Abstract
Background
This study aimed to investigate associations between self-reported sleep duration and general and abdominal obesity in Korean adults stratified according to gender and age.
Methods
Data from 41,805 adults, 18–110 years of age, collected by the Korea National Health and Nutrition Examination Survey (KNHANES) in 2007 and 2015, were analyzed. Multivariable logistic regression was used to calculate adjusted odds ratios (AORs) and 95% confidence intervals (CIs) for obesity and abdominal obesity by sleep duration after controlling for sociodemographic and lifestyle variables.
Results
Among individuals 30–49 years of age, there was an increased AOR for obesity only for sleep duration ≤ 5 hour/day compared with sleep duration 6 to 8 hour/day, both in men (OR, 1.25; 95% CI, 1.02–1.54) and women (OR, 1.56; 95% CI, 1.29–1.90), after controlling for covariates. Regarding women, there was increased AOR for abdominal obesity for sleep duration ≤ 5 hour/day (OR, 1.45; 95% CI, 1.18–1.78) and ≥ 9 hour/day (OR, 1.38; 95% CI, 1.09–1.76) compared with sleep duration 6 to 8 hour/day. However, for elderly individuals (≥ 65 years), there was a negative association between sleep duration ≤ 5 hour/day and obesity, but not with abdominal obesity, in both men and women.
Conclusion
This study demonstrated a significant association between sleep duration and obesity, which varied according to gender and age.
Keywords: Sleep Duration, Obesity, Abdominal Obesity, Sex, Age, KNHANES
Graphical Abstract
INTRODUCTION
Sleep plays a vital role in maintaining homeostasis and promoting individual health.1 The duration of sleep has shown decreasing secular trends alongside changes in modern society that require longer hours of work, more shift work and night activity, and technology use.2,3,4 These influences have reduced the average duration of sleep and have modified sleep patterns across westernized populations, with increased reports of fatigue, tiredness, and excessive daytime sleepiness.3 Published data from the National Sleep Foundation demonstrate a significant decline in the average duration of sleep of Americans in the past 100 years, with a loss of approximately 1.5 hours per night, from an average 9.0 hours per night in 1910 to an average 7.5 hours per night in 2014, and an average of 7.1 hours per night reported in 2015.5 Many have attributed this sleep curtailment to lifestyle changes influenced by cultural, social, and environmental factors.6,7,8,9
Many clinical studies have investigated the relationship between self-reported short sleep duration and a variety of adverse health outcomes such as obesity, type 2 diabetes, hypertension and cardiovascular disease, and mortality.10,11,12,13,14,15,16,17,18 Although these results do not necessarily imply a causal-effect relationship, they do point to a new interest in the health and social implications of sleep shortage and the potential importance for public health in modern society. However, a recent study reported that, compared with regular sleep duration of 6 to 8 hour/day, short sleep defined as < 6 hour/day, significantly increased the risk for central obesity and metabolic health risk in a healthy adult cohort,19 which suggests a causal-effect relationship.
Because obesity and body mass generally reflect years of accumulated morbidity and lifestyle factors, it is possible that the relationship between sleep duration and body mass differ between the gender and across age groups.20 For example, obesity in young adulthood may reflect more recent lifestyle and health factors, one of which may be short sleep duration. However, obesity in older age may reflect decades of accumulated risk factors, including comorbid conditions and hormonal factors, which in aggregate outweigh any effect(s) of short sleep duration. In Korea, there was a report that short sleep duration of ≤ 5 hour/day is significantly associated with increased risk of general and abdominal obesity in a total of 8,717 adults aged 20–65 years.21 In another study with 2,499 children and 7,431 adolescents in Korea, shorter sleep duration was significantly associated with an increase in body mass index (BMI) z-score.22
Men and women have different lifestyles, co-morbidities, hormonal influences, and social concepts, suggesting the possibility of different gender-related effects on sleep patterns and obesity. Women may experience severe sleep problems as well as increases in obesity and waist circumference due to menopause, and there are objective sleep disturbances in elderly men and women.23
Many previous studies have demonstrated that the relationship between sleep duration and age is nonlinear, suggesting important clues that these relationships may differ among adolescents, young adults, middle-age adults, and older adults.23,24 For example, the need for sleep is greater among adolescents and young adults, while some sleep disturbances peak in middle or elderly age.20 Nevertheless, it remains unclear whether there are gender and age, or racial or ethnic differences and associations, between sleep duration and obesity.
Although biological mechanisms linking sleep curtailment and obesity remain unclear, reduced circulating leptin and elevated ghrelin levels25,26,27 and inflammatory cytokines, such as high-sensitivity C-reactive protein,28 have been proposed as possible explanations in healthy young subjects. If sleep duration has clinical effects on obesity, modification of sleep pattern(s) may become an important intervention for obesity and its prevention.
Despite its public health significance, there are few reports describing the association between obesity and sleep duration according to gender and age. In an attempt to explain why there have been inconsistent results when analyzing sleep duration and obesity, this cross-sectional study aimed to assess the association between sleep duration and obesity — stratified according to age and gender — in a representative population-based sample of Korean adults using data from the Korea National Health and Nutrition Examination Survey (KNHANES) 2007 and 2015.
METHODS
Data source and study sample
The KNHANES is a nationally representative, population-based, cross-sectional survey of health and nutritional status among the Korean population.29 This survey consists of three distinct elements: health interview, health examination, and nutritional review.
Sampling weights were used to account for complex sampling to represent the entire non-institutionalized Korean population. Furthermore, to avoid bias from longitudinal changes in age and gender distributions, these factors were adjusted to reflect the Korean population distributions each year.
In the present study, data were collected from adults (≥ 18 years of age) who participated in three KNHANES cycles (2007–2009, 2010–2012, and 2013–2015) for the analysis of self-reported sleep duration patterns. Briefly, from a total of 56,752 participants ≥ 18 years of age, participants with missing data for sleep duration (n = 5,207), BMI (n = 209), and waist circumference (n = 96) were excluded. Individuals with missing values for any covariates, including education, marital status, household income, smoking, alcohol consumption, physical activity, and gender (n = 9,435) were also excluded. The final sample consisted of 41,805 adults (19,391 men; 22,414 women).
Operational definitions: sleep duration and other variables
Obesity was diagnosed using anthropometric data from each health examination. According to the Korean Society for the Study of Obesity (KSSO)30 and the World Health Organization (WHO) criteria,31 obesity is defined as a BMI ≥ 25 kg/m2 among individuals ≥ 18 years of age. Abdominal obesity was defined as waist circumference ≥ 90 cm in men and ≥ 85 cm in women according to the KSSO.32 The height and weight of all subjects were measured by a trained investigator while they wore light clothing and no shoes. Height was measured to the nearest 0.1 cm by using SECA 225 (SECA, Hamburg, Germany), and weight was measured to the nearest 0.1 kg using GL-6000-20 scale (CAS Co., Seoul, Korea). Sleep duration was defined as the self-reported response to the question: “How many hours of sleep do you usually get in a day on average?” The responses were categorized as ≤ 5 hour/day, 6 to 8 hour/day, and ≥ 9 hour/day. In addition, a self-reported questionnaire in the KNHANES 2007 and 2015 was used to obtain socioeconomic data for the following covariates based on previous literature: age, education, marital status, household income, alcohol intake, smoking status, and physical activity. Regular physical activity was dichotomized as “yes” or “no”: “no” was defined as no walking, moderate activity, or vigorous activity during a recent week; “yes” was defined as any physical activity with walking, moderate activity, or vigorous activity defined as below. Walking consisted of sessions of ≥ 30 minutes 5 days per week during a recent week and included all forms of walking. Moderate physical activity consisted of activity that was more strenuous or made one breath harder than usual and involved 30 minutes sessions ≥ 5 times per week during a recent week. Vigorous physical activity was defined as engaging in intense physical activity that made one very tired or breathing significantly more difficult than usual, and involved ≥ 20 minutes sessions (each time) 3 days per week during a recent week (e.g., running, jogging, mountain climbing, fast cycling, fast swimming, playing soccer, playing basketball, skipping rope, playing squash or singles tennis, transporting heavy objects). Work schedule patterns were grouped as daytime fixed work, shift work or other. Age was classified into four groups: 18–29 years (young adults); 30–49 years (middle-age adults); 50–64 years (older adults); and ≥ 65 years (elderly adults).
Statistical analyses
The KNHANES sampling weights accounting for the complex survey design, survey non-response and post-stratification were used.29 Continuous and categorical variables were compared among the three categories of self-reported sleep duration using analysis of variance (ANOVA) test and the χ2 test, respectively. Nominal variables were presented as number and percentage, and continuous variables were presented as mean ± standard error of the mean (SEM). Multivariable logistic regression was used to measure the adjusted odds ratios (AORs) and 95% confidence intervals (CIs) for obesity and abdominal obesity according to sleep duration, after controlling for education, marital status, household income, alcohol consumption, smoking status, and physical activity. All analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Ethics statement
All subjects participated voluntarily and provided informed consent for data collection. The KNHANES protocol was approved by the Korean Ministry of Health and Welfare, and the study was performed in accordance with the guidelines of the Declaration of Helsinki. The study was approved by the Institutional Review Board (IRB) of the Kangwon National University Hospital (IRB number: KNUH-2016-07-007).
RESULTS
Baseline characteristics of Korean adults according to gender and self-reported sleep duration
In the present study, there were 41,805 adults (19,391 men [46.4%] and 22,414 women [53.6%]). The mean (± SEM) age was 43.8 ± 0.13 years; BMI was 23.7 ± 0.02 kg/m2; waist circumference was 81.1 ± 0.08 cm; and sleep duration was 6.9 ± 1.3 hour/day (Table 1). General obesity was present in 13,203 (31.7%) participants and abdominal obesity in 10,712 (23.9%) (Table 1). There was a statistically higher prevalence of obesity (36.6% vs. 26.2%; P < 0.001) and abdominal obesity (25.8% vs. 21.9%; P < 0.001) in men compared with women, respectively.
Table 1. Baseline characteristics of participants in the KNHANES 2007–2015.
| Variables | Total | Men | Women | P valuea | |
|---|---|---|---|---|---|
| No. (%) | 41,805 (100) | 19,391 (46.4) | 22,414 (53.6) | ||
| Age, yr | 43.8 ± 0.13 | 43.9 ± 0.16 | 43.6 ± 0.15 | 0.06 | |
| 18–29 | 5,817 (21.2) | 2,533 (21.2) | 3,284 (21.1) | 0.002 | |
| 30–49 | 16,802 (44.4) | 7,209 (43.5) | 9,593 (45.3) | ||
| 50–64 | 11,125 (23.3) | 5,302 (24.0) | 5,823 (22.6) | ||
| ≥ 65 | 8,061 (11.1) | 4,347 (11.2) | 3,714 (11.0) | ||
| BMI, kg/m2 | 23.7 ± 0.02 | 24.1 ± 0.03 | 23.1 ± 0.03 | < 0.001 | |
| Waist circumference, cm | 81.10 ± 0.08 | 84.3 ± 0.09 | 77.5 ± 0.10 | < 0.001 | |
| Obesity | 13,203 (31.7) | 6,918 (36.6) | 6,285 (26.2) | < 0.001 | |
| Abdominal obesity | 10,712 (23.9) | 5,225 (25.8) | 5,487 (21.9) | < 0.001 | |
| Education, yr | < 0.001 | ||||
| ≤ 6 | 5,896 (10.1) | 1,982 (6.9) | 3,914 (13.6) | ||
| 7–12 | 15,311 (35.1) | 7,151 (34.0) | 8,160 (36.3) | ||
| ≥ 13 | 20,598 (54.8) | 10,258 (59.1) | 10,340 (50.2) | ||
| Marital status | < 0.001 | ||||
| Single | 6,610 (23.4) | 3,409 (26.9) | 3,201 (19.6) | ||
| Married | 30,472 (67.8) | 14,928 (68.5) | 15,544 (67.1) | ||
| Separated/divorced/widowed | 4,723 (8.7) | 1,054 (4.6) | 3,669 (13.3) | ||
| Household income | < 0.001 | ||||
| Lowest | 7,380 (14.1) | 3,419 (13.5) | 3,961 (14.8) | ||
| Lower middle | 10,579 (25.6) | 4,911 (25.2) | 5,668 (26.2) | ||
| Upper middle | 11,840 (30.1) | 5,493 (30.7) | 6,437 (29.6) | ||
| Highest | 12,006 (30.1) | 5,568 (30.7) | 6,438 (29.4) | ||
| Work schedule pattern (n = 33,353) | < 0.001 | ||||
| Daytime workers | 16,134 (53.0) | 8,740 (55.5) | 7,394 (49.7) | ||
| Shift workers | 4,548 (15.7) | 2,434 (16.2) | 2,114 (14.9) | ||
| Other | 12,671 (31.3) | 5,770 (28.2) | 6,901 (35.4) | ||
| Alcohol use | < 0.001 | ||||
| Non-drinker | 7,412 (14.8) | 2,418 (9.8) | 4,994 (20.2) | ||
| Moderate drinkers, ≤ 1–4 times/mon | 24,138 (59.1) | 9,300 (51.6) | 14,838 (67.4) | ||
| Heavy drinkers, ≥ 2 times/wk | 10,255 (26.1) | 7,673 (38.6) | 2,582 (12.5) | ||
| Smoking | < 0.001 | ||||
| Non-smoker | 23,018 (51.0) | 3,510 (20.0) | 19,508 (85.2) | ||
| Current smoker | 12,493 (33.6) | 10,536 (55.2) | 1,957 (9.7) | ||
| Former smoker | 6,294 (15.4) | 5,345 (24.8) | 949 (5.1) | ||
| Physical activity | < 0.001 | ||||
| Yes | 16,822 (39.0) | 8,339 (41.5) | 8,483 (36.2) | ||
| No | 24,983 (61.0) | 11,052 (58.5) | 13,931 (63.8) | ||
Data were summarized in number (%) or mean ± SEM, unless otherwise specified.
KNHANES = Korea National Health and Nutrition Examination Survey, BMI = body mass index, SEM = standard error of mean.
aP value: The χ2 test or t-test was used to compare categorical variables or continuous variables between men and women, respectively.
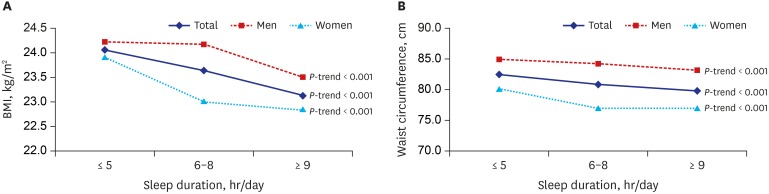
Table 2 summarizes the baseline characteristics of the 41,805 participants according to self-reported sleep duration. Sleep duration of 6 to 8 hour/day was reported by 77.6% of the subjects, and 14.7% slept ≤ 5 hour/day. Sleeping ≤ 5 hour/day was associated with a significant increase in general and abdominal obesity. The prevalence of obesity and abdominal obesity according to self-reported sleep duration is presented in Fig. 1. As sleep duration shortened, obesity and abdominal obesity became more prevalent.
Table 2. Baseline characteristics of Korean adults according to self-reported sleep duration in the KNHANES 2007–2015.
| Variables | Sleep duration (hr/day) | P valuea | |||
|---|---|---|---|---|---|
| ≤ 5 | 6–8 | ≥ 9 | |||
| No. (%) | 6,149 (14.7) | 32,456 (77.6) | 3,200 (7.7) | ||
| Age, yr | 50.0 ± 0.3 | 43.0 ± 0.1 | 41.6 ± 0.4 | < 0.001 | |
| BMI, kg/m2 | 24.1 ± 0.1 | 23.6 ± 0.0 | 23.1 ± 0.1 | < 0.001 | |
| Waist circumference, cm | 82.4 ± 0.2 | 81.0 ± 0.1 | 79.8 ± 0.2 | < 0.001 | |
| Obesity | 2,166 (36.3) | 10,120 (31.3) | 917 (27.3) | < 0.001 | |
| Abdominal obesity | 1,948 (29.8) | 7,940 (23.1) | 824 (22.9) | < 0.001 | |
| Gender | < 0.001 | ||||
| Men | 2,563 (47.4) | 15,458 (54.0) | 1,370 (45.4) | ||
| Women | 3,586 (52.6) | 16,998 (46.0) | 1,830 (54.6) | ||
| Education, yr | < 0.001 | ||||
| ≤ 6 | 1,670 (20.9) | 3,614 (7.9) | 612 (13.6) | ||
| 7–12 | 2,490 (39.4) | 11,674 (34.5) | 1,147 (33.9) | ||
| ≥ 13 | 1,989 (39.8) | 17,168 (57.6) | 1,441 (52.5) | ||
| Marital status | < 0.001 | ||||
| Single | 637 (16.9) | 5,283 (23.6) | 690 (32.7) | ||
| Married | 4,165 (65.3) | 24,139 (69.1) | 2,168 (59.2) | ||
| Separated/divorced/widowed | 1,347 (17.8) | 3,034 (7.3) | 342 (8.1) | ||
| Household income | < 0.001 | ||||
| Lowest | 1,775 (22.8) | 4,821 (12.0) | 784 (20.7) | ||
| Lower middle | 1,655 (26.1) | 8,048 (25.4) | 876 (27.5) | ||
| Upper middle | 1,366 (25.4) | 9,618 (31.1) | 856 (28.5) | ||
| Highest | 1,353 (25.7) | 9,969 (31.5) | 684 (23.3) | ||
| Work schedule pattern (n=33,353) | < 0.001 | ||||
| Daytime workers | 2,094 (52.2) | 13,069 (54.1) | 971 (42.6) | ||
| Shift workers | 669 (16.7) | 3,485 (15.0) | 394 (20.9) | ||
| Other | 1,791 (31.1) | 9,797 (30.9) | 1,083 (36.5) | ||
| Alcohol use | < 0.001 | ||||
| Non-drinker | 1,384 (19.1) | 5,345 (13.7) | 683 (17.8) | ||
| Moderate drinkers, ≤ 1–4 times/mon | 3,196 (53.0) | 19,177 (60.2) | 1,765 (58.6) | ||
| Heavy drinkers, ≥ 2 times/wk | 1,569 (27.9) | 7,934 (26.1) | 752 (23.6) | ||
| Smoking | 0.386 | ||||
| Non-smoker | 3,477 (52.3) | 17,802 (50.8) | 1,739 (51.0) | ||
| Current smoker | 1,751 (32.3) | 9,746 (33.7) | 996 (34.1) | ||
| Former smoker | 921 (15.4) | 4,908 (15.5) | 465 (14.9) | ||
| Physical activity | < 0.001 | ||||
| Yes | 2,435 (38.0) | 13,224 (39.5) | 1,163 (34.8) | ||
| No | 3,714 (62.0) | 19,232 (60.5) | 2,037 (65.2) | ||
Data were summarized in number (%) or mean ± SEM, unless otherwise specified.
KNHANES = Korea National Health and Nutrition Examination Survey, BMI = body mass index, SEM = standard error of mean, ANOVA = analysis of variance.
aP value: The χ2 test or ANOVA test was used to compare categorical variables or continuous variables across the groups of sleep duration, respectively.
Fig. 1. Association between self-reported sleep duration and BMI and waist circumference among Korean adults from 2007 to 2015.
BMI = body mass index.
Association between self-reported sleep duration and obesity and abdominal obesity according to age and gender in Korean adults
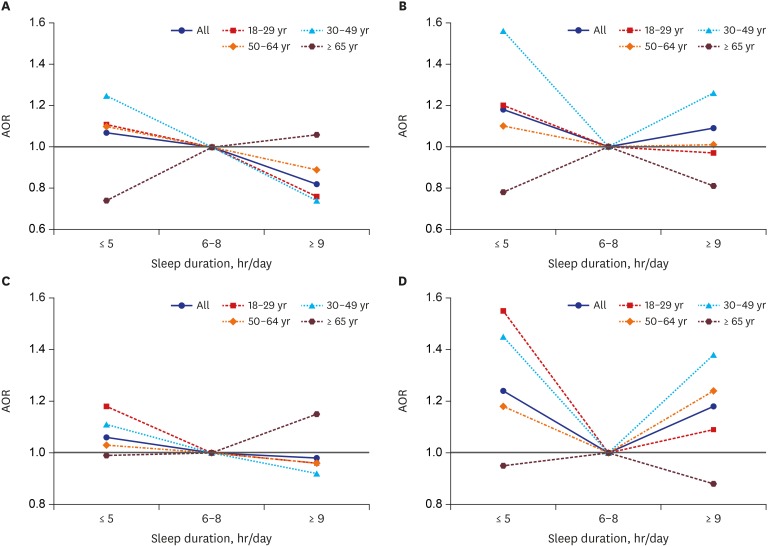
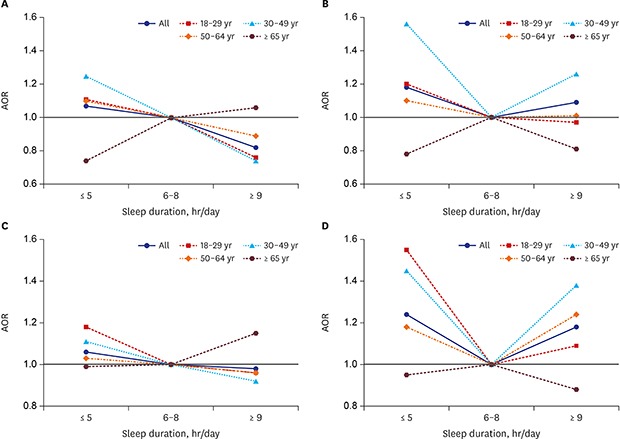
The association between sleep duration and obesity according to age and gender is shown in Table 3 and Fig. 2, after controlling for education, marital status, household income, alcohol consumption, smoking status, and physical activity. The ORs and 95% CIs for obesity and abdominal obesity across the three categories of sleep duration, using 6 to 8 hour/day of sleep as a reference, are presented in Tables 3 and 4.
Table 3. Association between self-reported sleep duration and obesity in the KNHANES 2007–2015.
| Variables | Total (n = 41,805) | Men (n = 19,391) | Women (n = 22,414) | ||||
|---|---|---|---|---|---|---|---|
| AORa | 95% CI | AORa | 95% CI | AORa | 95% CI | ||
| Total, hr | |||||||
| ≤ 5 | 1.13 | 1.05–1.23 | 1.07 | 0.95–1.22 | 1.18 | 1.07–1.32 | |
| 6–8 | 1.00 | 1.00 | 1.00 | ||||
| ≥ 9 | 0.83 | 0.74–0.93 | 0.82 | 0.69–0.96 | 1.09 | 0.93–1.27 | |
| 18–29 yr, hr | |||||||
| ≤ 5 | 1.13 | 0.87–1.47 | 1.11 | 0.77–1.61 | 1.20 | 0.82–1.76 | |
| 6–8 | 1.00 | 1.00 | 1.00 | ||||
| ≥ 9 | 0.77 | 0.59–0.99 | 0.76 | 0.52–1.11 | 0.97 | 0.68–1.38 | |
| 30–49 yr, hr | |||||||
| ≤ 5 | 1.36 | 1.18–1.57 | 1.25 | 1.02–1.54 | 1.56 | 1.29–1.90 | |
| 6–8 | 1.00 | 1.00 | 1.00 | ||||
| ≥ 9 | 0.89 | 0.73–1.07 | 0.74 | 0.54–1.01 | 1.26 | 1.00–1.58 | |
| 50–64 yr, hr | |||||||
| ≤ 5 | 1.09 | 0.94–1.25 | 1.10 | 0.88–1.37 | 1.10 | 0.91–1.32 | |
| 6–8 | 1.00 | 1.00 | 1.00 | ||||
| ≥ 9 | 0.91 | 0.73–1.14 | 0.89 | 0.66–1.20 | 1.01 | 0.74–1.38 | |
| ≥ 65 yr, hr | |||||||
| ≤ 5 | 0.80 | 0.70–0.92 | 0.74 | 0.60–0.92 | 0.78 | 0.65–0.95 | |
| 6–8 | 1.00 | 1.00 | 1.00 | ||||
| ≥ 9 | 0.92 | 0.74–1.15 | 1.06 | 0.79–1.41 | 0.81 | 0.58–1.13 | |
KNHANES = Korea National Health and Nutrition Examination Survey, AOR = adjusted odds ratio, CI = confidence interval.
aAdjusted for education, marital status, household income, alcohol consumption, smoking status, and physical activity.
Fig. 2. AOR of obesity and abdominal obesity among Korean adults stratified by gender and four age groups from 2007–2015. (A) AOR of obesity by age in men, (B) AOR of obesity by age in women, (C) AOR of abdominal obesity by age in men, and (D) AOR of abdominal obesity by age in women.
AOR = adjusted odds ratio.
Table 4. Association between self-reported sleep duration and abdominal obesity in the KNHANES 2007–2015.
| Variables | Total (n = 41,805) | Men (n = 19,391) | Women (n = 22,414) | ||||
|---|---|---|---|---|---|---|---|
| AORa | 95% CI | AORa | 95% CI | AORa | 95% CI | ||
| Total, hr | |||||||
| ≤ 5 | 1.17 | 1.08–1.26 | 1.06 | 0.94–1.20 | 1.24 | 1.11–1.37 | |
| 6–8 | 1.00 | 1.00 | 1.00 | ||||
| ≥ 9 | 0.99 | 0.89–1.10 | 0.98 | 0.83–1.14 | 1.18 | 1.02–1.37 | |
| 18–29 yr, hr | |||||||
| ≤ 5 | 1.28 | 0.95–1.74 | 1.18 | 0.79–1.77 | 1.55 | 0.98–2.46 | |
| 6–8 | 1.00 | 1.00 | 1.00 | ||||
| ≥ 9 | 1.01 | 0.77–1.34 | 0.96 | 0.63–1.44 | 1.09 | 0.74–1.58 | |
| 30–49 yr, hr | |||||||
| ≤ 5 | 1.25 | 1.08–1.44 | 1.11 | 0.92–1.34 | 1.45 | 1.18–1.78 | |
| 6–8 | 1.00 | 1.00 | 1.00 | ||||
| ≥ 9 | 1.08 | 0.89–1.31 | 0.92 | 0.67–1.25 | 1.38 | 1.09–1.76 | |
| 50–64 yr, hr | |||||||
| ≤ 5 | 1.12 | 0.98–1.27 | 1.03 | 0.84–1.27 | 1.18 | 1.00–1.39 | |
| 6–8 | 1.00 | 1.00 | 1.00 | ||||
| ≥ 9 | 1.03 | 0.84–1.26 | 0.96 | 0.73–1.27 | 1.24 | 0.93–1.66 | |
| ≥ 65 yr, hr | |||||||
| ≤ 5 | 0.99 | 0.87–1.12 | 0.99 | 0.81–1.20 | 0.95 | 0.80–1.12 | |
| 6–8 | 1.00 | 1.00 | 1.00 | ||||
| ≥ 9 | 1.01 | 0.85–1.21 | 1.15 | 0.89–1.49 | 0.88 | 0.67–1.16 | |
KNHANES = Korea National Health and Nutrition Examination Survey, AOR = adjusted odds ratio; CI = confidence interval.
aAdjusted for education, marital status, household income, alcohol consumption, smoking status, and physical activity.
Associations of sleep duration as a continuous variable with BMI and waist circumference as continuous variables are presented in Supplementary Figs. 1 and 2. There were significant and inverse associations of sleep duration with BMI and waist circumference (β = –0.18, P value < 0.0001; β = –0.50, P value < 0.0001, respectively).
Stratification according to age
Among 18- to 29-year-olds, in the adjusted analyses, sleep duration ≥ 9 hour/day was associated with a decreased prevalence of obesity (OR, 0.77; 95% CI, 0.59–0.99); however, there was no association between obesity and short sleep duration ≤ 5 hour/day. Among individuals in the 30–49 years of age group, the adjusted OR of prevalent obesity was 1.36-fold greater in those with a sleep duration ≤ 5 hour/day (OR, 1.36; 95% CI, 1.18–1.57) compared with those with sleep duration of 6 to 8 hour/day. In older adults (≥ 65 years), a significant decreased adjusted OR for obesity was found between sleep duration ≤ 5 hour/day and the risk for obesity (OR, 0.80; 95% CI, 0.70–0.92).
To evaluate the quality of life in association with sleep duration, health-related quality of life measured by the EuroQol-5D (EQ-5D) index by sleep duration according to age groups are presented in Supplementary Table 1. In older adults ≥ 65 years of age, a significant association was found between sleep duration and health-related quality of life (P value < 0.0001).
Stratification according to gender
In men, there was decreased prevalence of obesity (OR, 0.82; 95% CI, 0.69–0.96) in those with sleep hours ≥ 9 hour/day compared with those who slept 6 to 8 hour/day. However, among adults 30–49 years of age, the adjusted OR for obesity was 1.25-fold greater in those who slept ≤ 5 hour/day (OR, 1.25; 95% CI, 1.02–1.54) compared with those who slept 6 to 8 hour/day. In older men ≥ 65 years of age, a significant decreased adjusted OR for obesity was found between sleep duration ≤ 5 hour/day and the risk for obesity (OR, 0.74; 95% CI, 0.60–0.92).
In women, compared with sleep duration 6 to 8 hour/day, the adjusted OR (95% CI) for obesity was 1.18 (95% CI, 1.07–1.32) for those who slept ≤ 5 hour/day. Among adults 30–49 years of age, there was a significant increased adjusted OR for obesity in those who slept ≤ 5 hour/day (OR, 1.56; 95% CI, 1.00–1.90) and ≥ 9 hour/day (OR, 1.26; 95% CI, 1.00–1.58). In older women (≥ 65 years), a significantly decreased adjusted OR for obesity was found between sleep duration ≤ 5 hour/day and the risk for obesity (OR, 0.78; 95% CI, 0.65–0.95), similar to older men (≥ 65 years).
No significant association was found between sleep duration and the risk for abdominal obesity in any male group after adjusting for variables (Table 4). Women showed an increased adjusted OR for abdominal obesity in those who slept ≤ 5 hour/day (OR, 1.24; 95% CI, 1.11–1.37) and ≥ 9 hour/day (OR, 1.18; 95% CI, 1.02–1.37).
Among adult women 30–49 years of age, there was an increased adjusted OR for abdominal obesity in those who slept ≤ 5 hour/day (OR, 1.45; 95% CI, 1.18–1.78) and ≥ 9 hour/day (OR, 1.38; 95% CI, 1.09–1.76). Among adult women 50–64 years of age, there was a 1.18-fold greater adjusted OR for abdominal obesity only for those who slept ≤ 5 hour/day (OR, 1.18; 95% CI, 1.00–1.39) compared with those who slept 6 to 8 hour/day.
There was no association between sleep duration and abdominal obesity among the older adults (male or female ≥ 65 years of age), which was different from the negative association of general obesity and sleep duration for those who slept ≤ 5 hour/day (Table 4). A sleep duration of ≤ 5 hour/day was negatively associated with obesity but not with abdominal obesity in older adults (≥ 65 years of age) in men and women.
DISCUSSION
This study examined data from the 2007–2015 KNHANES to determine whether there is a relationship between sleep duration and obesity; our results suggest that it varies according to gender and age.
Among individuals 30–49 years of age, there was an increased adjusted OR for obesity only in those who slept ≤ 5 hour/day compared with those who slept 6 to 8 hour/day, both in men and women. There was a prominent increased adjusted OR for abdominal obesity in women who slept ≤ 5 hour/day and ≥ 9 hour/day compared with those who slept 6 to 8 hour/day, which was not shown in any age group for men. Interestingly, in the elderly adult group (≥ 65 years), there was a negative association between sleep duration ≤ 5 hour/day and obesity, but not with abdominal obesity, in both men and women. This relationship persisted even after adjusting for various confounding factors including education, marital status, smoking status, alcohol consumption, physical activity, and income.
This study demonstrated a significant relationship between sleep duration and obesity, which varied according to gender and age, as expected. There is a discrepancy between sleep duration and obesity, or between sleep duration and abdominal obesity, suggesting the influence of different pathogenic mechanisms for each type of obesity and sleep according to age and gender. Adults (men and women) 30–49 years of age exhibited a prominent positive relationship between sleep duration ≤ 5 hour/day and obesity. In addition, women 30–49 years of age exhibited a positive adjusted OR for abdominal obesity in short (≤ 5 hour/day) and long (≥ 9 hour/day) sleepers, compared with sleep duration of 6 to 8 hour/day, suggesting the presence of more pronounced effects in middle-age adult women.
However, there appeared to be no exact explanations for age and gender differences in the relationship between sleep duration and obesity. One possible explanation is that exposure to different types of stress, including socioeconomic and cultural factors and hormones at different ages, and race or ethnicity, may play a role in both short sleep and obesity among various age groups.33,34
In a previous study using the KNHANES 2001–2005, which included 8,717 adults 20–65 years of age, shorter sleep (≤ 5 hour/day) was associated with increased risk for obesity and abdominal obesity in both men and women, and the association between sleep duration and obesity appeared to be more prominent for obesity than for abdominal obesity for men than women, and for young adults 20–40 years of age than older adults.21 However, our study, which included data from 41,805 adults 18–110 years of age, showed different gender and age associations than previous studies in that there was higher association between women and abdominal obesity, especially in those 30–49 years of age.
Previous studies have reported inconsistent results when examining the association between sleep duration and obesity. One of the reasons for inconsistent results may be a wide age range. After examining the ages of participants in the conflicting studies, varying age ranges, such as 20 to 80 years, and average ages, may explain the varying results.20,35,36,37 Studies that included greater numbers of younger participants tended to find a linear relationship, and studies38,39,40 with middle-age subjects more frequently found U-shape associations between sleep duration and obesity,20,41,42,43 suggesting the importance of age factors. Other studies usually showed the strongest relationship between younger age groups and obesity40; however, our study showed a more prominent strong relationship in the 30–49 years age group than the 18–29 years age group, suggesting the influence of social factors, such as long work hours, night activity, and high alcohol intake,40,44 or racial differences45 in response to stressors such as short sleep or psychological distress.
Other explanations for the heterogeneity in the relationship between sleep duration and obesity include limitations such as no clear definitions or standards of normal sleep hours, lack of objective measurements of sleep duration, and a focus mostly on nocturnal sleep duration excluding naps.23 Nevertheless, explanations for the association between long sleep and obesity are sparse. It has been suggested that long sleepers may have low energy expenditure or may overestimate their actual sleep duration because of the long time in bed, and may have poor sleep quality.41 In adults > 65 years of age, short sleep has been associated with decreased risk for obesity; however, the reason for this apparent reverse relationship was not well clarified. There may be more complex confounding factors in elderly individuals, such as medical co-morbidities, complicated medication use, and other characteristics, which are of lesser concern for younger adults. However, there is also the potential for reverse causation because obesity leads to many co-morbidities, including sleep apnea that can disrupt sleep especially in elderly or obese individuals.
Strengths of the present study include its large nationally representative sample for both gender and age, as well as sufficient sample sizes and data for sleep duration, and exact measurements of BMI and waist circumference. However, there were also several limitations, the first of which was that it was a cross-sectional analysis and, therefore, we were unable to establish causality. In addition, sleep duration was self-reported by the participants. More reliable results could be achieved through objective means such as actigraphy, polysomnography, and/or using validated questionnaires that include measures of sleep duration or obtaining multiple subjective sleep durations over several days or weeks (including weekends or non-working days). Sleep duration should also be measured repeatedly and objectively. Nevertheless, a previous study demonstrated that self-reported sleep duration is significantly correlated with objective measurements of sleep hours.46
Future research should include a greater emphasis on longitudinal analysis to examine how sleep and obesity vary according to age and gender over time, and community-based randomized controlled trials to investigate how modification of sleep duration may induce actual weight loss and/or prevent the development of obesity in individuals with either very long or very short sleep duration.
Our findings demonstrated that in adults (both men and women) 30–49 years of age, shorter sleep duration was significantly associated with a modest increase in obesity. However, only women 30–49 years of age demonstrated an increased risk for abdominal obesity in short- and long-duration sleepers compared with those who slept 6 to 8 hour/day. The association between short sleep duration and obesity varied according to age, gender, and type of obesity.
Footnotes
Funding: This work was supported by grant number NRF-2016R1C1B2011968.
Disclosure: The authors have no potential conflict of interest to disclose.
- Conceptualization: Cho KH, Cho EH, Hur J, Shin D.
- Data curation: Shin D.
- Formal analysis: Shin D.
- Investigation: Cho KH, Hur J.
- Writing - original draft: Cho KH, Cho EH.
- Writing - review & editing: Cho KH, Cho EH, Hur J, Shin D.
SUPPLEMENTARY MATERIALS
Health-related quality of life measured by the EQ-5D index by sleep duration and age groups
Association between continuous sleep duration per day and continuous BMI in the Korea Health and Nutrition Examination Survey 2007–2005.
Association between continuous sleep duration per day and continuous waist circumference in the Korea Health and Nutrition Examination Survey 2007–2005.
References
- 1.Vyazovskiy VV, Walton ME, Peirson SN, Bannerman DM. Sleep homeostasis, habits and habituation. Curr Opin Neurobiol. 2017;44:202–211. doi: 10.1016/j.conb.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 2.Bixler E. Sleep and society: an epidemiological perspective. Sleep Med. 2009;10(Suppl 1):S3–S6. doi: 10.1016/j.sleep.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 3.Roth T. Sleep and society. Sleep Med. 2009;10(Suppl 1):S1–S2. doi: 10.1016/j.sleep.2009.07.006. [DOI] [PubMed] [Google Scholar]
- 4.Shin D, Hur J, Cho KH, Cho EH. Trends of self-reported sleep duration in Korean Adults: results from the Korea National Health and Nutrition Examination Survey 2007–2015. Sleep Med. 2018;52:103–106. doi: 10.1016/j.sleep.2018.08.008. [DOI] [PubMed] [Google Scholar]
- 5.National Sleep Foundation. 2015 Sleep in America® poll sleep and pain: summary of findings. [Updated 2015]. [Accessed May 1, 2018]. https://sleepfoundation.org/sleep-polls-data/sleep-in-america-poll/2015-sleep-and-pain.
- 6.Stamatakis KA, Kaplan GA, Roberts RE. Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up. Ann Epidemiol. 2007;17(12):948–955. doi: 10.1016/j.annepidem.2007.07.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yoon HS, Yang JJ, Song M, Lee HW, Han S, Lee SA, et al. Correlates of self-reported sleep duration in middle-aged and elderly Koreans: from the Health Examinees Study. PLoS One. 2015;10(5):e0123510. doi: 10.1371/journal.pone.0123510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ryu SY, Kim KS, Han MA. Factors associated with sleep duration in Korean adults: results of a 2008 community health survey in Gwangju metropolitan city, Korea. J Korean Med Sci. 2011;26(9):1124–1131. doi: 10.3346/jkms.2011.26.9.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Quan SA, Li YC, Li WJ, Li Y, Jeong JY, Kim DH. Gender differences in sleep disturbance among elderly Koreans: Hallym Aging Study. J Korean Med Sci. 2016;31(11):1689–1695. doi: 10.3346/jkms.2016.31.11.1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tamakoshi A, Ohno Y JACC Study Group. Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep. 2004;27(1):51–54. [PubMed] [Google Scholar]
- 11.Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Basta M, et al. Insomnia with short sleep duration and mortality: the Penn State cohort. Sleep. 2010;33(9):1159–1164. doi: 10.1093/sleep/33.9.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59(2):131–136. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 13.Gottlieb DJ, Redline S, Nieto FJ, Baldwin CM, Newman AB, Resnick HE, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006;29(8):1009–1014. doi: 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- 14.Singh M, Drake CL, Roehrs T, Hudgel DW, Roth T. The association between obesity and short sleep duration: a population-based study. J Clin Sleep Med. 2005;1(4):357–363. [PubMed] [Google Scholar]
- 15.Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, et al. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27(3):440–444. doi: 10.1093/sleep/27.3.440. [DOI] [PubMed] [Google Scholar]
- 16.Kim J, Kim HM, Kim KM, Kim DJ. The association of sleep duration and type 2 diabetes in Korean male adults with abdominal obesity: the Korean National Health and Nutrition Examination Survey 2005. Diabetes Res Clin Pract. 2009;86(2):e34–e36. doi: 10.1016/j.diabres.2009.06.027. [DOI] [PubMed] [Google Scholar]
- 17.Hwang HR, Lee JG, Lee S, Cha KS, Choi JH, Jeong DW, et al. The relationship between hypertension and sleep duration: an analysis of the fifth Korea National Health and Nutrition Examination Survey (KNHANES V-3) Clin Hypertens. 2015;21(1):8. doi: 10.1186/s40885-015-0020-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim BK, Kim BS, An SY, Lee MS, Choi YJ, Han SJ, et al. Sleep duration and glycemic control in patients with diabetes mellitus: Korea National Health and Nutrition Examination Survey 2007–2010. J Korean Med Sci. 2013;28(9):1334–1339. doi: 10.3346/jkms.2013.28.9.1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deng HB, Tam T, Zee BC, Chung RY, Su X, Jin L, et al. short sleep duration increases metabolic impact in healthy adults: a population-based cohort study. Sleep (Basel) 2017;40(10) doi: 10.1093/sleep/zsx130. [DOI] [PubMed] [Google Scholar]
- 20.Grandner MA, Schopfer EA, Sands-Lincoln M, Jackson N, Malhotra A. Relationship between sleep duration and body mass index depends on age. Obesity (Silver Spring) 2015;23(12):2491–2498. doi: 10.1002/oby.21247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park SE, Kim HM, Kim DH, Kim J, Cha BS, Kim DJ. The association between sleep duration and general and abdominal obesity in Koreans: data from the Korean National Health and Nutrition Examination Survey, 2001 and 2005. Obesity (Silver Spring) 2009;17(4):767–771. doi: 10.1038/oby.2008.586. [DOI] [PubMed] [Google Scholar]
- 22.Park S. The association between short sleep duration and body mass index among South Korean children and adolescents. J Sch Nurs. 2013;29(2):142–150. doi: 10.1177/1059840512450582. [DOI] [PubMed] [Google Scholar]
- 23.Ford ES, Li C, Wheaton AG, Chapman DP, Perry GS, Croft JB. Sleep duration and body mass index and waist circumference among U.S. adults. Obesity (Silver Spring) 2014;22(2):598–607. doi: 10.1002/oby.20558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sun W, Huang Y, Wang Z, Yu Y, Lau A, Ali G, et al. Sleep duration associated with body mass index among Chinese adults. Sleep Med. 2015;16(5):612–616. doi: 10.1016/j.sleep.2014.12.011. [DOI] [PubMed] [Google Scholar]
- 25.Mullington JM, Chan JL, Van Dongen HP, Szuba MP, Samaras J, Price NJ, et al. Sleep loss reduces diurnal rhythm amplitude of leptin in healthy men. J Neuroendocrinol. 2003;15(9):851–854. doi: 10.1046/j.1365-2826.2003.01069.x. [DOI] [PubMed] [Google Scholar]
- 26.Schmid SM, Hallschmid M, Jauch-Chara K, Born J, Schultes B. A single night of sleep deprivation increases ghrelin levels and feelings of hunger in normal-weight healthy men. J Sleep Res. 2008;17(3):331–334. doi: 10.1111/j.1365-2869.2008.00662.x. [DOI] [PubMed] [Google Scholar]
- 27.Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141(11):846–850. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 28.Meier-Ewert HK, Ridker PM, Rifai N, Regan MM, Price NJ, Dinges DF, et al. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol. 2004;43(4):678–683. doi: 10.1016/j.jacc.2003.07.050. [DOI] [PubMed] [Google Scholar]
- 29.Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES) Int J Epidemiol. 2014;43(1):69–77. doi: 10.1093/ije/dyt228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oh S, Yu T, Hur B, Ahn Y, Yoon Y, Shin S. A study on the standard of obesity by analyzing mortality rate and occurrence of disease related to obesity in Koreans. Korean J Obes. 2002;11(Suppl 3):304. [Google Scholar]
- 31.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 32.Lee SY, Park HS, Kim DJ, Han JH, Kim SM, Cho GJ, et al. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract. 2007;75(1):72–80. doi: 10.1016/j.diabres.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 33.Grandner MA, Martin JL, Patel NP, Jackson NJ, Gehrman PR, Pien G, et al. Age and sleep disturbances among American men and women: data from the U.S. Behavioral Risk Factor Surveillance System. Sleep (Basel) 2012;35(3):395–406. doi: 10.5665/sleep.1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Slopen N, Williams DR. Discrimination, other psychosocial stressors, and self-reported sleep duration and difficulties. Sleep (Basel) 2014;37(1):147–156. doi: 10.5665/sleep.3326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev. 2008;12(4):289–298. doi: 10.1016/j.smrv.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 36.Moraes W, Poyares D, Zalcman I, de Mello MT, Bittencourt LR, Santos-Silva R, et al. Association between body mass index and sleep duration assessed by objective methods in a representative sample of the adult population. Sleep Med. 2013;14(4):312–318. doi: 10.1016/j.sleep.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 37.Stamatakis KA, Brownson RC. Sleep duration and obesity-related risk factors in the rural Midwest. Prev Med. 2008;46(5):439–444. doi: 10.1016/j.ypmed.2007.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Meyer KA, Wall MM, Larson NI, Laska MN, Neumark-Sztainer D. Sleep duration and BMI in a sample of young adults. Obesity (Silver Spring) 2012;20(6):1279–1287. doi: 10.1038/oby.2011.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hasler G, Buysse DJ, Klaghofer R, Gamma A, Ajdacic V, Eich D, et al. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep. 2004;27(4):661–666. doi: 10.1093/sleep/27.4.661. [DOI] [PubMed] [Google Scholar]
- 40.Theorell-Haglöw J, Berglund L, Janson C, Lindberg E. Sleep duration and central obesity in women - differences between short sleepers and long sleepers. Sleep Med. 2012;13(8):1079–1085. doi: 10.1016/j.sleep.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 41.Chaput JP, Després JP, Bouchard C, Tremblay A. The association between sleep duration and weight gain in adults: a 6-year prospective study from the Quebec Family Study. Sleep. 2008;31(4):517–523. doi: 10.1093/sleep/31.4.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bjorvatn B, Sagen IM, Øyane N, Waage S, Fetveit A, Pallesen S, et al. The association between sleep duration, body mass index and metabolic measures in the Hordaland Health Study. J Sleep Res. 2007;16(1):66–76. doi: 10.1111/j.1365-2869.2007.00569.x. [DOI] [PubMed] [Google Scholar]
- 43.Hairston KG, Bryer-Ash M, Norris JM, Haffner S, Bowden DW, Wagenknecht LE. Sleep duration and five-year abdominal fat accumulation in a minority cohort: the IRAS family study. Sleep. 2010;33(3):289–295. doi: 10.1093/sleep/33.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Park S, Cho MJ, Chang SM, Bae JN, Jeon HJ, Cho SJ, et al. Relationships of sleep duration with sociodemographic and health-related factors, psychiatric disorders and sleep disturbances in a community sample of Korean adults. J Sleep Res. 2010;19(4):567–577. doi: 10.1111/j.1365-2869.2010.00841.x. [DOI] [PubMed] [Google Scholar]
- 45.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30(9):1096–1103. doi: 10.1093/sleep/30.9.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lockley SW, Skene DJ, Arendt J. Comparison between subjective and actigraphic measurement of sleep and sleep rhythms. J Sleep Res. 1999;8(3):175–183. doi: 10.1046/j.1365-2869.1999.00155.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Health-related quality of life measured by the EQ-5D index by sleep duration and age groups
Association between continuous sleep duration per day and continuous BMI in the Korea Health and Nutrition Examination Survey 2007–2005.
Association between continuous sleep duration per day and continuous waist circumference in the Korea Health and Nutrition Examination Survey 2007–2005.