Abstract
Peripheral ameloblastoma, a soft-tissue analogue of intraosseous ameloblastoma, is a rare odontogenic tumor with histologic characteristics of ameloblastoma. In contrast to conventional ameloblastoma, peripheral ameloblastomas are considered as innocuous lesions which usually do not show invasion of the underlying structures. Rarely, intraosseous ameloblastoma which penetrates the alveolar bone can fuse with the overlying oral epithelium and eventually manifest as an exophytic peripheral lesion. Such lesions which mimic peripheral ameloblastoma both clinically and microscopically are termed as peripheral intraosseous ameloblastoma. As per the existing criteria, soft-tissue ameloblastomas showing bone invasion are strictly excluded from the category of peripheral ameloblastoma and are considered as peripheral intraosseous ameloblastoma. We report a rare case of extraosseous ameloblastoma with clear origin from the superficial epithelium showing the presence of a few odontogenic islands in the underlying bone suggestive of a neoplastic osseous invasion. This paper discusses the diagnostic challenges associated with peripherally occurring ameloblastomas and stresses the need for accurate diagnosis in deciding the treatment modalities.
Keywords: Osseous invasion, peripheral ameloblastoma, peripheral intraosseous ameloblastoma
INTRODUCTION
Ameloblastoma, a tumor of odontogenic epithelial origin, is a true neoplasm of enamel organ-type tissue which does not undergo differentiation to the point of enamel formation.[1] They are usually slow-growing, locally invasive, intraosseous tumors that run a benign course. The extraosseous variant of ameloblastoma, also known as peripheral ameloblastoma, is quite rare and they comprise from 2% to 10% of all ameloblastoma reported.[2] They occur in soft tissues of tooth-bearing area though few cases in extragingival location also had been reported.[3,4] Clinically, the lesion may be mistaken for more common reactive lesions on the gingiva, and the diagnosis is usually made based on their microscopic appearance.
The peripheral ameloblastomas are found to be less aggressive and do not usually invade the underlying bone. These lesions are considered to be relatively innocuous in behavior as it lacks the persistent invasiveness of the intraosseous ameloblastoma.[2] More conservative management had been suggested as the treatment of choice, and most of the cases at present are managed by the surgical excision of tumor tissue without any osseous resection. Peripheral intraosseous ameloblastoma, on the other hand, represents a rare occurrence of intraosseous ameloblastoma which penetrates the alveolar bone, fuses with the overlying oral epithelium and eventually presents as an exophytic peripheral lesion. As these lesions are more aggressive in their behavior, extensive osseous resection of the involved bone has to be done to prevent any recurrence. The aim of this article is to present a rare case of peripheral ameloblastoma with clear origin from the gingival epithelium. Since there was an osseous invasion in this case, the importance of careful evaluation of tumor margins and the need for marginal mandibulectomy, if required, in the management of peripheral ameloblastoma is also stressed.
CASE REPORT
A 33-year-old male patient presented with the complaint of an asymptomatic growth of 5-month duration on the lingual gingiva in the left lower premolar region. On intraoral examination, an exophytic, sessile, oval-shaped mass measuring 2 cm × 1 cm was noticed in the lingual gingiva in relation to 33 and 34 [Figure 1]. The lesion was normal in color with white papillary projections on the surface. On palpation, it was firm in consistency, was slightly tender and fixed to the underlying tissue. The intraoral periapical radiograph of the region showed cupping resorption of the bone [Figure 2]. Based on the clinical presentation of a soft-tissue lesion on the gingiva with numerous papillary projections on the surface, a provisional diagnosis of papilloma was given. Pyogenic granuloma, peripheral giant cell granuloma, peripheral ossifying fibroma and peripheral odontogenic neoplasms were considered as differential diagnosis. Excisional biopsy was done, and the tissue was sent for histopathological examination.
Figure 1.
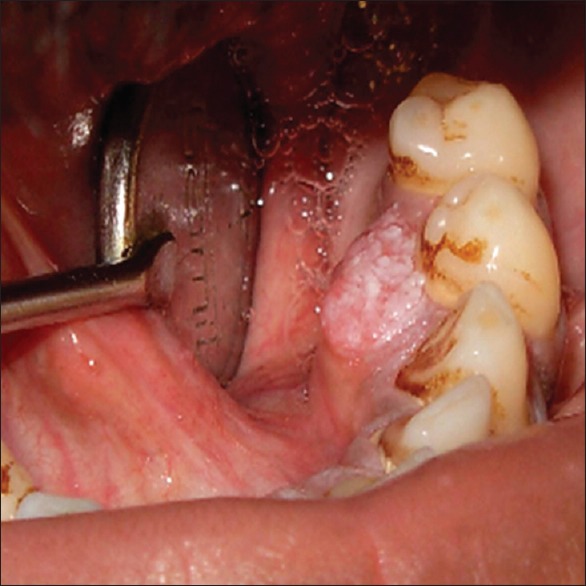
An exophytic sessile mass with papillary surface seen on the lingual gingiva in relation to the teeth, 33 and 34
Figure 2.

Intraoral periapical radiograph of the region showing cupping resorption of the bone
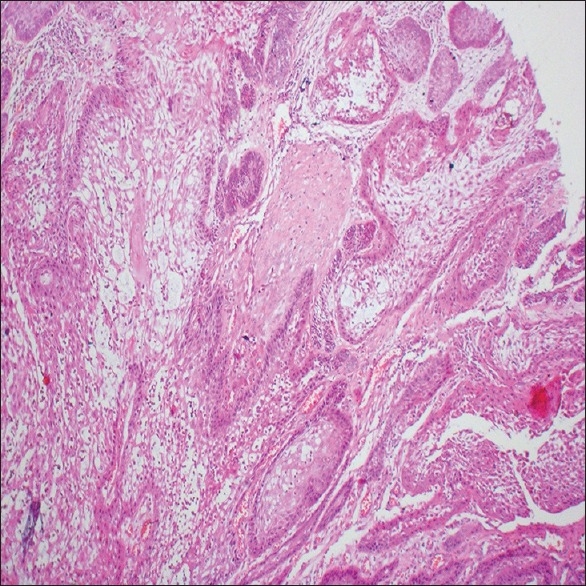
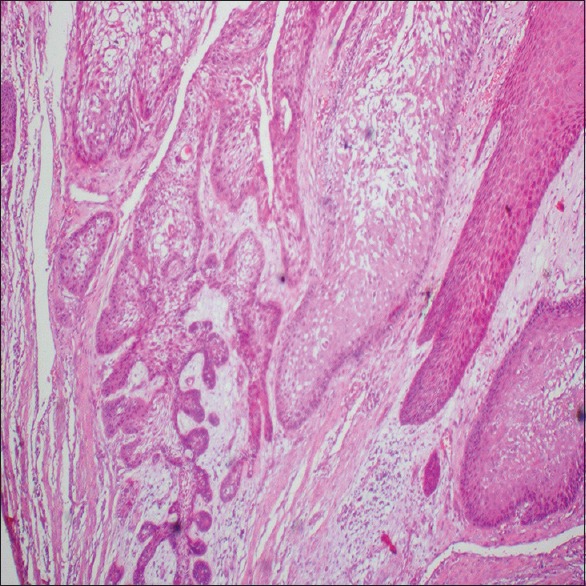
Microscopically, the lesional tissue showed a superficial hyperplastic stratified squamous epithelium with numerous papillary projections. At multiple areas, the epithelium showed ameloblastomatous change [Figure 3]. The proliferation of transformed epithelium with odontogenic islands budding off into the underlying connective tissue stroma [Figure 4] was noticed. Within the connective tissue stroma, there were numerous ameloblastomatous islands lined peripherally by tall columnar cells showing reversal of polarity and central stellate reticulum-like cells [Figure 5]. Some of these islands showed acanthomatous change [Figure 6]. The superficial epithelium showed positivity for the odontogenic marker, cytokeratin-19 (CK-19), confirming its odontogenic transformation [Figure 7]. The ameloblastomatous islands in the connective tissue stroma were also positive for the marker, CK-19 [Figure 8]. Based on the clinical and histopathological presentation, the lesion was diagnosed as peripheral ameloblastoma. Since saucerization of the bone, adjacent to the tumor, was noticed, marginal osteotomy was carried out to evaluate any bone involvement. Multiple sections from the decalcified peripheral bone were studied. A few odontogenic islands were noticed in one of the sections studied [Figures 9 and 10], while all the other sections showed intact cortical bone. Although the presence of tumor islands within the adjacent bone made us consider the possibility of a peripheral intraosseous ameloblastoma, based on the presence of an extraosseous ameloblastomatous lesion showing a clear origin from the superficial epithelium which had undergone odontogenic transformation and the presence of few tumor islands within the adjacent bone suggestive of a neoplastic invasion, the lesion was diagnosed as of peripheral ameloblastoma with neoplastic osseous invasion.
Figure 3.
Papillary superficial epithelium showing ameloblastomatous change (H&E, ×20)
Figure 4.
Odontogenic epithelial islands budding off from the superficial epithelium (H&E, ×20)
Figure 5.
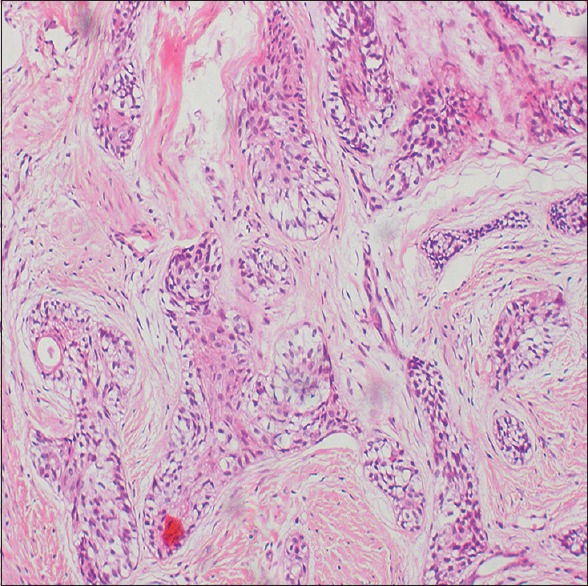
Ameloblastomatous islands in the connective tissue stroma showing peripheral tall columnar cell with reversal of polarity and central cells resembling stellate reticulum (H&E, ×20)
Figure 6.
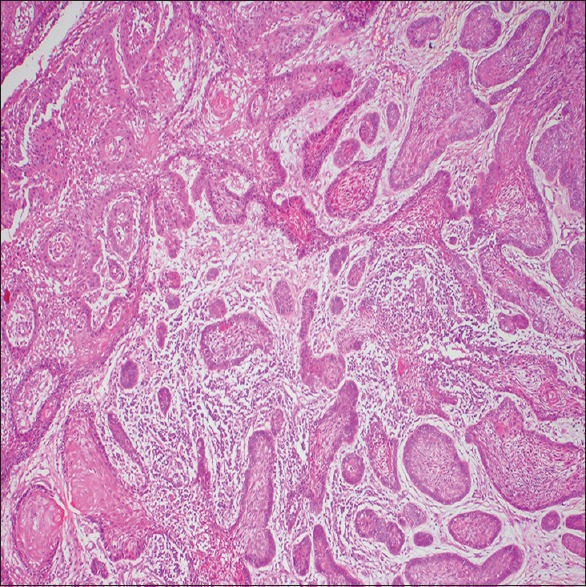
Acanthomatous change in ameloblastomatous epithelial islands (H&E, ×10)
Figure 7.
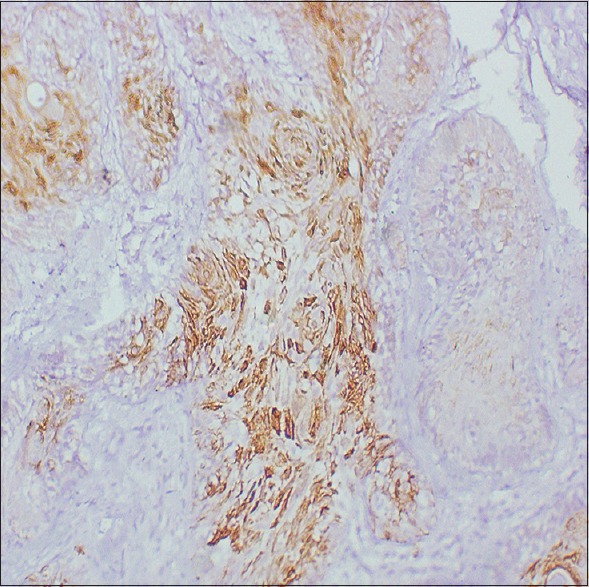
Superficial epithelium showing CK-19 positivity confirming odontogenic transformation (IHC, ×40)
Figure 8.
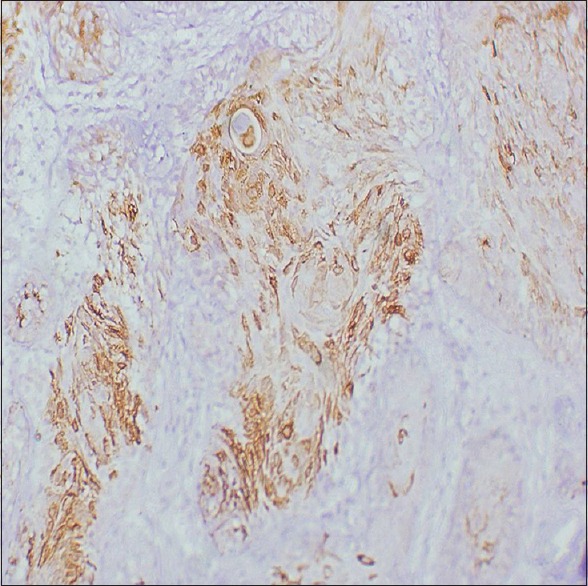
CK-19-positive odontogenic epithelial islands within the connective tissue stroma (IHC, ×40)
Figure 9.
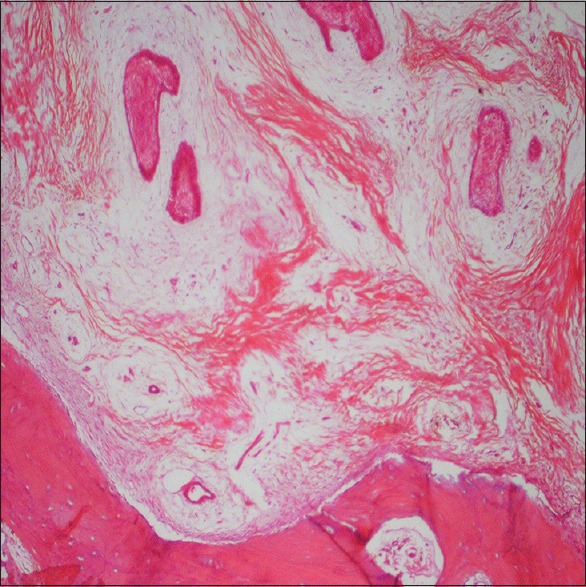
Tumor islands in the adjacent bone suggestive of neoplastic osseous invasion (H&E, ×10)
Figure 10.
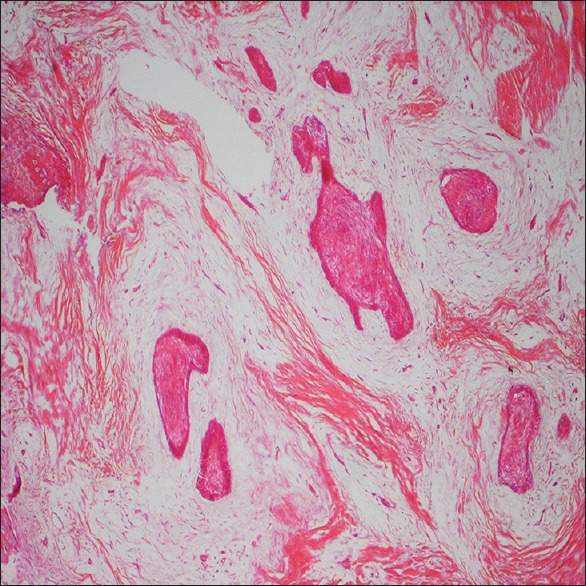
Ameloblastomatous odontogenic epithelial islands within the bone (H&E, ×10)
The healing of the area was uneventful; the patient was on a regular follow-up for a period of 2 years, and there was no recurrence of the lesion.
DISCUSSION
Peripheral ameloblastoma and peripheral intraosseous ameloblastoma are two clinical variants of ameloblastoma which present as an exophytic soft-tissue lesion, often posing a diagnostic challenge. Although these two lesions exhibit similar clinicopathological features, the difference in their biological behavior and management options makes their diagnostic distinction mandatory. Peripheral ameloblastoma was established as a distinct entity after the documentation of a tumor in soft tissue on the lingual surface of the premolar-molar region of the mandible with acceptable illustrative evidence by Stanley and Krogh.[5] The latest update on the WHO classification of odontogenic tumors retains the previous status of peripheral ameloblastoma as a separate subtype of ameloblastoma.[6] The controversy regarding their histogenesis still remains unsettled, and evidence favoring the rests of the dental lamina as well as the basal cells of the surface epithelium as the potential cellular sources of their origin had been discussed in the literature. The diagnostic criteria of peripheral ameloblastoma include the origin from the overlying epithelium, presence of odontogenic epithelium islands in the lesion and lack of potential to bone infiltration.[7] The term peripheral intraosseous ameloblastoma was introduced to differentiate peripheral ameloblastoma from intraosseous ameloblastoma arising from the marginal alveolar bone which perforates the bone and presents clinically as a peripheral mass. The presence of osseous invasion in lesions, which otherwise shows the features of peripheral ameloblastoma histopathologically, is said to be diagnostic of peripheral intraosseous ameloblastoma, and the presence or absence of ameloblastomatous islands within the adjacent bone had been used as a criterion to differentiate between these two lesions.[8]
The case discussed here presented as an exophytic papillary mass in the canine–premolar region of mandibular lingual gingiva, which is the most common site of involvement of peripheral ameloblastoma. Furthermore, microscopically, the lesion was found to be arising from the superficial epithelium, the odontogenic transformation of which was confirmed immunohistochemically using the odontogenic epithelial marker, CK-19. The lesional tissue showed features of follicular ameloblastoma with acanthomatous change and a marked tendency to show acanthomatous change in peripheral ameloblastoma had been well documented.[2,9] Although the presence of ameloblastomatous islands in the marginal osteotomy specimen corresponding to the cupping resorption seen in the radiograph supports the diagnosis of peripheral intraosseous ameloblastoma as per the existing criteria, the lesion was diagnosed as peripheral ameloblastoma with osseous invasion since a clear origin from the superficial epithelium was evident in this case. Philipsen et al. based on their review of 160 cases concluded that the biologic behavior of the peripheral ameloblastoma is in line with that of a hamartoma or persistent hyperplasia rather than that of a neoplasia,[9] and most of the authors are of the view that peripheral ameloblastoma may not involve the underlying bone.[9,10,11] However, we strongly believe that the osseous involvement cannot be taken as a criterion to substantiate whether the tumor arose from the bone or from the soft tissue above it. A few cases of peripheral ameloblastoma with osseous invasion suggesting the potential of peripheral ameloblastoma to infiltrate the bone had been reported earlier.[12,13,14] It was hypothesized that there exist two clinical types of peripheral ameloblastomas, the nonaggressive hamartomatous and the aggressive neoplastic variants.[15] The case presented here may represent the neoplastic variant with a more aggressive behavior which has the potential to invade the bone. Being an exophytic lesion, most of the cases of peripheral ameloblastomas are diagnosed earlier and excised much before a frank invasion of the underlying bone becomes noticeable and probably that will explain why osseous invasion was not seen in majority of the cases reported. Oral epithelium being considered as one of the sources of origin of intraosseous ameloblastoma;[1,16,17] it is possible that in cases where intraosseous ameloblastoma arises from the superficial epithelium, osseous involvement will be preceded by odontogenic transformation of the superficial epithelium followed by proliferation of odontogenic islands into the underlying connective tissue. Hence, there will be an extraosseous phase during which the tumor islands are seen exclusively within the soft tissue – a phase which may present as peripheral ameloblastoma. Hence, it can be speculated that peripheral ameloblastoma, at least in some cases, can occur as an initial event in the development of conventional intraosseous ameloblastoma stressing the need to deal these lesions with caution. The tumor margins must be carefully evaluated following excision of the lesion, and marginal osteotomy should always be considered if the margins are not found to be free of tumor.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rajendran R. Cyst and tumors of odontogenic origin. In: Rajendran R, Sivapathasundharam B, editors. Shafer's Textbook of Oral Pathology. 6th ed. Noida: Elsevier; 2009. pp. 254–308. [Google Scholar]
- 2.Reichart PA, Philipsen HP. Odontogenic Tumours and Allied Lesions. New Malden: Quintessence Publishing Co Ltd; 2004. pp. 59–67. [Google Scholar]
- 3.Ramnarayan K, Nayak RG, Kavalam AG. Peripheral ameloblastoma. Int J Oral Surg. 1985;14:300–1. doi: 10.1016/s0300-9785(85)80044-2. [DOI] [PubMed] [Google Scholar]
- 4.Isomura ET, Okura M, Ishimoto S, Yamada C, Ono Y, Kishino M, et al. Case report of extragingival peripheral ameloblastoma in buccal mucosa. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:577–9. doi: 10.1016/j.tripleo.2009.06.023. [DOI] [PubMed] [Google Scholar]
- 5.Stanley HR, Jr, Krogh HW. Peripheral ameloblastoma; report of a case. Oral Surg Oral Med Oral Pathol. 1959;12:760–5. doi: 10.1016/0030-4220(59)90124-0. [DOI] [PubMed] [Google Scholar]
- 6.Speight PM, Takata T. New tumour entities in the 4th edition of the world health organization classification of head and neck tumours: Odontogenic and maxillofacial bone tumours. Virchows Arch. 2018;472:331–9. doi: 10.1007/s00428-017-2182-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martelli-Júnior H, Souza LN, Santos LA, Melo-Filho MR, De Paula AM. Peripheral ameloblastoma: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:E31–3. doi: 10.1016/j.tripleo.2004.11.016. [DOI] [PubMed] [Google Scholar]
- 8.Ide F, Mishima K, Yamada H, Kikuchi K, Saito I, Kusama K, et al. Intraosseous ameloblastoma with a prominent extraosseous component: Pitfalls in diagnosis. Head Neck Pathol. 2010;4:192–7. doi: 10.1007/s12105-010-0182-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Philipsen HP, Reichart PA, Nikai H, Takata T, Kudo Y. Peripheral ameloblastoma: Biological profile based on 160 cases from the literature. Oral Oncol. 2001;37:17–27. doi: 10.1016/s1368-8375(00)00064-6. [DOI] [PubMed] [Google Scholar]
- 10.Sciubba JJ, Fantasia JE, Kahn LB. Tumors and Cysts of the Jaws. Washington DC: Armed Forces Institute of Pathology; 2001. [Google Scholar]
- 11.Gardner DG. Some current concepts on the pathology of ameloblastomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82:660–9. doi: 10.1016/s1079-2104(96)80441-0. [DOI] [PubMed] [Google Scholar]
- 12.Takai Y, Yamada N, Mizuno K. Peripheral ameloblastoma: Report of a case. Jpn J Oral Surg. 1982;28:295–9. [Google Scholar]
- 13.Miyamoto H, Iwatsubo T, Tamai K. A case of peripheral ameloblastoma developing in the anterior area of the maxilla. J Jpn Stomatol Soc. 1982;31:300–6. [Google Scholar]
- 14.Shiba R, Sakoda S, Yamada N. Peripheral ameloblastoma. J Oral Maxillofac Surg. 1983;41:460–3. doi: 10.1016/0278-2391(83)90132-5. [DOI] [PubMed] [Google Scholar]
- 15.Ide F, Kusama K, Tanaka A, Sakashita H. Peripheral ameloblastoma is not a hamartoma but rather more of a neoplasm. Oral Oncol. 2002;38:318–20. doi: 10.1016/s1368-8375(01)00124-5. [DOI] [PubMed] [Google Scholar]
- 16.Neville BW, Damm DD, Allen CM. Odontogenic cyst & tumours. In: Gnepp DR, editor. Diagnostic Surgical Pathology of the Head and Neck. 2nd ed. Philadelphia: Saunders Elsevier; 2009. pp. 785–838. [Google Scholar]
- 17.Nagamalini BR, Suneela S, Narayan TV, Shreedhar B, Mohanty L, Shenoy S, et al. Origin of ameloblastoma from basal cells of the oral epithelium- establishing the relation using neuroectodermal markers. J Clin Diagn Res. 2014;8:ZC44–7. doi: 10.7860/JCDR/2014/6740.5026. [DOI] [PMC free article] [PubMed] [Google Scholar]


