Graphical abstract
Comparison of present and previous study reports regarding muscles origin from ventricular walls.
Keywords: Papillary muscles, Left ventricle, Mitral valve, Heart
Abstract
Introduction
The two left ventricular papillary muscles are small structures at sternocostal and inferior wall but are vital to mitral valve competence. Extra papillary muscles could be found. Partial or complete rupture, complicating acute myocardial infarction, causes severe or even catastrophic mitral regurgitation, potentially correctable by surgery. Detailed knowledge of normal anatomy and variations is vital for accurate interpretation of information by echocardiography and for surgical repair.
Materials and methods
The material for present study consisted of 52 formalin fixed adult apparently normal cadaveric hearts belonging to either sex obtained from the Department of Anatomy. These hearts were dissected carefully to open the left ventricle and to expose the papillary muscles. According to their attitudinal position they were described as supero-lateral (S-L) and inferoseptal muscle (I-S) instead of conventional anterolateral and posteromedial. Different morphological features of papillary muscles were noted and measurements were taken.
Results
Classical picture of left ventricular papillary muscle was found only in 25% cases. Additionally extra muscles were found 34.61% and 71.15% in S-L and I-S group, respectively. Different shapes and pattern of papillary muscles were also been identified. An additional attribute of this study was measurement of length and breadth of papillary muscles which thus provides a base line data for further detailed studies in a large scale.
Conclusion
Oriental nomenclature is necessary not only for anatomist but also for electrocardiographers. Breadth of papillay muscle should be taken into morphometric account as for screening of hypertrophic cardiomyopathy. Proper anatomical knowledge is crucial for clinicians, surgeons and radiologists.
1. Introduction
Papillary muscles are myocardial structures of left ventricle, have importance out of proportion to their small size. Proper functioning of these muscles maintains the integrity of mitral valve, abnormalities of it ranges from a life-threatening emergency (muscle rupture) to an echocardiographic finding of doubtful clinical significance (muscle calcification).1
The two papillary muscles of left ventricle, named by convention anterolateral (A-L) and posteromedial (P-M) arise from sternocostal mural myocardium and diaphragmatic myocardium, respectively. According to anatomical position, diaphragmatic surface of heart placed inferiorly and sternocostal surface of left ventricle supero-laterally (S-L). So it is mysterious why morphologists throughout the centuries have chosen to describe the papillary muscles misnamed as the heart stands vertically on its apex.2 In true sense according to attitudinally, papillary muscles should be S-L and infero-septally (I-S) from sterocostal and diaphragmatic surface respectively. However locations of the papillary muscles can be distorted by alteration of size and shape of ventricle leading disturbed valvular function.3 During ventricular systole, synchronous contraction of papillary muscle and ventricular myocardium is believed to tauten the chordae tendineae and prevents prolapse of mitral valve leaflets normally. Loss of this contractile action results from myocardial infarction with subsequence papillary muscle fibrosis or ischemia.4 But previous studies5, 6 delineated that there is minimal or no correlation between papillary muscle dysfunction and mitral regurgitation, especially in those patients where left ventricular chamber size and function is normal.
Though muscles are two in number as a rule, there are usually groups of papillary muscles arranged fairly close together as a matter of course. At their bases, the muscles sometimes fused or have bridges of muscular or fibrous continuity before attaching to the ventricular wall. Extreme fusion results in parachute malformation with potential for valvular stenosis.3 Variations of papillary muscle can be explained embryologically. Heart muscle develops from the trabecular myocardial ridge by process of gradual delamination of ventricular wall. Incomplete delamination of trabecular ridge leads to morphological variations of papillary muscles.7
Now-a-days, advanced noninvasive modalities are used for detection and confirmation of anomalies but detail anatomical knowledge is required for the study and interpretation of the radiological images. Till now only few morphometric study of mitral valve papillary muscle has been reported. This study was done with an effort to extend the concepts previously presented as well as to overcome deficiencies in the knowledge of positional nomenclature, its gross architecture and variations with different parameters.
2. Method & material
Fifty-two formalin fixed human adult cadaveric hearts of either sex were procured from department of anatomy. Any specimens with grossly identifiable anomaly which might affect its topography or having calcification were excluded from the study. After cleaning the specimens, left ventricle was opened. Blood clots were removed and chamber was washed with water to visualize the structures. Position of the muscles from sternocostal and diaphragmatic wall of left ventricle was checked placing the heart anatomically. Muscles were named as S-L and I-S rather than so called A-L and P-M, respectively, which usually mentioned in all text books. After noticing the position of papillary muscles, the Mitral valve complex was dissected very carefully avoiding damage to any structures for proper view of each muscle from origin to tip for morphology. Extra muscles were checked and explored their position and arrangement. Morphological features of each muscle were examined as follows:
-
1.
Number of papillary muscle with spatial orientation in both walls.
-
2.
Shape of each papillary muscle by apex (conical, flattop, truncated, bifurcate & trifurcate).
-
3.
Pattern of extra or grouped papillary muscles (parallel or interconnected).
-
4.
Site of origin or attachment at ventricular wall (upper 1/3, middle 1/3, lower 1/3).
-
5.
Number of chordea attached at tip
-
6.
Attachment with cusps (anterior, posterior or both).
By using Vernier caliper and malleable millimeter ruler following parameters of papillary muscle were measured:
-
a)
Length of the muscle from summit to basal attachment at ventricular wall.
-
b)
Breadth of the muscle at its origin from ventricular wall.
All morphological records were made along with photographs. Statistical analysis was done using Statistica Software. Mean, median SD, 95% CI and p value of S-L and I-S papillary muscles were calculated and the results were tabulated. P-value < 0.05 was considered a significant. A bar diagram regarding the attachment in ventricular wall of both papillary muscles were prepared.
3. Results
Each of 52 specimens presented with both types of muscle though number of them varied. Minimum number of total muscle in ventricle was two and maximum was seven in number. Classical picture of one S-L and one I-S papillary muscle were present only in 25% cases (13 specimens). Single belly for S-L and I-S muscle was observed in 65.38% and 28.84% specimens respectively. Considering extra bellies, the maximum (07) number of muscles (two S-L & five I-S) were present in two specimens only. In 34.61% specimens’ accessory S-L muscle bellies (double, triple) and in 71.15% specimens’ accessory I-S muscle bellies (double, triple, quadruple & quintuple) was found. Striking feature is that extra muscle belly was more pronounced in inferior wall of ventricle (66 extra muscle bellies) in compare to S-L wall (25 extra bellies). Quadruple and quintuple bellies were present in I-S group muscle only. In cases of double papillary muscle, their arrangement varied in both wall of ventricle. They remained separated and parallel more in sternocostal surface (54.54%) but interconnected more in inferior wall (72.22%). When triple bellies were present, three predominantly interconnected in S-L (42.85%) but two interconnected and one separated chiefly in inferior surface.
Detail about number of muscles and arrangement of extra muscles were presented in Table 1.
Table 1.
Number and pattern of papillary muscles.
| Supero-Lateral N (%) | Infero-septal N (%) | |||
|---|---|---|---|---|
| No. of muscles | Present (52 Specimens) | Single | 34 (65.38%) | 15 (28.84%) |
| Double | 11 (21.15%) | 18 (34.61%) | ||
| Triple | 07 (13.46%) | 11 (21.15%) | ||
| Quadruple | 00 | 06 (11.53%) | ||
| Quintuple | 00 | 02 (03.84%) | ||
| Absent | 00 | 00 | ||
| Arrangement of extra muscles | Double belly (S-L:11specimens I-S:18specimens) | Parallel | 06 (54.54%) | 05 (27.77%) |
| Interlinked | 05 (45.45%) | 13 (72.22%) | ||
| Triple belly (S-L:07specimens I-S:11specimens) | Parallel | 02 (28.57%) | 00 | |
| Two interlinked & one separated | 02 (28.57%) | 06 (54.54%) | ||
| Three interlinked | 03 (42.85%) | 05 (45.45%) | ||
| Quadruple belly (S-L:00specimens I-S:06specimens) | Parallel | 00 | 02 (33.33%) | |
| Two pair interlinked | 00 | 02 (33.33%) | ||
| Two interlinked & two separated | 00 | 02 (33.33%) | ||
| Quintuple belly (S-L:00specimen I-S:02specimens) | Parallel | 00 | 00 | |
| Two pair interlinked & one separated | 00 | 02 (100%) |
Shapes of individual muscle belly were varied and they were classified as conical, flattop, truncated, bifurcated and trifurcated. S-L muscles were principally in truncated shape (66.23%) whether I-S muscles are primarily in conical type (45.76%). Flattop papillary muscles were found largely in S-L group but bifurcated and trifurcated papillary muscles were marked in I-S group.
S-L muscles took origin from upper and middle one-third of sternocostal wall in 45.45% and 51.94%, respectively. I-S muscle arose from middle one-third in 50% cases and rest from upper and lower one-third of diaphragmatic wall of ventricle. Apex of each papillary muscle was connected with mitral valve cusps via chordae tendineae which ranges from 2 to 14 in S-L group and 2–20 in I-S group. Notable attachment of S-L and I-S muscles with both mitral valve cusps like classical picture, only few accessory muscles of both group attached with either aortic or mural cusp.
Detail of shape of muscles, origin from ventricle, attachment of chordae and relation with mitral valve cusps were organized in Table 2.
Table 2.
Shape, origin, number of chordae and attachment with cusps of individual muscle.
| Supero-Lateral n (%) | Infero-Septal n (%) | ||
|---|---|---|---|
| Total number of muscle belly in ventricle | 77 | 118 | |
| Shape of Individual muscle belly | Conical | 04 (05.19%) | 54 (45.76%) |
| Flat top | 11 (14.28%) | 09 (07.62%) | |
| Truncated | 51 (66.23%) | 27 (22.88%) | |
| Bifurcated | 08 (10.38%) | 22 (18.64%) | |
| Trifurcated | 03 (03.89%) | 06 (05.08%) | |
| Site of origin from ventricular wall | Upper ⅓ | 35 (45.45%) | 31 (26.27%) |
| Middle ⅓ | 40 (51.94%) | 59 (50%) | |
| Lower ⅓ | 02 (02.59%) | 28 (23.72%) | |
| No. of Chordea attached to each muscle | Range | 02−14 | 02−20 |
| Mean | 06 | 11 | |
| Attachment of each muscle with mitral valve Cusps | Both | 55 (71.42%) | 86 (72.88%) |
| Only Anterior | 22 (28.57%) | 06 (05.08%) | |
| Only posterior | 00 | 26 (22.03%) | |
It was found that length and breadth at origin were varied not only between S-L and I-S group, but also in the accessory muscles of same group. Mean length and breadth of S-L muscle were 2.6 ± 0.88 cm and 0.90 ± 0.29 cm respectively, for I-S muscle 2.51 ± 0.62 cm and 0.89 ± 0.27 cm respectively. Detail morphometric data of papillary muscles were represented in Table 3.
Table 3.
Parameters of papillary muscles.
| Supero − Lateral Muscle |
Infero − Septal Muscle |
||||
|---|---|---|---|---|---|
| Length (cm) | Breadth (cm) | Length (cm) | Breadth (cm) | ||
| Median | 2.55 | 0.98 | 2.6 | 0.97 | |
| Mean | 2.6 | 0.90 | 2.51 | 0.89 | |
| SD | 0.88 | 0.29 | 0.62 | 0.27 | |
| 95% CI | LL | 2.35 | 0.82 | 2.34 | 0.81 |
| UL | 2.84 | 0.99 | 2.68 | 0.97 | |
| P value | >0.1 | 0.0002 | >0.1 | 0.023 | |
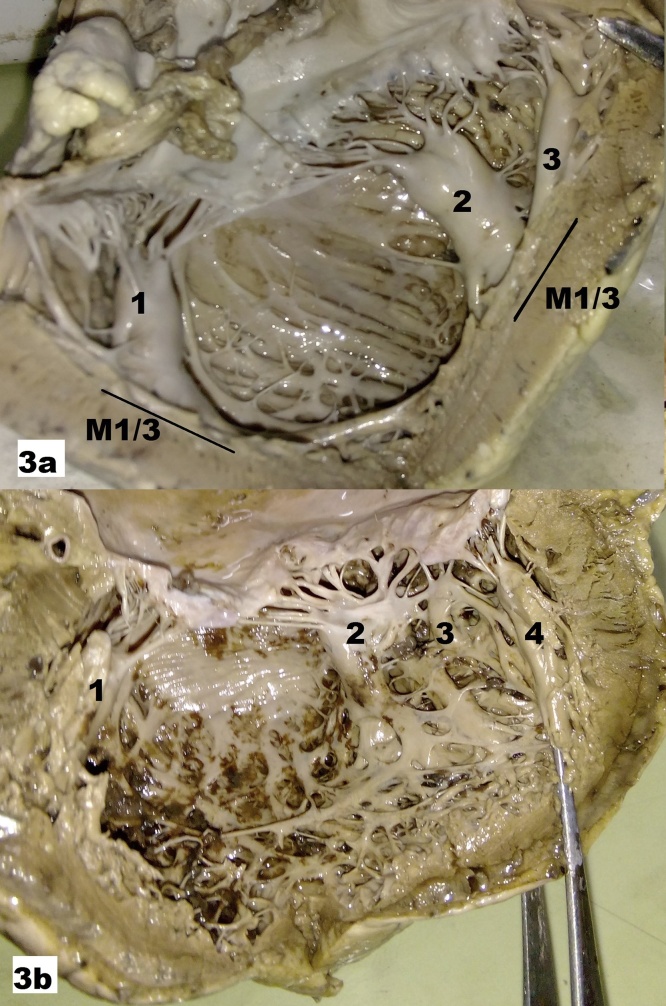
Fig. 1, Fig. 2, Fig. 3, Fig. 4. illustrate different position of muscles, number of muscles, shape of muscles and their origin at ventricular wall.
Fig. 1.
1(a) Sternocostal surface reflected medially. 1(b) Sternocostal surface reflected laterally. 1-S-L papillary muscle from sternocostal surface, 2-I-S papillary muscle from diaphragmatic surface, 3- Sternocostal surface, 4- Diaphragmatic surface.
Fig. 2.
2(a) Double parallel S-L(1,2) and I-S(3,4)papillary muscles. 1-Conical, 2-Truncated, 3- Trifurcated, 4- Flattop. 2(b) Double parallel S-L(1,2) and single I-S(3)papillary muscles. 1-Conical, 2-Truncated, 3- Bifurcated. U1/3–Upper ⅓ of ventricular wall; M1/3 − Middle⅓ of ventricular wall.
Fig. 3.
3(a) Single S-L(1) and Double parallel (2,3)papillary muscles. 1–Truncated, 2–Truncated, 3–Conical. M1/3–Middle ⅓ of ventricular wall. 3(b) Single S-L(1) and Triple interconnected I-S. (2,3,4)papillary muscles 1–Truncated, 2–Flattop, 3 & 4–Conical.
Fig. 4.
4(a) Double S-L (1,2) and Quintuple I-S(3,4,5,6&7)papillary muscles. 1 & 2–Interconnected, 3 & 4–Interconnected, 5–Separated, 6 & 7–Interconnected, 3- attached with both cusps, 4 & 5–attached with only posterior cusp. 3 & 4–Lower ⅓ of ventricular wall origin, 5–Middle ⅓ of ventricular wall origin, 6 & 7–Upper ⅓ of ventricular wall origin. 4(b) Single S-L and Double parallel I-S(2,3)papillary muscles. 1–Conical muscle from Middle ⅓ (M1/3) of ventricular wall attached with both cusps. 2 & 3–Conical muscles from Lower⅓ (L1/3) of ventricular wall attached with both cusps.
4. Discussion
It is essential that the heart should be considered in the attitudinally appropriate fashion particularly for electrocardiographers.2 In our study we described papillary muscles as S-L and I-S which is identical to consistently described as A-L and P-M papillary muscles by previous works and have been compared subsequently.
Both papillary muscles are vital to mitral valve competence. I-S muscles often get necrosis and rupture in inferior wall ischemia due to poor blood supply than S-L.8 It is estimated that 0.4 to 5.0% of all deaths after acute myocardial infarction are associated with papillary muscle rupture. Rupture of muscle usually occurs 2 to 7 days of post infarction and results in acute mitral regurgitation, pulmonary edema, and/or cardiogenic shock.1 The specific anatomic site (central body or one head) at which papillary muscle rupture occurs is an important determinant for the magnitude of regurgitation and the subsequent clinical course.9 Generally in a normal heart, the thickness of either papillary muscle is about the same as is that of the left ventricular free wall or ventricular septum. According to previous study, normally the so called A-L papillary muscle is slightly larger than the P-M. Just as the P-M and A-L papillary muscles can differ from each other in the same heart, considerable morphologic variation is observed in comparing either or both muscles from one heart with those of another.8 Victor and Nayak10 in their study stated that the mitral valve apparatus including papillary muscle is as unique to each individual as one’s own fingerprint.
Cheichi et al11 mentioned that the papillary muscles may be single, double, triple or more than three in number. An increased number and size of the papillary muscles, as well as their malformation, may cause left ventricular outflow tract obstruction and mitral regurgitation.2 Moreover an extra papillary muscle near apex may be mistaken for mural thrombi, especially if that segment of left ventricle happens to be infracted.1 Minimum number of total papillary muscle within ventricle is noted as 2 and maximum is 7 in present study. Classical papillary muscle found in present study is 25% but Gunnal et al12 found in 3.44% only. Previous report13 of extra papillary muscles more in posterior wall than anterior is close to our study. Maximum number of papillary muscle frequently seen by previous authors10, 14, 15 is three in sternocostal surface and four in diaphragmatic surface, though five and six muscle bellies also have been reported in previous two studies.10, 14 We have found five I-S muscle in 3.84% cases. Table 4 depicts a comparison detail about this.
Table 4.
Comparison of different studies regarding number of papillary muscles.
| Papillary Muscles | Authors |
||||||
|---|---|---|---|---|---|---|---|
| Present study | Victor et al. 10 | Gheorghitescu et al. 13 | Kavimani et al. 14 | Lakhanpal et al. 15 | Hospatana et al.16 | ||
| Muscle Of Sternocostal surface | One | 65.38% | 67% | 31.2% | 62% | 68.25% | 86.67% |
| Two | 21.15% | 27% | 56.25% | 31% | 30.15% | 13.33% | |
| Three | 13.46% | 4% | 12.50% | 2% | 1.58% | – | |
| Four | – | 1% | – | 2% | – | – | |
| Five | – | 1% | – | 2% | – | – | |
| Six | – | – | – | – | – | – | |
| Muscle Of Diaphragmatic surface | One | 28.84% | 50% | 25% | 49% | 74.60% | 60% |
| Two | 34.61% | 36% | 58.33% | 42% | 22.22% | 40% | |
| Three | 21.15% | 11% | 8.33% | 4% | 1.58% | – | |
| Four | 11.53% | 3% | 8.33% | 2% | 1.58% | – | |
| Five | 3.84% | – | – | 2% | – | – | |
| Six | – | – | – | 2% | – | – |
Different shapes of the papillary muscle have been provided by previous studies but its correlation with ventricular blood flow is yet pending. Though Gunnal et al12 stated that shape of papillary muscle affects the passage of blood flow and conical is the best to facilitate cardiovascular physiology by posing minimum obstruction to blood flow through ventricle, still we suggest in vivo flow study is needed. Victor and Nayak10 classified muscles as conical, mamillated, flattopped, grooved, stepped, weavy, arched, sloped and saucerised. All the papillary muscles in the left ventricle were cone shaped and posteriors are commonly bifid as per hospatana’s study.16 Gunnal et al. categorized muscles as conical, broad apex, pyramidal and fan shaped. He also specified that chances of left ventricular hypertrophy are higher in broad apex or fan shaped papillary muscles.12 We have found conical, flattop, truncated, bifurcated and trifurcated. Gheorghitescu13 noticed conical and cylindrical shape in 56.90% and 31.05% for so called A-L and 70.83% and 04.17% for P-M papillary muscle, respectively. Where 2–5 muscle bellies of same group present, various configurations such as two-tiered, interlinked, parallel, arched were recorded.10 We have observed parallel and/or interconnected (at base, middle or apex) muscle bellies present in same wall of ventricle. Few muscular bands also present across the cavity to interconnect between the both wall papillary muscles. It is stated that intragroups interconnections are more frequent than intergroup interconnections, with the latter limited to the exchange of a few strands at the level of the chordae tendineae.10
The geometry of the subvalvular apparatus is characterised by the distance from the annulus to the respective and to the contralateral papillary muscle. ‘Annulo-papillary distance’ has been found to be the same in systole as in diastole in normal hearts, regardless of loading conditions.17 In a prolapsed mitral valve, there is an excess of movement (overlapping) of one cusp in relation to the other focusing that the movement of prolapsing leaflet is possibly dependent on the architecture and location of the papillary muscles nearest to the valve.12 Brock RC18 said that papillary muscle normally arise from upper and middle thirds of left ventricle but Gunnal12 seen mostly from middle third. In present study origin of S-L papillary muscles are from middle third as well as from upper third of ventricular wall but 50% of I-S muscles are from middle third and rest from upper and lower third of the wall. Difference between present and previous study reports regarding origin of muscles depicted in bar diagram (Fig. 5). Each papillary muscle has an average of 12 chordae tendineae per head.8 In case of only two papillary muscles half of the chordae is under control of one single papillary muscle. If rupture involves the entire papillary muscle, regurgitation is overwhelming and rapidly fatal whether rupture confined to one head of papillary muscle is quantitatively similar to rupture of major chordae.9 Frailty of papillary muscle depends on their morphology and protected by compensatory collateral vascularization if multiple muscular interconnection bridges are present.19 So ischemia affecting base of individualized papillary muscle which receiving only central artery with few or no anastomotic connections, becomes more prone to rupture at apex due to the fragility of its truncal blood supply and to the degree of physical stress. It may be the reason why sclerosis or calcification of this apical region is frequently encountered as an incidental finding on 2-D echocardiography.12 In present study, most of the papillary muscle is attached via adequate number of chordae tendinae with cusps of mitral valve, but none directly to leaflets. Majority of papillary muscle are connected to both cusps except 27.11% − 28.57% accessory muscles which are in connection with single cusp (Table 2). Anomalous insertion of a papillary muscle directly into the anterior mitral leaflet without interposition of the chordae tendineae frequently leads to midventricular obstruction.8 In mitral valve replacement, retention of chordeopapillary support is being favored to preserve optimum function of left ventricle.
Fig. 5.
Comparison of present and previous study reports regarding muscles origin from ventricular walls.
Papillary muscles are significantly longer and thinner in compare to normal in dilated cardiomyopathy.1 Hospatana et al described that the length of so called A-L and P-M papillary muscle is 1.63 ± 0.50 cm and 2.14 ± 0.60 cm, respectively.16 They also analyzed that papillary muscles of the left ventricle is longer than that of right. Farzana et al. mentioned that the length of conventionally named A-L and P-M papillary muscle is 2.01 ± 0.25 cm and 1.81 ± 0.76 cm, respectively.20 According to our study length of S-L is 2.6 ± 0.88 cm which is similar to Farzana et al study20 but length of I-S muscle (2.51 ± 0.62 cm) is more than the previous study reports.16, 20
Isolated papillary muscle hypertrophy in normal ventricular mass, although unusual, obstruct the outflow tract, is considered as a newly identified subtype of hypertrophic cardiomyopathy.21, 22 Hypertrophy is defined as at least 1 of the 2 papillary muscles being more than 1.1 cm in the horizontal or vertical diameter or in both by echocardiographic measurement.23 As hyperechoic papillary muscle without clear hypertrophy is an important suspicion finding, so during ecocardiographic examination sonographer should pay attention in papillary muscle dimension and echogenecity.24 Till now no anatomical study has been reported about breadth as per our knowledge which needs to be highlighted now a day. We found breadth of S-L and I-S papillary muscle is 0.9 ± 0.29 cm and 0.89 ± 0.27 cm, respectively.
Surgical repair (resection, repositioning and realignment) is the gold standard treatment for mitral valve regurgitation.12 In case of extra papillary muscles; options will also increases to decide the degree and direction of realignment for surgical correction. Mitral valve replacement with homograft has now been tried. It is preferable to retain patient’s own papillary muscle for its vascularity, innervations and continuity with ventricular musculature.1 For homograft, proper fixation of graft to recipient papillary muscle using a side-by-side suture, as described by Acar and colleagues25 is the key for success.26 Although early results are encouraging long-term follow-up is clearly desired.
5. Conclusion
Analyzing the papillary muscles in this series, a considerable variation appeared. Through majority are compatible with previous results, some added predominant new value. Nomenclature, though yet to be acceptable, is crucial under consideration. A noticeable number of accessory inferior wall papillary muscles are present. Origin of I-S muscle from upper third of ventricular wall is also distinct. Our morphometric analysis, especially papillary muscle breadth, vital for hypertropic cardiomyopathy screening during echocardiography, must supplement the facts in cadaveric study. Still there is a clear need of future large-scale studies including specimens from individuals with mitral valve prolapse, dilated cardiomyopathy and left ventricular outflow tract obstruction to correlate the necropsic observation and clinical findings for au fait clarification of discrepancies.
Conflicts of interest
We have nothing to declare about any conflicts of interest.
Funding
None to declare.
References
- 1.Madu E.C., D’Cruz I.A. The vital role of papillary muscles in mitral and ventricular function: echocardiographic insights. Clin Cardiol. 1997;20:93–98. doi: 10.1002/clc.4960200203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson R.H. The relationship between the positions of the left ventricular papillary muscles and the direction of the QRS axis. J Electrophysiol Cardiol. 2016;49(5):675–679. doi: 10.1016/j.jelectrocard.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 3.Ho S.Y. Anatomy of the mitral valve. Heart. 2002;88(Suppl. 4):iv5–iv10. doi: 10.1136/heart.88.suppl_4.iv5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mittal A.K., Langston M., Cohn K.E., Selzer A., Kerth W.J. Combined papillary muscle and left ventricular wall dysfunction as a cause of mitral regurgitation. Circulation. 1971;44:174–180. doi: 10.1161/01.cir.44.2.174. [DOI] [PubMed] [Google Scholar]
- 5.Madu E.C., Baugh D.S., Reid E.C., Potu C. Papillary muscle function does not predict mitral regurgitation in patients with normal left ventricular systolic function: a transesophageal echocardiographic study − PM function and mitral regurgitation. Inter J Clin Med. 2011;2:178–183. [Google Scholar]
- 6.Messas E., Guerrero J.L., Handschumacher M.D. Paradoxic decrease in ischemic mitral regurgitation with papillary muscle dysfunction; insight from three- dimensional and contrast echocardiography with strain rate measurement. Circulation. 2001;104(16):1952–1957. doi: 10.1161/hc4101.097112. [DOI] [PubMed] [Google Scholar]
- 7.Oosthoek P.W., Wenink A.C., Wisse L.J., Gittenberger-de Groot A.C. Development of the papillary muscles of the mitral valve: morphogenetic background of parachute-like asymmetric mitral valves and other mitral valve anomalies. J Thorac Cardiovasc Surg. 1998;116:36–46. doi: 10.1016/S0022-5223(98)70240-5. [DOI] [PubMed] [Google Scholar]
- 8.Roberts W.C., Cohen L.S. Left ventricular papillary muscles: description of the normal and a survey of conditions causing them to be abnormal. Circulation. 1972;46:138–154. doi: 10.1161/01.cir.46.1.138. [DOI] [PubMed] [Google Scholar]
- 9.Perloff J.K., Roberts W.C. 1972. The Mitral Apparatus. Functional Anatomy of Mitral Regurgitation Circulation; p. XLVI. [DOI] [PubMed] [Google Scholar]
- 10.Victor S., Nayak V.M. Variations in the papillary muscles of the normal mitral valve and their surgical relevance. J Card Surg. 1995;10(5):597–607. doi: 10.1111/j.1540-8191.1995.tb00642.x. [DOI] [PubMed] [Google Scholar]
- 11.Chiechi M.A., Lees W.M., Thompson R. Functional anatomy of the normal mitral valve. J Thoracic Surg. 1956;32:378–398. [PubMed] [Google Scholar]
- 12.Gunnal S.A., Wabale R.N., Farooqui M.S. Morphological variations of papillary muscles in the mitral valve complex in human cadaveric hearts. Singapore Med J. 2013;54:44–48. doi: 10.11622/smedj.2013011. [DOI] [PubMed] [Google Scholar]
- 13.Gheorghitescu R., Toba M., Iliescu D.M., Bordei P. Anatomical consideration of the number and form of the papillary muscle in the left ventricle. ARS Med Tomitana. 2016;2(22):119–127. [Google Scholar]
- 14.Kavimani M., Johnson W.M.S., Jebakani C.F. Morphology of mitral papillary muscles −the bridges of vital link across the heart muscles. Natl J Basic Med Sci (NJBMS) 2011;2(1):18–22. [Google Scholar]
- 15.Lakhanpal A.V., Johri M.S., Shrivastava S.K., Verma S.K. Study of papillary muscles of mitral valve in central indians. IJCMR. 2016;3(7):2045–2048. [Google Scholar]
- 16.Hosapatna M., D Souza A., Das A.M., Supriya, Ankolekar V.H., D Souza A.S. Morphology of papillary muscles in human adults: a cadaveric study. Ibnosina J Med BS. 2014:168–172. [Google Scholar]
- 17.Garbi M., Monaghan M.J. Quantitative mitral valve anatomy and pathology. Echo Res Pract. 2015 Sep 1;2(3):R63–R72. doi: 10.1530/ERP-15-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brock R.C. The surgical and pathological anatomy of the mitral valve. Brit Heart J. 1952;14:489–497. doi: 10.1136/hrt.14.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nappi F., Cristiano S., Nenna A., Massimo Chello M. Ischemic mitral valve prolapse. J Thorac Dis. 2016;8(12):3752–3761. doi: 10.21037/jtd.2016.12.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Farzana T., Khalil M., Mannan S., Sultana J., Sumi M.S., Sultana R. Length of papillary muscles in both ventricles of different age group on Bangladeshi cadaver. Mymensingh Med J. 2015;24(January (1)):52–58. [PubMed] [Google Scholar]
- 21.Ferreira C., Delgado C., Vázquez M., Trinidad C., Vilar M. Isolated papillary muscle hypertrophy: a gap in our knowledge of hypertrophic cardiomyopathy? Rev Port Cardiol. 2014;33(June (6)):379. doi: 10.1016/j.repc.2014.01.015. [e1-5] [DOI] [PubMed] [Google Scholar]
- 22.Kobashi A., Suwa M., Ito T., Otake Y., Hirota Y., Kawamura K. Solitary papillary muscle hypertrophy as a possible form of hypertrophic cardiomyopathy. Jpn Circ J. 1998;62:811–816. doi: 10.1253/jcj.62.811. [DOI] [PubMed] [Google Scholar]
- 23.Sung K.T., Yun C.H., Hou C.J.Y., Hung C.L. Solitary accessory and papillary muscle hypertrophy manifested as dynamic mid-wall obstruction and symptomatic heart failure: diagnostic feasibility by multi-modality imaging. BMC Cardiovasc Disord. 2014;14:34. doi: 10.1186/1471-2261-14-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cresti A., Aquaro G.D., Picotti A., Kocabay G., Todiere G. Morphological and tissue alterations in one papillary muscle: an early sign of hypertrophic cardiomyopathy? Int Cardiovasc Res J. 2016;10(4):205–208. [Google Scholar]
- 25.Acar A., Tolan M., Berrebi A. Homograft replacement of the mitral valve graft selection, technique of implantation, and results in forty-three patients. J Thorac Cardiovasc Surg. 1996;111:367–380. doi: 10.1016/s0022-5223(96)70446-4. [DOI] [PubMed] [Google Scholar]
- 26.Doty D.B., Acar C. Mitral valve replacement with homograft. Ann Thorac Surg. 1998;66:2127–2131. doi: 10.1016/s0003-4975(98)01089-3. [DOI] [PubMed] [Google Scholar]