Abstract
The quadricuspid pulmonary valve is a relatively common congenital anomaly which is rarely complicated clinically and also tends to be under-diagnosed. The following case report shows a 62-year-old man with exertional dyspnea due to quadricuspid pulmonary valve stenosis that was diagnosed by using electrocardiography-gated multiple detector computed tomography. He was then treated effectively by transcatheter balloon pulmonary valvuloplasty using an Inoue balloon catheter.
<Learning Objective: The quadricuspid pulmonary valve is a congenital anomaly which is rarely complicated clinically and tends to be under-diagnosed. Electrocardiography-gated multiple detector computed tomography is a useful imaging modality for diagnosing the quadricusid pulmonary valve. Transcatheter pulmonary valvuloplasty with an Inoue balloon catheter was effective for treating quadricuspid pulmonary valve stenosis.>
Keywords: Quadricupid pulmonary valve, Pulmonary valve stenosis, Balloon pulmonary valvuloplasty
Introduction
The quadricuspid pulmonary valve (QPV) is a relatively common congenital anomaly which tends to be clinically silent thus, it is usually discovered post mortem or by imaging modalities such as multiple detector computed tomography (MDCT) incidentally. Transcatheter balloon pulmonary valvuloplasty (BPV) is the currently-preferred therapeutic modality for valvular pulmonary stenosis (PS) because of its safe procedure and favorable short- and long-term outcomes. The usefulness of the Inoue balloon catheter for BPV in adult PS cases has been reported based on its inherent ability compared with the conventional size-fixed balloon catheters.
Here we describe a case of symptomatic QPV stenosis diagnosed using electrocardiography (ECG)-gated MDCT, and treated by BPV using an Inoue balloon catheter.
Case report
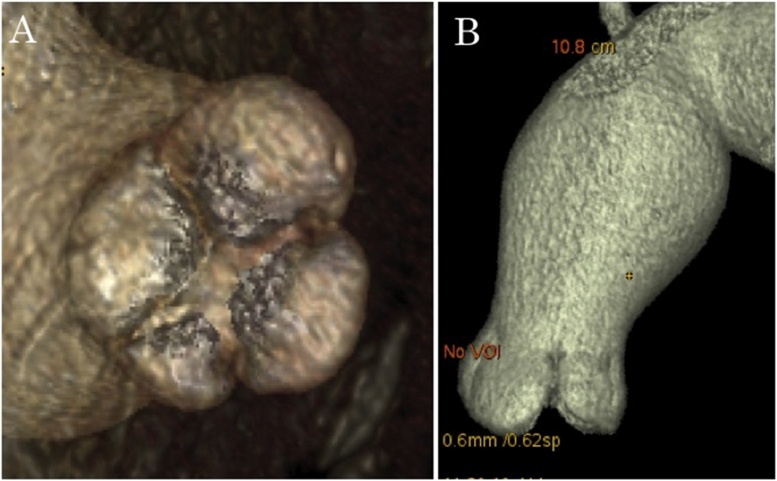
A 62-year-old man was referred to our hospital because of tall R waves in precordial leads and premature ventricular contractions originating from the right ventricular outflow tract, as discovered in an electrocardiogram during a health check-up. Clinical examinations revealed a grade 3 systolic murmur in the second right and left intercostal spaces. Transthoracic echocardiography showed a distortion of the left ventricular chamber and a markedly enlarged right atrium. The estimated pulmonary artery pressure was high; the peak gradient of the trans-tricuspid valve was 101 mmHg. There was a color Doppler mosaic at the pulmonary valve (PV), and the peak gradient was 67 mmHg, which led to the diagnosis of PS. No other cardiac anomalies, including aortic valve malformations, were observed. Diagnostic cardiac catheterization was then performed, and a typical dome-shaped PV with a dilated pulmonary trunk was observed by the right ventriculography. Right ventricular systolic pressure was 102 mmHg, yielding a peak-to-peak gradient across the PV of 82 mmHg without premature ventricular contractions. ECG-gated MDCT for the morphological assessment of the PV revealed QPV (Fig. 1A) in which the diameter of pulmonary annulus was 22 mm with the post-stenotic dilatation of the pulmonary trunk (Fig. 1B).
Fig. 1.
Electrocardiography-gated multiple detector computed tomography, showing quadricuspid pulmonary valve (A) and post-stenotic dilatation of pulmonary trunk (B).
Although we recommended the patient to undergo transcatheter BPV, he initially rejected it because he had no symptoms. However, five months later the patient presented with exertional dyspnea in association with frequent premature ventricular contractions, and thus consented to the treatment. The use of the Inoue percutaneous transvenous mitral commissurotomy (PTMC) balloon catheter for BPV was approved by the ethics committees of Hoshi General Hospital.
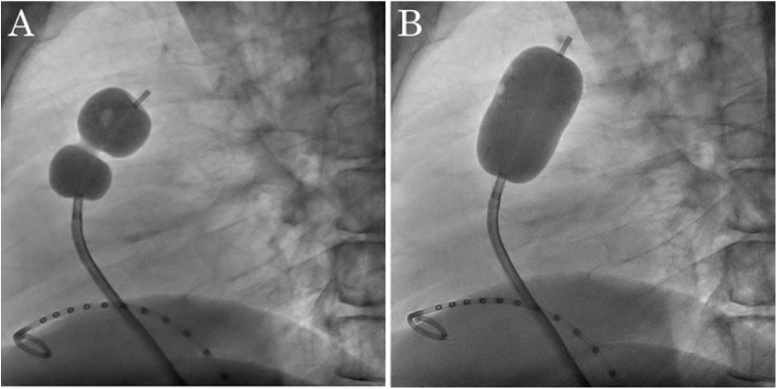
A 5-Fr sheath was inserted into the left femoral vein, and a pigtail catheter (Merit Medical Inc., South Jordan, UT, USA) was positioned in the right ventricle. A 6-Fr sheath was then inserted into the right femoral vein and the PV was crossed by a 6-Fr balloon wedge-pressure catheter (Teleflex, Morrisville, NC, USA). The peak-to-peak gradient across the PV was elevated to 126 mmHg with bigeminal pulse. Although the 0.035 in Amplatz Extra Stiff guidewire (Cook, Inc., Bloomington, IN, USA) failed to cross the PV along the balloon wedge-pressure catheter, which dropped down to the right ventricle, it succeeded in reaching the left pulmonary vein along the 5-Fr pigtail catheter (Terumo Corp., Tokyo, Japan). The Inoue PTMC balloon catheter (22-26 mm) was introduced to the PV along the Amplatz Extra Stiff guidewire and was dilated at 26 mm (Fig. 2), monitoring right ventricular pressure simultaneously. After dilation, right ventricular systolic pressure was immediately reduced to 48 mmHg, yielding a peak-to-peak gradient across the PV of 18 mmHg.
Fig. 2.
The Inoue balloon catheter, which was inflated partially at the stenotic pulmonary valve (A), and was inflated completely as the indentation disappeared (B).
After BPV, exertional dyspnea was improved with a decrease in serum brain natriuretic peptide levels from 548 to 176 pg/ml. Although bigeminal pulse persisted after the procedure, premature ventricular contractions declined gradually for several months. In the echocardiographic follow-up at eight months, the peak gradient at the PV had not risen again.
Discussion
Almost all cases of PS are congenital in origin since PVs are rarely affected by acquired diseases. Although PS is a relatively common adult congenital heart disease with an incidence of 0.12 per 1000 in adults [1], PS patients are usually asymptomatic even though the stenosis is severe. Balloon valvuloplasty is recommended in symptomatic adult PS patients with a peak-to-peak gradient across the PV greater than 30 mmHg at catheterization, and also in asymptomatic patients with a peak-to-peak gradient greater than 40 mmHg [2]. Although the patient in this case was asymptomatic at first even though his peak-to-peak gradient across the PV was 82 mmHg, the ventricular bigeminy, which increased the gradient by Brockenbrough phenomenon, caused the patient’s exertional dyspnea and therefore the decision to undergo BPV.
Transcatheter BPV for the treatment of valvular PS has replaced surgical valvotomy since Kan et al. first reported it in 1982 [3]. A number of studies have confirmed its safety and its favorable short- and long-term outcomes [4]. The use of Inoue balloons for BPV in adult valvular PS was first reported by Lau et al. in 1993 [5]. The usefulness of these balloons was based on their inherent ability to anchor at the PV during inflation, thus preventing abrupt forward movement, to allow stepwise dilation without the necessity of balloon exchanges, and to deflate within a relatively short time, allowing fast hemodynamic recovery. Adequate short- and long-term outcomes after BPV using Inoue balloons for adult valvular PS have been previously reported [6].
The QPV is also a relatively common congenital anomaly, which is usually discovered in postmortem specimens with an incidence of 1 in 400–2000 autopsies, depending on the series reported. It is commonly associated with aortic valve malformations because these semilunar valves originated from the same trunk embryologically. A number of anatomical variations have been reported, in which three equal-sized cusps with one smaller cusp is the most common morphology [7], as MDCT revealed in the present case. QPV tends to be under-diagnosed because the unfavorable anatomical relation of PV and the echo window makes it difficult to visualize PV clearly on echocardiography. Recent advances in MDCT technology permit cardiac CT to provide excellent images of PV, although only echocardiography can evaluate the functional abnormalities of PV. Thus, previous reports have shown the efficacy of ECG-gated MDCT [8] and magnetic resonance imaging [9] to evaluate the morphology of PV.
QPV can be an isolated anatomic variant and rarely complicated clinically, thus only a few cases have been reported of QPV associated with secondary valvular diseases such as PS and regurgitation [9], [10].
To the best of our knowledge, this is the first report to describe symptomatic quadricuspid PS treated by BPV using an Inoue balloon catheter. BPV using Inoue balloon catheters was an effective treatment for PS with QPV.
Conclusion
Our report showed a rare symptomatic adult PS case that was accompanied by QPV. ECG-gated MDCT was a useful modality for diagnosing QPV, and BPV using an Inoue balloon catheter was an effective treatment for quadricuspid PV stenosis.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1.Marelli A.J., Mackie A.S., Ionescu-Ittu R., Rahme E., Pilote L. Congenital heart disease in the general population: changing prevalence and age distribution. Circulation. 2007;115:163–172. doi: 10.1161/CIRCULATIONAHA.106.627224. [DOI] [PubMed] [Google Scholar]
- 2.Bonow R.O., Carabello B.A., Chatterjee K., de Leon A.C., Jr, Faxon D.P., Freed M.D., Gaasch W.H., Lytle B.W., Nishimura R.A., O’Gara P.T., O’Rourke R.A., Otto C.M., Shah P.M., Shanewise J.S. 2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease. J Am Coll Cardiol. 2008;52 doi: 10.1016/j.jacc.2008.05.007. e1-142. [DOI] [PubMed] [Google Scholar]
- 3.Kan J.S., White R.I., Jr., Mitchell S.E., Gardner T.J. Percutaneous balloon valvuloplasty: a new method for treating congenital pulmonary-valve stenosis. N Engl J Med. 1982;307:540–542. doi: 10.1056/NEJM198208263070907. [DOI] [PubMed] [Google Scholar]
- 4.Rao P.S., Galal O., Patnana M., Buck S.H., Wilson A.D. Results of three to 10 year follow up of balloon dilation of the pulmonary valve. Heart. 1998;80:591–595. doi: 10.1136/hrt.80.6.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lau K.W., Hung J.S., Wu J.J., Chern M.S., Yeh K.H., Fu M. Pulmonary valvuloplasty in adults using the Inoue balloon catheter. Catheter Cardiovasc Diagn. 1993;29:99–104. doi: 10.1002/ccd.1810290203. [DOI] [PubMed] [Google Scholar]
- 6.Liu S., Xu X., Liu G., Ding X., Zhao X., Qin Y. Comparison of immediate and long-term results between the single balloon and Inoue balloon techniques for percutaneous pulmonary valvuloplasty. Heart Lung Circ. 2015;24:40–45. doi: 10.1016/j.hlc.2014.05.020. [DOI] [PubMed] [Google Scholar]
- 7.Hurwitz L.E., Roberts W.C. Quadricuspid semilunar valve. Am J Cardiol. 1973;31:623–626. doi: 10.1016/0002-9149(73)90332-9. [DOI] [PubMed] [Google Scholar]
- 8.Jung S.Y. Quadricuspid pulmonary valve in an adult patient identified by transthoracic echocardiography and multi-detector computed tomography. Hellenic J Cardiol. 2015;56:266–268. [PubMed] [Google Scholar]
- 9.Shah R., Shriki J., Shinbane J.S. Cardiovascular magnetic resonance depiction of quadricuspid pulmonary valve with associated pulmonary regurgitation and pulmonary artery aneurysm. Tex Heart Inst J. 2014;41:349–350. doi: 10.14503/THIJ-12-2464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iosifescu A.G., Dorobantu L.F., Anca T.M., Iliescu V.A. Surgical treatment of a pulmonary artery aneurysm due to a regurgitant quadricuspid pulmonary valve. Interact Cardiovasc Thorac Surg. 2012;14:880–882. doi: 10.1093/icvts/ivs088. [DOI] [PMC free article] [PubMed] [Google Scholar]