Abstract
Background
The median age of single homeless adults is approximately 50 years. Older homeless adults have poor social support and experience a high prevalence of chronic disease, depression, and substance use disorders. Access to mobile phones and the internet could help lower the barriers to social support, social services, and medical care; however, little is known about access to and use of these by older homeless adults.
Objective
This study aimed to describe the access to and use of mobile phones, computers, and internet among a cohort of 350 homeless adults over the age of 50 years.
Methods
We recruited 350 participants who were homeless and older than 50 years in Oakland, California. We interviewed participants at 6-month intervals about their health status, residential history, social support, substance use, depressive symptomology, and activities of daily living (ADLs) using validated tools. We performed clinical assessments of cognitive function. During the 6-month follow-up interview, study staff administered questions about internet and mobile technology use. We assessed participants’ comfort with and use of multiple functions associated with these technologies.
Results
Of the 343 participants alive at the 6-month follow-up, 87.5% (300/343) completed the mobile phone and internet questionnaire. The median age of participants was 57.5 years (interquartile range 54-61). Of these, 74.7% (224/300) were male, and 81.0% (243/300) were black. Approximately one-fourth (24.3%, 73/300) of the participants had cognitive impairment and slightly over one-third (33.6%, 100/300) had impairments in executive function. Most (72.3%, 217/300) participants currently owned or had access to a mobile phone. Of those, most had feature phones, rather than smartphones (89, 32.1%), and did not hold annual contracts (261, 94.2%). Just over half (164, 55%) had ever accessed the internet. Participants used phones and internet to communicate with medical personnel (179, 64.6%), search for housing and employment (85, 30.7%), and to contact their families (228, 82.3%). Those who regained housing were significantly more likely to have mobile phone access (adjusted odds ratio [AOR] 3.81, 95% CI 1.77-8.21). Those with ADL (AOR 0.53, 95% CI 0.31-0.92) and executive function impairment (AOR 0.49; 95% CI 0.28-0.86) were significantly less likely to have mobile phones. Moderate to high risk amphetamine use was associated with reduced access to mobile phones (AOR 0.27, 95% CI 0.10-0.72).
Conclusions
Older homeless adults could benefit from portable internet and phone access. However, participants had a lower prevalence of smartphone and internet access than adults aged over 65 years in the general public or low-income adults. Participants faced barriers to mobile phone and internet use, including financial barriers and functional and cognitive impairments. Expanding access to these basic technologies could result in improved outcomes.
Keywords: homelessness, internet, cell phone, smartphone, aged and middle aged
Introduction
Background
In the past 25 years, the median age of individuals experiencing homelessness in the United States has risen [1]. Approximately half of the single adult homeless population is aged 50 years and older [1]. Adults with a current or recent experience of homelessness (homeless-experienced) have a high prevalence of chronic disease, functional and cognitive impairment, and substance use [2-4]. Homeless-experienced older adults’ competing needs for food and shelter, lack of stable mailing address, and limited social support complicate the receipt of longitudinal health care needed to manage these conditions [2,5].
Appropriate longitudinal health care relies on intervisit communication [6-9]. Mobile phones, email, and patient portals increase the consistency of intervisit communication between patients and clinicians and improve self-management of chronic diseases in the general population [5,10-14]. None of these requires a permanent address, and therefore, they could be used by people experiencing homelessness [11,15,16].
In addition to improving health care communication, these technologies have other potential health benefits for homeless individuals, including decreasing social isolation, connecting to social services, and identifying housing resources [17-21]. However, little is known about how older homeless-experienced adults use mobile and internet technologies.
Low-income housed individuals report barriers to technology use, such as lack of high-speed broadband access, limited English proficiency, and limited digital and linguistic literacy [14,22,23]. Low-income populations rely on smartphones, rather than computers, for internet access [14]. Older adults in the general population use technology at lower rates than younger adults [24,25]. Cost; low digital literacy; and cognitive, executive, and sensory impairments may limit use in this population [24-27].
Objectives
The limited literature about mobile phone and internet access among homeless populations has focused on younger populations [18,28]. Little is known about the use of mobile phones and internet by older adults who experience homelessness. In a population-based cohort of 350 homeless- experienced adults aged 50 years and older, we examined the prevalence of mobile phone (smartphones and feature phones), computer and internet access, purposes of use, types of service contracts and charging locations, and the factors associated with access to mobile phones.
Methods
Participants and Setting
The overall goal of the Health Outcomes of People Experiencing Homelessness in Older Middle Age (HOPE HOME) study is, among older homeless adults, to describe the life course events and level of geriatric conditions and to explore the association between life course events and geriatric conditions with acute health service utilization. Between July 2013 and June 2014, we used population-based sampling to recruit 350 homeless individuals aged 50 years or older in Oakland, California [29]. We recruited from homeless encampments, all overnight homeless shelters that served single adults over the age of 25 years (n=5), one recycling center close to homeless service agencies, and all free and low-cost meal programs serving at least 3 prepared meals a week (n=5). We constructed our sampling frame to approximate the source population; we randomly selected potential participants at each recruitment site [30,31].
After an initial screening for eligibility, we invited individuals to complete a detailed eligibility interview within 1 week. Participants were eligible for the study if they were English-speaking, aged 50 years or older, defined as homeless by the Homeless Emergency Assistance and Rapid Transition to Housing Act (HEARTH), [32] and able to give written informed consent as determined by a teach-back method [33]. We gave participants gift certificates worth US $25 for completing the screening and baseline interviews and US $20 for each semiannual follow-up visit. We gave participants a US $5 gift certificate for each monthly check-in between scheduled visits. The majority of study activities took place at St Mary’s Center, a nonprofit community-based organization serving low-income older adults. The institutional review board of the University of California, San Francisco approved the study.
Trained study staff administered structured baseline interviews and follow-up interviews at 6-month intervals. At the initial interview, study staff collected extensive contact information on participants, including a phone number, if the participant had one. Participants checked in monthly between study visits, by phone or in person, to enhance the follow-up process. During structured interviews at baseline and follow-up, participants reported information about housing history, demographic information, health history, health care utilization, drug and alcohol use, mental health, and social support, and completed assessments of functional and cognitive impairment. Participants remained in the study independent of their housing status at the time of follow-up. During the 6-month follow-up interview or, if missed, the next attended interview, study staff administered a module centered on the use of internet and mobile technology, as shown in Figure 1.
Figure 1.
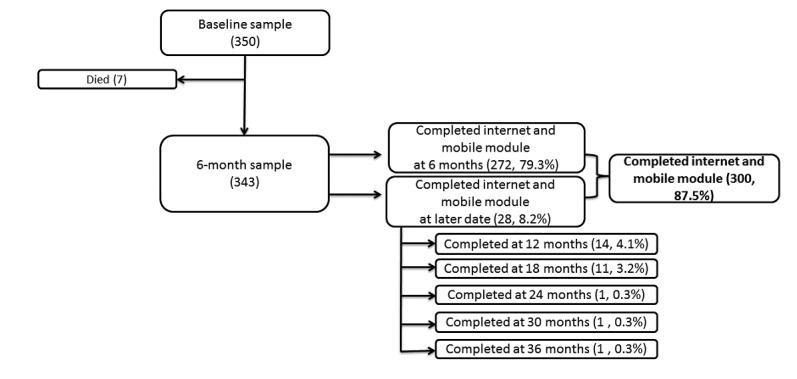
Recruitment flowchart.
In this analysis, we use all time-varying variables at the interview at which the participant completed the internet and mobile technology module. To assess differential loss to follow-up, we assessed whether participants who were eligible for, but did not complete, a mobile phone and internet interview were less likely to report having a phone number at enrollment than those who completed the interview.
Measures
Demographics
Demographic variables included age, sex, and race or ethnicity (black, white, Hispanic or Latino, Asian, other or mixed). We dichotomized participants as having completed a high school or General Educational Development (GED) degree versus having completed less than a high school equivalent degree. Participants reported their total income in the past 30 days, categorized as US $0-$150, $151-$700, $701-$1150, and over $1150. To assess health literacy, we used a validated one-item health literacy screen “How confident are you filling out medical forms by yourself?” (Not at all, A little bit, Somewhat, Quite a bit, Extremely) [34]. On the basis of validation studies within low-income populations, we considered those who reported being somewhat confident or less as having limited health literacy [35,36].
Focal Variables
Focal Independent Variable: Housing Status
At each interview, we determined whether participants still met the HEARTH criteria for homelessness, categorizing the participants’ current living situation as homeless, housed, or in an institution. As participants were either currently homeless, or had recently been homeless, and in keeping with the transient nature of homelessness, we described the sample as homeless-experienced [14].
Mobile Phone Access, Use, and Service Type
Participants reported if they had ever used a mobile phone (feature, smartphone, or both). We adapted Pew survey items based on prior research on information technologies among homeless populations [37,38]. We defined feature phones as phones allowing users to “make and receive phone calls and text messages, take pictures and perform basic Web browsing.” We defined smartphones as “a phone with a larger screen that allows functions like a mini computer and lets you check your email and use a number of different applications.” We asked participants if they had ever used a mobile phone; if yes, we asked whether they had current access to a mobile phone or had access in the past. We defined having access to a mobile phone as owning a mobile phone, borrowing one long term, being able to borrow one if needed, or being able to find one in an emergency. Participants reported whether they had current access to mobile phones, past access, or never had access. Our focal dependent variable was current access to a mobile phone.
We asked participants to report what type of mobile service they used (contract, month-to-month, prepaid, free phone, or other). If participants reported ever having access to a mobile phone, we asked them to report what they used it for (making phone calls, receiving phone calls, voicemail, or text messages). If participants had ever used a smartphone, we asked them if they used it to check and send email, access social networking sites, look up information on the internet, look up bus schedules, or get directions. We asked participants to report whether they used a mobile phone to contact others, and if so, whom they contacted. We asked participants if they had ever had their mobile phones stolen. If participants reported having had their phones stolen, we asked them how many times. We asked participants if they had ever lost a mobile phone. If they reported losing a phone, we asked how many times.
Ease of Use and Charging Locations
We asked participants to report, on a 5-point Likert scale (1=very easy to 6=I don’t know how to do this), how comfortable they were with performing the following actions on a mobile phone: making a call, answering a call, contacting 911 or emergency medical services, checking voicemail, and using text messaging. Participants rated the difficulty of using basic components of their phone, such as the buttons and screen. We asked participants where they charged their phones. To assess barriers to phone charging, we asked participants whether there were times they had not had mobile phone service because they did not have a place to charge their phones.
Computer, Internet, and Email Use
We asked participants if they had ever used a computer. If so, we asked if they had ever used the internet. We asked those who had ever used the internet if they had done so in the past 30 days. Among those with recent use, we asked where they used the internet and what they used the internet for. Potential venues included the following: on a mobile phone, in a public or university library, drop-in center or shelter, friend or relative’s house, internet café, coffee shop or restaurant, social service agency, motel or hotel lobby, church, and others. Uses included reading or sending email; getting news online; watching a video, downloading a music file or playing a game; browsing the internet for fun; searching for a fact or to answer a question; looking for information about a shelter or place to live, a hobby or interest, health or medical information, or about a job; checking social networking sites; doing research for school, training, or education; sending instant messages; refilling a prescription; and looking for a sex partner. For each of these response categories, we asked participants to note all those that were applicable.
We asked participants whether they had ever used email and if they had a current email account. We asked what they used their email for: staying in touch with family or friends, job searches, housing searches, staying in touch with a case manager or social worker, staying in touch with a health care provider, and other. We asked participants to note all that were applicable.
Descriptive Variables
Health History
We asked participants to rate their health status, dichotomized as poor or fair versus good, very good, or excellent [39]. On the basis of the National Health and Nutrition Examination Survey, we asked participants to report whether a health care provider had ever told them they had any of the 10 chronic conditions [3,40]. We created a composite variable for the total number of chronic conditions, categorized as none, 1, 2, or 3 or more. We asked participants if they had difficulty performing any activities of daily living (ADL): dressing, bathing or showering, eating, getting in or out of bed, or using the toilet [41]. We dichotomized participants as having any difficulty versus no ADL difficulty.
We administered the Modified Mini-Mental (3MS) Examination to assess global cognitive impairment [42] and the Trail Making Test B (Trails B) [43] to assess executive function. Comparing scores with age- and education-adjusted reference values, we categorized scores below the seventh percentile on the 3MS as cognitive impairment [44]. We classified the participants’ performance as “unable to complete” if their time to complete the Trails B lasted longer than 5 min. We interpreted scores with the demographically adjusted (age, gender, and race or ethnicity) norms for the Halstead-Reitan Neuropsychological Test Battery, which uses the Halstead-Reitan Battery (HRB) Norms scoring program [45].
Mental Health, Substance Use, and Social Support
We assessed depressive symptoms using the Center for Epidemiologic Studies Depression Scale (CES-D) [46]. On the basis of past studies with older adults, we classified scores of ≥22 as indicative of major depressive symptoms [47,48]. We considered participants who reported drinking ≥6 drinks on 1 occasion every month as heavy drinkers [49]. Using the World Health Organization’s Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) with a lengthened time frame of the past 6 months, we assessed illicit drug use for cocaine, opioids, or amphetamines [50]. We classified scores of ≥4 for any illicit drug as moderate to high risk use of an illicit substance. To assess social support, we asked participants how many close friends or relatives they had in whom they could confide (0, 1-5, or 6 or more) [51,52].
Analysis
We performed a descriptive analysis to assess the prevalence of mobile phone, computer, internet, and email use and the purposes of usage. To identify facilitators to mobile phone and internet use among older homeless adults, we assessed the ease of use, types of service, and charging locations. We assessed bivariable associations between current mobile phone use and a priori independent variables using logistic regression. We built our multivariable model by including variables with bivariable type 3 P values <.20, and reduced the model using backwards elimination retaining variables with P values <.05 for our final multivariable model. We implemented our models in SAS 9.4 (SAS Institute, Cary, NC).
Results
Follow-Up
Of the 350 individuals enrolled in the study, 7 died before the 6-month follow-up. Of the 343 participants alive by the 6-month follow-up, 300 (87.5% (300/343) completed the module on internet and mobile phone use. Of these, 79.3% (272/343) completed the mobile phone and internet module at 6 months and 8.2% (28/343) completed the module at a later date. (Figure 1). One-third (32.6%, 14/43) of those who were eligible but did not complete a mobile phone interview reported having a phone number at enrollment, compared with 68.0% (204/300) of those who completed the interview (P<.001).
Demographics
The median age of participants was 57.5 years (interquartile range 54-61). Most participants (74.7%) were male and black (81.0%; see Table 1). Approximately one-fourth had less than a high school or equivalent (eg, GED) education (24.7%). Most participants (74.3%) remained homeless at their follow-up interview. Approximately three-fourths (74.9%) reported having at least one confidant. Over ten percent (10.3%) reported heavy drinking, and approximately one-third met the criteria for moderate- to high-risk cocaine use (29.0%).
Table 1.
Participant characteristics of mobile phone use.
| Descriptive, health, and health-related variables | Total (N=300) | Currently own or have access to a mobile phone (N=217) | Owned or have access to a mobile phone (N=60) | Never owned or had access to a mobile phone in the past (N=23) | |
| Age in years, median (interquartile range) | 57.5 (54.0-61.0) | 57.0 (54.0-61.0) | 58.0 (54.0-61.0) | 58.0 (55.0-65.0) | |
| Male, n (%) | 224 (74.7) | 161 (74.2) | 44 (73) | 19 (83) | |
| Black, n (%) | 243 (81.0) | 183 (84.3) | 45 (75) | 15 (65) | |
| Completed less than high school degreea, n (%) | 74 (24.5) | 57 (26.2) | 10 (177) | 7 (30) | |
| Total income in past 30 days, n (%) | |||||
|
|
US $0-150 | 62 (20.6) | 41 (18.8) | 13 (22) | 8 (35) |
|
|
US $151-700 | 76 (25.3) | 55 (25.3) | 19 (32) | 2 (9) |
|
|
US $701-1150 | 128 (42.7) | 92 (42.3) | 24 (40) | 12 (52) |
|
|
More than US $1150 | 34 (11.3) | 29 (13.3) | 4 (7) | 1 (4) |
| Homeless at follow-up interviewb | 223 (74.3) | 149 (68.7) | 55 (92) | 19 (83) | |
| Social support, n (%) | 224 (74.9) | 169 (77.9) | 40 (67) | 15 (68) | |
| Number of confidantsc | |||||
|
|
None | 76 (25.3) | 49 (22.5) | 20 (33) | 7 (32) |
|
|
1 | 78 (26.0) | 55 (25.3) | 17 (28) | 6 (27) |
|
|
2 | 46 (15.3) | 33 (15.2) | 9 (15) | 4 (18) |
|
|
3 or more | 99 (33.0) | 80 (36.8) | 14 (23) | 5 (23) |
| Fair or poor health, n (%) | 166 (56.1) | 113 (52.8) | 39 (66) | 14 (61) | |
| Number of chronic conditions, n (%) | |||||
|
|
None | 76 (25.3) | 58 (26.7) | 13 (22) | 5 (22) |
|
|
1 | 103 (34.3) | 76 (35.0) | 18 (30) | 9 (39) |
|
|
2 | 88 (29.3) | 61 (28.1) | 19 (32) | 8 (35) |
|
|
3 or more | 33 (11.0) | 22 (10.1) | 10 (17) | 1 (4) |
| Activities of daily living impairment, n (%) | 128 (42.7) | 85 (39.1) | 31 (52) | 12 (52) | |
| Cognitive impairment (3MS, baseline)d, n (%) | 73 (24.3) | 46 (21.1) | 17 (28) | 10 (44) | |
| Executive function impairment (Trails B)e, n (%) | 100 (33.6) | 65 (29.9) | 27 (45) | 8 (35) | |
| Moderate-to-severe depressive symptomsf, n (%) | 94 (31.3) | 63 (29.0) | 22 (37) | 9 (43) | |
| Heavy drinkingg, n (%) | 31 (10.3) | 16 (7.3) | 11 (4) | 3 (13) | |
| Moderate-to-high risk amphetamines useh, n (%) | 19 (6.3) | 8 (3.6) | 9 (15) | 2 (9) | |
| Moderate-to-high risk cocaine usei, n (%) | 87 (29.0) | 59 (27.1) | 20 (33) | 8 (35) | |
| Moderate-to-high risk opioids usej, n (%) | 19 (6.3) | 12 (5.5) | 5 (8) | 2 (9) | |
aCompletion of high school degree included General Education Development (GED).
bHomeless as defined by the Homeless Emergency Assistance and Rapid Transition to Housing (HEARTH) Act.
cConfidant defined as “a close friend or family member in whom you can confide or talk about yourself and your problems.”
dModified Mini-Mental State Examination; less than seventh percentile based on Z-scores used.
eTrail Making Test; more than 5-min completion time on Trails B.
fScore of ≥22 on the Center for Epidemiologic Studies Depression Scale (CES-D).
gDrinking ≥6 drinks on one occasion every month.
hScore of ≥4 for any amphetamines using the World Health Organization’s Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST).
iScore of ≥4 for any cocaine using the World Health Organization’s Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST).
jScore of ≥4 for any opioids using the World Health Organization’s Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST).
Approximately one-third (31.8%) met the criteria for major depressive symptoms. Over half (56.1%) described their health as fair to poor and approximately three-fourths had at least one chronic condition (74.7%). Over 40% had ADL impairment (42.7%), approximately one-fourth had cognitive impairment (24.3%), and one-third had problems in executive functioning (33.6%).
Mobile Phone Access, Use, and Service Type
Almost all participants currently owned or had access to a mobile phone (72.3%) or had owned or had access to a mobile phone in the past (20.0%; see Table 2). Among those with current mobile phone access, 204 owned their phones, 4 borrowed phones for long term, 6 borrowed phones for short term, and 3 could access a mobile phone in an emergency. Among participants who currently or had ever had a phone (n=277), two-thirds had basic mobile phones, as opposed to smartphones.
Table 2.
Mobile phone use.
| Mobile phone use | Total (N=277), n (%) | Currently own or have access to a mobile phone (N=217), n (%) | Owned or had access to a mobile phone in the past (N=60), n (%) | P value | |
| Type of phone use or used | |||||
|
|
Feature phone | 186 (67.1) | 143 (65.9) | 43 (72) | .57 |
|
|
Smartphone | 89 (32.1) | 72 (33.1) | 17 (28) | —a |
|
|
Both | 2 (0.7) | 2 (0.9) | 0 (0) | — |
| Type of service | |||||
|
|
Contract | 16 (5.7) | 13 (5.9) | 3 (5) | .10 |
|
|
Month-to-month | 167 (60.3) | 130 (59.9) | 37 (62) | — |
|
|
Free phone | 52 (18.7) | 46 (21.1) | 6 (10) | — |
|
|
Prepaid | 26 (9.3) | 16 (7.3) | 10 (17) | — |
|
|
Other or don’t know | 16 (5.7) | 12 (5.5) | 4 (7) | — |
| Mobile phone features used | |||||
|
|
Make and receive phone calls | 277 (100.0) | 217 (100.0) | 60 (100) | >.99 |
|
|
Check and receive voicemails | 195 (70.4) | 162 (74.7) | 33 (55) | .003 |
|
|
Send and receive text messages | 172 (62.9) | 145 (66.8) | 27 (45) | .002 |
| Smartphone features used | |||||
|
|
Look up information on the internet | 66 (23.8) | 55 (25.3) | 11 (65) | .42 |
|
|
Check and send email | 53 (19.1) | 46 (21.1) | 7 (41) | .11 |
|
|
Get directions | 49 (17.6) | 41 (18.8) | 8 (47) | .53 |
|
|
Look up bus route or schedule | 37 (13.3) | 34 (15.6) | 3 (18) | .03 |
|
|
Check social networking sites | 24 (8.6) | 23 (10.5) | 1 (6) | .03 |
| Uses of phone to contact others | |||||
|
|
Use or used phone to contact relatives | 228 (82.3) | 178 (82.0) | 50 (83) | .81 |
|
|
Use or used phone to contact friends | 215 (77.6) | 171 (78.8) | 44 (73) | .37 |
|
|
Use or used phone to contact medical personnel | 179 (64.6) | 150 (69.1) | 29 (48) | .003 |
|
|
Use or used phone to contact social service agencies | 137 (49.5) | 115 (53.0) | 22 (37) | .03 |
|
|
Use or used phone to contact shelters or other housing providers | 85 (30.6) | 71 (32.7) | 14 (23) | .16 |
|
|
Use or used phone to contact (potential) employer | 64 (23.1) | 51 (23.5) | 13 (22) | .77 |
|
|
Use or used phone to contact (potential) landlord | 54 (19.4) | 44 (20.2) | 10 (17) | .53 |
|
|
Use or used phone to contact emergency services | 29 (10.4) | 25 (11.5) | 4 (7) | .28 |
| Ever had phone stolen | 146 (53.1) | 106 (49.3) | 40 (67) | .02 | |
| Number of times phone stolen |
|
|
|
|
|
|
|
0 | 129 (47.4) | 109 (51.2) | 20 (344) | .06 |
|
|
1-2 | 109 (40.1) | 80 (36.8) | 29 (49) | .06 |
|
|
≥3 | 34 (12.2) | 24 (11.0) | 10 (17) | .06 |
| Ever lost phone | 145 (52.9) | 113 (52.6) | 32 (54) | .81 | |
| Number of times lost phone | |||||
|
|
0 | 129 (47.4) | 102 (47.9) | 27 (46) | .30 |
|
|
1-2 | 106 (39.0) | 79 (36.4) | 27 (46) | .30 |
|
|
≥3 | 37 (12.2) | 32 (14.7) | 5 (9) | .30 |
aNot applicable.
More than three-fourths of participants with current or prior access to a phone (n=277) reported using phones to contact relatives (82.3%) and friends (77.6%; see Table 2). A majority of participants used phones to contact medical personnel (66.6%), and nearly half of them used phones to contact social service agencies (49.5%). Almost one-third used phones to contact shelters or other housing providers (30.7%). Approximately one-fourth used them to contact potential employers (23.1%). A smaller proportion used phones to contact potential landlords (19.5%; see Table 2). Over half reported having had their mobile phones stolen (53.1%) or lost (52.9%).
Ease of Use and Charging Locations
Over 80% of participants with experience with mobile phones reported that it was easy to use them (Table 3). Participants reported charging their phones at a variety of locations, most commonly at a relative or friend’s (34.3%) or a drop-in center or shelter (32.5%; see Table 3). Over half (56.1%) of those with past access to mobile phones versus approximately one-third (31.6%) of those with current mobile phone access reported not having service due to not having a place to charge their phones.
Table 3.
Ease of using mobile phone features and charging among participants who had ever used a mobile phone (N=277).
| Ease of use and charging locations | Total (N=277), n (%) | Currently own or have access to a mobile phone, (N=217), n (%) | Owned or had access to a mobile phone in the past, (N=60), n (%) | P value | |
| Proportion reporting very easy to neither easy nor difficult, n (%) | |||||
|
|
Punching buttons on the screen | 240 (86.6) | 191 (88.0) | 49 (82) | .20 |
|
|
Seeing the phone screen | 217 (78.3) | 174 (80.2) | 43 (72) | .16 |
|
|
Hearing the phone ring | 239 (86.3) | 189 (87.1) | 50 (83) | .45 |
|
|
Hearing people talk | 222 (80.1) | 179 (82.5) | 43 (72) | .06 |
|
|
Using voicemail | 191 (69.0) | 160 (73.7) | 31 (52) | .001 |
|
|
Using other mobile phone features (eg, contacts) | 198 (71.5) | 167 (77.0) | 31 (52) | <.001 |
| Charging locations | |||||
|
|
A friend or relative’s house | 95 (34.2) | 81 (37.3) | 14 (23) | .04 |
|
|
A drop-in center or homeless shelter | 90 (32.4) | 70 (32.2) | 20 (33) | .87 |
|
|
A library | 37 (13.3) | 25 (11.5) | 12 (20) | .09 |
|
|
A coffee shop or restaurant | 39 (14.0) | 24 (11.0) | 15 (25) | .01 |
|
|
A city power supply | 19 (6.8) | 9 (4.1) | 10 (17) | <.001 |
|
|
A social service or case management agency | 18 (6.4) | 13 (5.9) | 5 (8) | .51 |
|
|
A place where you pay to charge your phone | 3 (1.0) | 1 (0.5) | 2 (3) | .06 |
| No service due to lack of a charging locationa | 98 (35.3) | 66 (30.4) | 32 (56) | <.001 | |
a11 participants had missing data.
Computer and Internet Use
A majority of the participants reported using a computer (64.8%) or accessing the internet (55.0%) during their lifetime (see Table 4). Approximately one-third of the participants had used a computer (37.9%) or the internet (39.3%) in the past 30 days. Participants accessed the internet from a variety of locations, most of which were public. They used the internet for multiple functions including email (24.8%) and looking for information about housing (16.8%), medical information (15.1%), or a job (14.4%; see Table 4).
Table 4.
Computer, internet, and email use.
| Computer, internet, and email use | n (%) | |
| Ever used a computera | 193 (64.8) | |
| Currently use a computer | 113 (37.9) | |
| Ever used internet | 164 (55.0) | |
| Used internet, last 30 days | 117 (39.3) | |
| Venues where internet was usedb | ||
|
|
Public or university library | 59 (19.8) |
|
|
On mobile phone | 51 (17.1) |
|
|
Drop-in center or homeless shelter | 27 (9.1) |
|
|
Friend or relative’s house | 21 (7.0) |
|
|
Internet café, coffee shop, or restaurant | 11 (3.4) |
|
|
Social service agency | 8 (2.7) |
|
|
Motel or hotel lobby | 3 (1.0) |
|
|
Church | 1 (0.3) |
|
|
Workplace | 2 (0.7) |
|
|
Other venue | 26 (8.7) |
| Purpose of using the internet | ||
|
|
Read or send email | 74 (24.8) |
|
|
Get news online | 66 (22.1) |
|
|
Watch a video, download a music file, or play a game | 61 (20.5) |
|
|
Browse the internet for fun | 56 (18.8) |
|
|
Search for a fact or to answer a question | 50 (16.8) |
|
|
Look for information about a shelter or place to live | 50 (16.8) |
|
|
Look for information about a hobby or interest | 46 (15.4) |
|
|
Look for health or medical information | 45 (15.1) |
|
|
Look for information about a job | 43 (14.4) |
|
|
Check social networking sites (eg, Facebook or Twitter) | 43 (14.4) |
|
|
Do research for school or training, or obtain education | 25 (8.4) |
|
|
Send instant messages | 18 (6.0) |
|
|
Refill a prescription | 16 (5.4) |
|
|
Look for a (sex) partner | 4 (1.3) |
|
|
Know what email is | 234 (78.5) |
|
|
Know how to use email | 144 (48.3) |
|
|
Have an email account | 105 (35.2) |
| Uses of emailc | ||
|
|
Stay in touch with family or friends | 67 (22.5) |
|
|
Job searches | 46 (15.4) |
|
|
Housing searches | 40 (13.4) |
|
|
Stay in touch with health care providers | 21 (7.0) |
|
|
Stay in touch with case manager or social workers | 16 (5.4) |
|
|
Other | 21 (7.0) |
aTwo participants are not included in the computer and internet use section because they did not report whether they had ever used a computer, N=298
bThe denominator for internet venues and uses is 117.
cThe denominator for email variables ranges from 296.3 to 300.
Approximately one-third had a current email account (35.2%). The most common uses of email were staying in touch with family or friends and searching for jobs and housing (Table 4).
Factors Associated With Mobile Phone Access
In an adjusted multivariable regression model (see Table 5), we found that individuals who were housed at the time of this interview had 3.81 (adjusted odds ratio [AOR] 3.81, 95% CI 1.77-8.21) higher odds of currently owning a mobile phone, compared with those who were not housed (see Table 5). Moreover, 3 factors were associated with significantly lower odds of current mobile phone ownership: ADL impairment (AOR 0.53, 95% CI 0.31-0.92), executive function impairment (AOR 0.49, 95% CI 0.28-0.86), and moderate to high use of amphetamines (AOR 0.27, 95% CI 0.10-0.72).
Table 5.
Odds of current mobile phone use.
| Independent variables | Unadjusted odds ratio (95% CI) | P value | Adjusted odds ratio (95% CI) | P value | |
| Black | 2.06 (1.12-3.80) | .02 | —a | — | |
| Housedb | 3.75 (1.76-7.99) | <.001 | 3.81 (1.77-8.21) | <.001 | |
| Health history | |||||
|
|
Good to excellent health | 1.63 (0.96-2.78) | .07 | — | — |
|
|
ADL impairmentc | 0.60 (0.36-1.00) | .05 | 0.53 (0.31-0.92) | .02 |
|
|
Cognitive impairment (3MS, baseline)d | 0.56 (0.32-0.99) | .04 | — | — |
|
|
Executive function impairment (Trails B)e | 0.59 (0.35-1.01) | .05 | 0.49 (0.28-0.86) | .01 |
|
|
Heavy drinkingf | 0.58 (0.32-1.02) | .06 | — | — |
|
|
Moderate to high risk amphetamine useg | 0.25 (0.10-0.65) | .004 | 0.27 (0.10-0.72) | .01 |
aNot applicable.
bNot homeless as defined by the Homeless Emergency Assistance and Rapid Transition to Housing (HEARTH) Act.
cDifficulty performing one or more activities of daily living (ADL): dressing, bathing or showering, eating, getting in or out of bed, or using the toilet.
dModified Mini-Mental State Examination; less than seventh percentile based on Z-scores used.
eTrail Making Test; more than 5-min completion time on Trails B.
fDrinking ≥6 drinks on one occasion every month.
gScore of ≥4 for amphetamine use using the World Health Organization’s Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST).
Discussion
Principal Findings
In a sample of homeless-experienced adults aged 50 years and older, almost three-fourths of participants had current access to a mobile phone. Participants with phones used them for social support and communication with health care providers; however, few had annual phone contracts. Without annual contracts, it is likely that participants’ phone numbers changed frequently, limiting the utility for two-way communication.
Although compared with the general population, there was less use of the internet, a high proportion who reported ever having used the internet had used it in the prior 30 days, suggesting that individuals who had knowledge about the internet used it regularly [53]. Participants who did use the internet in the prior month used it to get directions, bus schedules, and to obtain information on employment and housing—all of which can be invaluable for individuals experiencing homelessness [5,54].
When we recruited our participants, all were homeless. A significantly higher proportion of those who were housed at the time of this interview had current access to a mobile phone. Those with current mobile phone access were significantly more likely to use phones to contact shelters or other housing providers than those without current access [55]. In our multivariable analysis, we found that being housed was significantly associated with current mobile phone ownership. A stable living situation may enable more consistent mobile phone ownership, or access to a mobile phone may have helped participants regain housing. Poor executive and cognitive functions and moderate to high risk amphetamine use were negatively associated with current mobile phone ownership. Each of these 3 factors can adversely affect an individual’s ability to participate in the type of anticipatory planning and organization required to obtain and maintain technology—even simple technology such as mobile phones. A majority of participants had lost or had their phones stolen, reflecting one of many adversities in the experience of homelessness.
Limitations
Our study has several limitations. First, our estimates of mobile phone access were likely overestimates. We introduced the mobile phone and internet module at the first follow-up interview after the baseline interview. There was differential loss to follow-up. Participants without phones at enrollment were less likely to complete the follow-up interview. Second, not all participants remained homeless at the time of the interview; those with housing were more likely to have phones than those without housing. Finally, we used a liberal definition of access to mobile phones, including those who owned or borrowed phones, or had access to one. We relied on participants to self-report mobile phone and internet use and did not have any way to verify these reports with phone bills, direct observation, or other methods.
Comparison With Prior Work
Participants’ access to mobile phones and the internet was much lower than the general population, of whom 95% own mobile phones (77% of which are smartphones) and 90% of whom use the internet [53]. Participants in our study had lower rates of smartphone and internet use when compared with low-income adults of any age [53,56,57]. Of the minority of participants who were able to access the internet, they accessed it most commonly via smartphones and public libraries. The prevalence of internet access via smartphones in our study was lower than that of those with low incomes in the general population [53]. A majority of participants reported having phones stolen and lost. Having assets stolen or lost is a common experience for people experiencing homelessness. If phones increase the risk of robbery, they may present a safety hazard for older homeless adults.
There are several ways in which older homeless adults could benefit from internet and phone access. Participants used these technologies for health care communication and to seek housing and employment information. Increasing internet and mobile phone access among older homeless adults could allow older homeless adults to more easily apply for housing or to search for housing in areas outside of urban centers that may be lower-cost. Internet and mobile phone access could also facilitate contact with potential employers and increase access to employment and social networking sites.
Mobile phones can facilitate communication with family or friends who may be able to provide instrumental as well as emotional support [17]. Social support has been shown to be associated with better health [58]. In addition, homeless individuals need low-barrier access to outpatient primary care; mobile phones and internet access could facilitate this. A pilot study that examined the feasibility and potential efficacy of using text messages to remind homeless veterans about appointments found that the veterans liked receiving the messages, and those messages may have improved appointment attendance [59]. Two-thirds of our participants reported using their phones to communicate with their health care providers, suggesting both interest and feasibility.
Our participants did not have annual phone contracts. This limited the possibilities for bidirectional communication due to interruptions in service and changing phone numbers. Previous research has cited barriers to mobile phone use among homeless individuals, including cost, fear of loss or theft, and a lack of knowledge about how to use mobile technology [19,37]. The widespread use of month-to-month, instead of annual plans, the use of borrowed (instead of owned) phones, and the relatively low proportion of people who had current access to phones may reflect these barriers, particularly cost. Although there are some programs to address financial barriers to mobile phone use among low-income populations, we found participants had low rates of enrollment in such programs. The “Lifeline” program provides Federal Assistance recipients and those who provide proof of low income with free feature or smartphones and pays for voice calls and texting for a year, with the possibility of recertification [60]. Although most of our participants met the criteria for this program, few reported using its free mobile phones and service. The Lifeline program requires a mailing address. Many people experiencing homelessness lack a stable mailing address, which could cause phone service interruptions.
Without the widespread adoption of phone contracts by homeless adults, health care providers should consider open access scheduling, which could allow homeless adults with any form of phone access to make appointments, while acknowledging their inability to receive appointment reminder calls and texts. Open access scheduling allows for same day appointments and does not rely on reminder calls for appointments scheduled far in advance. This could lower access barriers for individuals experiencing homelessness who may have minimal or no access to mobile phones and the internet. In addition, allowing mobile phone users to maintain the same phone number despite interruptions in service could increase their ability to communicate with health care providers.
Participants in our study did not report difficulty with using phone buttons or keyboard. However, impairments in ADLs and executive function were associated with lower odds of current mobile phone use. Given the levels of these impairments among our participants, more research is needed to match end users with appropriate training tools and technology. It is possible that many who use feature phones could make use of smartphones with appropriate access and training. Others may require improved access and training to make use of feature phone technology.
Another possibility is that impairments in ADLs and executive functioning indirectly decrease use of mobile phones by making it difficult to obtain mobile phones and maintain service. Participants without phones reported a higher likelihood of losing service due to not having a place to charge their phone. Therefore, multipronged approaches that include increasing access to phones, charging stations, and internet might be most effective in increasing the adoption of mobile technology among older adults experiencing homelessness.
Increased public access to high-speed internet and providing discounted smartphones for high-need, low-income individuals may increase access to the internet [61]. Private sector technology and telecommunication companies might also be incentivized to fund initiatives that increase the use of their services among underserved populations, increasing access to reliable mobile technology [61]. Older adults comprise an increasing proportion of the US population. One way for technology companies to increase adoption of mobile phones for older adults is to include them in participatory design and usability testing [62,63]. Adapting devices and tailoring online advanced features to meet the needs of older homeless adults could facilitate their inclusion in the digital economy.
Conclusions
This study is one of the first studies to examine mobile phone and internet use among a community-based sample of homeless adults over the age of 50 years [64]. The majority of participants with access to technology were able to take advantage of most mobile phone functions, although most of their mobile phones were feature phones with limited internet access. Participants used these technologies for health care communication, seeking information for housing, and looking for employment opportunities.
However, most participants did not have annual phone contracts—which can lead to new phone numbers with each new phone—and few had access to smartphones. Lowering financial barriers to allow annual mobile phone contracts and increasing the homeless individuals’ ability to access the internet via smartphones could promote more reliable and widespread use of these basic technologies. In addition, providers can take steps to optimize the technology individuals experiencing homelessness have access to, by offering open access and same-day scheduling and communication. More research is needed to determine if increasing access to mobile phones and internet can positively impact downstream health and economic outcomes among individuals experiencing homelessness.
The high prevalence of functional and executive function impairment in our study population was negatively associated with access to mobile phones. Advanced technological features might be challenging for this segment of the homeless- experienced population. Initiatives to increase access to technology among older homeless adults must address the needs of those with impairments and create technological features that fit the individuals’ needs and abilities.
Acknowledgments
The authors gratefully acknowledge their colleagues Claudia Ponath, Pamela Olsen, Nina Fiellin, Tauni Marin, and Kenneth Perez for their invaluable contributions to the Health Outcomes of People Experiencing Homelessness in Older Middle Age (HOPE HOME) study. They also acknowledge their colleague Angela Allen, who passed away in May 2015, for her incredible contributions to the study. The authors also thank the staff at St. Mary’s Center and the HOPE HOME Community Advisory board for their guidance and partnership. This study was funded by grants from the National Institute on Aging at the National Institutes of Health [K24AG046372, R01AG041860, and P30AG044281] and by the National Institute on Minority Health and Health Disparities [R25MD006832]. These funding sources had no role in the preparation, review, or approval of the manuscript.
Abbreviations
- ADL
activity of daily living
- AOR
adjusted odds ratio
- ASSIST
Alcohol, Smoking, and Substance Involvement Screening Test
- CES-D
Center for Epidemiologic Studies Depression Scale
- GED
General Educational Development
- HEARTH
Homeless Emergency Assistance and Rapid Transition to Housing
- HOPE HOME
Health Outcomes of People Experiencing Homelessness in Older Middle Age
- Trails B
Trail Making Test
- 3MS
Modified Mini-Mental State
Footnotes
Conflicts of Interest: None declared.
References
- 1.Hahn JA, Kushel MB, Bangsberg DR, Riley E, Moss AR. BRIEF REPORT: the aging of the homeless population: fourteen-year trends in San Francisco. J Gen Intern Med. 2006 Jul;21(7):775–8. doi: 10.1111/j.1525-1497.2006.00493.x. http://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0884-8734&date=2006&volume=21&issue=7&spage=775 .JGI493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown RT, Kimes RV, Guzman D, Kushel M. Health care access and utilization in older versus younger homeless adults. J Health Care Poor Underserved. 2010 Aug;21(3):1060–70. doi: 10.1353/hpu.0.0344.S1548686910300210 [DOI] [PubMed] [Google Scholar]
- 3.Brown RT, Hemati K, Riley ED, Lee CT, Ponath C, Tieu L, Guzman D, Kushel MB. Geriatric conditions in a population-based sample of older homeless adults. Gerontologist. 2017 Dec 01;57(4):757–66. doi: 10.1093/geront/gnw011. http://europepmc.org/abstract/MED/26920935 .gnw011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spinelli MA, Ponath C, Tieu L, Hurstak EE, Guzman D, Kushel M. Factors associated with substance use in older homeless adults: results from the HOPE HOME study. Subst Abus. 2017;38(1):88–94. doi: 10.1080/08897077.2016.1264534. http://europepmc.org/abstract/MED/27897965 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006 Jan;21(1):71–7. doi: 10.1111/j.1525-1497.2005.00278.x. https://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=0884-8734&date=2006&volume=21&issue=1&spage=71 .JGI278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arora S, Burner E, Terp S, Nok LC, Nercisian A, Bhatt V, Menchine M. Improving attendance at post-emergency department follow-up via automated text message appointment reminders: a randomized controlled trial. Acad Emerg Med. 2015 Jan;22(1):31–7. doi: 10.1111/acem.12503. doi: 10.1111/acem.12503. [DOI] [PubMed] [Google Scholar]
- 7.da Costa TM, Salomão PL, Martha AS, Pisa IT, Sigulem D. The impact of short message service text messages sent as appointment reminders to patients' cell phones at outpatient clinics in São Paulo, Brazil. Int J Med Inform. 2010 Jan;79(1):65–70. doi: 10.1016/j.ijmedinf.2009.09.001.S1386-5056(09)00133-6 [DOI] [PubMed] [Google Scholar]
- 8.Stubbs ND, Geraci SA, Stephenson PL, Jones DB, Sanders S. Methods to reduce outpatient non-attendance. Am J Med Sci. 2012 Sep;344(3):211–9. doi: 10.1097/MAJ.0b013e31824997c6.S0002-9629(15)30856-9 [DOI] [PubMed] [Google Scholar]
- 9.Wright A, Poon EG, Wald J, Feblowitz J, Pang JE, Schnipper JL, Grant RW, Gandhi TK, Volk LA, Bloom A, Williams DH, Gardner K, Epstein M, Nelson L, Businger A, Li Q, Bates DW, Middleton B. Randomized controlled trial of health maintenance reminders provided directly to patients through an electronic PHR. J Gen Intern Med. 2012 Jan;27(1):85–92. doi: 10.1007/s11606-011-1859-6. http://europepmc.org/abstract/MED/21904945 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schickedanz A, Huang D, Lopez A, Cheung E, Lyles CR, Bodenheimer T, Sarkar U. Access, interest, and attitudes toward electronic communication for health care among patients in the medical safety net. J Gen Intern Med. 2013 Jul;28(7):914–20. doi: 10.1007/s11606-012-2329-5. http://europepmc.org/abstract/MED/23423453 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cotter AP, Durant N, Agne AA, Cherrington AL. Internet interventions to support lifestyle modification for diabetes management: a systematic review of the evidence. J Diabetes Complications. 2014;28(2):243–51. doi: 10.1016/j.jdiacomp.2013.07.003. http://europepmc.org/abstract/MED/24332469 .S1056-8727(13)00165-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Irizarry T, DeVito DA, Curran CR. Patient portals and patient engagement: a state of the science review. J Med Internet Res. 2015;17(6):e148. doi: 10.2196/jmir.4255. http://www.jmir.org/2015/6/e148/ v17i6e148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patrick K, Griswold WG, Raab F, Intille SS. Health and the mobile phone. Am J Prev Med. 2008 Aug;35(2):177–81. doi: 10.1016/j.amepre.2008.05.001. http://europepmc.org/abstract/MED/18550322 .S0749-3797(08)00407-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Woods SS, Forsberg WC, Schwartz CE, Nazi Mk, Hibbard HJ, Houston KT, Gerrity M. The association of patient factors, digital access, and online behavior on sustained patient portal use: A prospective cohort of enrolled users. J Med Internet Res. 2017;19(10):A. doi: 10.2196/jmir.7895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Genz A, Kirk G, Piggott D, Mehta SH, Linas BS, Westergaard RP. Uptake and acceptability of information and communication technology in a community-based cohort of people who inject drugs: implications for mobile health interventions. JMIR Mhealth Uhealth. 2015 Jun 25;3(2):e70. doi: 10.2196/mhealth.3437. http://mhealth.jmir.org/2015/2/e70/ v3i2e70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stennett CR, Weissenborn MR, Fisher GD, Cook RL. Identifying an effective way to communicate with homeless populations. Public Health. 2012 Jan;126(1):54–6. doi: 10.1016/j.puhe.2011.09.020.S0033-3506(11)00275-7 [DOI] [PubMed] [Google Scholar]
- 17.Rice E, Kurzban S, Ray D. Homeless but connected: the role of heterogeneous social network ties and social networking technology in the mental health outcomes of street-living adolescents. Community Ment Health J. 2012 Dec;48(6):692–8. doi: 10.1007/s10597-011-9462-1. http://europepmc.org/abstract/MED/22075769 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rice E, Barman-Adhikari A. Internet and social media use as a resource among homeless youth. J Comput Mediat Commun. 2014 Jan 01;19(2):232–47. doi: 10.1111/jcc4.12038. http://europepmc.org/abstract/MED/25328374 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McInnes DK, Fix GM, Solomon JL, Petrakis BA, Sawh L, Smelson DA. Preliminary needs assessment of mobile technology use for healthcare among homeless veterans. PeerJ. 2015;3:e1096. doi: 10.7717/peerj.1096. doi: 10.7717/peerj.1096.1096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McInnes DK, Sawh L, Petrakis BA, Rao SR, Shimada SL, Eyrich-Garg KM, Gifford AL, Anaya HD, Smelson DA. The potential for health-related uses of mobile phones and internet with homeless veterans: results from a multisite survey. Telemed J E Health. 2014 Sep;20(9):801–9. doi: 10.1089/tmj.2013.0329. [DOI] [PubMed] [Google Scholar]
- 21.Rice E, Lee A, Taitt S. Cell phone use among homeless youth: potential for new health interventions and research. J Urban Health. 2011 Dec;88(6):1175–82. doi: 10.1007/s11524-011-9624-z. http://europepmc.org/abstract/MED/22076445 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Y, Lauche R, Sibbritt D, Olaniran B, Cook R, Adams J. Comparison of health information technology use between American Adults with and without chronic health conditions: findings from the National Health Interview Survey 2012. J Med Internet Res. 2017 Oct 05;19(10):e335. doi: 10.2196/jmir.6989. http://www.jmir.org/2017/10/e335/ v19i10e335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ackerman SL, Sarkar U, Tieu L, Handley MA, Schillinger D, Hahn K, Hoskote M, Gourley G, Lyles C. Meaningful use in the safety net: a rapid ethnography of patient portal implementation at five community health centers in California. J Am Med Inform Assoc. 2017 Mar 15; doi: 10.1093/jamia/ocx015.3072321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arthur T, Jerzy L. The internet , ecommerce and older people: an actor network approach to researching reasons for adoption and use. Logistics Inf Manage. 2003:56–63. doi: 10.1108/09576050310453741. [DOI] [Google Scholar]
- 25.Wildenbos GA, Peute L, Jaspers M. Facilitators and barriers of electronic health record patient portal adoption by older adults: a literature study. Stud Health Technol Inform. 2017;235:308–12. doi: 10.3233/978-1-61499-753-5-308. [DOI] [PubMed] [Google Scholar]
- 26.Lee C, Coughlin JF. Perspective: older adults' adoption of technology: an integrated approach to identifying determinants and barriers. J Prod Innov Manag. 2014 Jun 03;32(5):747–59. doi: 10.1111/jpim.12176. [DOI] [Google Scholar]
- 27.Olphert C, Damodaran L, May A. Towards digital inclusion - engaging older people in the 'digital world'. Proceedings of the 2005 international conference on Accessible Design in the Digital World; 2005 international conference on Accessible Design in the Digital World; August 23-25, 2005; Dundee, Scotland. BCS Learning & Development Ltd; 2005. pp. 17–17. https://ewic.bcs.org/content/ConWebDoc/3825 . [Google Scholar]
- 28.Jennings L, Lee N, Shore D, Strohminger N, Allison B, Conserve DF, Cheskin LJ. US minority homeless youth's access to and use of mobile phones: implications for mHealth intervention design. J Health Commun. 2016 Jul;21(7):725–33. doi: 10.1080/10810730.2015.1103331. [DOI] [PubMed] [Google Scholar]
- 29.Burnam M, Koegel P. Methodology for obtaining a representative sample of homeless persons: the Los-Angeles skid row study. Eval Rev. 1988;12(2):117–52. doi: 10.1177/0193841X8801200202. [DOI] [Google Scholar]
- 30.Lee CT, Guzman D, Ponath C, Tieu L, Riley E, Kushel M. Residential patterns in older homeless adults: results of a cluster analysis. Soc Sci Med. 2016 Mar;153:131–40. doi: 10.1016/j.socscimed.2016.02.004. http://europepmc.org/abstract/MED/26896877 .S0277-9536(16)30059-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Henry M, Watt R, Rosenthal L, Shivji A. Washington: DC: The U.S. Department of Housing and Urban Development: Office of Community Planning and Development. 2017. The 2017 Annual Homeless Assessment Report (AHAR) to Congress https://www.hudexchange.info/resources/documents/2017-AHAR-Part-1.pdf .
- 32.US Congress. 2009. [2018-01-01]. S. 896 HEARTH Act of 2009 https://www.hudexchange.info/resource/1717/s-896-hearth-act/
- 33.Dunn LB, Jeste DV. Enhancing informed consent for research and treatment. Neuropsychopharmacology. 2001 Jun;24(6):595–607. doi: 10.1016/S0893-133X(00)00218-9. doi: 10.1016/S0893-133X(00)00218-9.S0893133X00002189 [DOI] [PubMed] [Google Scholar]
- 34.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004 Sep;36(8):588–94. http://www.stfm.org/fmhub/fm2004/September/Lisa588.pdf . [PubMed] [Google Scholar]
- 35.Sarkar U, Schillinger D, López A, Sudore R. Validation of self-reported health literacy questions among diverse English and Spanish-speaking populations. J Gen Intern Med. 2011 Mar;26(3):265–71. doi: 10.1007/s11606-010-1552-1. http://europepmc.org/abstract/MED/21057882 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, Bradley KA, Nugent SM, Baines AD, Vanryn M. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008 May;23(5):561–6. doi: 10.1007/s11606-008-0520-5. http://europepmc.org/abstract/MED/18335281 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McInnes DK, Li AE, Hogan TP. Opportunities for engaging low-income, vulnerable populations in health care: a systematic review of homeless persons' access to and use of information technologies. Am J Public Health. 2013 Dec;103(Suppl 2):e11–24. doi: 10.2105/AJPH.2013.301623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pew Research Center. Pew Research Center; 2012. [2018-01-01]. March 15-April 3, 2012 – Cell Phones http://www.pewinternet.org/dataset/april-2012-cell-phones/ [Google Scholar]
- 39.Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996 Mar;34(3):220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention. Hyattsville, MD: Centers for Disease Control and Prevention; 2013. [2018-01-01]. National Health and Nutrition Examination Survey Questionnaire (NHANES) https://www.cdc.gov/nchs/data/nhanes/nhanes_13_14/2013-14_overview_brochure.pdf . [Google Scholar]
- 41.Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. 1983 Dec;31(12):721–7. doi: 10.1111/j.1532-5415.1983.tb03391.x. [DOI] [PubMed] [Google Scholar]
- 42.Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987 Aug;48(8):314–8. [PubMed] [Google Scholar]
- 43.Reitan RM. Validity of the Trail Making Test as an indicator of organic brain damage. Percept Mot Skills. 1958;8(3):271–6. doi: 10.2466/PMS.8.7.271-276. [DOI] [Google Scholar]
- 44.Bravo G, Hébert R. Age- and education-specific reference values for the Mini-Mental and modified Mini-Mental State Examinations derived from a non-demented elderly population. Int J Geriatr Psychiatry. 1997 Oct;12(10):1008–18. doi: 10.1002/(sici)1099-1166(199710)12:10<1008::aid-gps676>3.0.co;2-a.10.1002/(SICI)1099-1166(199710)12:10<1008::AID-GPS676>3.0.CO;2-A [DOI] [PubMed] [Google Scholar]
- 45.Heaton R. Revised Comprehensive Norms for an Expanded Halstead-Reitan Battery: Demographically Adjusted Neuropsychological Norms for African American and Caucasian Adults (HRB) Professional Manual. Lutz, Fla: Psychological Assessment Resources. Print. 2004 https://www.parinc.com/Products/Pkey/357 . [Google Scholar]
- 46.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977 Jun 01;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 47.Cheng ST, Chan AC. The Center for Epidemiologic Studies Depression Scale in older Chinese: thresholds for long and short forms. Int J Geriatr Psychiatry. 2005 May;20(5):465–70. doi: 10.1002/gps.1314. [DOI] [PubMed] [Google Scholar]
- 48.Haringsma R, Engels GI, Beekman ATF, Spinhoven P. The criterion validity of the Center for Epidemiological Studies Depression Scale (CES-D) in a sample of self-referred elders with depressive symptomatology. Int J Geriatr Psychiatry. 2004 Jun;19(6):558–63. doi: 10.1002/gps.1130. [DOI] [PubMed] [Google Scholar]
- 49.Babor T, Higgins-Biddle J, Saunders J, Monteiro M. World Health Organization. Geneva: 2001. [2018-01-01]. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for use in primary care http://apps.who.int/iris/handle/10665/67205 . [Google Scholar]
- 50.Humeniuk R, Henry-Edwards S, Ali R, Poznyak V, Monteiro M. World Health Organization. Geneva: 2010. ASSIST“The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Manual for use in primary care http://apps.who.int/iris/bitstream/10665/44320/1/9789241599382_eng.pdf . [Google Scholar]
- 51.Gielen AC, McDonnell KA, Wu AW, O'Campo P, Faden R. Quality of life among women living with HIV: the importance violence, social support, and self care behaviors. Soc Sci Med. 2001 Jan;52(2):315–22. doi: 10.1016/S0277-9536(00)00135-0.S0277953600001350 [DOI] [PubMed] [Google Scholar]
- 52.Gielen AC, O'Campo PJ, Faden RR, Kass NE, Xue X. Interpersonal conflict and physical violence during the childbearing year. Soc Sci Med. 1994 Sep;39(6):781–7. doi: 10.1016/0277-9536(94)90039-6. [DOI] [PubMed] [Google Scholar]
- 53.Pew Research Center. Washington DC: Pew Research Center; 2017. [2018-01-01]. Mobile Fact Sheet http://www.pewinternet.org/fact-sheet/mobile/ [Google Scholar]
- 54.Le Dantec CA, Edwards W. Designs on dignity: perceptions of technology among the homeless. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. Association for Computing Machinery; April 10, 2008; New York. 2008. Apr 10, pp. A–636. https://www.cc.gatech.edu/~keith/pubs/chi2008-homeless.pdf . [Google Scholar]
- 55.Eyrich-Garg KM. Sheltered in cyberspace? Computer use among the unsheltered ‘street’ homeless. Comput Human Behav. 2011 Jan;27(1):296–303. doi: 10.1016/j.chb.2010.08.007. [DOI] [Google Scholar]
- 56.Pew Research Center. Washington DC: Pew Research Center; 2017. [2018-01-01]. Tech adoption climbs among older adults http://www.pewinternet.org/2017/05/17/tech-adoption-climbs-among-older-adults/ [Google Scholar]
- 57.Pew Research Center. Washington DC: Pew Research Center; 2017. [2018-01-01]. Internet/Broadband Fact Sheet http://www.pewinternet.org/fact-sheet/internet-broadband/# . [Google Scholar]
- 58.Uchino BN, Cacioppo JT, Kiecolt-Glaser JK. The relationship between social support and physiological processes: a review with emphasis on underlying mechanisms and implications for health. Psychol Bull. 1996 May;119(3):488–531. doi: 10.1037/0033-2909.119.3.488. [DOI] [PubMed] [Google Scholar]
- 59.McInnes DK, Petrakis BA, Gifford AL, Rao SR, Houston TK, Asch SM, O'Toole TP. Retaining homeless veterans in outpatient care: a pilot study of mobile phone text message appointment reminders. Am J Public Health. 2014 Sep;104(Suppl 4):S588–94. doi: 10.2105/AJPH.2014.302061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lifeline Facts. 2017. Obama Phone https://www.obamaphone.com/lifeline-facts .
- 61.Jaeger P, Bertot J, Thompson K, Katz S, DeCoster E. The intersection of public policy and public access: digital divides, digital literacy, digital inclusion, and public libraries. Public Library Q. 2012;31(1):1–20. doi: 10.1080/01616846.2012.654728. [DOI] [Google Scholar]
- 62.Gustafson DH, Maus A, Judkins J, Dinauer S, Isham A, Johnson R, Landucci G, Atwood AK. Using the NIATx Model to implement user-centered design of technology for older adults. JMIR Hum Factors. 2016 Jan 14;3(1):e2. doi: 10.2196/humanfactors.4853. http://humanfactors.jmir.org/2016/1/e2/ v3i1e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Pak R, Price MM, Thatcher J. Age-sensitive design of online health information: comparative usability study. J Med Internet Res. 2009 Nov 16;11(4):e45. doi: 10.2196/jmir.1220. http://www.jmir.org/2009/4/e45/ v11i4e45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Eyrich-Garg KM. Mobile phone technology: a new paradigm for the prevention, treatment, and research of the non-sheltered “street” homeless? J Urban Health. 2010 May;87(3):365–80. doi: 10.1007/s11524-010-9456-2. http://europepmc.org/abstract/MED/20397058 . [DOI] [PMC free article] [PubMed] [Google Scholar]


