Abstract
Purpose
To compare the visualization of the choriocapillaris and deeper choroidal vessels in healthy eyes in en face swept-source optical coherence tomography (SS-OCT) versus SS-OCT angiography (SS-OCTA).
Methods
This is a cross-sectional study of consecutive eyes without chorioretinal disease. En face SS-OCT and SS-OCTA images of the choriocapillaris and choroid were assessed for visualization of the vasculature. Choroidal vessel densities (CVD) of the choriocapillaris, inner choroid, midchoroid, and outer choroid were calculated from binarized en face SS-OCT and SS-OCTA images. Paired t-tests and linear regression were used for statistical analysis.
Results
Twenty-seven eyes of 27 patients were included. There was no statistically significant difference between the CVDs of the midchoroid assessed with en face SS-OCT versus SS-OCTA (P = 0.21). However, there were statistically significant differences between the CVDs for the choriocapillaris (P < 0.001), inner choroid (P < 0.001), and outer choroid (P = 0.006). Qualitative analysis revealed incomplete visualization of vessels in the inner choroid and exaggeration of vessel lumens in the outer choroid with SS-OCTA.
Conclusions
Visualization of the choriocapillaris is superior with SS-OCTA, but it has numerous limitations that make visualization of deeper choroidal vessels less reliable when compared with en face SS-OCT. It is important to understand such limitations when using these technologies to study the choroidal vasculature in chorioretinal disease.
Translational Relevance
The presented study of optimal imaging techniques for the choroidal vessels of healthy eyes provides an important foundation for future investigations into the role of the choroidal vasculature in chorioretinal diseases.
Keywords: choroid, vessel density, swept source, choriocapillaris, optical coherence tomography angiography
Introduction
The development and increasingly widespread use of swept-source optical coherence tomography (SS-OCT) has enabled improved visualization of the choriocapillaris and choroid owing to use of a longer wavelength, tunable laser, and detection method that allows for faster scanning speeds.1 In addition, en face reconstruction of B-scans in a coronal orientation produces images capturing the course of deep choroidal vessels. Using en face SS-OCT, the choroidal vessel density (CVD) of the deep choroid can be quantified and has been analyzed in healthy eyes2 and numerous retinal pathologies, including age-related macular degeneration (AMD),3–5 polypoidal choroidal vasulopathy (PCV),6,7 diabetic retinopathy (DR),8–10 central serous retinopathy (CSR),11–13 and macular telangiectasia type 2.14 Though more limited by resolution, analysis of the choriocapillaris with en face SS-OCT has also been performed.15
SS-OCT angiography (SS-OCTA), which uses decorrelation signal generated from moving erythrocytes, has been shown to have the capability to image the choriocapillaris.16–18 Similar to en face SS-OCT, it has also been used to analyze CVD of deeper choroidal vessels.19 However, it is not known whether using SS-OCTA to image deeper choroidal vessels affords any advantages over en face SS-OCT. Our group recently showed that flow signal is not present in deeper choroidal vessels on SS-OCTA in eyes with intact retinal pigment epithelium (RPE).20
To our knowledge, there have been no previous studies directly comparing visualization of the choriocapillaris and deeper choroidal vessels in en face SS-OCT and SS-OCTA. We hypothesize that while SS-OCTA enhances visualization of the choriocapillaris, it may not provide an additional advantage over en face SS-OCT in the visualization of deep choroidal vessels. Herein, we analyze and compare the CVD of the choriocapillaris and choroid of healthy eyes using en face SS-OCT and SS-OCTA.
Methods
Study Design
This study was conducted as part of a cross-sectional study on retinal imaging performed at the Massachusetts Eye and Ear (MEE), Harvard Medical School, Boston, United States. This research adhered to the tenets of the Declaration of Helsinki. The institutional review board (IRB) of MEE approved the study protocol. All included participants provided written informed consent.
Study Subjects
An existing imaging protocol is in place at our institution whereby patients with chorioretinal disease may be imaged with Topcon DRI OCT-1 Triton (Topcon Corporation, Tokyo, Japan), which can simultaneously capture SS-OCTA and en face SS-OCT images. We reviewed this database and identified consecutive eyes without retinal or choroidal pathology from July 2016 to December 2017 with the following exclusion criteria: diagnosis of ocular hypertension or glaucoma with an optic nerve cup-disc ratio greater than 0.6, decreased media transparency that precluded appropriate OCT imaging, or blink or motion artifacts that could affect image analysis. Only one eye per patient was randomly selected for inclusion.
Clinical Study Protocol
Study subjects were imaged using the swept-source platform Topcon DRI OCT-1 Triton. Choroidal thickness (CT) was obtained with the built-in software of the device (Topcon FastMap, version 9.12.003.04). Automated segmentation was confirmed by an experienced grader (JCW), and manually corrected when necessary. Thickness maps were then created according to the conventional Early Treatment Diabetic Retinopathy Study (ETDRS) grid. Finally, the obtained CT values in the nine ETDRS different fields were registered. The average CT was defined as the arithmetic average of all subregions of the standard ETDRS grid. SS-OCTA was also obtained at the same visit with Topcon SS-OCT Angio (4.5 × 4.5 mm).
Choroidal Vessel Analysis
SS-OCTA and SS-OCT en face images of the default choriocapillaris slab (0–10.4 μm below Bruch's membrane) were exported. Images with substantial motion artifacts were excluded from analysis (n = 12). The midchoroid depth was defined as half of the average choroidal thickness. The inner and outer choroid depths were defined as one- and three-quarters of the average choroidal thickness, respectively. Individual SS-OCTA and en face SS-OCT image slices at these depths were exported. These images were imported into ImageJ (National Institutes of Health, Bethesda, MD) and binarized with the Niblack local thresholding function.21 The choroidal vascular density was calculated as a percentage area occupied by the choroidal vessels for each slice. For the choriocapillaris, bright pixels were counted within vessel lumens, whereas for the deeper choroid, dark pixels were within vessel lumens. Figure 1 displays an example summarizing this process.
Figure 1.
Representative example of image export and processing. SS-OCTA and en face SS-OCT images are exported from the choriocapillaris (A, I), inner choroid (B, J), midchoroid (C, K), and outer choroid (D, L). These images are then binarized in ImageJ using the Niblack local thresholding algorithm (E–H, M–P), which are used to calculate choroidal vessel density.
Statistical Analyses
Because only one eye from each patient was included for analysis, paired t-tests were used to determine statistically significant differences between CVDs of the choroicapillaris, inner choroid, midchoroid, and outer choroid from en face SS-OCT and SS-OCTA. In addition, to explore the effect of choroidal depth on these measurements, linear regression was performed on the difference between CVDs as measured by en face SS-OCT and SS-OCTA. For select representative eyes, the difference between CVDs was plotted as a function of choroidal depth.
All statistics were performed using Excel Data Analysis Toolpak (Microsoft, Redmond, WA) and P values less than 0.05 were considered statistically significant.
Results
Summary of Demographic and Clinical Characteristics
A total of 27 eyes without retinal or choroidal pathology from 27 patients were included in the study. The mean age was 52.4 ± 18.2 years (range, 21.8–81.6). Fifteen of 27 patients were female and 15 of 27 eyes were right eyes. The average visual acuity was 20/20. The average choroidal thickness was 253.3 ± 82.3 μm. The Table summarizes the average choroidal indices for the cohort.
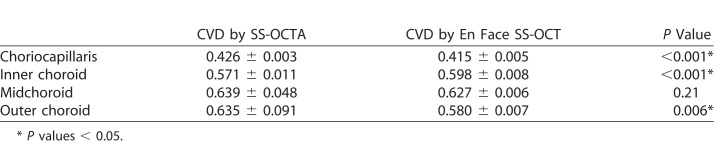
Table.
Summary of Average Choroidal Vascular Densities by SS-OCTA Compared With En Face SS-OCT
Qualitative and Quantitative Analysis of the Choriocapillaris
The CVD of the choriocapillaris as measured by SS-OCTA was significantly greater than that of en face SS-OCT (0.426 ± 0.003 vs. 0.415 ± 0.005, P < 0.001). Both SS-OCTA and en face SS-OCT images of the choriocapillaris were characterized by a grainy appearance. However, projection artifact from overlying retinal vessels were more prominently seen in en face SS-OCT images (Fig. 1I).
Qualitative and Quantitative Analysis of the Deeper Choroid
There was not a statistically significant difference between CVD of the midchoroid as measured by SS-OCTA and en face SS-OCT (0.639 ± 0.048 vs. 0.627 ± 0.006, P = 0.21). However, there was a statistically significant linear relationship between choroidal depth and the difference between CVDs of the midchoroid (P < 0.001). Figure 2 displays this trend with images from two representative examples of different choroidal depths.
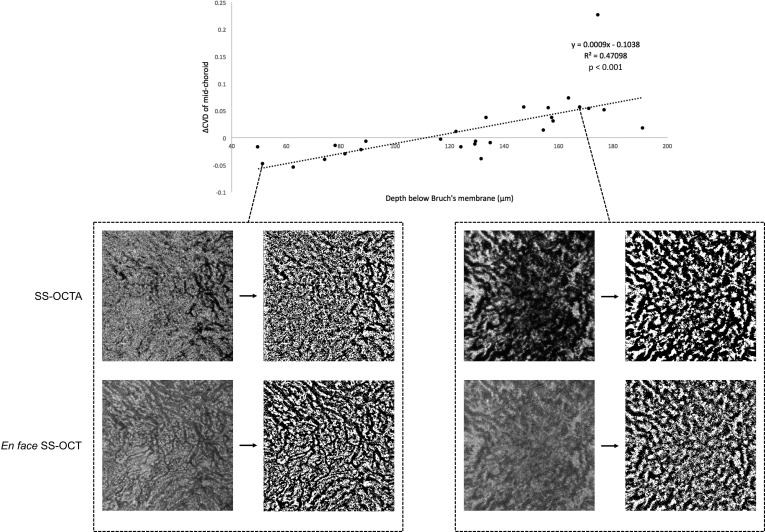
Figure 2.
Scatterplot of the difference in midchoroid choroidal vessel density (ΔCVD), defined as the CVD as measured by SS-OCTA minus the CVD as measured by en face SS-OCT versus choroidal depth of the midchoroid. There was a statistically significant positive linear relationship (P < 0.001). Two representative examples of SS-OCTA and en face SS-OCT and the resulting binarized images from each extreme in choroidal depth are displayed to illustrate this relationship.
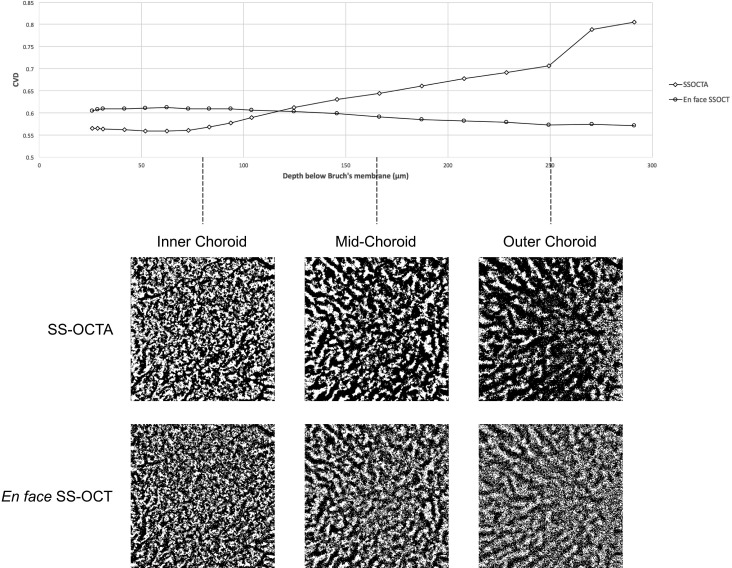
In the inner choroid, SS-OCTA tended to underpredict CVD compared with en face SS-OCT (0.571 ± 0.011 vs. 0.598 ± 0.008, P < 0.001). Qualitatively, it appeared that SS-OCTA did not fully capture all choroidal vessels visible on en face SS-OCT, especially smaller vessels in Sattler's layer. Conversely, in the outer choroid, SS-OCTA tended to overpredict CVD compared with en face SS-OCT (0.635 ± 0.091 vs. 0.580 ± 0.007, P = 0.006). Qualitatively, the choroidal vessels visualized on SS-OCTA appeared to have larger caliber than the corresponding vessels on en face SS-OCT. Figure 3 shows CVD calculated by SS-OCTA and en face SS-OCT as a function of choroidal depth for a single representative eye to demonstrate this phenomenon.
Figure 3.
Plot of CVD as measured by SS-OCTA and by en face SS-OCT versus depth below Bruch's membrane for one representative eye. Binarized images from SS-OCTA and en face SS-OCT of the inner choroid, midchoroid, and outer choroid are displayed.
Discussion
In this study, we assessed the ability of SS-OCTA to visualize choroidal vessels in the choriocapillaris and choroid as compared with en face SS-OCT. While en face SS-OCT and SS-OCTA are separate technologies and provide different information regarding the structure imaged, both have been used to study the choriocapillaris and choroidal vessels.6–19 In theory, while SS-OCTA should provide a more accurate representation of the choroidal vasculature because it detects decorrelation signal from erythrocytes within blood vessels, it does have numerous limitations.20 We found that for the choriocapillaris, the CVD as measured by SS-OCTA was significantly greater than that measured by en face SS-OCT. We observed that this difference was most likely due to projection artifact showing superficial retinal vessels in en face SS-OCT images. SS-OCTA has been used to image the choriocapillaris and it has been shown that in certain situations, such as imaging through drusen, SS-OCTA outperforms spectral-domain OCTA.18 In addition, flow voids corresponding to choriocapillaris dropout in various chorioretinal pathologies are well visualized by SS-OCTA.3 Nonetheless, images of the choriocapillaris obtained with SS-OCTA often appear to have a grainy texture, as was the case in our study. They appeared similar to corresponding en face SS-OCT images but with less prominent superficial retinal vessels, likely as a result of improvements in postprocessing removal of projection artifacts. The CVD measurements of the choriocapillaris obtained with SS-OCTA were similar to previously published reports.16 Improvements in the resolution of SS-OCTA images have also been made with ultra-high scanning rates17 and with averaging of multiple images22 in order to visualize individual choriocapillaris lobules.
In Sattler's and Haller's layers of the choroid, choroidal vessel lumens appear dark on structural en face SS-OCT. This translates to a relative lack of signal compared with the surrounding stroma and may be related to a combination of scattering of signal from the RPE and high-velocity flow rates in the choroidal vessels as compared with retinal vessels. The vessel lumens also appear dark on SS-OCTA, and we have previously shown that this is most likely related to light scattering and signal attenuation due to the RPE because in the absence of RPE, these vessels appear bright.20
In the inner choroid, both en face SS-OCT and SS-OCTA are able to visualize choroidal vessels in Sattler's layer. However, SS-OCTA did not appear to capture the choroidal vasculature as fully as en face SS-OCT, which led to consistent underestimation of CVD by SS-OCTA as compared with en face SS-OCT. The reason for this is unclear, but could be related to either partial detection of flow in smaller caliber vessels, or decorrelation projection artifact from the overlying choriocapillaris, which is rendered as bright signal and leads to the appearance that some vessels are not visualized because most vessels appear dark.
In the outer choroid, choroidal vessel lumens appeared larger in SS-OCTA than in en face SS-OCT, which led to consistent overestimation of CVD by SS-OCTA as compared with en face SS-OCT. This is likely related to a very low signal-to-noise ratio due to sensitivity roll-off with increasing imaging depth such that fewer signals meet the decorrelation threshold on SS-OCTA. This gives the appearance of deep choroidal vessels having exaggerated lumens. This phenomenon becomes more pronounced with increasing depth of imaging.
For the midchoroid, though we did not find a significant difference between the CVDs as measured by SS-OCTA and en face SS-OCT, there was a notable trend between depth of imaging at the midchoroid and difference in CVD. This trend was consistent with the above observations regarding visualization of the choroidal vessels in the inner and outer choroid. While CVD measurements of the midchoroid were not significantly different between SS-OCTA and en face SS-OCT, this was possibly due to an offsetting effect whereby the incomplete visualization of choroidal vessels on SS-OCTA was balanced by larger lumens for vessels that were visualized.
A recent study used en face SS-OCT and a very similar image analysis method to analyze CVD of the midchoroid in a large cohort of healthy eyes and found comparable results in CVD values.2 They additionally identified that age and choroidal thickness were significant factors in CVD but did not use SS-OCTA in their study. While most studies in the literature have used en face SS-OCT to analyze CVD, others have also used SS-OCTA.19
Limitations of this study include its retrospective nature and a relatively smaller sample size, though it is unlikely that including additional eyes would have changed the results of the study. Also, only a small area of the choroid (4.5 × 4.5 mm) was analyzed. The basis for our statements that SS-OCTA underpredicts CVD in the inner choroid and overpredicts CVD in the outer choroid is careful qualitative analysis in comparison to en face SS-OCT, though not completely objective as side by side comparison to histology was not possible. In the absence of histology, the true density of the choroidal vessels can only be inferred. Our findings are also applicable only to healthy eyes, as disease may alter which technology is more accurate for which layers in the choroid.
In conclusion, with increasing interest in the use of SS-OCT for the analysis of the choroidal vasculature in chorioretinal disease, and as the CVD becomes more widely used, it is important to understand the current limitations and imperfections in the technology and methodology. Analysis of the choriocapillaris should be performed with SS-OCTA rather than en face SS-OCT, which is limited by projection artifacts in this layer. As an overall measure, CVD as measured by SS-OCTA is comparable to en face SS-OCT in the midchoroid. However, for detailed analysis of the choroidal vasculature, SS-OCTA is more limited by low signal-to-noise ratio related to scattering of light from the RPE. Currently, en face SS-OCT seems to provide more robust visualization, though contrast between choroidal vessel lumen and stroma is suboptimal. Future improvements in SS-OCT and SS-OCTA technology may enable reliable high resolution and contrast visualization of choroidal vessels at all layers.
Acknowledgments
The authors thank William Lo, PhD and Boy Braaf, PhD for their expertise on the technical aspects of optical coherence tomography angiography.
Disclosure: J.C. Wang, None; I. Laíns, None; R.F. Silverman, None; L. Sobrin, None; D.G. Vavvas, None; J.W. Miller, None; J.B. Miller, None
References
- 1.Ferrara D, Waheed NK, Duker JS. Investigating the choriocapillaris and choroidal vasculature with new optical coherence tomography technologies. Prog Retin Eye Res. 2016;52:130–155. doi: 10.1016/j.preteyeres.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 2.Fujiwara A, Morizane Y, Hosokawa M, et al. Factors affecting choroidal vascular density in normal eyes: quantification using en face swept-source optical coherence tomography. Am J Ophthalmol. 2016;170:1–9. doi: 10.1016/j.ajo.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 3.Choi W, Moult EM, Waheed NK, et al. Ultrahigh-speed, swept-source optical coherence tomography angiography in nonexudative age-related macular degeneration with geographic atrophy. Ophthalmology. 2015;122:2532–544. doi: 10.1016/j.ophtha.2015.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zheng F, Gregori G, Schaal KB, et al. Choroidal thickness and choroidal vessel density in nonexudative age-related macular degeneration using swept-source optical coherence tomography imaging. Invest Opthalmology Vis Sci. 2016;57:6256–6264. doi: 10.1167/iovs.16-20161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Laíns I, Wang J, Providência J, et al. Choroidal changes associated with subretinal drusenoid deposits in age-related macular degeneration using swept-source optical coherence tomography. Am J Ophthalmol. 2017;180 doi: 10.1016/j.ajo.2017.05.021. [DOI] [PubMed] [Google Scholar]
- 6.Bakthavatsalam M, Ng DS-C, Lai FH-P, et al. Choroidal structures in polypoidal choroidal vasculopathy, neovascular age-related maculopathy, and healthy eyes determined by binarization of swept source optical coherence tomographic images. Graefes Arch Clin Exp Ophthalmol. 2017;255:935–943. doi: 10.1007/s00417-017-3591-3. [DOI] [PubMed] [Google Scholar]
- 7.Cheung CMG, Yanagi Y, Mohla A, et al. Characterization and differentiation of polypoidal choroidal vasculopathy using swept source optical coherence tomography angiography. Retina. 2017;37:1464–1474. doi: 10.1097/IAE.0000000000001391. [DOI] [PubMed] [Google Scholar]
- 8.Murakami T, Uji A, Suzuma K, et al. In Vivo choroidal vascular lesions in diabetes on swept-source optical coherence tomography. PLoS One. 2016;11:e0160317. doi: 10.1371/journal.pone.0160317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tan K-A, Laude A, Yip V, Loo E, Wong EP, Agrawal R. Choroidal vascularity index - a novel optical coherence tomography parameter for disease monitoring in diabetes mellitus? Acta Ophthalmol. 2016;94:e612–e616. doi: 10.1111/aos.13044. [DOI] [PubMed] [Google Scholar]
- 10.Wang JC, Laíns I, Providência J, et al. Diabetic choroidopathy: choroidal vascular density and volume in diabetic retinopathy with swept-source optical coherence tomography. Am J Ophthalmol. 2017;184:75–83. doi: 10.1016/j.ajo.2017.09.030. [DOI] [PubMed] [Google Scholar]
- 11.Kuroda Y, Ooto S, Yamashiro K, et al. Increased choroidal vascularity in central serous chorioretinopathy quantified using swept-source optical coherence tomography. Am J Ophthalmol. 2016;169:199–207. doi: 10.1016/j.ajo.2016.06.043. [DOI] [PubMed] [Google Scholar]
- 12.Ferrara D, Mohler KJ, Waheed N, et al. En face enhanced-depth swept-source optical coherence tomography features of chronic central serous chorioretinopathy. Ophthalmology. 2014;121:719–726. doi: 10.1016/j.ophtha.2013.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuroda Y, Ooto S, Yamashiro K, et al. Increased choroidal vascularity in central serous chorioretinopathy quantified using swept-source optical coherence tomography. Am J Ophthalmol. 2016;169:199–207. doi: 10.1016/j.ajo.2016.06.043. [DOI] [PubMed] [Google Scholar]
- 14.Wolff B, Basdekidou C, Vasseur V, Sahel J-A, Gaudric A, Mauget-Faÿsse M. “En face” optical coherence tomography imaging in type 2 idiopathic macular telangiectasia. Retina. 2014;34:2072–2078. doi: 10.1097/IAE.0000000000000208. [DOI] [PubMed] [Google Scholar]
- 15.Ferrara D, Mohler KJ, Waheed N, et al. En face enhanced-depth swept-source optical coherence tomography features of chronic central serous chorioretinopathy. Ophthalmology. 2014;121:719–726. doi: 10.1016/j.ophtha.2013.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang Q, Chan S, Yang JY, et al. Vascular density in retina and choriocapillaris as measured by optical coherence tomography angiography. Am J Ophthalmol. 2016;168:95–109. doi: 10.1016/j.ajo.2016.05.005. [DOI] [PubMed] [Google Scholar]
- 17.Zhang Q, Zheng F, Motulsky EH, et al. A novel strategy for quantifying choriocapillaris flow voids using swept-source OCT angiography. Invest Opthalmology Vis Sci. 2018;59:203–211. doi: 10.1167/iovs.17-22953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lane M, Moult EM, Novais EA, et al. Visualizing the choriocapillaris under drusen: comparing 1050-nm swept-source versus 840-nm spectral-domain optical coherence tomography angiography. Invest Opthalmology Vis Sci. 2016;57(9):OCT585–OCT590. doi: 10.1167/iovs.15-18915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nicolò M, Rosa R, Musetti D, Musolino M, Saccheggiani M, Traverso CE. Choroidal vascular flow area in central serous chorioretinopathy using swept-source optical coherence tomography angiography. Invest Opthalmology Vis Sci. 2017;58:2002–2010. doi: 10.1167/iovs.17-21417. [DOI] [PubMed] [Google Scholar]
- 20.Diaz JD, Wang JC, Oellers P, et al. Imaging the deep choroidal vasculature using spectral domain and swept source optical coherence tomography angiography. J Vitreoretin Dis. 2018;2:146–154. doi: 10.1177/2474126418771805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saxena LP. Niblack's binarization method and its modifications to real-time applications: a review. Artif Intell Rev. Jul, 2017. pp. 1–33.
- 22.Uji A, Balasubramanian S, Lei J, Baghdasaryan E, Al-Sheikh M, Sadda SR. Choriocapillaris imaging using multiple en face optical coherence tomography angiography image averaging. JAMA Ophthalmol. 2017;135:1197–1204. doi: 10.1001/jamaophthalmol.2017.3904. [DOI] [PMC free article] [PubMed] [Google Scholar]