Abstract
Introduction
Fruit extract of Tribulus terrestris (TT) bears aphrodisiac and antioxidative properties. Antimicrobial drug, metronidazole (MTZ) impairs the spermatogenic activity and fertility in males.
Objective
Validation of the use of fruit extract of TT as a supplement against MTZ-induced fertility impairment in males.
Methods
Adult Swiss strain male mice were administered with 500mg/kgBW/day of MTZ for 28 days. Low (100mg/kgBW/day) and high (200mg/kgBW/day) doses of TT were administered simultaneously with MTZ (500mg/kgBW/day) for same duration. All males were cohabited with virgin proestrus females. Vaginal plug formation was observed to calculate the libido index. Cohabited females were sacrificed on fifteenth day of gestation to dissect out the ovaries and uteri. Fertility index, quantal pregnancy, pre-implantation and post-implantation losses were calculated.
Results
MTZ-treated males showed unaltered mating ability, however, the females impregnated by such males exhibited marked alterations in the fertility index, quantal pregnancy and pre- and post-implantation losses. Supplementation with low dose of TT failed to restore such reproductive toxicities exhibited by administration of MTZ. However, the altered reproductive toxicities were reinstated to control values following supplementation with high dose of TT.
Conclusion
The fruit extract of TT may emerge as an effective herbal remedy, correcting the drug-induced fertility impairments in males.
Keywords: Female mice, fertility, male mice, metronidazole, Tribulus terrestris
Introduction
Herbal extracts are well established for infertility therapy and fertility regulation. The role of certain herbs in improving the reproductive impairments is well documented.1–2 Tribulus terrestris (TT) has emerged as a new source of antioxidant for infertility therapy.3 It is a flowering plant, belonging to family Zygophyllaceae4 and bears several pharmacological properties.5–7 This indigenous herb is also used in the Indian and Chinese system of medicine for the treatment of various reproductive disorders, especially in the males.8–10 The fruit of TT contains a number of different chemical substances including saponins, glycosides, flavonoids, alkaloids, resins, tannins, sugar, sterols and essential oil.11–12 Among the saponins isolated from the fruit extract of TT, protodioscin is the most popular active substance present in the extract,13–14 bearing aphrodisiac property.10 The existence of antioxidative flavonoid compound in the ethanolic fruit extract of TT has also been well documented.15–16 Our earlier findings have reported safety evaluation of the fruit extract of TT on the male reproductive health of the laboratory mouse.17 Further, ameliorating potentiality of TT has been proved against cadmium chloride-18, cypermethrin-19 and diabetes-20 induced testicular injury in the rat.
Impairments in spermatogenic activity and fertility21 and sperm morphology and fertility22 of the male mice following administration of MTZ, in our earlier findings, raised the scope to carry out a supplementation study using the fruit extract of TT in order to ameliorate its side-effects. Metronidazole (MTZ) is the first nitroimidazole,23 used for the treatment of Helicobacter pylori infections, amoebiasis, giardiasis, trichomoniasis, vaginal infections, antibiotic-associated pseudomembranous colitis, symptomatic amoebiasis24 and Crohn's disease.24–25 Earlier findings have suggested the intervention of metronidazole on the male reproductive health and fertility of laboratory rodents.26–34 The drug at the dose of 500mg/kg BW/day, administered for 4 weeks, is reported to impair spermatogenic activity21 and sperm morphology and fertility22 in the mice.
Our earlier findings have reported the beneficial properties of TT in ameliorating the MTZ-induced spermatogenic inhibition, arising as a consequence of oxidative stress in the testis35 and alterations in the histopathology of the epididymis36 in the mice. These observations raised the possibility that the interrupted fertility in male mice21 may also be corrected using the fruit extract of TT. Thus, the present study was designed with the aim to ascertain the use of the fruit extract of TT against MTZ-induced fertility impairment in the male mice.
Materials and Methods
Experimental animals
Thirty adult Swiss strain male mice (12 weeks old), and sixty adult Swiss strain female mice (10–12 weeks old), weighing 25–30g, were used in the study. All the mice were housed under standard husbandry conditions of temperature (24 ± 20°C), light (photoperiod of 14 hours light and 10 hours dark) and relative humidity (60 to 70%), in polypropylene cages, with rice husk as the bedding material. Animals were maintained on pelleted food and water ad libitum. The use of the mice was approved by the Animal Ethical Committee, Banaras Hindu University, Varanasi, India (No. Dean/11-12/CAEC/263).
Drug
MTZ (purchased from CDH, India) was dissolved in double distilled water and administered orally. The fruit of TT was purchased from the local market of Varanasi and got identified from the Department of Botany, Banaras Hindu University (Voucher No. Zygo-2013-1). The extract of the fruit was prepared by adopting the method of Hussain and co-authors10 and dissolved in distilled water for administration.
Dose selection
The human therapeutic dose of MTZ was selected and translated to mice.37 The doses of TT were standardized according to its ameliorating efficacy on MTZ-induced impairments in the fertility of the male mice.
Experimental design
The animals were divided into six groups of five each in which Group I and II served as untreated and vehicle-treated (distilled water) controls, respectively. Mice of Group III were administered with MTZ (500mg/kg BW/day) while that of Group IV were administered with the fruit extract of TT (200mg/kg BW/day), for 28 consecutive days. Mice of Groups V and VI were co-administered with MTZ (500mg/kg BW/day) and both doses of the fruit extract of TT (100mg/kg BW/day and 200mg/kg BW/day), respectively, for 28 consecutive days.
Mating ability and fertility test
Five males of each group were caged separately with two virgin proestrus females for overnight and according to the presence of vaginal plug and implantation sites in females, the mating ability and fertility of the males were assessed, respectively. The females impregnated with the treated males were weighed on the fifteenth day of gestation and sacrificed by cervical dislocation. The ovaries were removed to count the number of corpus luteum. To determine the total number of implantation sites, the uteri were dissected out and placed in 10% ammonium sulfide solution, which stained the hemosiderin pigment of resorbed implanted sites blue black.38 The numbers of live implants, as well as the pre- and post-implantation losses were noted.
Calculation
Libido index (%) = Total no. of males mated with females ÷ Total no. of males caged with females × 100
Fertility index (%) = Total no. of pregnant females ÷ Total no. of females exposed for mating × 100
Quantal pregnancy (%) = Total no. of pregnant females ÷ Total no. of females mated with the males × 100
Pre-implantation loss = Corpus luteum − (Total no. of resorbed implants + Total no. of live implants + Total no. of dead implants)
Post-implantation loss = Total no. of resorbed implants + Total no. of dead implants
Statistical analysis
Percentage values of libido index, quantal pregnancy and fertility index were analyzed by using Chi-square test. The values of the number of live implants as well as pre- and post-implantation losses were represented as mean ± S.E. in each group and analyzed by ANOVA followed by Newman- Keul's multiple range. Values were considered significant at p < 0.05.
Results
Libido index
The libido index of all the treated mice remained unimpaired, as compared with the controls (Table 1).
Table 1.
Effect of oral administration of MTZ and co-administration of MTZ and the fruit extract of TT for 28 consecutive days on the percentage of libido index, quantal pregnancy and fertility index
| Groups | Libido Index (%) |
Quantal Pregnancy (%) |
Fertility Index (%) |
| Untreated Control | 100.00 | 100.00 | 100.00 |
| Vehicle-treated Control | 100.00 | 100.00 | 100.00 |
| MTZ (500mg/kgBW/day) | 83.33 | 37.50a | 25.00a |
| TT (200mg/kgBW/day) | 100.00 | 100.00 | 100.00 |
| MTZ(500mg/kgBW/day) + TT (100mg/kgBW/day) |
83.33 | 71.42 | 50.00 |
| MTZ (500mg/kgBW/day) + TT (200mg/kgBW/day) |
83.33 | 88.88b | 66.66b |
Values are expressed in percentage.
significantly different from controls by Chi-square test at p < 0.05,
significantly different from MTZ (500mg/kgBW/day) by Chi-square test at p < 0.05
Fertility index
The females exhibited marked reduction in the fertility index to 25% when impregnated with the male mice, administered with 500mg/kg BW/day of MTZ (Table 1). This marked reduction was reinstated to 50% in the females, impregnated with the male mice, co-administered with 500mg/kg BW/day of MTZ and 100mg/kg BW/day of the fruit extract of TT and to 66.66% in the females impregnated with the male mice co-administered with 500mg/kg BW/day of MTZ and 200mg/kg BW/day of the fruit extract of TT (Table 1).
Quantal pregnancy
The females exhibited marked reduction in the quantal pregnancy to 37.50% when impregnated with the male mice, administered with 500mg/kg BW/day of MTZ (Table 1). This marked reduction was reinstated to approximately 71.42% in the females impregnated with the male mice co-administered with 500mg/kg BW/day of MTZ and 100mg/kg BW/day of the fruit extract of TT and to 88.88% in the females impregnated with the male mice co-administered with 500mg/kg BW/day of MTZ and 200mg/kg BW/day of the fruit extract of TT (Table 1).
Number of live implants
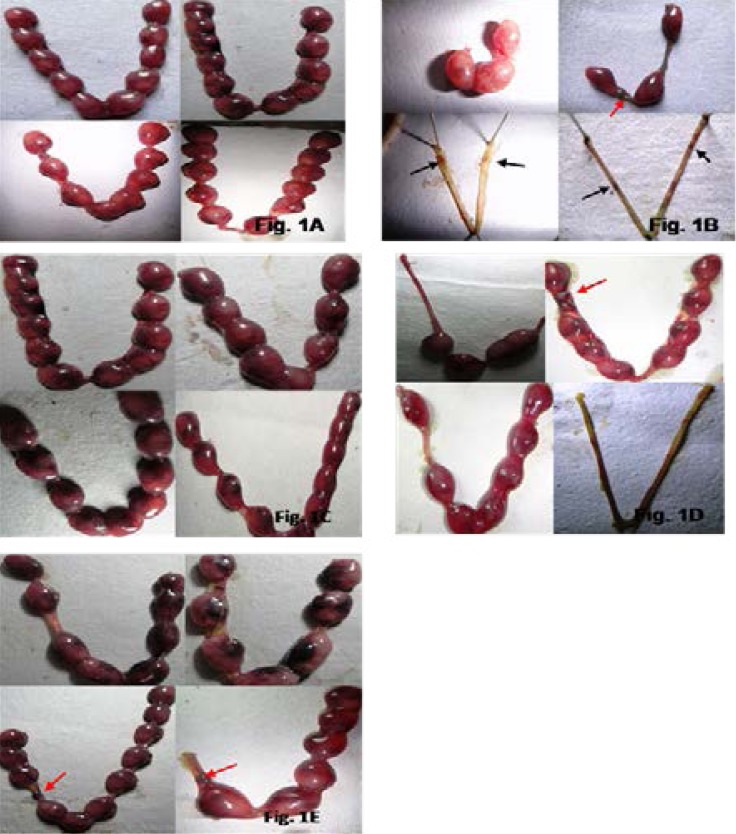
The number of live implants declined significantly in the females cohabited with the male mice, administered with 500mg/kg BW/day of MTZ, as compared with the controls (Table 2; Fig. 1B). The females impregnated with the male mice, co-administered with 500mg/kg BW/day of MTZ and 100mg/kg BW/day of the fruit extract of TT, did not show significant increase in the number of live implants (Table 2; Fig. 1D). However, significant increase was noticed in the same in the females impregnated with the male mice, co-administered 500mg/kg BW/day of MTZ and 200mg/kg BW/day of the fruit extract of TT, as compared to those administered with 500mg/kg BW/day of MTZ (Table 2; Fig. 1E), thus attained the values similar to the controls
Table 2.
Effect of oral administration of MTZ and co-administration of MTZ and the fruit extract of TT for 28 consecutive days on the number of live implants, pre-implantation loss and post-implantation loss
| Groups | No. of live implants |
Pre-implantation Loss |
Post-implantation Loss |
| Untreated Control | 7.62 ± 0.80 | 3.98 ± 0.94 | 0.75 ± 0.25 |
| Vehicle-treated Control | 7.25 ± 0.53 | 4.25 ± 1.13 | 0.41 ± 0.14 |
| MTZ(500mg/kgBW/day) | 2.75 ± 1.1a | 6.25 ± 1.1 | 1.25 ± 0.52 |
| TT (200mg/kgBW/day) | 8.33 ± 1.07 | 3.50 ± 0.76 | 0.33 ± 0.36 |
| MTZ(500mg/kgBW/day) + TT (100mg/kgBW/day) |
3.33 ± 1.13 | 6.08 ± 1.12 | 0.83 ± 0.22 |
| MTZ(500mg/kgBW/day) + TT (200mg/kgBW/day) |
5.41± 1.25b | 3.16 ± 0.73 | 0.16 ± 0.11 |
Values are mean ± SE of 10 females.
Values are considered significant by ANOVA followed by Newman- Keul's multiple range test at p < 0.05.
significantly different from controls,
significantly different MTZ(500mg/kgBW/day).
Fig. 1.
Implantation sites in the uterus of the female mice impregnated with (A.) the control male mice. Note the normal range of the numbers of implanted embryos in the left and right uteri. (B.) the male mice administered with 500mg/kgBW/day of MTZ for 28 days. Note the post-implantation loss indicated by the least number of implanted embryos in the uterus, the dead implant (red arrow) and the resorption sites indicated by scars (black arrow) observed in the uterus devoid of implanted embryos. (C.) the male mice administered with 200mg/kgBW/day of the fruit extract of TT for 28 days. Note the normal range of the numbers of implanted embryos in the left and right uteri. (D.) the male mice co-administered with MTZ (500mg/kgBW/day) and the fruit extract of TT (100mg/kgBW/day) for 28 days. Note the post-implantation loss indicated by the dead implant (red arrow), the partial recovery in the number of implanted embryos as the left and right uteri of one female was still devoid of implanted embryos. (E.) the male mice in Gr. VIII, co-administered with MTZ (500mg/kgBW/day) and the fruit extract of TT (200mg/kgBW/day) for 28 days. Note the recovery in the number of implanted embryos in the uterus. Also note a dead implant (red arrow) in the left uteri of two females.
Pre-implantation loss
Females impregnated with the male mice administered with 500mg/kg BW/day of MTZ showed a marked increase in the pre-implantation loss, as compared to the controls (Table 2; Fig. 1B). However, this loss was restored, comparable to the controls, only in the females impregnated with the males co-administered with 500mg/kg BW/day of MTZ and 200mg/kg BW/day of the fruit extract of TT (Table 2; Fig. 1E).
Post-implantation loss
Females impregnated with the male mice administered with 500mg/kg BW/day of MTZ showed a marked increase in the post-implantation loss, as compared to the controls (Table 2; Fig. 1B). However, a noticeable restoration was noted by showing a decrease in such losses, comparable to the controls, only in the females impregnated with the males co-administered with 500mg/kg BW/day of MTZ and 200mg/kg BW/day of the fruit extract of TT (Table 2; Fig. 1E).
Discussion
The present study centres around the ameliorating potentiality of the fruit extract of TT against MTZ-induced fertility impairment. The ameliorating fertilizing potentiality was evidenced by evaluating the libido index, quantal pregnancy, number of live implants, pre-implantation loss and post-implantation loss.
In the present study, MTZ administration did not affect the libido index of the mice. The libido index ranging between 80–90% suggests the unaltered mating ability of the mice, administered with 500mg/kg BW/day of MTZ. Since, libido index is an androgen-dependent parameter38 therefore, its unaltered range noticed in the present study reflects the optimal level of serum testosterone in the mice administered with MTZ (500mg/kg BW/day). This reflection is supported by the unaltered level of serum testosterone as reported in our earlier finding21.
Inspite of the unaltered mating ability of the treated males, significantly reduced number of live implants, with profound elevation in the pre-implantation and post-implantation losses were noted in the females, impregnated with the males, administered with 500mg/kg BW/day of MTZ. These findings suggest the impaired fertilizing potential of the spermatozoa, which may be due to alterations in the sperm quality. A high percentage of sperm with progressive motility is related to high fertilization index.39 Therefore, the decline in the fertility index of the females with reduced number of live implants in the uteri might be due to severely depressed motility of epididymal spermatozoa in the mice administered with 500mg/kg BW/day of MTZ as reported in our earlier findings,36 thus, suggesting an impaired sperm transport in the reproductive tract.
Further, the decline in quantal pregnancy indicates the anti-implantation effect of MTZ. Pre-implantation losses might have arisen due to disruption of events which are prerequisite for fertilization or an impairment in the production of cytokines, growth factor and various types of adhesion molecules either by the developing blastocyst or by the uterine epithelium around the site of implantation. 40–42 The increase in the post-implantation loss following 500mg/kg BW/day of MTZ administration may be attributed to the direct damage to the sperm DNA, caused by the free radicals or reactive oxygen species released by the inflammatory cells.42 The post-implantation loss may also be attributed to the oxidative stress, produced in the testis of MTZ-treated mice, as reported in our earlier study.35
In the present study, fertility of the MTZ-treated males was improved following co- administrations of MTZ and 200mg/kg BW/day of the fruit extract of TT, as evidenced by recovery in the fertility index, quantal pregnancy, the number of live implants and pre- and post-implantation losses in the females impregnated with such males. Our earlier findings reporting the reappearance of several spermatozoa in the epididymal lumen, as evidenced through histopathological study, following co-administrations of 500mg/kg BW/day of MTZ and 200mg/kg BW/day of the fruit extract of TT36, also support the present study. Therefore, improvements in the number of live implants and pre- and post-implantation losses might be due to the beneficial properties exhibited by the fruit extract of TT on the quality and quantity of spermatozoa, 43–47 thus increasing the fertility potential of the MTZ-treated mice.
Conclusion
MTZ, administered at the dose of 500mg/kg BW/day for 28 days impairs the fertility in the males. The fruit extract of TT bears the potentiality to restore the impaired fertility and hence, may emerge as an effective herbal remedy in improving the drug-induced fertility impairments in the males.
Acknowledgement
The authors are thankful to Banaras Hindu University and UGC, New Delhi, for providing financial assistance.
Conflict of interest
None.
References
- 1.Riaz A, Khan RA, Ahmed S, Afroz S. Assessment of acute toxicity and reproductive capability of a herbal combination. Pak J Pharm Sci. 2010;23:291–294. PubMed. [PubMed] [Google Scholar]
- 2.Adaay MH, Mattar AG. Effect of aqueous and ethanolic extracts of Tribulus terrestris, Phoenix dactylifera and Nasturtium officinale mixture on some reproductive parameters in male mice. J Baghdad Sci. 2012;9:640–650. [Google Scholar]
- 3.Zheleva-Dimitrova D, Obreshkova D, Nedialkov P. Antioxidant activity of Tribulus terrestris- A natural product in infertility therapy. Int J Pharm Pharmaceut Sci. 2012;4:508–511. [Google Scholar]
- 4.Sharma PC, Yelne MB, Dennis TJ. Database on medicinal plants used in Ayurveda and Sidha. Vol. 3. New Delhi: CCRAS, Dept. of AYUSH, Ministry of Health and Family Welfare, Govt. of India; 2000. p. 229. [Google Scholar]
- 5.Bhandari B, Deepti C, Kohli SK. Pharmacological effects of Tribulus terrestris, A Review. Int J Contem Med. 2013:1. [Google Scholar]
- 6.Verma P, Galib, Patgiri BJ, Prajapato PK. Tribulus terrestris: A phytopharmacological review. JAyur Hol Med. 2013;1:37–43. [Google Scholar]
- 7.Hashim S, Bhakt T, Marwat KB, Jan A. Medicinal properties, phytochemistry and pharmacology of Tribulus terrestris (Zygophyllaceae) Pak J Bot. 2014;46:399–404. [Google Scholar]
- 8.Brown AG, Vukovich MD, Martini ER, Kohut LM, Frank WD, Jackson DA, et al. Endocrine and lipid responses to chronic androstenediol-herbal supplementation in 30 to 58 year old men. J Am Coll Nutr. 2002;20:520–528. doi: 10.1080/07315724.2001.10719061. PubMed. [DOI] [PubMed] [Google Scholar]
- 9.Gauthaman K, Ganesan AP, Prasad RN. Sexual effects of puncturevine (Tribulus terrestris) extract (protodioscin): an evaluation using a rat model. J Alternat Complement Med. 2003;9:257–265. doi: 10.1089/10755530360623374. [DOI] [PubMed] [Google Scholar]
- 10.Hussain AA, Muhammad AA, Ibrahim HH, Abbas A. Study of the biological activities of Tribulus terrestris extracts. World Acad Sci Engin Technol. 2009;57:433–435. [Google Scholar]
- 11.Raja M, Venkataraman R. Pharmacognostical studies on Tribulus terrestris and Tribulus alatus. Der Pharmacia Sinica. 2011;2:136–139. [Google Scholar]
- 12.Kumar A, Bhardwaj A. Comparative, qualitative and quantitative chemotypic characterization among North India Tribulus terrestris. Int Res J Pharm. 2012;3:212–218. [Google Scholar]
- 13.Mahato SB, Sahu NP, Ganguli AN, Miyahara K, Kawasaki TJ, Steroidal glycosides. of Tribulus terrestris. J Chem Soc Perkin Trans. 1981;1:2405–2410. [Google Scholar]
- 14.Koumanov F, Bozadjieva E, Andreeva M, Platonva E, Ankov V. Clinical trial of Tribestan. Expt Med. 1982;1:2–4. [Google Scholar]
- 15.Gomathi S, Shanmugapriya A, Bharathi V, Gayathri G, Karpagam T. Antimicrobial activities and phytochemical studies of aqueous and ethanolic fruit extracts of Tribulus terrestris. IJPI'S J Pharma Herbal Formul. 2012;2:47–51. [Google Scholar]
- 16.Mitra N, Mohammad-Mehndi D, Mohammad-Reza Z. Tribulus terrestris (Zygophyllaceae) flavonoid compounds. Int J Mod Bot. 2012;2:35–39. [Google Scholar]
- 17.Kumari M, Kumar P, Singh P. Safety Evaluation of Tribulus terrestris on the male reproductive health of laboratory mouse. Int J Pharma Phytopharmacol Res. 2015;4(5):281–287. [Google Scholar]
- 18.Rajendar B, Bharavi K, Rao GS, Kishore PVS, Kumar PR, Kumar CSVS, Patel PT. Protective effect of an aphrodisiac herb Tribulus terrestris linn on cadmium-induced testicular damage. Ind J Pharmacol. 2011;43:568–573. doi: 10.4103/0253-7613.84974. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharma P, Haq AU, Singh R. Cypermethrin induced reproductive toxicity in male Wistar rats: Protective role of Tribulus terrestris. J Environ Biol. 2012;34:857–862. [PubMed] [Google Scholar]
- 20.Tag HM, Abdelazek HMA, Mahoud YS, El-Shenawy NS. Efficacy of Tribulus terrestris extract and metformin on fertility indices and oxidative stress of testicular tissue in streptozotocin-induced diabetic male rats. African J Pharm Pharmacol. 2015;9:1088–1098. [Google Scholar]
- 21.Kumari M, Singh P. Study on the reproductive and fertility of the male mice following administration of metronidazole. Int J Fertil Steril. 2013;3:225–238. [PMC free article] [PubMed] [Google Scholar]
- 22.Kumari M, Singh P. Effects of metronidazole on sperm morphology and fertility of the laboratory mouse. J Sci Res. 2015;59:71–80. [Google Scholar]
- 23.Edwards DI. Nitroimidazole drugs-action and resistance mechanisms, 1: Mechanisms of action. J Antimicrob Chemo. 1993;31:9–20. doi: 10.1093/jac/31.1.9. [DOI] [PubMed] [Google Scholar]
- 24.Lofmark S, Edlund C, Nord CE. Metronidazole is still the drug of choice for the treatment of anaerobic infections. Clin Infect Dis. 2010;20:16–23. doi: 10.1086/647939. [DOI] [PubMed] [Google Scholar]
- 25.Achkar JP, Hanauer SB. Medical therapy to reduce postoperative Crohn's disease recurrence. Am J Gastroenterol. 2000;95:1139–1146. doi: 10.1111/j.1572-0241.2000.02000.x. PubMed. [DOI] [PubMed] [Google Scholar]
- 26.McClain RM, Downing JC, Edgcomb JE. Effect of metronidazole on fertility and testicular function in male rats. Toxicol Sci. 1989;12:386–396. doi: 10.1016/0272-0590(89)90014-6. [DOI] [PubMed] [Google Scholar]
- 27.Grover JK, Vats V, Srinivas M, Das SN, Gupta DK, Mitra DK. Effect of metronidazole on spermatogenesis and FSH, LH and testosterone levels of pre-pubertal rats. Indian J Exp Biol. 2001;39:1160–1152. [PubMed] [Google Scholar]
- 28.El-Nahas AF, El-Ashmawy IM. Reproductive and cytogenetic toxicity of metronidazole in male mice. Pharmacol Toxicol. 2004;94:226–231. doi: 10.1111/j.1742-7843.2004.pto940505.x. [DOI] [PubMed] [Google Scholar]
- 29.Mudry MD, Carballo M, Labal de Vinuesa M, González Cid M, Larripa I. Mutagenic bioassay of certain pharmacological drugs: III. Metronidazole (MTZ) Mutat Res. 1994;305:127–132. doi: 10.1016/0027-5107(94)90230-5. [DOI] [PubMed] [Google Scholar]
- 30.Raji Y, Kunle-Alabi OT, Olaleye SB, Gbadegesin MA, Awobajo FO, Osonuga OA, Odukanmi AO, Salami SA, Bolarinwa AF. Impact of α-tocopherol on metronidazole and tetracycline-induced alterations in reproductive activities of male albino rats. J Bio Sci. 2007;7:41–46. [Google Scholar]
- 31.Sohrabi D, Alipour M, Mellati AA. Effect of metronidazole on spermatogenesis, plasma gonadotrophins and testosterone in rats. Iranian J Reprod Med. 2007;5:69–72. [Google Scholar]
- 32.Karbalay-Doust S, Noorafshan A. Ameliorative effects of curcumin on the spermatozoa tail length, count, motility and testosterone serum level in metronidazole-treated mice. Prag Med Rep. 2011;112:288–297. [PubMed] [Google Scholar]
- 33.Ligha AE, Bokolo B, Didia BC. Antifertility potential of metronidazole in male Wistar rats. Pak J Biol Sci. 2012;15:224–230. doi: 10.3923/pjbs.2012.224.230. PubMed. [DOI] [PubMed] [Google Scholar]
- 34.Oda SS. Histopathological and biochemical alterations of metronidazole-induced toxicity in male rats. Global Veterin. 2012;9:303–310. [Google Scholar]
- 35.Kumari M, Singh P. Tribulus terrestris ameliorates metronidazole-induced spermatogenic inhibition and testicular oxidative stress in the laboratory mouse. Indian J Pharmacol. 2015;47:304–310. doi: 10.4103/0253-7613.157129. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kumari M, Singh P. Ameliorating potentiality of Tribulus terrestris against metronidazole-induced epididymal alterations. Int J Recent Sci Res. 2014;5:1926–1932. [Google Scholar]
- 37.Reagen-Shaw S, Nihal M, Ahmad N. Dose translation from animal to human revisited. The FASEB J. 2007;22:659–661. doi: 10.1096/fj.07-9574LSF. [DOI] [PubMed] [Google Scholar]
- 38.Narotsky MG, Brownie CF, Kavlock RJ. Critical period of carbon tetrachloride-induced pregnancy loss in Fischer-344 rats, with insights into the detection of resorption sites by ammonium sulfide staining. Teratol. 1997;56:252–261. doi: 10.1002/(SICI)1096-9926(199710)56:4<252::AID-TERA4>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 39.Donnelly ET, Lewis SEM, McNally JA, Thompson W. In vitro fertilization and pregnancy rates: the influence of sperm motility and morphology on IVF outcome. Fertil Steril. 1998;70:305–314. doi: 10.1016/s0015-0282(98)00146-0. PubMed. [DOI] [PubMed] [Google Scholar]
- 40.Wu FCW. Androgen and male sexual function. In: Bhasin S, et al., editors. Pharmacology, biology and clinical applications of androgens, current status and future aspects. New York: Willey Liss; 1996. pp. 191–199. [Google Scholar]
- 41.Denker HW. Implantation : a cell biological paradox. J Exp Zool. 1993;266:541–558. doi: 10.1002/jez.1402660606. [DOI] [PubMed] [Google Scholar]
- 42.Haimovici F, Anderson DJ. Cytokines and growth factors in implantation. Microscopy Res Tech. 1993;25:201–207. doi: 10.1002/jemt.1070250303. [DOI] [PubMed] [Google Scholar]
- 43.Chellman GJ, Bus JS, Working PK. Role of epididymal inflammation in the induction of dominant lethal mutations in F344 rat sperm by methyl chloride. Proc Natl Acad Sci USA. 1986;83:8087–8091. doi: 10.1073/pnas.83.21.8087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Arsyad KM. Effect of protodioscin on the quality and quantity of sperms from males with moderate idiopathic oligozoospermia. Medica. 1996;22:614–618. PubMed. [Google Scholar]
- 45.Singh PK, Singh AP, Gupta AK, Chaudhary S. Beneficial effects of aqueous fruit extract of Tribulus terrestris on testicular and serum biochemistry of albino rats. J Ecophysiol Occup Hlth. 2009;9:217–223. [Google Scholar]
- 46.Martino-Andrade Aj, Morais RN, Spercoski KM, Rossi SC, Vechi MF, Golin M, Lombardi NF, Greca CS, Dalsenter PR. Effects of Tribulus terrestris on endocrine sensitive organs in male and female Wistar rats. J Ethanopharmacol. 2010;127:165–170. doi: 10.1016/j.jep.2009.09.031. PubMed. [DOI] [PubMed] [Google Scholar]
- 47.Singh S, Nair V, Gupta YK. Evaluation of the aphrodisiac activity of Tribulus terrestris Linn. In sexually sluggish male albino rats. J Pharmacol Pharmacother. 2012;3:43–47. doi: 10.4103/0976-500X.92512. [DOI] [PMC free article] [PubMed] [Google Scholar]