Abstract
The posterolateral corner (PLC) of the knee is the main restraint to varus forces of the knee as well as posterolateral rotation of the tibia relative to the femur. Primary PLC repairs have been associated with a high failure rate in past literature. However, with modern improved arthroscopic instrumentation and devices, there has been a renewed interest in repair of the ligaments around the knee. Internal bracing with suture tape augmentation encourages healing and allows early mobilization. This article describes, with video illustration, PLC repair with suture tape augmentation.
The posterolateral corner (PLC) of the knee is the main restraint to varus forces of the knee as well as posterolateral rotation of the tibia relative to the femur.1 The PLC consists of 3 major stabilizers: the lateral collateral ligament (LCL), the popliteofibular ligament, and the popliteal tendon.2 Most PLC injuries are associated with anterior cruciate ligament or posterior cruciate ligament ruptures, with isolated injuries being rare.3 It is important to identify PLC injuries, in particular in multiligament knee injuries, because rerupture of the cruciate ligaments has been associated with untreated PLC injuries.4, 5, 6
PLC reconstruction procedures are the most widely used surgical option to treat both acute and chronic injuries.7, 8 Primary PLC repairs have been thought to be insufficient in providing adequate functional outcomes and have been associated with a high failure rate in past literature.9 However, with modern improved arthroscopic instrumentation and devices, there has been a renewed interest in repair of the ligaments around the knee.10 We describe PLC repair with suture tape augmentation that encourages healing and allows early mobilization (Video 1).
Surgical Technique
The patient is placed in the supine position, and a tourniquet is placed on the upper thigh. The injured leg is prepared and draped in the surgeon's preferred position, similarly to any procedure around the knee. Appropriate landmarks are palpated and marked (Fig 1). A curved incision is used, passing just superior to the lateral epicondyle. A flap is then dissected from the iliotibial band down to the head of the fibula. Two deep incisions are made in the iliotibial band to permit accurate suture tape placement and to allow additional tensioning at the end of the procedure (Fig 2). The peroneal nerve is identified and protected under direct vision.
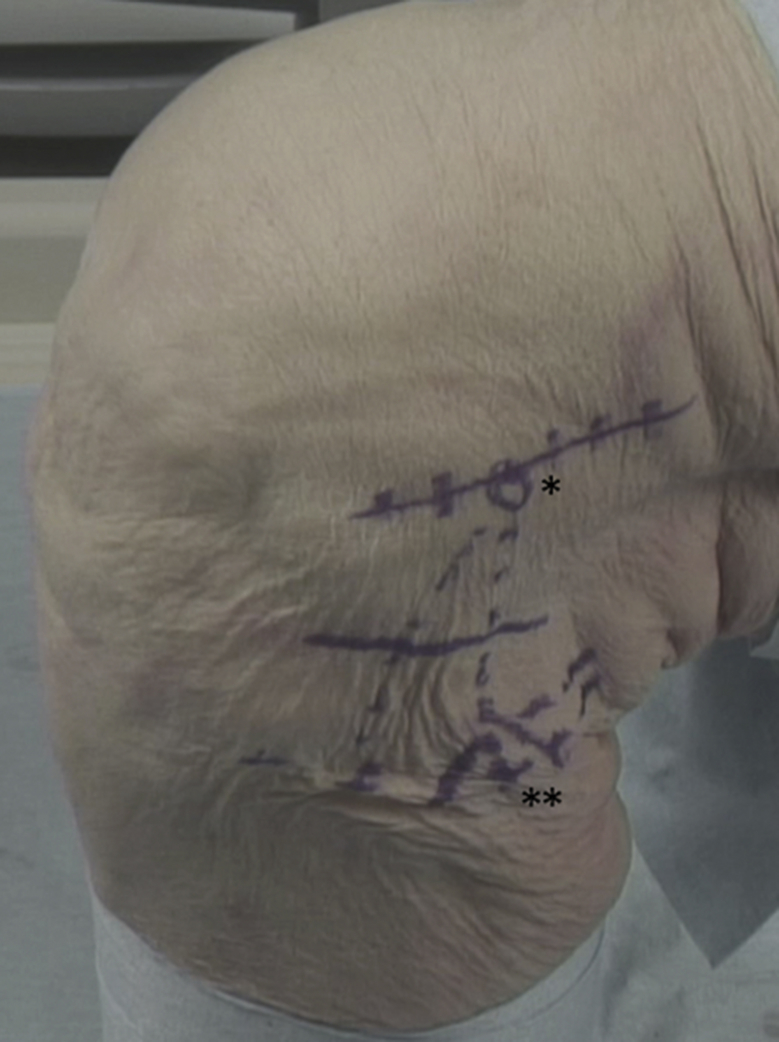
Fig 1.
Left knee, lateral view. Appropriate landmarks are marked before the procedure begins, including the lateral epicondyle (1 asterisk) and the head of the fibula (2 asterisks), which are key landmarks for suture tape placement.
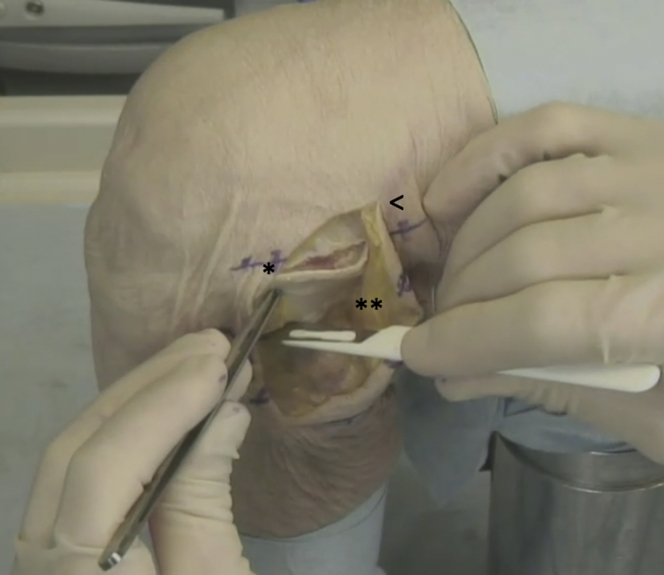
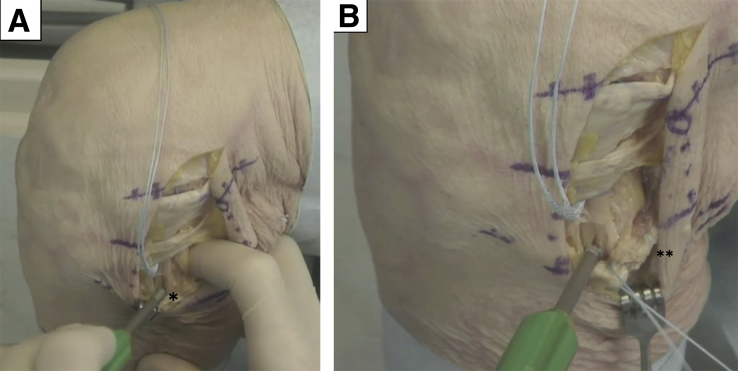
Fig 2.
Left knee, lateral view. A curved incision (arrowhead) passing just superior to the lateral epicondyle is used; then, 2 deep incisions (1 and 2 asterisks) are made in the iliotibial band to enable accurate suture tape placement and to permit tensioning.
The next step is to predrill with a 4.5-mm drill and tap at the origin of the LCL just proximal to the lateral epicondyle, with the surgeon ensuring that this is performed perpendicular to the cortex. A 4.75-mm SwiveLock (Arthrex) preloaded with FiberTape (Arthrex) is then inserted, with the surgeon ensuring it is flush with the cortex (Fig 3). The FiberTape is an ultrahigh-strength 2-mm-wide tape, consisting of long-chain ultrahigh-molecular-weight polyethylene. The suture tape is then shuttled toward the head of the fibula, mirroring the LCL (Fig 4).
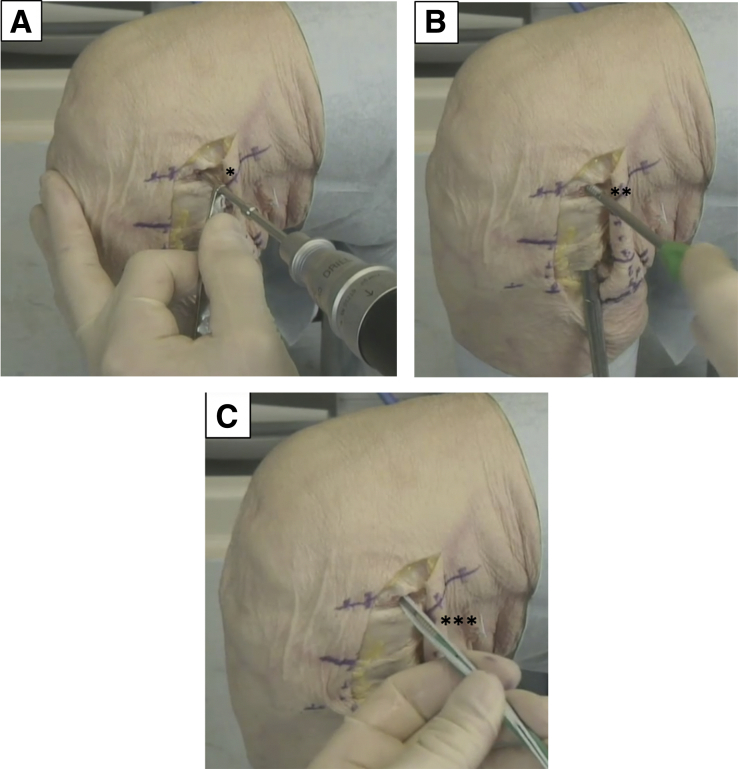
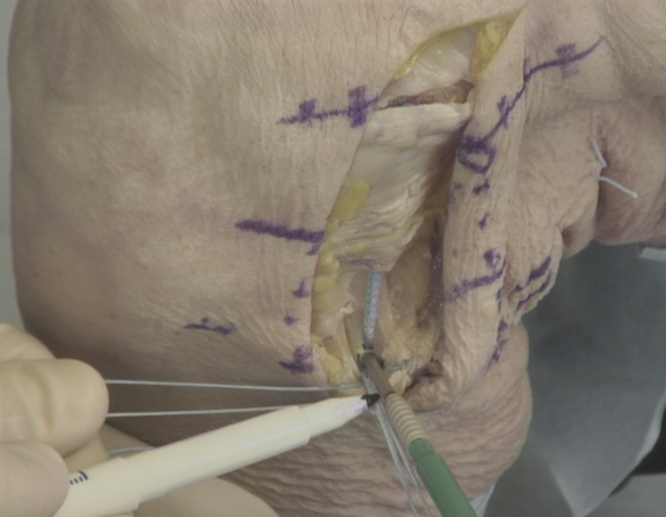
Fig 3.
Left knee, lateral view. (A, B) The origin of the lateral collateral ligament is identified just proximal to the lateral epicondyle and then predrilled (1 asterisk) and tapped (2 asterisks). (C) The suture tape preloaded in the anchor is inserted (3 asterisks), with the surgeon ensuring it is flush with the cortex.
Fig 4.
Left knee, lateral view. The suture tape (1 asterisk) is shuttled from the lateral epicondyle (2 asterisks) to the head of the fibula (3 asterisks), mirroring the lateral collateral ligament.
The head of the fibula is exposed, and the insertion point of the LCL is identified. The technique aims to restore the soft-tissue balance around the head of the fibula, which is recognized as the focus of injury during disruption of the PLC. The next step is to predrill with a 4.5-mm drill and tap while the surgeon uses his or her finger to protect the peroneal nerve. A whipstitch is inserted in the biceps tendon (Fig 5). The 4.75-mm suture anchor is then advanced to the end of the tap, and the laser line is marked after the knee is put through a range of motion with the foot in a neutral position with no additional tension, which should identify the anatomic length of the LCL (Fig 6). The anchor is inserted until it is flush with the cortex, and the core suture is retained and used as a post to secure soft-tissue sutures. Repair is then performed using the core suture from the anchor and the whipstitch around the biceps tendon, thereby providing a rebalancing of the soft tissues around the head of the fibula. No attempt is made to directly repair the popliteus, although the suture tape can be split with 1 strand used to repair the anterolateral ligament if required. Finally, the iliotibial band is repaired (Fig 7). This is an essential component of the technique because this sheet of soft tissue is also attenuated during injury, and slight double breasting with approximately 5 mm of overlap improves the stability of the soft-tissue repair.
Fig 5.
Left knee, lateral view. (A) The head of the fibula is exposed, and predrilling and tapping (1 asterisk) are performed at the lateral collateral ligament insertion point. (B) A whipstitch is inserted in the biceps tendon (2 asterisks).
Fig 6.
Left knee, lateral view. The 4.75-mm suture anchor is advanced to the end of the tap, and the laser line is marked; then, the anchor is advanced into the head of the fibula.
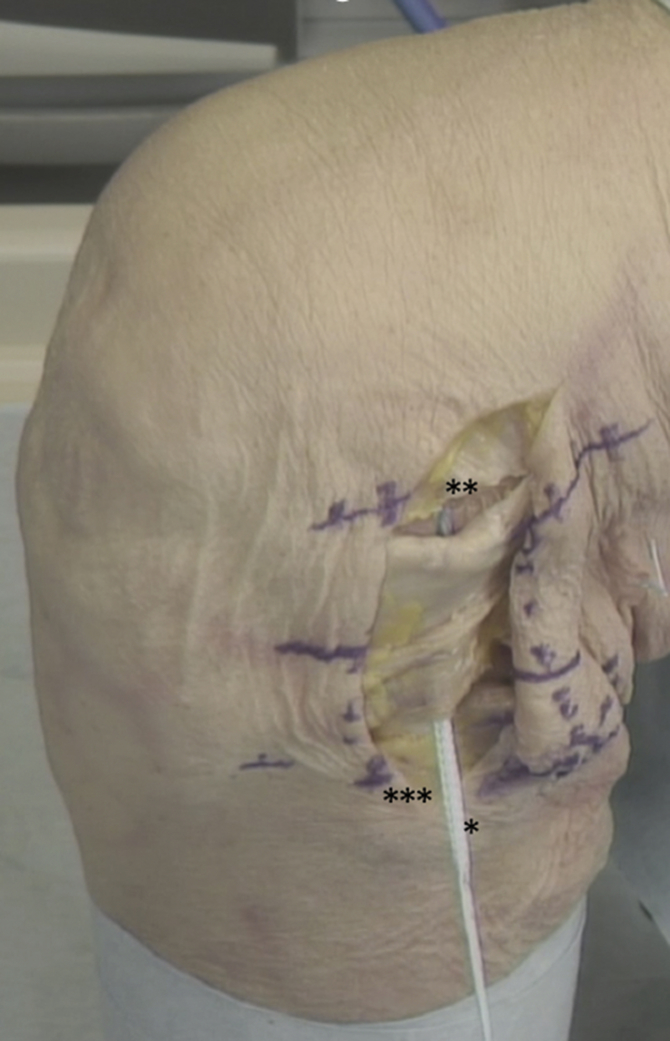
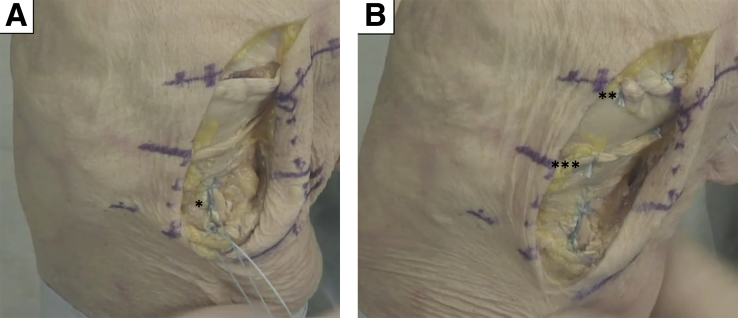
Fig 7.
Left knee, lateral view. (A) The repair consists of the core suture from the anchor and the whipstitch around the biceps tendon (1 asterisk). (B) Both incisions in the iliotibial band are repaired (2 and 3 asterisks).
Patients are allowed to fully bear weight with crutches as required during the first few weeks. Physical therapy focuses on early range of movement, muscle control, and restoration of function. Patients are allowed to perform sports when the neuromuscular function has recovered. No brace is required. Advantages and disadvantages as well as pearls and pitfalls of this technique are shown in Tables 1 and 2.
Table 1.
Advantages and Disadvantages of Posterolateral Corner Repair With Suture Tape Augmentation
| Advantages | Disadvantages |
|---|---|
| Simple and reproducible | Mild suture anchor irritation during end-range extension |
| No graft harvest required | Synthetic augmentation |
| Facilitates rehabilitation |
Table 2.
Pearls and Pitfalls of Posterolateral Corner Repair With Suture Tape Augmentation
| Pearls | Pitfalls |
|---|---|
| Restoration of the soft-tissue balance around the head of the fibula is achieved. | Excessive tensioning can occur if not positioned in neutral. |
| A full range of motion with the foot in neutral should be established before insertion of the augmentation. | Peroneal nerve exposure can occur. |
| Occasional sutures can be passed through the FiberTape to prevent cheese wiring of the soft tissues and to improve the overall strength of the construct. | The popliteofibular ligament is not addressed. |
Discussion
Several techniques have been described in the literature for the operative management of patients with injuries to the PLC, including both repair and reconstruction procedures.9 Historically, PLC injuries were treated with primary repair with satisfactory outcomes.11, 12 However, more recent studies have indicated high failure rates with primary PLC repair leading to reconstruction techniques becoming more common. Stannard et al.13 reported on 64 PLC injuries with 39 patients undergoing repair with suture anchors and 25 patients undergoing reconstruction with either tibialis anterior or tibialis posterior allografts. Failure occurred in 37% of the repairs in comparison with 9% of the reconstructions. In addition, Levy et al.14 concluded that PLC reconstruction was a more reliable option than PLC repair in a similar study in which they compared 10 repairs using suture anchors with 18 reconstructions using Achilles tendon with bone allograft. Failure occurred in 40% of the PLC repairs. However, these repair techniques lacked augmentation, which protects the PLC during the healing phase.
Several other reconstruction procedures have been described in the literature, with a number of different techniques and grafts. Schechinger et al.15 reported satisfactory outcomes in 16 patients who underwent PLC reconstruction with Achilles tendon allograft similarly to the technique used by Levy et al.14 Ibrahim et al.16 showed improved outcomes in 20 patients with multiligament knee injuries who underwent PLC reconstruction with contralateral hamstring. Furthermore, Geeslin and LaPrade17 reported successful results of an anatomic PLC reconstruction with repair of the avulsed structures of the PLC in 25 patients.
PLC repair with suture tape augmentation as described in this Technical Note reinforces the ligament, acts as a secondary stabilizer, and allows early mobilization, thereby providing protection that in theory should prevent the failures previously associated with primary repair. Recovery is accelerated and muscle atrophy is prevented because graft harvest is not required and the procedure is less invasive than standard reconstruction procedures.
In conclusion, this Technical Note has described the technique of PLC repair with suture tape augmentation. A number of advantages are associated with this technique, as shown in Table 1, and we have observed excellent clinical results. Nonetheless, clinical studies are necessary to establish the overall outcomes of this procedure.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: Arthrex has facilitated the making of the video for this surgical technique. C.H.W.H. reports that Antwerp University Hospital receives support from Research Foundation Flanders Research Foundation Flanders (FWO) under reference T001017N not related to this manuscript. L.D. receives support from Mathys Medical for consultancy regarding hip replacement. G.M.M. is a consultant for and receives royalties from Arthrex and has a patent for the InternalBrace. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Narrated step-by-step guide for the posterolateral corner (PLC) repair technique with suture tape augmentation in a left knee from a lateral view. Appropriate landmarks are marked before the procedure begins. A curved incision is then made, passing just superior to the lateral epicondyle. Two deep incisions are made in the iliotibial band. The origin of the lateral collateral ligament (LCL) is identified; then, an anchor preloaded with suture tape is inserted and shuttled to the head of the fibula, where it is secured with a further anchor. This procedure is simple and reproducible and facilitates rehabilitation.
References
- 1.Chahla J., Moatshe G., Dean C.S., LaPrade R.F. Posterolateral corner of the knee: Current concepts. Arch Bone Jt Surg. 2016;4:97–103. [PMC free article] [PubMed] [Google Scholar]
- 2.LaPrade R.F., Ly T.V., Wentorf F.A., Engebretsen L. The posterolateral attachments of the knee: A qualitative and quantitative morphologic analysis of the fibular collateral ligament, popliteus tendon, popliteofibular ligament, and lateral gastrocnemius tendon. Am J Sports Med. 2003;31:854–860. doi: 10.1177/03635465030310062101. [DOI] [PubMed] [Google Scholar]
- 3.LaPrade R.F., Terry G.C. Injuries to the posterolateral aspect of the knee. Association of anatomic injury patterns with clinical instability. Am J Sports Med. 1997;25:433–438. doi: 10.1177/036354659702500403. [DOI] [PubMed] [Google Scholar]
- 4.LaPrade R.F., Muench C., Wentorf F., Lewis J.L. The effect of injury to the posterolateral structures of the knee on force in a posterior cruciate ligament graft: A biomechanical study. Am J Sports Med. 2002;30:233–238. doi: 10.1177/03635465020300021501. [DOI] [PubMed] [Google Scholar]
- 5.LaPrade R.F., Resig S., Wentorf F., Lewis J.L. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force. A biomechanical analysis. Am J Sports Med. 1999;27:469–475. doi: 10.1177/03635465990270041101. [DOI] [PubMed] [Google Scholar]
- 6.Harner C.D., Vogrin T.M., Höher J., Ma C.B., Woo S.L. Biomechanical analysis of a posterior cruciate ligament reconstruction. Deficiency of the posterolateral structures as a cause of graft failure. Am J Sports Med. 2000;28:32–39. doi: 10.1177/03635465000280011801. [DOI] [PubMed] [Google Scholar]
- 7.Moulton S.G., Geeslin A.G., LaPrade R.F. A systematic review of the outcomes of posterolateral corner knee injuries, part 2: Surgical treatment of chronic injuries. Am J Sports Med. 2016;44:1616–1623. doi: 10.1177/0363546515593950. [DOI] [PubMed] [Google Scholar]
- 8.Shon O.J., Park J.W., Kim B.J. Current concepts of posterolateral corner injuries of the knee. Knee Surg Relat Res. 2017;29:256–268. doi: 10.5792/ksrr.16.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Geeslin A.G., Moulton S.G., LaPrade R.F. A systematic review of the outcomes of posterolateral corner knee injuries, part 1: Surgical treatment of acute injuries. Am J Sports Med. 2016;44:1336–1342. doi: 10.1177/0363546515592828. [DOI] [PubMed] [Google Scholar]
- 10.Mackay G.M., Blyth M.J., Anthony I., Hopper G.P., Ribbans W.J. A review of ligament augmentation with the InternalBrace™: The surgical principle is described for the lateral ankle ligament and ACL repair in particular, and a comprehensive review of other surgical applications and techniques is presented. Surg Technol Int. 2015;26:239–255. [PubMed] [Google Scholar]
- 11.Baker C.L., Norwood L.A., Hughston J.C. Acute posterolateral rotatory instability of the knee. J Bone Joint Surg Am. 1983;65:614–618. [PubMed] [Google Scholar]
- 12.DeLee J.C., Riley M.B., Rockwood C.A. Acute posterolateral rotatory instability of the knee. Am J Sports Med. 1983;11:199–207. doi: 10.1177/036354658301100403. [DOI] [PubMed] [Google Scholar]
- 13.Stannard J.P., Brown S.L., Farris R.C., McGwin G., Volgas D.A. The posterolateral corner of the knee: Repair versus reconstruction. Am J Sports Med. 2005;33:881–888. doi: 10.1177/0363546504271208. [DOI] [PubMed] [Google Scholar]
- 14.Levy B.A., Dajani K.A., Morgan J.A., Shah J.P., Dahm D.L., Stuart M.J. Repair versus reconstruction of the fibular collateral ligament and posterolateral corner in the multiligament-injured knee. Am J Sports Med. 2010;38:804–809. doi: 10.1177/0363546509352459. [DOI] [PubMed] [Google Scholar]
- 15.Schechinger S.J., Levy B.A., Dajani K.A., Shah J.P., Herrera D.A., Marx R.G. Achilles tendon allograft reconstruction of the fibular collateral ligament and posterolateral corner. Arthroscopy. 2009;25:232–242. doi: 10.1016/j.arthro.2008.09.017. [DOI] [PubMed] [Google Scholar]
- 16.Ibrahim S.A., Ghafar S., Salah M. Surgical management of traumatic knee dislocation with posterolateral corner injury. Arthroscopy. 2013;29:733–741. doi: 10.1016/j.arthro.2012.11.021. [DOI] [PubMed] [Google Scholar]
- 17.Geeslin A.G., LaPrade R.F. Outcomes of treatment of acute grade-III isolated and combined posterolateral knee injuries: A prospective case series and surgical technique. J Bone Joint Surg Am. 2011;93:1672–1683. doi: 10.2106/JBJS.J.01639. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Narrated step-by-step guide for the posterolateral corner (PLC) repair technique with suture tape augmentation in a left knee from a lateral view. Appropriate landmarks are marked before the procedure begins. A curved incision is then made, passing just superior to the lateral epicondyle. Two deep incisions are made in the iliotibial band. The origin of the lateral collateral ligament (LCL) is identified; then, an anchor preloaded with suture tape is inserted and shuttled to the head of the fibula, where it is secured with a further anchor. This procedure is simple and reproducible and facilitates rehabilitation.