Abstract
A systematic review and network meta-analysis (NMA) of randomized controlled trials (RCTs) evaluating the core components of cardiac rehabilitation (CR), nutritional counseling (NC), risk factor modification (RFM), psychosocial management (PM), patient education (PE), and exercise training (ET)) was undertaken. Published RCTs were identified from database inception dates to April 2017, and risk of bias assessed using Cochrane’s tool. Endpoints included mortality (all-cause and cardiovascular (CV)) and morbidity (fatal and non-fatal myocardial infarction (MI), coronary artery bypass surgery (CABG), percutaneous coronary intervention (PCI), and hospitalization (all-cause and CV)). Meta-regression models decomposed treatment effects into the main effects of core components, and two-way or all-way interactions between them. Ultimately, 148 RCTs (50,965 participants) were included. Main effects models were best fitting for mortality (e.g., for all-cause, specifically PM (hazard ratio HR = 0.68, 95% credible interval CrI = 0.54–0.85) and ET (HR = 0.75, 95% CrI = 0.60–0.92) components effective), MI (e.g., for all-cause, specifically PM (hazard ratio HR = 0.76, 95% credible interval CrI = 0.57–0.99), ET (HR = 0.75, 95% CrI = 0.56–0.99) and PE (HR = 0.68, 95% CrI = 0.47–0.99) components effective) and hospitalization (e.g., all-cause, PM (HR = 0.76, 95% CrI = 0.58–0.96) effective). For revascularization (including CABG and PCI individually), the full interaction model was best-fitting. Given that each component, individual or in combination, was associated with mortality and/or morbidity, recommendations for comprehensive CR are warranted.
Keywords: coronary heart disease, cardiac rehabilitation, systematic review
1. Introduction
Coronary heart disease (CHD) is one of the most prevalent health conditions globally [1], with an estimate of 422 million prevalent cases in 2015 [2]. Cardiac rehabilitation (CR) is designed to optimize secondary prevention of CHD [3,4]. Reviews have established that CR participation is associated with approximately 20% lower cardiovascular mortality and morbidity [5].
CR has evolved from an exercise-focused program, to a comprehensive, multi-component model of care to address all CHD risk factors [6]. Indeed, learned CR societies have published statements listing the so-called “core components” of CR [3,4,7,8,9,10], to promote delivery of all evidence-based secondary prevention recommendations [11]. These have been internationally agreed through the International Council of Cardiovascular Prevention and Rehabilitation [12], namely, nutritional counseling (NC), risk factor modification (RFM), psychosocial management (PM), patient education (PE), and exercise training (ET).
A recent meta-analysis demonstrated that CR programs offering more core components achieved greater reductions in all-cause mortality than those offering less [11]. However, reviews of the effectiveness of CR to date have not considered the impact of the individual components (except exercise). Expert recommendations to deliver each core component should be tested [12], in such a way that the “complexity” of CR can be considered and to ensure there is evidence to support delivery of each component [13]. Clearly, delivery of comprehensive CR requires more human and financial resources, and thus only those components with impact should be offered. Accordingly, the objective of this review was to evaluate the comparative effectiveness of the core components of CR on mortality and morbidity, considering main and multiplicative impacts.
2. Methods
The systematic review was undertaken with consideration of the Cochrane Handbook guidelines [14] and reported in compliance with the extension Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement for Network meta-analysis (NMA) [15,16]. NMA was used to test the comparative effectiveness of the 5 CR components.
2.1. Information Sources and Search Strategy
Studies were identified through a systematic, comprehensive search of the following databases from inception through 27 April 2017: MEDLINE (Ovid), EMBASE (Ovid), CINHAL (Ebsco), PsycINFO (Ovid), Cochrane Database of Systematic Reviews (CDSR), Cochrane Central Register of Controlled Trials (Cochrane Central); Web of Science (SCI-EXPANDED, SSCI, CPCI-S, CPCI-SSH). Reference lists of systematic reviews and meta-analyses identified through the search were screened for additional potentially-eligible trials.
The search strategy was designed, and search undertaken, by an information specialist experienced in systematic reviews (J.M.B.) following the Cochrane systematic review methodology [14]. It included controlled vocabulary (MeSH) and natural language terms in the following concept areas: myocardial ischemia, health education, psychotherapy, smoking cessation and synonyms. No date or language limits were applied. A detailed search strategy for MEDLINE (Ovid) is provided in Supplemental File 1. The final Medline strategy was translated into syntax appropriate for each database used.
2.2. Inclusion and Exclusion Criteria
Randomized controlled trials (RCTs) evaluating any combination of the core components of CR were eligible for inclusion. Participants were adults who had had a myocardial infarction (MI; including MI with non-obstructive coronary arteries or cardiac syndrome X), or who had undergone revascularization (coronary artery bypass grafting (CABG), percutaneous coronary intervention (PCI)), or whom had angina pectoris or coronary artery disease established by angiography.
Studies had to include at least one of the core components of CR [4], namely NC, RFM (≥2 of dyslipidemia, hypertension, obesity, diabetes, and/or smoking), PM (e.g., stress management, social support, psychotherapy), PE (may include lifestyle counseling), ET (including at least some form of aerobic exercise), or any combination thereof [4,17]. Usual Care (UC) could include standard medical care, such as evidence-based medications at the time of randomization, but participants could not be randomized to drug therapy or to surgery.
Studies also had to report mortality or morbidity outcomes, assessed after six or more months of follow-up. The co-primary outcomes were all-cause and cardiovascular (CV) mortality. Secondary pre-specified outcomes were total MI, fatal MI, non-fatal MI, total revascularization, CABG, PCI, as well as all-cause and CV hospitalization.
Studies of patients participating in CR following heart valve surgery, heart failure, heart transplants or implanted with either cardiac resynchronization therapy or implantable defibrillators solely were excluded. Studies of participants who completed a CR program prior to randomization, who were randomized participants prior to cardiovascular surgery, or evaluated the same CR components in both arms were excluded (e.g., the only difference was the setting or type of nutritional intervention), as were non-English studies.
2.3. Study Selection
Two investigators (N.N.K., T.A.F. or G.C.) first independently reviewed the titles and abstracts of all identified citations. Full-texts of potentially-eligible citations were then similarly considered to establish whether they met the inclusion criteria. Finally, 2 investigators also searched the reference lists of relevant reviews and included studies. Any disagreements were resolved by consensus or consultation with another author (S.L.G.) at each stage of the review.
2.4. Data Extraction Process and Quality Assessment
Using a standardized data abstraction sheet, two investigators (N.N.K., T.A.F. or G.C.) also independently extracted the data for each included study (i.e., components in each arm and outcomes; the former were checked by S.L.G.), and independently assessed the risk of bias using the Cochrane assessment tool [18]. Blinding was deemed complete when outcome assessors were masked. Patient blinding was not deemed to be relevant because of the nature of the interventions.
2.5. Data Synthesis and Analysis
Each study arm was characterized by the combination of the 5 core components of CR delivered in that arm. A Bayesian random-effects NMA model was computed, in which the differences in outcomes between arms in a study were expressed as a function of their core components—An approach developed for complex interventions [19]. The model accounted for the correlation of treatment effects in trials with more than two arms [20].
Three increasingly complex possibilities were explored for the roles of the core components of CR: (1) a main-effects model, in which the effects of the components were additive; (2) a two-way interaction model, in which effects also depended on pairwise combinations of components; and (3) a full-interaction model, in which each possible combination of the core components had a distinct effect. The best-fitting model was chosen upon consideration of the deviance information criterion (DIC), a measure of model fit that penalizes larger models. As there was variability in the length of follow-up across RCTs (6–300 months), the model linked the probability of an outcome to the predictor variables through the complementary log–log link, with the logarithm of follow-up time as an offset. In the main effects model, the effects of core component are estimated as hazard ratios (HR) for the presence of the component versus its absence.
The effect of the core CR components was estimated for each outcome using Markov chain Monte Carlo (MCMC) implemented in JAGS in R software (version 3.5.1) with the rjags (version 4–6) and R2jags (version 0.5–7) packages. The first 75,000 iterations were discarded, and all results were based on a further sample of at least 75,000 iterations. Four chains with different initial values were run in parallel to assess convergence using the Gelman-Rubin diagnostic statistics and plots. Heterogeneity and model fit were assessed using standard approaches [21,22,23]. Results are presented as posterior medians and 95% central credible intervals (95% CrI). The MCMC simulation framework also allowed for the presentation of other summaries of key clinical and policy interest, such as the probability that a particular core component is most effective for each outcome evaluated. Minimally-informative priors were used for all parameters [19]. Analyses were done in the intention-to-treat populations, with the clinical follow-up period closest to two years.
3. Results
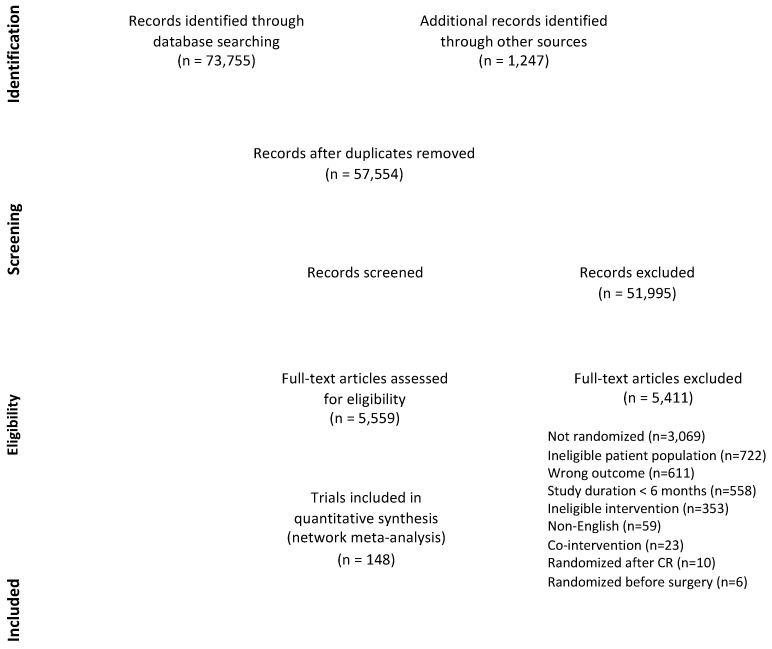
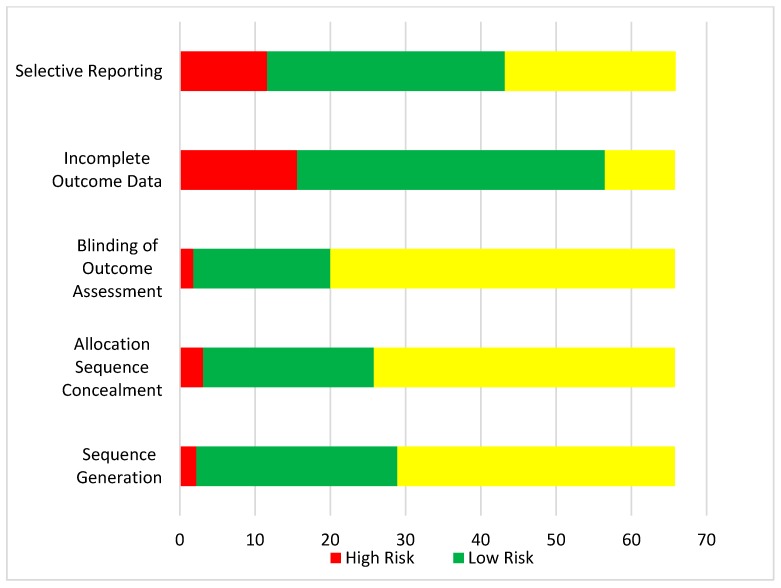
Figure 1 displays the process of study identification and selection. There were 148 RCTs assessing 50,965 participants included in the NMA; citations and characteristics are provided in Supplemental File 2 (References [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171] are cited in the supplementary materials). Risk of bias assessments are shown in Figure 2. Included RCTs were undertaken between 1975 and 2017, most often in the United States (n = 34, 23.0%) and the United Kingdom (n = 16, 10.8%). Three (2.0%) were cluster RCTs [68,106,121].
Figure 1.
Flow Diagram.
Figure 2.
Risk of Bias in Included Trials, N = 148. Note: Blinding was considered low-risk when outcome assessors were masked (i.e., single-blinded). Patient blinding would not be possible given the nature of the interventions.
Characteristics of included RCTs by outcome can be found in Table 1. Overall, 118 (79.7%) RCTs with 44,462 participants reported the primary outcome of all-cause mortality, while 42 (28.4%) RCTs with 16,770 participants reported the other primary outcome of CV mortality. The secondary endpoints were reported in 16–52 RCTs (10.8–35.1%) with 4261–16,947 participants. The mean duration of follow-up was 25.3 months (standard deviation (SD) 34.6 months).
Table 1.
Characteristics of included patients and trial follow-up time by endpoint.
| # | N | Indication (Post-MI %) | Age (Mean Years, SD) | Sex (% male) | Follow-Up (Mean Months, SD) | |
|---|---|---|---|---|---|---|
| All Endpoints | 143 | 69,910 | 55 (37.2%) | 58.7 (6.4) | 83.1 | 36.5 (38.3) |
| Primary Endpoints | ||||||
| All-Cause Mortality | 118 | 44,462 | 50 (90.9%) | 58.9 (6.4) | 85.6 | 37.2 (35.9) |
| CV Mortality | 42 | 16,770 | 21 (38.2%) | 56.9 (6.5) | 92.9 | 47.9 (48.7) |
| Secondary Endpoints | ||||||
| Any MI | 52 | 16,690 | 28 (50.9%) | 55.6 (5.4) | 86.5 | 42.3 (43.7) |
| Fatal MI | 16 | 4261 | 9 (16.4%) | 53.7 (4.5) | 100.0 | 47.7 (51.8) |
| Non-Fatal MI | 31 | 11,919 | 18 (32.7%) | 54.5 (4.3) | 83.9 | 46.2 (47.3) |
| Any Revascularization | 49 | 16,947 | 25 (45.5%) | 56.8 (4.9) | 83.3 | 34.9 (38.9) |
| CABG | 33 | 7391 | 18 (32.7%) | 56.3 (4.9) | 84.4 | 33.0 (38.9) |
| PCI | 23 | 8859 | 10 (18.2%) | 56.8 (4.8) | 87.0 | 27.0 (16.0) |
| Any Hospitalization | 45 | 14,440 | 16 (29.1%) | 59.0 (5.8) | 82.6 | 31.5 (33.5) |
| CV Hospitalization | 24 | 7925 | 10 (18.2%) | 57.6 (4.1) | 88.0 | 28.5 (30.1) |
# = Number of trials reporting endpoint. N = number of patients randomized. SD = standard deviation. CV = cardiovascular. MI = myocardial infarction. CABG = coronary artery bypass surgery. PCI = percutaneous coronary intervention.
The number of RCT arms evaluating each combination of the core components (overall and outcome-specific) can be found in Supplemental File 3. The majority of included RCTs were designed with two arms (n = 142, 95.9%), and six RCTs had three arms. Overall, PE was the most-frequently evaluated individual core component of CR (26 RCT arms), followed by ET (21 RCT arms). The combination of PE and RFM (12 RCT arms) was the most frequently evaluated combination of core components followed by PE and PM (9 RCT arms), the combination of PE and ET (8 RCT arms), and the combination of NC, PE, ET, PM and RMF (8 RCT arms). Usual care (no CR) was evaluated in 75 control RCT arms.
Finally, with regard to participant characteristics in included RCTs (Table 1 and Supplemental File 2), the mean age was 58.7 years (standard deviation (SD) = 6.4) and the mean proportion of males in the trials was 83.1%. Thirty-seven percent of trials (n = 55) included only post-MI patients.
Effects of Core Components
Table 2 shows the model fit statistics for each model considered. For the most part, differences in the DIC between models were small, and where the difference was <2, the simpler model was preferred. The main effects model was the best-fitting model for all outcomes except revascularization (total, CABG and PCI). The 2-way interaction model had the smallest DIC for fatal MI, but as the decrease in DIC was only 2.1, the simpler main effects was considered best.
Table 2.
Deviance Information Criterion by Model and Outcome.
| Outcome | Model | ||
|---|---|---|---|
| Main Effects | Two-Way Interaction | Full-Interaction | |
| All-Cause Mortality | 1147.7 | 1147.5 | 1148.7 |
| CV Mortality | 415.8 | 415.8 | 417.2 |
| Total MI | 536.4 | 536.8 | 538.6 |
| Fatal MI | 143.5 | 141.4 | 142.0 |
| Non-Fatal MI | 318.4 | 319.3 | 317.9 |
| Revascularization † | 545.8 | 545.7 | 537.0 |
| CABG † | 319.0 | 319.2 | 314.9 |
| PCI † | 239.8 | 237.6 | 236.2 |
| All-Cause Hospitalization | 549.9 | 549.9 | 551.4 |
| CV Hospitalization | 275.0 | 277.0 | 279.3 |
CV = cardiovascular. MI = myocardial infarction. CABG = coronary artery bypass surgery. PCI = percutaneous coronary intervention. † full interaction model better fitting. See Supplemental File 4.
Table 3 shows the posterior medians and 95% CrIs, along with the probability that each of the CR components was the most effective, for each of the outcomes where the main-effects model was preferred. Plots of the full posterior distributions are shown in Supplemental File 4. With regard to the primary outcomes, the CR core components of PM and ET had clear benefits and were the two most effective for reducing the hazard of all-cause mortality; no core components had CrIs that excluded 1 for CV mortality (but EX, RFM and PM had HRs near 0.75 and CrIs that lay mostly below 1). With regard to secondary endpoints, the CR core components of PE, followed by ET and PM were effective for reducing the hazard of total MI, and ET for fatal MI (no effective components for non-fatal MI). The CR core component of PM was most effective for reducing the hazard of all-cause and CV-cause hospitalization.
Table 3.
Estimates for Effects of Core Components and Probability of Having Largest Effect for Main Effects Model by Outcome.
| Outcome | Component | ||||
|---|---|---|---|---|---|
| Nutritional Counseling | Risk Factor Modification | Psychosocial Management | Patient Education | Exercise Training | |
| All-Cause Mortality | |||||
| Estimate & 95% Credible Interval | 1.07 (0.78–1.46) |
0.87 (0.66–1.15) |
0.68 (0.54–0.85) |
0.98 (0.78–1.20) |
0.74 (0.60–0.92) |
| Probability Best | 0.01 | 0.04 | 0.67 | 0.01 | 0.28 |
| CV Mortality | |||||
| Estimate & 95% Credible Interval | 1.11 (0.68–1.74) |
0.72 (0.43–1.22) |
0.76 (0.53–1.11) |
0.95 (0.62–1.39) |
0.75 (0.53–1.05) |
| Probability Best | 0.03 | 0.40 | 0.24 | 0.06 | 0.28 |
| Total MI | |||||
| Estimate & 95% Credible Interval | 0.94 (0.56–1.55) |
0.86 (0.54–1.38) |
0.76 (0.57–0.99) |
0.68 (0.47–0.99) |
0.75 (0.56–0.99) |
| Probability Best | 0.08 | 0.10 | 0.17 | 0.45 | 0.20 |
| Fatal MI | |||||
| Estimate & 95% Credible Interval | 1.99 (0.57–6.86) |
0.54 (0.13–2.34) |
0.50 (0.21–1.13) |
0.58 (0.25–1.13) |
0.54 (0.31–0.87) |
| Probability Best | 0.01 | 0.34 | 0.29 | 0.15 | 0.21 |
| Non-Fatal MI | |||||
| Estimate & 95% Credible Interval | 0.93 (0.37–2.47) |
1.05 (0.37–2.68) |
0.86 (0.51–1.40) |
0.83 (0.42–1.47) |
0.78 (0.45–1.28) |
| Probability Best | 0.23 | 0.16 | 0.16 | 0.21 | 0.25 |
| All-Cause Hospitalization | |||||
| Estimate & 95% Credible Interval | 1.19 (0.70–1.94) |
0.97 (0.67–1.38) |
0.76 (0.58–0.96) |
0.87 (0.63–1.18) |
0.83 (0.60–1.13) |
| Probability Best | 0.04 | 0.06 | 0.49 | 0.16 | 0.25 |
| CV Hospitalization | |||||
| Estimate & 95% Credible Interval | 0.37 (0.09–1.45) |
0.70 (0.44–1.14) |
0.78 (0.55–1.00) |
1.03 (0.73–1.41) |
0.75 (0.39–1.12) |
| Probability Best | 0.74 | 0.11 | 0.04 | 0.00 | 0.11 |
CV = cardiovascular. MI = myocardial infarction.
Finally, for revascularization outcomes, the full interaction models were best-fitting; estimated HRs with respect to a control group having none of the components are shown in Table 4.
Table 4.
Odds Ratio Point Estimates for Core Component Combinations in Comparison to Usual Care, for Full Interaction Model for Revascularization (total).
| Components | Arms (n) | Odds Ratio (Mean) | Odds Ratio (Median) | Credible Intervals | p (OR < 1) | |
|---|---|---|---|---|---|---|
| 2.5% | 97.5% | |||||
| NC | 2 | 0.83 | 0.79 | 0.47 | 1.38 | 81.4 |
| RFM | 4 | 0.29 | 0.26 | 1.12 | 0.59 | 100.0 |
| PM | 5 | 0.93 | 0.93 | 0.66 | 1.24 | 70.2 |
| NC, PM | 2 | 1.26 | 1.11 | 0.40 | 2.96 | 41.5 |
| ET | 14 | 0.78 | 0.77 | 0.54 | 1.08 | 93.5 |
| RFM, ET | 2 | 1.92 | 1.65 | 0.61 | 4.82 | 16.2 |
| PM, ET | 2 | 0.72 | 0.65 | 0.25 | 1.67 | 83.4 |
| NC, PM, ET | 1 | 0.16 | 0.13 | 0.03 | 0.50 | 99.8 |
| NC, RFM, PM, ET | 1 | 2.49 | 1.76 | 0.36 | 8.89 | 23.4 |
| PE | 12 | 0.91 | 0.89 | 0.56 | 1.43 | 69.8 |
| NC, PE | 1 | 0.43 | 0.36 | 0.13 | 1.11 | 96.3 |
| NC, RFM, PE | 3 | 0.66 | 0.64 | 0.40 | 1.06 | 96.3 |
| PM, PE | 7 | 0.93 | 0.92 | 0.66 | 1.26 | 74.0 |
| RFM, PM, PE | 2 | 1.09 | 0.98 | 0.45 | 2.36 | 51.5 |
| ET, PE | 1 | 0.92 | 0.85 | 0.41 | 1.85 | 68.8 |
| NC, ET, PE | 2 | 1.38 | 1.07 | 0.29 | 4.03 | 45.9 |
| RFM, ET, PE | 1 | 1.44 | 1.29 | 0.48 | 3.26 | 30.9 |
| NC, FFM, ET, PE | 1 | 1.55 | 1.18 | 0.26 | 5.16 | 41.9 |
| PM, ET, PE | 3 | 0.80 | 0.75 | 0.36 | 1.50 | 78.8 |
| NC, PM, ET, PE | 1 | 1.07 | 0.80 | 0.20 | 3.45 | 61.8 |
| RFM, PM, ET, PE | 1 | 1.65 | 1.34 | 0.41 | 4.62 | 31.7 |
| NC, RFM, PM, ET, PE | 3 | 0.34 | 0.31 | 0.15 | 0.69 | 99.7 |
OR, odds ratio. NC: Nutritional Counseling; RFM: Risk Factor Modification; PM: Psychosocial Management; PE: Patient Education; ET: Exercise Training.
4. Discussion
Using methods that have not yet been applied in this field, through this review, the effectiveness of core CR components has been elucidated for the first time. Results of this NMA establish that the comprehensive delivery of the recommended core components is associated with reductions in mortality and morbidity. The core components of PM, ET and RFM each clearly reduced the hazard of mortality, with PE, ET and PM each reducing the hazard of morbidity (i.e., MI, re-hospitalization). All core components interacted synergistically to reduce revascularization.
Previous meta-analyses have demonstrated the benefits of CR in reducing mortality and morbidity [5,172,173,174,175]. However, more recent reviews have suggested that CR may have less benefit in the current era of optimal medical therapy and given advances in acute CV care [176]. The most recent update of the most rigorous of the reviews (i.e., by the Cochrane Collaboration) [5] showed CR writ large reduced CV mortality (but not all-cause), and similarly reported reductions in hospitalization. They did not report benefit for reducing revascularization, but results herein highlight the importance of offering all core components to reduce these procedures. In traditional meta-analyses, components delivered in active comparison arms are not taken into account (or the specific components in the intervention arms for that matter), which can bias towards the null. Taken together with results from the van Halwejin et al. meta-analysis showing better impact with more components [11], it can be concluded that comprehensive CR has substantial benefit in reducing mortality and morbidity.
As has been demonstrated in previous reviews [3,5,177,178,179,180,181,182], the results herein confirm the centrality of the exercise component of CR in reducing mortality and morbidity. The results also provide evidence for the first time to support other core components of CR and recommend that programs be “comprehensive”, particularly PM and PE. Previous reviews in patients with CHD of PM have only reported non-significant 7–20% reductions in all-cause and CV mortality, and have not evaluated its effects on hospitalization (all-cause or CV) [183], and of PE have reported reductions in cardiovascular events and improvements in quality of life [184]. The beneficial effects of PM observed using NMA methods were compelling.
4.1. Implications
Accordingly, the results of this review support guideline recommendations for the delivery of all the core components, to all indicated patients, given that the benefits have again been replicated. Given that CR is chronically under-resourced [185], many programs do not have the capacity to deliver all components however [186]. In a recent survey of all CR programs globally, PM was reported as the component least likely to be offered of those assessed herein [187]. Moreover, many programs reported limited human health resources in the area of PM (e.g., psychologists, social workers, but not nurses) [187,188,189]. Policy-makers must ensure CR is adequately resourced so not only all patients in need can access it given the additional evidence of benefits forwarded herein, but that patients receive all components, delivered by trained and regulated providers. For PM, this should likely involve depression screening, stress management and social support. Indeed, most CR guidelines call for a multidisciplinary team, comprised of healthcare professionals who have expertise covering all the core components [7].
There are some important directions for future research which flow from this work. Which combination of core components can optimize cost-effectiveness, and impacts of core components on patient-reported outcomes such as quality of life should be investigated.
4.2. Limitations
This review has several limitations. First, information provided in the included RCTs was often insufficient to assess their risk of bias. That patients and providers cannot be blind to arm allocation in CR RCTs cannot be overcome, however, future trials must aspire to the highest standards for conducting and reporting RCTs [190].
Second, there was some ambiguity in coding NC and PE in some trials, as they were in some cases a small part of RFM. This may have impacted the findings for these components, and hence the impact of these components on outcomes may be under-estimated. The level of detail in intervention description did seem to improve with time, but trialists are urged to report their interventions in accordance with TiDIER reporting guidelines [191].
In conclusion, using a novel approach, which takes into consideration the core components of CR, this review has reiterated the significant benefits of comprehensive CR participation in reducing mortality and morbidity. The findings herein confirm the centrality of ET as the key component of CR, and also provide strong evidence for the benefit of the other CR components, particularly PM. Policies are needed to standardize the delivery of comprehensive CR, ensuring delivery of these beneficial core components to all CHD patients.
Acknowledgments
We are grateful to Hoch, Jeffrey, Pechlivanoglou, Petros, Naimark, David M., and Wijeysundera, Harindra C. for early input on the direction of this work.
Supplementary Materials
The following are available online at http://www.mdpi.com/2077-0383/7/12/514/s1, Supplemental File 1: Search Strategy for MEDLINE; Supplemental File 2: Characteristics of Included Trials; Supplemental File 3: Core Components Evaluated in Study Arms of Included Trials by Endpoint; Supplemental File 4: Graphical Display of Distribution for Each Core Component for Each Outcome (main-effects model).
Author Contributions
Conceptualization, N.N.K. and M.K.; Methodology, N.N.K. and J.M.B.; Formal Analysis, G.T.; Investigation, N.N.K., T.A.F. and G.C.; Data Curation, G.T.; Writing—Original Draft Preparation, N.N.K. and M.K.; Writing—Review & Editing, S.L.G., G.C., V.R., T.D.-K., J.M.B. and D.A.A.; Supervision, M.K. and S.L.G; Project Administration, S.L.G.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.World Health Organization (WHO) Global Health Observatory Data Repository. [(accessed on 7 December 2014)]; Available online: http://apps.who.int/gho/data/?theme=main.
- 2.Roth G.A., Johnson C., Abajobir A., Abd-Allah F., Abera S.F., Abyu G., Ahmed M., Aksut B., Alam T., Alam K., et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017;70:1–25. doi: 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leon A.S., Franklin B.A., Costa F., Balady G.J., Berra K.A., Stewart K.J., Thompson P.D., Williams M.A., Lauer M.S. Cardiac rehabilitation and secondary prevention of coronary heart disease: An American Heart Association scientific statement from the Council on Clinical Cardiology (Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention) and the Council on Nutrition, Physical Activity, and Metabolism (Subcommittee on Physical Activity), in collaboration with the American association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2005;111:369–376. doi: 10.1161/01.CIR.0000151788.08740.5C. [DOI] [PubMed] [Google Scholar]
- 4.Balady G.J., Williams M.A., Ades P.A., Bittner V., Comoss P., Foody J.M., Franklin B., Sanderson B., Southard D. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: A scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation. 2007;115:2675–2682. doi: 10.1161/CIRCULATIONAHA.106.180945. [DOI] [PubMed] [Google Scholar]
- 5.Anderson L., Oldridge N., Thompson D.R., Zwisler A.D., Rees K., Martin N., Taylor R.S. Exercise-Based Cardiac Rehabilitation for Coronary Heart Disease Cochrane Systematic Review and Meta-Analysis. J. Am. Coll. Cardiol. 2016;67:1–12. doi: 10.1016/j.jacc.2015.10.044. [DOI] [PubMed] [Google Scholar]
- 6.Piepoli M.F., Corrà U., Adamopoulos S., Benzer W., Bjarnason-Wehrens B., Cupples M., Dendale P., Doherty P., Gaita D., Höfer S., et al. Secondary prevention in the clinical management of patients with cardiovascular diseases. Core components, standards and outcome measures for referral and delivery: A policy statement from the cardiac rehabilitation section of the European Association for Cardiovascular Prevention & Rehabilitation. Endorsed by the Committee for Practice Guidelines of the European Society of Cardiology. Eur. J. Prev. Cardiol. 2014;21:664–681. doi: 10.1177/2047487312449597. [DOI] [PubMed] [Google Scholar]
- 7.Cardiac Rehabilitation and Cardiovascular Disease Prevention (CACR) Canadian Guidelines for Cardiac Rehabilitation and Cardiovascular Disease Prevention 2015. [(accessed on 5 July 2017)]; Available online: https://cacpr.ca/Guidelines.
- 8.Woodruffe S., Neubeck L., Clark R.A., Gray K., Ferry C., Finan J., Sanderson S., Briffa T.G. Australian Cardiovascular Health and Rehabilitation Association (ACRA) core components of cardiovascular disease secondary prevention and cardiac rehabilitation 2014. Heart Lung Circul. 2015;24:430–441. doi: 10.1016/j.hlc.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 9.Buckley J.P., Furze G., Doherty P., Speck L., Connolly S., Hinton S., Jones J.L. BACPR scientific statement: British standards and core components for cardiovascular disease prevention and rehabilitation. Heart. 2013;99:1069–1071. doi: 10.1136/heartjnl-2012-303460. [DOI] [PubMed] [Google Scholar]
- 10.Hamm L.F., Sanderson B.K., Ades P.A., Berra K., Kaminsky L.A., Roitman J.L., Williams M.A. Core competencies for cardiac rehabilitation/secondary prevention professionals: 2010 update: Position statement of the American Association of Cardiovascular and Pulmonary Rehabilitation. J. Cardiopulm. Rehabil. Prev. 2011;31:2–10. doi: 10.1097/HCR.0b013e318203999d. [DOI] [PubMed] [Google Scholar]
- 11.Van Halewijn G., Deckers J., Tay H.Y., van Domburg R., Kotseva K., Wood D. Lessons from contemporary trials of cardiovascular prevention and rehabilitation: A systematic review and meta-analysis. Int. J. Cardiol. 2017;232:294–303. doi: 10.1016/j.ijcard.2016.12.125. [DOI] [PubMed] [Google Scholar]
- 12.Kachur S., Chongthammakun V., Lavie C.J., De Schutter A., Arena R., Milani R.V., Franklin B.A. Impact of cardiac rehabilitation and exercise training programs in coronary heart disease. Prog. Cardiovasc. Dis. 2017;60:103–114. doi: 10.1016/j.pcad.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 13.Clark A.M. What are the components of complex interventions in healthcare? Theorizing approaches to parts, powers and the whole intervention. Soc. Sci. Med. 2013;93:185–193. doi: 10.1016/j.socscimed.2012.03.035. [DOI] [PubMed] [Google Scholar]
- 14.Higgins J.P.T., Altman D.G., Sterne J.A.C. Chapter 8: Assessing Risk of Bias in Included Studies. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) [(accessed on 14 June 2017)]; Available online: http://handbook-5-1.cochrane.org.
- 15.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS. Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hutton B., Salanti G., Caldwell D.M., Chaimani A., Schmid C.H., Cameron C., Ioannidis J.P., Straus S., Thorlund K., Jansen J.P., et al. The PRISMA extension statement for reporting of systematic reviews incorporating network metaanalyses of health care interventions: Checklist and explanations. Ann. Intern. Med. 2015;162:777–784. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- 17.Balady G.J., Ades P.A., Comoss P., Limacher M., Pina I.L., Southard D., Williams M.A., Bazzarre T. Core components of cardiac rehabilitation/secondary prevention programs: A statement for healthcare professionals from the American Heart Association and the American Association of Cardiovascular and Pulmonary Rehabilitation Writing Group. Circulation. 2000;102:1069–1073. doi: 10.1161/01.CIR.102.9.1069. [DOI] [PubMed] [Google Scholar]
- 18.Higgins J.P., Altman D.G., Gøtzsche P.C., Jüni P., Moher D., Oxman A.D., Savovic J., Schulz K.F., Weeks L., Sterne J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Welton N.J., Caldwell D.M., Adamopoulos E., Vedhara K. Mixed treatment comparison meta-analysis of complex interventions: Psychological interventions in coronary heart disease. Am. J. Epidemiol. 2009;169:1158–1165. doi: 10.1093/aje/kwp014. [DOI] [PubMed] [Google Scholar]
- 20.Franchini A.J., Dias S., Ades A.E., Jansen J.P., Welton N.J. Accounting for correlation in network meta-analysis with multi-arm trials. Res. Synth. Methods. 2012;3:142–160. doi: 10.1002/jrsm.1049. [DOI] [PubMed] [Google Scholar]
- 21.Dias S., Sutton A.J., Ades A.E., Welton N.J. Evidence synthesis for decision making 2: A generalized linear modeling framework for pairwise and network meta-analysis of randomized controlled trials. Med. Decis. Mak. 2013;33:607–617. doi: 10.1177/0272989X12458724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dias S., Sutton A.J., Welton N.J., Ades A.E. Evidence synthesis for decision making 3: Heterogeneity—Subgroups, meta-regression, bias, and bias-adjustment. Med. Decis. Mak. 2013;33:618–640. doi: 10.1177/0272989X13485157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dias S., Welton N.J., Sutton A.J., Caldwell D.M., Lu G., Ades A.E. Evidence synthesis for decision making 4: Inconsistency in networks of evidence based on randomized controlled trials. Med. Decis. Mak. 2013;33:641–656. doi: 10.1177/0272989X12455847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Albus C., Theissen P., Hellmich M., Griebenow R., Wilhelm B., Aslim D., Schicha H., Köhle K. Long-term effects of a multimodal behavioral intervention on myocardial perfusion-a randomized controlled trial. Int. J. Behav. Med. 2009;16:219–226. doi: 10.1007/s12529-008-9030-4. [DOI] [PubMed] [Google Scholar]
- 25.Albus C. A stepwise psychotherapy intervention to reduce risk in coronary artery disease (SPIRR-CAD)—Results of a randomised, controlled multicentre trial. J. Psychosom. Res. 2014;76:495. doi: 10.1016/j.jpsychores.2014.03.017. [DOI] [PubMed] [Google Scholar]
- 26.Aldana S.G., Greenlaw R., Salberg A., Merrill R.M., Hager R., Jorgensen R.B. The effects of an intensive lifestyle modification program on carotid artery intima-media thickness: A randomized trial. Am. J. Heal. Promot. 2007;21:510–516. doi: 10.4278/0890-1171-21.6.510. [DOI] [PubMed] [Google Scholar]
- 27.Allison T.G., Farkouh M.E., Smars P.A., Evans R.W., Squires R.W., Gabriel S.E., Kopecky S.L., Gibbons R.J., Reeder G.S. Management of coronary risk factors by registered nurses versus usual care in patients with unstable angina pectoris (a chest pain evaluation in the emergency room [CHEER] substudy) Am. J. Cardiol. 2000;86:133–138. doi: 10.1016/S0002-9149(00)00848-1. [DOI] [PubMed] [Google Scholar]
- 28.Andersson A., Sundel K.L., Undén A.L., Schenck-Gustafsson K., Eriksson I. A five-year rehabilitation programme for younger women after a coronary event reduces the need for hospital care. Scand. J. Public Health. 2010;38:566–573. doi: 10.1177/1403494810377125. [DOI] [PubMed] [Google Scholar]
- 29.Appels A., van Elderen T., Bär F., van der Pol G., Erdman R.A., Assman M., Trijsburg W., van Diest R., van Dixhoorn J., Pedersen S.S. Effects of a behavioural intervention on quality of life and related variables in angioplasty patients. Results of the EXhaustion Intervention Trial. J. Psychosom. Res. 2006;61:1–7. doi: 10.1016/j.jpsychores.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 30.Asbury E.A., Webb C.M., Collins P. Group support to improve psychosocial well-being and primary-care demands among women with cardiac syndrome X. Climacteric. 2011;14:100–104. doi: 10.3109/13697137.2010.499181. [DOI] [PubMed] [Google Scholar]
- 31.Bambauer K.Z., Aupont O., Stone P.H., Locke S.E., Mullan M.G., Colagiovanni J., McLaughlin T.J. The Effect of a Telephone Counseling Intervention on Self-Rated Health of Cardiac Patients. Psychosom. Med. 2005;67:539–545. doi: 10.1097/01.psy.0000171810.37958.61. [DOI] [PubMed] [Google Scholar]
- 32.Barnason S., Zimmerman L., Nieveen J., Schulz P., Miller C., Hertzog M., Tu C. Influence of a symptom management telehealth intervention on older adults’ early recovery outcomes after coronary artery bypass surgery. Heart Lung J. Acute Crit. Care. 2009;38:364–376. doi: 10.1016/j.hrtlng.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Beckie T.M., Beckstead J.W. The effects of a cardiac rehabilitation program tailored for women on global quality of life: A randomized clinical trial. J. Womens Health. 2010;19:1977–1985. doi: 10.1089/jwh.2010.1937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Belardinelli R.B., Paolini P., Cianci G.C.G., Piva R.P.R., Solenghi M.S.M. The efficay of exercise training after coronary angioplasty: The ETICA trial. Eur. Heart. J. 2001;22:200. doi: 10.1016/s0735-1097(01)01236-0. [DOI] [PubMed] [Google Scholar]
- 35.Belardinelli R., Paolini I., Cianci G., Piva R., Georgiou D., Purcaro A. Exercise training intervention after coronary angioplasty: The ETICA trial. J. Am. Coll. Cardiol. 2001;37:1891–1900. doi: 10.1016/S0735-1097(01)01236-0. [DOI] [PubMed] [Google Scholar]
- 36.Bengtsson K. Rehabilitation after myocardial infarction. A controlled study. Scand. J. Rehabil. Med. 1983;15:1–9. doi: 10.3109/03009748609092661. [DOI] [PubMed] [Google Scholar]
- 37.Beresnevaite M. Exploring the benefits of group psychotherapy in reducing alexithymia in coronary heart disease patients: A preliminary study. Psychother. Psychosom. 2000;69:117–122. doi: 10.1159/000012378. [DOI] [PubMed] [Google Scholar]
- 38.Berkman L.F., Blumenthal J., Burg M., Carney R.M., Catellier D., Cowan M.J., Czajkowski S.M., DeBusk R., Hosking J., Jaffe A., et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction the enhancing recovery in coronary heart disease patients (ENRICHD) randomized trial. JAMA. 2003;289:3106–3116. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- 39.Bertie J., King A., Reed N., Marshall A.J., Ricketts C. Benefits and weaknesses of a cardiac rehabilitation programme. J. R. Coll. Physicians. Lond. 1992;26:147–151. [PMC free article] [PubMed] [Google Scholar]
- 40.Bethell H.J.N., Turner S.C., Mulleet M.A. Cardiac rehabilitation in the community: 11-year follow-up after a randomized controlled trial. Coronary Health Care. 1999;3:183–188. doi: 10.1016/S1362-3265(99)80042-X. [DOI] [Google Scholar]
- 41.Black J.L., Allison T.G., Williams D.E., Rummans T.A., Gau G.T. Effect of intervention for psychological distress on rehospitalization rates in cardiac rehabilitation patients. Psychosomatics. 1998;39:134–143. doi: 10.1016/S0033-3182(98)71360-X. [DOI] [PubMed] [Google Scholar]
- 42.Blasco A., Carmona M., Fernández-Lozano I., Salvador C.H., Pascual M., Sagredo P.G., Somolinos R., Muñoz A., García-López F., Escudier J.M., et al. Evaluation of a telemedicine service for the secondary prevention of coronary artery disease. J. Cardiopulm. Rehabil. Prev. 2012;32:25–31. doi: 10.1097/HCR.0b013e3182343aa7. [DOI] [PubMed] [Google Scholar]
- 43.Blumenthal J.A., Jiang W., Babyak M.A., Krantz D.S., Frid D.J., Coleman R.E., Waugh R., Hanson M., Appelbaum M., O’Connor C., et al. Stress management and exercise training in cardiac patients with myocardial ischemia effects on prognosis and evaluation of mechanisms. Arch. Intern. Med. 1997;157:2213–2223. doi: 10.1001/archinte.1997.00440400063008. [DOI] [PubMed] [Google Scholar]
- 44.Blumenthal J.A., Sherwood A., Smith P.J., Watkins L., Mabe S., Kraus W.E., Ingle K., Miller P., Hinderliter A. Enhancing cardiac rehabilitation with stress management training: A randomized clinical efficacy trial. Circulation. 2016;133:1341–1350. doi: 10.1161/CIRCULATIONAHA.115.018926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Broadbent E., Ellis C.J., Thomas J., Gamble G., Petrie K.J. Further development of an illness perception intervention for myocardial infarction patients: A randomized controlled trial. J. Psychosom. Res. 2009;67:17–23. doi: 10.1016/j.jpsychores.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 46.Burgess A.W., Lerner D.J., D’Agostino R.B., Vokonas P.S., Hartman C.R., Gaccione P. A randomized control trial of cardiac rehabilitation. Soc. Sci. Med. 1987;24:359–370. doi: 10.1016/0277-9536(87)90154-7. [DOI] [PubMed] [Google Scholar]
- 47.Burr M.L., Ashfield-Watt P., Dunstan F., Fehily A.M., Breay P., Ashton T., Zotos P.C., Haboubi N.A., Elwood P.C. Lack of benefit of dietary advice to men with angina: Results of a controlled trial. Eur. J. Clin. Nutr. 2003;57:193–200. doi: 10.1038/sj.ejcn.1601539. [DOI] [PubMed] [Google Scholar]
- 48.Burell G. Behaviour modification after coronary artery bypass graft surgery: Effects on cardiac morbidity and mortality. J. Rehabil. Sci. 1995;8:39–40. [Google Scholar]
- 49.Byrkjeland R., Njerve I.U., Anderssen S., Arnesen H., Seljeflot I., Solheim S. Effects of exercise training on HbA 1c and VO 2peak in patients with type 2 diabetes and coronary artery disease: A randomised clinical trial. Diabetes Vasc. Dis. Res. 2015;12:325–333. doi: 10.1177/1479164115590552. [DOI] [PubMed] [Google Scholar]
- 50.Carson Carson P., Phillips R., Lloyd M., Tucker H., Neophytou M., Buch N.J., Gelson A., Lawton A., Simpson T. Exercise after myocardial infarction: A controlled trial. J. R. Coll. Physicians Lond. 1982;16:147–151. [PMC free article] [PubMed] [Google Scholar]
- 51.Chow C.K., Redfern J., Hillis G.S., Thakkar J., Santo K., Hackett M.L., Jan S., Graves N., de Keizer L., Barry T., et al. Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease. JAMA. 2015;314:1255–1263. doi: 10.1001/jama.2015.10945. [DOI] [PubMed] [Google Scholar]
- 52.Claesson M., Birgander L.S., Jansson J.H., Lindahl B., Burell G., Asplund K., Mattsson C. Cognitive-behavioural stress management does not improve biological cardiovascular risk indicators in women with ischaemic heart disease: A randomized-controlled trial. J. Intern. Med. 2006;260:320–331. doi: 10.1111/j.1365-2796.2006.01691.x. [DOI] [PubMed] [Google Scholar]
- 53.Clark N.M., Janz N.K., Dodge J.A., Schork M.A., Fingerlin T.E., Wheeler J.R.C., Liang J., Keteyian S.J., Santinga J.T. Changes in functional health status of older women with heart disease: Evaluation of a program based on self-regulation. J. Gerontol. 2000;55:S117–S126. doi: 10.1093/geronb/55.2.S117. [DOI] [PubMed] [Google Scholar]
- 54.Cohen A., Assyag P., Boyer-Chatenet L., Cohen-Solal A., Perdrix C., Dalichampt M., Michel P.L., Montalescot G., Ravaud P., Steg P.G., et al. An Education Program for Risk Factor Management After an Acute Coronary Syndrome. JAMA Intern. Med. 2014;174:40–48. doi: 10.1001/jamainternmed.2013.11342. [DOI] [PubMed] [Google Scholar]
- 55.Costa e Silva R., Pellanda L., Portal V., Maciel P., Furquim A., Schaan B. Transdiciplinary approach to the follow-up of patients after myocardial infarction. Clinics. 2008;63:489–496. doi: 10.1590/S1807-59322008000400013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cupples M.E., McKnigth A. Five year follow up of patients at high cardiovascular risk who took part in randomised controlled trial of health promotion. BMJ. 1999;319:687–688. doi: 10.1136/bmj.319.7211.687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dalal H.M., Evans P.H., Campbell J.L., Taylor R.S., Watt A., Read K.L., Mourant A.J., Wingham J., Thompson D.R., Pereira Gray D.J. Home-based versus hospital-based rehabilitation after myocardial infarction: A randomized trial with preference arms—Cornwall Heart Attack Rehabilitation Management Study (CHARMS) Int. J. Cardiol. 2007;119:202–211. doi: 10.1016/j.ijcard.2006.11.018. [DOI] [PubMed] [Google Scholar]
- 58.Davidson K.W., Gidron Y., Mostofsky E., Trudeau K.J. Hospitalization cost offset of a hostility intervention for coronary heart disease patients. J. Consult. Clin. Psychol. 2007;75:657–662. doi: 10.1037/0022-006X.75.4.657. [DOI] [PubMed] [Google Scholar]
- 59.Davidson K.W., Rieckmann N., Clemow L., Schwartz J.E., Shimbo D., Medina V., Albanese G., Kronish I., Hegel M., Burg M.M. Enhanced depression care for patients with acute coronary syndrome and persistent depressive symptoms coronary psychosocial evaluation studies randomized controlled trial. Arch. Intern. Med. 2010;170:600–608. doi: 10.1001/archinternmed.2010.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.De Lorgeril M., Salen P., Martin J.-L., Monjaud I., Delaye J., Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: Final report of the Lyon diet heart study. Circulation. 1999;99:779–785. doi: 10.1161/01.CIR.99.6.779. [DOI] [PubMed] [Google Scholar]
- 61.DeBusk R.F., Miller N.H., Superko H.R., Dennis C.A., Thomas R.J., Lew H.T., Berger W.E., III, Heller R.S., Rompf J., Gee D., et al. A Case-Management System for Coronary Risk Factor Modification after Acute Myocardial Infarction. Ann. Intern. Med. 1994;120:721–729. doi: 10.7326/0003-4819-120-9-199405010-00001. [DOI] [PubMed] [Google Scholar]
- 62.Donohue J.M., Belnap B.H., Men A., He F., Roberts M.S., Schulberg H.C., Reynolds C.F., III, Rollman B.L. Twelve-month cost-effectiveness of telephone-delivered collaborative care for treating depression following cabg surgery: A randomized controlled. Gen. Hosp. Psychiatry. 2014;36:453–459. doi: 10.1016/j.genhosppsych.2014.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Du L., Dong P., Jia J., Li Z., Lai L., Yang X., Wang S., Yang X., Li Z., Shang X., et al. Impacts of intensive follow-up on the long-term prognosis of percutaneous coronary intervention in acute coronary syndrome patients—A single center prospective randomized controlled study in a Chinese population. Eur. J. Prev. Cardiol. 2016;23:1077–1085. doi: 10.1177/2047487315607041. [DOI] [PubMed] [Google Scholar]
- 64.Dugmore L.D., Tipson R.J., Phillips M.H., Flint E.J., Stentiford N.H., Bone M.F., Littler W.A. Changes in cardiorespiratory fitness, psychological wellbeing, quality of life, and vocational status following a 12 month cardiac exercise rehabilitation programme. Heart. 1999;81:359–366. doi: 10.1136/hrt.81.4.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Edworthy S.M., Baptie B., Galvin D., Brant R.F., Churchill-Smith T., Manyari D., Belenkie I. Effects of an enhanced secondary prevention program for patients with heart disease: A prospective randomized trial. Can. J. Cardiol. 2007;23:1066–1072. doi: 10.1016/S0828-282X(07)70875-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Engblom E., Hletanent E.K., Hamalafnent H., Kallioj V., Lnberg M., Knutst L.-R. Exercise habits and physical performance during comprehensive rehabilitation after coronary artery bypass surgery. Eur. Heart J. 1992;13:1053–1059. doi: 10.1093/oxfordjournals.eurheartj.a060313. [DOI] [PubMed] [Google Scholar]
- 67.Erdman R.A.M., Duivenvoorden H.J. Psychologic evaluation of a cardiac rehabilitation program: A randomized clinical trial in patients with myocardial infarction. J. Cardiac. Rehabil. 1983;3:696–704. [Google Scholar]
- 68.Fihn S.D., Bucher J.B., McDonell M., Diehr P., Rumsfeld J.S., Doak M., Dougherty C., Gerrity M., Heidenreich P., Larsen G., et al. Collaborative care intervention for stable ischemic heart disease. Arch. Intern. Med. 2011;171:1471–1479. doi: 10.1001/archinternmed.2011.372. [DOI] [PubMed] [Google Scholar]
- 69.Frasure-Smith N., Prince R. The Ischemic heart disease life stress monitoring program: 18-month mortality results. Psychosom. Med. 1985;47:431–445. doi: 10.1097/00006842-198509000-00003. [DOI] [PubMed] [Google Scholar]
- 70.Frasure-Smith N., Lespérance F., Prince R.H., Verrier P., Garber R.A., Juneau M., Wolfson C., Bourassa M.G. Randomised trial of home-based psychosocial nursing intervention for patients recovering from myocardial infarction. Lancet. 1997;350:473–479. doi: 10.1016/S0140-6736(97)02142-9. [DOI] [PubMed] [Google Scholar]
- 71.Fridlund B., Pihlgren C., Wannestig L.B. A supportive–educative caring rehabilitation programme; improvements of physical health after myocardial infarction. J. Clin. Nurs. 1992;1:141–146. doi: 10.1111/j.1365-2702.1992.tb00084.x. [DOI] [Google Scholar]
- 72.Friedman M., Thoresen C.E., Gill J.J., Powell L.H., Ulmer D., Thompson L., Price V.A., Rabin D.D., Breall W.S., Dixon T., et al. of type A behavior and reduction in cardiac recurrences in postmyocardial infarction patients. Am. Heart J. 1984;108:237–248. doi: 10.1016/0002-8703(84)90606-9. [DOI] [PubMed] [Google Scholar]
- 73.Froelicher V., Jensen D., Genter F., Sullivan M., McKirnan M.D., Witztum K., Scharf J., Strong M.L., Ashburn W. A randomized trial of exercise training in patients with coronary heart disease. JAMA. 1984;252:1291–1297. doi: 10.1001/jama.1984.03350100021023. [DOI] [PubMed] [Google Scholar]
- 74.Furber S., Butler L., Phongsavan P., Mark A., Bauman A. randomised controlled trial of a pedometer-based telephone intervention to increase physical activity among cardiac patients not attending cardiac rehabilitation. Patient Educ. Couns. 2010;80:212–218. doi: 10.1016/j.pec.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 75.Furze G., Cox H., Morton V., Chuang L.H., Lewin R.J., Nelson P., Carty R., Norris H., Patel N., Elton P. Randomized controlled trial of a lay-facilitated angina management programme. J. Adv. Nurs. 2012;68:2267–2279. doi: 10.1111/j.1365-2648.2011.05920.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ghroubi S., Elleuch W., Abid L., Kammoun S., Elleuch M.-H. The effects of cardiovascular rehabilitation after coronary stenting. Ann. Phys. Rehabil. Med. 2012;55:e309. doi: 10.1016/j.rehab.2012.07.779. [DOI] [PubMed] [Google Scholar]
- 77.Giallauria F., Cirillo P., Lucci R., Pacileo M., Lorenzo A.D., D’Agostino M., Moschella S., Psaroudaki M., Del Forno D., Orio F., et al. Left ventricular remodelling in patients with moderate systolic dysfunction after myocardial infarction: Favourable effects of exercise training and predictive role of N-terminal pro-brain natriuretic peptide. Eur. J. Cardiovasc. Prev. Rehabil. 2008;15:113–118. doi: 10.1097/HJR.0b013e3282f00990. [DOI] [PubMed] [Google Scholar]
- 78.Giannuzzi P., Tavazzi L., Temporelli P.L., Corrà U., Imparato A., Gattone M., Giordano A., Sala L., Schweiger C., Malinverni C. Long-term physical training and left ventricular remodelling after anterior myocardial infraction: Results of the exercise in anterior myocardial infraction (EAMI) trial. J. Am. Coll. Cardiol. 1993;22:1821–1829. doi: 10.1016/0735-1097(93)90764-R. [DOI] [PubMed] [Google Scholar]
- 79.Giannuzzi P., Temporelli P.L., Corra U., Gattone M., Giordano A., Tavazzi L. Attenuation of unfavorable remodeling by exercise training in post infarction patients with left ventricular dysfunction: Results of the exercise in left ventricular dysfunction (ELVD) trial. Circulation. 1997;96:1790–1797. doi: 10.1161/01.CIR.96.6.1790. [DOI] [PubMed] [Google Scholar]
- 80.Gortner S.R., Gilliss C.L., Shinn J.A., Sparacino P.A., Rankin S., Leavitt M., Price M., Hudes M. Improving recovery following cardiac surgery: A randomized clinical trial. J. Adv. Nurs. 1988;13:649–661. doi: 10.1111/j.1365-2648.1988.tb01459.x. [DOI] [PubMed] [Google Scholar]
- 81.Gulliksson M., Burrel G., Vessby B., Lundin L., Toss H., Svardsudd K. Randomized controlled trial of cognitive behavioral therapy vs standard treatment to prevent recurrent cardiovascular events in patients with coronary heart disease. secondary prevention in Uppsala primary health care project (SUPRIM) Arch. Inter. Med. 2011;171:134–140. doi: 10.1001/archinternmed.2010.510. [DOI] [PubMed] [Google Scholar]
- 82.Gutschker A., Schaller K., Geissler W. Results of physical conditioning in patients with acute myocardial infarction over 65 years of age. Cardiology. 1977;62:109. [Google Scholar]
- 83.Hämäiäinen H., Kallio V., Knuts L.R., Arstila M., Aaito-Setälä L., Härmälä V., Kaarsalo E., Laurila S., Pere E. Community approach in rehabilitation and secondary prevention after acute myocardial infarction: Results of a randomized clinical trial. J. Cardiopulm. Rehabil. 1991;11:221–226. doi: 10.1097/00008483-199107000-00003. [DOI] [Google Scholar]
- 84.Hambrecht R., Niebauer J., Marburger C., Grunze M., Kälberer B., Hauer K., Schlierf G., Kübler W., Schuler G. Various intensities of leisure time physical activity in patients with coronary artery disease: Effects on cardiorespiratory fitness and progression of coronary atherosclerotic lesions. J. Am. Coll. Cardiol. 1993;22:468–477. doi: 10.1016/0735-1097(93)90051-2. [DOI] [PubMed] [Google Scholar]
- 85.Hanssen T.A., Nordrehaug J.E., Eide G.E., Hanestad B.R. Improving outcomes after myocardial infarction: A randomized controlled trial evaluating effects of a telephone follow-up intervention. Eur. J. Cardiovasc. Prev. Rehabil. 2007;14:429–437. doi: 10.1097/HJR.0b013e32801da123. [DOI] [PubMed] [Google Scholar]
- 86.Harald T., Reimer O., Tijssen J.G.P., Peters R.J.G. Non-Cardiac Readmissions Are Reduced in Patients Attending a Nurse-Coordinated Prevention Program: Results from the RESPONSE Randomised Clinical Trial. EuroPrevent Congress of the European Association of Preventive Cardiology; Lisbon, Portugal: 2015. [Google Scholar]
- 87.Haskell W.L., Alderman E.L., Fair J.M., Maron D.J., Mackey S.F., Superko H.R., Williams P.T., Johnstone I.M., Champagne M.A., Krauss R.M., et al. Effects of intensive multiple risk factor reduction on coronary atherosclerosis and clinical cardiac events in men and women with coronary artery disease. The Stanford Coronary Risk Intervention Project (SCRIP) Circulation. 1994;89:975–990. doi: 10.1161/01.CIR.89.3.975. [DOI] [PubMed] [Google Scholar]
- 88.Hawkes A.L., Patrao T.A., Atherton J., Ware R.S., Taylor C.B., O’Neil A., Foreman R., Oldenburg B.F. Effect of a telephone-delivered coronary heart disease secondary prevention program (ProActive Heart) on quality of life and health behaviours: Primary outcomes of a randomised controlled trial. Int. J. Behav. Med. 2013;20:413–424. doi: 10.1007/s12529-012-9250-5. [DOI] [PubMed] [Google Scholar]
- 89.Heller R.F., Knapp J.C., Valenti L.A., Dobson A.J. Secondary prevention after acute myocardial infarction. Am. J. Cardiol. 1993;72:759–762. doi: 10.1016/0002-9149(93)91058-P. [DOI] [PubMed] [Google Scholar]
- 90.Higgins H.C., Hayes R.L., Mckenna K.T. Rehabilitation outcomes following percutaneous coronary interventions (PCI) Patient Educ. Couns. 2001;43:219–230. doi: 10.1016/S0738-3991(00)00164-6. [DOI] [PubMed] [Google Scholar]
- 91.Hofman-Bang C., Lisspers J., Nordlander R., Nygren A., Sundin O., Ohman A., Rydén L. Two-year results of a controlled study of residential rehabilitation for patients treated with percutaneous transluminal coronary angioplasty. A randomized study of a multifactorial programme. Eur. Heart J. 1999;20:1465–1474. doi: 10.1053/euhj.1999.1544. [DOI] [PubMed] [Google Scholar]
- 92.Jolly K., Taylor R.S., Lip G.Y.H., Singh S. Reproducibility and safety of the incremental shuttle walking test for cardiac rehabilitation. Int. J. Cardiol. 2008;125:144–145. doi: 10.1016/j.ijcard.2007.01.037. [DOI] [PubMed] [Google Scholar]
- 93.Jones D.A., West R.R. Psychological rehabilitation after myocardial infarction: Multicentre randomised controlled trial. BMJ. 1996;313:1517–1521. doi: 10.1136/bmj.313.7071.1517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kallio V., Hämäläinen H., Hakkila J., Luurila O. Reduction in sudden deaths by a multifactorial intervention programme after acute myocardial infarction. Lancet. 1979;314:1091–1094. doi: 10.1016/S0140-6736(79)92502-9. [DOI] [PubMed] [Google Scholar]
- 95.Karlsson M.R., Edström-Plüss C., Held C., Henriksson P., Billing E., Wallén N.H. Effects of expanded cardiac rehabilitation on psychosocial status in coronary artery disease with focus on typed characteristics. J. Behav. Med. 2007;30:253–261. doi: 10.1007/s10865-007-9096-5. [DOI] [PubMed] [Google Scholar]
- 96.Koertge J., Janszky I., Sundin Ö., Blom M., Georgiades A., László K.D., Alinaghizadeh H., Ahnve S. Effects of a stress management program on vital exhaustion and depression in women with coronary heart disease: A randomized controlled intervention study. J. Intern. Med. 2008;263:281–293. doi: 10.1111/j.1365-2796.2007.01887.x. [DOI] [PubMed] [Google Scholar]
- 97.Kure C.E., Ski C.F., Stewart S., Chan Y.K., Carrington M.J., Thompson D.R. Potential impact of depression on health outcomes in a randomised control trial of multidisciplinary, nurse-led, home based intervention (HBI) to reduce secondary cardiac events. Glob. Heart. 2014;9:e29. doi: 10.1016/j.gheart.2014.03.1320. [DOI] [Google Scholar]
- 98.La Rovere M.T., Bersano C., Gnemmi M., Specchia G., Schwartz P.J. Exercise-induced increase in baroreflex sensitivity predicts improved prognosis after myocardial infarction. Circulation. 2002;106:945–949. doi: 10.1161/01.CIR.0000027565.12764.E1. [DOI] [PubMed] [Google Scholar]
- 99.Leemrijse C.J., Peters R.J.G., von Birgelen C., van Dijk L., van Hal J.M., Kuijper A.F., Snaterse M., Veenhof C. The telephone lifestyle intervention ‘Hartcoach’ has modest impact on coronary risk factors: A randomised multicentre trial. Eur. J. Prev. Cardiol. 2016;23:1658–1668. doi: 10.1177/2047487316639681. [DOI] [PubMed] [Google Scholar]
- 100.Lehmann N., Paul A., Moebus S., Budde T., Dobos G.J., Michalsen A. Effects of lifestyle modification on coronary artery calcium progression and prognostic factors in coronary patients 3-Year results of the randomized SAFE-LIFE trial. Atherosclerosis. 2011;219:630–636. doi: 10.1016/j.atherosclerosis.2011.08.050. [DOI] [PubMed] [Google Scholar]
- 101.Leizorovicz A., Sait-Pierre A., Vasselon C., Boissel J.P. Comparison of a rehabilitation programme, a counselling programme and usual care after an acute myocardial infarction: Results of a long-term randomized trial. Eur. Heart J. 1991;12:612–616. doi: 10.1093/oxfordjournals.eurheartj.a059948. [DOI] [PubMed] [Google Scholar]
- 102.Lewin B., Robertson I.H., Cay E.L., Irving J.B., Campbell M. Effects of self-help post-myocardial-irfaction rehabilitation on psychological adjustment and use of health services. Lancet. 1992;339:1036–1040. doi: 10.1016/0140-6736(92)90547-G. [DOI] [PubMed] [Google Scholar]
- 103.Lewin R.J.P., Furze G., Robinson J., Griffith K., Wiseman S., Pye M., Boyle R. A randomised controlled trial of a self-management plan for patients with newly diagnosed angina. Br. J. Gen. Pract. 2002;52:194–196. [PMC free article] [PubMed] [Google Scholar]
- 104.Lidell E., Fridlund B. Long-term Effects of a Comprehensive Rehabilitation Programme after Myocardial Infarction. Scand. J. Caring Sci. 1996;10:67–74. doi: 10.1111/j.1471-6712.1996.tb00314.x. [DOI] [PubMed] [Google Scholar]
- 105.Lie I., Arnesen H., Sandvik L., Hamilton G.H., Bunch E. Effects of a home-based intervention program on anxiety and depression 6 months after coronary artery bypass grafting: A randomized controlled trial. J. Psychosom. Res. 2007;62:411–418. doi: 10.1016/j.jpsychores.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 106.Lin C.Y., Yaseri M., Pakpour A.H., Malm D., Broström A., Fridlund B., Burri A., Webb T.L. Can a multifaceted intervention including motivational interviewing improve medication adherence, quality of life, and mortality rates in older patients undergoing coronary artery bypass surgery? A multicenter, randomized controlled trial with 18-month follow-up. Drugs Aging. 2017;34:143–156. doi: 10.1007/s40266-016-0429-3. [DOI] [PubMed] [Google Scholar]
- 107.Manchanda S.C., Narang R., Reddy K.S., Sachdeva U., Prabhakaran D., Dharmanand S., Rajani M., Bijlani R. Retardation of coronary atherosclerosis with yoga lifestyle intervention. J. Assoc. Physicians India. 2000;48:687–694. [PubMed] [Google Scholar]
- 108.Marcus S., Orha I., Cioranu R., Apetrei E. Long-Term (25 Years) Efficacy of Comprehensive Post Myocardial Infarction Rehabilitation Program. XXI Congress of the European Society of Cardiology; Bologna, Spain: 1999. [Google Scholar]
- 109.Maroto-Montero J.M., Ramírez R.A., Morales-Durán M.D., de Pablo Zarzosa C., Abraira V. Cardiac rehabilitation in patients with myocardial infarction: A 10-year follow-up study. Rev. Esp. Cardiol. 2005;58:1181–1187. doi: 10.1016/S1885-5857(06)60397-6. [DOI] [PubMed] [Google Scholar]
- 110.Marra S., Paolillo V., Spadaccini F., Angelino P.F. Long-term follow-up after a controlled randomized post-myocardial infarction rehabilitation programme: Effects on morbidity and mortality. Eur. Heart J. 1985;6:656–663. doi: 10.1093/oxfordjournals.eurheartj.a061917. [DOI] [PubMed] [Google Scholar]
- 111.Mayou R.A., Thompson D.R., Clements A., Davies C.H., Goodwin S.J., Normington K., Hicks N., Price J. Guideline-based early rehabilitation after myocardial infarction. J. Psychosom. Res. 2002;52:89–95. doi: 10.1016/S0022-3999(01)00300-2. [DOI] [PubMed] [Google Scholar]
- 112.Meisinger C., Stollenwerk B., Kirchberger I., Seidl H., Wende R., Kuch B., Holle R. Effects of a nurse-based case management compared to usual care among aged patients with myocardial infarction: Results from the randomized controlled KORINNA study. BMC Geriatr. 2013;13:115. doi: 10.1186/1471-2318-13-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Michalsen A., Grossman P., Lehmann N., Knoblauch N.T., Paul A., Moebus S., Budde T., Dobos G.J. Psychological and quality-of-life outcomes from a comprehensive stress reduction and lifestyle program in patients with coronary artery disease: Results of a randomized trial. Psychother. Psychosom. 2005;74:344–352. doi: 10.1159/000087781. [DOI] [PubMed] [Google Scholar]
- 114.Miller N.H., Haskell W.L., Berra K., Debusk R.F., Iii B., Lew H. Home versus group exercise training for increasing functional capacity after myocardial infarction. Circulation. 1984;70:645–649. doi: 10.1161/01.CIR.70.4.645. [DOI] [PubMed] [Google Scholar]
- 115.Mittag O., China C., Hoberg E., Juers E., Kolenda K.D., Richardt G., Maurischat C., Raspe H. Outcomes of cardiac rehabilitation with versus without a follow-up intervention rendered by telephone (Luebeck follow-up trial): Overall and gender-specific effects. Int. J. Rehabil. Res. 2006;29:295–302. doi: 10.1097/MRR.0b013e328010ba9a. [DOI] [PubMed] [Google Scholar]
- 116.Mohiuddin S.M., Mooss A.N., Hunter C.B., Grollmes T.L., Cloutier D.A., Hilleman D.E. Intensive smoking cessation intervention reduces mortality in high-risk smokers with cardiovascular disease. Chest. 2007;131:446–452. doi: 10.1378/chest.06-1587. [DOI] [PubMed] [Google Scholar]
- 117.Moholdt T., Bekken V.M., Grimsmo J., Slørdahl S.A., Wisløff U. Home-Based aerobic interval training improves peak oxygen uptake rqual to residential cardiac rehabilitation: S randomized, controlled trial. PLoS. One. 2012;7:e41199. doi: 10.1371/journal.pone.0041199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Molino-Lova R., Pasquini G., Vannetti F., Paperini A., Forconi T., Polcaro P., Zipoli R., Cecchi F., Macchi C. Effects of a structured physical activity intervention on measures of physical performance in frail elderly patients after cardiac rehabilitation: A pilot study with 1-year follow-up. Intern. Emerg. Med. 2013;8:581–589. doi: 10.1007/s11739-011-0654-z. [DOI] [PubMed] [Google Scholar]
- 119.Muñiz J., Gómez-Doblas J.J., Santiago-Pérez M.I., Lekuona-Goya I., Murga-Eizagaetxebarría N., de Teresa-Galván S.S.E., Cruz-Fernández J.M., Castro-Beiras A., CAM2 Project Working Group The effect of post-discharge educational intervention on patients in achieving objectives in modifiable risk factors six months after discharge following an episode of acute coronary syndrome, (CAM-2 Project): A randomized controlled trial. Health Qual. Life Outcomes. 2010;8:137. doi: 10.1186/1477-7525-8-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Munk P.S., Staal E.M., Butt N., Isaksen K., Larsen A.I. High-intensity interval training may reduce in-stent restenosis following percutaneous coronary intervention with stent implantation. Am. Heart J. 2009;158:734–741. doi: 10.1016/j.ahj.2009.08.021. [DOI] [PubMed] [Google Scholar]
- 121.Murphy A.W., Cupples M.E., Smith S.M., Byrne M., Byrne M.C., Newell J. Effect of tailored practice and patient care plans on secondary prevention of heart disease in general practice: Cluster randomised controlled trial. BMJ. 2009;339:b4220. doi: 10.1136/bmj.b4220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Mutwalli H., Fallows S., Ashmeg A., Abukhudair W., Arnous A., Zamzami M. A controlled trial of home-based cardiac rehabilitation versus usual hospital care in cardiac patients. J. Saudi Heart Assoc. 2012;24:286. doi: 10.1016/j.jsha.2012.06.231. [DOI] [Google Scholar]
- 123.Myers J., Goebbels U., Dzeikan G., Froelicher V., Bremerich J., Mueller P., Buser P., Dubach P. Exercise training and myocardial remodeling in patients with reduced ventricular function: One-year follow-up with magnetic resonance imaging. Am. Heart J. 2000;139:252–261. doi: 10.1016/S0002-8703(00)90234-5. [DOI] [PubMed] [Google Scholar]
- 124.Naughton J., Dorn J., Oberman A., Gorman P.A., Cleary P. Maximal exercise systolic pressure, exercise training, and mortality in myocardial infarction patients. Am. J. Cardiol. 2000;85:416–420. doi: 10.1016/S0002-9149(99)00765-1. [DOI] [PubMed] [Google Scholar]
- 125.Neubeck L., Freedman S., Briffa T., Bauman A., Redfern J. Four-year follow-up of the choice of health options in prevention of cardiovascular events randomized controlled trial. Eur J Cardiovasc Prev. Rehabil. 2011;18:278–286. doi: 10.1097/HJR.0b013e32833cca66. [DOI] [PubMed] [Google Scholar]
- 126.Oerkild B., Frederiksen M., Hansen J.F., Prescott E. Home-based cardiac rehabilitation is an attractive alternative to no cardiac rehabilitation for elderly patients with coronary heart disease: Results from a randomised clinical trial. BMJ Open. 2012;2:1820. doi: 10.1136/bmjopen-2012-001820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Oldenburg B., Perkins R.J., Andrews G. Controlled trial of psychological intervention in myocardial infarction. J. Consul. Clin. Psychol. 1985;53:852–859. doi: 10.1037/0022-006X.53.6.852. [DOI] [PubMed] [Google Scholar]
- 128.Oldridge N., Guyatt G., Jones N., Crowe J., Singer J., Feeny D., McKelvie R., Runions J., Streiner D., Torrance G. Effects on quality of life with comprehensive rehabilitation after acute myocardial infarction. Am. J. Cardiol. 1991;67:1084–1089. doi: 10.1016/0002-9149(91)90870-Q. [DOI] [PubMed] [Google Scholar]
- 129.Oranta O., Luutonen S., Salokangas R.K., Vahlberg T., Leino-Kilpi H. The effects of interpersonal counselling on health-related quality of life after myocardial infarction. J. Clin. Nurs. 2011;20:3373–3382. doi: 10.1111/j.1365-2702.2011.03798.x. [DOI] [PubMed] [Google Scholar]
- 130.Ornish D., Brown S.E., Billings J.H., Billings J.H., Armstrong W.T., Ports T.A., McLanahan S.M., Kirkeeide R.L., Brand R.J., Gould K.L. Can lifestyle changes reverse coronary heart disease? Lancet. 1990;336:129–133. doi: 10.1016/0140-6736(90)91656-U. [DOI] [PubMed] [Google Scholar]
- 131.Orth-Gomer K., Schneiderman N., Wang H.X., Walldin C., Blom M., Jernberg T. Stress reduction prolongs life in women with coronary disease: The stockholm women’s intervention trial for coronary heart disease (SWITCHD) Circ. Cardiovasc. Qual. Outcomes. 2009;2:25–32. doi: 10.1161/CIRCOUTCOMES.108.812859. [DOI] [PubMed] [Google Scholar]
- 132.Otterstad J.E. Influence on lifestyle measures and five-year coronary risk by a comprehensive lifestyle intervention programme in patients with coronary heart disease. Eur. J. Cardiovasc. Prev. Rehabil. 2003;10:429–437. doi: 10.1097/01.hjr.0000107024.38316.6a. [DOI] [PubMed] [Google Scholar]
- 133.Park J.H., Tahk S.J., Bae S.H., Son Y.J. Effects of a psychoeducational intervention for secondary prevention in Korean patients with coronary artery disease: A pilot study. Int. J. Nurs. Pract. 2013;19:295–305. doi: 10.1111/ijn.12067. [DOI] [PubMed] [Google Scholar]
- 134.Raffo J.A., Luksic I.Y., Kappagoda C.T., Mary D.A.S.G., Whitaker W., Linden R.J. Effects of physical training on myocardial ischaemia in patients with coronary artery disease. Br. Heart J. 1980;43:262–269. doi: 10.1136/hrt.43.3.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Rahe R.H., O’Neil T., Hagan A., Arthur R.J. Brief group therapy following myocardial infarction: Eighteen-month follow-up of a controlled trial. Int. J. Psychiatry Med. 1975;6:349–358. doi: 10.2190/T9C0-E5L6-0BJ1-5QF1. [DOI] [PubMed] [Google Scholar]
- 136.Rakowska J.M. Brief strategic therapy in first myocardial infarction patients with increased levels of stress: A randomized clinical trial. Anxiety Stress Coping. 2015;28:687–705. doi: 10.1080/10615806.2015.1004323. [DOI] [PubMed] [Google Scholar]
- 137.Redfern J., Briffa T., Ellis E., Freedman S.B. Choice of secondary prevention improves risk factors after acute coronary syndrome: 1-year follow-up of the CHOICE (Choice of Health Options In prevention of Cardiovascular Events) randomised controlled trial. Heart. 2009;95:468–475. doi: 10.1136/hrt.2008.150870. [DOI] [PubMed] [Google Scholar]
- 138.Rollman B.L., Belnap B.H., LeMenager M.S., Mazumdar S., Houck P.R., Counihan P.J., Kapoor W.N., Schulberg H.C., Reynolds C.F., III Telephone-delivered collaborative care for treating post-cabg depression a randomized controlled trial. JAMA. 2009;302:2095–2103. doi: 10.1001/jama.2009.1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Roman O., Gutierrez M., Luksic I., Chavez E., Camuzzi A.L., Villalón E., Klenner C., Cumsille F. Cardiac rehabilitation after acute myocardial infarction: 9-year controlled follow-up study. Cardiology. 1983;70:223–231. doi: 10.1159/000173598. [DOI] [PubMed] [Google Scholar]
- 140.Roncella A., Pristipino C., Cianfrocca C., Scorza S., Pasceri V., Pelliccia F., Denollet J., Pedersen S.S., Speciale G. One-year results of the randomized, controlled, short-term psychotherapy in acute myocardial infarction (STEP-IN-AMI) trial. Int. J. Cardiol. 2013;170:132–139. doi: 10.1016/j.ijcard.2013.08.094. [DOI] [PubMed] [Google Scholar]
- 141.Saffi M.A.L., Polanczyk C.A., Rabelo-Silva E.R. Lifestyle interventions reduce cardiovascular risk in patients with coronary artery disease: A randomized clinical trial. Eur. J. Cardiovasc. Nurs. 2014;13:436–443. doi: 10.1177/1474515113505396. [DOI] [PubMed] [Google Scholar]
- 142.Salminen M., Isoaho R., Vahlberg T., Ojanlatva A., Kivelä S.-L. Effects of a health advocacy, counselling, and activation programme on depressive symptoms in older coronary heart disease patients. Int. J. Geriatr. Psychiatry. 2005;20:552–558. doi: 10.1002/gps.1323. [DOI] [PubMed] [Google Scholar]
- 143.Santaularia N., Caminal J., Arnau A., Perramon M., Montesinos J., Abenoza Guardiola M., Jaarsma T. The efficacy of a supervised exercise training programme on readmission rates in patients with myocardial ischemia: Results from a randomised controlled trial. Eur. J. Cardiovasc. Nurs. 2017;16:201–212. doi: 10.1177/1474515116648801. [DOI] [PubMed] [Google Scholar]
- 144.Schneider R.H., Grim C.E., Rainforth M.V., Kotchen T., Nidich S.I., Gaylord-King C., Salerno J.W., Kotchen J.M., Alexander C.N. Stress reduction in the secondary prevention of cardiovascular disease: Randomized, controlled trial of transcendental meditation and health education in blacks. Circ. Cardiovasc. Qual. Outcomes. 2012;5:750–758. doi: 10.1161/CIRCOUTCOMES.112.967406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Schuler G., Hambrecht R., Schlierf G., Niebauer J., Hauer K., Neumann J., Hoberg E., Drinkmann A., Bacher F., Grunze M., et al. Regular physical exercise and low-fat diet. Effects on progression of coronary artery disease. Circulation. 1992;86:1–11. doi: 10.1161/01.CIR.86.1.1. [DOI] [PubMed] [Google Scholar]
- 146.Sebregts E.H.W.J., Falger P.R.J., Appels A., Kester A.D.M., Bär F.W.H.M. Psychological effects of a short behavior modification program in patients with acute myocardial infarction or coronary artery bypass grafting. A randomized controlled trial. J. Psychosom. Res. 2005;58:417–424. doi: 10.1016/j.jpsychores.2004.02.021. [DOI] [PubMed] [Google Scholar]
- 147.Shaw L.W., Oberman A., Barnes G., Eggert D., Barton S.N., Hellerstein H., Insua J., Yoran C., Fardy P., Franklin B.A., et al. Effects of a prescribed supervised exercise program on mortality and cardiovascular morbidity in patients after a myocardial infarction the national exercise and heart disease project. Am. J. Cardiol. 1981;48:39–46. doi: 10.1016/0002-9149(81)90570-1. [DOI] [PubMed] [Google Scholar]
- 148.Singh R.B., Rastogi S.S., Verma R., Laxmi B., Singh R., Ghosh S., Niaz M.A. Randomised controlled trial of cardioprotective diet in patients with recent acute myocardial infarction: Results of one year follow up. BMJ. 1992;304:1015–1019. doi: 10.1136/bmj.304.6833.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Singh R.B., Dubnov G., Niaz M.A., Ghosh S., Singh R., Rastogi S.S., Manor O., Pella D., Berry E.M. Effect of an Indo-Mediterranean diet on progression of coronary artery disease in high risk patients (Indo-Mediterranean Diet Heart Study): A randomised single-blind trial. Lancet. 2002;360:1455–1461. doi: 10.1016/S0140-6736(02)11472-3. [DOI] [PubMed] [Google Scholar]
- 150.Sivarajan E.S., Bruce R.A., Lindskog B.D., Almes M.J., Belanger L., Green B. Treadmill test responses to an early exercise program after myocardial infarction: A randomized study. Circulation. 1982;65:1420–1428. doi: 10.1161/01.CIR.65.7.1420. [DOI] [PubMed] [Google Scholar]
- 151.Specchia G., De Servi S., Scirè A., Assandri J., Berzuini C., Angoli L., La Rovere M.T., Cobelli F. Interaction between exercise training and ejection fraction in predicting prognosis after a first myocardial infarction. Circulation. 1996;94:978–982. doi: 10.1161/01.CIR.94.5.978. [DOI] [PubMed] [Google Scholar]
- 152.Stahle A., Mattsson E., Ryden L., Unden A.L., Nordlander R. Improved physical fitness and quality of life following training of elderly patients after acute coronary events—A 1-year follow-up randomized controlled study. Eur. Heart J. 1999;20:1475–1484. doi: 10.1053/euhj.1999.1581. [DOI] [PubMed] [Google Scholar]
- 153.Stern M.J., Gorman P.A., Kaslow L. The group counseling v exercise therapy study a controlled intervention with subjects following myocardial infarction. Arch. Intern. Med. 1983;143:1719–1725. doi: 10.1001/archinte.1983.00350090097016. [DOI] [PubMed] [Google Scholar]
- 154.Strandberg T.E., Pitkala K.H., Berglind S., Nieminen M.S., Tilvis R.S. Multifactorial intervention to prevent recurrent cardiovascular events in patients 75 years or older: The drugs and evidence-based medicine in the elderly (DEBATE) study: A randomized, controlled trial. Am. Heart J. 2006;152:585–592. doi: 10.1016/j.ahj.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 155.Todd C., Bradnam M.S., Cooke M.B., Ballantyne D. Effects of daily high-intensity exercise on myocardial perfusion in angina pectoris. Am. J. Cardiol. 1991;68:1593–1599. doi: 10.1016/0002-9149(91)90315-C. [DOI] [PubMed] [Google Scholar]
- 156.Toobert D.J., Glasgow R.E., Radcliffe J.L. Physiologic and related behavioral outcomes from the women’s lifestyle heart trial. Ann. Behav. Med. 2000;22:1–9. doi: 10.1007/BF02895162. [DOI] [PubMed] [Google Scholar]
- 157.Trzcieniecka-Green A., Steptoe A. The effects of stress management on the quality of life of patients following acute myocardial infarction or coronary bypass surgery. Eur. Heart J. 1996;17:1663–1670. doi: 10.1093/oxfordjournals.eurheartj.a014749. [DOI] [PubMed] [Google Scholar]
- 158.Turner A., Hambridge J., Baker A., Bowman J., McElduff P. Randomised controlled trial of group cognitive behaviour therapy versus brief intervention for depression in cardiac patients. Aust. N. Z. J. Psychiatry. 2013;47:235–243. doi: 10.1177/0004867412460592. [DOI] [PubMed] [Google Scholar]
- 159.Vahedian-Azimi A., Miller A.C., Hajiesmaieli M., Kangasniemi M., Alhani F., Jelvehmoghaddam H., Fathi M., Farzanegan B., Ardehali S.H., Hatamian S., et al. Cardiac rehabilitation using the Family-Centered Empowerment Model versus home-based cardiac rehabilitation in patients with myocardial infarction: A randomised controlled trial. Open Heart. 2016;3:e000349. doi: 10.1136/openhrt-2015-000349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Vale M.J., Jelinek M.V., Best J.D., Dart A.M., Grigg L.E., Hare D.L., Ho B.P., Newman R.W., McNeil J.J., COACH Study Group Coaching patients On Achieving Cardiovascular Health (COACH): A multicenter randomized trial in patients with coronary heart disease. Arch. Intern. Med. 2003;163:2775–2783. doi: 10.1001/archinte.163.22.2775. [DOI] [PubMed] [Google Scholar]
- 161.Van Dlxhoorn J., Duivenvoordenf H.J., Staal J.A., Poolf J., Verhagef F. Cardiac events after myocardial infarction: Possible effect of relaxation therapy. Eur. Heart J. 1987;8:1210–1214. doi: 10.1093/oxfordjournals.eurheartj.a062194. [DOI] [PubMed] [Google Scholar]
- 162.Vermeulen A., Lie K.I., Durrer D. Effects of cardiac rehabilitation after myocardial infarction: Changes in coronary risk factors and long-term prognosis. Am. Heart J. 1983;105:798–801. doi: 10.1016/0002-8703(83)90243-0. [DOI] [PubMed] [Google Scholar]
- 163.Vona M., Chapuis L., Iannino T., Ferrari E., Von Segesser L.K. Efficacy of two long-term intervention strategies to promote long-term adherence to lifestyle changes and to reduce cardiovascular events in patients with coronary artery disease. Eur. Heart J. 2009;30:474. [Google Scholar]
- 164.Vona M., Iannino T., De Pascalis S., Gallardo C., Cook S., Vermeulen B. Impact of endothelial dysfunction improvement after exercise training on prognosis in patients with recent myocardial infarction. Circulation. 2010;122:A13764. [Google Scholar]
- 165.West R.R., Jones D.A., Henderson A.H. Rehabilitation after myocardial infarction trial (RAMIT): Multi-centre randomised controlled trial of comprehensive cardiac rehabilitation in patients following acute myocardial infarction. Heart. 2012;98:637–644. doi: 10.1136/heartjnl-2011-300302. [DOI] [PubMed] [Google Scholar]
- 166.Wheeler J.R., Janz N.K., Dodge J.A. Can a disease self-management program reduce health care costs? The case of older women with heart disease. Med. Care. 2003;41:706–715. doi: 10.1097/01.MLR.0000065128.72148.D7. [DOI] [PubMed] [Google Scholar]
- 167.Wilhelmsen L., Sanne H., Elmfeldt D., Grimby G., Tibblin G., Wedel H. A controlled trial of physical training after myocardial infarction effects on risk factors, nonfatal reinfarction, and death. Prev. Med. 1975;4:491–508. doi: 10.1016/0091-7435(75)90035-3. [DOI] [PubMed] [Google Scholar]
- 168.Xavier D., Gupta R., Kamath D., Sigamani A., Devereaux P.J., George N., Joshi R., Pogue J., Pais P., Yusuf S. Community health worker-based intervention for adherence to drugs and lifestyle change after acute coronary syndrome: A multicentre, open, randomised controlled trial. Lancet Diabetes Endocrinol. 2016;4:244–253. doi: 10.1016/S2213-8587(15)00480-5. [DOI] [PubMed] [Google Scholar]
- 169.Yu C.M., Lau C.P., Chau J., McGhee S., Kong S.L., Cheung B.M., Li L.S. A short course of cardiac rehabilitation program is highly cost effective in improving long-term quality of life in patients with recent myocardial infarction or percutaneous coronary intervention. Arch. Phys. Med. Rehabil. 2004;85:1915–1922. doi: 10.1016/j.apmr.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 170.Zetta S., Smith K., Jones M., Allcoat P., Sullivan F. Evaluating the angina plan in patients admitted to hospital with angina: A randomized controlled trial. Cardiovasc. Ther. 2011;29:112–124. doi: 10.1111/j.1755-5922.2009.00109.x. [DOI] [PubMed] [Google Scholar]
- 171.Zhu L.X., Ho S.C., Sit J.W.H., He H.G. The effects of a transtheoretical model-based exercise stage-matched intervention on exercise behavior in patients with coronary heart disease: A randomized controlled trial. Patient Educ. Couns. 2014;95:384–392. doi: 10.1016/j.pec.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 172.Abell B., Glasziou P., Hoffmann T. The contribution of individual exercise training components to clinical outcomes in randomised controlled trials of cardiac rehabilitation: A systematic review and meta-regression. Sports Med. Open. 2017;3:19. doi: 10.1186/s40798-017-0086-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Anderson L., Sharp G.A., Norton R.J., Dalal H., Dean S.G., Jolly K., Cowie A., Zawada A., Taylor R.S. Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst. Rev. 2017;6:CD007130. doi: 10.1002/14651858.CD007130.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Kraal J.J., Vromen T., Spee R., Kemps H.M.C., Peek N. The influence of training characteristics on the effect of exercise training in patients with coronary artery disease: Systematic review and meta-regression analysis. Int. J. Cardiol. 2017;245:52–58. doi: 10.1016/j.ijcard.2017.07.051. [DOI] [PubMed] [Google Scholar]
- 175.Rauch B., Davos C.H., Doherty P., Saure D., Metzendorf M.I., Salzwedel A., Völler H., Jensen K., Schmid J.P. The prognostic effect of cardiac rehabilitation in the era of acute revascularisation and statin therapy: A systematic review and meta-analysis of randomized and non-randomized studies—The Cardiac Rehabilitation Outcome Study (CROS) Eur. J. Prev. Cardiol. 2016;23:1914–1939. doi: 10.1177/2047487316671181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Powell R., Mcgregor G., Ennis S., Kimani P.K., Underwood M. Is exercise-based cardiac rehabilitation effective? A systematic review and meta-analysis to re-examine the evidence. BMJ Open. 2018;8:e019656. doi: 10.1136/bmjopen-2017-019656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Clark A.M., Harding L., Vandermeer B., McAlister F.A. Meta-analysis: Secondary prevention programs for patients with coronary artery disease. Ann. Intern. Med. 2005;143:659–672. doi: 10.7326/0003-4819-143-9-200511010-00010. [DOI] [PubMed] [Google Scholar]
- 178.O’Connor G.T., Buring J.E., Yusuf S., Goldhaber S.Z., Olmstead E.M., Paffenbarger R.S., Jr., Hennekens C.H. An overview of randomized trials of rehabilitation with exercise after myocardial infarction. Circulation. 1989;80:234–244. doi: 10.1161/01.CIR.80.2.234. [DOI] [PubMed] [Google Scholar]
- 179.Oldridge N.B., Guyatt G.H., Fischer M.E., Rimm A.A. Cardiac rehabilitation after myocardial infarction. Combined experience of randomized clinical trials. JAMA. 1988;260:945–950. doi: 10.1001/jama.1988.03410070073031. [DOI] [PubMed] [Google Scholar]
- 180.Jolliffe J.A., Rees K., Taylor R.S., Thompson D., Oldridge N., Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst. Rev. 2001:CD001800. doi: 10.1002/14651858.CD001800. [DOI] [PubMed] [Google Scholar]
- 181.Heran B.S., Chen J.M., Ebrahim S., Moxham T., Oldridge N., Rees K., Thompson D.R., Taylor R.S. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst. Rev. 2011:CD001800. doi: 10.1002/14651858.CD001800.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Oldridge N. Exercise-based cardiac rehabilitation in patients with coronary heart disease: Meta-analysis outcomes revisited. Future Cardiol. 2012;8:729–751. doi: 10.2217/fca.12.34. [DOI] [PubMed] [Google Scholar]
- 183.Whalley B., Thompson D.R., Taylor R.S. Psychological interventions for coronary heart disease: Cochrane systematic review and meta-analysis. Int. J. Behav. Med. 2014;21:109–121. doi: 10.1007/s12529-012-9282-x. [DOI] [PubMed] [Google Scholar]
- 184.Anderson L., Brown J.P., Clark A.M., Dalal H., Rossau H.K., Bridges C., Taylor R.S. Patient education in the management of coronary heart disease. Cochrane Database Syst. Rev. 2017;6:CD008895. doi: 10.1002/14651858.CD008895.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Chaves G.S.S., Ghisi G.L.M., Grace S.L., Oh P., Ribeiro A.L., Britto R.R. Effects of comprehensive cardiac rehabilitation on functional capacity in a middle-income country: A randomised controlled trial. Heart. 2018:1–8. doi: 10.1136/heartjnl-2018-313632. [DOI] [PubMed] [Google Scholar]
- 186.Pesah E., Turk-Adawi K., Supervia M., Lopez Jimenez F., Bogdanska N., Grace S.L. Cardiac rehabilitation delivery in low- and middle-income countries: Availability, characteristics and barriers. World NCDs Congress. Chandigarh, India. November. Int. J. Non-Commun. Dis. 2017;2:s57–s58. [Google Scholar]
- 187.Supervia M., Turk-Adawi K., Lopez Jimenez F., Pesah E., Rongjing D., Britto R., Bjarnason-Wehrens B., Derman W., Abreu A., Babu A., et al. Nature of cardiac rehabilitation services around the globe. eClinicalMedicine. 2018 under review. [Google Scholar]
- 188.Turk-Adawi K., Sarrafzadegan N., Grace S.L. Global availability of cardiac rehabilitation. Nat. Rev. Cardiol. 2014;11:586–596. doi: 10.1038/nrcardio.2014.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Turk-Adawi K.I., Terzic C., Bjarnason-Wehrens B., Grace S.L. Cardiac rehabilitation in Canada and Arab countries: Comparing availability and program characteristics. BMC Health Serv. Res. 2015;15:521. doi: 10.1186/s12913-015-1183-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Schulz K.F., Altman D.G., Moher D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8:1. doi: 10.1186/1741-7015-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Hoffmann T.C., Glasziou P.P., Boutron I., Milne R., Perera R., Moher D., Altman D.G., Barbour V., Macdonald H., Johnston M., et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:1687. doi: 10.1136/bmj.g1687. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.