Abstract
Context:
Early detection of oral cancer is of paramount importance in determining the prognosis of oral cancer. Literature suggests that several diagnostic modalities have been proposed to aid a clinician in early detection of oral cancer without much conclusive evidence.
Aims:
The present study aims to compare toluidine blue and chemiluminescence screening methods in early detection of carcinoma in North Indian population and also to evaluate these methods with histopathological diagnosis.
Methods:
In this prospective study, 42 patients with clinically visible premalignant lesions were included. Demographic data were collected, and suspicious lesions were examined by chemiluminescence light (Vizilite) and followed by local application of toluidine blue (Mashberg's recommendation). Findings were recorded for each lesion under standard incandescent light as positive or negative. Biopsy and histopathological analysis of the tissues were performed.
Statistical Analysis:
Sensitivity, specificity and positive and negative predictive values for the chemiluminescence technique and toluidine blue were calculated for diagnostic tests.
Results and Conclusions:
In the present study, toluidine blue test was found to be moderately sensitive (63.33%) whereas chemiluminescence test (Vizilite) was found to be highly sensitive (90%); however, the test has limited specificity (50%). Thus, the study concluded that both toluidine blue and Vizilite can be used as an adjunct to simple, conventional visual examination and in screening procedure for oral potentially malignant disorders.
Keywords: Chemiluminescence, sensitivity, specificity, toluidine blue
INTRODUCTION
Among all the malignancies, oral cancer is the tenth most common cancer in the world with a marked geographic difference in occurrence and hence remains a serious oral health problem worldwide.[1] The highest rates in the world for oral cancer are found in France, the Indian subcontinent, Brazil and Central/Eastern Europe.[2] The common occurrence among Indian population is attributed to the well-established association of oral cancer with betel-quid chewing.[3] Oral cancer has one of the lowest survival rates of 30%–80%, within a 5-year period.[4,5,6,7] The WHO reported oral cancer as having one of the highest mortality ratios among all malignancies,[5] due to delayed diagnosis and the surgical treatment causing facial disfigurement, impaired speech and malnutrition.[8] The absence of a reliable method for early diagnosis of oral cancer is responsible for the delay in diagnosis and thus poor prognosis. Even a thorough clinical examination cannot reliably identify early malignancies as they might not be clinically palpable and might resemble the surrounding normal mucosa in color. Furthermore, early lesions might resemble reactive or inflammatory condition. Thus, identifying a clinically suspicious or undetectable lesion through some diagnostic adjunct has gained importance, whereby diagnosis can be confirmed by biopsy at an earlier stage.[9]
Noninvasive screening tools such as toluidine blue allow a clinician to more reliably evaluate the high-risk sites in the oral cavity. The newer modalities such as chemiluminescence use wavelengths that reveal obvious differences in the color of suspected lesions compared to the surrounding healthy tissue. This offers the clinician the potential to identify dysplastic cells in earlier stages and to discover unseen borders. These diagnostic adjuncts aid in diagnosing suspicious areas in premalignant lesions, offering a promise in terms of early diagnosis and thereby instituting early treatment. Thus, the present study aims to compare these screening methods to find out their efficacy in early detection of carcinoma and also to compare these methods with gold standard biopsy.
METHODS
The study design involved screening of clinically visible oral potentially malignant disorders and malignant lesions with the conventional toluidine blue vital staining and the newer chemiluminescence technique. This study was approved by the Institutional Ethical committee, and all the guidelines given in the Declaration of Helsinki were followed.
Forty-two individuals (37 males and 5 females), between 21 and 60 years of age, reporting to the Department of Oral Pathology and Microbiology, presenting with the clinically evident oral potentially malignant and malignant pathologies were included in the study after obtaining informed consent.
Demographic data were collected, suspicious lesions were examined conventionally under incandescent light and the findings were recorded. This was followed by chemiluminescence examination where the patient was asked to rinse oral cavity by 1% acetic acid solution for 1 min. Room lights were dimmed, the oral cavity was examined under chemiluminescence light (Vizilite) and the findings were recorded. Mucosa which appeared as decreased blue or dark was recorded as negative finding, and the mucosa appearing as improved “aceto-white” was considered a positive finding.
This was followed by examination with 1% toluidine blue where all visualized lesions were again swabbed with 1% acetic acid followed by local application of toluidine blue (Mashberg's recommendation) with a presoaked swab for 2 min. The patient was then asked to rinse the oral cavity by 1% acetic acid to remove any extra toluidine blue. Retention of toluidine blue was recorded for each lesion under standard incandescent light as positive or negative. Special care was taken to remove mechanical retention of the dye to reduce false-positive results. After rinsing the mouth with 1% acetic acid, dye from the retention areas was again wiped with cotton bud soaked in 1% acetic acid.
Biopsy and histopathological analysis of the tissues were performed. The paraffin-embedded specimens were cut into 3–4 μm thick sections and stained with hematoxylin-eosin. The tissues were analyzed and were classified as negative (acanthosis, inflammatory lesions), positive which included dysplasia (subdivided into mild dysplasia, moderate dysplasia, severe dysplasia and carcinoma in situ), oral lichen planus, oral submucous fibrosis, proliferative verrucous leukoplakia and invasive carcinoma (squamous cell carcinoma [SCC] and verrucous carcinoma). The definition of invasive carcinoma was based on the detection of infiltrative growth patterns for individual malignant cells or glands. Results from biopsy were considered as gold standard of diagnosis.
The data obtained were statistically analyzed. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value for the chemiluminescent technique and toluidine blue were calculated using the UK Centre for Evidence-Based Medicine online calculator for diagnostic test. Sensitivity, specificity, accuracy, PPV and negative predictive value were calculated using the following formulae:
Sensitivity = (true positives/[true positive + false negative]) ×100
Specificity = (true negatives/[true negative + false positive]) ×100
Accuracy = sensitivity + specificity
Predictive value for a positive result (PV+) = (true positive/[true positive + false positive]) ×100
Predictive value for a negative result (PV−) = (true negative/[true negative + false negative]) ×100.
The SPSS 20.0 software package for Macintosh (IBM, Armonk, NY, USA) was used for data analysis.
RESULTS
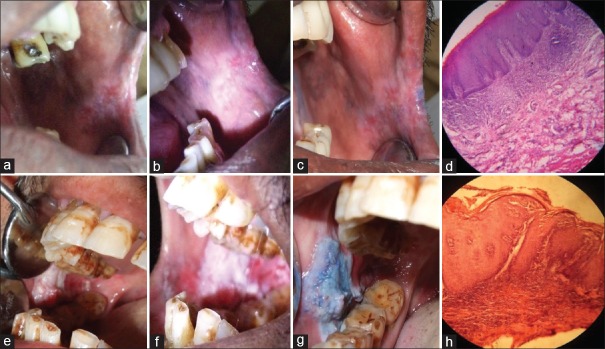
Clinically, leukoplakia was the most common finding with 23 cases (54.8%) either alone or in combination with other oral potentially malignant disorders, followed by oral submucous fibrosis (OSMF) and rest presenting as oral lichen planus, tobacco pouch keratosis, verrucous lesions and oral carcinoma. Chemiluminescence diagnosed 18 dysplasia (90%), 3 carcinomas in situ (100%), 4 (100%) cases of SCC and 2 (100%) cases of verrucous carcinoma to be positive giving true-positive results [Table 1 and Figure 1]. Toluidine blue diagnosed 10 dysplasia (50%), 2 carcinomas in situ (66%), 4 SCCs (100%), 2 verrucous carcinomas (100%) and 1 proliferative verrucous leukoplakia (100%) cases to be positive giving true-positive results [Figure 2]. Few false positive and few false negative were also seen [Figures 3 and 4]. Toluidine blue provided positive findings in 21 (50%) cases whereas chemiluminescence provided positive findings in 33 (78.6%) cases (P = 0.006).
Table 1.
Correlation between toluidine blue/chemiluminescence positivity and histopathological findings
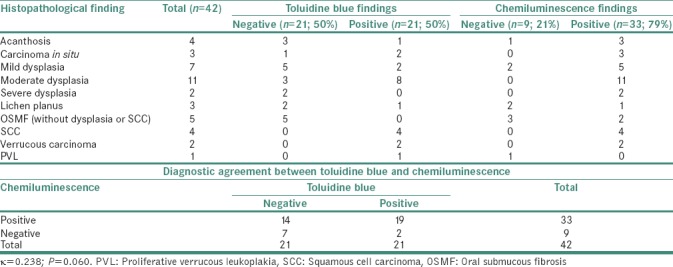
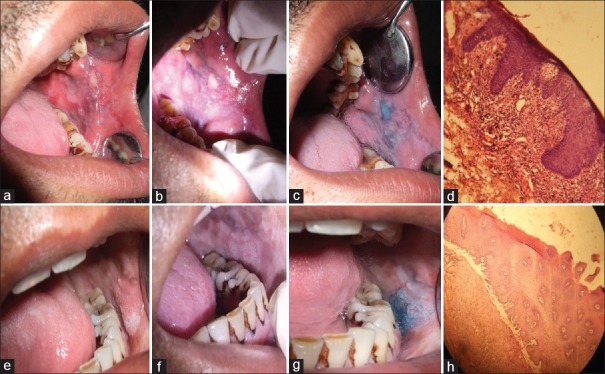
Figure 1.

Use of Vizilite as an oral cancer screening method. (a) Activating Vizilite capsule by flexing it, (b) examination of the patient's oral cavity with Vizilite, (c) application of toluidine blue stain with cotton bud, (d) removal of mechanical retention of dye with 1% acetic acid
Figure 2.
Use of Vizilite and toluidine blue stain as an oral cancer screening method. (a) Clinically identified leukoplakia on left buccal mucosa under conventional visual examination, (b) Vizilite true positive, (c) toluidine blue true positive, (d) histopathologically moderate epithelial dysplasia (H&E, ×10), (e) clinically identified proliferative verrucous leukoplakia on left buccal mucosa under conventional visual examination, (f) Vizilite false negative, (g) toluidine blue true positive, (h) histopathologically proliferative verrucous leukoplakia (H&E, ×10)
Figure 3.
Use of Vizilite and toluidine blue stain as an oral cancer screening method. (a) Clinically identified nonhomogenous leukoplakia on left buccal mucosa under conventional visual examination, (b) Vizilite true positive, (c) toluidine blue false negative, (d) histopathologically mild epithelial dysplasia (H&E, ×10), (e) clinically identified nonhomogenous leukoplakia on left buccal mucosa under conventional visual examination, (f) Vizilite true positive, (g) toluidine blue true positive, (h) histopathologically carcinoma in situ (H&E, ×10)
Figure 4.
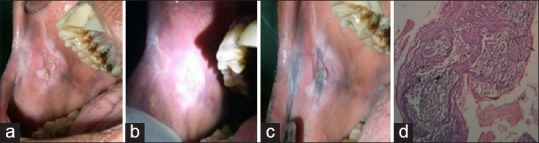
(a) Clinically identified Nonhomogenous leukoplakia on left buccal mucosa under conventional visual examination, (b) Vizilite True Positive, (c) Toluidine blue True positive, (d) Histopathologically Oral squamous cell carcinoma (H&E 10X)
Histopathologically, dysplasia was the most common entity (in different grades) followed by OSMF. The diagnostic efficacy of both the tools was measured in terms of sensitivity, specificity, PPV and negative predictive value. The toluidine blue test was found to be moderately sensitive with a sensitivity of 63.33%; however, the test was highly specific showing a specificity of 83.33%. The PPV of the test was quite high with a PPV of 90.48%; however, the negative predictive value was very low, i.e., 47.62%.
The Vizilite was found to be highly sensitive with a sensitivity of 90%; however, the test has limited specificity of 50%. The PPV of the test was quite high with a PPV of 81.82%; however, the negative predictive value was just moderate, i.e., 66.67%. Diagnostic agreement between toluidine blue and chemiluminescence was low with a κ = 0.238 (P < 0.05) [Table 1].
DISCUSSION
Literature indicates the poor prognosis of patients with oral SCC, despite advances in management strategies with regard to its treatment. Early diagnosis and institution of the treatment remain the key to improved patient survival;[10] hence, the present study attempts to illustrate the efficacy of toluidine blue and chemiluminescence in diagnosing oral potentially malignant disorders and oral cancer.
Toluidine blue is a cationic metachromatic dye that stains deoxyribonucleic acid and/or may be retained in intracellular spaces of dysplastic epithelium and clinically may appear as royal blue areas.[11] Theoretically, dysplastic and malignant cells have higher nucleic acid content than normal, and thus, staining of suspicious lesions with this dye can aid recognition of mucosal changes.[12] It is one of the most accepted screening tools used since a long time and has even been suggested as an alternative to frozen sections in developing countries.[13,14] The usefulness and reliability of toluidine blue dye which binds to malignant or dysplastic tissues have been demonstrated in many studies.[15,16,17,18,19,20,21,13,14]
In the present study, toluidine blue stained only 50% of dysplasia positive though serious pathologies such as SCC and verrucous carcinoma cases were 100% positive, showing a sensitivity of 63.33% and a specificity of 83.33%, which is consistent with previous findings of Lingen et al. in 2008.[22] In contrast, various investigators have reported higher sensitivity (95%–88.23%) and lower specificity (76.9%–42.4%).[11,12,13,14,15,16,17,18,19,20,21,22,23,24,25] In the present study, care was taken to eliminate the mechanical retention of the dye, which was responsible for false-positive results in most of the studies and which may account for the higher sensitivity for carcinoma cases.[18,19] Missmann et al.[15] and Miller et al.[16] stated that the plausible reason for giving high sensitivity and specificity for malignant lesions and not premalignant lesions could be that toluidine blue appears to stain only 3–4 cell layers deep. Therefore, early invasive SCCs that might be surfaced by intact epithelium, keratinization and not exposed to the oral environment do not take up the stain. The results of our study showed that diagnostic agreement between toluidine blue and histopathology was low although statistically it was a significant association (P < 0.05), which is in agreement with Upadhyay et al.'s observations regarding the questionable reliability of toluidine blue staining due to this high false-positive and false-negative results.[26] Güneri et al. also indicated the confusion regarding the blue color perception in the oral lesions;[27] hence, the low degree of observer agreement deters the use of toluidine blue as a substitute for histopathology as has been seen in other studies.[5,9,16,18]
Chemiluminescence (Vizilite) is the other screening test used in the study which has been approved for use in the United States by the Food and Drug Administration since November 2001. Normal epithelium will absorb chemiluminescent light and appear dark, whereas hyperkeratinized or dysplastic lesions appear white. The difference in color could be related to altered epithelial thickness or to the higher density of nuclear content and mitochondrial matrix that preferentially reflects light in the pathological tissues.[12] Most of the studies have shown that chemiluminescence increases the brightness and margins of oral mucosal white lesions and thus assists in identification of mucosal lesions not considered under conventional visual examination.[28,29,30]
The present study reveals Vizilite to be highly sensitive (90%) with a limited specificity (50%). The PPV of the test was quite high with a value of 81.82%; however, the negative predictive value was just moderate i.e., 66.67%. Two case–control studies suggested varied opinion regarding accuracy of Vizilite ranging from 18.2% to 80.6%.[31,19] However, both studies reported sensitivity to be 100% and specificity as low as 0% and 14.2%. Vashisht et al. reported sensitivity and specificity of Vizilite to be 95.45% and 84.6%, respectively,[20] whereas Awan et al. reported it to be as 77.3% and 27.8%, respectively.[30] The results of the present study are consistent with systematic reviews done by Giovannacci et al. and Nagi et al., who reported sensitivity of Vizilite ranging from 77.1% to 100% and specificity ranging from 0% to 27.8%.[32,33]
In the present study, the diagnostic agreement between chemiluminescence (Vizilite) and histopathology was average with a Kappa value of 0.432, although statistically it was a significant association (P = 0.006) yet lack of above average agreement prohibited the use of chemiluminescence as a substitute for histopathology. We further observed that the technique is painless, is easy to learn and may help in identifying suspicious lesions missed during visual inspection under incandescent overhead and halogen dental illumination.
One of the drawbacks of the test is, its per patient cost according to socioeconomic status of the country is very high and kit can be used only once per patient. Several benign oral lesions (leukoedema, frictional irritation, lichenoid mucositis) are readily recognized because of their clinical appearance and may be misinterpreted as positive. This may be because the epithelium in these lesions shows hyperkeratinization and/or chronic inflammatory infiltrate, which reflect the chemiluminescent light, more strongly than normal tissue. This was also reiterated by Farah et al., who indicated that Vizilite illumination does not discriminate between keratotic, inflammatory, malignant or potentially malignant oral mucosal white lesions, and thus, a high index of suspicion, expert clinical judgment and scalpel biopsy are still essential for proper patient care.[31]
It is also emphasized that large-scale studies are required to further refine issues related to the selectivity and specificity of the test in correlation with the clinical, cytological and histological features of oral epithelial lesions. In the present study, it was observed that Vizilite is helpful in delineating the borders of the lesions which could be easily missed by conventional visual examination. Few of satellite lesions were also detected which were not recognized on conventional visual examination consistent with the literature.[34,19]
Diagnostic agreement between toluidine blue and chemiluminescence (Vizilite) was very low with a κ = 0.238 (P = 0.060), thus showing that both the tests behaved differently. Sensitivity of Vizilite was greater than toluidine blue in the present study, indicating that it is a more effective test for screening oral cancer, as was equivocal with the finding of Ram and Siar.[19] However, Mehrotra et al. suggested that VELscope was found to have a higher sensitivity when compared with Vizilite.[35]
Although toluidine blue showed varied results, it was 100% positive for all malignant lesions, and thus, we hypothesize that it can help accelerate the decision to perform a biopsy and assist in the selection of the most suspicious site. Further, this technique is simple, noninvasive and cheap. We also agree with the findings of Epstein et al. that chemiluminescence (Vizilite) helps in delineating border of the lesions that extended beyond the clinical borders,[36] but its per patient cost is high. Thus, both the tests hold their importance as screening devices and can be used in cancer screening procedures.
CONCLUSIONS
The present study provides evidence that chemiluminescence is more sensitive in detecting suspicious lesion by enhancing the clinical examination, but it has certain limitations, prohibiting its use in making final diagnosis of the lesions. Toluidine blue gave variable results but was 100% sensitive in detecting malignant lesions, so it might help in the detection of most suspicious site in the lesion for biopsy. To definitively identify the sensitivity and specificity of toluidine blue in detecting such lesions, further studies with more samples are required. Histopathology remains the gold standard for confirmatory diagnosis, whereas both the tests can be used as an adjunct to conventional visual examination.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Park's Textbook of Preventive and Social Medicine. 21st ed. [Last accessed on 2014 Aug 20]. Goodreads. Available from: https://www.goodreads.com/work/best_book/22273649-park-s-textbook-of-preventive-and-socialmedicine-21-edition .
- 2.Johnson N. Tobacco use and oral cancer: A global perspective. J Dent Educ. 2001;65:328–39. [PubMed] [Google Scholar]
- 3.Downer MC, Evans AW, Hughes Hallet CM, Jullien JA, Speight PM, Zakrzewska JM, et al. Evaluation of screening for oral cancer and precancer in a company headquarters. Community Dent Oral Epidemiol. 1995;23:84–8. doi: 10.1111/j.1600-0528.1995.tb00206.x. [DOI] [PubMed] [Google Scholar]
- 4.Neville BW, Day TA. Oral cancer and precancerous lesions. CA Cancer J Clin. 2002;52:195–215. doi: 10.3322/canjclin.52.4.195. [DOI] [PubMed] [Google Scholar]
- 5.Kujan O, Glenny AM, Duxbury J, Thakker N, Sloan P. Evaluation of screening strategies for improving oral cancer mortality: A Cochrane systematic review. J Dent Educ. 2005;69:255–65. [PubMed] [Google Scholar]
- 6.Epstein JB, Gorsky M, Cabay RJ, Day T, Gonsalves W. Screening for and diagnosis of oral premalignant lesions and oropharyngeal squamous cell carcinoma: Role of primary care physicians. Can Fam Physician. 2008;54:870–5. [PMC free article] [PubMed] [Google Scholar]
- 7.Sargeran K, Murtomaa H, Safavi SM, Vehkalahti MM, Teronen O. Survival after diagnosis of cancer of the oral cavity. Br J Oral Maxillofac Surg. 2008;46:187–91. doi: 10.1016/j.bjoms.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 8.Canto MT, Horowitz AM, Child WL. Views of oral cancer prevention and early detection: Maryland physicians. Oral Oncol. 2002;38:373–7. doi: 10.1016/s1368-8375(01)00074-4. [DOI] [PubMed] [Google Scholar]
- 9.Hedge MC, Kamath PM, Shreedharan S, Dannana NK, Raju RM. Supravital staining: It's role in detecting early malignancies. Indian J Otolaryngol Head Neck Surg. 2006;58:31–4. doi: 10.1007/BF02907735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehrotra R, Gupta DK. Exciting new advances in oral cancer diagnosis: Avenues to early detection. Head Neck Oncol. 2011;3:33. doi: 10.1186/1758-3284-3-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pallagatti S, Sheikh S, Aggarwal A, Gupta D, Singh R, Handa R, et al. Toluidine blue staining as an adjunctive tool for early diagnosis of dysplastic changes in the oral mucosa. J Clin Exp Dent. 2013;5:e187–91. doi: 10.4317/jced.51121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Messadi DV. Diagnostic aids for detection of oral precancerous conditions. Int J Oral Sci. 2013;5:59–65. doi: 10.1038/ijos.2013.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Junaid M, Suhail A, Umer B, Nawaz A, Ikram M, Sobani ZU, et al. Toluidine blue: Yet another low cost method for screening oral cavity tumour margins in third world countries. J Pak Med Assoc. 2013;63:835–7. [PubMed] [Google Scholar]
- 14.Junaid M, Choudhary MM, Sobani ZA, Murtaza G, Qadeer S, Ali NS, et al. A comparative analysis of toluidine blue with frozen section in oral squamous cell carcinoma. World J Surg Oncol. 2012;10:57. doi: 10.1186/1477-7819-10-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Missmann M, Jank S, Laimer K, Gassner R. A reason for the use of toluidine blue staining in the presurgical management of patients with oral squamous cell carcinomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:741–3. doi: 10.1016/j.tripleo.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 16.Miller RL, Simms BW, Gould AR. Toluidine blue staining for detection of oral premalignant lesions and carcinomas. J Oral Pathol. 1988;17:73–8. doi: 10.1111/j.1600-0714.1988.tb01510.x. [DOI] [PubMed] [Google Scholar]
- 17.Patton LL. The effectiveness of community-based visual screening and utility of adjunctive diagnostic aids in the early detection of oral cancer. Oral Oncol. 2003;39:708–23. doi: 10.1016/s1368-8375(03)00083-6. [DOI] [PubMed] [Google Scholar]
- 18.Onofre MA, Sposto MR, Navarro CM. Reliability of toluidine blue application in the detection of oral epithelial dysplasia and in situ and invasive squamous cell carcinomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:535–40. doi: 10.1067/moe.2001.112949. [DOI] [PubMed] [Google Scholar]
- 19.Ram S, Siar CH. Chemiluminescence as a diagnostic aid in the detection of oral cancer and potentially malignant epithelial lesions. Int J Oral Maxillofac Surg. 2005;34:521–7. doi: 10.1016/j.ijom.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 20.Vashisht N, Ravikiran A, Samatha Y, Rao PC, Naik R, Vashisht D, et al. Chemiluminescence and toluidine blue as diagnostic tools for detecting early stages of oral cancer: An in vivo study. J Clin Diagn Res. 2014;8:ZC35–8. doi: 10.7860/JCDR/2014/7746.4259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chaudhry A, Manjunath M, Ashwatappa D, Krishna S, Krishna AG. Comparison of chemiluminescence and toluidine blue in the diagnosis of dysplasia in leukoplakia: A cross-sectional study. J Investig Clin Dent. 2016;7:132–40. doi: 10.1111/jicd.12141. [DOI] [PubMed] [Google Scholar]
- 22.Lingen MW, Kalmar JR, Karrison T, Speight PM. Critical evaluation of diagnostic aids for the detection of oral cancer. Oral Oncol. 2008;44:10–22. doi: 10.1016/j.oraloncology.2007.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Epstein JB, Feldman R, Dolor RJ, Porter SR. The utility of tolonium chloride rinse in the diagnosis of recurrent or second primary cancers in patients with prior upper aerodigestive tract cancer. Head Neck. 2003;25:911–21. doi: 10.1002/hed.10309. [DOI] [PubMed] [Google Scholar]
- 24.Allegra E, Lombardo N, Puzzo L, Garozzo A. The usefulness of toluidine staining as a diagnostic tool for precancerous and cancerous oropharyngeal and oral cavity lesions. Acta Otorhinolaryngol Ital. 2009;29:187–90. [PMC free article] [PubMed] [Google Scholar]
- 25.Chainani-Wu N, Madden E, Cox D, Sroussi H, Epstein J, Silverman S, Jr, et al. Toluidine blue aids in detection of dysplasia and carcinoma in suspicious oral lesions. Oral Dis. 2015;21:879–85. doi: 10.1111/odi.12358. [DOI] [PubMed] [Google Scholar]
- 26.Upadhyay J, Rao NN, Upadhyay RB, Agarwal P. Reliability of toluidine blue vital staining in detection of potentially malignant oral lesions – Time to reconsider. Asian Pac J Cancer Prev. 2011;12:1757–60. [PubMed] [Google Scholar]
- 27.Güneri P, Epstein JB, Ergün S, Boyacioğlu H. Toluidine blue color perception in identification of oral mucosal lesions. Clin Oral Investig. 2011;15:337–45. doi: 10.1007/s00784-010-0398-6. [DOI] [PubMed] [Google Scholar]
- 28.Scully C, Ward-Booth RP. Detection and treatment of early cancers of the oral cavity. Crit Rev Oncol Hematol. 1995;21:63–75. doi: 10.1016/1040-8428(94)00165-0. [DOI] [PubMed] [Google Scholar]
- 29.Huber MA, Bsoul SA, Terezhalmy GT. Acetic acid wash and chemiluminescent illumination as an adjunct to conventional oral soft tissue examination for the detection of dysplasia: A pilot study. Quintessence Int. 2004;35:378–84. [PubMed] [Google Scholar]
- 30.Awan KH, Morgan PR, Warnakulasuriya S. Utility of chemiluminescence (ViziLite™) in the detection of oral potentially malignant disorders and benign keratoses. J Oral Pathol Med. 2011;40:541–4. doi: 10.1111/j.1600-0714.2011.01048.x. [DOI] [PubMed] [Google Scholar]
- 31.Farah CS, McCullough MJ. A pilot case control study on the efficacy of acetic acid wash and chemiluminescent illumination (ViziLite) in the visualisation of oral mucosal white lesions. Oral Oncol. 2007;43:820–4. doi: 10.1016/j.oraloncology.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 32.Giovannacci I, Vescovi P, Manfredi M, Meleti M. Non-invasive visual tools for diagnosis of oral cancer and dysplasia: A systematic review. Med Oral Patol Oral Cir Bucal. 2016;21:e305–15. doi: 10.4317/medoral.20996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nagi R, Reddy-Kantharaj YB, Rakesh N, Janardhan-Reddy S, Sahu S. Efficacy of light based detection systems for early detection of oral cancer and oral potentially malignant disorders: Systematic review. Med Oral Patol Oral Cir Bucal. 2016;21:e447–55. doi: 10.4317/medoral.21104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.British Columbia Oral Cancer Prevention Program, BC Cancer Agency, College of Dental Surgeons of British Columbia. Guideline for the early detection of oral cancer in British Columbia 2008. J Can Dent Assoc. 2008;74:245. [PubMed] [Google Scholar]
- 35.Mehrotra R, Singh M, Thomas S, Nair P, Pandya S, Nigam NS, et al. A cross-sectional study evaluating chemiluminescence and autofluorescence in the detection of clinically innocuous precancerous and cancerous oral lesions. J Am Dent Assoc. 2010;141:151–6. doi: 10.14219/jada.archive.2010.0132. [DOI] [PubMed] [Google Scholar]
- 36.Epstein JB, Silverman S, Jr, Epstein JD, Lonky SA, Bride MA. Analysis of oral lesion biopsies identified and evaluated by visual examination, chemiluminescence and toluidine blue. Oral Oncol. 2008;44:538–44. doi: 10.1016/j.oraloncology.2007.08.011. [DOI] [PubMed] [Google Scholar]