on empirical literature. This direction began with from NICHD funding in 1993 to develop the Program Archive on Sexuality, Health, and Adolescence, a collection of replication kits for empirically validated teen pregnancy and youth sexually transmitted infections (STIs) and HIV prevention programs. NIAID launched a similar project in the late 1990’s for adult HIV prevention. Card and associates’ framework [38] also had an HIV focus, although it was described as applying to other intervention topics.
The CSAP-sponsored conference, represented here as the earliest framework [34], highlighted issues in balancing program fidelity and adaptation and guidance. This conference and Backer’s work around the same time was cited by most framework developers. McKleroy and associates [19], for example, in reporting the draft of the MAP (Map of the Adaptation Process, p. 62) framework described the project as aiming to add more detail and step-by-step guidance to assist intervention implementers in navigating the many issues raised by CSAP and others. Subsequently, Wingood and DiClemente [20] characterized MAP as too complex for community-based organizations and proposed ADAPT-ITT, a sequential process, with origins in ethnography [44] and cultural adaptation of EBIs [2].
Rolleri and associates [11] reported later on the CDC’s Division of Reproductive Health Adaptation Guidance Project (begun in 2006), acknowledging Backer [34], Solomon et al. [39], McKleroy el al. [19], Wingood and DiClemente [20], and an early version of IM ADAPT [7] that had focused on teen pregnancy prevention [30]. This new framework piloted the practitioner-friendly green-yellow-red light adaptation schema that appears on websites that discuss adaptation (e.g., Putting Public Health in Action Training Workshop of the Cancer Prevention and Control Research Network: http://cpcrn.org/).
Citing most of the models above, Chen and associates [37] observed that it is “now both possible and necessary to focus on articulating separate steps of the process rather than offering general advice” (p. 2). Their foci were (a) methods to identify population differences through participant feedback, which they believed had received too little priority, and (b) a process for deciding what to change, which they noted had highly variable actors across the previous frameworks. The intervention mapping framework was first reported in a 1998 article and 2001 textbook by Bartholomew et al. [35,36] as a tool for program design, adoption, and implementation. It has recently been revised with the most recent iteration known as “IM Adapt” published recently [5]. The authors contrasted their “how-to” approach with previous frameworks, which describe more general processes. Finally, four frameworks do not appear to reflect the same origins as the others: cultural adaptation [40], contextual translation process [41], Planned Adaptation [42], and cultural adaptation process [43]. Three cite the same writers on cultural adaptation [2, 40], but they do not cite the other frameworks. Williams et al., the one article with an international adaptation of an EBI [40], also cited Castro [2] and Solomon’s work [39] in their adaptation process
Common steps in the adaptation process
The frameworks we identified consisted of different steps with some overlap. We identified 11 program adaptation steps and grouped them into the following categories: (a) assess community, (b) understand the EBI(s), (c) select the EBI, (d) consult with experts, (e) consult with stakeholders, (f) decide what needs adaptation, (g) adapt the original program, (h) train staff, (i) test the adapted materials, (j) implement, and (k) evaluate (Table 1).
Table 1.
| Key adaptation steps and descriptions
| Step name | Step descriptions |
|---|---|
| 1.Assess community | • Identify behavioral determinants and risk behaviors of the new target population using focus groups, interviews, needs assessments, and logic models • Assess organizational capacity to implement the program |
| 2.Understand the intervention | • Identify and review relevant EBPs and their program materials • Understand the theory behind the programs and their core elements |
| 3.Select intervention | • Select the program that best matches the new population and context |
| 4.Consult with experts | • Consult content experts, including original program developers, as needed • Incorporate expert advice into program |
| 5.Consult with stakeholders | • Seek input from advisory boards and community planning groups where program implementation takes place • Identify stakeholder partners who can champion program adoption in new setting and ensure program fidelity |
| 6.Decide what needs adaptation | • Decide whether to adapt or implement original program • Theater test selected EBP using new target population and other stakeholders to generate adaptations • Determine how original and new target population/setting differ in terms of risk and protective factors • Identify areas where EBP needs to be adapted and include possible changes in program structure, content, provider, or delivery methods • Retain fidelity to core elements • Systematically reduce mismatches between the program and the new context |
| 7.Adapt the original program | • Develop adaptation plan • Adapt the original program contents through collaborative efforts • Make cultural adaptations continuously through pilot testing • Core components responsible for change should not be modified |
| 8.Train staff | • Select and train staff to ensure quality implementation |
| 9.Test the adapted materials | • Pretest adapted materials with stakeholder groups • Conduct readability tests • Pilot test adapted EBP in new target population • Modify EBP further if necessary |
| 10.Implement | • Develop implementation plan based on results generated in previous steps • Identify implementers, behaviors, and outcomes • Develop scope, sequence, and instructions • Execute adapted EBP |
| 11.Evaluate | • Document the adaptation process and evaluate the process and outcomes of the adapted intervention as implemented • Write evaluation questions; choose indicators, measures, and the evaluation design; plan data collection, analysis, and reporting • Employ empowerment evaluation approach framework to improve program implementation |
Framework descriptions of the steps were similar, with some variation. The Supplementary Table 1 file presents the steps as described by each author(s) of the 13 frameworks. For example, descriptions of the assessing community step often included conducting needs assessments, focus groups, and interviews to ascertain the community context and risk factors of the new target population [7, 20, 33, 39, 40, 43]. Three frameworks also included an assessment of the implementing organization’s capacity [7, 19, 20]. Understanding the intervention included both identifying relevant EBIs [7, 19, 20], the program theory/logic [16, 33, 34, 42] and the EBI’s core elements [7, 16, 19, 34, 38]. In the step deciding what needs adaptation, most authors recommended examining mismatches between the original program model and the new context [38, 39, 41, 42] and identifying areas where the EBI needs to be adapted [7, 16, 19, 20, 34, 38, 40–42]. Fidelity to the core program was also mentioned in this step [16, 34, 39].
Summary of commonalities across frameworks
Eight common steps were: 1) assess community or population of interest, 2) understand the original EBI(s), 3) select an EBI, 4) decide what needs to be adapted, 5) adapt the original program, 5) test the adapted materials, 6) implement the invention, and 7) evaluate (Table 2). According to our categorization, the most common step is decide what needs adaptation, mentioned 12 times (93%), followed by understand the EBI, cited in 8 (69%) out of the 12 frameworks. The next commonly noted step includes adapt the original program, cited in 8) (62%) studies assess the community and evaluate were included in seven (54%) frameworks. Finally, seven (54%) frameworks reported select EBI and test the adapted materials as program adaptation steps and five (42%) noted implement as a step.
Table 2.
| Summary of program adaptation steps by the 13 adaptation frameworks
| Gray literature | Scientific literature | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adaptation steps | IM ADAPT [7] |
CSAP’s guidelines for balancing program fidelity/ adaptation
[34] |
RTIPs adaptation guidelines [33] | Map of adaptation process (MAP) [19] | Research- based program adaptation [39] | Adapting evidence-based programs to new contexts [41] | ADAPT-ITT [20] | Cultural adaptation process [43] | Planned adaptation [42] | Step framework [38] | M-PACE [37] | General adaptation guidance: a guide to adapting evidence-based sexual health curricula [16] |
Cultural adaptation of an EB nursing intervention
[40] |
N
(%) |
| 1. Assess community | + | + | + | + | + | + | + | 7 (54) |
||||||
| 2. Understand the EBI | + | + | + | + | + | + | + | + | + | 9 (69) |
||||
| 3. Select EBI | + | + | + | + | + | + | + | 7 (54) |
||||||
| 4. Consult with experts | + | + | + | + | + | 5 (42) |
||||||||
| 5. Consult with stakeholders | + | + | + | + | + | 5 (38) |
||||||||
| 6. Decide what needs adaptation | + | + | + | + | + | + | + | + | + | + | + | + | 12 (93) |
|
| 7. Adapt the original program | + | + | + | + | + | + | + | + | 8 (62) |
|||||
| 8. Train staff | + | + | + | 3 (25) |
||||||||||
| 9. Test the adapted materials | + | + | + | + | + | + | + | 7 (54) |
||||||
| 10. Implement | + | + | + | + | + | 5 (42) |
||||||||
| 11. Evaluate | + | + | + | + | + | + | + | 7 (54) |
||||||
| 8 | 5 | 8 | 10 | 4 | 3 | 8 | 7 | 4 | 4 | 3 | 3 | 8 | ||
Some adaptation concepts were used across steps by multiple authors. For example, culture was included by Bartholomew et al [7], who recommend judging how well the original delivery, design features, and cultural elements fit the new setting and population when deciding what needs adaptation, and also by Kumpfer and colleagues [43] who state that adapting the original program should involve making cultural adaptations continuously through pilot testing. In total, core elements were discussed by seven of the frameworks [16, 19, 20, 34, 38, 39, 43] in three different steps (steps 2, 8, and 9).
Adaptation insights from the different frameworks
Card, Solomon, and Cunningham [38] recommend that the adaptation process begin by reviewing the materials and making changes in 5 areas including language (comprising the actual language, literacy level, and culture), updating research-based information, ensuring images and examples are up to date and culturally relevant, and updating staff training and evaluation materials based on the adaptation. Lee and colleagues [42] recommend evaluating the adapted program and including instruments to assess effects of the new program components. We categorized resources related to EBI program adaptation into two types from the gray literature search: Toolkits and Guidance documents (Supplementary Table 2).
Citations of adaptation frameworks
We also assessed the number of citations for each adaptation framework. Table 3 provides the citation counts for each framework included in the scoping study as of November 2016. “Finding the balance: Program fidelity and adaptation in substance abuse prevention: A state-of-the-art review” from the Center for Substance Abuse Prevention [34] was the most cited framework, with 216 citations. This was also the oldest framework, published in 2002. The most cited scientific article was Map of the Adaptation Framework [19] with 168 citations. Wingood and DiClemente’s ADAPT-ITT Model [20] was the second most cited study with 105 citations. The Research-based Program Adaptation model [39] was cited 68 times. These frameworks were published in 2006, 2008, and 2006, respectively. This is not surprising since the field of HIV prevention is one of the first to have developed a clearinghouse of HIV research-tested packaged prevention programs (Diffusion of Evidence-based Interventions (DEBI)) and many communities nationally and internationally have adopted or adapted these interventions to new populations and/or settings.
Table 3.
| Citation counts of published adaptation frameworks
| Frameworka | Citations |
|---|---|
| CSAP’s guidelines for balancing program fidelity/ adaptation [34]b | 216 |
| RTIPs guidelines for choosing and adapting programs [33] | n/a |
| Map of adaptation process[19] | 168 |
| Research-based program adaptation [39] | 68 |
| Adapting evidence-based programs to new contexts [41] | 7 |
| ADAPT-ITT [20] | 105 |
| Cultural adaptation process [43] | 69 |
| Planned adaptation [42] | 45 |
| Step framework [38] | 19 |
| Method for program adaptation through community engagement (M-PACE) [37] | 14 |
| General adaptation guidance: a guide to adapting evidence-based sexual health curricula [16] | 4 |
| Cultural adaptation of an EB nursing intervention [40] | 3 |
| Using intervention mapping to adapt EBIs [7] | 1 |
aFrom Scopus and Web of Science (duplicates removed); bfrom Google Scholar, as of November 22, 2016.
DISCUSSION
This study is the first to systematically identify adaptation frameworks or models and contributes to the literature by offering a clearinghouse of frameworks and recommending standard steps used in these frameworks. Several adaptation frameworks exist to guide practitioners and researchers in systematically making adaptations in the topic areas of HIV, STI, pregnancy, and substance abuse prevention. Only Map of the Adaptation Process covered fully program planning and delivery, whereas the majority focused on adaptation as a stand-alone process. Many of the frameworks offer general guidance on adapting EBIs for new populations and settings [7, 16, 19, 20, 34, 39, 41]. However, a few frameworks focus specifically on cultural adaptations [35, 40, 42, 43]. Culture is often defined as comprising of shared common values, practices or beliefs, or learned through social interactions [45,46]. A critical task in program adaptation is the consideration of the culture in many steps (e.g., assessment of the community for the adapted intervention, selecting the program with the best fit or deciding what to needs to be adapted). Resnicow and colleagues suggest examining interventions for cultural modifications in the area of surface structures (presentation such as images and language) versus deep structure (content changes) [47]. These adaptation frameworks help practitioners explore the issue of culture further in program adaptation in terms of definitions (surface/deep structure, mismatches between the original program and the next population/context, local or culturally relevant adaptations to be made in terms of names, lifestyle, and entertainment).
Common adaptation steps
In our review of the various adaptation frameworks, we found eight common adaptation steps. These critical tasks could serve as key core adaptation steps for the practitioners in the field; however, they may not represented the recommended steps without further study or validation from the practice community. However, the range of steps found is interesting to note for practitioners as well. Many of the frameworks not only provide a step-by-step adaptation process, but they also describe a case study of the adaptation [7, 38, 42].
However, there were differences in how some of the adaptation frameworks described some steps. For deciding what needs to be adapted, many frameworks addressed different adaptation concepts. Importantly, some addressed understanding core elements (program fidelity), whereas others discussed considerations of fit and making planned adaptations (i.e., deciding what needs to be adapted). There was some diversity in addressing identifying differences in the population, implementation plan and/or evaluation methods from the original program to the new program. For testing the adapted materials, many focused on pilot testing only the adapted materials with the population of interest or planning groups; however, a few recommended pilot testing the entire program, delivery, and evaluation [19, 20, 33, 43]. That process of piloting a full implementation also would help determine if the recruitment strategies, setting and other program parameters are feasible and acceptable to the new population. Other steps in the frameworks less frequently identified were consulting with experts [19, 20, 33, 34, 37], consulting with stakeholders [19, 34, 37, 41], and training staff [20, 33, 43]. Central to adaptation is maintaining fidelity to the core components, or essential ingredients related to the program theory, when making adaptations [48]. One strategy crucial to this process is consultation with the original developers or experts who can give scientific advice on current epidemiology statistics related to the target health issues, behaviors, the core components, what may be suitable program deviations (e.g., shortening, lengthening, departing) [4], culture/context [20, 42], and other technical advice. However, this may be challenging due to barriers to reaching original developers (e.g., lack of a program website, move from original agency), comfort in working with scientific/technical experts, and time constraints for adaptation.
Finally, few of the frameworks addressed adaptations to implementation guides and protocols based on decisions made in adapting the program itself and sustainability of the program. And, few recommended training of implementers that may entail recruiters, facilitators, evaluators, and data staff [20]. This may be due to the presence of implementation manuals/facilitator’s guides or issues related to time to train due to desire to implement programs quickly in the community. However, some researchers have identified training on an EBI as a critical step to quality adoption [49,50] or implementation of an intervention [10]. Of note, there were few frameworks from international settings outside of the USA; only one was reported here [40].
Implications for future research
Understanding of EBIs adaptation is relatively nascent in the field of implementation science. It is unknown whether applying one of the identified frameworks is useful and effective. In addition, there is much to be learned about adaptations of EBIs in terms of their process, and outcomes (health and implementation outcomes [51]) based on the current literature. Our findings suggest some recommendations for future research. It is important that EBI adaptations be documented so that their collective results can be evaluated and their impact be better understood. Research could explore the effectiveness of EBIs that have applied any of these adaptation frameworks on participant outcomes (e.g., perceived relevance, satisfaction) and intervention outcomes. Furthermore, qualitative research conducted within evaluations could describe key reasons, types of changes [52], adaptation processes, other taxonomies related to adaptation [4, 13, 14], and outcomes of evaluation to describe further aspects of adaptation outlined in these frameworks. Finally, the development for reporting guidelines for program adaptation will offer a standardized method of describing adaptations in a consistent manner to allow for further comparisons and research on this area.
This study has several limitations. First, our search strategies may have failed to identify all relevant adaptation frameworks or models. However, we incorporated gray and published literature in addition to different databases searches. We also limited our searches to public health or community settings and did not focus on policies, clinical care, or interventions from other disciplines. In addition, we did not focus our search on cultural adaptations specifically, and there are theories and frameworks focused on modifications for cultural reasons (e.g., Cultural Accommodation Model). A book entitled Cultural Adaptations present some frameworks for cultural adaptations for evidence-based treatments [53]. Finally, the value and utility of these frameworks are not known. We know that there is general awareness of three of these frameworks from the citation counts, but their general helpfulness to the field from the practitioners’ perspective has not been researched.
This scoping review makes a contribution by summarizing common steps adaptation frameworks that are essential in the translation of evidence-based interventions into local communities (T3) and synthesizing their historical roots. These findings can help practitioners consider employing frameworks for adapting an EBI as an option even if at first, it was considered irrelevant due to differences in program audience and/or context [42] and guide them in a systematic adaptation. Our results highlight 13 frameworks that could provide guidance to public health practitioners, and we identified eight common steps across the frameworks, described with varying levels of specificity. Future research can assess the extent to which researchers and practitioners apply these adaptation framework tasks or steps in their adaptation of EBIs and the extent to which adapted interventions have positive impacts on health outcomes and its acceptability and satisfaction for the population of interest.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Translational Behavioral Medicine online.
Compliance with Ethical Standards
Conflicts of Interest: The authors declare that they have no competing interests.
Ethical Approval: This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent: This study was a secondary analyses of published literature and did not involve human participants and informed consent was not needed.
Acknowledgments
These findings have not been published before and are not being submitted for publication elsewhere. Part of these data, including the figure of scoping study adaptation frameworks and Table 2, have been reported in a short presentation at the NIH Science of Dissemination and Implementation Research conference in December 2016. The authors have all of the primary data and we agree to allow Translational Behavioral Medicine staff’s review of the data, if requested. R01CA163526, Increasing Reach and Implementation of Evidence Based Programs for Cancer Control (Mullen, Fernandez, Multi-PIs), National Cancer Institute. U48 DP005017-01S8, Cancer Prevention and Control Research Network, Centers for Disease Control and Prevention’s Prevention Research Centers Program and the National Cancer Institute.
References
- 1. Carvalho ML, Honeycutt S, Escoffery C, Glanz K, Sabbs D, Kegler MC. Balancing fidelity and adaptation: implementing evidence-based chronic disease prevention programs. j Public Health Manag Pract. 2013; 19(4): 348–356. [DOI] [PubMed] [Google Scholar]
- 2. Castro FG, Barrera M Jr, Martinez CR Jr. The cultural adaptation of prevention interventions: resolving tensions between fidelity and fit. Prev Sci. 2004; 5(1): 41–45. [DOI] [PubMed] [Google Scholar]
- 3. Galbraith JS, Stanton B, Boekeloo B et al. Exploring implementation and fidelity of evidence-based behavioral interventions for HIV prevention: lessons learned from the focus on kids diffusion case study. Health Educ Behav. 2009; 36(3): 532–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Stirman S, Kimberly J, Cook N, Calloway A, Castro F, Charns M. The sustainability of new programs and innovations: a review of the empirical literature and recommendations for future research. Implement Sci. 2012; 7(1): 1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brown CH, Curran G, Palinkas LA et al. An Overview of Research and Evaluation Designs for Dissemination and Implementation. Annu Rev Public Health. 2017; 38: 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Westfall JM, Mold J, Fagnan L. Practice-based research–“Blue Highways” on the NIH roadmap. Jama. 2007; 297(4): 403–406. [DOI] [PubMed] [Google Scholar]
- 7. Bartholomew Eldredge L, Highfield L, Hartman M, Mullen P, Leerlooijer J, Fernandez M. Using Intervention Mapping to Adapt Evidence-Based Interventions. In: Bartholomew Eldredge L, Markham C, Ruiter R, Fernandez M, Kok G, Parcel G, eds. Planning health promotion programs: an intervention mapping approach. San Francisco, CA: Jossey-Bass; 2016: 597–649. [Google Scholar]
- 8. Krivitsky LN, Parker SJ, Pal A, Meckler L, Shengelia R, Reid MC. A systematic review of health promotion and disease prevention program adaptations: how are programs adapted? In: Wethington E, Dunifon RE, eds. Research for the public good: Applying the methods of translational research to improve human health and well-being. Washington, DC: American Psychological Association; 2012: 73–99. [Google Scholar]
- 9. Rabin BA, Brownson RC, Haire-Joshu D, Kreuter MW, Weaver NL. A glossary for dissemination and implementation research in health. j Public Health Manag Pract. 2008; 14(2): 117–123. [DOI] [PubMed] [Google Scholar]
- 10. Durlak JA, DuPre EP. Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am j Community Psychol. 2008; 41(3-4): 327–350. [DOI] [PubMed] [Google Scholar]
- 11. Botvin GJ, Baker E, Dusenbury L, Botvin EM, Diaz T. Long-term follow-up results of a randomized drug abuse prevention trial in a white middle-class population. Jama. 1995; 273(14): 1106–1112. [PubMed] [Google Scholar]
- 12. Domitrovich CE, Greenberg MT. The study of implementation: Current findings from effective programs that prevent mental disorders in school-aged children. J Educ Psychol Consult. 2000; 11(2): 193–221. [Google Scholar]
- 13. Moore JE, Bumbarger BK, Cooper BR. Examining adaptations of evidence-based programs in natural contexts. j Prim Prev. 2013; 34(3): 147–161. [DOI] [PubMed] [Google Scholar]
- 14. Hill LG, Maucione K, Hood BK. A focused approach to assessing program fidelity. Prev Sci. 2007; 8(1): 25–34. [DOI] [PubMed] [Google Scholar]
- 15. Chambers DA, Norton WE. The Adaptome: Advancing the Science of Intervention Adaptation. Am j Prev Med. 2016; 51(4 suppl 2): S124–S131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rolleri LA, Fuller TR, Firpo-Triplett R, Lesesne CA, Moore C, Leeks KD. Adaptation Guidance for Evidence-Based Teen Pregnancy and STI/HIV Prevention Curricula: From Development to Practice. Am j Sex Educ. 2014; 9(2): 135–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. van Achterberg T, Schoonhoven L, Grol R. Nursing implementation science: how evidence-based nursing requires evidence-based implementation. j Nurs Scholarsh. 2008; 40(4): 302–310. [DOI] [PubMed] [Google Scholar]
- 18. Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: models for dissemination and implementation research. Am j Prev Med. 2012; 43(3): 337–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. McKleroy VS, Galbraith JS, Cummings B et al. ; ADAPT Team Adapting evidence-based behavioral interventions for new settings and target populations. aids Educ Prev. 2006; 18(4 suppl A): 59–73. [DOI] [PubMed] [Google Scholar]
- 20. Wingood GM, DiClemente RJ. The ADAPT-ITT model: a novel method of adapting evidence-based HIV Interventions. j Acquir Immune Defic Syndr. 2008;47(suppl 1):S40–S46. [DOI] [PubMed] [Google Scholar]
- 21. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009; 4(1): 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mitchell SA, Fisher CA, Hastings CE, Silverman LB, Wallen GR. A thematic analysis of theoretical models for translational science in nursing: mapping the field. Nurs Outlook. 2010; 58(6): 287–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005; 8(1): 19–32. [Google Scholar]
- 24. Davis K, Drey N, Gould D. What are scoping studies? A review of the nursing literature. Int j Nurs Stud. 2009; 46(10): 1386–1400. [DOI] [PubMed] [Google Scholar]
- 25. Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010; 5(1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hart C. Doing a literature search: a comprehensive guide for the social sciences. Sage: Thousand Oaks, CA; 2001. [Google Scholar]
- 27. Benzies KM, Premji S, Hayden KA, Serrett K. State-of-the-evidence reviews: advantages and challenges of including gray literature. Worldviews Evid Based Nurs. 2006; 3(2): 55–61. [DOI] [PubMed] [Google Scholar]
- 28.Escoffery E, Liang S, Lebow-Skelley E et al. Systematic review of adaptations of public health evidence-based interventions, in progress. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tortolero SR, Markham CM, Parcel GS et al. Using intervention mapping to adapt an effective HIV, sexually transmitted disease, and pregnancy prevention program for high-risk minority youth. Health Promot Pract. 2005; 6(3): 286–298. [DOI] [PubMed] [Google Scholar]
- 30. Highfield L, Hartman MA, Mullen PD, Rodriguez SA, Fernandez ME, Bartholomew LK. Intervention Mapping to Adapt Evidence-Based Interventions for Use in Practice: Increasing Mammography among African American Women. Biomed Res Int. 2015; 2015: 160103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ribisl KM, Fernandez ME, Friedman DB et al. Impact of the Cancer Prevention and Control Research Network: Accelerating the Translation of Research Into Practice. Am j Prev Med. 2017; 52(3S3): S233–S240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Fernández ME, Melvin CL, Leeman J et al. The cancer prevention and control research network: An interactive systems approach to advancing cancer control implementation research and practice. Cancer Epidemiol Biomarkers Prev. 2014; 23(11): 2512–2521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. National Cancer Institute. Guidelines for choosing and adapting programs (Research-tested Intervention Programs) Available at http://rtips.cancer.gov/rtips/reference/adaptation_guidelines.pdf. Accessibility verified June 6, 2017.
- 34. Backer T. Finding the balance: Program fidelity and adaptation in substance abuse prevention: A state-of-the-art review. Rockville, MD: Center for Substance Abuse Prevention. Substance Abuse and Mental Health Services Administration; 2002. [Google Scholar]
- 35. Bartholomew LK, Parcel GS, Kok G. Intervention mapping: a process for developing theory- and evidence-based health education programs. Health Educ Behav. 1998; 25(5): 545–563. [DOI] [PubMed] [Google Scholar]
- 36. Bartholomew LK, Parcel G, Kok G, Gottlieb N.. Intervention mapping: designing theory-and evidence-based health promotion programs. Mountain View, CA: Mayfield; 2001. [Google Scholar]
- 37. Chen EK, Reid MC, Parker SJ, Pillemer K. Tailoring evidence-based interventions for new populations: a method for program adaptation through community engagement. Eval Health Prof. 2013; 36(1): 73–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Card JJ, Solomon J, Cunningham SD. How to adapt effective programs for use in new contexts. Health Promot Pract. 2011; 12(1): 25–35. [DOI] [PubMed] [Google Scholar]
- 39. Solomon J, Card JJ, Malow RM. Adapting efficacious interventions: advancing translational research in HIV prevention. Eval Health Prof. 2006; 29(2): 162–194. [DOI] [PubMed] [Google Scholar]
- 40. Williams AB, Wang H, Burgess J, Li X, Danvers K. Cultural adaptation of an evidence-based nursing intervention to improve medication adherence among people living with HIV/AIDS (PLWHA) in China. Int j Nurs Stud. 2013; 50(4): 487–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Smith E, Caldwell L. Adapting evidence-based programs to new contexts: what needs to be changed?j Rural Health. 2007;23(suppl):37–41. [DOI] [PubMed] [Google Scholar]
- 42. Lee SJ, Altschul I, Mowbray CT. Using planned adaptation to implement evidence-based programs with new populations. Am j Community Psychol. 2008; 41(3-4): 290–303. [DOI] [PubMed] [Google Scholar]
- 43. Kumpfer KL, Pinyuchon M, Teixeira de Melo A, Whiteside HO. Cultural adaptation process for international dissemination of the strengthening families program. Eval Health Prof. 2008; 31(2): 226–239. [DOI] [PubMed] [Google Scholar]
- 44. Wainberg ML, Alfredo González M, McKinnon K et al. Targeted ethnography as a critical step to inform cultural adaptations of HIV prevention interventions for adults with severe mental illness. Soc Sci Med. 2007; 65(2): 296–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Scheer J. Culture and disability: An anthropological point of view. San Francisco, CA: Jossey-Bass; 1994. [Google Scholar]
- 46. Wilson BD, Miller RL. Examining strategies for culturally grounded HIV prevention: a review. aids Educ Prev. 2003; 15(2): 184–202. [DOI] [PubMed] [Google Scholar]
- 47. Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn Dis. 1999; 9(1): 10–21. [PubMed] [Google Scholar]
- 48. Eke AN, Neumann MS, Wilkes AL, Jones PL. Preparing effective behavioral interventions to be used by prevention providers: the role of researchers during HIV Prevention Research Trials. aids Educ Prev. 2006; 18(4 suppl A): 44–58. [DOI] [PubMed] [Google Scholar]
- 49. Sussman S, Valente TW, Rohrbach LA, Skara S, Pentz MA. Translation in the health professions: converting science into action. Eval Health Prof. 2006; 29(1): 7–32. [DOI] [PubMed] [Google Scholar]
- 50. Elliott DS, Mihalic S. Issues in disseminating and replicating effective prevention programs. Prev Sci. 2004; 5(1): 47–53. [DOI] [PubMed] [Google Scholar]
- 51. Proctor E, Silmere H, Raghavan R et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011; 38(2): 65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Cooper BR, Shrestha G, Hyman L, Hill L. Adaptations in a Community-Based Family Intervention: Replication of Two Coding Schemes. j Prim Prev. 2016; 37(1): 33–52. [DOI] [PubMed] [Google Scholar]
- 53. Bernal G, Domemnech Rodriguez MM.. Cultural adaptations: Tools for evidence-basd practice with diverse populations. Washingon, DC: American Psyconolgic Association; 2012. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.