Abstract
(1) Background: Community pharmacy personnel help mitigate risks of self-care by consumers who seek over-the-counter (OTC) medicines or treatment of symptoms and/or conditions. Exchange of information facilitates the OTC consultation, but pharmacy personnel often report difficulties in engaging consumers in a dialogue. The aim of this study was to describe the development of a behaviour change intervention to enhance information exchange between pharmacy personnel and consumers during OTC consultations in community pharmacies. (2) Methods: The Behaviour Change Wheel methodological framework was used to link factors that influence consumer engagement with information exchange during OTC consultations with intervention functions to change behaviour. Options generated were rationalized and the final intervention strategy was derived. (3) Results: Education, persuasion, environmental restructuring, and modelling were determined to be potential intervention functions. The intervention incorporated placing situational cues in the form of posters in the community pharmacy modelling information exchange behaviour, persuading through highlighting the benefits of exchanging information and educating about its importance. (4) Conclusions: A systematic, theoretically underpinned approach was applied to develop candidate interventions to promote information exchange in OTC consultations. The feasibility and efficacy of the intervention strategy has since been tested and will be reported elsewhere.
Keywords: communication, nonprescription drugs, pharmacists, community pharmacy services, behaviour change, health behaviour
1. Introduction
Community pharmacy personnel manage over-the-counter (OTC) enquiries every day [1,2], which include requests for named OTC medicines as well as the treatment of symptoms and/or conditions [3,4]. Consumers are becoming increasingly confident in self-managing minor ailments by using information from a variety of sources, such as the internet, to self-diagnose and select medicines they view to be appropriate [5,6]. This is facilitated by the wide range of OTC medicines available from community pharmacies in many countries, which require varying levels of involvement by pharmacy personnel, depending on the legal classification and regulation [7,8,9]. Furthermore, community pharmacies are accessible, often with extended opening hours, and without the need to book an appointment to see a pharmacist [10,11,12,13].
Benefits of consumers in engaging with self-care for minor ailments include convenience, and time and cost savings [6,14]. However, there is a risk that consumers could misdiagnose their condition(s), resulting in delays in initiating appropriate treatment [6,14]. Consumers may also underestimate the risks of OTC medicines, which could result in adverse effects [15,16,17,18,19]. Pharmacy personnel play an important role in mitigating the risks associated with self-care. Community pharmacists are qualified to manage the complexity of OTC enquiries in the community pharmacy setting by engaging with consumers in a consultation [20,21,22]. Gathering information from consumers about the symptom or condition, the person’s medical history and medicines, and their treatment goals, assists pharmacists in providing appropriate recommendations [2,23]. Many factors influence information exchange during OTC consultations, including the communication skills of pharmacy personnel, consumer expectation to purchase an OTC medicine without needing to answer questions, privacy, and the legal classification of the medicine [24,25,26,27,28,29,30,31,32,33,34,35,36,37].
Pharmacists and pharmacy personnel often report difficulties in engaging consumers in a dialogue, particularly when the request is for a specific medicine by name [25,27,38,39,40]. OTC consultations ideally should involve two-way communication “between the pharmacist and the patient in which the pharmacist ascertains the needs of the patient and provides them with information required to effectively use medicines and/or therapeutic devices” [20] (p. 50). This interaction requires clinical knowledge and reasoning, as well as effective communication. There is substantial evidence, however, that the management of the diverse range of OTC enquiries encountered in community pharmacies is sub-optimal, and that this is mainly due to inadequate information gathering and/or advice or information provision by pharmacy personnel [1,26,27,28,29,31,32,41,42,43,44,45,46]. While there has been a number of interventions to improve the exchange of information between pharmacy personnel and consumers, with varying levels of success [47], there are also studies which show that pharmacy personnel are not complying with appropriate standards [26,29,41,42,43,45].
The aim of this study was to describe the development of a behaviour change intervention to enhance information exchange between pharmacy personnel and consumers during OTC enquiries in community pharmacies.
2. Materials and Methods
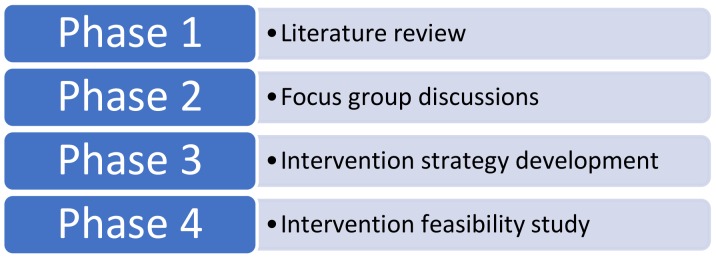
This study was the third phase of a larger project with the aim of enhancing the quality management of OTC consultations in community pharmacies (Figure 1).
Figure 1.
Project phases.
In the first phase, a systematic literature review identified interventions targeted towards improving communication between consumers and pharmacy personnel during OTC consultations in the community pharmacy setting [47]. Focus group discussions were then conducted to determine pharmacist, non-pharmacist pharmacy personnel and consumer perspectives regarding barriers and facilitators for information exchange during OTC consultations in community pharmacies [39]. The results from the first two phases identified that to enhance information exchange between pharmacy personnel and consumers during OTC enquiries, consumers needed to engage with the process. The methodology described in the Behaviour Change Wheel (BCW) [48] was subsequently used to develop an intervention strategy to target this behaviour.
Underpinning Theory
The BCW is a validated methodological framework developed from the synthesis of 19 behaviour change frameworks to assist researchers to apply the COM-B (Capability Opportunity Motivation—Behaviour) model of behaviour in any setting to develop an intervention strategy. The BCW identifies sources of behaviour in terms of the complex interactions between capability, opportunity and motivation.
The Theoretical Domains Framework (TDF) [49] was also applied in this study. The TDF is a validated derivation of the COM-B which identifies 14 domains that determine behaviour. In Table 1, the TDF domains are linked to source behaviours of COM-B. An analysis using TDF provides a more detailed understanding of determinants of behaviour from which an intervention strategy can be developed.
Table 1.
Capability, opportunity, motivation–behaviour model (COM-B) linked with the Theoretical Domains Framework (TDF) domains.
| COM-B Source Behaviour | TDF Domain |
|---|---|
| CAPABILITY | Skills (Cognitive and interpersonal; Physical) |
| Knowledge | |
| Memory, attention and decision processes | |
| Behavioural regulation | |
| OPPORTUNITY | Social influences |
| Environmental context and resources | |
| MOTIVATION | Social and professional role and identity |
| Belief about capabilities | |
| Optimism | |
| Belief about consequences | |
| Intentions | |
| Goals | |
| Reinforcement | |
| Emotion |
The BCW describes interventions in terms of nine functions: (i) education, (ii) persuasion, (iii) incentivisation, (iv) coercion, (v) training, (vi) restriction, (vii) environmental restructuring, (viii) modelling and (ix) enablement. A function of an intervention is an aspect of the intervention that influences behaviour. The BCW links intervention functions with behaviour change techniques (BCTs), which are the active components that can be used in the intervention strategy [50]. The BCTs are assessed against the APEASE (Affordability, Practicability, Effectiveness and cost effectiveness, Acceptability, Side-effects/safety, Equity) [51] criteria and to enable decisions on intervention content and delivery that are within the scope of the study.
In Phase 3, a 2-stage process was used to develop the intervention. In Stage 1, to fully understand the target behaviour, an independent duplicate (LS, KW) behavioural ‘diagnosis’ of consumer engagement with information exchange during OTC consultations was conducted, using themes from the focus groups undertaken in Phase 2 [39]. The researchers coded focus group themes to the COM-B model and TDF. The results were discussed with a psychologist experienced in pharmacy practice (L. Smith, see Acknowledgments) until consensus was reached. Independent duplicate (LS, KW) mapping of the key factors that influenced this behaviour to intervention functions and BCTs [48] was conducted (Stage 2). Disagreements were resolved by consensus and involvement of a third researcher, when required (RC). Options for the intervention were generated by the research team (LS, KW, LH, MW, RC) then rationalised (LS, KW) through assessment against the APEASE criteria [51] and discussion. The final intervention strategy was decided by consensus (LS, KW, LH, MW, RC).
3. Results
3.1. Stage 1: Behavioural Analysis
A behavioural diagnosis on the target behaviour, as described in the BCW and resulting COM-B and TDF coded themes from Phase 2 focus group discussions, was conducted (Table 2).
Table 2.
Behavioural diagnosis using themes from focus group meetings.
| Target Behaviour: Consumer Engaging in Information Exchange. | |||
|---|---|---|---|
| COM-B and TDF * | Barrier | Is There a Need for Change? | Intervention Function |
| PSYCHOLOGICAL CAPABILITY | |||
|
Knowledge (An awareness of the existence of something) [52] |
Consumers did not understand the role and responsibilities of pharmacists. |
√ | Education |
| Consumers did not understand the qualifications of pharmacists. | √ | ||
| Consumers did not understand the risks of medicine use. | √ Consumers do not perceive risks with OTC medicines. Consumers believe medicines available without prescription are safe. | ||
|
Cognitive and interpersonal skills (An ability or proficiency acquired through practice) [52] |
Pharmacy personnel consultation & communication skills | Improving these skills may improve interactions. | Training |
| PHYSICAL OPPORTUNITY | |||
|
Environmental context and resources (Any circumstance of a person’s situation or environment that discourages or encourages the development of skills and abilities, independence, social competence, and adaptive behaviour) [52] |
Privacy is required for conversations. | √ Discussing health can be a sensitive issue. | Training Restriction Environmental restructuring Enablement |
| Pharmacy personnel should have time to engage in interactions | √ | ||
| Pharmacists were not always identifiable | √ | ||
| Appropriate remuneration for pharmacist consultations is required | √ | ||
| The environment should look like a professional/healthcare setting | Potentially yes. Some community pharmacies are very retail/warehouse/discount oriented. | ||
| The OTC consultation area is not always clearly identifiable | √ | ||
| REFLECTIVE MOTIVATION | |||
|
Social and professional role and identity (A coherent set of behaviours and displayed personal qualities of an individual in a social or work setting) [52] |
Consumers did not trust the person asking questions | √ Consumers do not know the role of the pharmacist | Education Persuasion Modelling |
| Service between pharmacies and personnel is not consistent so consumers did not know what to expect | √ | ||
|
Belief about capabilities (Acceptance of the truth, reality, or validity about an ability, talent, or facility that a person can put to constructive use) [52] |
Consumers believed they are able to appropriately self-asses their condition before consultation | √ | Education Persuasion Modelling Enablement |
| Consumers did not believe pharmacy personnel were able to help with OTC enquiries | √ | ||
|
Belief about consequences (Acceptance of the truth, reality, or validity regarding outcomes of a behaviour in a given situation) [52] |
Consumers did not understand the risks of medicine use | √ Consumers engage in information exchange if they ask about a symptom but not if they ask for a specific product | Education Persuasion Modelling |
| Consumers did not know that being asked questions is for their benefit | √ | ||
| Consumers did not know that their consultation information will be kept confidential | √ Consumers do not know that pharmacy personnel are bound by privacy laws | ||
|
Intentions (A conscious decision to perform a behaviour or a resolve to act in a certain way) [52] |
Consumers expected to purchase an OTC product without exchanging information | √ | Education Persuasion Incentivisation Coercion Modelling |
| Consumers expected to answer questions if asking about a symptom | √ | ||
| Consumers resisted information exchange if repeatedly requesting the same product | √ | ||
| AUTOMATIC MOTIVATION | |||
|
Reinforcement (Increasing the probability of a response by arranging a dependent relationship, or contingency, between the response and a given stimulus) [52] |
Consumers did not feel it necessary to be asked questions (not from focus group but an observation of the research group) |
√ If consumers exchange information and have a positive outcome as a result, this will subconsciously encourage information exchange behaviours in future consultations. | Training Incentivisation Coercion Environmental restructuring |
| Behavioural diagnosis of the relevant COM-B components | Psychological capability, physical opportunity, reflective and automatic motivation need to change in order for the target behaviour “consumer engaging in information exchange” to occur. | ||
* COM-B: Capability Opportunity Motivation—Behaviour model of behaviour; TDF: Theoretical Domains Framework.
3.2. Stage 2: Identify Intervention Options, Content and Implementation Options
Education, persuasion, environmental restructuring, and modelling were determined to be potential intervention functions (Table 3) that met the APEASE criteria.
Table 3.
Linking intervention functions to Behaviour Change Techniques (BCTs).
| Intervention Function | BCTs Identified to Enable Delivery of the Intervention Function | BCT Examples |
|---|---|---|
| Education |
|
Explain the role and responsibilities of the pharmacist. Explain the qualifications of the pharmacist. Explain the risks of OTC medicine use. Explain the confidentiality of personal information. |
| Persuasion |
|
Inform consumers about positive health consequences from information exchange. |
| Environmental restructuring |
|
Pharmacy personnel to wear badges identifying their role. Provide cues/prompts for engaging in information exchange. |
| Modelling |
|
Demonstrate the type of questions that might be asked. |
The BCTs identified to be able to deliver the four intervention functions are listed in Table 3 with examples of BCTs to address identified barriers.
3.3. Intervention Strategy
The research team discussed the results of the analysis and developed the intervention. Situational cues, in the form of a poster displayed in a community pharmacy (environmental restructuring), depicting consumers with OTC enquiries engaging in information exchange (modelling), highlighting the benefit of this behaviour (persuasion) and the reasons why it is important (education), were identified as the most appropriate intervention. A second poster depicting a pharmacist and information about the qualifications and role of a pharmacist was developed. An additional situational cue, in the form of a badge, was developed to be worn by pharmacy personnel to identify their position as either pharmacist or pharmacy assistant.
4. Discussion
This study described the development of an intervention strategy to enhance information exchange during OTC consultations. With the growing trend for self-care and the empowerment of consumers to make health decisions, it is essential that their safety is protected through the expertise available from pharmacists and other pharmacy personnel.
A systematic, theory-based approach was undertaken to fully understand the key components impacting information exchange.
The target of most interventions to date has been pharmacy personnel, with varying degrees of success [47]. Interventions targeting consumers have been neglected [47]. Through the systematic process, the behaviour of interest was identified to be information exchange and the consumer’s engagement in information exchange was determined to be the target as there was a scarcity of interventions directed at the consumer.
The scope of this study was to derive an intervention to promote information exchange. The strength of this study lies in using a rigorously developed theory-based methodology for the systematic development of an intervention. The steps involved in the intervention development are described in detail, therefore making it reproducible.
5. Conclusions
A systematic, theoretically underpinned approach was applied to candidate interventions to promote information exchange in OTC consultations. The feasibility and efficacy of the intervention has since been tested and will be reported elsewhere.
Acknowledgments
The authors would like to thank Lorraine Smith for her assistance with understanding behaviours.
Author Contributions
Conceptualization: L.J.S., L.H., M.C.W. and R.M.C.; methodology: L.J.S. and K.W.; writing original draft: L.J.S.; review and editing of manuscript: K.W., L.H., M.C.W. and R.M.C.
Funding
This research was funded by the Pharmaceutical Society of Western Australia J.M. O’Hara grant. MW was funded by the Health Foundation Improvement Science Fellowship.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Collins J.C., Schneider C.R., Faraj R., Wilson F., De Almeida Neto A.C., Moles R.J. Management of common ailments requiring referral in the pharmacy: A mystery shopping intervention study. Int. J. Clin. Pharm. 2017;39:697–703. doi: 10.1007/s11096-017-0505-8. [DOI] [PubMed] [Google Scholar]
- 2.Blenkinsopp A., Paxton P., Blenkinsopp J. Symptoms in the Pharmacy: A Guide to the Management of Common Illness. 6th ed. Blackwell Publishing Ltd.; Oxford, UK: 2009. [Google Scholar]
- 3.Boardman H., Lewis M., Croft P., Trinder P., Rajaratnam G. Use of community pharmacies: A population-based survey. J. Public Health. 2005;27:254–262. doi: 10.1093/pubmed/fdi032. [DOI] [PubMed] [Google Scholar]
- 4.Benrimoj S.I., Frommer M.S. Community pharmacy in Australia. Aust. Health Rev. 2004;28:238–246. doi: 10.1071/AH040238. [DOI] [PubMed] [Google Scholar]
- 5.Hibbert D., Bissell P., Ward P.R. Consumerism and professional work in the community pharmacy. Sociol. Health Illn. 2002;24:46–65. doi: 10.1111/1467-9566.00003. [DOI] [Google Scholar]
- 6.Hughes C.M., McElnay J.C., Fleming G.F. Benefits and risks of self medication. Drug Saf. 2001;24:1027–1037. doi: 10.2165/00002018-200124140-00002. [DOI] [PubMed] [Google Scholar]
- 7.Therapeutic Goods Administration Reasons for Scheduling Delegate’s Final Decisions, June 2017. [(accessed on 29 August 2017)]; Available online: https://www.tga.gov.au/scheduling-decision-final/scheduling-delegates-final-decisions-june-2017.
- 8.Association of the European Self-Medication Industry. [(accessed on 24 October 2017)]; Available online: http://www.aesgp.eu/facts-figures/otc-ingredients/#undefined.
- 9.US Food and Drug Administration What Are Over-the-Counter (OTC) Drugs and How Are They Approved? [(accessed on 23 October 2017)]; Available online: https://www.fda.gov/aboutfda/transparency/basics/ucm194951.htm.
- 10.Khdour M.R., Hallak H.O. Societal perspectives on community pharmacy services in West Bank—Palestine. Pharm Pract. 2012;10:17–24. doi: 10.4321/S1886-36552012000100004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Todd A., Copeland A., Husband A., Kasim A., Bambra C. Access all areas? An area-level analysis of accessibility to general practice and community pharmacy services in England by urbanity and social deprivation. BMJ Open. 2015;5 doi: 10.1136/bmjopen-2014-007328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paola S. “Convenience and Accessibility” An Evaluation of the First Pharmacist-Administered Vaccinations in WA Has Shown Positive Results for Patient and Practitioner. [(accessed on 24 October 2018)]; Available online: https://ajp.com.au/news/providing-convenience-accessibility/
- 13.Lam B. How to Increase the Accessibility of Pharmacists When the Pharmacy Is Open. [(accessed on 8 December 2017)]; Available online: http://www.pharmaceutical-journal.com/news-and-analysis/event/how-to-increase-the-accessibility-of-pharmacists-when-the-pharmacy-is-open/20066487.article.
- 14.Bennadi D. Self-medication: A current challenge. J. Basic Clin. Pharm. 2014;5:19–23. doi: 10.4103/0976-0105.128253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fielding S., Slovic P., Johnston M., Lee Amanda J., Bond Christine M., Watson Margaret C. Public risk perception of non-prescription medicines and information disclosure during consultations: A suitable target for intervention? Int. J. Pharm. Pract. 2018 doi: 10.1111/ijpp.12433. [DOI] [PubMed] [Google Scholar]
- 16.Roumie C., Griffin M.R. Over-the-counter analgesics in older adults—A call for improved labelling and consumer education. Drugs Aging. 2004;21:485–498. doi: 10.2165/00002512-200421080-00001. [DOI] [PubMed] [Google Scholar]
- 17.Calamusa A., Di Marzio A., Cristofani R., Arrighetti P., Santaniello V., Alfani S., Carducci A. Factors that influence Italian consumers’ understanding of over-the-counter medicines and risk perception. Patient Educ. Couns. 2012;87:395–401. doi: 10.1016/j.pec.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 18.Stosic R., Dunagan F., Palmer H., Fowler T., Adams I. Responsible self-medication: Perceived risks and benefits of over-the-counter analgesic use. Int. J. Pharm. Pract. 2011;19:236–245. doi: 10.1111/j.2042-7174.2011.00097.x. [DOI] [PubMed] [Google Scholar]
- 19.Mullan J., Weston Kathryn M., Bonney A., Burns P., Mullan J., Rudd R. Consumer knowledge about over-the-counter NSAIDs: They don’t know what they don’t know. Aust. N. Z. J. Public Health. 2017;41:210–214. doi: 10.1111/1753-6405.12589. [DOI] [PubMed] [Google Scholar]
- 20.Pharmaceutical Society of Australia . Professional Practice Standards—Version 5—2017. Pharmaceutical Society of Australia; Deakin West, Australia: 2017. [Google Scholar]
- 21.Pharmaceutical Society of Australia . National Competency Standards Framework for Pharmacists in Australia 2016. Pharmaceutical Society of Australia; Deakin West, Australia: 2016. [Google Scholar]
- 22.Bell J., Dziekan G., Pollack C., Mahachai V. Self-Care in the twenty first century: A vital role for the pharmacist. Adv. Ther. 2016;33:1691–1703. doi: 10.1007/s12325-016-0395-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organisation The Role of the Pharmacist in Self-Care and Self-Medication. 4th WHO Consultative Group on the Role of the Pharmacist, Ed. [(accessed on 14 September 2017)];1998 Available online: http://apps.who.int/medicinedocs/en/d/Jwhozip32e/#Jwhozip32e.
- 24.Watson M.C., Johnston M., Entwistle V., Lee A.J., Bond C.M., Fielding S. Using the theory of planned behaviour to develop targets for interventions to enhance patient communication during pharmacy consultations for non-prescription medicines. Int. J. Pharm. Pract. 2014;22:386–396. doi: 10.1111/ijpp.12095. [DOI] [PubMed] [Google Scholar]
- 25.Watson M.C., Cleland J.A., Bond C.M. Simulated patient visits with immediate feedback to improve the supply of over-the-counter medicines: A feasibility study. Fam. Pract. 2009;26:532–542. doi: 10.1093/fampra/cmp061. [DOI] [PubMed] [Google Scholar]
- 26.Watson M., Bond C., Grimshaw J., Johnston M. Factors predicting the guideline compliant supply (or non-supply) of non-prescription medicines in the community pharmacy setting. Qual. Saf. Health Care. 2006;15:53–57. doi: 10.1136/qshc.2005.014720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berger K., Eickhoff C., Schulz M. Counselling quality in community pharmacies: Implementation of the pseudo customer methodology in Germany. J. Clin. Pharm. Ther. 2005;30:45–57. doi: 10.1111/j.1365-2710.2004.00611.x. [DOI] [PubMed] [Google Scholar]
- 28.Rutter P.M., Horsley E., Brown D.T. Evaluation of community pharmacists’ recommendations to standardized patient scenarios. Ann. Pharmacother. 2004;38:1080–1085. doi: 10.1345/aph.1D519. [DOI] [PubMed] [Google Scholar]
- 29.Watson M.C., Hart J., Johnston M., Bond C.M. Exploring the supply of non-prescription medicines from community pharmacies in Scotland. Pharm. World Sci. 2008;30:526–535. doi: 10.1007/s11096-008-9202-y. [DOI] [PubMed] [Google Scholar]
- 30.Krishnan H.S., Schaefer M. Evaluation of the impact of pharmacist’s advice giving on the outcomes of self-medication in patients suffering from dyspepsia. Pharm. World Sci. 2000;22:102–108. doi: 10.1023/A:1008733207854. [DOI] [PubMed] [Google Scholar]
- 31.Schneider C.R., Everett A.W., Geelhoed E., Kendall P.A., Murray K., Garnett P., Salama M., Clifford R.M. Provision of primary care to patients with chronic cough in the community pharmacy setting. Ann. Pharmacother. 2011;45:402–408. doi: 10.1345/aph.1P514. [DOI] [PubMed] [Google Scholar]
- 32.Schneider C.R., Everett A.W., Geelhoed E., Padgett C., Ripley S., Murray K., Kendall P.A., Clifford R.M. Intern pharmacists as change agents to improve the practice of nonprescription medication supply: Provision of salbutamol to patients with asthma. Ann. Pharmacother. 2010;44:1319–1326. doi: 10.1345/aph.1P142. [DOI] [PubMed] [Google Scholar]
- 33.Queddeng K., Chaar B., Williams K. Emergency contraception in Australian community pharmacies: A simulated patient study. Contraception. 2011;83:176–182. doi: 10.1016/j.contraception.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 34.Kippist C., Wong K., Bartlett D., Bandana S. How do pharmacists respond to complaints of acute insomnia? A simulated patient study. Int. J. Clin. Pharm. 2011;33:237–245. doi: 10.1007/s11096-011-9482-5. [DOI] [PubMed] [Google Scholar]
- 35.Kelly F.S., Williams K.A., Benrimoj S.I. Does advice from pharmacy staff vary according to the nonprescription medicine requested? Ann. Pharmacother. 2009;43:1877–1886. doi: 10.1345/aph.1L121. [DOI] [PubMed] [Google Scholar]
- 36.Watson M.C., Bond C.M., Grimshaw J.M., Mollison J., Ludbrook A., Walker A.E. Educational strategies to promote evidence-based community pharmacy practice: A cluster randomized controlled trial. Fam. Pract. 2002;19:529–536. doi: 10.1093/fampra/19.5.529. [DOI] [PubMed] [Google Scholar]
- 37.Watson M.C., Bond C.M. The evidence-based supply of non-prescription medicines: Barriers and beliefs. Int. J. Pharm. Pract. 2004;12:65–72. doi: 10.1211/0022357023475. [DOI] [PubMed] [Google Scholar]
- 38.Kaae S., Saleem S., Kristiansen M. How do Danish community pharmacies vary in engaging customers in medicine dialogues at the counter—An observational study. Pharm Pract. (Granada) 2014;12:422. doi: 10.4321/S1886-36552014000300006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Seubert L.J., Whitelaw K., Boeni F., Hattingh L., Watson M.C., Clifford R.M. Barriers and facilitators for information exchange during over-the-counter consultations in community pharmacy: A focus group study. Pharmacy. 2017;5:65. doi: 10.3390/pharmacy5040065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hanna L.-A., Hughes C. ‘First, do no harm’: Factors that influence pharmacists making decisions about over-the-counter medication. Drug Saf. 2010;33:245–255. doi: 10.2165/11319050-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 41.Watson M.C., Bond C.M., Johnston M., Mearns K. Using human error theory to explore the supply of nonprescription medicines from community pharmacies. Qual. Saf. Health Care. 2006;15:244–250. doi: 10.1136/qshc.2005.014035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schneider C.R., Everett A.W., Geelhoed E., Kendall P.A., Clifford R.M. Measuring the assessment and counselling provided with the supply of non-prescription asthma reliever medication: A simulated patient study. Ann. Pharmacother. 2009;43:1512–1518. doi: 10.1345/aph.1M086. [DOI] [PubMed] [Google Scholar]
- 43.Schneider C.R., Emery L., Brostek R., Clifford R.M. Evaluation of the supply of antifungal medication for the treatment of vaginal thrush in the community pharmacy setting: A randomized controlled trial. Pharm. Pract. (Granada) 2013;11:132–137. doi: 10.4321/S1886-36552013000300002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Benrimoj S.I., Werner J.B., Raffaele C., Roberts A.S., Costa F.A. Monitoring quality standards in the provision of non-prescription medicines from Australian Community Pharmacies: Results of a national programme. Qual. Saf. Health Care. 2007;16:354–358. doi: 10.1136/qshc.2006.019463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schneider C.R., Gudka S., Fleischer L., Clifford R.M. The use of a written assessment checklist for the provision of emergency contraception via community pharmacies: A simulated patient study. Pharm. Pract. 2013;11:127–131. doi: 10.4321/S1886-36552013000300001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Watson M.C., Cleland J., Inch J., Bond C.M., Francis J. Theory-based communication skills training for medicine counter assistants to improve consultations for non-prescription medicines. Med. Educ. 2007;41:450–459. doi: 10.1111/j.1365-2929.2007.02723.x. [DOI] [PubMed] [Google Scholar]
- 47.Seubert L.J., Whitelaw K., Hattingh L., Watson M.C., Clifford R.M. Interventions to enhance effective communication during over-the-counter consultations in the community pharmacy setting: A systematic review. Res. Soc. Adm. Pharm. 2017 doi: 10.1016/j.sapharm.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 48.Michie S., Atkins L., West R. The Behaviour Change Wheel. A Guide to Designing Interventions. 1st ed. Silverback Publishing; Great Britain, UK: 2014. [Google Scholar]
- 49.Atkins L., Francis J., Islam R., O’Connor D., Patey A., Ivers N., Foy R., Duncan E.M., Colquhoun H., Grimshaw J.M., et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement. Sci. 2017;12:77. doi: 10.1186/s13012-017-0605-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Michie S., Johnston M. Behavior Change Techniques. In: Gellman M.D., Turner J.R., editors. Encyclopedia of Behavioral Medicine. Springer; New York, NY, USA: 2013. pp. 182–187. [Google Scholar]
- 51.Michie S., van Stralen M., West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011;6 doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cane J., O’Connor D., Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement. Sci. 2012;7 doi: 10.1186/1748-5908-7-37. [DOI] [PMC free article] [PubMed] [Google Scholar]