Abstract
Objectives
We evaluated trends in hypertension prevalence, awareness, treatment and control in an Indian urban population over 25 years. Trends were projected to year 2030 to determine attainment of World Health Organization (WHO) Global Monitoring Framework targets.
Methods
Adult participants (n = 7440, men 4237, women 3203) enrolled in successive population based studies in Jaipur, India from years 1991 to 2015 were evaluated for hypertension prevalence, awareness, treatment and control. The studies were performed in years 1991–93 (n = 2212), 1999–01 (n = 1123), 2003–04 (n = 458), 2006–07 (n = 1127), 2009–10 (n = 739) and 2012–15 (n = 1781). Descriptive statistics are reported. We used logarithmic forecasting to year 2030 and compared outcomes to WHO target of 25% lower prevalence and >50% control.
Results
The age-adjusted hypertension prevalence (%) among adults in successive studies increased from 29.5, 30.2, 36.5, 42.1, 34.4 to 36.1 (R2 = 0.41). Increasing trends were observed for hypertension awareness (13, 44, 49, 44, 49, 56; R2 = 0.63); treatment in all (9, 22, 38, 34, 41, 36; R2 = 0.68) and aware hypertensives (61, 66, 77, 79, 70, 64; R2 = 0.46); and control in all (2, 14, 13, 18, 21, 21; R2 = 0.82), aware (12, 33, 27, 46, 37, 37; R2 = 0.54) and treated (9, 20, 21, 48, 36, 49; R2 = 0.80) hypertensive participants. Projections to year 2030 show increases in prevalence to 44% (95% CI 43–45), awareness to 82% (81–83), treatment to 62% (61–63), and control to 36% (35–37).
Conclusion
Hypertension prevalence, awareness, treatment and control rates are increasing among urban populations in India. Better awareness is associated with greater control. The rates of increase are off-target for WHO Global Monitoring Framework and UN Sustainable Development Goals.
Keywords: Non-communicable diseases, Lower-middle income countries, Sustainable development goals, Hypertension epidemiology, India
1. Introduction
The United Nations (UN) has focused on increasing burden of non-communicable disease (NCDs) in middle- and low-income countries and has called for reducing this burden. In response, the World Health Organization (WHO) has committed to reducing premature mortality from NCDs by 25% by the year 2025 in its 25 × 25 target.1 WHO has proposed comprehensive plan to reduce smoking and tobacco use, harmful alcohol use, salt intake, physical inactivity, and elevated blood pressure and glucose levels to reduce the risk of premature mortality from NCDs under the NCD Global Monitoring Framework (NCD-GMF).2 Among the NCDs, the most important target is reduction in mortality from cardiovascular disease (CVD) and WHO has proposed, and participating countries have agreed, for relative reduction in tobacco use by 30%, harmful alcohol intake by 10%, salt consumption by 30%, prevalence of hypertension by 25%, control of CVD risk factors in at least 50% and stem the rising tide of obesity and diabetes.2 Lately, the UN has adopted the sustainable development goals (SDGs) and the goal number 3, target number 4 aims for a 33% reduction of NCD mortality by 2030.3 It has been estimated that achievement of these goals will require substantial reductions in CVD, which is the leading cause of premature NCD mortality and accounts for over half of all NCD-related deaths.4, 5, 6
The most important strategy for reducing CVD mortality, apart from smoking cessation, is blood pressure (BP) control.6, 7 BP control is poor worldwide. Prospective Urban Rural Epidemiology (PURE) study evaluated hypertension awareness, treatment and control in 17 countries at various stages of economic development and reported that control was about 50% in high income countries and less than 10% in lower middle income and low income countries.8 Studies in USA and Western Europe have reported increasing hypertension control over the last 50 years.9 US Joint National Committee-7 reported that hypertension treatment and control was about 25–30% in mid-sixties and increased to more than 70% in recent years.10 Similar data were reported by National Health and Nutrition Evaluation Surveys (NHANES) from 1988 to 2008.11 The NHANES studies from 1999 to 2012 reported that while prevalent hypertension was unchanged during these years (30–31%), increase was observed in hypertension treatment (from 60% to 75%) and its control especially among the treated (from 53% to 69%).12 Similar rates of hypertension treatment and control have been reported from many Western European and some high-income countries.8, 9
There is limited information on status of hypertension control in low and lower-middle income countries.13 In India, studies have reported low hypertension treatment and control rates in various parts of the country, lower in rural than in urban.14, 15, 16 Anchala et al performed a meta-analysis of studies that reported hypertension awareness, treatment and control.14 Low rates of hypertension awareness, treatment and control, respectively, were calculated in urban (42%, 38% and 20%) as well as rural areas (25%, 24% and 11%).14 South Asian cohorts in PURE study reported similar low rate of hypertension awareness, treatment and control, respectively, in urban (46%, 38% and 15%) as well as rural (33%, 24% and 9%) locations.17 Only a few studies in India have reported on changes in hypertension prevalence using serial studies,18, 19, 20, 21 however, time-trends in hypertension treatment and control using multiple studies with uniform methodology has not been performed. We prospectively performed multiple cross sectional studies among urban population in Jaipur, India, over the past 25 years to assess prevalence of various cardiovascular risk factors.22, 23, 24, 25, 26, 27 We reported increasing trends in cardiometabolic risk factors such as obesity, abdominal obesity, metabolic syndrome, diabetes and hypercholesterolemia.28 A stable trend in hypertension prevalence was observed in these studies.28 To determine trends in hypertension awareness, treatment and control over the 25-year period we performed the present study. We then projected these trends in hypertension prevalence, awareness, treatment and control to assess whether Indian populations are poised to achieve the hypertension control target of 50% proposed by WHO Global Monitoring framework.2
2. Methods
We performed a series of cross sectional epidemiological studies in Jaipur in western India (Jaipur Heart Watch, JHW) in the last 25 years to determine cardiovascular risk factors in urban participants.22, 23, 24, 25, 26, 27 All the studies were approved by institutional ethics committees and supported financially by different organizations. The first study (JHW-1) was conducted in years 1992–1994. This study was designed to investigate people at random and to cover large and varied areas of this city with the intention of including a wide range of urban subjects.22 Jaipur is divided into 70 municipal wards. Randomly chosen wards from different regions of the city were identified to cover different socioeconomic groups. Details of adult populations in those wards were available from the voters’ lists. The total adult population in each ward varied from 15,000 to 30,000. The male:female ratio of Jaipur residents >20 years old is 1000:865. We randomly selected 500 persons (268 men, 232 women) from each locality from the list of voters. When the random number corresponded to the individual <20 years of age it was assigned to the next person on the list. The target study sample was 3000 with a population-proportionate male:female ratio, thus 1609 men and 1391 women were invited to participate. Formula for calculation of sample size is based on WHO recommendations and reported earlier.22 In the second urban study (JHW-2) we targeted 950 men and 850 women in the same locations as in JHW-1 and could examine 1123 participants (62.4%, men 550 men, women 573).23 In this study we targeted all the participants for the fasting blood sample. The third (JHW-3), fourth (JHW-4), fifth (JHW-5) and sixth (JHW-6) studies were in middle-SES location-specific studies targeted at a smaller sample in the above three municipal wards24, 25, 26, 27 or in specific endogamous ethnic communities.24, 27 The sample sizes were derived using WHO guidelines to estimate differences in risk factor prevalence.29
2.1. Data collection
Methodological details have been reported earlier.22 A detailed proforma was utilized for data collection. Briefly, we collected information regarding demographic data, history of major illnesses such as coronary heart disease, hypertension, diabetes or high cholesterol levels, and smoking or tobacco intake. Brief questions were asked to evaluate physical activity and diet but the results were considered inadequate and not included in various analyses. Physical examination was performed to assess height, weight, waist and hip size and BP using previously reported methodology.30 BP was measured in sitting position using calibrated mercury instruments. Three readings were obtained at 5 min intervals and lowest value retained. We also obtained data on body mass index (BMI), and fasting blood glucose and total cholesterol, high density lipoprotein (HDL) cholesterol, triglycerides and low density lipoprotein (LDL) cholesterol. Internal and external quality control was maintained in all the studies to ensure uniformity of methodology.
2.2. Diagnostic criteria
Hypertension was diagnosed when systolic BP was ≥140 mm Hg and/or diastolic BP ≥ 90 mm Hg or a person was a known hypertensive. Hypertension awareness status was estimated as proportion of all participants with hypertension (BP ≥ 140 and/or ≥90 mm Hg) who were aware of their hypertensive status having been diagnosed before by a physician or any other healthcare provider. Treatment status was defined as (a) proportion of overall hypertensive participants on drug treatment or (b) aware/known hypertensive participants on treatment. Hypertension control was defined as BP < 140 mm Hg systolic and <90 mm Hg diastolic and determined as percentage of (a) all participants with hypertension, (b) participants with known hypertension and (c) hypertensive participants on drug treatment.29 Diagnostic criteria for other cardiovascular risk factors such as tobacco use and smokers, overweight and obesity, abdominal obesity, dyslipidemia and diabetes have been reported.28
2.3. Statistical analyses
Prevalence rates are reported in percent. Age-specific prevalence rates have been determined for decadal intervals from 20 to 70+ years. Age-adjustment of various prevalence rates has been performed by direct method using the WHO standard world population.29 Hypertension awareness, treatment and control rates are in percent. Age-adjustment of these rates has not been performed. Significance of trends in hypertension prevalence, awareness, treatment and control rates has been determined using Mantel-Haenszel X2 test for trend. Projections for hypertension awareness, treatment and control to the year 2030 have been performed using data of all the JHW studies (JHW-1–JHW-6). Projections were performed with Microsoft Excel software with the trend analysis command. Forecasting to the year 2030 was performed using logarithmic trend estimations within this program. 95% confidence intervals (CI) were calculated using Newcombe’s method.31 Two-tailed p values less than 0.05 have been considered significant.
3. Results
Total participants in various Jaipur Heart Watch studies are 7440 (men 4237, women 3203). In all the studies men outnumber women and age-group specific details are shown in Table 1. Age-group specific hypertension prevalence is reported in Table 2. There is a significantly increasing trend in hypertension prevalence. Age- and sex-adjusted hypertension prevalence in successive studies was 29.5%, 30.2%, 36.5%, 42.1%, 34.4% and 36.1% (R2 = 0.41, ptrend < 0.001).
Table 1.
Participants enrolled in various Jaipur Heart Watch studies.
| Study | Years performed | Year reported [Reference] | Target sample |
Participants enrolled |
|||
|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Total | |||
| JHW-1 | 1991–1994 | 199521 | 1600 | 1400 | 1415 | 797 | 2212 |
| JHW-2 | 1999–2001 | 200222 | 950 | 850 | 550 | 573 | 1123 |
| JHW-3 | 2003–2004 | 200423 | 320 | 280 | 226 | 232 | 458 |
| JHW-4 | 2006–2007 | 200724 | 750 | 650 | 556 | 571 | 1127 |
| JHW-5 | 2009–2011 | 201225 | 600 | 500 | 451 | 288 | 739 |
| JHW-6 | 2012–2014 | 201526 | 1250 | 1250 | 1039 | 742 | 1781 |
JHW: Jaipur Heart Watch.
Table 2.
Hypertension prevalence at various age-groups in the JHW studies.
| JHW-1 | JHW-2 | JHW-2 | JHW-4 | JHW-5 | JHW-6 | |
|---|---|---|---|---|---|---|
| Years | 1991–94 | 1999–01 | 2003–04 | 2006–07 | 2009–11 | 2012–14 |
| 20–29 | 10.9 | 10.2 | 14.1 | 20.7 | 22.7 | 16.2 |
| 30–39 | 20.9 | 25.7 | 34.6 | 36.2 | 19.6 | 27.5 |
| 40–49 | 34.8 | 40.3 | 57.0 | 63.3 | 36.8 | 41.4 |
| 50–59 | 61.6 | 54.5 | 74.4 | 67.7 | 54.9 | 60.0 |
| 60–69 | 55.7 | 59.0 | 77.6 | 72.2 | 64.2 | 67.9 |
| 70+ | 49.5 | 67.4 | 84.6 | 82.2 | 65.2 | 72.5 |
JHW: Jaipur Heart Watch.
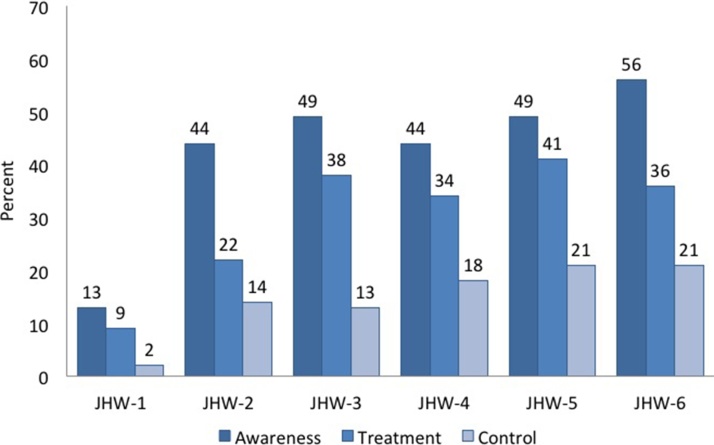
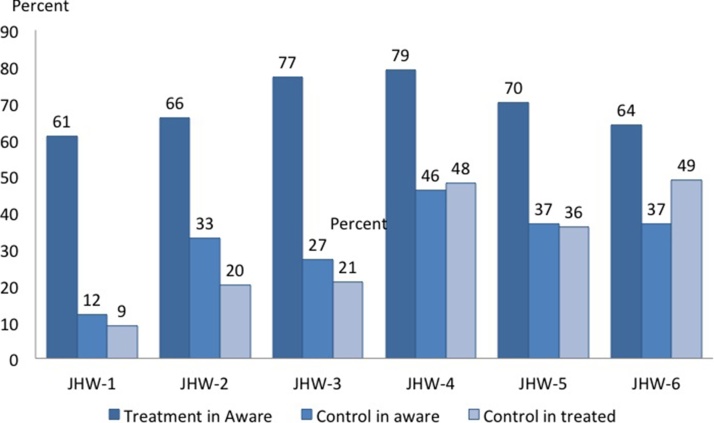
Trends in hypertension awareness show significant increase from 13% in JHW-1 to more than 45% in later studies (Fig. 1). Unadjusted awareness rates are 13%, 44%, 49%, 44%, 49% and 56% (R2 = 0.63). Trends in hypertension treatment among all participants with hypertension increased from 9% in JHW-1 to 22%, 38%, 34%, 41% and 36% in JHW-2–JHW-6 studies (R2 = 0.45). Among participants with known hypertension it increased from 61% in JHW-1 to 66%, 77%, 79%, 70% and 64% in JHW-2–JHW-6 studies respectively (R2 = 0.45) (Fig. 2). Significantly greater proportion of hypertension patients received treatment if they were aware of it (Fig. 2). Hypertension control was low among all hypertensive participants but increased from 2% in JHW-1 to 14%, 13%, 18%, 21% and 21% (R2 = 0.85) over the 25-year period (Fig. 1). Trends in hypertension control were significantly greater among aware hypertensive participants: 12% to 33%, 27%, 46%, 37% and 37% (R2 = 0.45) and treated hypertensives: 9% to 20%, 21%, 48%, 36% and 49% (R2 = 0.45) (ptrend < 0.001) (Fig. 2).
Fig. 1.
Trends in hypertension awareness, treatment and control in successive Jaipur Heart Watch studies. Data are in percent.
Fig. 2.
Hypertension treatment and control rates (%) in participants who are aware of the hypertensive status in successive Jaipur Heart Watch studies.
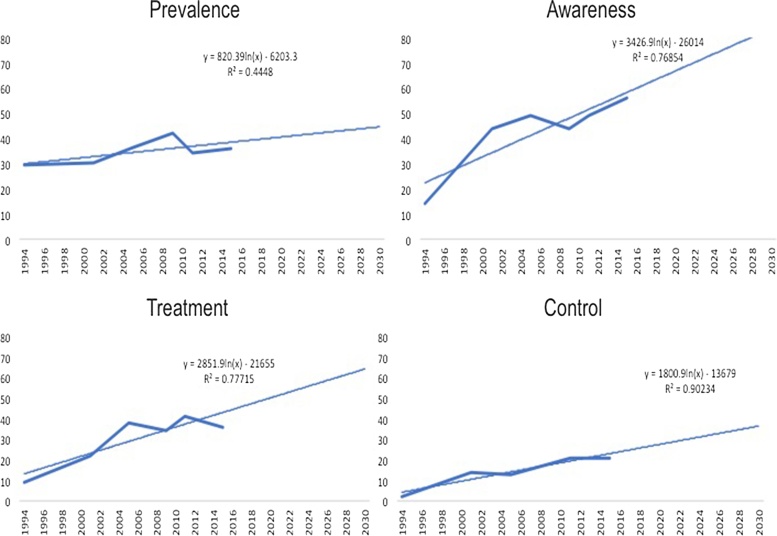
Projections for hypertension prevalence, awareness, treatment and control to the year 2030 using data from all JHW studies and logarithmic forecasting are shown in Fig. 3. Hypertension prevalence would increase to 44% (95% CI, 43–45%) in year 2030, a relative increase by 17%, instead of a relative decline by 25% by the year 2030 proposed by WHO.2 Calculations also show that hypertension awareness would increase to 82% (95% CI 81–83%) (logarithmic regression equation, y = 3426.9ln(x) − 26014), treatment rate to 62% (95% CI 61–63%) (y = 2851.9ln(x) − 21655) and control to 36% (95% CI 35–37%) (y = 1800.9ln(x) − 13679) (Fig. 3). WHO Global Monitoring Framework has recommended hypertension control in at least 50% patients with raised BP by the year 2025 to achieve cardiovascular disease control targets for UN Sustainable Development Goals.1, 3 The projections from the present study are significantly lower at 36% (p < 0.01).
Fig. 3.
Projections for hypertension prevalence, awareness, treatment and control rates among all hypertensive participants for the year 2030 using logarithmic forecasting from Jaipur Heart Watch studies.
4. Discussion
Hypertension prevalence has increased among an Indian urban population over the past 25 years. The rates of hypertension awareness, treatment and control are also increasing. This study also shows that better hypertension awareness is associated with greater hypertension treatment and its control. Increasing hypertension is opposite to targets of WHO Global Monitoring Framework.2 The increase in treatment and control rates are also lower than the proposed WHO targets. As this study is confined to an urban Indian population we cannot extrapolate the data to rural India where no similar studies exist. Previous Indian studies have reported that hypertension prevalence is increasing more rapidly in rural as compared to urban Indian populations.15 Therefore the prevalence of hypertension could be greater in rural populations in the next 15 years, a situation similar to high and middle income countries.8 Studies have also reported that hypertension treatment and control rates are 50% lower in rural than in the urban Indian populations14 and therefore the control would be lower than in the present study.
There are only limited studies in India that have reported changes in hypertension prevalence using prospective cross-sectional study design. Ahlawat et al. reported changes in prevalence of various cardiovascular risk factors in Chandigarh (North India) over a 30-year period.18 Age and sex adjusted prevalence of hypertension according to current criteria increased from 27% in 1968 to 45% in 1997. In Vellore (South India) studies in rural and urban populations were performed in 1991–94 and 2010–12 to assess changes in cardiovascular risk factors.19 In rural populations there was a doubling of hypertension while in the urban it increased by 50%. Age-adjusted prevalence of hypertension in rural population increased in men from 8% to 17% and in women from 7% to 12% while in urban populations the increase was in men from 20% to 27% and in women from 17% to 22%. Goyal et al. reported changes in risk factors in a rural Punjab population over a 20 year period from 1994 to 2012 and reported increase in hypertension prevalence from 15% to 27%.20 Roy et al reported changes in hypertension prevalence in Delhi and National Capital Region of India in urban and rural populations in 1991–94 and 2010–12.21 Hypertension prevalence increased in both populations, in urban from 23% to 42% and in rural from 11% to 29%. Similar increase in hypertension prevalence has been observed in other low and lower-middle income countries.13 In our study the change in hypertension prevalence has followed an uneven course and the difference in the age- and sex-adjusted prevalence in JHW-1 and JHW-6 studies in 29.5%–36.1%, a relative increase of +22%. This is lower than the urban studies from Chandigarh (+67%), Vellore (men +36%, women, +30%) and Delhi (+83%) and much lower than rural studies in Punjab (+102%), Vellore (men +115%, women 64%) and Delhi (+158%). Roy et al did not observe an increase in hypertension awareness, treatment and control rates in and around Delhi.21 This is in contrast to the present study where increasing trend in hypertension awareness, treatment and control is observed (Fig. 3).
NCDRiSC (NCD Risk Factor Collaboration) investigators studied changes in mean systolic BP and hypertension prevalence in various parts of the world including South Asian countries and India using multiple data sources.32 It was reported that hypertension prevalence in India increased from 1980 to 2015 in men from 24% to 28% (+16.7%) and in women from 22% to 27% (+22.7%). These results are not dissimilar to our study. Projected increase in hypertension by +17% in our urban population is contrary to the stated goals of WHO Global Monitoring Framework who advise a relative reduction in hypertension prevalence of 25%.2 Increase of hypertension in low and lower-middle income developing countries has been attributed to multiple factors.13, 16 Studies have reported that this is likely due to combination of demographic and epidemiological transition, changing lifestyles with increase in dietary fat and salt, low physical activity and increasing obesity and abdominal obesity.13, 16, 33 Studies have reported that social determinants of health, such as urbanization and higher wealth and educational status in India are associated with greater hypertension prevalence.17 There has been a rapid increase in overweight and obesity in India in the last 20 years and this correlates well with the increasing hypertension prevalence.34, 35 In a previous JHW study report we have shown that increasing overweight, abdominal obesity and obesity in India correlated significantly with the increasing hypertension prevalence.36
Awareness, treatment and control of hypertension is gradually increasing in India although there are large rural-urban disparities.14, 15 Anchala et al performed meta-analysis of hypertension epidemiology articles in India from 1953 to 2015.14 Overall estimates for rates of awareness, treatment, and control of hypertension were 42.0% (35.2–48.9), 37.6% (24.0–51.2), and 20.2% (11.6–28.7) for urban Indians and 25.3% (21.4–29.3), 25.1% (17.0–33.1), and 10.7% (6.5–15.0) for rural Indians. Similar urban-rural differences have been reported from other low-income countries.37 The WHO Study on Aging and Global Health (SAGE) evaluated hypertension prevalence, awareness, treatment and control in older adults >50 years of age.38 Hypertension prevalence was 32.3% in the Indian cohort (similar in urban and rural participants in this study)38 but awareness, treatment and control rates were similar to the present study. In our study, a slow increase in awareness, treatment and control is a cause of concern. Moreover, as our study is confined to urban Indians, it is likely that the rates of hypertension awareness, treatment and control would be lower in rural populations as reported in previous studies.14, 39 The current rates of hypertension awareness and control in this urban population of India are similar to the data in US about 50 years ago.40 More studies are needed to identify hypertension control trends in populations from low- and lower-middle income countries.
A number of measures are available for increasing hypertension treatment and control in India and other low income countries.9, 10, 16, 41, 42 Increasing awareness of hypertension with screening programs leads to greater chances of treatment and better control of hypertension.42 Similar findings are observed in the present study. Treatment and control rates in those of are aware of the hypertension are double to those not aware (Fig. 2). Other interventions to improve hypertension control include policy-level, health system-level, population-level and clinic based individual-level interventions. Policy and system level interventions should be focused on public education and screening, while population level interventions should focus on reduced intake of salt and alcohol, smoking cessation, promotion of healthy diet and facilitation of physical activity. Individual level interventions should be on better physician education who should promote individual lifestyle changes, appropriate pharmacotherapy and control of vascular risk factors along with efforts to improve adherence.41, 42, 43 Million Hearts Initiative in the US is focused on increasing hypertension control using policy, population level and clinic-based interventions.44 Similar program needs to be developed in India and other lower middle income countries to reduce hypertension related cardiovascular morbidity and mortality.
This study has strengths and limitations. Strengths include a 25-year span of multiple cross-sectional studies, similar locations and use of uniform methodology in all the studies. Some of the limitations such as nation-wide validity and applicability in absence of rural data and fluctuating hypertension prevalence (Table 2) have already been highlighted. Other limitations are lack of a single cohort prospective study, variable sample sizes, low female representation, variability in structure of communities and locations, no data on causes for increase in hypertension in each study, and lack of data on causes for low rates of awareness, treatment and control of hypertension. Increasing hypertension treatment and control is important for achieving the WHO Global Monitoring Framework targets for delivering UN Sustainable Development Goals in India. The SDG goal number 3 is focused on health and section 3.4 has recommended reduction in NCD related mortality by one-third through prevention and treatment strategies. To achieve this goal it would be important to focus on better control of hypertension in India.
Disclosures
No author has any conflicts of interest to declare.
References
- 1.World Health Organization. NCD global monitoring framework. Available at: http://www.who.int/nmh/global_monitoring_framework/en/; (Accessed March 14, 2017).
- 2.World Health Organization. Draft comprehensive global monitoring framework and targets for the prevention and control of noncommunicable diseases. Available at: http://apps.who.int/gb/ebwha/pdf_files/WHA66/A66_8-en.pdf; (Accessed March 14, 2017).
- 3.United Nations. Sustainable development goals. Available at: http://www.un.org/pga/wp-content/uploads/sites/3/2015/08/120815_outcome-document-of-Summit-for-adoption-of-the-post-2015-development-agenda.pdf; (Accessed March 17, 2017).
- 4.Kontis V., Mathers C.D., Rehm J. Contribution of six risk factors to achieving the 25 × 25 non-communicable disease mortality reduction target: a modeling study. Lancet. 2014;384:427–437. doi: 10.1016/S0140-6736(14)60616-4. [DOI] [PubMed] [Google Scholar]
- 5.Kontis V., Mathers C.D., Bonita R. Regional contributions of six preventable risk factors to achieving the 25 × 25 non-communicable disease mortality reduction target: a modeling study. Lancet Glob Health. 2015;3:e746–e757. doi: 10.1016/S2214-109X(15)00179-5. [DOI] [PubMed] [Google Scholar]
- 6.Sacco R.L., Roth G.A., Reddy K.S. The heart of 25 by 25: achieving the goal of reducing global and regional premature deaths from cardiovascular diseases and stroke: a modeling study from the American Heart Association and World Heart Federation. Circulation. 2016;133:e674–690. doi: 10.1161/CIR.0000000000000395. [DOI] [PubMed] [Google Scholar]
- 7.Olsen M.H., Angell S.Y., Asma S. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on Hypertension. Lancet. 2016;388:2665–2712. doi: 10.1016/S0140-6736(16)31134-5. [DOI] [PubMed] [Google Scholar]
- 8.Chow C.K., Teo K.K., Rangarajan S. Prevalence, awareness, treatment and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310:959–968. doi: 10.1001/jama.2013.184182. [DOI] [PubMed] [Google Scholar]
- 9.Poulter N., Prabhakaran D., Caulfield M. Hypertension. Lancet. 2015;386:801–812. doi: 10.1016/S0140-6736(14)61468-9. [DOI] [PubMed] [Google Scholar]
- 10.Chobanian A.V., Bakris G.L., Black H.R., Cushman W.C., Green L.A., Izzo J.L. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. [DOI] [PubMed] [Google Scholar]
- 11.Egan B.M., Zhao Y., Axon R.N. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 12.Egan B.M., Li J., Hutchison F.N., Ferdinand K.C. Hypertension in the United States, 1999-2012: progress toward Healthy People 2020 goals. Circulation. 2014;130:1692–1699. doi: 10.1161/CIRCULATIONAHA.114.010676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ibrahim M.M., Damasceno A. Hypertension in developing countries. Lancet. 2012;380:611–619. doi: 10.1016/S0140-6736(12)60861-7. [DOI] [PubMed] [Google Scholar]
- 14.Anchala R., Kannuri N.K., Pant H. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32:1170–1177. doi: 10.1097/HJH.0000000000000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta R. Convergence in urban-rural prevalence of hypertension in India. J Hum Hypertens. 2016;30:79–82. doi: 10.1038/jhh.2015.48. [DOI] [PubMed] [Google Scholar]
- 16.Gupta R., Khedar R.S., Panwar R.B. Strategies for better hypertension control in India and other lower-middle income countries. J Assoc Physicians India. 2016;64(9):58–64. [PubMed] [Google Scholar]
- 17.Gupta R., Kaur M., Islam S. Association of household wealth, educational status and social capital with hypertension awareness, treatment and control in South Asia. Am J Hypertens. 2017;30:373–381. doi: 10.1093/ajh/hpw169. [DOI] [PubMed] [Google Scholar]
- 18.Ahlawat S.K., Singh M.M.C., Kumar R., Kumari S., Sharma B.K. Time trends in the prevalence of hypertension and associated risk factors in Chandigarh. J Indian Med Assoc. 2002;100:547–555. [PubMed] [Google Scholar]
- 19.Oommen A.M., Abraham V.J., George K., Jose V.J. Rising trend of cardiovascular risk factors between 1991 and 1994 and 2010-2012: a repeat cross sectional survey in urban and rural Vellore. Indian Heart J. 2016;68:263–269. doi: 10.1016/j.ihj.2015.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goyal A., Kahlon P., Jain D. Trend in prevalence of coronary artery disease and risk factors over two decades in rural Punjab. BMJ Heart Asia. 2017;9:e010938. doi: 10.1136/heartasia-2017-010938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roy A., Praveen P.A., Amarchand R. Changes in hypertension prevalence, awareness, treatment and control rates over twenty years in National Capital Region of India. BMJ Open. 2017;7:e015639. doi: 10.1136/bmjopen-2016-015639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gupta R., Prakash H., Majumdar S., Sharma S.C., Gupta V.P. Prevalence of coronary heart disease and coronary risk factors in an urban population of Rajasthan. Indian Heart J. 1995;47:331–338. [PubMed] [Google Scholar]
- 23.Gupta R., Gupta V.P., Sarna M. Prevalence of coronary heart disease and risk factors in an urban Indian population: Jaipur Heart Watch-2. Indian Heart J. 2002;54:59–66. [PubMed] [Google Scholar]
- 24.Gupta R., Sarna M., Thanvi J., Rastogi P., Kaul V., Gupta V.P. High prevalence of multiple coronary risk factors in Punjabi Bhatia community: Jaipur Heart Watch-3. Indian Heart J. 2004;57:646–652. [PubMed] [Google Scholar]
- 25.Gupta R., Kaul V., Bhagat N. Trends in prevalence of coronary risk factors in an urban Indian population: Jaipur Heart Watch-4. Indian Heart J. 2007;59:346–353. [PubMed] [Google Scholar]
- 26.Gupta R., Sharma K.K., Gupta A. Persistent high prevalence of cardiovascular risk factors in the urban middle-class in India: Jaipur Heart Watch-5. J Assoc Physicians India. 2012;60(3):11–16. [PubMed] [Google Scholar]
- 27.Dhabariya R., Agrawal M., Gupta R., Mohan I., Sharma K.K. Cardiometabolic risk factors in the Agarwal business community in India: Jaipur Heart Watch-6. Indian Heart J. 2015;67:347–350. doi: 10.1016/j.ihj.2015.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gupta R., Guptha S., Gupta V.P., Agrawal A., Gaur K., Deedwania P.C. Twenty year trends in cardiovascular risk factors in India and influence of educational status. Eur J Prev Cardiol. 2012;19:1258–1271. doi: 10.1177/1741826711424567. [DOI] [PubMed] [Google Scholar]
- 29.Luepkar R.V., Evans A., McKeigue P., Reddy K.S. 3rd ed. World Health Organization; Geneva: 2002. Cardiovascular survey methods. [Google Scholar]
- 30.Gupta R., Sharma A.K., Gupta V.P., Bhatnagar S., Rastogi S., Deedwania P.C. Increased variance in blood pressure distribution and changing hypertension prevalence in an urban Indian population. J Hum Hypertens. 2003;17:535–540. doi: 10.1038/sj.jhh.1001588. [DOI] [PubMed] [Google Scholar]
- 31.Newcombe R.G. Two sided confidence intervals for the single proportion: comparison of seven methods. Stat Med. 1998;17:857–872. doi: 10.1002/(sici)1097-0258(19980430)17:8<857::aid-sim777>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 32.NCD Risk Factor Collaboration Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389:37–55. doi: 10.1016/S0140-6736(16)31919-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gupta R., Gupta S. Hypertension epidemiology in India: trends in prevalence, awareness, treatment and control. RUHS J Health Sci. 2017;2:40–46. [Google Scholar]
- 34.Siddiqui M.Z., Donato R. Overweight and obesity in India: policy issues from an exploratory multilevel analysis. Health Policy Plan. 2016;31:582–591. doi: 10.1093/heapol/czv105. [DOI] [PubMed] [Google Scholar]
- 35.Shrivastava U., Misra A., Mohan V., Unnikrishnan R., Bachani D. Obesity, diabetes and cardiovascular disease in India: public health challenges. Diabetes Res. 2017;13:65–80. doi: 10.2174/1573399812666160805153328. [DOI] [PubMed] [Google Scholar]
- 36.Gupta R., Gupta V.P., Bhagat N. Obesity is a major determinant of coronary risk factors in India: Jaipur Heart Watch Studies. Indian Heart J. 2008;60:26–33. [PubMed] [Google Scholar]
- 37.Sarki A.M., Nduka C.U., Stranges S., Kandala N.-B., Uthman O.A. Prevalence of hypertension in low- and middle-income countries: a systematic review and meta-analysis. Medicine. 2015;95:e1959. doi: 10.1097/MD.0000000000001959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lloyd-Sherlock P., Beard J., Minicucci N., Ebrahim S., Chatterji S. Hypertension among older adults in low- and middle-income countries: prevalence, awareness and control. Int J Epidemiol. 2015;43:116–128. doi: 10.1093/ije/dyt215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gupta R., Pandey R.M., Misra A. High prevalence and low hypertension awareness, treatment and control in Asian Indian women. J Hum Hypertens. 2012;26:585–593. doi: 10.1038/jhh.2011.79. [DOI] [PubMed] [Google Scholar]
- 40.Burt V.L., Cutler J.A., Higgins M. Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population data from the Health Examination Surveys, 1960 to 1991. Hypertension. 1995;26:60–69. doi: 10.1161/01.hyp.26.1.60. [DOI] [PubMed] [Google Scholar]
- 41.Gupta R., Yusuf S. Towards better hypertension control in India. Indian J Med Res. 2014;139:657–660. [PMC free article] [PubMed] [Google Scholar]
- 42.Angell S., De Cock M., Frieden T.R. A public health approach to global management of hypertension. Lancet. 2015;385:825–827. doi: 10.1016/S0140-6736(14)62256-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Frieden T.R., Bloomberg M.R. Saving an additional 100 million lives. Lancet. 2017 doi: 10.1016/S0140-6736(17)32443-1. EPub. [DOI] [PubMed] [Google Scholar]
- 44.Lloyd-Jones D.M., Huffman M.D., Karmali K.N. Estimating longitudinal risks and benefits from cardiovascular preventive therapies among Medicare patients: the Million Hearts Longitudinal ASCVD Risk Assessment Tool. J Am Coll Cardiol. 2017;69:1617–1636. doi: 10.1016/j.jacc.2016.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]