Abstract
Background
The existing evidence on the treatment of complicated appendicitis favors conservative treatment rather than acute appendicectomy. Update traditional meta-analysis and consequently cumulative meta-analysis was performed to track the accumulation of evidence over time.
Methods
Studies were identified by a systematic literature search of the EMBASE, PubMed, Cochrane Library and Google Scholar databases. The main outcome measures were duration of the first hospitalization, overall duration of hospitalization, duration of intravenous (IV) antibiotic treatment, overall complications, abdominal/pelvic abscesses, wound infections, re-admissions and unplanned re-operations.
Results
Overall complications, abdominal/pelvic abscesses, wound infections and unplanned procedures were significantly lower in the conservative treatment cohort. In contrast, subgroup analysis of three randomized controlled trials (RCTs) revealed no significant difference in abdominal/pelvic abscesses (odds ratio (OR): 0.46, 95% confidence interval (CI): 0.17 - 1.29, P = 0.14). No significant differences were found in the duration of the first and overall hospitalizations. Of the note, high-quality RCTs demonstrated a shorter hospital stay by 1 day for the laparoscopic appendicectomy cohort compared to conservative treatment (mean difference (MD): -0.99, 95% CI: -1.31 to -0.67, P < 0.0001).
Conclusion
The present meta-analysis demonstrates that a shift in paradigm has begun, with a more widespread use of the laparoscopic approach for the management of complicated appendicitis.
Keywords: Acute appendicitis, Appendiceal or appendicular phlegmon, Appendicular or appendiceal abscess, Complicated appendicitis
Introduction
Acute appendicitis is one of the most common surgical emergencies. The lifetime risk is 8.6% among male individuals and 6.7% among female individuals. In contrast, the risk of undergoing appendicectomy shows an opposite trend, with 12% for male individuals and 23% for female individuals [1]. In the population presenting with acute appendicitis, 3.8-5% may develop complicated appendicitis in the form of an enclosed inflammatory mass, which, on the basis of radiological criteria, can be defined as phlegmon or abscess [2].
There is evidence that the incidence rate of appendicitis presenting with enclosed inflammation is moving towards an increase in trend due to the management of acute appendicitis by antibiotics therapy alone. Using antibiotics as a first-line treatment has demonstrated a 73% success rate, with treatment failures and crossover to surgery at 48 h occurring in half of patients; moreover, the risk of recurrence within 1 year is 50%, which one can consider as a main risk factor for developing complicated appendicitis [3-5].
To date there are no standardized management guidelines for complicated appendicitis. Moreover, a significant heterogeneity has been reported with regard to preferences in appropriate management among consultants and registrars [6, 7].
The most recent meta-analysis published [8] in 2010 showed that there was evidence of significantly fewer overall complications in patients who received conservative treatment as compared to those who underwent immediate appendicectomy. No differences were demonstrated in the duration of first hospitalization, overall duration of hospital stay and duration of intravenous (IV) antibiotics therapy.
The aim of the present study was to estimate the impact of the effect size of new studies on the robustness of the statistical significance of existing meta-analyses comparing acute appendicectomy versus conservative treatment for complicated appendicitis using traditional and cumulative meta-analyses approaches.
Materials and Methods
The PRISMA statement checklist for reporting systematic review and meta-analysis was followed for this study.
Literature search
Using the search terms in both the free text and MESH terms (“laparoscopic or open appendicectomy” or “appendectomy”; “conservative” or “non-surgical treatment” or “management”; “inflammatory” or “appendiceal” or “appendicular mass”; “abscess”; “phlegmon”), a systematic search of the literature published over the last 30 years was performed using the EMBASE, Medline (PubMed), Cochrane Library and Google scholar databases. A gray literature search in the clinicaltrials.gov website was also performed. References of the retrieved articles were checked manually for further studies. Disagreements between the authors were resolved by consensus-based discussions.
Study selection, inclusion and exclusion criteria
Only studies that compared laparoscopic or open appendicectomy versus conservative treatment for complicated appendicitis were included in this study. They should have fulfilled the following criteria: 1) treatment clearly documented as surgical or conservative and indications, inclusion and matching criteria reported for each treatment cohort; 2) report of at least one outcome measure; 3) only the most recent publication included, in the case of multiple publications by the same institution.
Studies on acute uncomplicated appendicitis, diffuse peritonitis and those in which it was impossible to clearly calculate the outcomes were excluded from the analysis.
Data extraction and outcomes
Two reviewers (PG and KK) independently extracted the following summary data for the included studies: name of authors; study design and year of publication; number of patients included in the surgical and conservative arms; duration of the first hospitalization; overall duration of hospitalization; duration of IV antibiotic treatment; overall complications; abdominal/pelvic abscesses; wound infections; re-admissions; and unplanned re-operations.
Definitions
Duration of the first hospitalization included the day of the first admission; overall duration of hospitalization included admissions for complications and interval appendicectomy; duration of IV antibiotic treatment included all IV courses as an inpatient and excluded any oral courses; overall complications and wound infections were defined as superficial or deep, but excluded any abscess formation; abdominal/pelvic abscesses diagnosed after computerized axial tomography (CAT) scan; re-operation was defined as any operation resulting from post-operative complications after acute or interval appendicectomy.
Statistical analysis
The methodological quality of all included studies was assessed using the validated Newcastle-Ottawa scale (NOS) [9]; studies scoring ≥ 7 were considered of high quality. The assessment of randomized controlled trials (RCTs) was based on Cochrane’s criteria, that is, random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and differences in baseline characteristics [10].
Statistical analysis was conducted using both STATA software (version 15; Stata Corp. LP, College Station, TX, USA) and Review Manager 5.3 software (Cochrane Collaboration, Oxford, UK). Heterogeneity was assessed using the I2 test, and cut-off values of 25%, 50% and 75% were considered of low, moderate and high heterogeneity, respectively [11]. Where this occurred, both fixed- and random-effects models were generated, and the conclusions were compared, with the latter used where there were discrepancies. In cases of I2 values less than 25%, fixed-effects models were used throughout.
Dichotomous variables were analyzed based on odds ratio (OR) with 95% confidence intervals (CI). For the outcomes being considered, the reference categories were selected such that OR < 1 favored the acute appendicectomy.
Continuous variables were combined based on both the mean difference (MD) and the standardized mean difference (SMD). For studies that did not report the means and variances of the two groups, these values were estimated from the median, range and the size of sample, using the technique described by Hozo et al, where possible [12].
In all analyses, the point estimate was considered significant at P < 0.05.
Sensitivity analysis
Analyses of both primary and secondary outcomes were calculated using both random- and fixed-effect models, to assess the impact of heterogeneity on the robustness of the conclusions. Cumulative analysis was performed to track the accumulation of evidence and to detect whether the results of the meta-analysis were dominated by a particular study [13].
Results
Search strategy and characteristics of included studies
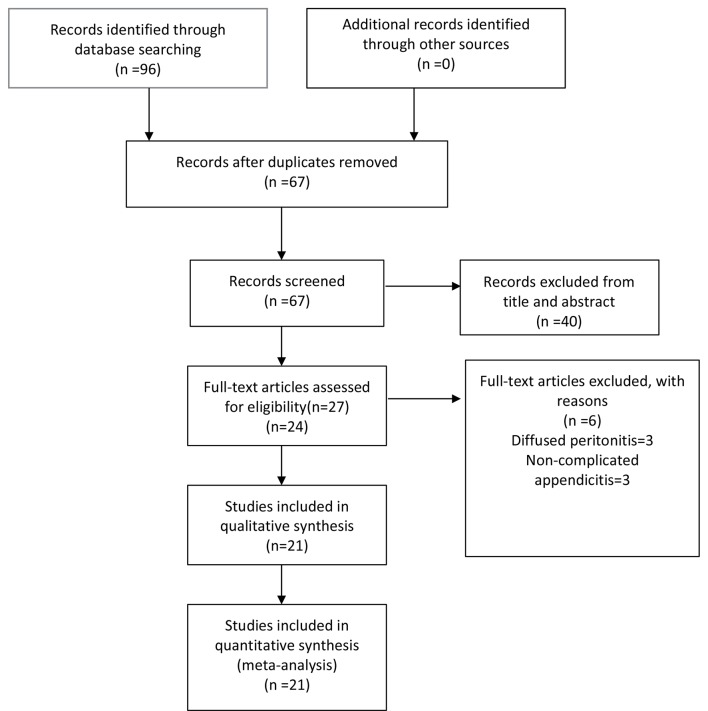
Twenty-one studies were included from an initial pool of 96, comprising a total of 1,864 patients, of which 810 (43.45%) were in the acute appendicectomy arm and 932 (56.55%) were in the conservative treatment arm; 17 were retrospective studies, one prospective, and three RCTs, including 140 patients [14-34]. Overall, 14 out of 21 [14, 15, 21-27, 29-34] studies were classified as high-quality studies (Fig. 1, Table 1). Among the three RCTs, the study by Mentula et al [34] was classified the best, followed by the study by St Peter et al [33], classified as the second best.
Figure 1.
Flow diagram of the search strategy.
Table 1. Characteristics of the Included Studies.
| Authors year study design | AA (n) | CM (n) | Age AA-CM (years ± SD) | Inclusion criteria* | Matching criteria** | NOS |
|---|---|---|---|---|---|---|
| Mentula et al [34], 2015 RCT | 30 | 30 | 45 ± 14 46 ± 13.75 |
2, 3, 5 | 1, 2, 3, 4, 5, 7, 9, 10 | 9 |
| St Peter et al [33], 2010 RCT | 20 | 20 | 10.1 ± 4.2 8.8 ± 4.2, P = 0.31 |
2, 3, 4, 5 | 1, 3, 5, 7, 8 | 9 |
| Aranda-Narvaez et al [32], 2010 RS | 15 | 15 | 35.8 ± 12 35.4 ± 12 |
2, 3, 4, 5 | 1, 2, 3, 4, 6, 7, 8, 9 | 7 |
| Roach et al [31], 2007 RS | 60 | 32 | NR | 1, 3, 4, 5, 6 | 1, 2, 7, 8 | 7 |
| Henry et al [30], 2007 RS | 48 | 48 | 8.5 - 9 | 1, 3, 6 | 1, 2, 7, 8 | 8 |
| Erdogan et al [29], 2005 RS | 19 | 21 | 8 | 1, 3, 4 | 1, 2, 3, 5, 7, 8 | 5 |
| Kumar et al [28], 2004 RCT | 20 | 20 | 31.6 ± 14.6 26 ± 12.4 |
3, 4 | 2 | 5 |
| Ho et al [27], 2004 RS | 27 | 32 | 12 - 11 | 1, 3, 4, 6 | 1, 2, 3, 5, 7, 8 | 9 |
| Brown et al [26], 2003 RS | 36 | 68 | 31 - 35 | 2, 4, 5 | 1, 2, 4, 6, 7, 8 | 7 |
| Samuel et al [25], 2002 PS | 34 | 48 | 7 - 7 | 1, 3, 4, 5 | 1, 2, 3 | 7 |
| Tingstedt et al [24], 2002 RS | 43 | 50 | 42 - 50 | 2, 3, 4, 5 | 1, 2, 3, 6, 7, 8 | 8 |
| Oliak et al [23], 2001 RS | 67 | 88 | 31 - 35 | 2, 3, 4, 5 | 1, 2, 3, 4, 6, 7, 8 | 9 |
| Bufo et al [22], 1998 RS | 46 | 41 | 10 - 11 | 1, 3, 4, 5, 6 | 1, 2, 3, 7, 8 | 8 |
| Handa et al [21], 1997 RS | 8 | 6 | 7 - 8 | 1, 3, 5 | 1, 2, 3, 7 | 7 |
| Hume et al [20], 1995 RS | 78 | 69 | 48 - 43 | 2, 3, 4, 5 | 1, 2 | 6 |
| Gahukambe et al [19], 1993 RS | 7 | 59 | < 12 | 1, 3, 4 | 2 | 5 |
| Hoffmann et al [18], 1991 RS | 19 | 28 | 35 - 37 | 1, 2, 3, 4, 5 | 1, 3 | 4 |
| Lewin et al [17], 1988 RS | 95 | 98 | 49 | 2, 3, 4, 5 | 1, 2, 3 | 4 |
| Gomez-Lorenzo et al [16], 1987 RS | 89 | 106 | 39 - 53 | 1, 2, 3, 4 | 1, 2, 3, 7, 8 | 8 |
| Foran et al [15], 1978 RS | 13 | 30 | 30 - 34 | 2, 3, 4, 5 | 2, 3, 7, 8, 9 | 8 |
| Gastrin et al [14], 1969 RS | 36 | 23 | < 15 | 1, 3, 4, 5 | 1, 2, 3 | 6 |
| Pooled n = 1,864 | 810 (43%) | 932 (57%) | HQ = 14 |
AA: acute appendicectomy; CM: conservative management; RS: retrospective study; RCT: randomized controlled trial; NOS: Newcastle-Ottawa scale; NR: non-reported; HQ: high quality; ASA: American Society of Anesthesiologists. *Inclusion criteria: 1 = pediatric cases, 2 = adults, 3 = clinical symptoms, 4 = appendicular mass, 5 = appendicular abscess, 6 = perforated appendix. **Matching criteria: 1 = sex, 2 = age, 3 = duration of symptoms, 4 = ASA, 5 = body mass index, 6 = heart rate, 7 = white blood cells, 8 = temperature, 9 = C-reactive protein, 10 = size of appendicular mass.
Duration of first and overall hospital stay, duration of intravenous antibiotic treatment and re-operations
There were no evidence of significant differences in the duration of first hospitalization (MD: -0.48, 95% CI: -3.11 - 2.16, P = 0.27; I2 = 98%), overall hospitalization (MD: -0.48, 95% CI: -2.86 - 1.89, P = 0.69; I2 = 99%) or the duration of IV antibiotic treatment and re-operations between the two cohorts (MD: -0.52, 95% CI: -2.42 - 1.38, P = 0.59; I2 = 94% and Peto OR: 1.41, 95% CI: 0.64 - 2.13, P = 0.40; I2 = 80%), respectively (Table 2).
Table 2. Outcomes of Interest.
| Outcome of interest | No. of studies, no. of patients | Statistical method, estimated effect, 95% CI | P value | I2 (%) |
|---|---|---|---|---|
| Duration of first hospitalization [15, 17, 23-27, 30, 34] | 9, 885 | MD: -0.48, 95% CI: -3.11 -2.16 | 0.72 | 98 |
| Overall duration of hospitalization [18, 21, 24-26, 28, 31, 33, 34] | 10, 605 | MD: -0.48, 95% CI: -2.86 -1.89 | 0.69 | 94 |
| Overall duration of hospitalization RCTs [28, 33, 34] | 3, 140 | MD: 1.48, 95% CI: -2.60 -5.57 (RE) MD: -0.94, 95% CI: -1.26 to -0.62 (FE) |
0.48 < 0.001 |
86 86 |
| Overall duration of hospitalization high-quality RCTs [33, 34] | 2, 100 | MD: -0.99, 95% CI: -1.31 to -0.67 (FE) | < 0.001 | 0 |
| Duration of IV antibiotics [22, 24, 25, 27, 34] | 5, 383 | MD: -0.52, 95% CI: -2.42 - 1.38 | 0.59 | 94 |
| Re-operations [14, 16, 20, 22, 34] | 5, 423 | Peto OR: 1.41, 95% CI: 0.64 - 3.13 | 0.40 | 81 |
| Overall complications [14-34] | 20, 1,660 | Peto OR: 2.90, 95% CI: 2.31 - 3.65 | < 0.001 | 78 |
| Abdominal/pelvic abscesses RCTs [33, 34] | 2, 100 | OR: 0.46, 95% CI: 0.17 - 1.29 | 0.14 | 0 |
| Abdominal/pelvic abscesses [14, 16, 17, 23, 26, 30, 31, 32-34] | 11, 1,116 | OR: 3.13, 95% CI: 1.18 - 8.30 | 0.02 | 71 |
| Wound infections [16, 17, 19, 20, 22, 23, 26-28, 30, 32] | 12, 1,094 | OR: 3.95, 95% CI: 1.95 - 8.00 | < 0.001 | 43 |
RCTs: randomized controlled trials; IV: intravenous; MD: mean difference; RE: random-effects; FE: fixed-effects; OR: odds ratio.
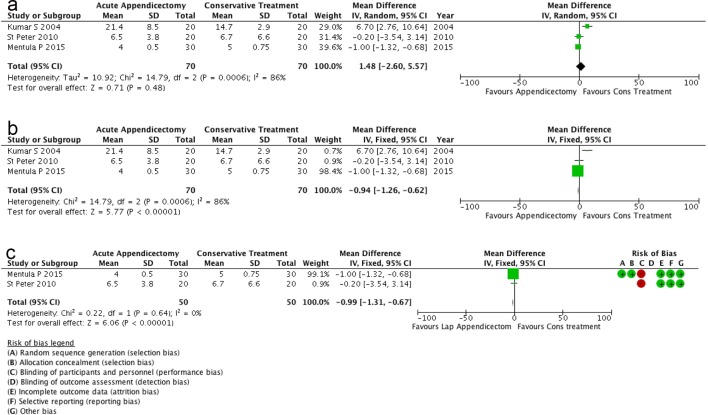
Subgroup analysis of RCT overall duration of hospital stay
There was a discrepancy between the fixed- and random-effects models with regard to overall hospital stay between the two cohorts; the former was (MD: 1.48, 95% CI: -2.60 - 5.57, P = 0.48; I2 = 86%) and the latter was significantly shorter by 1 day (MD: -0.94, 95% CI: 1.26 to -0.62, P < 0.001; I2 = 86%). In addition, in RCTs of high quality, the length of hospital stay was significantly shorter by 1 day as well for the cohort of laparoscopic appendicectomy compared to conservative treatment (MD: -0.99, 95% CI: -1.31 - -0.67, P < 0.001; I2 = 0%) (Fig. 2, Table 2).
Figure 2.
(a) Overall duration of hospital stay of the whole sample. (b) Overall duration of hospital stay of RCTs. (c) Overall duration of hospital stay of the high-quality RCTs.
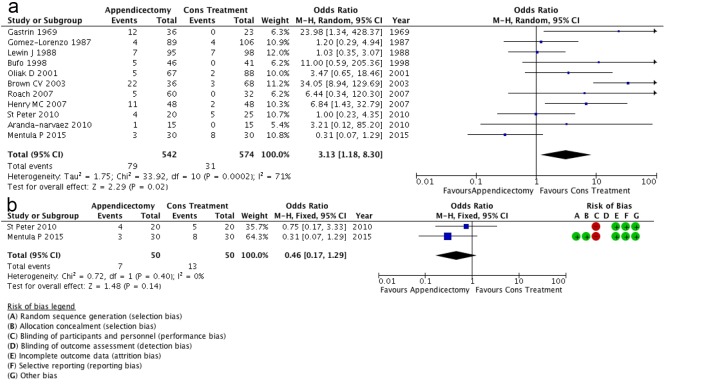
Overall complications, abdominal/pelvic abscesses and wound infections
There was evidence that conservative treatment had a lower incidence rate for overall complications, abdominal/pelvic abscesses and wound infections compared to the surgical approach (OR: 3.16, 95% CI: 1.73 - 5.79, P = 0.0002, I2 = 78%; OR: 3.13, 95% CI: 1.18 - 8.30, P = 0.02, I2 = 71%; OR: 3.95, 95% CI: 1.95 - 8.00, P < 0.001, I2 = 43%), respectively (Fig. 3).
Figure 3.
(a) Abdominal/pelvic abscesses of the whole sample illustrating favor of the conservative treatment. (b) Statistically non-significant studies of St Peter et al [33] and Mentula et al [34] demonstrating an impact of preference for laparoscopic appendicectomy compared to conservative treatment.
Subgroup analysis of RCT abdominal/pelvic abscesses
On the contrary to the retrospective studies, there was no evidence of significant differences between the laparoscopic appendicectomy and conservative treatment cohorts (OR: 0.46, 95% CI: 0.17 - 1.29, P = 0.14; I2 = 0%) (Fig. 3).
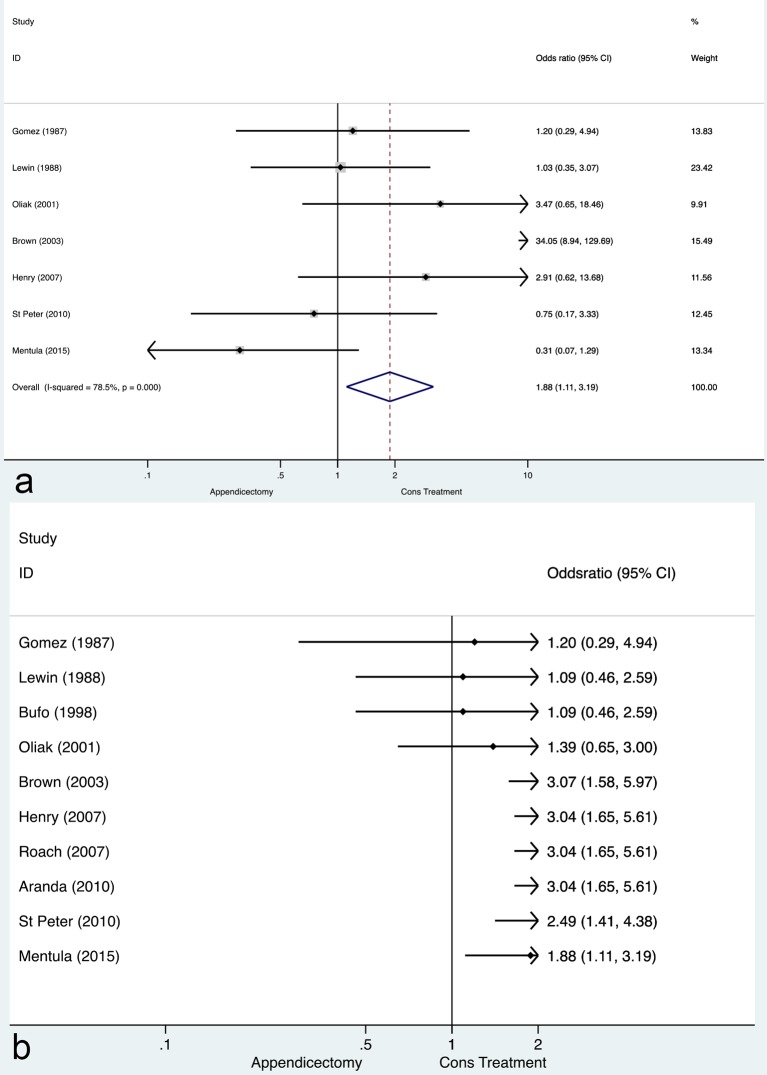
Cumulative analysis
With regard to the outcome of abdominal/pelvic abscesses, the accumulated evidence over the last 30 years can be divided into three periods. From 1987 until 2001, the resulting effect size on the efficacy of conservative treatment was non-significant. The study of Brown et al [26] published in 2003 was a turning point. It actually doubled the effect size on efficacy of the conservative treatment from OR 1.39 (95% CI: 0.65 - 3.00) to OR 3.07 (95% CI: 1.58 - 5.97) and it remained stable until 2010. However, the first RCT published by St Peter et al [33] in 2010 pointed towards an initial reduction in the effect size, and subsequently, the RCT by Mentula et al [34] further reduced the effect size from OR 3.04 (95% CI: 1.65 - 5.61) to OR 1.88 (95% CI: 1.11 - 3.19) (Fig. 4).
Figure 4.
Traditional and cumulative meta-analysis of complicated appendicitis. (a) Traditional meta-analysis; (b) cumulative meta-analysis.
Discussion
The aim of the present study was to track accumulated evidence regarding acute appendicectomy or conservative treatment for complicated appendicitis over time, and to estimate the specific effect of each new study on evidence deduced from a previously published meta-analysis. No significant differences were detected with regard to the duration of the first and overall hospitalization periods or the duration of IV antibiotic treatment. However, RCTs of high quality demonstrated significantly shorter hospital stays, by 1 day, for the laparoscopic appendicectomy arm compared with conservative treatment. The above result was the same for the subgroup including the three RCTs (Fig. 2).
To date evidence derived from the current meta-analysis has demonstrated significantly fewer overall complications, abdominal/pelvic abscesses and wound infections on conservative treatment compared to those in the surgical intervention cohorts. However, no significant difference was demonstrated between laparoscopic appendicectomy and conservative treatment in high-quality RCTs; moreover, the point estimates of effect of both studies favored the laparoscopic appendicectomy procedure. Of the note, this finding demonstrates that the impact of the effect size of RCTs on the existing evidence has triggered shift of paradigm favoring laparoscopic approach.
Cumulative analysis of results from the last 30 years based on the outcome of abdominal/pelvic abscesses defines three periods, as follows. From 1987 to 2001, the effect size of efficacy of the conservative treatment was non-significant. In 2003, the study by Brown et al [26] influenced the effect size, and the efficacy of conservative treatment became statistically significant, which remains valid until now. Finally, after the publication of the two RCTs [33, 34] in 2010, the effect size was further reduced from OR 3.04 (95% CI: 1.65 - 5.61) to OR 1.88 (95% CI: 1.11 - 3.19). The last finding demonstrates start of shift of paradigm on favor of laparoscopic approach.
Summarizing the results, we can describe two contrasting differences between the present meta-analysis and the previous one: first, laparoscopic appendicectomy cohort demonstrated a shorter hospital stay by 1 day, and second, although statistically non-significant, laparoscopic appendicectomy cohort showed a better incidence rate for abdominal/pelvic abscesses (Fig. 3). However, the management of complicated appendicitis remains controversial. Factors that can influence the approach could be the local infrastructure and the established criteria for interventional radiology for drainable abscesses; the specific expertise and skill required for the laparoscopic approach; and the surgeon’s preferences, based on expertise and seniority. The principal limitations of the present study are that it includes mainly retrospective analyses and only three RCTs, of which only two are of high quality. Therefore, the results may have influenced by selection, institutional and national bias.
Future multi-institutional RCT adequately powered with strict selection criteria, predefined outcomes, and a homogenous population, may provide new evidence which would help to shed further light on the management of complicated appendicitis.
Conflict of Interest
None.
Financial Support
None.
Ethical Approval
This study does not contain any studies with human participants or animals performed by any of the authors
References
- 1.Snyder MJ, Guthrie M, Cagle S. Acute Appendicitis: Efficient Diagnosis and Management. Am Fam Physician. 2018;98(1):25–33. [PubMed] [Google Scholar]
- 2.Tannoury J, Abboud B. Treatment options of inflammatory appendiceal masses in adults. World J Gastroenterol. 2013;19(25):3942–3950. doi: 10.3748/wjg.v19.i25.3942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salminen P, Paajanen H, Rautio T, Nordstrom P, Aarnio M, Rantanen T, Tuominen R. et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA. 2015;313(23):2340–2348. doi: 10.1001/jama.2015.6154. [DOI] [PubMed] [Google Scholar]
- 4.Flum DR. Clinical practice. Acute appendicitis—appendectomy or the "antibiotics first" strategy. N Engl J Med. 2015;372(20):1937–1943. doi: 10.1056/NEJMcp1215006. [DOI] [PubMed] [Google Scholar]
- 5.Sallinen V, Akl EA, You JJ, Agarwal A, Shoucair S, Vandvik PO, Agoritsas T. et al. Meta-analysis of antibiotics versus appendicectomy for non-perforated acute appendicitis. Br J Surg. 2016;103(6):656–667. doi: 10.1002/bjs.10147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmed I, Deakin D, Parsons SL. Appendix mass: do we know how to treat it? Ann R Coll Surg Engl. 2005;87(3):191–195. doi: 10.1308/1478708051649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Irfan M, Hogan AM, Gately R, Lowery AJ, Waldron R, Khan W, Barry K. Management of the acute appendix mass: a survey of surgical practice. Ir Med J. 2012;105(9):303–305. [PubMed] [Google Scholar]
- 8.Simillis C, Symeonides P, Shorthouse AJ, Tekkis PP. A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon) Surgery. 2010;147(6):818–829. doi: 10.1016/j.surg.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 9.Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Lossos M, Tugwell P. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- 10.Higgins JPT, Greens S, editors. Cochrane handbook for systematic reviews of interventions. Chichester, UK: John Willey & Son Ltd; 2011. [Google Scholar]
- 11.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sterne JA. Cumulative meta-analysis. The Stata Technical Bulletin. 1998;42:13–16. [Google Scholar]
- 14.Gastrin U, Josephson S. Appendiceal abscess-acute appendectomy or conservative treatment. Acta Chir Scand. 1969;135(6):539–542. [PubMed] [Google Scholar]
- 15.Foran B, Berne TV, Rosoff L. Management of appendicular mass in children. Arch Surg. 1978;113:1144–1145. doi: 10.1001/archsurg.1978.01370220030005. [DOI] [PubMed] [Google Scholar]
- 16.Gomez-Lorenzo E, Dominguez Sanchez J, Octavio de Toledo JM, Alvarez G, Bernadez J, Sierra JA, Dominguez Sanchez P, Vila Rodriguez R. Appendiceal plastron: comparative study of emergency appendicectomy with conservative treatment (195 cases) Rev Esp Enferm Apar Dig. 1987;71:151–155. [PubMed] [Google Scholar]
- 17.Lewin J, Fenyo G, Engstrom L. Treatment of appendiceal abscess. Acta Chir Scand. 1988;154(2):123–125. [PubMed] [Google Scholar]
- 18.Hoffmann J, Rolff M, Lomborg V, Franzmann M. Ultraconservative management of appendiceal abscess. J R Coll Surg Edinb. 1991;36(1):18–20. [PubMed] [Google Scholar]
- 19.Gahukamble DB, Khamage AS, Gahukamble LD. Management of appendicular mass in children. Ann Trop Paediatr. 1993;13(4):365–367. doi: 10.1080/02724936.1993.11747672. [DOI] [PubMed] [Google Scholar]
- 20.Hume T, Nylamo E. Conservative versus operative treatment of appendiceal abscess. Experience of 147 consecutive patients. Ann Chir Gynaecol. 1995;84:33–36. [PubMed] [Google Scholar]
- 21.Handa N, Muramori K, Taguchi S. Early appendectomy versus an interval appendectomy for appendiceal abscess in children. Fukuoka Igaku Zasshi. 1997;88(12):389–394. [PubMed] [Google Scholar]
- 22.Bufo AJ, Shah RS, Li MH, Cyr NA, Hollabaugh RS, Hixson SD. et al. Interval appendicectomy for perforated appendicitis in children. J Laparoendosc Adv Surg Tech. 1998;8:209–214. doi: 10.1089/lap.1998.8.209. [DOI] [PubMed] [Google Scholar]
- 23.Oliak D, Yamini D, Udani VM, Lewis RJ, Arnell T, Vargas H, Schropp KP. et al. Initial non-operative management for periappendiceal abscess. Dis Colon Rectum. 2001;44:956–941. doi: 10.1007/BF02235479. [DOI] [PubMed] [Google Scholar]
- 24.Tingstedt B, Bexe-Lindskog E, Ekelund M, Andersson R. Management of appendiceal masses. Eur J Surg. 2002;168(11):579–582. doi: 10.1080/11024150201680001. [DOI] [PubMed] [Google Scholar]
- 25.Samuel M, Hosie G, Holmes K. Prospective evaluation of nonsurgical versus surgical management of appendiceal mass. J Pediatr Surg. 2002;37(6):882–886. doi: 10.1053/jpsu.2002.32895. [DOI] [PubMed] [Google Scholar]
- 26.Brown CV, Abrishami M, Muller M, Velmahos GC. Appendiceal abscess: immediate operation or percutaneous drainage? Am Surg. 2003;69(10):829–832. [PubMed] [Google Scholar]
- 27.Ho CM, Chen Y, Lai HS, Lin WH, Hsu WM, Chen WJ. Comparison of critical conservative treatment versus emergency operation in children with ruptured appendicitis with tumor formation. J Formos Med Assoc. 2004;103(5):359–363. [PubMed] [Google Scholar]
- 28.Kumar S, Jain S. Treatment of appendiceal mass: prospective, randomized clinical trial. Indian J Gastroenterol. 2004;23(5):165–167. [PubMed] [Google Scholar]
- 29.Erdogan D, Karaman I, Narci A, karaman A, Cavusoglu YH, Aslan MK, Cakmak O. Comparison of two methods for the management of appendicitis mass in children. Pediatr Surg Int. 2005;21:81–83. doi: 10.1007/s00383-004-1334-0. [DOI] [PubMed] [Google Scholar]
- 30.Henry MC, Gollin G, Islam S, Sylvester K, Walker A, Silverman BL, Moss RL. Matched analysis of nonoperative management vs immediate appendectomy for perforated appendicitis. J Pediatr Surg. 2007;42(1):19–23. doi: 10.1016/j.jpedsurg.2006.09.005. discussion 23-14. [DOI] [PubMed] [Google Scholar]
- 31.Roach JP, Partrick DA, Bruny JL, Allshouse MJ, Karrer FM, Ziegler MM. Complicated appendicitis in children: a clear role for drainage and delayed appendectomy. Am J Surg. 2007;194(6):769–772. doi: 10.1016/j.amjsurg.2007.08.021. discussion 772-763. [DOI] [PubMed] [Google Scholar]
- 32.Aranda-Narvaez JM, Gonzalez-Sanchez AJ, Marin-Camero N, Montiel-Casado C, Lopez-Ruiz P, Sanchez-Perez B, Alvarez-Alcalde A. et al. Conservative approach versus urgent appendectomy in surgical management of acute appendicitis with abscess or phlegmon. Rev Esp Enferm Dig. 2010;102(11):648–652. doi: 10.4321/S1130-01082010001100005. [DOI] [PubMed] [Google Scholar]
- 33.St Peter SD, Aguayo P, Fraser JD, Keckler SJ, Sharp SW, Leys CM, Murphy JP. et al. Initial laparoscopic appendectomy versus initial nonoperative management and interval appendectomy for perforated appendicitis with abscess: a prospective, randomized trial. J Pediatr Surg. 2010;45(1):236–240. doi: 10.1016/j.jpedsurg.2009.10.039. [DOI] [PubMed] [Google Scholar]
- 34.Mentula P, Sammalkorpi H, Leppaniemi A. Laparoscopic surgery or conservative treatment for appendiceal abscess in adults? A randomized controlled trial. Ann Surg. 2015;262(2):237–242. doi: 10.1097/SLA.0000000000001200. [DOI] [PubMed] [Google Scholar]