Abstract
Introduction:
Dental diseases are universal in nature. Their presence and severity may vary from one individual to another and is also affected by multiple factors such as gender, knowledge, attitude and the affordability of dental/oral care. Gay, bisexual and transgender community is one among the socially disadvantaged community in our country. The present study was carried out in the city of Pune, India, to evaluate the prevalence of dentition status and the treatment needs among the men who have sex with men (MSMs) and transgenders (TGs) and its correlation with the oral health-related quality of life.
Materials and Methods:
The sample size was 270. Convenience sampling was followed. The WHO oral health assessment for 1997 was used to record dentition status and treatment needs. Oral Health Impact Profile-14 was used to record the oral health-related quality of life. SPSS 22.0 (Chicago, IL, USA) was used for statistical analysis. All P < 0.05 were considered to be statistically significant.
Results:
There was no statistically significant difference seen across the various domains in the overall impact of the oral quality of life. There was a significant correlation between the decayed teeth, missing teeth and overall decayed, missing and filled teeth scores with respect to the seven domains. Problems arising due to past dental experience (dental caries), lost natural tooth structures replaced with restorative material and a cumulative impact significantly affected the outcome of the oral health-related quality of life of the participants.
Conclusion:
There was an alteration in quality of life of the MSMs and TGS with respect to dental caries. This calls for an intervention that is tailor-made to meet the needs of this group.
Keywords: Dental caries, dentition status, men who have sex with men, transgender, treatment needs
INTRODUCTION
Dental diseases are universal in nature. Their presence and severity may vary from one individual to another and is also affected by multiple factors such as gender, knowledge, attitude and the affordability to dental/oral care. Neglect of oral diseases can largely lead to loss of tooth and also negatively affect the quality of life led by the person due to inability to chew, speak and also unpleasant esthetics.[1] In India, dental services are provided by both public and private sector, yet due to brain drain and improper distribution of health-care workers, oral health is still at the back foot.[2] According to Chandrima and Gunjan, the third genders, especially the hijras, in India are a vulnerable lot, who are not always recipient of the available health-care resources.[3] Gay, bisexual and transgender community is one among the socially disadvantaged community in our country. Social stigma associated with these communities largely affects their access to oral health care and hence special attention is needed to improve their oral health.[4] A study in Pakistan reported that stigma associated with such communities affects their access to oral health care adversely.[5] In general, the attitude toward gay, bisexual and transgender community in Indian society is discriminatory and biased. Violence against these communities is very common and they are most vulnerable.[6] It hinders these people from seeking health care. There is also a greater chance for them in indulging into various forms of addictions such as tobacco, alcohol and other forms of substance abuse[6] that severely affects not only their general health but also their oral health. These groups indulge in unsafe oral sex and also in peer influenced harmful activities that could debilitate their health status.
According to the Joint United Nations Programme on HIV and AIDS, the prevalence of HIV infection among MSM in capital cities from nearly 80 countries is on average 13 times higher than that of general populations in these countries.[7] With such life-threatening conditions prevalent among them, dental neglect is an expected outcome. Like this, most of the data related to this special group, national and international data focus largely only on the general health disparities and oral health hardly finds a mention. Hence, there is a need for a baseline data among these groups of people, for planning public health interventions and for helping them to achieve optimum oral health standards. The present study was carried out in the city of Pune, India, to evaluate the prevalence of dentition status and the treatment needs among the men who have sex with men (MSMs) and transgenders (TGs) and its correlation with the oral health-related quality of life.
Materials and Methods
Ethical clearance for the study was obtained from the Ethics Committee of Samapathik Trust (a non-governmental organization [NGO] working in the field of health and support for the lesbian, gay, bisexual, transgender (LGBT) groups), Budhwar Peth, Pune. The NGO activities cover the entire city of Pune and nearby areas. Initially, a pilot study was carried out among 30 participants. Based on the prevalence of dental caries, the final sample size was calculated to be 270. All the MSMs and TGs registered with the NGO for health and rehabilitative purposes that were ready to provide a written informed consent were included in the study. Convenience sampling technique was followed to achieve the desired sample size. The oral health-related quality of life questionnaire (Oral Health Impact Profile-14 (OHIP-14))[8] was translated into Hindi and validated and used to record the oral health-related quality of life. The dentition status and treatment needs of the participants were recorded using the WHO oral health assessment form of 1997.[9] Community periodontal index probe and mouth mirror were used. All norms of sterilization and disinfection were followed meticulously. Not more than thirty participants were examined per day. Type III examination was carried out during the field work where these people report for blood testing and condom distribution at weekly basis. No incentives in any kind were provided to the participants. Those with oral problems were provided with oral health education and referral to the nearby teaching institutions to seek appropriate dental treatment. The data collected were entered in Microsoft Excel 2013 and cleaned. SPSS 22.0 (IBM Analytics, New York, Chicago, USA) was used to carry out the statistical analysis. Chi-square test was performed to see for any association among the quality of life and decayed, missing and filled teeth (DMFT) index. All P < 0.05 were considered to be statistically significant.
RESULTS
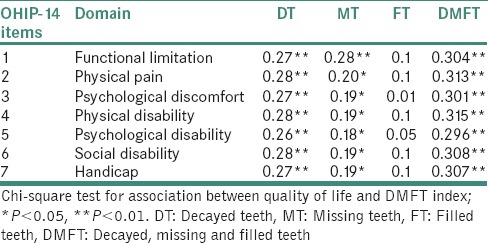
Overall 270 MSMs and TGs participated in the study, of which 241 (89.3%) were MSMs and 29 (10.7%) were TGs. Maximum participants were from the younger age group between 18 and 24 years [Table 1]. The DMFT index was calculated based on the findings of the dentition status. The total decayed teeth (DT) score was 1262, missing teeth (MT) score was 72, filled teeth (FT) score was 38 and the overall DMFT score was 1372. About 188 (69.6%) out of 270 had dental caries, 40 (14.8%) out of 270 had teeth and only 9 (3.3%) had some form of restoration. Table 2 shows the mean of DT, MT, FT and DMFT among the study participants. Out of the 270, only 80 (29.6%) had ever been to a dentist due to some problem. The others avoided going for a dental treatment out of fear, lack of awareness or due to economic constraints. About 114 (42.2%) currently had some form of dental problem but did not prefer to consult a dentist for the same. The maximum requirement of treatment for the participants was in the form of one surface filling followed by pulp care and restoration [Table 3]. Maximum prevalence with respect to the OHIP domains was of psychological discomfort (tense), and 36.3% felt that their life was less satisfying after the dental problems set in [Table 4]. There was no statistically significant difference seen across the various domains in the overall impact of the oral quality of life. There was a significant correlation between the DT, MT and overall DMFT scores with respect to the seven domains. Problems arising due to past dental experience (dental caries), lost natural tooth structures replaced with restorative material and a cumulative impact significantly affected the outcome of the oral health-related quality of life of the participants [Table 5].
Table 1.
Demographic distribution of the participants
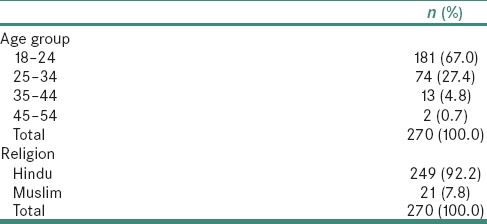
Table 2.
Mean of the decayed, missing and filled scores of the participants
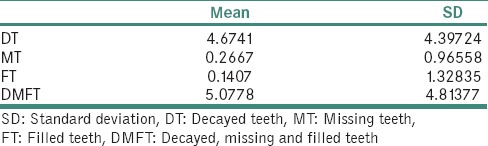
Table 3.
Distribution of the participants based on the type of treatment required
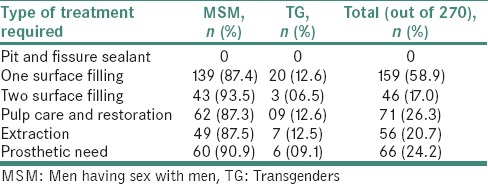
Table 4.
Reported impacts of oral dental problems on the quality of life
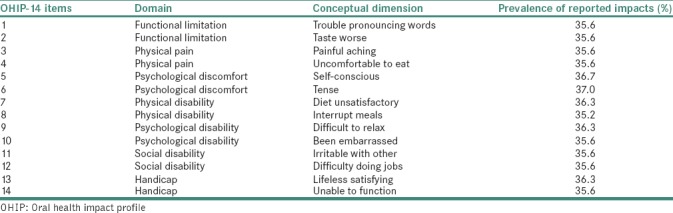
Table 5.
Association between the parameters of oral health impact profile - 14 and decayed, missing and filled teeth index
DISCUSSION
The study is the first of its kind to highlight a pressing problem in relation to the effect of the dental problems over the quality of life of the MSMs and transgender population. A large part of the study population had DT which needed treatment. A quarter of the community required pulp care and restoration. Since no Indian data are available, a direct comparison cannot be made. Dental caries untreated over a period, surely leads to loss of tooth and inhibits the functioning capacity related to mastication and also esthetics. Social inequalities are a major hurdle toward self-perceived oral health behavior.[10] Overall, we observed that all the domains of the quality of life were affected in this population due to the existing dental problem. In the present study, almost a quarter of the study population needed prosthetic treatment in one form or the other, which was higher than the findings of another study in India (51.5%).[11] The reason for this great difference in prosthetic needs may be due to the reason that our majority of the study population were in the elderly age group in their study. Of the 291 conditions studied between 1990 and 2010 in the Global Burden of Disease Study, it was found that oral diseases were highly prevalent affecting 3.9 billion people worldwide.[12] Untreated caries in permanent teeth was the most prevalent condition (affecting 35% of population), whereas severe tooth loss was the 36th most prevalent condition (affecting 2% of the global population).[12] The prevalence of untreated dental caries in the present study population was nearly twice that of the global findings. With comparison to the general population, the last survey in India (2002–2003) reported that among adults, the dental caries prevalence was 77.6%. This is slightly higher than our study findings.[13] According to Hongal et al, a\the attitudes of the community towards special groups like the eunuchs, have been reflected even in the health care settings.[11] Most of the health-care facilities are concentrated only with respect to HIV or other sexually transmitted diseases and oral health takes a back seat.
It is a proven fact that oral diseases greatly affect the quality of life. In the present study population, there was a strong association between pain, discomfort, stress, irritability and functional disability with the decayed and the missing component of DMFT index. Since no previous study has been reported among this special group, a direct comparison cannot be made. The impact of dental caries and tooth loss proves the urgent need to encompass dental health also in the overall needs of this population and not be limited to only sexual health. The MSMs and TGs are known for performing oral sex. The orogenital contacts increase the risk of a lot of microbes and alter the oral hygiene to a great extent which coupled with lack of oral health knowledge and adequate oral hygiene can further deteriorate the existing disease state. The details of oral sex and its implications with respect to oral health were not covered during our survey. Most of the participants were not comfortable to answer questions related to unsafe oral sex practices and hence that data could not be covered. Nevertheless, further studies need to focus on this parameter for understanding the prevalence of diseases and possible oral infections that may arise as a challenge among these people.
The study has certain limitations. We used convenience sampling, though not strictly. A door-to-door survey of this group is impossible since most of them do not reveal their sexual orientations easily. Only those who were registered with the community-based organization, Samapathik Trust, were covered. We did not get permission from other organizations working for this group, so a lot more MSMs and TGs were left out; hence, the population is not necessarily representative sample. Although referral for cases that needed treatment to the nearest government hospital was provided and oral health education and awareness was carried out, the impact of the same could not be followed up. Further studies are essential to reveal the impact of the interventions on oral health status and also the quality of life. Stigma and discrimination is an essential factor in these people failing to seek treatments for any form of health-related issues. This holds true, especially for the TGs who are not a welcome face everywhere. Hence, special clinics or outlets need to be set up to cater to the needs of these people. It is also necessary to have a sensitization among upcoming dentists so that it is easy for them to be mentally prepared to handle these patients.
CONCLUSION
The present study highlighted the high prevalence of dental problems among the MSMs and TGs. There is a definite association between dental caries and tooth loss with the oral health-related quality of life. There was an alteration in quality of life of the MSMs and TGS with respect to dental caries. This calls for an intervention that is tailor-made to meet the needs of this group. Health education should look beyond sexually transmitted infections and also encompass oral health for such vulnerable populations.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank the staff of Samapathik Trust for their valuable time and assistance during the course of the study.
REFERENCES
- 1.Sussex PV. Edentulism from a New Zealand perspective – A review of the literature. N Z Dent J. 2008;104:84–96. [PubMed] [Google Scholar]
- 2.Tandon S. Challenges to the oral health workforce in India. J Dent Educ. 2004;68:28–33. [PubMed] [Google Scholar]
- 3.Chandrima C, Gunjan S. Hijra status in India. In: Chatterjee C, editor. Vulnerable groups in India. 1st ed. Mumbai: Publisher Centre for Enquiry into Health and Allied Themes; 2007. pp. 1–2. [Google Scholar]
- 4.Khan SA, Dawani N, Bilal S. Perceptions and myths regarding oral health care amongst strata of low socio economic community in Karachi, Pakistan. J Pak Med Assoc. 2012;62:1198–203. [PubMed] [Google Scholar]
- 5.Nagarajan M, Srinivasan V, Ranganathan K. Prevalence of loss of teeth among Gay, Bisexuals and Transgenders populations in Karaikal, Puducherry, India. Acta Biomed Sci. 2017;4:82–4. [Google Scholar]
- 6.Hongal S, Torwane NA, Goel P, Byarakele C, Mishra P, Jain S, et al. Oral health-related knowledge, attitude and practices among Eunuchs (hijras) residing in Bhopal city, Madhya Pradesh, India: A cross-sectional questionnaire survey. J Indian Soc Periodontol. 2014;18:624–31. doi: 10.4103/0972-124X.142459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.UNAIDS, HIV/AIDS, Global Report: UNAIDS Report on the Global AIDS Epidemic: 2012. UNAIDS; 2012. [Google Scholar]
- 8.Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–90. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. Oral Health Surveys, Basic Methods. 4th ed. Geneva: World Health Organization; 1997. [Google Scholar]
- 10.Patrick DL, Lee RS, Nucci M, Grembowski D, Jolles CZ, Milgrom P, et al. Reducing oral health disparities: A focus on social and cultural determinants. BMC Oral Health. 2006;6(Suppl 1):S4. doi: 10.1186/1472-6831-6-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hongal S, Torwane N, Chandrashekhar B, Saxena V, Chavan K. An evaluation of dental prosthetic status and prosthetic needs among eunuchs (trans genders) residing in Bhopal city, Madhya Pradesh, India: A cross-sectional study. Ann Med Health Sci Res. 2014;4:943–8. doi: 10.4103/2141-9248.144921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marcenes W, Kassebaum NJ, Bernabé E, Flaxman A, Naghavi M, Lopez A, et al. Global burden of oral conditions in 1990-2010: A systematic analysis. J Dent Res. 2013;92:592–7. doi: 10.1177/0022034513490168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bali RK, Mathur VB, Talwar PP, Chanana HB. National Oral Health Survey and Fluoride Mapping. New Delhi: Dental Council of India; 2002-03. [Google Scholar]


