Abstract
AIM
To determine social, logistical and demographic factors that influence time to discharge in a short stay pathway (SSP) by following total knee arthroplasty (TKA).
METHODS
The study included primary TKA’s performed in a high-volume arthroplasty center from January 2016 through December 2016. Potential variables associated with increased hospital length of stay (LOS) were obtained from patient medical records. These included age, gender, race, zip code, body mass index (BMI), number of pre-operative medications used, number of narcotic medications used, number of patient reported allergies (PRA), simultaneous bilateral surgery, tobacco use, marital status, living arrangements, distance traveled for surgery, employment history, surgical day of the week, procedure end time and whether the surgery was performed during a major holiday week. Multivariate step-wise regression determined the impact of social, logistical and demographic factors on LOS.
RESULTS
Eight hundred and six consecutive primary SSP TKA’s were included in this study. Patients were discharged at a median of 49 h (post-operative day two). The following factors increased LOS: Simultaneous bilateral TKA [46.1 h longer (P < 0.001)], female gender [4.3 h longer (P = 0.012)], age [3.5 h longer per ten-year increase in age (P < 0.001)], patient-reported allergies [1.1 h longer per allergy reported (P = 0.005)], later procedure end-times [0.8 h longer per hour increase in end-time (P = 0.004)] and Black or African American patients [6.1 h longer (P = 0.047)]. Decreased LOS was found in married patients [4.8 h shorter (P = 0.011)] and TKA’s performed during holiday weeks [9.4 h shorter (P = 0.011)]. Non-significant factors included: BMI, median income, patient’s living arrangement, smoking status, number of medications taken, use of pre-operative pain medications, distance traveled to hospital, and the day of surgery.
CONCLUSION
The cost of TKA is dependent upon LOS, which is affected by multiple factors. The clinical care team should acknowledge socio-demographic factors to optimize LOS.
Keywords: Total knee replacement, Total knee arthroplasty, Cost, Risk factors, Length of stay
Core tip: In an effort to decrease post-operative length of stay (LOS), many institutions continue to develop optimal discharge pathways. Since LOS is dependent upon many variables, we sought to define which socio-demographic factors influence LOS in total knee arthroplasty (TKA). Six factors were found to increase LOS: Age, gender, Black or African American race, simultaneous bilateral TKA, later procedure end times and number of PRA. Two factors decreased LOS, patient being married and surgery during a major public holiday week. While none of the patient specific factors are modifiable by the clinician, we do have the ability to optimize surgical schedule and allocation of resources.
INTRODUCTION
Increased utilization of total joint arthroplasty (TJA) is expected to result in a pronounced economic burden on the United States health care system[1]. Subsequently, cost reductions even at the individual case level can translate into a substantial cost savings to the overall system[2]. In-hospital length of stay (LOS) has been shown to directly influence the total cost of joint arthroplasty when patients are discharged home[3,4]. Since LOS is a modifiable cost factor, increased focus has been placed on implementing measures that aim to discharge patients from the hospital as soon as safely possible. The recent development of short stay pathways is a direct result of advancements in surgical, anesthetic and rehabilitation techniques. While there are concerns regarding the overall safety of short stay pathways (SSP) compared to conventional postoperative pathway (CPP), the literature suggests that drastic reductions in LOS can be accomplished without increasing complication rates[5].
Factors influencing LOS such as age, gender and perioperative complications have been previously described in the literature under CPP for hip and knee arthroplasty[6,7]. At the earliest, patients in these CPP studies were discharged on the 3rd day following surgery[6-8]. Keswani et al[8] found that patients with later surgical start times and end of the week procedure days (Thursday and Friday) had longer LOS in a CPP. However, a separate study performed at an institution utilizing a SSP found that surgical day of the week had no correlation with LOS[9]. Another institution utilizing SSP investigated the influence of preoperative patient characteristics and perioperative surgical factors related to prolonged LOS[10,11]. Regardless there remains limited data on the factors influencing LOS following TKA in a SSP.
The primary purpose of this study was to assess the influence of social, logistical and demographic factors on time to discharge in a SSP for TKA. The findings from this study may further enhance preoperative and perioperative risk stratification models that already incorporate patient characteristics and perioperative surgical factors but neglect other potentially influential variables.
MATERIALS AND METHODS
Methods
A retrospective chart review was performed for a consecutive series of 806 elective primary TKA’s performed at a single specialty hospital from January 2016 to December 2016. All procedures were performed by one of 3 experienced surgeons, each performing more than 250 TKA’s per year. All surgeries, regardless of LOS, were performed using the hospital’s SSP for each phase of care. This study was evaluated and an Institutional Review Board (IRB) exemption was given for this work by the Texas Orthopedic Hospital IRB (TOH203e).
Short stay protocol
All patients at this institution undergo a formal preoperative screening process to ensure they are safe for surgery and postoperative care within our specialty hospital. Active renal replacement therapy, active lung disease requiring home oxygen support, or active cardiac disease requiring a defibrillator exclude the patient from surgery at this institution. Each patient is medicated preoperatively with celecoxib 200 mg, Neurontin 100 mg, and acetaminophen 650 mg. Intra-operative anesthesia consists of a propofol infusion with no inhalation anesthetic and no muscle relaxation. During the procedure a periarticular anesthetic of weight-based ropivicaine 0.5% and morphine 5-10 mg is injected into the soft tissues prior to closure. All patients are given 1 g intravenous (IV) tranexamic acid prior to incision and 1 gram prior to closure, unless it is contraindicated, at which point it is administered topically. Post-operative medication regimen consists of a combination of hydrocodone, tramadol, methocarbamol, dexamethasone and IV ketorolac. Deep vein thrombosis prophylaxis consists of aspirin or rivaroxaban per surgeon discretion and is continued for 4 wk. Patients are mobilized approximately 2 h after surgery with physical therapists. Standing is attempted, and if tolerated, patients are allowed to walk with a walker and assistance as far as they can tolerate. Continuous passive motion devices were used during the study period per surgeon discretion. The following morning patients undergo their second session with the physical therapists. The three surgeons included in this study independently round on their patients on all days, including weekends and holidays. Patients were discharged as soon as they had adequate oral pain control, are safe to ambulate and mobilize with an assistive device and are hemodynamically stable.
Study outcomes
Potential variables associated with increased hospital LOS were obtained from patient medical records. These included age, gender, race, zip code, body mass index (BMI), number of pre-operative medications used, number of narcotic medications used, number of patient reported allergies (PRA), simultaneous bilateral surgery, tobacco use, marital status, living arrangements, distance traveled for surgery, employment history, surgical day of the week, procedure end time and whether the surgery was performed during a major holiday week. Thanksgiving, Christmas and New Year’s Eve were the major holidays included in the study. The patient’s zip code was used to obtain the median household income of the zip code from the 2016 American Community Survey performed by the United States Census Bureau[12].
Baseline demographics, surgical factors, and social factors were summarized by mean (± SD) for continuous factors or by count and percentages for categorical factors in order to characterize the study population. Multivariate regression analysis was performed to determine the contribution of demographic, logistical and social factors on LOS. A stepwise model was used to determine the number of factors significantly associated with LOS. Statistical significance was defined as P < 0.05 and SPSS 24 (IBM Corp., Armonk, NY, United States) was used for statistical analyses.
RESULTS
A total of 806 primary TKA cases were included in the study. There were 491 female (60.9%) patients and the average age of the study population was 64.5 years. 76.6% of the study population were identified as White, 11.4% as other, 7.8% black/African American, 2.2% identified as Asian and 1.9% declined to state. The median LOS was 49.0 h with a range from 18-236 h. All subject characteristics that were included in the analysis are depicted in Table 1.
Table 1.
Baseline subject characteristics
| Factor | mean ± SD or n (%) |
| Number of patients | 806 |
| Gender | |
| Male | 315 (39.1) |
| Female | 491 (60.9) |
| Age (yr) | 64.5 ± 8.5 |
| Race | |
| Asian | 18 (2.2) |
| Black/African American | 63 (7.8) |
| White | 617 (76.6) |
| Other | 94 (11.4) |
| Decline to state | 16 (1.9) |
| Body mass index | 33.81 ± 7.4 |
| Employed | 347 (43.1) |
| Median income by zip code | $66586 ± 25562 |
| Marital Status | |
| Single | 105 (13.0) |
| Married | 593 (73.6) |
| Widow/widower | 66 (8.2) |
| Divorced | 42 (5.2) |
| Patient lives alone (Y) | 99 (12.3) |
| Smoker | |
| Current | 68 (8.4) |
| Former | 232 (28.8) |
| Never | 506 (62.8) |
| Number of allergies | 1.5 ± 2.2 |
| Number of medications | 6.1 ± 4.8 |
| Pre-operative pain meds (Y) | 108 (13.4) |
| Simultaneous bilateral total knee arthroplasty | 37 (4.6) |
| Distance from hospital (miles) | 61.95 ± 122.8 |
| Day of surgery | |
| Monday | 242 (30.0) |
| Tuesday | 175 (21.7) |
| Wednesday | 129 (16.0) |
| Thursday | 194 (24.1) |
| Friday | 61 (7.6) |
| Saturday | 5 (0.6) |
| Holiday week surgery | 43 (5.3) |
| Surgery end time (h:min) | 11:05 ± 2:22 |
In our study population, the constant (or baseline regression model) for LOS was 22.7 h (P = 0.004). Adding or subtracting beta coefficients for other factors predicts individual patient LOS. Multiple regression identified six factors that increased LOS (Table 2): Simultaneous bilateral TKA [46.1 h longer (P < 0.001)], female gender [4.3 h longer (P = 0.012)], age [3.5 h longer per ten-year increase in age (P < 0.001)], number of PRA’s [1.1 h longer per each reported number of allergies (P = 0.005)], later procedure end-times [0.8 h longer per hour increase in end-time (P = 0.040)] and Black or African American patients [6.1 h longer (P = 0.047)]. Two factors were found to decrease LOS: Patients being married [4.8 h shorter (P = 0.011)] and TKA’s performed during major holiday weeks [9.4 h shorter (P = 0.011)]. Non-significant factors included: BMI, median income, patient’s living arrangement, smoking status, number of medications taken, use of pre-operative pain medications, distance traveled to hospital, and the day of surgery.
Table 2.
Significant factors predicting length of stay
| Factor | Beta coefficient (h)1 | Std. error | P value |
| Constant | 22.7 | 7.8 | 0.004 |
| Simultaneous bilateral total knee arthroplasty | 46.1 | 4.1 | < 0.001 |
| Gender (female) | 4.3 | 1.7 | 0.012 |
| Age (per 10 yr) | 3.5 | 1.0 | < 0.001 |
| Patient is married | -4.8 | 1.9 | 0.011 |
| Number of allergies | 1.1 | 0.4 | 0.005 |
| Holiday week surgery | -9.4 | 3.6 | 0.011 |
| Surgery end time | 0.8 | 0.4 | 0.040 |
| Black/African American | 6.1 | 3.0 | 0.047 |
In our study population, the constant for length of stay (LOS) was 22.7 h. Adding or subtracting beta coefficients for other factors predicts individual patient LOS.
DISCUSSION
LOS is a modifiable cost factor in the overall expense of TJA. Increased emphasis has been placed on both employing SSP and optimizing risk stratification models that identify those who may or may not be appropriate candidates for SSP. Our study identified simultaneous bilateral TKA, female gender, increased age, increased number of PRA, later surgery end time and race identified as Black or African American as factors that increased LOS. Two factors, patient being married and procedures performed during major holiday weeks decreased LOS.
Increased age and female gender are factors that are known to correlate with increased LOS in SSP[11,13]. Both simultaneous bilateral TKA[14] and patient identified race as non-Caucasian[15] have been shown to increase LOS in CPP as well as SSP. Our data showed that patients identifying as Black or African American had a significantly longer LOS after TKA, while other racial groups (White and Other) showed no difference in LOS. Racial disparities in utilization, complication rates and outcomes of arthroplasty are prevalent in the literature[15-17], however, race is often confounded with socioeconomic factors. In our study, Black patients had a longer LOS but median household income was not a significant factor influencing LOS. Further analysis showed that the median income of Black patients in our study was just over $41000 while both White and Other patients was over $60000 (Figure 1). According to the American Community Survey the median income for the United States in 2016 was $55322[12], so in our patient population Black patients were well under the United States median income while White and Other patients were slightly above. Thus, increased LOS in Black patients may not be entirely due to race, as socioeconomic factors may also be confounded by race. Future studies will need to further define the complex relationships between race, socioeconomic status, perioperative outcomes and LOS in TJA.
Figure 1.
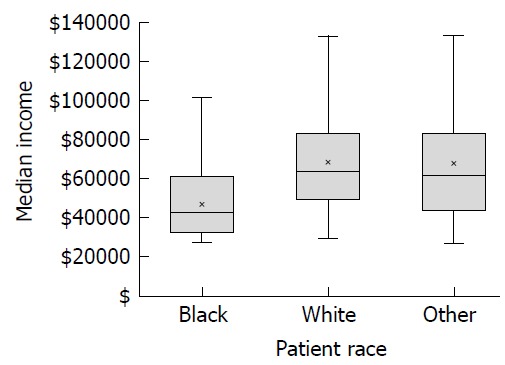
Median income level by race with the bold horizontal line representing the median, the box shows the 25% to 75% range, the x is the mean and the whiskers represent the entire range of the data.
To our knowledge, marital status has not previously been shown to demonstrate any influence on LOS following TKA. While limited, the literature outside of orthopedics suggests that being married may be associated with better treatment outcomes[18,19]. However, marital status has been shown to affect outcomes following TKA as patients that are married have better overall outcomes following TKA[20]. In our study, married patients had a decreased postoperative LOS. Our findings corroborate the general trend in the literature, with a positive association between being married and improved treatment outcomes. Notably, marital status has recently been identified as a key variable that should be investigated in future research on outcomes of knee and hip surgery[21].
Prior studies indicate that increasing amounts of PRA’s is associated with worse outcomes following total hip and knee arthroplasty[22-24]. Interestingly, the patient reported “allergy” is often a misnomer as only 15% of PRA’s studied in a community hospital setting represented a true IgE mediate hypersensitivity reaction[25]. In a study utilizing data from the Canadian Community Health registry, an association between mood and anxiety disorders and PRA reporting was demonstrated[26]. As the relationship between PRA and psychiatric disorders is further elucidated, their impact on all aspects of TJA is becoming more apparent. In a prospective study of 446 patients undergoing primary hip and knee arthroplasty, Otero el al[22] found that patients reporting at least 1 allergy had significantly lower postoperative SF-36 physical component score compared to those reporting no allergies. In a retrospective review, McLawhorn et al[23] demonstrated that increasing number of PRAs was associated with both worse satisfaction and Western Ontario and McMaster Universities Arthritis Index scores, in addition to increased LOS following TKA in a CPP. The median LOS of the patients included in their TKA cohort was 4.0 d. Our study found that for each reported allergy, LOS increased by 0.8 h. While this may seem to be an insignificant amount of time, it is not uncommon to encounter patients with many PRAs in practice; in our study, one patient reported twenty-three. In an SSP, increasing the LOS by just a few hours may represent the difference in an additional day spent in the hospital.
The relationship between surgical day of the week and LOS has previously been studied in both CPP and SSP. In separate retrospective reviews, both Muppavarapu et al[27] and Keswani et al[8] found that patients who underwent TJA or total hip arthroplasty (THA) respectively, on Thursday or Friday had significantly longer hospital LOS compared to patients undergoing those procedures earlier in the week. These two studies represented a CPP as the LOS of the patients included these studies was greater than 3 d. A comprehensive PubMed search found only one study that investigates the effect of surgical day of the week on LOS in an SSP for total joint arthroplasty. In a cohort of patients with an average LOS of < 2 d, Edwards et al[9] found that surgical day of the week did not influence time to discharge. Our results were similar as surgical day of the week did not influence LOS in our SSP. These findings suggest that as LOS decreases the overall impact of performing a procedure towards the end of the week may diminish.
The influence of surgical start time on LOS has been investigated across several surgical subspecialties with the evidence suggesting that as cases begin later in the day, LOS increases[28,29]. Earnest et al[28] suspected that initial post-operative care is delayed for patients admitted in the afternoon because clinical workup and management usually occurs in the morning. Only one study has investigated the influence of surgical timing on LOS in total joint arthroplasty. In a cohort of THA patients receiving conventional postoperative care pathways, Keswani et al[8] found that procedures starting after 2 PM were associated with longer LOS compared to procedures starting prior to 2 PM. We found that LOS was slightly shorter for every hour later the procedure ended. In our institution’s SSP, post-operative protocols do not depend on the time of day as staffing is consistent between shifts. Patients are encouraged to work with a physical therapist just a few hours after surgery when clinically feasible. Our findings suggest that unlike CPP, in SSP the surgical start time of the procedure is less critical.
The relationship between public holidays and LOS across all medical fields has never been reported, a few studies have sought to understand the influence of holidays on clinical outcomes and readmission[30-32]. In our study, patients undergoing TKA during major public holiday weeks were found to have decreased LOS as compared to patients having surgery during a normal week. Several factors likely influence these findings including patient, surgeon and staff related variables. As our study included three surgeons, the most senior surgeon performed fewer procedures during holiday weeks and also had a slightly higher LOS average, possibly confounding the lower LOS holiday week results. While these results do leave room for speculation, the present study could not delineate any additional conclusions from these findings; therefore this is an area that future studies should consider investigating further.
Our study had several limitations. First, the data used was retrospectively collected and therefore susceptible to inherent bias in its analysis. Secondly, race identification was limited to what was reported in the chart and the ‘other’ classification likely encompassed a variety of distinct ethnicities that could not be further discerned. Third, there was potential for type II statistical error as certain variables approached but did not reach significance in this study. As it pertains to LOS, several variables that were originally thought to be relevant factors were not. In particular, distance traveled and pre-operative narcotic use did not reach significance in our cohort.
In an effort to decrease post-operative LOS, many institutions continue to develop optimal discharge pathways following TKA. Since LOS is dependent upon many variables, we sought to define which social, logistical and demographic factors influence LOS in TKA. Six factors were found to increase LOS in a SSP: Age, gender, Black or African American race, simultaneous bilateral TKA, later procedure end times and number of PRA’s. Two factors decreased LOS in an SSP, patient being married and surgery during a major public holiday week. While none of the patient specific factors (e.g., age, race, gender, marital status, socioeconomic status, and PRA’s) are modifiable by the clinician, we do have the ability to optimize surgical schedule and allocation of resources. When refining predictive models for LOS, in addition to considering known clinical factors, the care team should also appreciate the extent that social, demographic and logistical factors influence LOS. Furthermore, the influence of these factors may depend on whether a CPP or an SSP model is being employed.
ARTICLE HIGHLIGHTS
Research background
Time to discharge or in-hospital length of stay (LOS) has been shown to directly influence the total cost of joint arthroplasty when patients are discharged home. Since LOS is a modifiable cost factor, increased focus has been placed on implementing measures that aim to discharge patients from the hospital as soon as safely possible. The recent development of short stay pathways is a direct result of advancements in surgical, anesthetic and rehabilitation techniques. Traditional factors such as age, gender, comorbidities and perioperative complications have been studied extensively and influence LOS. Patient social, logistical and demographic factors are non-modifiable factors but potentially influence LOS.
Research motivation
The motivation behind this research was to further improve short stay pathways by evaluating non-traditional factors that potentially could influence LOS. Our hypothesis was that social, logistical and demographic factors influence LOS following total knee arthroplasty (TKA) in a short stay pathway.
Research objectives
The primary purpose of this study was to assess the influence of social, logistical and demographic factors on time to discharge in a short stay pathway following TKA. The findings from this study may further enhance preoperative and perioperative risk stratification models that already incorporate patient characteristics and perioperative surgical factors but neglect other potentially influential variables.
Research methods
A retrospective chart review was performed for a consecutive series of 806 elective primary TKA’s performed at a single specialty hospital from January 2016 to December 2016. Potential variables associated with increased hospital LOS were obtained from patient medical records. These included age, gender, race, zip code, body mass index (BMI), number of pre-operative medications used, number of narcotic medications used, number of patient reported allergies (PRA), simultaneous bilateral surgery, tobacco use, marital status, living arrangements, distance traveled for surgery, employment history, surgical day of the week, procedure end time and whether the surgery was performed during a major holiday week. Thanksgiving, Christmas and New Year’s Eve were the major holidays included in the study. Baseline demographics, surgical factors, and social factors were summarized by mean (± SD) for continuous factors or by count and percentages for categorical factors in order to characterize the study population. Multivariate regression analysis was performed to determine the contribution of demographic, logistical and social factors on LOS.
Research results
Patients were discharged at a median of 49 h (post-operative day two). Six factors increased LOS: Simultaneous bilateral TKA, female gender, age, patient-reported allergies, later procedure end-times, and Black or African American patients. Decreased LOS was found in married patients and TKA’s performed during holiday weeks. Non-significant factors included: BMI, median income, patient’s living arrangement, smoking status, number of medications taken, use of pre-operative pain medications, distance traveled to hospital, and the day of surgery.
Research conclusions
The cost of TKA is dependent upon LOS, which is affected by multiple factors. The clinical care team should acknowledge socio-demographic factors to further optimize short stay pathways and decrease LOS.
Research perspectives
In an effort to decrease post-operative LOS, many institutions continue to develop optimal discharge pathways following TKA. Since LOS is dependent upon many variables, we sought to define which social, logistical and demographic factors influence LOS in TKA. Six factors were found to increase LOS in a short stay pathway: Age, gender, Black or African American race, simultaneous bilateral TKA, later procedure end times and number of PRA’s. Two factors decreased LOS: Patient being married and surgery during a major public holiday week. While none of the patient specific factors (e.g., age, race, gender, marital status, socioeconomic status, and PRA’s) are modifiable by the clinician, we do have the ability to optimize surgical schedule and allocation of resources. When refining predictive models for LOS, in addition to considering known clinical factors, the care team should also appreciate the extent that social, demographic and logistical factors influence LOS.
Footnotes
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Institutional review board statement: This study was evaluated and an IRB exemption was given for this work by the Texas Orthopedic Hospital’s IRB (TOH203e).
Informed consent statement: Patients were not required to give informed consent to the study because the analysis used anonymous clinical data and the study was given an IRB exemption.
Conflict-of-interest statement: All authors declare no conflicts-of-interest related to this article but the following authors have financial relationships to report in general: Robin Goytia reports personal fees from Innomed, outside the submitted work; Gregory Stocks reports stock ownership from Nimbic Systems, Inc., outside the submitted work; Mark Brinker reports personal fees from Zimmer Biomet, outside the submitted work.
Peer-review started: October 4, 2018
First decision: October 29, 2018
Article in press: December 10, 2018
P- Reviewer: Fenichel I, Wu CC S- Editor: Ji FF L- Editor: A E- Editor: Bian YN
Contributor Information
Ugonna N Ihekweazu, Fondren Orthopedic Group, Houston, TX 77030, United States; Fondren Orthopedic Research Institute, Fondren Orthopedic Group, Houston, TX 77030, United States.
Garrett H Sohn, Department of Orthopedic Surgery, Baylor College of Medicine, Houston, TX 77030, United States.
Mitzi S Laughlin, Fondren Orthopedic Research Institute, Fondren Orthopedic Group, Houston, TX 77030, United States. mitzi.laughlin@fondren.com.
Robin N Goytia, Fondren Orthopedic Group, Houston, TX 77030, United States; Fondren Orthopedic Research Institute, Fondren Orthopedic Group, Houston, TX 77030, United States.
Vasilios Mathews, Fondren Orthopedic Group, Houston, TX 77030, United States; Fondren Orthopedic Research Institute, Fondren Orthopedic Group, Houston, TX 77030, United States.
Gregory W Stocks, Fondren Orthopedic Group, Houston, TX 77030, United States; Fondren Orthopedic Research Institute, Fondren Orthopedic Group, Houston, TX 77030, United States.
Anay R Patel, Fondren Orthopedic Group, Houston, TX 77030, United States; Fondren Orthopedic Research Institute, Fondren Orthopedic Group, Houston, TX 77030, United States.
Mark R Brinker, Fondren Orthopedic Group, Houston, TX 77030, United States; Fondren Orthopedic Research Institute, Fondren Orthopedic Group, Houston, TX 77030, United States.
References
- 1.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 2.Teeny SM, York SC, Benson C, Perdue ST. Does shortened length of hospital stay affect total knee arthroplasty rehabilitation outcomes? J Arthroplasty. 2005;20:39–45. doi: 10.1016/j.arth.2005.04.025. [DOI] [PubMed] [Google Scholar]
- 3.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. JAMA. 2012;308:1227–1236. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meyers SJ, Reuben JD, Cox DD, Watson M. Inpatient cost of primary total joint arthroplasty. J Arthroplasty. 1996;11:281–285. doi: 10.1016/s0883-5403(96)80079-9. [DOI] [PubMed] [Google Scholar]
- 5.Stambough JB, Nunley RM, Curry MC, Steger-May K, Clohisy JC. Rapid recovery protocols for primary total hip arthroplasty can safely reduce length of stay without increasing readmissions. J Arthroplasty. 2015;30:521–526. doi: 10.1016/j.arth.2015.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rissanen P, Aro S, Paavolainen P. Hospital- and patient-related characteristics determining length of hospital stay for hip and knee replacements. Int J Technol Assess Health Care. 1996;12:325–335. doi: 10.1017/s0266462300009661. [DOI] [PubMed] [Google Scholar]
- 7.Forrest G, Fuchs M, Gutierrez A, Girardy J. Factors affecting length of stay and need for rehabilitation after hip and knee arthroplasty. J Arthroplasty. 1998;13:186–190. doi: 10.1016/s0883-5403(98)90097-3. [DOI] [PubMed] [Google Scholar]
- 8.Keswani A, Beck C, Meier KM, Fields A, Bronson MJ, Moucha CS. Day of Surgery and Surgical Start Time Affect Hospital Length of Stay After Total Hip Arthroplasty. J Arthroplasty. 2016;31:2426–2431. doi: 10.1016/j.arth.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 9.Edwards PK, Hadden KB, Connelly JO, Barnes CL. Effect of Total Joint Arthroplasty Surgical Day of the Week on Length of Stay and Readmissions: A Clinical Pathway Approach. J Arthroplasty. 2016;31:2726–2729. doi: 10.1016/j.arth.2016.05.057. [DOI] [PubMed] [Google Scholar]
- 10.Sibia US, King PJ, MacDonald JH. Who Is Not a Candidate for a 1-Day Hospital-Based Total Knee Arthroplasty? J Arthroplasty. 2017;32:16–19. doi: 10.1016/j.arth.2016.06.055. [DOI] [PubMed] [Google Scholar]
- 11.Sibia US, MacDonald JH, King PJ. Predictors of Hospital Length of Stay in an Enhanced Recovery After Surgery Program for Primary Total Hip Arthroplasty. J Arthroplasty. 2016;31:2119–2123. doi: 10.1016/j.arth.2016.02.060. [DOI] [PubMed] [Google Scholar]
- 12.US Census Bureau. American Community Survey, 2016 [cited 20 April 2018]. Detailed tables [Internet] Available from: URL: https://factfinder.census.gov/faces/nav/jsf/pages/community_facts.xhtml.
- 13.Husted H, Holm G, Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop. 2008;79:168–173. doi: 10.1080/17453670710014941. [DOI] [PubMed] [Google Scholar]
- 14.Suleiman LI, Edelstein AI, Thompson RM, Alvi HM, Kwasny MJ, Manning DW. Perioperative Outcomes Following Unilateral Versus Bilateral Total Knee Arthroplasty. J Arthroplasty. 2015;30:1927–1930. doi: 10.1016/j.arth.2015.05.039. [DOI] [PubMed] [Google Scholar]
- 15.Inneh IA. The Combined Influence of Sociodemographic, Preoperative Comorbid and Intraoperative Factors on Longer Length of Stay After Elective Primary Total Knee Arthroplasty. J Arthroplasty. 2015;30:1883–1886. doi: 10.1016/j.arth.2015.05.032. [DOI] [PubMed] [Google Scholar]
- 16.Martsolf GR, Barrett ML, Weiss AJ, Kandrack R, Washington R, Steiner CA, Mehrotra A, SooHoo NF, Coffey R. Impact of Race/Ethnicity and Socioeconomic Status on Risk-Adjusted Hospital Readmission Rates Following Hip and Knee Arthroplasty. J Bone Joint Surg Am. 2016;98:1385–1391. doi: 10.2106/JBJS.15.00884. [DOI] [PubMed] [Google Scholar]
- 17.Singh JA, Lu X, Rosenthal GE, Ibrahim S, Cram P. Racial disparities in knee and hip total joint arthroplasty: an 18-year analysis of national Medicare data. Ann Rheum Dis. 2014;73:2107–2115. doi: 10.1136/annrheumdis-2013-203494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Franks MM, Stephens MA, Rook KS, Franklin BA, Keteyian SJ, Artinian NT. Spouses’ provision of health-related support and control to patients participating in cardiac rehabilitation. J Fam Psychol. 2006;20:311–318. doi: 10.1037/0893-3200.20.2.311. [DOI] [PubMed] [Google Scholar]
- 19.Aizer AA, Chen MH, McCarthy EP, Mendu ML, Koo S, Wilhite TJ, Graham PL, Choueiri TK, Hoffman KE, Martin NE, et al. Marital status and survival in patients with cancer. J Clin Oncol. 2013;31:3869–3876. doi: 10.1200/JCO.2013.49.6489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roubion RC, Fox RS, Townsend LA, Pollock GR, Leonardi C, Dasa V. Does Marital Status Impact Outcomes After Total Knee Arthroplasty? J Arthroplasty. 2016;31:2504–2507. doi: 10.1016/j.arth.2016.04.017. [DOI] [PubMed] [Google Scholar]
- 21.Lieberman JR, Teuscher D, Berry DJ, Vail TP. 2015. AAOS’ comments on CMS’ Comprehensive Care for Joint Replacement Payment Model for Acute Care Hospitals Furnishing Lower Extremity Joint Replacement Services Proposed Rule [CMS-5516-P] Available from: URL: https://innovation.cms.gov/initiatives/cjr. [Google Scholar]
- 22.Otero JE, Graves CM, Gao Y, Olson TS, Dickinson CC, Chalus RJ, Vittetoe DA, Goetz DD, Callaghan JJ. Patient-Reported Allergies Predict Worse Outcomes After Hip and Knee Arthroplasty: Results From a Prospective Cohort Study. J Arthroplasty. 2016;31:2746–2749. doi: 10.1016/j.arth.2016.07.040. [DOI] [PubMed] [Google Scholar]
- 23.McLawhorn AS, Bjerke-Kroll BT, Blevins JL, Sculco PK, Lee YY, Jerabek SA. Patient-Reported Allergies Are Associated With Poorer Patient Satisfaction and Outcomes After Lower Extremity Arthroplasty: A Retrospective Cohort Study. J Arthroplasty. 2015;30:1132–1136. doi: 10.1016/j.arth.2015.01.043. [DOI] [PubMed] [Google Scholar]
- 24.Graves CM, Otero JE, Gao Y, Goetz DD, Willenborg MD, Callaghan JJ. Patient reported allergies are a risk factor for poor outcomes in total hip and knee arthroplasty. J Arthroplasty. 2014;29:147–149. doi: 10.1016/j.arth.2014.02.040. [DOI] [PubMed] [Google Scholar]
- 25.Chen CJ, Cheng CF, Lin HY, Hung SP, Chen WC, Lin MS. A comprehensive 4-year survey of adverse drug reactions using a network-based hospital system. J Clin Pharm Ther. 2012;37:647–651. doi: 10.1111/j.1365-2710.2012.01359.x. [DOI] [PubMed] [Google Scholar]
- 26.Patten SB, Williams JV. Self-reported allergies and their relationship to several Axis I disorders in a community sample. Int J Psychiatry Med. 2007;37:11–22. doi: 10.2190/L811-0738-10NG-7157. [DOI] [PubMed] [Google Scholar]
- 27.Muppavarapu RC, Chaurasia AR, Schwarzkopf R, Matzkin EG, Cassidy CC, Smith EL. Total joint arthroplasty surgery: does day of surgery matter? J Arthroplasty. 2014;29:1943–1945. doi: 10.1016/j.arth.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 28.Earnest A, Chen MI, Seow E. Exploring if day and time of admission is associated with average length of stay among inpatients from a tertiary hospital in Singapore: an analytic study based on routine admission data. BMC Health Serv Res. 2006;6:6. doi: 10.1186/1472-6963-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Slaughter KN, Frumovitz M, Schmeler KM, Nick AM, Fleming ND, dos Reis R, Munsell MF, Westin SN, Soliman PT, Ramirez PT. Minimally invasive surgery for endometrial cancer: does operative start time impact surgical and oncologic outcomes? Gynecol Oncol. 2014;134:248–252. doi: 10.1016/j.ygyno.2014.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sebghatollahi V, Ghomi K, Tamizifar B, Minakari M, Khodadoustan M. The Relationship between the Time of Endoscopy and Morbidity and Mortality Rates in Patients with Upper Gastrointestinal Bleeding. Adv Biomed Res. 2017;6:81. doi: 10.4103/2277-9175.210664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Orsini J, Rajayer S, Ahmad N, Din N, Morante J, Malik R, Shim A. Effects of time and day of admission on the outcome of critically ill patients admitted to ICU. J Community Hosp Intern Med Perspect. 2016;6:33478. doi: 10.3402/jchimp.v6.33478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Richards MK, Yanez D, Goldin AB, Grieb T, Murphy WM, Drugas GT. Factors associated with 30-day unplanned pediatric surgical readmission. Am J Surg. 2016;212:426–432. doi: 10.1016/j.amjsurg.2015.12.012. [DOI] [PubMed] [Google Scholar]


