Abstract
Objective: We aimed to (1) examine differences in observed visual attention and motor activity, as well as comprehension of a science video between children with and without attention-deficit/hyperactivity disorder (ADHD) and (2) explore if psychostimulant medication improves ADHD behaviors and comprehension of a science video in children with ADHD.
Method: Children aged 7–11 with (n = 91) and without (n = 45) ADHD watched a science video and then completed a comprehension test. Then, children with ADHD began a 4-week within-subject, randomized, double-blind crossover trial of methylphenidate (MPH). At post-testing, children were randomized to receive placebo or their optimal dosage, watched another science film, and completed a comprehension test.
Results: Children with ADHD exhibited higher rates of motor activity during, and worse comprehension of material discussed within, the science video. Mediation models revealed that increased motor activity suppressed between-group differences in comprehension. MPH improved comprehension and visual attention, but not motor activity during the science video.
Conclusion: Children with ADHD may benefit from MPH to improve comprehension of and sustained attention during audiovisually presented learning material.
Keywords: listening comprehension, visual attention, motor activity, methylphenidate, ADHD
Introduction
Children with attention-deficit/hyperactivity disorder (ADHD) experience a wide range of impairments in social, home, and academic functioning (cf. Frazier et al. 2007; Wehmeier et al. 2010; Normand et al. 2013; Barkley 2014). Difficulties at school, including classroom behavior and academic performance, are the source of most referrals for children with ADHD (Pelham et al. 2005; American Psychiatric Association 2013). In fact, many of the academic difficulties experienced by children with ADHD can be traced back to the various classroom behaviors that they exhibit. In classroom observation studies, children with ADHD are significantly more off-task (Kofler et al. 2008; Imeraj et al. 2013), hyperactive (Porrino et al. 1983; DuPaul and Rapport 1993; Vile Junod et al. 2006), and disruptive (Abikoff et al. 2002; Lauth et al. 2006) and complete fewer classroom assignments (Rapport et al. 1994; Molina et al. 2009) relative to their typically developing (TD) peers.
Some of these classroom behaviors may reflect difficulties with comprehending or keeping up with the pace of information presented orally by the teacher, leading to various off-task and disruptive classroom behaviors (Jalongo 2010). Indeed, several DSM-5 (American Psychiatric Association 2013) ADHD inattentive symptoms seem closely linked to comprehension of orally presented information (e.g., failing to give close attention to details, appearing not to listen, and difficulty following instructions). Therefore, impairments in comprehension and subsequent recall of information may be intrinsic to ADHD rather than attributable to coexisting disorders (e.g., auditory processing or language disorder; McInnes et al. 2003).
The comprehension of information presented orally, often referred to as listening comprehension, is a fundamental skill required for successful academic attainment (Bashir and Scavuzzo 1992). This is not surprising as 50%–75% of students' classroom time is spent listening to the teacher, other students, or audiovisual presentations (Jalongo 2010). Listening comprehension is the ability to understand the meaning of spoken language and connect incoming information with material learned previously. It involves not only basic language skills (e.g., syntactic knowledge and vocabulary) but also higher order cognitive processing, including comprehension monitoring, theory of mind, and working memory (Kim 2015, 2016).
Extant research shows that children with ADHD comprehend and recall less than TD peers when listening to auditory instruction of educational material. This comprehension deficit has been demonstrated across a variety of paradigms, including listening to auditory text (Tannock et al. 1993; Lorch et al. 2004; Bellani et al. 2011; Cain and Bignell 2014; Papaeliou et al. 2015) and audiovisual presentations that feature narrative content (e.g., stories, television sitcoms; Lorch et al. 2004; Bailey et al. 2009, 2011) and/or expository instruction (i.e., instruction for learning new material; Landau et al. 1992; Lorch et al. 2000; Orban et al. 2017).
Some of these studies have attempted to examine children's behavior during these television programs to better understand possible ADHD-specific mechanisms that might lead to poor comprehension of audiovisual material containing narrative and/or expository content (Landau et al. 1992; Lorch et al. 2000, 2004; Bailey et al. 2009). We focus our review on the comprehension of expository television programs as we were primarily interested in understanding children's comprehension of academically oriented information.
One construct that has been explored is the impact of distraction on comprehension of expository audiovisual information. In general, studies found that children with ADHD exhibited similar rates of visual attention to televised content relative to control children; however, when appealing toys were present, all children were significantly less attentive, with children with ADHD being even less attentive than controls (Landau et al. 1992; Lorch et al. 2000). Correspondingly, children with ADHD recalled overall less information and had particular difficulty with cued recall for inferential questions from the video; however, they did perform equally well as TD controls on cued recall of facts (Lorch et al. 2000). These studies also identified that higher rates of visual attention to the television programs were associated with better comprehension (Landau et al. 1992; Lorch et al. 2000).
More recently, Orban et al. (2017) assessed ADHD-related visual attention deficits by comparing the behavior of children with ADHD and TD children during an expository “math” video relative to a preferred nonacademic video. Children with ADHD displayed less visual attention toward the math video than controls, but were not different from controls during the nonacademic video task. This study, however, did not explore comprehension of the videos to determine whether decreased visual attention was associated with poorer comprehension of the audiovisual material.
Several studies have suggested that hyperactive behaviors in the form of gross motor activity may be beneficial in helping children with ADHD to better attend during cognitively demanding and low-stimulating activities (Kofler et al. 2016). Excessive gross motor activity may act as a compensatory behavior to maintain arousal and attention during cognitively demanding activities for children with ADHD (Sarver et al. 2015; Hartanto et al. 2016). Moreover, a study by Kercood and Banda (2012) found that sitting on an exercise ball or doodling during a listening comprehension task resulted in improved comprehension and time spent on task; however, this study had a small sample that included only one of four children with an existing ADHD diagnosis. These findings suggest that minor physical activities (e.g., shaking/tapping limbs and sitting on an exercise ball) may be helpful in maintaining one's level of arousal or focused attention during cognitively demanding and/or low stimulating activities.
Overall, the extant literature seems to suggest that in distracting environments (e.g., classrooms), children with ADHD recall less information and experience difficulty integrating what they have learned to make causal connections or inferences, as a result of not visually attending to the task (Lorch et al. 2000, 2004). In addition, excessive gross motor activity often reported by teachers and parents may be helpful, rather than harmful, and serve as a compensatory mechanism for prefrontal cortex hypoarousal (Sarver et al. 2015; Hartanto et al. 2016).
The impact of psychostimulant medications on comprehension of educational material is unclear. Indeed, psychostimulant medications, such as methylphenidate (MPH), produce large beneficial effects on decreasing inattentive and hyperactive/impulsive behaviors (MTA Cooperative Group 1999), improve a range of cognitive deficits (Tannock et al. 1995; Epstein et al. 2011; Hawk et al. 2018), and are associated with improved productivity during classroom seatwork activities (Hawk et al. 2018) in children with ADHD. However, psychostimulant medications on their own typically do not improve learning related outcomes (Molina et al. 2009; Langberg and Becker 2012).
Only one study to date has investigated the effects of psychostimulant medications on listening comprehension of expository information in children with ADHD. McInnes et al. (2007) reported that psychostimulant medications improved children's ability to infer content from orally presented material, but did not improve comprehension of factual information; however, the authors noted that the lack of medication effects may have been due to a ceiling effect of comprehension scores. In addition, this study had a rather small sample size (n = 16).
The purpose of the current study was to (1) examine between-group differences (i.e., ADHD vs. controls) in comprehension of an expository instructional video given the frequent use of videos to augment teacher-led instruction in today's classrooms, (2) determine the extent to which visual attention and motor activity mediate between-group differences in comprehension, (3) evaluate the impact of medication on observed visual attention and motor activity during the video, as well as comprehension after the video, and (4) determine the extent to which visual attention and motor activity mediate between-group differences (placebo vs. medication group) in scores on the comprehension measure.
We expected unmedicated children with ADHD to be less visually attentive, more motorically active, and less accurate in their comprehension of information during the expository video task relative to TD children. We also expected that higher rates of visual attention in TD children compared with those with ADHD would mediate ADHD-related deficits in comprehension. Based on extant literature suggesting that motor activity may be compensatory in children with ADHD, we also hypothesized that higher rates of motor activity would mediate ADHD-related deficits in comprehension such that between-group differences in recall accuracy would be magnified after controlling for high rates of motor activity in the ADHD group.
For the medication trial, we hypothesized that MPH would lead to improvements in visual attention, motor activity, and comprehension of the audiovisual material presented and that higher rates of visual attention would attenuate between-group differences (MPH vs. placebo) in comprehension. We also predicted that medication effects on comprehension would be mediated by motor activity, such that between-group differences in comprehension would be magnified after controlling for high rates of motor activity in the placebo group. Finally, because we had access to a relatively large sample with adequate numbers of the two most common ADHD subtypes (i.e., Predominantly Inattentive Type and Combined Type), we also explored whether ADHD subtype impacted the hypothesized pattern of effects.
Methods
Participants
Of 149 children between the ages of 7 and 11 who participated in the baseline visit, 144 children contributed data for the behavioral observations (see Statistical analyses section for missing data analyses) across both baseline and medication visits. Ninety-nine of these participants were diagnosed with ADHD (47 with Combined Type and 52 with Predominantly Inattentive Type), and 45 were classified as control participants. Study participants had no neurological conditions, developmental disabilities, serious medical conditions, or history of brain injury. All participants with standardized scores below 80 for the full scale intelligence quotient (IQ) score on the Wechsler Abbreviated Scale of Intelligence (WASI) and for the achievement score on the Wechsler Individual Achievement Test, Second Edition (WIAT-II) reading or numerical operation subtests were excluded from the study to rule out children with possible intellectual or learning disabilities, respectively.
Stimulant-naive participants in the ADHD group were recruited through community referrals from schools, physicians, and mental health professionals. Diagnostic status was determined using methods similar to those used in the Multimodal Treatment Study of Children with ADHD (MTA; MTA Cooperative Group 1999). Specifically, children met the six of nine DSM-IV ADHD symptom criteria for each ADHD symptom domain (i.e., inattention and/or hyperactivity/impulsivity) if the parent's responses to the ADHD symptom on the Diagnostic Interview Schedule for Children-Parent Report Version 4.0 (DISC-P; Shaffer et al. 2000) and the teacher's responses to the ADHD symptoms on the Vanderbilt ADHD Teacher Rating Scale [VARS; Wolraich et al. (1998)] included at least six of the nine symptoms in a symptom domain as occurring often or very often.
It was required that a parent reported a minimum of at least four symptoms in an ADHD symptom domain on the DISC-P to meet criteria for that domain. If six or more symptoms were present only in the inattentive domain, the child met criteria for ADHD Inattentive Subtype (ADHD-I). If six or more symptoms were present in both the inattentive and hyperactive-impulsive domains, the child met criteria for ADHD Combined Subtype (ADHD-C). In addition to meeting the DSM-IV ADHD symptom criteria, children must also have fulfilled DSM-IV criteria B through E (i.e., age of onset, cross-setting impairment, and rule out of other causal conditions) based upon DISC-P responses.
Control participants were recruited through local schools and a database of local families interested in participating in research studies. They met study criteria if their parent endorsed three or fewer ADHD symptoms in both symptom domains and did not meet criteria for any DSM-IV oppositional defiant or conduct disorders on the DISC-P (Shaffer et al. 2000).
Procedures
This study was approved by the institutional review board. Children with ADHD and control participants underwent an initial screening visit during which their caregivers were administered the DISC-P interview and children were administered the WASI. This was followed by two assessment visits, each lasting ∼2 hours, during which children completed a battery of tasks administered as part of a larger study, including the naturalistic video task described below.
Within 1 week, children with ADHD then began a medication titration trial. The 4-week within subject, randomized, double-blind crossover trial of long-acting OROS (Osmotic-controlled Release Oral delivery System) MPH (CONCERTA®; Janssen Pharmaceuticals, Inc., Titusville, NJ) included three active dosage weeks (18, 27, 36 mg for children <25 kg; 18, 36, or 54 mg for children ≥25 kg) and 1 week of placebo, as described in prior investigations. At the end of each week, parents and teachers filled out Vanderbilt ADHD Rating Scales (Wolraich et al. 1998) and Pittsburgh Side Effects Rating Scales (Pelham et al. 1993), and the study physician also met with participant families and completed a Clinical Global Impressions-Improvement (CGI-I) form to assess response to medication.
At the end of the medication titration trial, two physicians blindly reviewed graphs portraying each week's parent, teacher, and clinician ratings, and each chose an optimal week based on the balance between effectiveness and side effects. Clinician agreement on optimal week (84% agreement) was comparable to that reported in the MTA study (MTA Cooperative Group 1999). Disagreements were resolved through a consensus process. ADHD symptom ratings showed significant improvement during the optimal dose week compared with the placebo week, with effect sizes for these behavioral effects of MPH equaling 0.82 and 0.87 (Cohen's d) for parent and teacher ratings, respectively.
At the conclusion of the medication titration trial, children were randomized to receive placebo or the optimal dosage from the medication titration trial for a week. During that week, children repeated the baseline battery of tasks, including the expository video task (post-testing). All post-testing began between 1 and 4 hours after medication/placebo ingestion. Children in the control group did not participate in follow-up visits.
Expository video task
The expository video task was designed to simulate watching a classroom educational video that a teacher might show in conjunction with a science lesson. It consisted of watching one of two videos (∼20 minutes in length). The videos were titled “Solids, Liquids, Gases: A First Look” and “Plants: A First Look” (Rainbow Educational Media 2001a, 2001b). Two videos were used to minimize boredom or fatigue from watching the video twice and to decrease the potential impact of practice effects on comprehension scores (i.e., children with ADHD watched one of the videos at baseline and the other video after the medication trial in a counterbalanced manner). Each video featured an off-screen narrator presenting informational content while also showing audiovisual content consistent with the information being narrated and often involved children in the video interacting with their environment to emphasize concepts.
Participants were told the name of the science video they were to watch, that they would be video recorded, and that they should pay attention because they would be given a short quiz afterward. Children completed an eight question quiz at the conclusion of the video to assess their comprehension, as well as cognitive attention to the instructional video. Total number correct out of eight questions served as the dependent variable. Test–retest reliability (r = 0.70) of the postvideo quiz was adequate based on the placebo group's pre–post scores (n = 44). Video recall accuracy was correlated significantly with a measure of reading ability on the WIAT (r = 0.40–0.44).
Noldus Observer XT (Noldus Information Technology 2008) was used to continuously code the onset and offset of each behavior. These codings provided the number of times and duration for each behavioral occurrence for each participant. Four coders were trained and calibrated on the coding scheme using a random set of 20 videos. Furthermore, coders met periodically to code together another random subset of videos (20; 7%) in an attempt to decrease coder drift.
Two behaviors (visual attention and fidgeting) were coded. On-task behavior, referred to as visual attention, was defined as visual attention (child's visual gaze) directed toward the television screen. Fidgeting behavior was coded as a general measure of motor activity. Fidgeting behavior included shifting, rocking, tapping/drumming fingers, or playing with hair, face, fingernails, or pockets.
Task behaviors were summarized as follows. We calculated the percent of on-task behavior (i.e., visual attention) by dividing the total number of seconds coded as visually attending to the video by the total number of seconds of the video duration. Percent fidgeting was calculated by dividing the total number of seconds coded as fidgeting by the total number of seconds of the video duration.
Thirty-five percent of the recordings were randomly chosen and double-coded for reliability. Reliability was assessed with intraclass correlation coefficients (ICCs) for the two variables used to derive our summary variables: total duration of on-task behavior (i.e., visual attention) and total duration of fidgeting. Interrater agreement was high for both visual attention and fidgeting at baseline and postvisit (all ICCs ≥0.89).
Statistical analyses
All analyses were conducted using Mplus software version 7.3 (Muthén and Muthén 2012), with the exception of examining group differences in the demographic variables and missing data which was conducted with SPSS software version 24.0 (IBM Corporation 2016).
The association between diagnostic (ADHD vs. Controls) and medication (MPH vs. Placebo) status and video recall accuracy was evaluated using linear regressions correcting for a “ceiling effect” for the video recall accuracy (comprehension) variable using the “censored = ” response variable function in Mplus. Grade in school (e.g., second grade) was used as a covariate in all analyses due to its significant positive association with the comprehension measure (r = 0.38–0.51) indicating that children in a higher grade in school performed better on the comprehension measure.
The current study evaluated the effects of two potential mediators (i.e., percent visual attention and fidgeting) to determine the role of these mediators in understanding diagnostic and medication status group differences in video recall accuracy. Correlations were examined between all dependent, independent, and mediating variables (see Supplementary Tables S1 and S2; Supplementary Data are available online at www.liebertpub.com/cap) for both the baseline and medication trial. Mplus software was used to conduct “censored from above” response variable mediation analyses. Missing data were handled through maximum likelihood estimation, and the significance of the indirect effect was determined using 90% confidence intervals (CIs) calculated from 5000 bootstrap draws. Analyses were conducted first using the entire ADHD sample, followed by analyses for ADHD subtypes (Appendix 1 for subtype analyses).
With regards to missing data at baseline, eight children with ADHD and one control participant had missing behavioral observations. The reasons for the missing behavioral observations at baseline were as follows: two video observations were lost due to mechanical errors (e.g., video camera dysfunction; ADHD n = 2; Control n = 0), four participants did not complete the video task (ADHD n = 3; Control n = 1), and three participants exhibited problematic behavior that interfered with watching the video (e.g., sleeping and crying; ADHD n = 3; Control n = 0). Of the 92 children with ADHD who completed the postvisit of the medication titration trial,1 one video observation was lost due to a mechanical error and two participants were excluded from the medication trial analyses due to accidentally receiving the same video twice.2
We compared participants with no missing/omitted data (baseline n = 136; postvisit n = 89) with those participants who had missing/omitted video data (baseline n = 9; postvisit n = 14) on the following variables: age, grade, sex, race, full scale IQ, oppositional defiant disorder (ODD), conduct disorder, anxiety disorder, mood disorder, and parent- or teacher-rated ADHD symptom scores. For the baseline visit, participants with missing data were younger (p = 0.03), had lower full scale IQ scores (p = 0.02), and were rated as more inattentive by their parent (p = 0.04). There were no other significant differences between these participants for any of the variables. For the medication trial postvisit, there were no significant differences between participants with complete data compared to those with missing/omitted data for any of the above variables.
Results
Baseline demographics
Baseline study sample characteristics are shown in Table 1. Chi-square analyses and one-way analyses of variances were conducted to investigate demographic differences between the children with ADHD and control children. As expected, children with ADHD exhibited higher rates of parent and teacher reported symptoms of inattention and hyperactivity–impulsivity. Children with ADHD had lower IQ scores than controls. IQ was not used as a covariate due to it being contraindicated when groups are not randomly assigned, outcome measures share variance with the grouping variable, and samples include neurodevelopmental disorders (Miller and Chapman 2001; Dennis et al. 2009). The rates of comorbid anxiety and disruptive behavior disorders among children with ADHD are consistent with studies in the ADHD literature (MTA Cooperative Group 1999). Means and standard deviations for visual attention, fidgeting, and video recall accuracy are reported in Table 2.
Table 1.
Demographic and Clinical Characteristics of the Baseline and Medication Trial Samples
| Baseline | Medication trial | |||||
|---|---|---|---|---|---|---|
| ADHD (n = 91) | Control (n = 45) | Group comparison | Randomized to MPH (n = 45) | Randomized to Placebo (n = 44) | Group comparison | |
| No. of females | 25 | 14 | ns | 15 | 10 | ns |
| No. of each ethnicity | ||||||
| Caucasian | 66 | 37 | ns | 38 | 30 | ns |
| African American | 14 | 7 | ns | 4 | 11 | Placebo > MPH* |
| Hispanic | 2 | 1 | ns | 1 | 1 | ns |
| Asian | 2 | 0 | ns | 0 | 0 | ns |
| American Indian | 2 | 0 | ns | 1 | 0 | ns |
| Did not report | 5 | 0 | ns | 1 | 2 | ns |
| ADHD subtype | ||||||
| Inattentive type | 47 | — | — | 21 | 24 | ns |
| Combined type | 44 | — | — | 24 | 20 | ns |
| No. with specified comorbid psychological disorder from DISC-P | ||||||
| Oppositional defiant disorder | 34 | 0 | ADHD > C** | 18 | 15 | ns |
| Conduct disorder | 4 | 0 | ns | 1 | 3 | ns |
| Any anxiety disorder | 33 | 2 | ADHD > C** | 15 | 14 | ns |
| Any mood disorder | 2 | 0 | ns | 1 | 0 | ns |
| Age in years, M (SD) | 8.09 (1.4) | 8.3 (1.4) | ns | 8.2 (1.3) | 8.0 (1.2) | ns |
| Grade in school, M (SD) | 2.6 (1.3) | 2.8 (1.4) | ns | 2.6 (1.4) | 2.6 (1.3) | ns |
| WASI full scale IQ, SD | 106.4 (12.4) | 116.4 (14.3) | ADHD < C** | 106.2 (12.6) | 105.3 (13.1) | ns |
| Parent Vanderbilt Severity Scores, M (SD) | ||||||
| Inattention | 20.6 (4.8) | 2.5 (2.1) | ADHD > C** | 21.0 (4.5) | 21.1 (4.4) | ns |
| Hyperactivity/impulsivity | 16.4 (6.4) | 1.3 (1.3) | ADHD > C** | 17.0 (6.6) | 16.3 (5.8) | ns |
| Teacher Vanderbilt Severity Scores, M (SD) | ||||||
| Inattention | 20.3 (5.1) | 3.3 (3.1) | ADHD > C** | 20.2 (4.8) | 20.1 (5.6) | ns |
| Hyperactivity/impulsivity | 14.4 (7.7) | 2.0 (3.3) | ADHD > C** | 14.1 (7.7) | 14.0 (7.9) | ns |
| Titration Trial optimal dosage mg/kg, M (SD) | — | — | — | 1.09 (0.5) | 1.14 (0.5) | ns |
p < 0.05; **p < 0.01.
ADHD, attention-deficit/hyperactivity disorder; C, Controls; DISC-P, Diagnostic Interview Schedule for Children, Parent report; IQ, intelligence quotient; M, mean; MPH, methylphenidate; ns, nonsignificant; SD, standard deviation; WASI, Wechsler Abbreviated Scale of Intelligence.
Table 2.
Means, Standard Deviations, and Pairwise Comparisons for Attention-Deficit/Hyperactivity Disorder Entire Sample, Attention-Deficit/Hyperactivity Disorder Combined Subtype, Attention-Deficit/Hyperactivity Disorder Inattentive Subtype, and Control Samples at Baseline
| Pairwise comparisons | ||||||||
|---|---|---|---|---|---|---|---|---|
| ADHD ALL (n = 91) | ADHD-C (n = 44) | ADHD-I (n = 47) | Control (n = 45) | Cohen's d (p) | ||||
| Mean (SD) Range | ADHD ALL vs. Control | ADHD-C vs. Control | ADHD-I vs. Control | ADHD-C vs. ADHD-I | ||||
| Visual attention | ||||||||
| % Mean (SD) | 92.3 (7.6) | 91.0 (8.2) | 93.6 (6.7) | 94.8 (6.5) | 0.35 (0.059) | 0.51 (0.024) | 0.18 (0.42) | 0.35 (0.12) |
| Range | 54.2–99.9 | 54.2–99.5 | 58.9–99.9 | 74.1–100 | ||||
| Fidgeting | ||||||||
| % Mean (SD) | 55.6 (24.1) | 56.3 (22.8) | 54.9 (25.2) | 47.4 (20.6) | 0.36 (0.024) | 0.41 (0.047) | 0.33 (0.09) | 0.06 (0.74) |
| Range | 6.8–99.3 | 9.7–94.2 | 6.8–99.3 | 5.7–90.5 | ||||
| Accuracy | ||||||||
| Mean (SD) | 6.5 (2.5) | 6.4 (1.8) | 6.4 (1.5) | 7.3 (1.0) | 0.38 (0.001) | 0.62 (0.009) | 0.70 (0.006) | 0.0 (0.55) |
| Range | 0–8 | 0–8 | 1–8 | 3–8 | ||||
Accuracy measured in number of correct answers out of eight questions. p Values derived from regression analysis in Mplus with diagnostic status predicting the corresponding variable.
ADHD, attention-deficit/hyperactivity disorder; ADHD-C, ADHD Combined Subtype; ADHD-I, ADHD Inattentive Subtype; SD, standard deviation.
Association between diagnostic status and video recall accuracy
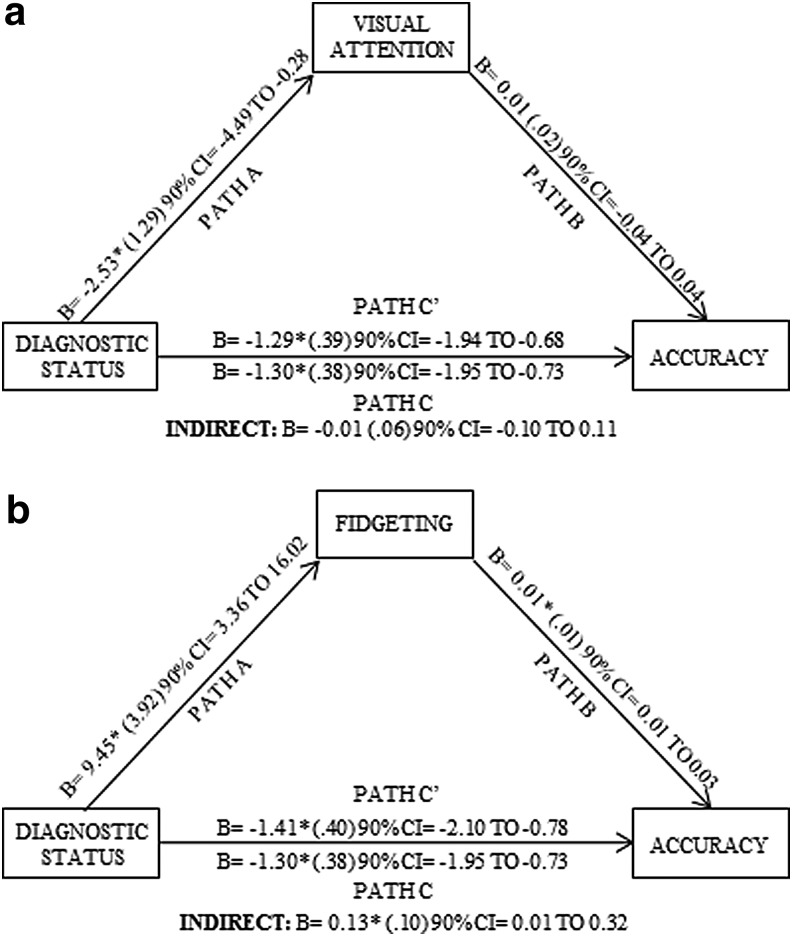
Diagnostic status (TD = 0; ADHD = 1) was negatively associated with recall accuracy whereby the ADHD group performed worse on the video recall measure relative to control children after controlling for grade (B = −1.30; 90% CI = −1.95 to −0.73). The mediating role of visual attention and fidgeting on the relationship between diagnostic status and video recall accuracy was examined separately (Fig. 1a, b). ADHD subtype analyses did not differ greatly from the full ADHD sample and indirect effects were nonsignificant; therefore, these results are included in Appendix 1.
FIG. 1.
Baseline visual attention and fidgeting mediation models. Figures depict (a) visual attention and (b) fidgeting as a mediator (m) between diagnostic status (x) and accuracy (y). In mediation, Path A represents the effect of x on m. Path B represents the effect of m on y, controlling for x. Path C′ represents the effect of x on y controlling for m. Path C represents the total effect or the effect of x on y before mediation. Estimate in parentheses reflects standard error.
Baseline mediation analyses
Children with ADHD were significantly less attentive to the video relative to controls (B = −2.53; 90% CI = −4.49 to −0.28). Visual attention was not significantly associated with video recall accuracy (B = 0.01; 90% CI = −0.04 to 0.04) when controlling for diagnostic differences. The indirect effect of visual attention was not significant (B = −0.01; 90% CI = −0.10 to 0.11), demonstrating that visual attention did not serve as a significant mediator in the relationship between ADHD status and video recall accuracy (Fig. 1a).
Children with ADHD demonstrated significantly higher rates of fidgeting (B = 9.45; 90% CI = 3.36–16.02) during the video. Higher rates of fidgeting (B = 0.01; 90% CI = 0.01–0.03) were positively associated with better recall accuracy after the video when controlling for diagnostic status. The indirect effect was significant (B = 0.13; 90% CI = 0.01–0.32), indicating that fidgeting served as mediator of diagnostic differences in video recall accuracy. Examination of the C′ pathway indicated that the presence of high rates of fidgeting in children with ADHD resulted in the suppression of between-group differences in video recall accuracy. Specifically, the magnitude of the between-group difference in recall accuracy was greater after accounting for variance in motor activity (Fig. 1b).
Medication trial demographics
Medication trial sample characteristics are shown in Table 1. The groups randomized to the MPH versus placebo for post-testing did not differ in terms of age, sex, ADHD subtype, IQ, baseline ADHD symptom scores, or mental health comorbidity; however, a higher proportion of African American children were randomized to the placebo group than the MPH group (Table 1). Means and standard deviations for the visual attention, fidgeting, and video recall accuracy are reported in Table 3. Optimal dosage (mg/kg) for the Placebo and MPH groups is reported in Table 1. The number of children assigned to each optimal dose based on titration trial results for each group was as follows: Placebo group (0 mg, n = 13; 18 mg, n = 7; 27 mg, n = 4; 36 mg, n = 14; and 54 mg, n = 6) and MPH group (0 mg, n = 10; 18 mg, n = 11; 27 mg, n = 1; 36 mg, n = 15; and 54 mg, n = 8).
Table 3.
Means, Standard Deviations, and Pairwise Comparisons for Attention-Deficit/Hyperactivity Disorder Entire Sample, Attention-Deficit/Hyperactivity Disorder Combined Subtype, Attention-Deficit/Hyperactivity Disorder Inattentive Subtype in Methylphenidate and Placebo Groups
| Pairwise comparisons to Placebo | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| MPH | Placebo | Cohen's d (p) | |||||||
| ADHD ALL (n = 45) | ADHD-C (n = 24) | ADHD-I (n = 21) | ADHD ALL (n = 44) | ADHD-C (n = 20) | ADHD-I (n = 24) | ADHD ALL | ADHD-C | ADHD-I | |
| Visual attention | |||||||||
| % Mean (SD) | 95.3 (4.4) | 94.8 (4.1) | 95.9 (4.7) | 91.2 (7.9) | 89.6 (9.1) | 92.6 (6.4) | 0.64 (0.001) | 0.76 (0.01) | 0.58 (0.049) |
| Range | 77–100 | 87–100 | 77–100 | 71–100 | 71–100 | 71–100 | |||
| Fidgeting | |||||||||
| % Mean (SD) | 49.1 (22.7) | 50.7 (21.8) | 47.4 (21.4) | 46.2 (23.4) | 46.1 (21.9) | 46.2 (24.5) | 0.13 (0.58) | 0.21 (0.61) | 0.05 (0.87) |
| Range | 1.5–89.0 | 8.1–89.0 | 1.5–83.8 | 7.3–98.9 | 10.1–89.9 | 7.3–98.9 | |||
| Accuracy | |||||||||
| Mean (SD) | 7.0 (1.2) | 6.9 (1.3) | 7.0 (1.0) | 6.4 (1.6) | 6.5 (1.5) | 6.4 (1.7) | 0.43 (0.002) | 0.29 (0.06) | 0.42 (0.009) |
| Range | 4–8 | 4–8 | 5–8 | 2–8 | 2–8 | 3–8 | |||
Accuracy measured in number of correct answers out of eight questions. Pairwise comparison p values derived from regression analysis in Mplus with medication status predicting the corresponding variable; therefore, discrepancies between p values are due to differences in Mplus estimating using maximum likelihood versus maximum likelihood with bootstrapping.
ADHD, attention-deficit/hyperactivity disorder; ADHD-C, ADHD Combined Subtype; ADHD-I, ADHD Inattentive Subtype; MPH, methylphenidate; SD, standard deviation.
Association between medication status and video recall accuracy
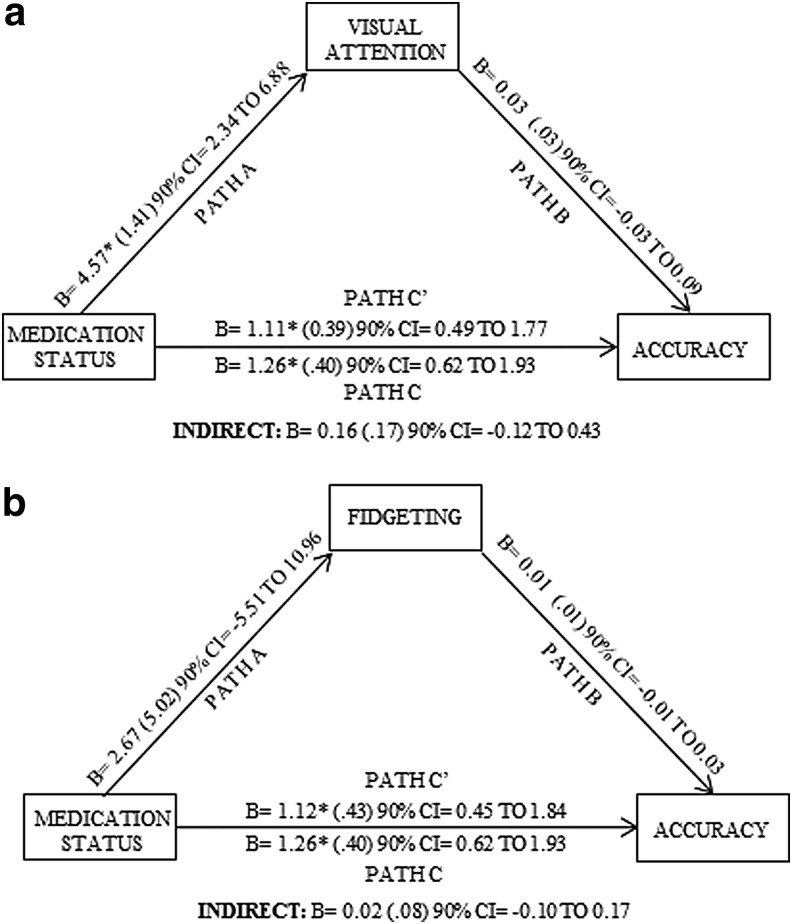
Medication status was positively associated with video recall accuracy whereby the children randomized to the MPH group performed better on the video recall measure relative to children randomized to the placebo group (B = 1.26; 90% CI = 0.62–1.93). The mediating roles of visual attention and fidgeting on the relationship between medication status and video recall accuracy were examined separately (Fig. 2a, b). ADHD subtype analyses did not differ substantially from the full ADHD sample, and all indirect effects were nonsignificant. These results are described in Appendix 1.
FIG. 2.
Medication trial visual attention and fidgeting mediation models. Figures depict (a) visual attention and (b) fidgeting as a mediator (m) between medication status (x) and accuracy (y) in the medication titration trial for participants with ADHD. In mediation, Path A represents the effect of x on m. Path B represents the effect of m on y, controlling for x. Path C′ represents the effect of x on y controlling for m. Path C represents the total effect or the effect of x on y before mediation. Estimate in parentheses reflect standard error.
MPH affects mediation analysis
Children in the MPH group were significantly more attentive during the video relative to children in the placebo group (B = 4.57; 90% CI = 2.34–6.88). Visual attention was not significantly associated with video recall accuracy (B = 0.03; 90% CI = −0.03 to 0.09) when controlling for medication status. The indirect effect of visual attention was not significant (B = 0.16; 90% CI = −0.12 to 0.43), demonstrating that visual attention did not serve as a significant mediator in the relationship between medication status and video recall accuracy (Fig. 2a).
Children in the MPH group did not differ from children in the placebo group in percent time fidgeting during the video (B = 2.67; 90% CI = −5.51 to 10.96). Fidgeting was not significantly associated with video recall accuracy (B = 0.01; 90% CI = −0.01 to 0.03) when controlling for medication status. The indirect effect of fidgeting (B = 0.02; 90% CI = −0.10 to 0.17) was not significant, demonstrating that fidgeting was not a significant mediator in the relationship between medication status and video recall accuracy (Fig. 2b).
Discussion
The results of the present study indicate that children with ADHD are less accurate in their recall of information from an expository science video relative to TD peers. This finding is supported by past investigations reporting that children with ADHD recall less information from televised programming (Landau et al. 1992; Lorch et al. 2000) and auditory presentations (Tannock et al. 1993; Bellani et al. 2011; Cain and Bignell 2014; Papaeliou et al. 2015) than TD children. Although significant, the difference in scores on the comprehension measure in the current study between the ADHD and control group may appear inconsequential (i.e., 6.5 vs. 7.4 or 81% vs. 91% of the ADHD and control group, respectively); however, missing information from various classroom activities because of inattention can have a compounding effect over time.
Given that children with ADHD missed 10% more information from an eight-item quiz during a 20-minute expository film in a laboratory setting, it is expected that this percentage would be greater with less stimulating, more cognitively demanding academic content or activities (Orban et al. 2017), as well as within distracting environments (Landau et al. 1992; Lorch et al. 2000).
Children with ADHD were also found to be less visually attentive relative to TD controls during the expository science film. This finding is consistent with the extant literature that children with ADHD are less visually attentive to educational television programs (Landau et al. 1992; Lorch et al. 2000; Orban et al. 2017) and classroom instruction (Imeraj et al. 2013) compared to TD peers. In addition, children with ADHD exhibited higher rates of motor activity during the expository film relative to TD controls. While no study to date has investigated rates of motor activity during audiovisual presentations in children with ADHD, several studies have demonstrated that children with ADHD exhibit increased motor activity during academic (Porrino et al. 1983; Abikoff et al. 2002; Vile Junod et al. 2006) and cognitively demanding activities (Rapport et al. 2009; Sarver et al. 2015; Hartanto et al. 2016).
Mediation analyses were performed as a next step to understand the mechanism between diagnostic status and recall accuracy; however, contrary to our hypotheses, visual attention did not serve as a significant mediator. This finding is inconsistent with previous investigations that found nonsignificant differences in video comprehension when controlling for visual attention (Lorch et al. 2000, 2004). We may have been unable to detect a significant indirect effect due to restricted range related to ceiling effects of high rates of attention (i.e., average visual attention 90% or higher) and recall accuracy (i.e., average correct 80% higher) in our sample. For example, Lorch et al. (2000) tested visual attention of two videos differing in narrative and expository information, in the presence of distracting toys, and assessed accuracy with over 20 questions which may have promoted more variability in the visual attention and comprehension variables to allow them to detect a mediation effect.
In addition in the current study, the correlation between visual attention and accuracy was significant for the control group (r = 0.43), but not for the ADHD group (r = 0.01). This suggests that higher rates of visual attention are associated with better recall accuracy in TD children, but neither higher nor lower rates of visual attention are associated with better or worse recall in children with ADHD. One explanation is that, despite having their eyes directed toward the screen, children with ADHD were not cognitively attending to the film and were engaging in other types of off-task behavior (e.g., mind wandering) during the video; therefore, the mechanism leading to worse comprehension in the ADHD group may have been due to an unmeasured variable, such as cognitive inattention, as opposed to behavioral inattention.
As predicted, fidgeting was a significant mediator that suppressed between-group differences in recall accuracy. In other words, between-group differences in recall were magnified when controlling for higher rates of fidgeting in children with ADHD. This is consistent with a theory that fidgeting behaviors exhibited by children with ADHD during academic or cognitively demanding tasks may serve as a compensatory mechanism by increasing gross motor activity to augment cortical underarousal (Rapport et al. 2009; Sarver et al. 2015). Indeed, prior research has reported that children with ADHD exhibit more gross motor activity during working memory tasks (Sarver et al. 2015; Hartanto et al. 2016) and core academic subjects (Porrino et al. 1983; Abikoff et al. 2002) and that higher rates of gross motor activity improve, rather than hinder, performance on cognitively demanding tasks (Kercood and Banda 2012; Sarver et al. 2015; Hartanto et al. 2016) in children with ADHD.
MPH significantly improved video recall accuracy although the effect size of this improvement was small (d = 0.28). MPH was also associated with improved visual attention (d = 0.49), but did not result in changes in motor activity. Extant research indicates that MPH improves on-task behavior in children with ADHD during in vivo (Evans et al. 2001; Pelham et al. 2002) and laboratory analog (Wigal et al. 2011; Hawk et al. 2018) classroom settings (Prasad et al. 2013), but is not been associated with sustained improvement in academic functioning (Molina et al. 2009; Currie et al. 2014). In addition, a prior study found that MPH resulted in increased comprehension of inferential information, but not basic facts, from an auditory listening task in children with ADHD (McInnes et al. 2007). This is inconsistent with the findings from the current study as most of the questions presented were factual; however, no study to date has examined medication effects on comprehension of expository audiovisual information.
While improvements in video recall accuracy and visual attention to task were evident, visual attention did not serve as a significant mediator in the relationship between medication status and recall accuracy. This may have been due to a ceiling effect of already high rates of accuracy and visual attention with and without MPH. In addition, because the questions tested factual information from the video, the extent to which one physically orients themselves to the television screen may be less essential to one's understanding of the content. That is, one may not be physically oriented to the screen, but may still be able to comprehend the factual content of the film. Future studies may benefit from including inferential questions to determine if physical orientation (i.e., eyes on the screen) impacts one's inferential understanding of information during audiovisual presentations.
There are several limitations that potentially reduce the generalizability of this study's findings. First, this study evaluated children's behavior during and comprehension of an educational science video: videos are not perfect analogs to classroom instruction, but are often used to augment teacher-led instruction.
Second, our observed rates of attention to task were higher for the ADHD group in the current study compared to previous investigations of attention in the context of in vivo classrooms (i.e., ADHD = 40%–81% and TD = 80%–91%; Kofler et al. 2009; Imeraj et al. 2013) and video instruction (i.e., ADHD = 84% and TD = 93%; Orban et al. 2017). This may be due to the fact that children in this study watched the video in a room with minimal distractions (e.g., no other students) which is not typical of regular classroom environments. Given that children with ADHD are prone to exhibiting off-task behavior in the presence of salient distractions (Landau et al. 1992; Lorch et al. 2000), our ability to detect robust differences in video recall accuracy and visual attention in children with ADHD relative to controls may have been somewhat limited. Nonetheless, we were able to detect between-group differences, as well as medication effects, on visual attention and accuracy despite these ceiling effects; however, the ceiling effects may have impaired our ability to detect the mediation effects.
Third, the comprehension measure consisted of only eight, primarily factual, questions about the content of a 20-minute video; therefore, these results may not generalize to broad comprehension measures, as well as other educational settings.
Fourth, the ADHD sample was stimulant-naive, was recruited from both community and clinical sources, had a high rate of predominantly inattentive subtype, had average IQ scores, and had lower rates of mental health comorbidity than those recruited solely from subspecialty clinics. Thus, the results of the current study may not generalize to all children with ADHD.
Finally, we were unable to measure how the effects of cognitive inattention (e.g., mind wandering) may play a role in comprehension. Future studies may benefit from including measures of cognitive functioning (e.g., working memory) and electrophysiology (e.g., EEG) to determine whether behavioral inattention versus cognitive dysfunction contributes unique variance to comprehension abilities in children with ADHD.
Conclusion
Children with ADHD were less visually attentive and accurate in their recall of information from, and exhibit more motor activity during, an expository science video relative to TD peers. Mediation analyses revealed that diagnostic differences in video comprehension were magnified when controlling for higher rates of fidgeting in children with ADHD. MPH significantly improved video recall accuracy and visual attention to the video, but did not improve fidgeting behaviors. In addition, visual attention and fidgeting did not serve as significant mediators between medication status and video recall accuracy.
Clinical Significance
MPH may be helpful in increasing attention during televised instruction of expository information. Increased attention to a task may also have the added benefit of reducing disruptive behaviors that frequently occur in classrooms (Abikoff et al. 2002; Lauth et al. 2006).
Supplementary Material
Appendix 1: Subtype Analyses
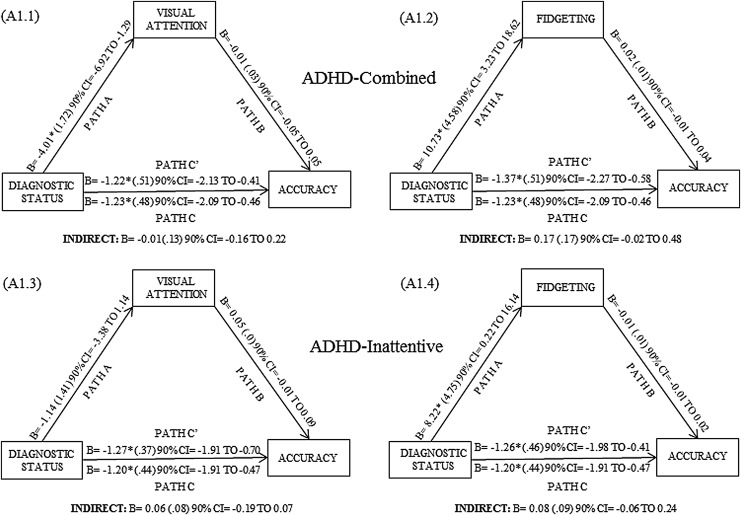
Subtype analyses for baseline mediation analysis
A subtype analysis was undertaken to determine if the pattern of results reported above was consistent when examining different subtypes of attention-deficit/hyperactivity disorder (ADHD). Consistent with the findings reported above, both children with ADHD-Combined Subtype (ADHD-C) (B = −1.23; 90% confidence interval [CI] = −2.09 to −0.46; Appendix Fig. A1.1, A1.2) and ADHD-Predominantly Inattentive Subtype (ADHD-I) (B = −1.20; 90% CI = −1.91 to −0.47; Appendix Fig. A1.3–A1.4) were less accurate in their recall of the video. Children with ADHD-C were less visually attentive compared to controls (B = −4.01; 90% CI = −6.92 to −1.29), but this pathway was not significant for the ADHD-I group. Both children with ADHD-C (B = 10.73; 90% CI = 3.23–18.62) and ADHD-I (B = 8.22; 90% CI = 0.22–16.14) exhibited higher rates of fidgeting during the video relative to the control group. No other paths in the mediation model, including the indirect effects, were significant when examining ADHD subtypes separately. See Appendix Figures A1.1–A1.4 for estimates of direct and indirect effects for separate ADHD subtypes.
APPENDIX FIG. A1.
Subtype baseline mediation models. Figures depict (A1.1) visual attention and (A1.2) depicts fidgeting as a mediator (m) between diagnostic status (x) and accuracy (y) in the ADHD-Combined and Control groups. Figures (A1.3) and (A1.4) examine visual attention and fidgeting as mediators in the ADHD-Inattentive and Control groups. In mediation, Path A represents the effect of x on m. Path B represents the effect of m on y, controlling for x. Path C′ represents the effect of x on y controlling for m. Path C represents the total effect or the effect of x on y before mediation. Estimate in parentheses reflects standard errors. ADHD, attention-deficit/hyperactivity disorder.
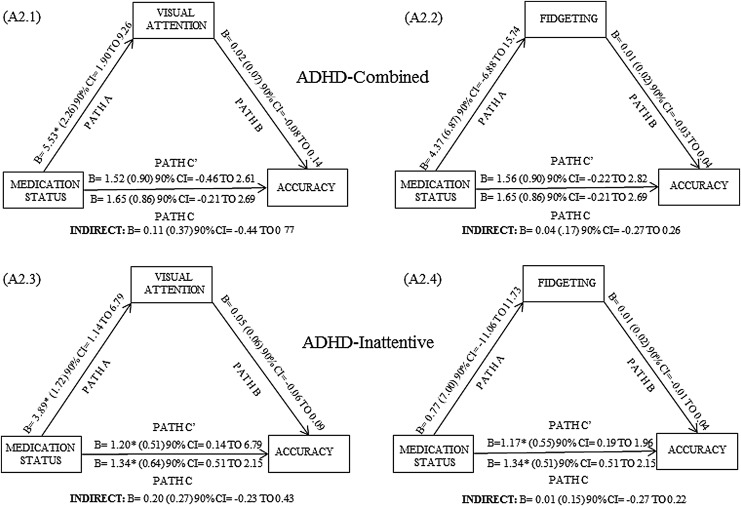
Subtype analyses for methylphenidate effects
A subtype analysis was undertaken to determine if the pattern of results reported above was consistent when examining different subtypes of ADHD for the medication trial. When examining ADHD subtypes separately, children with ADHD-I subtype (B = 1.34; 90% CI = 0.51–2.15), but not ADHD-C subtype (B = 1.65; 90% CI = −0.21 to 2.69), in the methylphenidate (MPH) group had higher recall accuracy relative to the placebo group. Children with ADHD-C (B = 5.53; 90% CI = 1.90–9.26) and ADHD-I (B = 3.89; 90% CI = 1.14–6.79) in the MPH group exhibited higher rates of attention during the video relative to the placebo group. There were no subtype differences in the MPH group compared to the placebo group in rates of fidgeting during the video. No other paths in the mediation model, including the indirect effects, were significant when examining ADHD subtypes separately. See Appendix Figures A2.1–A2.4 for estimates of direct and indirect effects for separate ADHD subtypes.
APPENDIX FIG. A2.
Subtype Medication Trial Mediation Models. Figures depict (A2.1) visual attention and (A2.2) fidgeting as a mediator (m) between medication status (x) and accuracy (y) in the ADHD-Combined sample in the medication titration trial. Figures (A2.3) and (A2.4) examine visual attention and fidgeting as mediators in the ADHD-Inattentive sample in the medication titration trial. In mediation, Path A represents the effect of x on m. Path B represents the effect of m on y, controlling for x. Path C′ represents the effect of x on y controlling for m. Path C represents the total effect or the effect of x on y before mediation. Estimate in parentheses reflects standard error. ADHD, attention-deficit/hyperactivity disorder.
Footnotes
Eleven participants dropped out of the study prior to the post-test visit.
ADHD participants (n = 7) with missing baseline data (i.e., due to mechanical or behavioral problems) who completed the medication titration trial and participated in the postvisit were included in the medication trial analyses.
Disclosures
Jeffery N. Epstein, has received research support from Akili Interactive Labs, received royalties from Multi-Health Systems, Inc., received consulting fees from the American Academy of Pediatrics and American Board of Pediatrics, and received licensing fees from Optimal Medicine, Inc. and IXICO.
References
- Abikoff HB, Jensen PS, Arnold LE, Hoza B, Hechtman L, Pollack S, Martin D, Alvir J, March JS, Hinshaw S, Vitiello B, Newcorn J, Greiner A, Cantwell DP, Conners CK, Elliott G, Greenhill LL, Kraemer H, Pelham WE, Jr, Severe JB, Swanson JM, Wells K, Wigal T: Observed classroom behavior of children with ADHD: Relationship to gender and comorbidity. J Abnorm Child Psychol 30:349–359, 2002 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed. Arlington: American Psychiatric Publishing; 2013 [Google Scholar]
- Barkley RA. (ed): Attention-Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment, 5th ed. New York, Guilford Publications, 2014 [Google Scholar]
- Bashir AS, Scavuzzo A: Children with language disorders: Natural history and academic success. J Learn Disabil 25:53–65, 1992 [DOI] [PubMed] [Google Scholar]
- Bailey UL, Derefinko KJ, Milich R, Lorch EP, Metze A: The effects of stimulant medication on free recall of story events among children with ADHD. J Psychopathol Behav Assess 33:409–419, 2011 [Google Scholar]
- Bailey UL, Lorch EP, Milich R, Charnigo R: Developmental changes in attention and comprehension among children with attention deficit hyperactivity disorder. Child Dev 80:1842–1855, 2009 [DOI] [PubMed] [Google Scholar]
- Bellani M, Moretti A, Perlini C, Brambilla P: Language disturbances in ADHD. Epidemiol Psychiatr Sci 20:311–315, 2011 [DOI] [PubMed] [Google Scholar]
- Cain K, Bignell S: Reading and listening comprehension and their relation to inattention and hyperactivity. Br J Educ Psychol 84:108–124, 2014 [DOI] [PubMed] [Google Scholar]
- Currie J, Stabile M, Jones L: Do stimulant medications improve educational and behavioral outcomes for children with ADHD? J Health Econ 37:58–69, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Francis DJ, Cirino PT, Schachar R, Barnes MA, Fletcher JM: Why IQ is not a covariate in cognitive studies of neurodevelopmental disorders. J Int Neuropsychol Soc 15:331–343, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DuPaul GJ, Rapport MD: Does methylphenidate normalize the classroom performance of children with attention deficit disorder? J Am Acad Child Adolesc Psychiatry 32:190–198, 1993 [DOI] [PubMed] [Google Scholar]
- Epstein JN, Brinkman WB, Froehlich T, Langberg JM, Narad ME, Antonini TN, Sheils K, Simon JO, Altaye M: Effects of stimulant medication, incentives, and event rate on reaction time variability in children with ADHD. Neuropsychopharmacology 36:1060–1072, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans SW, Pelham WE, Smith BH, Bukstein O, Gnagy EM, Greiner AR, Altenderfer L, Baron-Myak C: Dose–response effects of methylphenidate on ecologically valid measures of academic performance and classroom behavior in adolescents with ADHD. Exp Clin Psychopharmacol 9:163–175, 2001 [DOI] [PubMed] [Google Scholar]
- Frazier TW, Youngstrom EA, Glutting JJ, Watkins MW: ADHD and achievement: Meta-analysis of the child, adolescent, and adult literatures and a concomitant study with college students. J Learn Disabil 40:49–65, 2007 [DOI] [PubMed] [Google Scholar]
- Hartanto TA, Krafft CE, Iosif AM, Schweitzer JB: A trial-by-trial analysis reveals more intense physical activity is associated with better cognitive control performance in attention-deficit/hyperactivity disorder. Child Neuropsychol 22:618–626, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawk LW, Jr, Fosco WD, Colder CR, Waxmonsky JG, Pelham WE, Jr, Rosch KS: How do stimulant treatments for ADHD work? Evidence for mediation by improved cognition. J Child Psychol Psychiatr 2018. [Epub ahead of print]. DOI: 10.1111/jcpp.12917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IBM Corporation: IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corporation; 2016 [Google Scholar]
- Imeraj L, Antrop I, Sonuga-Barke E, Deboutte D, Deschepper E, Bal S, Roeyers H: The impact of instructional context on classroom on-task behavior: A matched comparison of children with ADHD and non-ADHD classmates. J Sch Psychol 51:487–498, 2013 [DOI] [PubMed] [Google Scholar]
- Jalongo MR: Listening in early childhood: An interdisciplinary review of the literature. Int J Listening 24:1–18, 2010 [Google Scholar]
- Kercood S, Banda DR: The effects of added physical activity on performance during a listening comprehension task for students with and without attention problems. Int J App Educ Stud 13:19–32, 2012 [Google Scholar]
- Kim YSG: Language and cognitive predictors of text comprehension: Evidence from multivariate analysis. Child Dev 86:128–144, 2015 [DOI] [PubMed] [Google Scholar]
- Kim YSG: Direct and mediated effects of language and cognitive skills on comprehension of oral narrative texts (listening comprehension) for children. J Exp Child Psychol 141:101–120, 2016 [DOI] [PubMed] [Google Scholar]
- Kofler MJ, Raiker JS, Sarver DE, Wells EL, Soto EF: Is hyperactivity ubiquitous in ADHD or dependent on environmental demands? Evidence from meta-analysis. Clin Psychol Rev 46:12–24, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kofler MJ, Rapport MD, Alderson RM: Quantifying ADHD classroom inattentiveness, its moderators, and variability: A meta-analytic review. J Child Psychol Psychiatry 49:59–69, 2008 [DOI] [PubMed] [Google Scholar]
- Landau S, Lorch EP, Milich R: Visual attention to and comprehension of television in attention‐deficit hyperactivity disordered and normal boys. Child Dev 63:928–937, 1992 [PubMed] [Google Scholar]
- Langberg JM, Becker SP: Does long-term medication use improve the academic outcomes of youth with attention-deficit/hyperactivity disorder? Clin Child Fam Psychol Rev 15:215–233, 2012 [DOI] [PubMed] [Google Scholar]
- Lauth GW, Heubeck BG, Mackowiak K: Observation of children with attention-deficit hyperactivity (ADHD) problems in three natural classroom contexts. Br J Educ Psychol 76:385–404, 2006 [DOI] [PubMed] [Google Scholar]
- Lorch EP, Milich R, Sanchez RP, van den Broek P, Baer S, Hooks K, Hartung C, Welsh R: Comprehension of televised stories in boys with attention deficit/hyperactivity disorder and nonreferred boys. J Abnorm Psychol 109:321–330, 2000 [DOI] [PubMed] [Google Scholar]
- Lorch EP, O'Neil K, Berthiaume KS, Milich R, Eastham D, Brooks T: Story comprehension and the impact of studying on recall in children with attention deficit hyperactivity disorder. J Clin Child Adolesc Psychol 33:506–515, 2004 [DOI] [PubMed] [Google Scholar]
- McInnes A, Bedard AC, Hogg-Johnson S, Tannock R: Preliminary evidence of beneficial effects of methylphenidate on listening comprehension in children with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol 17:35–49, 2007 [DOI] [PubMed] [Google Scholar]
- McInnes A, Humphries T, Hogg-Johnson S, Tannock R: Listening comprehension and working memory are impaired in attention-deficit hyperactivity disorder irrespective of language impairment. J Abnorm Child Psychol 31:427–443, 2003 [DOI] [PubMed] [Google Scholar]
- Miller GA, Chapman JP. Misunderstanding analysis of covariance. J Abnorm Psychol 110:40–48, 2001 [DOI] [PubMed] [Google Scholar]
- Molina BS, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, Epstein JN, Hoza B, Hechtman L, Abikoff HB, Elliott GR, Greenhill LL, Newcorn JH, Wells KC, Wigal T, Gibbons RD, Hur K, Houck PR, MTA Cooperative Group: The MTA at 8 years: Prospective follow-up of children treated for combined-type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry 48:484–500, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MTA Cooperative Group: Multimodal Treatment Study of Children with ADHD. A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 56:1073–1086, 1999 [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO: Mplus Version 7. Los Angeles, CA: Muthén & Muthén, 1998 [Google Scholar]
- Noldus Information Technology: The Observer XT. Wageningen, The Netherlands: Noldus Information Technology b. v., 2008 [Google Scholar]
- Normand S, Schneider BH, Lee MD, Maisonneuve MF, Chupetlovska-Anastasova A, Kuehn SM, Robaey P: Continuities and changes in the friendships of children with and without ADHD: A longitudinal, observational study. J Abnorm Child Psychol 41:1161–1175, 2013 [DOI] [PubMed] [Google Scholar]
- Orban SA, Rapport MD, Friedman LM, Eckrich SJ, Kofler MJ: Inattentive behavior in boys with ADHD during classroom instruction: The mediating role of working memory processes. J Abnorm Child Psychol 46:713–727, 2017 [DOI] [PubMed] [Google Scholar]
- Papaeliou CF, Maniadaki K, Kakouros E: Association between story recall and other language abilities in schoolchildren with ADHD. J Atten Disord 19:53–62, 2015 [DOI] [PubMed] [Google Scholar]
- Pelham WE, Carlson C, Sams SE, Vallano G, Dixon MJ, Hoza B: Separate and combined effects of methylphenidate and behavior modification on boys with attention deficit-hyperactivity disorder in the classroom. J Consult Clin Psychol 61:506–515, 1993 [DOI] [PubMed] [Google Scholar]
- Pelham WE, Jr, Fabiano GA, Massetti GM: Evidence-based assessment of attention deficit hyperactivity disorder in children and adolescents. J Clin Child Adolesc Psychol 34:449–476, 2005 [DOI] [PubMed] [Google Scholar]
- Pelham WE, Hoza B, Pillow DR, Gnagy EM, Kipp HL, Greiner AR, Waschbusch DA, Trane ST, Greenhouse J, Wolfson L, Fitzpatrick E: Effects of methylphenidate and expectancy on children with ADHD: Behavior, academic performance, and attributions in a summer treatment program and regular classroom settings. J Consult Clin Psychol 70:320–335, 2002 [PubMed] [Google Scholar]
- Porrino LJ, Rapoport JL, Behar D, Sceery W, Ismond DR, Bunney WE: A naturalistic assessment of the motor activity of hyperactive boys: I. Comparison with normal controls. Arch Gen Psychiatry 40:681–687, 1983 [DOI] [PubMed] [Google Scholar]
- Prasad V, Brogan E, Mulvaney C, Grainge M, Stanton W, Sayal K: How effective are drug treatments for children with ADHD at improving on-task behaviour and academic achievement in the school classroom? A systematic review and meta-analysis. Eur Child Adolesc Psychiatry 22:203–216, 2013 [DOI] [PubMed] [Google Scholar]
- Rainbow Educational Media (Producer): Plants: A First Look [Motion picture]. Evanston, IL, United Learning, 2001a [Google Scholar]
- Rainbow Educational Media (Producer): Solids Liquids, Gases: A First Look [Motion picture]. Evanston, IL, United Learning, 2001b [Google Scholar]
- Rapport MD, Bolden J, Kofler MJ, Sarver DE, Raiker JS, Alderson RM: Hyperactivity in boys with attention-deficit/hyperactivity disorder (ADHD): A ubiquitous core symptom or manifestation of working memory deficits? J Abnorm Child Psychol 37:521–534, 2009 [DOI] [PubMed] [Google Scholar]
- Rapport MD, Denney C, DuPaul GJ, Gardner MJ: Attention deficit disorder and methylphenidate: Normalization rates, clinical effectiveness, and response prediction in 76 children. J Am Acad Child Adolesc Psychiatry 33:882–893, 1994 [DOI] [PubMed] [Google Scholar]
- Sarver DE, Rapport MD, Kofler MJ, Raiker JS, Friedman LM: Hyperactivity in attention-deficit/hyperactivity disorder (ADHD): Impairing deficit or compensatory behavior? J Abnorm Child Psychol 43:1219–1232, 2015 [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME: NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry 39:28–38, 2000 [DOI] [PubMed] [Google Scholar]
- Tannock R, Ickowicz A, Schachar R: Differential effects of methylphenidate on working memory in ADHD children with and without comorbid anxiety. J Am Acad Child Adolesc Psychiatry 34:886–896, 1995 [DOI] [PubMed] [Google Scholar]
- Tannock R, Purvis KL, Schachar RJ: Narrative abilities in children with attention deficit hyperactivity disorder and normal peers. J Abnorm Child Psychol 21:103–117, 1993 [DOI] [PubMed] [Google Scholar]
- Vile Junod RE, DuPaul GJ, Jitendra AK, Volpe RJ, Cleary KS: Classroom observations of students with and without ADHD: Differences across types of engagement. J Sch Psychol 44:87–104, 2006 [Google Scholar]
- Wehmeier PM, Schacht A, Barkley RA: Social and emotional impairment in children and adolescents with ADHD and the impact on quality of life. J Adolesc Health 46:209–217, 2010 [DOI] [PubMed] [Google Scholar]
- Wigal SB, Wigal T, Schuck S, Brams M, Williamson D, Armstrong RB, Starr HL: Academic, behavioral, and cognitive effects of OROS® methylphenidate on older children with ADHD. J Child Adolesc Psychopharmacol 21:121–131, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolraich ML, Feurer ID, Hannah JN, Baumgaertel A, Pinnock TY: Obtaining systematic teacher reports of disruptive behavior disorders utilizing DSM-IV. J Abnorm Child Psychol 26:141–152, 1998 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.