Abstract
Background
Non-consensual removal of condoms, colloquially referred to as ‘stealthing’, is the removal of a condom during sex by a sexual partner when consent has been given for sex with a condom only.
Methods
We conducted a cross-sectional survey to determine how commonly women and men who have sex with men (MSM) attending Melbourne Sexual Health Centre had experienced stealthing, and analysed situational factors associated with the event. Responses were linked to demographic information extracted from patient files.
Results
1189 of 2883 women (41.2%), and 1063 of 3439 MSM (30.9%) attending the clinic during the study period completed the survey. Thirty-two percent of women (95% CI: 29%,35%) and 19% of MSM (95% CI: 17%,22%) reported having ever experienced stealthing. Women who had been stealthed were more likely to be a current sex worker (Adjusted Odds Ratio [AOR] 2.87, 95% CI: 2.01,4.11, p <0.001). MSM who had experienced stealthing were more likely to report anxiety or depression (AOR 2.13, 95% CI: 1.25,3.60, p = 0.005). Both female and male participants who had experienced stealthing were three times less likely to consider it to be sexual assault than participants who had not experienced it (OR 0.29, 95% CI: 0.22,0.4 and OR 0.31, 95% CI: 0.21,0.45 respectively).
Conclusions
A high proportion of women and MSM attending a sexual health service reported having experienced stealthing. While further investigation is needed into the prevalence of stealthing in the general community, clinicians should be aware of this practice and consider integrating this question into their sexual health consultation. Understanding situational factors would assist in the development of preventive strategies, particularly female sex workers and MSM.
Introduction
Non-consensual removal of condoms, colloquially referred to as ‘stealthing’[1] or ‘stealth-breeding’ [2], refers to the practice of a sexual partner covertly removing a condom, when consent has been given for condom protected sex only [1]. Condoms are used as a primary preventative method of protecting against sexually transmitted infections (STI), human immunodeficiency virus (HIV) and pregnancy, being 80 to 98.6% effective [3–5]. Stealthing may result in the transmission of STIs, HIV, or unintended pregnancy, and could have significant personal and public health implications.
Studies of undergraduate students have found consent for sexual intercourse to be mostly communicated through non-verbal means [6, 7], with consent for sexual intercourse often implied in the process of asking for or applying a condom [6]. Brodsky has argued that condom removal without mutual agreement violates consent to sex [1].
In young adult heterosexual relations, it is common for male partners to engage in condom resistance tactics [8]. Several studies have identified stealthing as a method of birth control sabotage [9, 10], as well as a means of intentional HIV transmission [11]. Anecdotal research by Brodsky focusing on heterosexual and heteronormative relations, and theoretical research by Brennan focusing on condom-less sex between men, argue these are not the primary motivators for this act [1, 2].
In spite of public interest in stealthing, there are no scientific articles that investigate how common it is, who is most at risk, and the outcomes for those who report being stealthed. We aimed to investigate the proportion of sexual health centre patients reporting nonconsensual removal of condoms: 1) among heterosexual women and 2) among men who have sex with men, as well as associated risk factors. For the purpose of this study, ‘stealthing’ was defined as condom removal without consent, where consent to sex was conditional upon use of a condom.
Methods
Population and setting
This was a cross-sectional questionnaire-based study conducted amongst women and gay and other men who have sex with men (MSM) attending the Melbourne Sexual Health Centre (MSHC) in Victoria, Australia, between the 22nd December 2017 and the 22nd February 2018. MSHC is the largest public sexual health service in Victoria, Australia. The centre provides around 50,000 consultations every year, 37% with women and 36% with MSM [12]. Clinic attendees routinely complete a computer assisted self-interview (CASI) about their sexual history prior to seeing a triage nurse.
Study measurement
Women and MSM presenting to MSHC, aged 18 or over, were invited to complete an electronic questionnaire containing questions about stealthing after completing CASI. Participants read a patient information and consent form which detailed the nature of the survey, and patients could only commence the questionnaire after ticking a box stating ‘Yes- willing to help’. Due to the potential of the questionnaire to cause distress when recalling the stealthing event, the participant information included advertisement of free counselling services available at MSHC and elsewhere. The Alfred Hospital Ethics Committee approved the study (number 494/17).
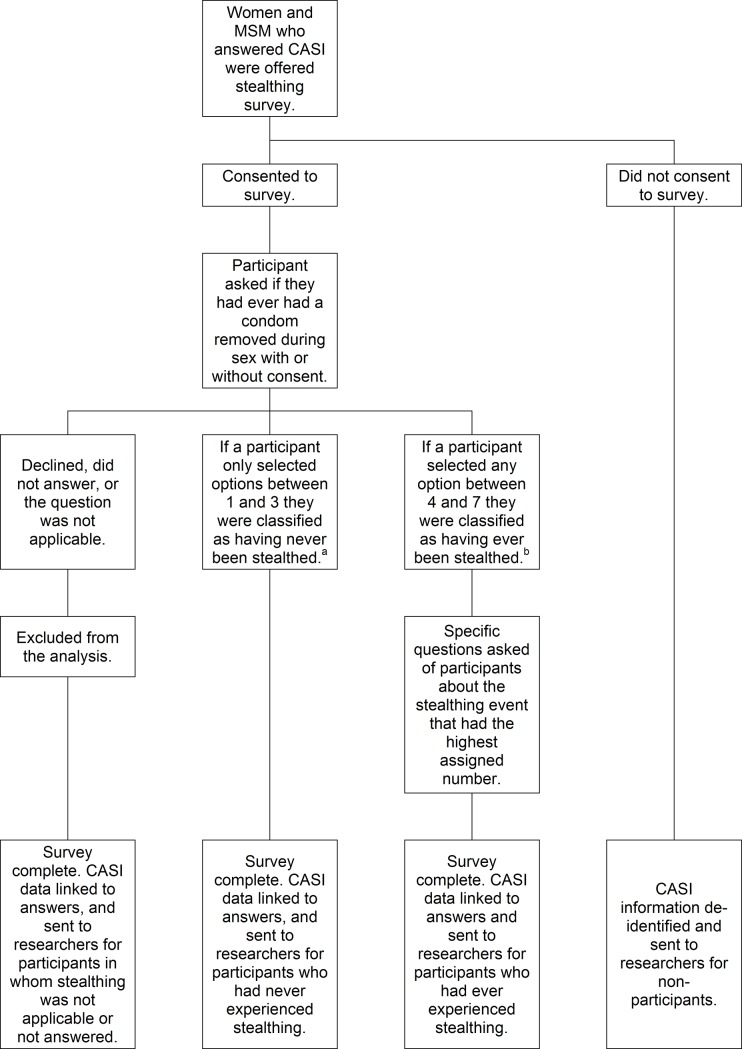
Age, number of sexual partners, and HIV status were extracted electronically from routinely collected clinic records for respondents and non-respondents, de-identified for non-respondents, and linked to questionnaire responses for respondents (Fig 1).
Fig 1. Possible pathways for patients offered the survey, and the classification for analysis of nonconsensual condom removal.
Abbreviations: MSM = men who have sex with men; CASI = computer assisted self-interviewing. aParticipants were classified as never having experienced stealthing if they responded either: 1) they had never had a condom removed during sex, 2) that a condom had been removed with permission, or 3) that a condom was removed without permission but they willingly continued sex. bParticipants were deemed to have experienced stealthing if they reported: 4) condom removal without permission and sex continued unwillingly, 5) condom removal without permission and sex was discontinued, 6) condom removal during sex but they did not realise until afterwards, or 7) the condom was never put on despite being requested.
The questionnaire asked whether the participant had ever had a condom removed during sex with or without permission and at what point the participant noticed. Participants could choose from a hierarchy of seven responses describing the circumstances. Multiple responses were allowed for those reporting multiple occurrences, and there was no time limit applied to the reported event. Participants were deemed not to have experienced stealthing if they responded either: 1) they had never had a condom removed during sex, 2) that a condom had been removed with permission, or 3) that a condom was removed without permission but they willingly continued sex. Participants were deemed to have experienced stealthing if they reported: 4) condom removal without permission and sex continued unwillingly, 5) condom removal without permission and sex was discontinued, 6) condom removal during sex but they did not realise until afterwards, or 7) the condom was never put on despite being requested. If a participant only selected options between 1 and 3 they were classified as never having been stealthed. If a participant selected any option between 4–7, regardless of whether they had also selected options between 1 and 3, they were classified as ever having been stealthed (Fig 1).
Participants who reported stealthing were asked further questions about the specific event (Fig 1). Participants who had selected multiple options were asked about the incident with the highest assigned number. For instance if they reported several stealthing events with differing scenarios and selected both response 4 and 5, then specific questions were asked about “event 5” only–i.e. condom removal without permission and sex was discontinued. Questions included: when the incident occurred, how long they had known the partner, how they would describe the relationship, where they had met, whether either person had been using drugs or alcohol, whether the event was reported to the police, and what they perceived were the consequences of the condom removal. All respondents were asked whether they considered the removal of a condom without consent to be sexual assault.
Statistical analysis
All analyses were performed using Stata IC version 14. MSM who reported only insertive anal sex and no receptive anal sex while completing CASI were excluded from the dataset prior to analysis of questionnaire responses, as experiencing stealthing was considered unlikely if the male was only the insertive partner. Risk factors for experiencing stealthing in women and MSM were not compared to each other as they are different populations. Univariable and multivariate analyses were performed to determine the differences in demographics between non-respondents and respondents, and the differences between those who had and had not experienced stealthing. Variables were included in multivariate models if the p-value was ≤0.1; if correlated, the variable most strongly associated with the outcome was used. Models were built in a backward-stepwise fashion, using the likelihood ratio test to determine the significance of the contribution of each variable. Ninety-five percent binomial confidence intervals (CIs) were calculated for all proportions. We assumed 100 patients would complete the survey each week and estimated 2% would report ever being stealthed. The 95% confidence interval around an estimated 2% prevalence of stealthing after six weeks (600 responses) would be 1.0%, 3.5%.
Results
During the study period, 2883 women and 3439 MSM attended the clinic, of whom 1189 women (41%, 95%CI: 39%,43%) and 1063 MSM (31%, 95%CI: 29%,32%) completed the survey (classified as respondents).
Female respondents were more likely than non-respondents to have had sex overseas in the last twelve months (adjusted odds ratio [AOR] 1.49, 95% CI: 1.26,1.77, p<0.001) and were less likely to be a current sex worker (AOR 0.78, 95% CI: 0.63,0.96, p = 0.02) (Table 1). Compared to MSM non-respondents, the men who responded were more likely to have had sex overseas in the last twelve months (AOR 1.70, 95% CI: 1.37,2.11, p<0.001), and were less likely to be HIV positive (AOR 0.60, 95% CI: 0.38,0.95, p = 0.029) (Table 1).
Table 1. Demographics and epidemiological features of respondents versus non-respondents to survey on rates of non-consensual removal of condoms (stealthing) in a STI clinic (N = 6322).
| Female non-respondents n = 1694 (%; 95% CI) or median [range] | Female respondents n = 1189 (%; 95% CI) or median [range] | Unadjusted Odds Ratio (95% CI) | p-value | Adjusted Odds Ratioa (95% CI) | p-value | ||||||
| Age | 27 | [16–74] | 26 | [18–64] | |||||||
| Employment | |||||||||||
| Employed | 958 | (60; 57,62) | 689 | (60; 57,62) | 1 | ||||||
| Not in the labour forceb | 641 | (40; 38,43) | 467 | (40; 38,43) | 1.01 | (0.87,1.18) | 0.87 | ||||
| Aboriginal and/or Torres Strait Islander peoples | |||||||||||
| No | 1479 | (99; 98,99) | 1074 | (99; 98,99) | 1 | ||||||
| Yes | 16 | (1; 0,2) | 14 | (1; 1,2) | 1.20 | (0.59,2.48) | 0.613 | ||||
| Sex overseas | |||||||||||
| No | 817 | (60; 57,62) | 485 | (48; 45,52) | 1 | 1 | |||||
| Yes | 552 | (40; 38,43) | 517 | (52; 48,55) | 1.58 | (1.35,1.86) | <0.001 | 1.49 | (1.26,1.77) | <0.001 | |
| Injecting drug use | |||||||||||
| Never injected | 1420 | (98; 97,99) | 1023 | (98; 97,99) | 1 | ||||||
| Ever injected | 26 | (2; 1,3) | 22 | (2; 1,3) | 1.17 | (0.66,2.08) | 0.582 | ||||
| Current sex worker | |||||||||||
| No | 1095 | (76; 74,78) | 856 | (82; 79,84) | 1 | 1 | |||||
| Yes | 348 | (24; 22,26) | 191 | (18; 16,21) | 0.70 | (0.58,0.86) | <0.001 | 0.78 | (0.63,0.96) | 0.020 | |
| Condom Use in the last 3mo with male partners | |||||||||||
| Not always | 1014 | (83; 81,85) | 765 | (82; 80,85) | 1 | ||||||
| Always | 204 | (17; 15,19) | 163 | (18; 15,20) | 1.06 | (0.84,1.33) | 0.619 | ||||
| Number of male sexual partners in the last 3mo | 1 | [0–50] | 1 | [0–15] | |||||||
| Male non-respondents n = 2376 (%; 95% CI) or median [range] | Male respondents n = 1063 (%; 95% CI) or median [range] | Unadjusted Odds Ratio (95% CI) | p-value | Adjusted Odds Ratioc (95% CI) | p-value | ||||||
| Age | 30 | [16–82] | 30 | [18–75] | |||||||
| Employment | |||||||||||
| Employed | 1480 | (67; 65,69) | 644 | (64; 61,67) | 1 | ||||||
| Not in the labour forceb | 742 | (33; 31,35) | 361 | (36; 33,39) | 1.12 | (0.96,1.31) | 0.161 | ||||
| Aboriginal and/or Torres Strait Islander peoples | |||||||||||
| No | 2114 | (99; 98,99) | 978 | (99; 99,100) | 1 | 1 | |||||
| Yes | 26 | (1; 1,2) | 5 | (1; 0,1) | 0.42 | (0.16,1.09) | 0.073 | 0.64 | (0.21,1.97) | 0.441 | |
| Sex overseas | |||||||||||
| No | 1365 | (70; 69,72) | 542 | (61; 58,64) | 1 | 1 | |||||
| Yes | 587 | (30; 28,32) | 345 | (39; 36,42) | 1.48 | (1.25,1.75) | <0.001 | 1.70 | (1.37,2.11) | <0.001 | |
| Injecting drug use | |||||||||||
| Never injected | 2048 | (96; 96,97) | 914 | (97; 96,98) | 1 | ||||||
| Ever injected | 75 | (4; 3,4) | 28 | (3; 2,4) | 0.84 | (0.55,1.3) | 0.428 | ||||
| Current sex worker | |||||||||||
| No | 2126 | (>99; 99,100) | 933 | (99; 98,99) | 1 | 1 | |||||
| Yes | 9 | (<1; 0,1) | 10 | (1; 1,2) | 2.53 | (1.03,6.25) | 0.044 | 2.72 | (0.97,7.59) | 0.057 | |
| Condom Use in the last 3mo with male partners | |||||||||||
| Not always | 1379 | (74; 72,76) | 616 | (71; 68,74) | 1 | ||||||
| Always | 492 | (26; 24,29) | 246 | (29; 26,32) | 1.12 | (0.93,1.34) | 0.220 | ||||
| HIV status | |||||||||||
| Negative | 1279 | (91; 90,93) | 558 | (95; 92,96) | 1 | 1 | |||||
| Positive | 119 | (9; 7,10) | 32 | (5; 4,8) | 0.62 | (0.41,0.92) | 0.019 | 0.61 | (0.38,0.97) | 0.038 | |
| Use of prep | |||||||||||
| No | 1844 | (81; 79,82) | 861 | (83; 81,85) | 1 | ||||||
| Yes | 436 | (19; 18,21) | 174 | (17; 15,19) | 0.85 | (0.70,1.04) | 0.112 | ||||
| Number of male sexual partners in the last 3mo | 3 | [0–100] | 3 | [0–140] | |||||||
Abbreviations: n = number; CI = confidence interval; mo = months; HIV = human immunodeficiency virus; PrEP = HIV pre-exposure prophylaxis
aAdjusted model for females includes: sex overseas and current sex worker
bNot in the labour force includes both those who are unemployed and/or students
cAdjusted model for males includes: Aboriginal and/or Torres Strait Islander peoples, sex overseas, current sex worker and HIV status.
Data missing for: <5% of PrEP data; <5%-10% of employment data; 5–15% of Aboriginal and/or Torres Strait Islander peoples data; 10–15% of current sexworker data; 10%-20% of sex overseas data and injecting drug use data; 15- ≥20% of condom use data; and >20% of HIV data. Proportions are calculated using available data.
Of the 1189 women and 1063 MSM who consented to the survey and answered the first question: 60 (5%) women and 64 men (6%) declined to answer whether they had experienced stealthing, 45 (4%) women and 37 (3%) men deemed the question to be not applicable to them i.e. they never used condoms, or did not engage in penetrative sex with men and 90 (8%) men were removed from the analysis, as they had only reported insertive anal sex and not reported receptive anal sex in CASI (Table 2).
Table 2. Reported events of non-consensual removal of condoms (stealthing) amongst patients presenting to a STI clinic (N = 2252)a.
| Female respondents n = 1189 (%; 95% CI) | Male respondents n = 1063 (%; 95% CI) | ||||
|---|---|---|---|---|---|
| Classified as not experiencing ‘stealthing’ | |||||
| Never stealthed | 420 | (35; 33,38) | 496 | (47; 44,50) | |
| Condom removed w permission | 455 | (38; 35,41) | 315 | (30; 27,32) | |
| Condom removed w/o permission but continued willingly | 104 | (9; 7,10) | 77 | (7; 6,9) | |
| Classified as experiencing ‘stealthing’ | |||||
| Condom removed w/o permission, and continued unwillingly | 108 | (9; 8,11) | 52 | (5; 4,6) | |
| Condom removed w/o permission, and stopped | 135 | (11; 10,13) | 65 | (6; 5,8) | |
| Condom removed w/o permission, but didn't realise until afterwards | 147 | (12; 11,14) | 60 | (6; 4,7) | |
| Condom never put on but had been requested | 84 | (7; 6,9) | 41 | (4; 3,5) | |
| Removed from further analysis | |||||
| Not applicableb | 45 | (4; 3,5) | 127 | (12; 10,14) | |
| Decline answer | 60 | (5; 4,6) | 64 | (6; 5,8) | |
Abbreviations: n = number; CI = confidence interval; w = with; w/o = without.
aPatients could select multiple options, to report multiple events occurring, i.e. events are not mutually exclusive, therefore percentages do not sum to 100. Percentages represent the proportion of participants who have reported the event. If reporting multiple events, patients were classified in the analysis based off the highest numbered event they reported, if 1 is Never and 7 is ‘Condom never put on even though requested’.
bNot applicable refers to patients who have not/do not engaged in penetrative penile sex, includes 97 MSM who responded to survey but reported no receptive anal sex and 30 who selected not applicable.
Three hundred and forty-six of the remaining 1084 women (32%, 95% CI: 29%,35%) and 168 of the remaining 872 MSM (19%, 95% CI: 17%,22%) reported having ever experienced stealthing (Table 3). Of those who had experienced stealthing, forty-two women (12%, 95% CI: 9%,16%) and 23 MSM (14%, 95% CI: 9%,20%) presented to the clinic on the day of the questionnaire following a reported stealthing incident (Table 4).
Table 3. Risk factors associated with non-consensual removal of condoms (stealthing) in patients presenting to a STI clinic (N = 2042).
| Womenwho have not had been stealthed n = 738 (%; 95% CI) or median [range] | Women who have have been stealthed n = 346 (%; 95% CI) or median [range] | Unadjusted Odds Ratio (95% CI) | p-value | Adjusted Odds Ratio (95% CI)a | p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 26 | [18–58] | 26 | [18–55] | |||||||
| Number of male sexual partners in the last 3mo | 2 | [0–15] | 1 | [0–15] | |||||||
| Employmentb | |||||||||||
| Employed | 439 | (61; 57,65) | 189 | (56; 51,62) | 1 | ||||||
| Not in the labour force | 281 | (39; 35,43) | 146 | (44; 38,49) | 1.21 | (0.93,1.57) | 0.161 | ||||
| Education level | |||||||||||
| Did not complete high school | 18 | (2; 1,4) | 13 | (4; 2,6) | 1 | ||||||
| High school/Certificate/Diploma | 238 | (33; 29,36) | 134 | (39; 34,45) | 0.78 | (0.37,1.64) | 0.512 | ||||
| University degree | 475 | (65; 61,68) | 195 | (57; 52,62) | 0.57 | (0.35,1.47) | 0.131 | ||||
| Aboriginal and/or Torres Strait Islander peoples | |||||||||||
| No | 672 | (99; 98,99) | 319 | (98; 96,99) | 1 | ||||||
| Yes | 8 | (1; 1,2) | 5 | (2; 1,4) | 1.31 | (0.43,4.06) | 0.632 | ||||
| Australian/New Zealander | |||||||||||
| No | 441 | (63; 59,66) | 166 | (51; 45,56) | 1 | ||||||
| Yes | 264 | (37; 34,41) | 160 | (49; 44,55) | 1.61 | (1.23,2.09) | <0.001 | 1.26 | (0.94,1.70) | 0.122 | |
| Current sex worker | |||||||||||
| No | 573 | (87; 85,90) | 215 | (71; 65,76) | 1 | ||||||
| Yes | 83 | (13; 10,15) | 89 | (29; 24,35) | 2.86 | (2.04,4.01) | <0.001 | 2.87 | (2.01,4.11) | <0.001 | |
| Injecting drug use | |||||||||||
| Never injected | 644 | (98; 97,99) | 295 | (97; 95,99) | 1 | ||||||
| Ever injected | 11 | (2; 1,3) | 8 | (3; 1,5) | 1.59 | (0.63,3.99) | 0.325 | ||||
| Sex overseas | |||||||||||
| No | 303 | (47; 44,51) | 136 | (47; 41,53) | 1 | ||||||
| Yes | 335 | (53; 49,56) | 153 | (53; 47,59) | 1.02 | (0.77,1.34) | 0.903 | ||||
| Use other contraceptives in addition to condomsc | |||||||||||
| No | 293 | (46; 42,50) | 112 | (47; 40,53) | 1 | ||||||
| Yes | 339 | (54; 50,58) | 128 | (53; 47,60) | 0.94 | (0.733,1.33) | 0.936 | ||||
| MSM who have not been stealthed n = 704 (%; 95% CI) or median [range] | MSM who have been stealthed n = 168 (%, 95% CI) or median [range] | Unadjusted Odds Ratio (95% CI) | p-value | Adjusted Odds Ratio (95% CI)d | p-value | ||||||
| Age | 30 | [18–75] | 29 | [18–58] | |||||||
| Number of male sexual partners in the last 3mo | 3 | [0–140] | 3 | [0–100] | |||||||
| Employment | |||||||||||
| Employed | 435 | (65; 61,69) | 98 | (61; 53,68) | 1 | ||||||
| Not in the labour force | 232 | (35; 31,39) | 63 | (39; 32,47) | 1.20 | (0.85,1.72) | 0.302 | ||||
| Education level | |||||||||||
| Did not complete high school | 24 | (3; 2,5) | 7 | (4; 2,8) | 1 | ||||||
| High school/Certificate/Diploma | 183 | (26; 23,30) | 34 | (20; 14,27) | 0.64 | (0.25,1.60) | 0.336 | ||||
| University degree | 494 | (70; 67,74) | 127 | (76; 68,82) | 0.88 | (0.37,2.09) | 0.775 | ||||
| Aboriginal and/or Torres Strait Islander peoples | |||||||||||
| No | 701 | (100; 99,100) | 166 | (99; 97,100) | 1 | ||||||
| Yes | 2 | (0; 0,1) | 1 | (1; 0,3) | 2.11 | (0.19,23.42) | 0.543 | ||||
| Australian/New Zealander | |||||||||||
| No | 343 | (50; 46,54) | 83 | (49; 42,57) | 1 | ||||||
| Yes | 342 | (50; 46,54) | 85 | (51; 43,58) | 1.03 | (0.73,1.44) | 0.877 | ||||
| Current sex worker | |||||||||||
| No | 622 | (99; 98,100) | 151 | (99; 95,100) | 1 | ||||||
| Yes | 5 | (1; 0,2) | 2 | (1; 0,5) | 1.65 | (0.32,8.57) | 0.553 | ||||
| Injecting drug use | |||||||||||
| Never injected | 611 | (97; 96,98) | 145 | (96; 92,99) | 1 | ||||||
| Ever injected | 18 | (3; 2,4) | 6 | (4; 1,8) | 1.4 | (0.55,3.60) | 0.480 | ||||
| Sex overseas | |||||||||||
| No | 354 | (60; 56,64) | 82 | (57; 49,66) | 1 | ||||||
| Yes | 237 | (40; 36,44) | 61 | (43; 34,51) | 1.11 | (0.77,1.61) | 0.577 | ||||
| HIV status | |||||||||||
| No | 375 | (95; 93,97) | 96 | (2; 85,97) | 1 | ||||||
| Yes | 19 | (5; 3,7) | 8 | (8; 3,15) | 1.64 | (0.70,3.87) | 0.255 | ||||
| Use of prep | |||||||||||
| No | 582 | (84; 81,87) | 126 | (78; 71,84) | 1 | 1 | |||||
| Yes | 110 | (16; 13,19) | 35 | (22; 16,29) | 1.47 | (0.96,2.25) | 0.077 | 1.16 | (0.70,1.92) | 0.567 | |
| Drugs use with anal sex w/o a condom in the last 12moe | |||||||||||
| No | 222 | (58; 53,63) | 58 | (55; 45,64) | 1 | ||||||
| Yes | 162 | (42; 37,47) | 48 | (45; 36,55) | 1.13 | (0.74,1.75) | 0.569 | ||||
| Drunk during anal sex w/o a condom in the last 12moe | |||||||||||
| No | 219 | (57; 52,62) | 53 | (50; 41,60) | 1 | ||||||
| Yes | 166 | (43; 38,48) | 52 | (50; 40,59) | 1.29 | (0.84,1.99) | 0.242 | ||||
| Anal sex w/o a condom with known HIV positive in the last 12moe | |||||||||||
| No | 319 | (83; 79,87) | 83 | (82; 73,89) | 1 | ||||||
| Yes | 65 | (17; 13,21) | 18 | (18; 11,27) | 1.06 | (0.60,1.89) | 0.832 | ||||
| Anal sex w/o a condom with someone of unknown HIV status in the last 12moe | |||||||||||
| No | 189 | (50; 45,55) | 39 | (38; 29,48) | 1 | 1 | |||||
| Yes | 190 | (50; 45,55) | 63 | (62; 52,71) | 1.61 | (1.03,2.51) | 0.038 | 1.51 | (0.96,2.39) | 0.075 | |
| Self-reported health issues, such as anxiety or depression, which may have affected your decision to use condoms for anal sex?e | |||||||||||
| No | 318 | (85; 81,89) | 74 | (73; 63,81) | 1 | 1 | |||||
| Yes | 55 | (15; 11,19) | 28 | (27; 19,37) | 2.19 | (1.30,3.68) | 0.003 | 2.13 | (1.25,3.6) | 0.005 | |
Abbreviations: n = number; CI = confidence interval; mo = months; MSM = men who have sex with men; HIV = human immunodeficiency virus; PrEP = HIV pre-exposure prophylaxis; w/o = without
aAdjusted model for females includes: Australian and current sex worker
bNot in the labour force includes both those who are unemployed and/or students
cWomen who reported not using contraception due to pregnancy were excluded (2 females who did not have condoms removed, and 10 who did).
dAdjusted model for males includes: use of prep, condom use with someone of uncertain HIV status, health issues (anxiety & depression) affecting decisions to use condoms.
eThese questions were asked only to patients who had reported unprotected anal sex since their last HIV test as part of their routine computer assisted self-interviewing (CASI).
Data missing for: <5% of employment data, education data and PrEP data; <5%-10% of Aboriginal and/or Torres Strait Islander peoples data and Australian data; 10%-15% of injecting drug use data and current sex worker data, 10%-20% sex overseas data; 10- ≥20% contraception data; and ≥20% of HIV status and questions on issues affecting decisions to use condoms. Proportions are calculated using available data.
Table 4. Situational factors surrounding non-consensual removal of condoms (stealthing) reported by patients presenting to a STI clinic (N = 523).
| Women n = 346 (%; 95% CI) |
MSM n = 168 (%; 95% CI) |
||||
|---|---|---|---|---|---|
| When the incident occurred | |||||
| Here today for this reason | 42 | (12; 9,16) | 23 | (14; 9,20) | |
| In the last 3mo | 59 | (17; 13,22) | 20 | (12; 7,18) | |
| 3–12 mo ago | 78 | (23; 18,28) | 35 | (21; 15,28) | |
| More than 12 months ago | 120 | (35; 30,40) | 78 | (46; 39,54) | |
| More than 1 occasion | 43 | (13; 9,17) | 12 | (7; 4,12) | |
| Relationship | |||||
| Did not know him well | 101 | (30; 25,36) | 102 | (61; 54,69) | |
| Friend | 33 | (10; 7,14) | 10 | (6; 3,11) | |
| Friend with benefits/ Sex buddy | 51 | (15; 12,20) | 30 | (18;13,25) | |
| Casually dating | 54 | (16; 12,21) | 22 | (13; 8,19) | |
| Relationship | 25 | (8; 5,11) | 2 | (1; 0,4) | |
| Client (of sex worker) | 69 | (21; 16,25) | 0 | (0; 0,2)a | |
| Relationship duration | |||||
| Less than a day (<24hrs) | 126 | (38; 33,44) | 85 | (52; 44,59) | |
| One day to one month | 95 | (29; 24,34) | 39 | (24; 17,31) | |
| More than one month | 107 | (33; 28,28) | 41 | (25; 18,32) | |
| Met through | |||||
| Smartphone dating app/Internet | 64 | (20; 15,24) | 110 | (67; 59,74) | |
| (Gay) bar or party | 50 | (15; 12,20) | 20 | (12; 8,18) | |
| Gay sauna, beats of SOPV, sex party | 2 | (1; 0,2) | 24 | (15; 10,21) | |
| Friend, or friend of friend | 94 | (29; 24,34) | 6 | (4; 1,8) | |
| Co-workers | 22 | (7; 4,10) | 3 | (2; 0,5) | |
| Sex work | 76 | (23; 19,28) | 0 | (0; 0,2)a | |
| Travel | 15 | (5; 3,7) | 0 | (0; 0,2)a | |
| Other (café, park etc.) | 4 | (1; 0,3) | 1 | (1; 0,3) | |
| Drugs used by partnerbc | |||||
| None | 75 | (27; 22,33) | 63 | (53; 44,62) | |
| Alcohol | 188 | (68; 62,73) | 48 | (40; 31,50) | |
| Cannabis/marijuana/hash | 28 | (10; 7,14) | 4 | (3; 1,8) | |
| Ecstasy | 12 | (4; 2,7) | 4 | (3; 1,8) | |
| Speed/ice/meth | 5 | (2; 1,4) | 6 | (5; 2,11) | |
| GHB | 2 | (1; 0,3) | 3 | (2; 1,7) | |
| Cocaine | 10 | (4; 2,7) | 3 | (2; 1,7) | |
| Heroin | 1 | (<1; 0,2) | 0 | (0; 0,3)a | |
| Other | 1 | (<1; 0,2) | 3 | (2; 1,7) | |
| Drugs used by respondentbd | |||||
| None | 135 | (41; 36,47) | 87 | (54; 46,62) | |
| Alcohol | 186 | (57; 51,62) | 65 | (41; 33,49) | |
| Cannabis/marijuana/hash | 21 | (6; 4,10) | 3 | (2; 0,5) | |
| Ecstasy | 9 | (3; 1,5) | 4 | (3; 1,6) | |
| Speed/ice/meth | 5 | (2; 0,4) | 8 | (5; 2,9) | |
| GHB | 2 | (1; 0,2) | 3 | (2; 0,5) | |
| Cocaine | 8 | (2; 1,5) | 4 | (3; 1,6) | |
| Heroin | 1 | (<1; 0,2) | 0 | (0; 0,2)a | |
| Other | 0 | (0; 0,1)a | 4 | (3; 1,6) | |
| Condom removal discussed with partner | |||||
| No | 128 | (39; 33,44) | 74 | (45; 37,52) | |
| Yes | 204 | (61; 56,67) | 92 | (55; 48,63) | |
| Consequences of condom removalb | |||||
| None | 85 | (25; 21,30) | 62 | (38; 30,46) | |
| Emotional stress | 190 | (56; 51,62) | 86 | (52; 45,60) | |
| Caught an STI | 26 | (8; 5,11) | 9 | (5; 3,10) | |
| Contracted HIV | 2 | (1; 0,2) | 3 | (2; 0,5) | |
| Fight | 49 | (14; 11,19) | 15 | (9; 5,15) | |
| Relationship broke up | 30 | (9; 6,12) | 6 | (4; 1,8) | |
| Other | 42 | (12; 9,16) | 12 | (7; 4,12) | |
| Reported to the police | |||||
| No | 336 | (99; 97,100) | 163 | (98; 95,100) | |
| Yes | 3 | (1; 0,3) | 3 | (2; 0,5) | |
Abbreviations: n = number; CI = confidence interval; MSM = men who have sex with men; mo = months; SOPV = sex on premises venue; GHB = Gamma-hydroxybutyrate; STI = sexually transmitted infection; HIV = human immunodeficiency virus
aone-sided, 97.5% confidence interval
bPatients could select multiple options, to report multiple events occurring, i.e. events are not mutually exclusive, therefore percentages do not sum to 100. Percentages represent the proportion of participants who have reported the event.
c64 women (19%) and 47 MSM (28%) were unsure as to whether or not their partner had used any alcohol and/or other drugs and were removed from the analysis.
d11 women (3%) and 6 MSM (4%) were unsure as to whether or not they had used any alcohol and/or other drugs and were removed from the analysis.
Data missing from up to 5% of female respondents and up to 3% of male respondents; proportions are calculated using available data.
On multivariate analysis, women who had been stealthed were more likely to be a current sex worker than those who had never experienced stealthing (AOR 2.87, 95% CI: 2.01,4.11, p<0.001) (Table 3), and MSM who had been stealthed were more likely to report ‘health issues, such as anxiety or depression which may have affected their decision to use condoms for anal sex’ than those who had never experienced stealthing (AOR 2.13, 95% CI: 1.25,3.60, p = 0.005) (Table 3).
Most women met the male partner who had stealthed them through friends (29%, 95% CI: 24%,34%) or sex work (23%, 95% CI: 19%,28%). MSM reporting stealthing most commonly described the partner as someone they “did not know well” (61%) and had predominantly met them through geosocial dating applications or online (67%, 95% CI: 59%,74%) (Table 4).
At the time of the stealthing incident, 41% (95% CI: 36%,47%) of women and 54% (95% CI: 46%,62%) of MSM reported being sober, while 57% (95% CI: 51%,62%) of women and 41% (95% CI: 33%,49%) of MSM had consumed alcohol. Twelve percent of women and 13% of MSM had used other drugs either in addition to or without alcohol (Table 4). The majority of women reported their partner had consumed alcohol (68%, 95% CI: 62%,73%) and/or other drugs (19%), with only 27% (95% CI: 22%,33%) stating the partner had been sober when the incident occurred. Many MSM believed their partner to be sober (53%, 95% CI: 44%,62%), with 40% (95% CI: 31%,50%) of partners under the influence of alcohol, and 12% using additional/or other drugs (Table 4).
The majority of women (61%) and MSM (55%) discussed the removal of the condom with their partners after the event. Over half of the participants reported being emotionally stressed following the incident. Eight percent of women and five percent of MSM reported they thought they had acquired an STI following the event. One percent of women and two percent of MSM believed they had acquired HIV as a consequence of being stealthed (Table 4). Only 1% of people stealthed reported this experience to the police (Table 4).
Both female and MSM participants who had experienced stealthing were less likely to consider it to be sexual assault than participants who had not experienced stealthing. Amongst women, 62% (95% CI: 56%,67%) of those stealthed considered it to be assault, compared to 85% (95% CI: 82%,87%) of those not stealthed (OR 0.29, 95%CI: 0.22,0.4, p<0.001). Amongst men, 61% (95% CI: 53%,69%) of those stealthed considered it to be assault versus 84% (95% CI: 81%,86%) of those not stealthed (OR 0.31, 95%CI: 0.21,0.45, p<0.001).
Discussion
Although increasingly discussed in international media, there is little scientific research on non-consensual removal of condoms, popularly termed ‘stealthing’. To our knowledge this is the first study investigating how common stealthing is, the context in which it occurred, the impact on individuals, and how those stealthed perceive the event. A surprising proportion of clients attending a sexual health centre in Melbourne (32% of women and 19% of MSM) reported removal of a condom in a situation where they would not have willingly engaged in sexual intercourse without one—in other words, a violation of their consent [1].
These data need to be interpreted in the context of a STI clinic population which is generally a higher risk group than the general population. Our data show that 4% of women and 3% of MSM presenting to our clinic during the study period were attending following a stealthing incident. This equates to over 1200 consultations per year [12]. These data suggest that stealthing is common and should be considered when assessing patients in STI services.
Female respondents were less likely to be a current sex worker and MSM respondents were less likely to be HIV positive, compared to non-respondents. It is possible that both sex workers and HIV positive men were less likely to complete the survey due to privacy concerns, especially with regards to condom use and their legal obligations, which vary state by state in Australia. In Victoria, sex workers are legally required to use condoms with clients[13], and while those who are HIV positive are not legally required to disclose their HIV status, they must take reasonable precautions to prevent HIV transmission to those they are engaging in penetrative sex with[14]. Reasonable precaution refers to correct use of condoms and lube during intercourse. While female sex workers were less represented in respondents than non-respondents, 18% of participants were sex workers and we still observed an association between being a sex worker and being more likely to be stealthed. Low numbers of HIV positive men participating may have limited our ability to examine any association between stealthing and HIV status. Lastly, both women and MSM who had been overseas recently were more likely to respond to our survey. This may bias our findings towards individuals who may have participated due to recent high risk sexual encounters, in the context of overseas travel[15].
Women who experienced stealthing were three times more likely to be sex workers compared to those who had not. In the Law and Sex Worker Health (LASH) Survey conducted in Australia, 8% of respondents reported assault by clients [16]. However the LASH survey did not compare rates of assault to the general population or differentiate between physical and sexual assault, and only examined assault in the workplace. Perkins' (1991) research with Sydney-based brothel workers found that 20% of sex workers experienced rape while working. Outside the workplace sex workers experienced higher levels of sexual assault compared with non-sex workers, with 46.9% reporting rape, compared to 21.9% of health workers and 12.7% of students [17]. Our data are consistent with these findings that sex workers are at increased risk of non-consensual sex acts.
Sixty-seven percent of MSM who had experienced stealthing met the partner via geosocial dating applications, for example Grindr, Tinder or Scruff. This is comparable to the number of MSM meeting partners through dating applications (70%) [18]. Sexual encounters initiated online are more likely to include unprotected anal intercourse [19], however it has also been found that meeting partners online increases the likelihood of discussion between partners of preferred sexual practices compared to meeting partners offline [19, 20]. MSM who had been stealthed were twice as likely to report having anxiety or depression. Depressive symptoms and anxiety are predictive of condom non-use [21] and higher levels of depression are related to lower levels of self-efficacy for sexual safety [22]. MSM who have anxiety or depression may be vulnerable to stealthing for this reason.
In this study, the majority of women (73%) believed the partner who had stealthed them to be under the influence of alcohol and/or other drugs. In heterosexual relations, the link between alcohol consumption and committal of sexual assault is well documented [23, 24]. Condom resistance tactics and sexual aggression with female partners are more commonly employed by men with history of sexual aggression and alcohol intoxication [25, 26]. Additionally, both alcohol consumption [27] and condom use [28, 29] have been associated with erectile dysfunction. Men with erection issues are more likely to engage in unprotected sex, misuse condoms [28, 29], and are more likely to remove condoms before sex is over (p = 0.001) [29]. Literature supports our finding that heterosexual men who have consumed alcohol may be at increased risk of committing nonconsensual sex acts, and may be removing the condom to maintain an erection.
Whilst the majority of those reporting stealthing considered it sexual assault, they were three times less likely to consider stealthing sexual assault than those who had never experienced it. The US National Crime Victimization Survey found 20% of female victim narratives contained excuses for offenders’ behaviour, denials of injury, or justification of the incident as the victims’ fault [30]. This allowed the women to avoid the distress of labelling themselves victims of a crime, or their partners as criminals [30]. Victims of stealthing may also not yet view themselves as sexual assault victims as stealthing is a relatively new topic. Sexual assault is a term with many connotations and there are cultural myths as to who is a ‘real’ sexual victim [31], with the type of violence experienced influencing society’s view as to whether a woman is a victim [32]. Our current language around sexual assault (and in this case, stealthing) may require expansion- until an act is named as assault it cannot be viewed as such, and cannot be reported or legislated against [33]. A limitation of this study is that we did not ask respondents why they did not consider stealthing to be sexual assault.
Stealthing has potentially serious consequences. The majority of patients reported consequences following the stealthing incident, with over half experiencing emotional stress. Although literature contains estimates as to the rate of STI and HIV transmission during sexual assault, it is difficult to establish if an STI has been acquired from a specific event. The Centers for Disease Control and Prevention (CDC) guidelines recommend testing all people for STIs following sexual assault [34], with the caveat that many positive tests will be from a pre-existing STI [35]. MSM patients with condom malfunction or condom-less sex presenting in a 72 hour window fulfil criteria for HIV Non-Occupational Post Exposure Prophylaxis (nPEP) [36, 37], and therefore MSM who present reporting non-consensual condom removal should be prescribed it.
This study has several limitations. Firstly, this study was offered in English only, which means it cannot be generalised to attendees who are not fluent in English. Secondly, this study may be subject to responder bias, as those who have experienced stealthing may have been more likely to answer the survey. Given this is a retrospective survey, participant responses may be subject to recall bias, and specific contextual situational factors and outcomes were asked about one event only for those stating it had happened on more than one occasion. While some participants within our study attributed the acquisition of STIs to being stealthed, this cannot be verified. According to attribution theory [38] following an adverse event people will make attributions to understand and control their environment[39], with situational factors often exaggerated when there is a negative outcome [40], and thus patients could be incorrectly attributing contracting a STI to the stealthing event.
Despite these limitations, this study has a large sample size with over two thousand responses. Accurate statistics describing the prevalence and incidence of sexual assault are difficult to obtain since the majority of assaults are not reported to authorities and victims often do not access services [31]. Only 1% of patients reporting stealthing in this study reported the event to the police. Although this study may be subject to recall bias, population surveys are the best means of learning the true extent and nature of these crimes, rather than relying on crime statistics. This is the first study to describe how commonly this practice is occurring.
In summary, stealthing was commonly experienced by our clinic population, with a third of women and a fifth of MSM reporting it, with situational contexts often involving alcohol and/or drugs in women, and geosocial networking applications in MSM. Sex work was a clear risk factor identified among women, and risk factors for MSM included anxiety and depression. Knowledge of these risk factors can enable services to ask about stealthing in target groups and offer specific support and counselling. Further community-based research would help determine the prevalence in the broader population and studies that link behavioural measures to biological outcomes would help to quantify the STI risk associated with this practice.
Acknowledgments
We would like to acknowledge Jun Kit Sze and Afrizal for technical assistance and assistance with data collection for this project, and Melbourne Sexual Health Centre counsellors Jocelyn Verry and Peter Hayes for their support of this project.
Data Availability
Information obtained in this survey is highly sensitive and confidential and includes patient health record data. Furthermore, we are unable to share data as it would be in breach our ethics approval. Our participant information and consent form specifically states that individual participant information will only be accessible to the study team and will not be disseminated further in an identifiable way, i.e. only presented as aggregated data or statistics - "Information obtained in this research project that can identify you will remain confidential and will be stored securely indefinitely. The database containing the questionnaires and the code linking these to your name will remain at Melbourne Sexual Health Centre, on password-protected servers, and only the study team will have access. Your information will only be used for this research project, or future research at this centre, and will not be disclosed except as required by law. The results of this research will be published and presented at conferences in such a way that you are not identified." Therefore we have presented all data collected in an aggregate way in the paper so that it is non-identifiable, as approved by our ethics committee. Data is required to be securely stored in keeping with requirements from Alfred Hospital Ethics Committee who can be contacted through Angela Henjak at research@alfred.org.au for queries regarding accessing the data. Any questions regarding the data itself should be directed to Rosie Latimer at rlatimer@mshc.org.au or A/Professor Catriona Bradshaw at cbradshaw@mshc.org.au.
Funding Statement
RLL and VJC are supported by an Australian Government Research Training Program (RTP) Scholarship. TRHR and EPFC are supported by NHMRC early career fellowship no.1091536, 1091226, respectively. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Brodsky A. "Rape-Adjacent": Imaging Legal Responses to Nonconsensual Condom Removal. Columbia Journal of Gender and Law. 2017;32(2):183–210. [Google Scholar]
- 2.Brennan J. Stealth breeding: bareback without consent. Psychology & Sexuality. 2017;8(4):318–33. 10.1080/19419899.2017.1393451 [DOI] [Google Scholar]
- 3.Holmes KK, Levine R, Weaver M. Effectiveness of condoms in preventing sexually transmitted infections. Bull World Health Organ. 2004;82(6):454–61. [PMC free article] [PubMed] [Google Scholar]
- 4.Pinkerton SD, Abramson PR. Effectiveness of condoms in preventing HIV transmission. Social Science & Medicine. 1997;44(9):1303–12. 10.1016/s0277-9536(96)00258-4 [DOI] [PubMed] [Google Scholar]
- 5.Weller SC, Davis-Beaty K, Weller SC. Condom effectiveness in reducing heterosexual HIV transmission. 2002. 10.1002/14651858.cd003255 [DOI] [Google Scholar]
- 6.Hickman SE, Muehlenhard CL. “By the semi‐mystical appearance of a condom”: How young women and men communicate sexual consent in heterosexual situations. Journal of Sex Research. 1999;36(3):258–72. 10.1080/00224499909551996 [DOI] [Google Scholar]
- 7.Humphreys T. Perceptions of sexual consent: the impact of relationship history and gender. J Sex Res. 2007;44(4):307–15. 10.1080/00224490701586706 . [DOI] [PubMed] [Google Scholar]
- 8.Davis KC, Stappenbeck CA, Norris J, George WH, Jacques-Tiura AJ, Schraufnagel TJ, et al. Young Men's Condom Use Resistance Tactics: A Latent Profile Analysis. The Journal of Sex Research. 2014;51(4):454–65. 10.1080/00224499.2013.776660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miller E, Decker MR, McCauley HL, Tancredi DJ, Levenson RR, Waldman J, et al. Pregnancy coercion, intimate partner violence and unintended pregnancy. Contraception. 2010;81(4):316–22. 10.1016/j.contraception.2009.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moore A, Frohwirth L, Miller E. Male reproductive control of women who have experienced intimate partner violence in the United States. Social Science & Medicine. 2010;70:1737–44. [DOI] [PubMed] [Google Scholar]
- 11.Klein H Generationing, Stealthing, and Gift Giving: The Intentional Transmission of HIV by HIV-Positive Men to their HIV-Negative Sex Partners. Health Psychology Research. 2014;2(3):1582 10.4081/hpr.2014.1582 PMC4768590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chow EP, Fehler G, Chen MY, Bradshaw CS, Denham I, Law MG, et al. Testing commercial sex workers for sexually transmitted infections in Victoria, Australia: an evaluation of the impact of reducing the frequency of testing. PLoS One. 2014;9(7):e103081 10.1371/journal.pone.0103081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de Jong AS, Rahamat-Langendoen JC, van Alphen P, Hilt N, van Herk C, Pont S, et al. Large two-centre study into the prevalence of Mycoplasma genitalium and Trichomonas vaginalis in the Netherlands. Int J STD AIDS. 2016;27(10):856–60. 10.1177/0956462415596496. . [DOI] [PubMed] [Google Scholar]
- 14.Kidd P. Laying down the law. Positive Living Magazine. [Google Scholar]
- 15.Sundbeck M, Agardh A, Östergren P-O. Travel abroad increases sexual health risk-taking among Swedish youth: a population-based study using a case-crossover strategy. Global health action. 2017;10(1):1330511–. 10.1080/16549716.2017.1330511 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Donovan B, Harcourt C., Egger S., Watchirs Smith L., Schneider K., Kaldor J.M., Chen M.Y., Fairley C.K., Tabrizi S. The Sex Industry in New South Wales: a Report to the NSW Ministry of Health 2012. [Google Scholar]
- 17.Perkins R. Working girls: Prostitutes, their life and social control Canberra: Australian Institute of Criminology. [Google Scholar]
- 18.Chow EP, Cornelisse, Read TRH, Hocking JS, Walker S, Chen MY, et al. Risk practices in the era of smartphone apps for meeting partners: a cross-sectional study among men who have sex with men in Melbourne, Australia. AIDS Patients Care and STDs. 2016;4(30):151–4. PubMed Central PMCID: PMC27028181. [DOI] [PubMed] [Google Scholar]
- 19.Horvath KJ, Oakes JM, Rosser BRS. Sexual Negotiation and HIV Serodisclosure among Men who Have Sex with Men with Their Online and Offline Partners. Journal of Urban Health. 2008;85(5):744–58. 10.1007/s11524-008-9299-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carballo-Diéguez A, Miner M, Dolezal C, Rosser BRS, Jacoby S. Sexual Negotiation, HIV-Status Disclosure, and Sexual Risk Behavior Among Latino Men Who Use the Internet to Seek Sex with Other Men. Archives of Sexual Behavior. 2006;35(4):473–81. 10.1007/s10508-006-9078-7 [DOI] [PubMed] [Google Scholar]
- 21.Lehrer JA, Shrier LA, Gortmaker S, Buka S. Depressive Symptoms as a Longitudinal Predictor of Sexual Risk Behaviors Among US Middle and High School Students. Pediatrics. 2006;118(1):189–200. 10.1542/peds.2005-1320 [DOI] [PubMed] [Google Scholar]
- 22.Alvy LM, McKirnan DJ, Mansergh G, Koblin B, Colfax GN, Flores SA, et al. Depression is Associated with Sexual Risk Among Men Who Have Sex with Men, but is Mediated by Cognitive Escape and Self-Efficacy. AIDS and Behavior. 2011;15(6):1171–9. 10.1007/s10461-010-9678-z [DOI] [PubMed] [Google Scholar]
- 23.Abbey A. Alcohol-related sexual assault: a common problem among college students. Journal of Studies on Alcohol, Supplement. 2002;(s14):118–28. 10.15288/jsas.2002.s14.118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abbey A, McAuslan P. A Longitudinal Examination of Male College Students' Perpetration of Sexual Assault. Journal of Consulting and Clinical Psychology. 2004;72(5):747–56. 10.1037/0022-006X.72.5.747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Davis KC, Danube CL, Neilson EC, Stappenbeck CA, Norris J, George WH, et al. Distal and Proximal Influences on Men’s Intentions to Resist Condoms: Alcohol, Sexual Aggression History, Impulsivity, and Social-Cognitive Factors. AIDS and Behavior. 2016;20(1):147–57. 10.1007/s10461-015-1060-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Davis KC. The influence of alcohol expectancies and intoxication on men's aggressive unprotected sexual intentions. Exp Clin Psychopharmacol. 2010;18(5):418–28. 10.1037/a0020510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rubin HB, Henson DE. Effects of alcohol on male sexual responding. Psychopharmacology. 1976;47(2):123–34. 10.1007/bf00735810 [DOI] [PubMed] [Google Scholar]
- 28.Musacchio NS, Hartrich M, Garofalo R. Erectile Dysfunction and Viagra Use: What’s up with College-Age Males? Journal of Adolescent Health. 2006;39(3):452–4. 10.1016/j.jadohealth.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 29.Graham CA, Crosby R, Yarber WL, Sanders SA, McBride K, Milhausen RR, et al. Erection loss in association with condom use among young men attending a public STI clinic: potential correlates and implications for risk behaviour. Sex Health. 2006;3(4):255–60. 10.1071/SH06026#sthash.sSPI7LIS.dpuf . [DOI] [PubMed] [Google Scholar]
- 30.Weiss KG. “Boys Will Be Boys” and Other Gendered Accounts:An Exploration of Victims' Excuses and Justifications for Unwanted Sexual Contact and Coercion. Violence Against Women. 2009;15(7):810–34. 10.1177/1077801209333611 . [DOI] [PubMed] [Google Scholar]
- 31.Lievore D. Non-reporting and hidden recording of sexual assault: an international literature review Australian Institute of Criminology, Canberra, Australia; 2003. [Google Scholar]
- 32.Healicon A. The Politics of Sexual Violence: Rape, Identity and Feminism Basingstoke, UK: Palgrave Macmillian; 2016. [Google Scholar]
- 33.Grady C. The complicated, inadequate language of sexual violence. Vox. 2017 30/11/2017.
- 34.Jiang J, Liu P, Cao NX, Gong XD. The prevalence of mycoplasma genitalium and chlamydia trachomatis at various anatomical sites of men who have sex with men in five cities of china. Sexually transmitted infections. 2015;91:A30–A1. 10.1136/sextrans-2015-052270.93 [DOI] [Google Scholar]
- 35.Sachs CJ, Thomas B. Sexual Assault, Infectious Disease Prophylaxis: Treasure Island (FL): StatPearls Publishing; 2018. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482239/. [PubMed] [Google Scholar]
- 36.McDougal SJ, Alexander J, Dhanireddy S, Harrington RD, Stekler JD. Non-Occupational Post-Exposure Prophylaxis for HIV: 10-Year Retrospective Analysis in Seattle, Washington. PLoS ONE. 2014;9(8):e105030 10.1371/journal.pone.0105030 PMC4139302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pinkerton SD, Martin JN, Roland ME, Katz MH, Coates TJ, Kahn JO. Cost-effectiveness of HIV postexposure prophylaxis following sexual or injection drug exposure in 96 metropolitan areas in the United States. AIDS. 2004;18(15):2065–73. . [DOI] [PubMed] [Google Scholar]
- 38.Kelley HH. Attribution theory in social psychology. Nebraska Symposium on Motivation. 1967;15:192–238. [Google Scholar]
- 39.Wong P, Weiner B. Why People Ask “Why” Questions and the Heuristics of Attributional Search1981. 650–63 p. [Google Scholar]
- 40.Heider F. The psychology of interpersonal relations Hillsdale, New Jersey: Lawrence Erlbaum Associates; 1958. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Information obtained in this survey is highly sensitive and confidential and includes patient health record data. Furthermore, we are unable to share data as it would be in breach our ethics approval. Our participant information and consent form specifically states that individual participant information will only be accessible to the study team and will not be disseminated further in an identifiable way, i.e. only presented as aggregated data or statistics - "Information obtained in this research project that can identify you will remain confidential and will be stored securely indefinitely. The database containing the questionnaires and the code linking these to your name will remain at Melbourne Sexual Health Centre, on password-protected servers, and only the study team will have access. Your information will only be used for this research project, or future research at this centre, and will not be disclosed except as required by law. The results of this research will be published and presented at conferences in such a way that you are not identified." Therefore we have presented all data collected in an aggregate way in the paper so that it is non-identifiable, as approved by our ethics committee. Data is required to be securely stored in keeping with requirements from Alfred Hospital Ethics Committee who can be contacted through Angela Henjak at research@alfred.org.au for queries regarding accessing the data. Any questions regarding the data itself should be directed to Rosie Latimer at rlatimer@mshc.org.au or A/Professor Catriona Bradshaw at cbradshaw@mshc.org.au.