Abstract
Background
Patients with polytrauma are expected to have a higher risk of mortality than the summation of expected mortality for their individual injuries. This study was designed to investigate the outcome of polytrauma patients, diagnosed by abbreviated injury scale (AIS) ≥ 3 for at least two body regions, at a level I trauma center.
Methods
Detailed data of 694 polytrauma patients and 2104 non-polytrauma patients with an overall Injury Severity Score (ISS) ≥ 16 and hospitalized between January 1, 2009, and December 31, 2014 for treatment of all traumatic injuries, were retrieved from the Trauma Registry System. Two-sided Fisher exact or Pearson chi-square tests were used to compare categorical data. The unpaired Student t-test was used to analyze normally distributed continuous data, and the Mann–Whitney U-test was used to compare non-normally distributed data. Propensity-score matching in a 1:1 ratio was performed using NCSS software with logistic regression to evaluate the effect of polytrauma on in-hospital mortality.
Results
There was no significant difference in short-term mortality between polytrauma and non-polytrauma patients, regardless of whether the comparison was made among the total patients (11.4% vs. 11.0%, respectively; p = 0.795) or among the selected propensity score-matched groups of patients following controlled covariates including sex, age, systolic blood pressure, co-morbidities, Glasgow Coma Scale scores, injury region based on AIS.
Conclusions
Polytrauma defined by AIS ≥3 for at least two body regions failed to recognize a significant difference in short-term mortality among trauma patients.
Keywords: Polytrauma, Abbreviated injury scale, Injury severity, Monotrauma, Multiple trauma, Mortality
At a glance commentary
Scientific background on the subject
Although polytrauma is generally used to describe trauma patients whose injuries were severe and involved multiple body regions, the term ‘polytrauma’ lacks a universally accepted definition. This study was designed to validate the definition of polytrauma determined by abbreviated injury scale (AIS) ≥ 3 for at least two body regions.
What this study adds to the field
This study revealed that patients with polytrauma defined by AIS ≥ 3 failed to recognize a significant difference in short-term mortality between the polytrauma and non-polytrauma patients. Additional criteria such as the relevant pathophysiologic change may be required for a better definition of polytrauma.
The monotrauma indicates an injury to one body region and multitrauma or multiple trauma depict those who had injuries to more than one body region, regardless of the injury severity. In addition, severely injured and major trauma had been used to indicate a patient with high injury severity [1], [2]. Under the basic concept of a combination of injuries that causes a life-threatening condition, polytrauma is generally used to describe trauma patients whose injuries were severe and involved multiple body regions [3], [4], compromise the patient's physiology and potentially cause dysfunction of uninjured organs [5]. These polytrauma patients are expected to have a higher risk of morbidity and mortality than the summation of expected morbidity and mortality of their individual injuries [1].
Some authors suggested that at least two anatomical regions have to be injured for a patient to be identified as having critically ill trauma [4], [5], [6], [7]. Border et al. [4] and Osterwalder [8] defined polytrauma as presence of ≥2 significant injuries. However, the cut-off of abbreviated injury scale (AIS) ≥ 2 would enable identifying a patient with fairly low injury severity score (ISS) such as 8, 12, and 13 as having polytrauma, which would not make the score specific enough [5]. Furthermore, Butcher et al. define ‘polytrauma’ as an injured patient with AIS ≥3 points in at least two different body regions [8]. With associated higher mortality, more frequent ICU admissions, and longer hospital and ICU stays, this characteristic captured the greatest percentage of the worst outcomes and a significantly larger percent of the clinically diagnosed polytrauma patients than those who were diagnosed via the definition, ISS >15 or ISS >17 [7].
However, although a universally accepted definition for polytrauma is vital for comparing datasets, the term ‘polytrauma’ lacks a universally accepted and validated definition [1]. Before applying the definition of the term in the clinical setting, we designed this study to investigate the outcome of the polytrauma patients, diagnosed by AIS ≥3 for at least two body regions, admitted and treated for all trauma injuries at a level I trauma center. The primary hypothesis of this study was that these polytrauma patients have a worse outcome than those patients with similar injury severity but without polytrauma.
Methods
Ethics statement
This study was pre-approved by the Institutional Review Board (IRB) of the Chang Gung Memorial Hospital (approval number 104-1783B). Informed consent was waived according to IRB regulations.
Study design
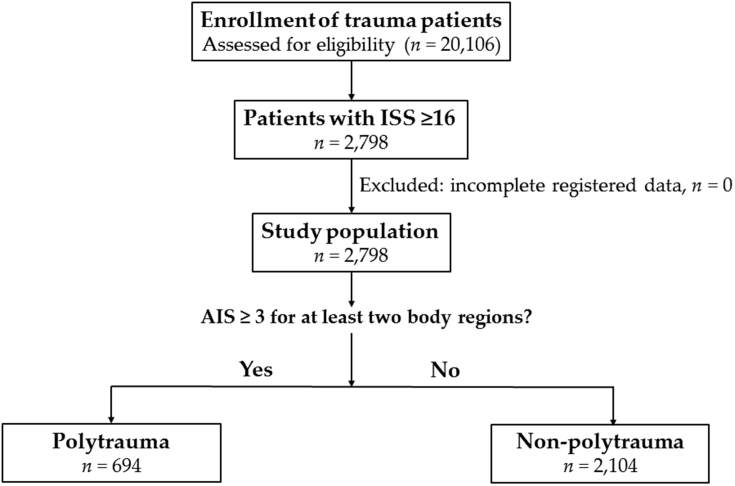
This retrospective study reviewed data of all 20,106 hospitalized patients registered in the Trauma Registry System of a level I regional trauma center [9], [10] from January 1, 2009, to December 31, 2014 (Fig. 1). The Trauma Registry System, which was established in our hospital since 2009, collected the data of patient characteristics, injury characteristics, injury mechanism, and outcome of patients hospitalized due to all trauma cause. All the registered data were input into hospital-based databank by two qualified nurses with specific responsibility for the integrity of the registered data. All patients with an overall ISS ≥16 and hospitalized for treatment of traumatic injuries were included in the study (n = 2798). A patient with AIS ≥3 in two or more different body regions was considered to have polytrauma (n = 694). Other patients who had an overall ISS ≥16 but did not fit into the above criteria of polytrauma were defined as non-polytrauma patients (n = 2104). This group consisted of patients with (1) an AIS of 4 or 5 with injury at one body region and no additional or only minor (1 or 2 points) injury at a second ISS region, (2) an AIS of 3 with injury at one body region and two additional injuries (2 points) at a second and third ISS region. Patients with incomplete registered data would be excluded (n = 0). Detailed patient information retrieved from the Trauma Registry System including: age; sex; trauma mechanism; initial Glasgow Coma Scale (GCS) score in the emergency department (ED); vital signs assessed by the physician upon arrival at the ED and procedures performed by the physician at the ED (cardiopulmonary resuscitation, intubation, chest tube insertion, and blood transfusion); AIS severity score for each body region; ISS; The Trauma and Injury Severity Score (TRISS); rates of associated injuries; revised trauma score (RTS); hospital length of stay (LOS); LOS in ICU; and in-hospital mortality. Pre-existing comorbidities and chronic diseases including diabetes mellitus (DM), hypertension (HTN), coronary artery diseases (CAD), congestive heart failure (CHF), cerebrovascular accident (CVA), and end-stage renal disease (ESRD) were also identified. The ISS is expressed as the median and interquartile range (IQR, Q1–Q3). Odds ratios (ORs) of the associated conditions and injuries of the patients were calculated with 95% confidence intervals (CIs). The data collected were compared using IBM SPSS Statistics for Windows, version 20.0 (IBM Corp., Armonk, NY, USA). Two-sided Fisher exact or Pearson chi-square tests were used to compare categorical data. The unpaired Student t-test was used to analyze normally distributed continuous data, which was reported as mean ± standard deviation. The Mann–Whitney U-test was used to compare non-normally distributed data. To minimize confounding effects of baseline covariates that may be related to the outcome assessment, propensity scores were estimated by multiple logistic regression analysis with adjustments for patient age, sex, systolic blood pressure (SBP), GCS, injuries based on AIS, and ISS. After calculation of the propensity scores, a 1:1 matched study group was created by the Greedy method and a 0.2 caliper width using NCSS software (NCSS 10; NCSS Statistical software, Kaysville, Utah). A conditional logistic regression was used for evaluating the effect of polytrauma on mortality with crude OR being calculated with 95% CI as well as the adjusted odd ratio (AOR) for mortality adjusted by the ISS. All results are presented as the mean ± standard error. A p-value less than 0.05 was considered statistically significant.
Fig. 1.
Flow chart of the study population.
Results
Injury characteristics and severity of patients with polytrauma
As shown in Table 1, the mean age of patients with polytrauma was less than of those without polytrauma (46.2 ± 19.9 years and 50.8 ± 22.2 years, respectively; p < 0.001). No significant sex-specific predominance was noted among patients with polytrauma. Significantly lower rates of pre-existing co-morbidities including DM, HTN, and CVA were found among patients with polytrauma than those without polytrauma. GCS scores were significantly lower for patients with polytrauma than for non-polytrauma patients (11.5 ± 4.4 vs. 11.9 ± 4.2, respectively; p = 0.028); however, the difference in GCS scores was less than 1 point. Significantly more patients with polytrauma had a GCS ≤8 and significantly fewer patients with polytrauma had a GCS ≥13 compared to non-polytrauma patients. Analysis of AIS, regardless of the criteria of AIS ≥1 or ≥3, revealed that patients with polytrauma had sustained significantly higher rates of face, thoracic, abdomen, and extremity injuries than non-polytrauma patients, while non-polytrauma patients had sustained significantly higher rates of head and neck injury. In addition, a significantly higher ISS was found in patients with polytrauma than in non-polytrauma patients (median [IQR: Q1–Q3], 26 [22–34] vs. 17 [16], [17], [18], [19], [20], [21], respectively; p < 0.001). When stratified by ISS (16–24 or ≥25), among patients with polytrauma, more patients had an ISS ≥ 25 and fewer patients had an ISS of 16–24 as compared to non-polytrauma patients. The patients with polytrauma presented with a significantly lower RTS (6.8 ± 1.5 vs. 7.0 ± 1.3, respectively; p < 0.001) and TRISS (0.803 ± 0.246 vs. 0.872 ± 0.200, respectively; p < 0.001) than that in non-polytrauma patients.
Table 1.
Demographics and injury characteristics of patients with and without polytrauma.
| Variables | Polytrauma n = 694 | Non-polytrauma n = 2104 | Odds Ratio (95% CI) | p |
|---|---|---|---|---|
| Age | 46.2 ± 19.9 | 50.8 ± 22.2 | – | <0.001 |
| Sex | ||||
| Male | 479 (69.0) | 1385 (65.8) | 1.2 (0.96–1.39) | 0.122 |
| Female | 215 (31.0) | 719 (34.2) | 0.9 (0.72–1.04) | 0.122 |
| Co-morbidity | ||||
| DM | 72 (10.4) | 299 (14.2) | 0.7 (0.53–0.92) | 0.010 |
| HTN | 141 (20.3) | 551 (26.2) | 0.7 (0.58–0.89) | 0.002 |
| CAD | 19 (2.7) | 75 (3.6) | 0.8 (0.46–1.27) | 0.294 |
| CHF | 1 (0.1) | 15 (0.7) | 0.2 (0.03–1.52) | 0.141 |
| CVA | 7 (1.0) | 102 (4.8) | 0.2 (0.09–0.43) | <0.001 |
| ESRD | 0 (0.0) | 3 (0.1) | – | 1.000 |
| GCS | 11.5 ± 4.4 | 11.9 ± 4.2 | – | 0.028 |
| ≤8 | 195 (28.1) | 493 (23.4) | 1.3 (1.05–1.55) | 0.013 |
| 9–12 | 86 (12.4) | 267 (12.7) | 1.0 (0.75–1.26) | 0.837 |
| ≥13 | 413 (59.5) | 1344 (63.9) | 0.8 (0.70–0.99) | 0.039 |
| AIS, n (%) | ||||
| Head/Neck | 521 (75.1) | 1780 (84.6) | 0.5 (0.45–0.68) | <0.001 |
| Face | 222 (32.0) | 453 (21.5) | 1.7 (1.42–2.07) | <0.001 |
| Thorax | 496 (71.5) | 391 (18.6) | 11.0 (9.00–13.38) | <0.001 |
| Abdomen | 265 (38.2) | 184 (8.7) | 6.4 (5.20–7.99) | <0.001 |
| Extremity | 510 (73.5) | 595 (28.3) | 7.0 (5.79–8.53) | <0.001 |
| AIS ≥ 3, n (%) | ||||
| Head/Neck | 467 (67.3) | 1679 (79.8) | 0.5 (0.43–0.63) | <0.001 |
| Face | 26 (3.7) | 0 (0.0) | – | <0.001 |
| Thorax | 459 (66.1) | 248 (11.8) | 14.6 (11.90–17.95) | <0.001 |
| Abdomen | 179 (25.8) | 60 (2.9) | 11.8 (8.70–16.11) | <0.001 |
| Extremity | 347 (50.0) | 54 (2.6) | 38.0 (27.89–51.68) | <0.001 |
| ISS, median (IQR) | 26 (22–34) | 17 (16–21) | – | <0.001 |
| 16–24 | 240 (34.6) | 1701 (80.8) | 0.1 (0.10–0.15) | <0.001 |
| ≥25 | 454 (65.4) | 403 (19.2) | 8.0 (6.60–9.66) | <0.001 |
| RTS | 6.8 ± 1.5 | 7.0 ± 1.3 | – | <0.001 |
| TRISS | 0.8 ± 0.25 | 0.9 ± 0.2 | – | <0.001 |
| Mortality, n (%) | 79 (11.4) | 232 (11.0) | 1.0 (0.79–1.36) | 0.795 |
| Hospital LOS (days) | 20.2 ± 15.9 | 15.4 ± 15.9 | – | <0.001 |
| ICU, n (%) | ||||
| ISS 16–24 | 143 (20.6) | 1161 (55.2) | 0.2 (0.17–0.26) | <0.001 |
| ISS ≥ 25 | 380 (54.8) | 371 (17.6) | 5.7 (4.69–6.81) | <0.001 |
| LOS in ICU (days) | 7.1 ± 9.8 | 6.9 ± 12.1 | – | 0.670 |
Associated management and injuries among patients with polytrauma
Patients with polytrauma exhibited higher ORs for presenting with worse hemodynamic measures than non-polytrauma patients. These measures included a systolic blood pressure (SBP) of <90 mmHg, heart rate of >100 beats/min, and respiratory rate of <10 or >29 times/min (Table 2). In addition, patients with polytrauma had higher odds for requiring procedures at the ED, including cardiopulmonary resuscitation, intubation, chest tube insertion, and blood transfusion. Regarding the associated injuries (Table 3), patients with polytrauma had statistically significantly lower ORs for sustaining epidural hematomas (OR 0.6, 95% CI 0.49–0.77; p < 0.001), subdural hematomas (OR 0.4, 95% CI 0.37–0.53; p < 0.001), and cerebral contusions (OR 0.6, 95% CI 0.48–0.75; p < 0.001) than non-polytrauma patients. Notably, 297 (42.8%) of the 694 polytrauma patients and 1629 (77.4%) of the 2104 non-polytrauma patients have a head/neck AIS of ≥4 points. In contrast, patients with polytrauma had statistically significantly higher ORs for sustaining maxillofacial trauma, thoracic trauma, abdominal trauma, and extremity trauma than non-polytrauma patients.
Table 2.
Worse physiological response upon arrival and procedures performed at the emergency department for patients with and without polytrauma.
| Variables | Polytrauma n = 694 | Non-polytrauma n = 2104 | Odds Ratio (95% CI) | p |
|---|---|---|---|---|
| Physiology at ED, n (%) | ||||
| SBP < 90 mmHg | 77 (11.1) | 88 (4.2) | 2.9 (2.08–3.93) | <0.001 |
| HR > 100 beats/min | 273 (39.3) | 543 (25.8) | 1.9 (1.56–2.23) | <0.001 |
| RR < 10 or > 29 times/min | 35 (5.0) | 45 (2.1) | 2.4 (1.55–3.81) | <0.001 |
| Procedures at ED, n (%) | ||||
| Cardiopulmonary resuscitation | 12 (1.7) | 12 (0.6) | 3.1 (1.37–6.86) | 0.004 |
| Intubation | 114 (16.4) | 261 (12.4) | 1.4 (1.09–1.76) | 0.007 |
| Chest tube insertion | 99 (14.3) | 72 (3.4) | 4.7 (3.42–6.45) | <0.001 |
| Blood transfusion | 180 (25.9) | 154 (7.3) | 4.4 (3.50–5.62) | <0.001 |
Table 3.
Significant associated injuries among patients with and without polytrauma.
| Variables | Polytrauma n = 694 | Non-polytrauma n = 2104 | Odds Ratio (95% CI) | P |
|---|---|---|---|---|
| Head trauma, n (%) | ||||
| Epidural hematoma (EDH) | 112 (16.1) | 500 (23.8) | 0.6 (0.49–0.77) | <0.001 |
| Subdural hematoma (SDH) | 249 (35.9) | 1178 (56.0) | 0.4 (0.37–0.53) | <0.001 |
| Cerebral contusion | 106 (15.3) | 487 (23.1) | 0.6 (0.48–0.75) | <0.001 |
| Maxillofacial trauma, n (%) | ||||
| Nasal fracture | 17 (2.4) | 18 (0.9) | 2.9 (1.49–5.68) | 0.001 |
| Maxillary fracture | 87 (12.5) | 197 (9.4) | 1.4 (1.06–1.81) | 0.016 |
| Mandibular fracture | 31 (4.5) | 42 (2.0) | 2.3 (1.43–3.68) | <0.001 |
| Thoracic trauma, n (%) | ||||
| Rib fracture | 283 (40.8) | 288 (13.7) | 4.3 (3.57–5.28) | <0.001 |
| Hemothorax | 98 (14.1) | 72 (3.4) | 4.6 (3.38–6.38) | <0.001 |
| Pneumothorax | 114 (16.4) | 63 (3.0) | 6.4 (4.62–8.78) | <0.001 |
| Hemopneumothorax | 97 (14.0) | 75 (3.6) | 4.4 (3.21–6.02) | <0.001 |
| Lung contusion | 71 (10.2) | 59 (2.8) | 4.0 (2.77–5.64) | <0.001 |
| Thoracic vertebral fracture | 30 (4.3) | 52 (2.5) | 1.8 (1.13–2.82) | 0.012 |
| Abdominal trauma, n (%) | ||||
| Intra-abdominal injury | 59 (8.5) | 86 (4.1) | 2.2 (1.55–3.07) | <0.001 |
| Hepatic injury | 117 (16.9) | 62 (2.9) | 6.7 (4.84–9.21) | <0.001 |
| Splenic injury | 64 (9.2) | 37 (1.8) | 5.7 (3.75–8.59) | <0.001 |
| Retroperitoneal injury | 10 (1.4) | 5 (0.2) | 6.1 (2.09–18.02) | 0.001 |
| Renal injury | 23 (3.3) | 20 (1.0) | 3.6 (1.95–6.54) | <0.001 |
| Lumbar vertebral fracture | 48 (6.9) | 32 (1.5) | 4.8 (3.05–7.59) | <0.001 |
| Sacral vertebral fracture | 19 (2.7) | 8 (0.4) | 7.4 (3.21–16.92) | <0.001 |
| Extremity trauma, n (%) | ||||
| Clavicle fracture | 120 (17.3) | 195 (9.3) | 2.0 (1.60–2.62) | <0.001 |
| Humeral fracture | 51 (7.3) | 31 (1.5) | 5.3 (3.37–8.36) | <0.001 |
| Radial fracture | 80 (11.5) | 52 (2.5) | 5.1 (3.59–7.37) | <0.001 |
| Ulnar fracture | 52 (7.5) | 41 (1.9) | 4.1 (2.68–6.20) | <0.001 |
| Pelvic fracture | 93 (13.4) | 56 (2.7) | 5.7 (4.01–7.98) | <0.001 |
| Femoral fracture | 173 (24.9) | 28 (1.3) | 24.6 (16.33–37.12) | <0.001 |
| Patella fracture | 22 (3.2) | 12 (0.6) | 5.7 (2.81–11.59) | <0.001 |
| Tibia fracture | 94 (13.5) | 30 (1.4) | 10.8 (7.11–16.50) | <0.001 |
| Fibular fracture | 68 (9.8) | 25 (1.2) | 9.0 (5.66–14.41) | <0.001 |
Outcome of patients with polytrauma
As shown in Table 1, mortality was found in 79 (11.4%) of 694 patients with polytrauma and 232 (11.0%) of 2104 patients without polytrauma. Patients with polytrauma did not present a significantly different lethality than non-polytrauma patients (OR 1.0, 95% CI 0.79–1.36; p = 0.795). Those fatal patients were significantly older, had a lower GCS scores, had a higher rate of head/neck injury, and had a significantly higher ISS than those patients who survived (Table 4). After propensity-score matching, mortality outcome was compared in 181 well-balanced pairs of patients (Table 4). In these propensity score–matched patients, there was no significant difference in sex, age, co-morbidities, SBP, GCS, injury region based on AIS, and ISS. Logistic regression analysis of these well-balanced pairs of patients showed that the association of polytrauma did not significantly influence mortality (OR 0.5, 95% CI 0.16–1.32; p = 0.147). In addition, compared to non-polytrauma patients, patients with polytrauma had significantly longer hospital LOS (20.2 days vs. 15.4 days, respectively; p < 0.001), and a higher proportion of patients had an ISS ≥25 (54.8% vs. 17.6%, respectively; p < 0.001) but a lower proportion of patients with an ISS of 16–24 (20.6% vs. 55.2%, respectively; p < 0.001) were admitted to the ICU; however, the LOS in the ICU was not significantly different between patients with or without polytrauma (7.1 days vs. 6.9 days, respectively; p = 0.670) (Table 1).
Table 4.
Patient cohorts before and after the propensity-score matching.
| Before matching |
After matching |
|||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Death n = 311 | Survival n = 2487 | OR (95%CI) | P | Death n = 181 | Survival n = 181 | OR (95%CI) | P |
| Sex | ||||||||
| Male | 205 (65.9) | 1659 (66.7) | 1.0 (0.75–1.24) | 0.780 | 133 (73.5) | 133 (73.5) | 1.0 (0.63–1.60) | 1.000 |
| Female | 106 (34.1) | 828 (33.3) | 1.0 (0.81–1.33) | 0.780 | 48 (26.5) | 48 (26.5) | 1.0 (0.63–1.60) | 1.000 |
| Age | 56.2 ± 21.4 | 48.9 ± 21.6 | – | <0.001 | 52.9 ± 21.5 | 52.9 ± 21.0 | – | 0.980 |
| Co-morbidity | ||||||||
| DM | 40 (12.9) | 331 (13.3) | 1.0 (0.68–1.37) | 0.826 | 13 (7.2) | 13 (7.2) | 1.0 (0.45–2.22) | 1.000 |
| HTN | 86 (27.7) | 606 (24.4) | 1.2 (0.91–1.55) | 0.205 | 41 (22.7) | 41 (22.7) | 1.0 (0.61–1.64) | 1.000 |
| CAD | 21 (6.8) | 73 (2.9) | 2.4 (1.45–3.95) | <0.001 | 6 (3.3) | 6 (3.3) | 1.0 (0.32–3.16) | 1.000 |
| CHF | 3 (1.0) | 13 (0.5) | 1.9 (0.53–6.54) | 0.410 | 0 (0.0) | 0 (0.0) | – | – |
| CVA | 15 (4.8) | 94 (3.8) | 1.3 (0.74–2.25) | 0.370 | 3 (1.7) | 3 (1.7) | 1.0 (0.20–5.02) | 1.000 |
| ESRD | 2 (0.6) | 1 (0.0) | 16.1 (1.46–177.97) | 0.034 | 0 (0.0) | 0 (0.0) | – | – |
| SBP mmHg | 141.9 ± 60.1 | 146.6 ± 38.1 | – | 0.184 | 150.9 ± 49.5 | 149.2 ± 39.6 | – | 0.710 |
| GCS | 6.8 ± 4.4 | 12.5 ± 3.8 | – | <0.001 | 8.1 ± 4.8 | 8.0 ± 4.8 | – | 0.710 |
| AIS, n (%) | ||||||||
| Head/Neck | 275 (88.4) | 2026 (81.5) | 1.7 (1.21–2.50) | 0.002 | 161 (89.0) | 161 (89.0) | 1.0 (0.52–1.93) | 1.000 |
| Face | 40 (12.9) | 635 (25.5) | 0.4 (0.31–0.61) | <0.001 | 20 (11.0) | 20 (11.0) | 1.0 (0.52–1.93) | 1.000 |
| Thorax | 77 (24.8) | 810 (32.6) | 0.7 (0.52–0.89) | 0.005 | 43 (23.8) | 43 (23.8) | 1.0 (0.62–1.62) | 1.000 |
| Extremity | 85 (27.3) | 1020 (41.0) | 0.5 (0.42–0.70) | <0.001 | 51 (28.2) | 51 (28.2) | 1.0 (0.63–1.58) | 1.000 |
| ISS | 25 (25–34) | 19 (16–24) | – | <0.001 | 25 (20–29) | 25 (18–29) | – | 0.076 |
| Polytrauma | 79 (25.4) | 615 (24.7) | 1.0 (0.79–1.36) | 0.795 | 45 (24.9) | 51 (28.2) | 0.5 (0.16–1.32) | 0.147 |
Discussion
Many studies had defined polytrauma as an ISS >15 [11], an ISS > 16 [12], an ISS > 18 [13], an ISS ≥ 18 [14], [15], or an ISS > 25 [16]. If lower cut-offs are used (>15 or >16), a fairly low injury severity, e.g., AIS of 2 in two regions plus AIS of 3 (22 + 22 + 32 = 17), may be included. If higher cut-offs are used (>20 or >25), the specificity would be increased at the expense of the exclusion of patients with AIS = 3 injuries in two body regions [1]. Different studies have pointed out the limited prognostic value of ISS in terms of mortality prediction [17], [18], [19]. Furthermore, ISS is hardly ever calculated on admission, which makes it difficult to be a useful tool for prognostic during initial resuscitation [20]. Whatever the definition of polytrauma presents a difference or not in term of mortality, ISS could be only more useful for secondary triage or ICU admission. In contrast, the ‘polytrauma’ definition of Butcher and colleagues with AIS ≥3 in at least two different body regions [2], [6], [8] seemed more reasonable and feasible in identifying the polytrauma patients. This definition was shown to be a better predictor of morbidity and mortality than the definition with an ISS >15 or ISS >17 [2], [6], [8]. However, in this study, we failed to demonstrate a significant difference in short-term mortality between the polytrauma and non-polytrauma patients. These results are in contrast to the basic assumption that polytrauma patients are expected to have a higher risk of mortality than the summation of expected mortality of their individual injuries [1]. Because the ISS score had been already calculated from three different injured body regions, if there was no worse outcome of these polytrauma patients, then we can just use multitrauma or multiple trauma to profile these patients and use ISS to depict the patient outcome, and there was no necessary of the use of polytrauma to describe the patient condition. Moreover, Paffrath et al. had reported the mortality rate of the polytrauma patients with AIS ≥3 in at least two different body regions was even lower (18.7%) than in the whole group with an ISS ≥ 16 points (20.4%) [17]. The discrepancy of our results to those reported by Butcher and colleagues may be attributed to the exclusion of non-polytrauma patients with head injuries in their series. Because the head injury may have an inherently morbidity and mortality rate than the injury to other regions [21], [22], the exclusion of the head injuries from the non-polytrauma patients can offer advantages for outcome comparison but would limit its feasibility in the clinical setting. In this study, 77.4% of non-polytrauma patients had a head/neck AIS ≥4 points. Polytrauma can indeed affect all body regions and all organs in an endless amount of combinations. The exclusion of the majority of patients from one specific group would result in a bias in the interpretation and limit the usefulness of conclusions in clinical application.
AIS/ISS does not reflect the physiological course after injury, which can be very dynamic in nature and may profoundly influence outcomes. Therefore, the definition of polytrauma by the number of injured body regions would make it difficult to be distinguished from the concept of “multiple trauma”. To improve the specificity of the polytrauma definition, some additional qualifying criteria for the body regions had been proposed, such as laparotomy involvement [23]; injuries leading to severe shock [24]; and involving at least one vital organ necessitating patient admission to a trauma ICU [25]. However, these additional criteria seemed to be limited and unverified. The levels of variation differ among trauma centers may be quite different. A combination of injury severity, relevant pathophysiologic change, or physiologic changes in the clinical condition is useful [3]. Kondo et al. documented a good predictive power for GCS, age, and SBP in terms of mortality after an examination of the datasets from 35,732 patients of 115 hospitals from the Japan Trauma Data Bank [26]. An international consensus meeting in 2012 first tried to specify the term ‘polytrauma’ by combining the concept of injuries in different body regions and physiological risk factors [27]. With a minimum addition of one of five standardized physiological responses (hypotension [SBP ≤ 90 mmHg], unconsciousness [GCS score ≤ 8], acidosis [BE ≤ −6.0], coagulopathy [PTT ≥ 40 s or INR ≥ 1.4], and age [≥70 years]) to the definition of ISS ≥ 16 and AIS ≥ 3 for at least two body regions, an improved definition of polytrauma was determined [5], [28]. A sustained increase in coverage of mortality was noted, with the ancillary physiologic variables supplementary to the injury scoring [5].
Our study has some limitations that should be acknowledged. First, owing to the retrospective design of the study, there is inherent selection bias. Second, the patients declared dead on hospital arrival or at the accident scene were not included in the Trauma Registry Database, which may have led to a bias. Third, the study population, limited to a single urban trauma center in southern Taiwan, may not be representative of other populations and a prospective study conducted in multiple trauma centers may provide more validated information. Fourth, the descriptive study design with the lack of data regarding indication of hospitalization and admission into ICU, type of surgery, and the long-term mortality of patients prevents evaluation of the effects of any particular treatment intervention. This means that we could only rely on the assumption of uniform assessment and management of patients with or without polytrauma. For example, in this study, the patients of the polytrauma group present with worse hymodynamic measures and GCS compared to that of the non-polytrauma group, but the short-term mortality was similar between the groups. Although the results support the concept that the definition of polytrauma is insufficient, however, the results may be confounded by some un-explored factors, such as there was a possibility that the trauma team activation was more common for the polytrauma group and therefore this group of patients has been treated more aggressively in the resuscitation stage. Finally, the cost and resource used were not evaluated in this study.
Conclusion
This study of hospitalized trauma patients based on the Trauma Registry System at a level I trauma center revealed that patients with polytrauma defined by AIS ≥3 failed to recognize a significant difference in short-term mortality among trauma patients.
Conflicts of interest
The authors declare that they have no competing interests.
Funding
This research was supported by a grant CMRPG8G1301 from Chang Gung Memorial Hospital to Ching-Hua Hsieh.
Footnotes
Peer review under responsibility of Chang Gung University.
References
- 1.Butcher N., Balogh Z.J. The definition of polytrauma: the need for international consensus. Injury. 2009;40(S 4):S12–S22. doi: 10.1016/j.injury.2009.10.032. [DOI] [PubMed] [Google Scholar]
- 2.Butcher N.E., D'Este C., Balogh Z.J. The quest for a universal definition of polytrauma: a trauma registry-based validation study. J Trauma Acute Care Surg. 2014;77:620–623. doi: 10.1097/TA.0000000000000404. [DOI] [PubMed] [Google Scholar]
- 3.Tscherne H. The treatment of the seriously injured at an emergency station. Chirurg. 1966;37:249–252. [PubMed] [Google Scholar]
- 4.Border J.R., LaDuca J., Seibel R. Priorities in the management of the patient with polytrauma. Prog Surg. 1975;14:84–120. doi: 10.1159/000398211. [DOI] [PubMed] [Google Scholar]
- 5.Pape H.C., Lefering R., Butcher N., Peitzman A., Leenen L., Marzi I. The definition of polytrauma revisited: an international consensus process and proposal of the new 'Berlin definition'. J Trauma Acute Care Surg. 2014;77:780–786. doi: 10.1097/TA.0000000000000453. [DOI] [PubMed] [Google Scholar]
- 6.Tscherne H., Regel G., Sturm J.A., Friedl H.P. Degree of severity and priorities in multiple injuries. Chirurg. 1987;58:631–640. [PubMed] [Google Scholar]
- 7.Butcher N., Balogh Z.J. AIS>2 in at least two body regions: a potential new anatomical definition of polytrauma. Injury. 2012;43:196–199. doi: 10.1016/j.injury.2011.06.029. [DOI] [PubMed] [Google Scholar]
- 8.Osterwalder J.J. Could a regional trauma system in eastern Switzerland decrease the mortality of blunt polytrauma patients? A prospective cohort study. J Trauma. 2002;52:1030–1036. doi: 10.1097/00005373-200206000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Hsieh C.H., Hsu S.Y., Hsieh H.Y., Chen Y.C. Differences between the sexes in motorcycle-related injuries and fatalities at a Taiwanese level I trauma center. Biomed J. 2017;40:113–120. doi: 10.1016/j.bj.2016.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hsieh C.H., Liu H.T., Hsu S.Y., Hsieh H.Y., Chen Y.C. Motorcycle-related hospitalizations of the elderly. Biomed J. 2017;40:121–128. doi: 10.1016/j.bj.2016.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sikand M., Williams K., White C., Moran C.G. The financial cost of treating polytrauma: implications for tertiary referral centres in the United Kingdom. Injury. 2005;36:733–737. doi: 10.1016/j.injury.2004.12.026. [DOI] [PubMed] [Google Scholar]
- 12.Biewener A., Aschenbrenner U., Rammelt S., Grass R., Zwipp H. Impact of helicopter transport and hospital level on mortality of polytrauma patients. J Trauma. 2004;56:94–98. doi: 10.1097/01.TA.0000061883.92194.50. [DOI] [PubMed] [Google Scholar]
- 13.Hildebrand F., Giannoudis P., Kretteck C., Pape H.C. Damage control: extremities. Injury. 2004;35:678–689. doi: 10.1016/j.injury.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 14.Bone L.B., Babikian G., Stegemann P.M. Femoral canal reaming in the polytrauma patient with chest injury. A clinical perspective. Clin Orthop Relat Res. 1995;318:91–94. [PubMed] [Google Scholar]
- 15.Pape H.C., Remmers D., Rice J., Ebisch M., Krettek C., Tscherne H. Appraisal of early evaluation of blunt chest trauma: development of a standardized scoring system for initial clinical decision making. J Trauma. 2000;49:496–504. doi: 10.1097/00005373-200009000-00018. [DOI] [PubMed] [Google Scholar]
- 16.McLain R.F. Functional outcomes after surgery for spinal fractures: return to work and activity. Spine. 2004;29:470–477. doi: 10.1097/01.brs.0000092373.57039.fc. [DOI] [PubMed] [Google Scholar]
- 17.Paffrath T., Lefering R., Flohe S. How to define severely injured patients? -- an Injury Severity Score (ISS) based approach alone is not sufficient. Injury. 2014;45(S 3):S64–S69. doi: 10.1016/j.injury.2014.08.020. [DOI] [PubMed] [Google Scholar]
- 18.Haider A.H., Villegas C.V., Saleem T., Efron D.T., Stevens K.A., Oyetunji T.A. Should the IDC-9 Trauma Mortality Prediction Model become the new paradigm for benchmarking trauma outcomes? J Trauma Acute Care Surg. 2012;72:1695–1701. doi: 10.1097/TA.0b013e318256a010. [DOI] [PubMed] [Google Scholar]
- 19.Tohira H., Jacobs I., Mountain D., Gibson N., Yeo A. Systematic review of predictive performance of injury severity scoring tools. Scand J Trauma Resuscitation Emerg Med. 2012;20:63. doi: 10.1186/1757-7241-20-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Napolitano L.M., Ferrer T., McCarter R.J., Jr., Scalea T.M. Systemic inflammatory response syndrome score at admission independently predicts mortality and length of stay in trauma patients. J Trauma. 2000;49:647–652. doi: 10.1097/00005373-200010000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Patel H.C., Bouamra O., Woodford M., King A.T., Yates D.W., Lecky F.E. Trends in head injury outcome from 1989 to 2003 and the effect of neurosurgical care: an observational study. Lancet. 2005;366:1538–1544. doi: 10.1016/S0140-6736(05)67626-X. [DOI] [PubMed] [Google Scholar]
- 22.Holland M.C., Mackersie R.C., Morabito D., Campbell A.R., Kivett V.A., Patel R. The development of acute lung injury is associated with worse neurologic outcome in patients with severe traumatic brain injury. J Trauma. 2003;55:106–111. doi: 10.1097/01.TA.0000071620.27375.BE. [DOI] [PubMed] [Google Scholar]
- 23.Cerra F.B., Mazuski J., Teasley K., Nuwer N., Lysne J., Shronts E. Nitrogen retention in critically ill patients is proportional to the branched chain amino acid load. Crit Care Med. 1983;11:775–778. doi: 10.1097/00003246-198310000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Deby-Dupont G., Haas M., Pincemail J., Braun M., Lamy M., Deby C. Immunoreactive trypsin in the adult respiratory distress syndrome. Intensive Care Med. 1984;10:7–12. doi: 10.1007/BF00258062. [DOI] [PubMed] [Google Scholar]
- 25.Blacker D.J., Wijdicks E.F. Clinical characteristics and mechanisms of stroke after polytrauma. Mayo Clin Proc. 2004;79:630–635. doi: 10.4065/79.5.630. [DOI] [PubMed] [Google Scholar]
- 26.Kondo Y., Abe T., Kohshi K., Tokuda Y., Cook E.F., Kukita I. Revised trauma scoring system to predict in-hospital mortality in the emergency department: Glasgow Coma Scale, Age, and Systolic Blood Pressure score. Crit Care. 2011;15:R191. doi: 10.1186/cc10348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pape H.C. Classification of patients with multiple injuries--is the polytrauma patient defined adequately in 2012? Injury. 2012;43:127–128. doi: 10.1016/j.injury.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 28.Rau C.S., Wu S.C., Kuo P.J., Chen Y.C., Chien P.C., Hsieh H.Y. Polytrauma defined by the new Berlin definition: a validation test based on propensity-score matching approach. Int J Environ Res Publ Health. 2017;14:E1045. doi: 10.3390/ijerph14091045. [DOI] [PMC free article] [PubMed] [Google Scholar]