Abstract
Background
Attention-Deficit / Hyperactivity Disorder (ADHD) is one of the most prevalent behavioural disorder among children and adolescents with HIV infection (CA-HIV).
Objective
To explore the explanations used by adolescents with HIV/AIDS, caregivers and health workers to understand and explain ADHD in HIV/AIDS.
Methods
This was a qualitative sub-study nested within a larger research project whose focus was on mental health among HIV infected children and adolescents in Kampala and Masaka, Uganda (CHAKA study, 2014–2017). Participants were recruited from five study sites: two in Kampala and three in Masaka. We purposively sampled 10 ADHD adolescent-caregiver dyads equally divided between the Masaka and Kampala sites, age groups and gender. Semi-structured interviews were carried out within 12 months of baseline. Ten HIV health workers (two from each study site) participated. The ten health workers were assessed about their knowledge related to psychiatric disorders (especially ADHD in HIV/AIDS), services available for such clients and gaps in service provision for CA-HIV with behavioural / emotional disorders. Participants were recruited over one month. Taped interviews were transcribed and preliminary coding categories generated based on the research questions. Broad categories of related codes were then generated to derive a coding framework. Thematic analyses were conducted to elicit common themes emerging from the transcripts.
Results
Explanations used by respondents to express their understanding related to ADHD among CA-HIV included; psychosocial stressors, biomedical manifestations, personal traits and supernaturalism, which affected health seeking behaviour.
Conclusion
In contexts similar to those in Uganda, treatment approaches for ADHD among HIV positive CA-HIV should consider the explanations provided by CA-HIV, caregivers to CA-HIV and HIV health workers.
Keywords: ADHD, explanations, children / adolescents with HIV/AIDS (CA-HIV), compliance, Uganda
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by inattention, impulsivity, and hyperactivity1–3. Addressing the personal experiences and understanding empowers the patient, educates the caregiver, helps practitioners to appreciate that caregivers have some knowledge thus focusing on ‘a two-way flow of information'4. There is a belief in the role of the environment in the causation of ADHD and that changes in the environment are needed for treatment4. In addition, it is believed that children with ADHD are talented, gifted, with unique learning styles and strong interests, which, when accommodated, may assist their condition4. Children with ADHD may be drawn to innate healing measures, namely, engaging in rhythmical activities likely to assist their unique brain physiology4. Pharmaceutical treatment may not be sufficient for children and adolescents with ADHD and as a result, parents may use spirituality or religion as a resource5.
Illness explanations can determine help-seeking behaviour and service utilization. Illness explanations and help-seeking behaviors vary greatly depending on factors such as location, religion and social class. Individuals use resources practically, often hold multiple models of health/illness and as a result, the same people may seek help from multiple sources, when available6.
There is paucity of information concerning illness explanations about adolescent health in Uganda. Hitherto, no publication has attempted to establish how adolescents with HIV/AIDS, caregivers to CA-HIV and HIV health workers understand and explain ADHD in HIV/AIDS in the Ugandan situation. The current study was done to bridge this knowledge gap.
Methodology
This study was part of a larger research project (A cohort of 1336 children / adolescent-caregiver dyads), on mental health among HIV infected children and adolescents in Kampala and Masaka, Uganda (CHAKA study, 2014–2017). CHAKA aimed to investigate the prevalence and incidence of mental health problems among children and adolescents with HIV/AIDS. This qualitative sub-study to investigate the illness explanations related to ADHD used a methodology previously used in Goa India7. In this sub-study, the researcher purposively sampled 10 ADHD CA-HIV-caregiver dyads in which the child / adolescent had ADHD at baseline, equally divided between the Masaka and Kampala sites, children and adolescent age groups, and gender. Serial semi-structured interviews were carried out within 12 months of baseline. Baseline interviews addressed the illness explanations. Interview guides were used to explore how adolescents with HIV/AIDS, caregivers of CA-HIV and HIV health workers understood and explained ADHD in HIV/AIDS in the Ugandan situation. Participants were recruited over a month's period.
Study site
In Kampala, CA-HIV-caregiver dyads and HIV health workers were recruited from Lubowa Joint Clinical Research Centre (Lubowa, JCRC) Department of Paediatrics Clinic and from the Children's HIV Care Clinic of Nsambya hospital. In Masaka, CA-HIV-caregiver dyads were recruited from the Children's Clinic at The AIDS Support Organisation (TASO), Uganda Cares Masaka (both of which are located on the grounds of Masaka Regional Referral Hospital) and Kitovu Mobile AIDS Organisation which is located at Soweto, Masaka.
Study population
Study participants were adolescents with HIV/AIDS and ADHD, caregivers to CA-HIV with ADHD and HIV health workers at the five HIV specialized clinics in Kampala and Masaka, Uganda. The 30 participants included 10 adolescents with HIV/AIDS and ADHD, 10 caregivers to CA-HIV with ADHD, and 10 HIV health workers. In cases where both mother and father were willing to participate, one parent chose to be the caregiver and completed the demographic form. The demographic data of the participants are presented in Table 1.
Table 1.
Socio-demographic characteristics
| Kampala study sites |
Masaka study sites | ||||||
| Subgroup | N | Age categories |
Nsambya Homecare |
JCRC Lubowa |
TASO Masaka |
Uganda cares Masaka |
Kitovu Mobile AIDS Support Organisation |
| Total | 30 | 6(20%) | 6(20%) | 6(20%) | 6(20%) | 6(20%) | |
| Adolescents with ADHD and HIV/AIDS |
10 | 12–17 | 2(20%) | 2(20%) | 2(20%) | 2(20%) | 2(20%) |
| Caregivers to CA-HIV and ADHD |
10 | 18–52 | 2(20%) | 2(20%) | 2(20%) | 2(20%) | 2(20%) |
| HIV health workers |
10 | 25–40 | 2(20%) | 2(20%) | 2(20%) | 2(20%) | 2(20%) |
| Male | 14 | 3(21.4%) | 1(7.1%) | 2(14.3%) | 3(21.4%) | 5(35.7%) | |
| Female | 16 | 3(18.8%) | 5(31.3%) | 4(25%) | 3(18.8) | 1(6.3%) | |
CA-HIV and their caregivers were eligible for study enrolment if: i) the adolescent was aged between 12 and 17 years of age; ii) their caregiver was older than 17 years of age; and iii) both were able to speak English or Luganda (the local language spoken in the study area). In households where more than one CA-HIV was attending the study clinic, only one child per household was selected for inclusion into the quantitative (main) study by simple random sampling whereby all CA-HIV had an equal chance of being selected but in this sub-study, the researcher used purposive sampling. The children and adolescents involved in the study were 10. There were 10 caregivers to CA-HIV involved in the study; and 10 HIV health workers. Participants were enrolled from the five clinics. CA-HIV and their caregivers were excluded from the study if they were: i) unable to understand the study instruments for whatever reason; ii) too sick and required immediate medical attention; iii) experiencing severe psychiatric problem(s) that required admission and treatment at a major psychiatric hospital.
Materials
An MP3 recorder (Olympus Digital Voice Recorder WS-320M) was used to audio record interviews. Voice files were stored on the computer. A safety cabinet at MRC Entebbe was used to store consent forms for 3 years. A locked cabinet in the office at MRC Entebbe was used to store demographic data and transcribed interview data, which did not have participant names or identifiers.
Data collection procedure
Initially a pilot study was undertaken at Nsambya hospital where up to three CA-HIV-caregiver dyads and three HIV health workers were interviewed using the translated interview guides (separately attached). An interview schedule was piloted to assess comprehension of items and correct potential conceptual confusion. Case vignettes were used to enable participants identify manifestations of ADHD, reflect upon such experiences, enable them express their own experiences and share their illness explanations. Consent was obtained from the caregivers and assent from children older than 8 years and adolescents. As far as possible, appointments were scheduled to coincide with regular clinic visits. All interviews were carried out at the clinics in partitioned study tents which were erected to ensure privacy and limit distraction. Information was audio recorded by the researcher using digital recording. All interviews had to last between 30 to 45 minutes. This data was downloaded into computer storage and transcribed. Participants were re-reimbursed their transport costs and each child / adolescent was given a small gift as a token of appreciation for their participation at the close of each appointment. Participants not attending scheduled study appointments were contacted by telephone. Thirty interviews were conducted: sixteen in Luganda (local language), and fourteen in English. Interviews conducted in Luganda were translated into English and all interviews were transcribed.
Analysis
The taped interviews were transcribed. Special attention was given to the way local vocabulary was used for psychological phenomena. The interviews were read and, through an inductive process, preliminary coding categories were generated based on the research questions. The reliability of the coding system was tested by carrying out blinded, double coding of four interviews and, as a result, a refined consensus coding category was derived. Broad categories of related codes were then generated to derive a coding framework. After coding all the interviews, thematic analyses were conducted to elicit common themes which emerged from the transcripts.
Conceptual framework
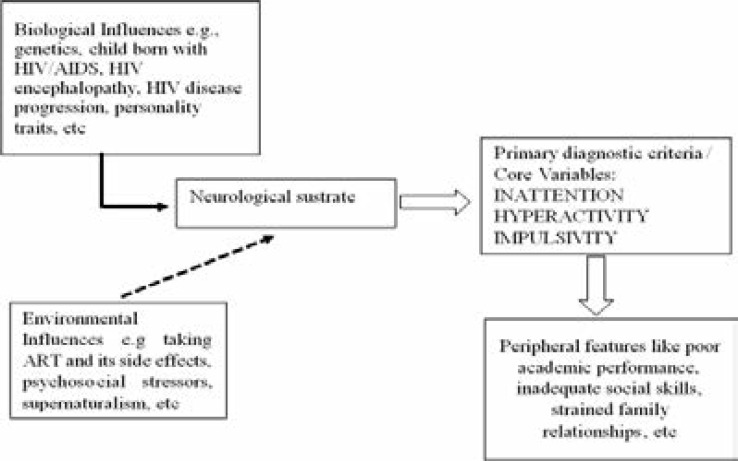
The ‘conceptual framework for ADHD illness narratives' is based on extant literature8 as illustrated in Figure 1 which suggests that biological influences (e.g., genetics, CA-HIV born with HIV/AIDS, HIV encephalopathy, HIV disease progression, personality traits, etc), plus environmental influences ( e.g taking ART and its side effects, psychosocial stressors, supernaturalism, etc) give rise to individual differences in the functional properties of neurobiological systems (e.g., dopaminergic-noradrenergic neurotransmission) that are etiologically responsible for the core psychological (i.e., cognitive and behavioural) features of ADHD. Secondary and peripheral features of ADHD (e.g., those listed as associated features in the Diagnostic and Statistical Manual of Mental Disorders 4th ed. [DSM-IV]; American Psychiatric Association, 1994) are conceptualized here as causal by-products of core features5.
Figure 1.
Conceptual framework for ADHD illness narratives
Ethical and scientific clearance
Ethical and scientific clearance for this study was sought and obtained from the Science and Ethical Committee of the Uganda Virus Research Institute (Ref: GC/127/14/04/459) and the Uganda National Council for Science and Technology (Research Registration number : HS 1601). It was made clear to all participants (adolescents and caregivers) that refusal to participate in this study would not have any negative impact upon their treatment and care. Some of the interview questions were likely to cause psychological distress; the researcher had received training on how to sensitively deliver interviews and handle situations in which sensitive information was disclosed or emotional distress observed. Participants found to have ADHD were managed in the children /adolescent mental health clinic at Butabika Hospital childrens' ward. In cases of psychiatric emergencies, the researcher (who is a Clinical Psychologist) provided emergency intervention and consulted a specialized child / adolescent mental health professional for further management.
Results
Thematic analysis showed four themes: 1) “Psychosocial Stressors, 2) “Biomedical manifestations”, 3) “Personal Traits”, and 4) “Supernaturalism”, as reflected in Table 2. Most participants were females (16) who accounted for 53% and males (14) accounted for 47%. Each of the five study sites had an equal number of participants (6) who accounted for 20%.
Table 2.
Explanatory models (illness narrative) used by CA-HIV, caregiver to CA-HIV and HIV health workers
| Psychosocial stressors (53.3%) n=16 |
Biomedical manifestations (33%) N=10 |
Personal Traits (6.7%) n=2 |
Supernaturalism (6.7%) n=2 |
|
|
Illness narrative of Adolescent with HIV/AIDS |
Extreme life-events (especially loss of parent(s) |
ART and its side effects |
Genetic factors |
Evil spirits (demons) sent from relatives |
| Rejection from relatives / caregivers |
||||
| HIV related Stigma |
HIV disease progression |
Witch-craft | ||
|
Illness narrative of Caregivers to CA-HIV |
Orphan-hood and long-term grief / worries |
ART and its side effects |
Stubbornness | Evil spirits (demons) sent from relatives |
| Family related issues (conflicts) |
||||
| Lack of adequate resources within the home environment |
HIV disease progression |
Witch-craft | ||
|
Illness narratives of HIV Health workers |
Inadequate parenting |
HIV encephalopathy |
||
| Inadequate care Lack of love / attention Rejection from families of CA-HIV |
Naming of the condition in the vignettes (ADHD)
Participants provided varying responses regarding the name of the condition in the vignette (ADHD). The naming of a condition had a greater cultural significance because the name gave significant control, power, and authority to a CA-HIV and their caregivers. Majority (9 out of 10) of adolescents who had ADHD with HIV/AIDS referred to the condition in the vignette as “eddalu lya kawukka ka siriimu”, which literally meant “mental illness related to HIV/AIDS” and certainly believed that such a condition could be treated by medical professionals specialized in HIV care at one of the specialized HIV facilities. Most (5 out of 10) caregivers to CA-HIV with ADHD named the condition in the case vignette as some form of a learning difference (Style / Difficulty / Disability) and believed that such a conditioned could be managed by educational professionals in a special needs school. Similarly, other caregivers to CA-HIV referred to the condition in the case vignette as “their childs' / adolescents' nature”, locally expressed in Luganda as “kikula kye”, and believed that such a condition could be managed by strict parenting. Some caregivers (2 out of 10) to CA-HIV with ADHD referred to the condition as “mental illness related to HIV/AIDS”, which was expressed in Luganda language as “eddalu lya kawukka ka siriimu”. Two other caregivers to CA-HIV with ADHD called it “Stubbornness”, locally expressed in Luganda language as “mputtu”, and believed that such a condition could be managed by strict parenting and use of disciplinary measures. Most (7 out of 10) of the HIV health workers called the condition as “attentional and hyperactive disorder”, while some (3 out of 10) HIV health workers called the condition “an HIV related mental illness”, and they suggested that such a condition could be managed by psychiatrists and other related mental health professionals.
Common illness explanations (themes) used by respondents to understand and explain ADHD among CA-HIV
Psychosocial stressors (53.3%); four adolescents who had HIV/AIDS suggested that “loss of a parent(s) and the HIV stigma are responsible for the extreme behavioural difficulties similar to the difficulties expressed by the child /adolescent in the vignette”. A typical example is an adolescent (interview#1) who expressed his concerns in Luganda as “okufiirwaako abazadde, okusosolebwa olwookuba n'akawukka akaleeta obulwadde bwa'mukenenya, by'ebimmu ebileeta obuzibu mu'nneeyisa efaananako ne'eyo esomedwa”, which literally meant “loss of parent(s) and HIV related stigma are some of the causes of the behavioural difficulties related to those in the vignette”. Two other adolescents suggested that “this behavioural problem in the case vignette was a result of rejection from significant caregivers that caused CA-HIV to act-out in that way”. An example is the adolescent (interview#2) who expressed his related concerns; “I was rejected by my father because of being HIV positive, my father rented for me a house when I was 11 years and later abandoned me there, I starved, I tried to stay with other relatives but faced the same rejection due to my status……all that could explain the difficulties am experiencing that are similar to those expressed in the vignette that I read”. Six caregivers suggested that “orphan-hood (longterm grief) and lack of adequate resources within the home environment for CA-HIV caused this behavioural problem in this case vignette”. An example is a caregiver (interview#3) who narrated that “okufirwaako a bazadde, ebbula ly'ebyeetaagisa ebimala, n'obutabanguko mu makka byebireeta obuzibu mu'nneeyisa efananako nn'eyo essomedwa”, which literally meant that “orphanhood, inadequate resources and family conflicts were some of the causes of the behavioural difficulties similar to those expressed in the vignette”. Another caregiver suggested that “the cause of the behavioural problem in the vignette could be due to family related issues (conflicts)”. Two HIV health workers suggested that “inadequate parenting and lack of love / attention caused this behavioural problem and the symptoms of this problem may be the way that CA-HIV happen to express their call for attention (love)”. One HIV health worker suggested that “the problem in the vignette was caused by inadequate care, coupled with rejection from families of CA-HIV”
Biomedical manifestations (33%): Three adolescents suggested that “this case in the vignette was a result of the ART and its side effects for an extended period of time plus the advanced HIV disease”. A typical example is an adolescent (interview# 4) who narrated in Luganda as “okumira eddagala ly'obulwadde obuleeta akawukka ka mukenenya ekiseera ekiwanvu, n'okukula kw'obulwadde bwa'mukenenya by'ebireeta ebuzibu mu'nneeyisa efaananako n'eyo esomedwa”, which literally meant that “taking ART for an extended period and advanced HIV were the causes of the behavioural difficulties similar to the ones expressed in the vignette”.
Conclusion
The understanding and illness explanations used by respondents to explain the cause of ADHD among CA-HIV included: psychosocial stressors, biomedical manifestations, personal traits and supernaturalism. In contexts similar to those in Uganda, treatment approaches for ADHD among HIV positive CA-HIV should consider the explanations provided by CA-HIV, caregivers to CA-HIV and HIV health workers.
Acknowledgments
The authors wish to thank the managers and staff at the five study sites (Lubowa Joint Clinical Research Centre, Nsambya homecare department Children's HIV Care clinic - Nsambya hospital, the Children's clinic at The AIDS Support Organisation - TASO Masaka, Uganda Cares / Masaka Regional Referral Hospital and Kitovu Mobile AIDS Organisation - Masaka for permitting the study to be conducted at their specialised HIV/AIDS clinics. Appreciation is extended to the Medical Research Council, Uganda (MRC, Uganda) for funding and facilitating the study. Appreciation is extended to the diligent work of research assistants Fred Nyiiro Alabiike, Jalia Nakaweesa, Diana Namugumya, Jackie Mary Mbabazi, Silvan Turinayo, Philip Amanyire, Ponsiano Twinomujune and Gerald Ssegawa. Appreciation is extended to the participants for their time and trust. This study was funded by an MRC/DfID (MRC African Research Leaders MR/L004623/1) grant awarded to Professor Eugene Kinyanda after winning an African Leadership Award.
Authors' contributions
RSM, EK, GZR, JO and KDG have made substantial contributions to conception, design, acquisition of data, drafting the manuscript, revising it critically and gave the final approval of this version to be published. Each author participated sufficiently in this work and takes public responsibility for appropriate portions of the content.
Conflict of interest disclosure
The authors report no conflict of interest in this work.
References
- 1.Biederman J, Monuteaux MC, Mick E, Spencer T, Wilens TE, Silva JM, et al. Young adult outcome of attention deficit hyperactivity disorder: a controlled 10-year follow-up study. Psychological Medicine. 2006;36(2):167–179. doi: 10.1017/S0033291705006410. [DOI] [PubMed] [Google Scholar]
- 2.Group Health Coooperative, author. ADHD Diagnosis and Treatment Guideline 2006–2012. [Google Scholar]
- 3.Swanson JM, Kinsbourne M, Nigg J, Lanphear B, Stefanatos GA, Volkow N, et al. Etiologic subtypes of attention-deficit/hyperactivity disorder: brain imaging, molecular genetic and environmental factors and the dopamine hypothesis. Neuropsychology review. 2007;17(1):39–59. doi: 10.1007/s11065-007-9019-9. [DOI] [PubMed] [Google Scholar]
- 4.Orlando CW. ‘Parental Explanatory Models of Children's Attention Deficit Hyperactive Disorder’. Doctor of Philosophy in Psychology Saybrook Graduate School and Research Center.: Saybrook Graduate School and Research Center; 2007. [Google Scholar]
- 5.Orlando CW. ‘Parental Explanatory Models of Children's Attention Deficit Hyperactive Disorder’. San Francisco, California: Saybrook Graduate School and Research Center; 2007. [Google Scholar]
- 6.Pierre A, Minn P, Sterlin C, Annoual PC, Jaimes A, Raphael F, et al. [Culture and mental health in Haiti : a literature review] Sante mentale au Quebec. 2010;35(1):13–47. doi: 10.7202/044797ar. [DOI] [PubMed] [Google Scholar]
- 7.Andrew G, Cohen A, Salgaonkar S, Patel V. The explanatory models of depression and anxiety in primary care: a qualitative study from India. BMC Research Notes. 2012;5:499. doi: 10.1186/1756-0500-5-499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rapport MD. A Conceptual Model of Child Psychopathology: Implications for Understanding Attention Deficit Hyperactivity Disorder and Treatment Efficacy. Journal of Clinical Child Psychology. 2001;30(1):48–58. doi: 10.1207/S15374424JCCP3001_6. [DOI] [PubMed] [Google Scholar]
- 9.Fielden SJ, Sheckter L, Chapman GE, Alimenti A, Forbes JC, Sheps S, et al. Growing up: perspectives of children, families and service providers regarding the needs of older children with perinatally-acquired HIV. AIDS care. 2006;18(8):1050–1053. doi: 10.1080/09540120600581460. PubMed. [DOI] [PubMed] [Google Scholar]
- 10.Petersen I, Bhana A, Myeza N, Alicea S, John S, Holst H, et al. Psychosocial challenges and protective influences for socio-emotional coping of HIV+ adolescents in South Africa: a qualitative investigation. AIDS care. 2010;22(8):970–978. doi: 10.1080/09540121003623693. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thapar A, Cooper M, Jefferies R, Stergiakouli E. What causes attention deficit hyperactivity disorder? Archives of disease in childhood. 2012;97(3):260–265. doi: 10.1136/archdischild-2011-300482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mellins CA, Brackis-Cott E, Leu CS, Elkington KS, Dolezal C, Wiznia A, et al. Rates and types of psychiatric disorders in perinatally human immunodeficiency virus-infected youth and seroreverters. Journal of Child Psychology and Psychiatry, and allied disciplines. 2009;50(9):1131–1138. doi: 10.1111/j.1469-7610.2009.02069.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS, et al. Grand challenges in global mental health. Nature. 2011;475(7354):27–30. doi: 10.1038/475027a. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gadow KD, Angelidou K, Chernoff M, Williams PL, Heston J, Hodge J, et al. Longitudinal study of emerging mental health concerns in youth perinatally infected with HIV and peer comparisons. Journal of Developmental and Behavioral Pediatrics: JDBP. 2012;33(6):456–468. doi: 10.1097/DBP.0b013e31825b8482. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nachman S, Chernoff M, Williams P, Hodge J, Heston J, Gadow KD. Human immunodeficiency virus disease severity, psychiatric symptoms, and functional outcomes in perinatally infected youth. Archives of Pediatrics & Adolescent Medicine. 2012;166(6):528–535. doi: 10.1001/archpediatrics.2011.1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wood SM, Shah SS, Steenhoff AP, Rutstein RM. The impact of AIDS diagnoses on long-term neurocognitive and psychiatric outcomes of surviving adolescents with perinatally acquired HIV. AIDS (London, England) 2009;23(14):1859–1865. doi: 10.1097/QAD.0b013e32832d924f. [DOI] [PubMed] [Google Scholar]
- 17.Havens JF, Mellins CA, Hunter JS. Psychiatric aspects of HIV/AIDS in childhood and adolescence. In: RUTTER M TE, editor. Child and adolescent psychiatry. Oxford: Blackwell; 2008. [Google Scholar]
- 18.Mellins CA, Malee KM. Understanding the mental health of youth living with perinatal HIV infection: lessons learned and current challenges. Journal of the International AIDS Society. 2013;16:18593. doi: 10.7448/IAS.16.1.18593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Monroe SM, Simons AD. Diathesis-stress theories in the context of life stress research: implications for the depressive disorders. Psychological bulletin. 1991;110(3):406–425. doi: 10.1037/0033-2909.110.3.406. [DOI] [PubMed] [Google Scholar]