Abstract
Objectives and background
Hysterectomy is the most commonly performed major gynecological operation for both benign and malign gynecologic conditions. After hysterectomy, although some investigators have declared an increased incidence of urinary and anorectal dysfunction, some others could not show any connection.
Methods
The voluntary patients were divided in two groups: abdominal hysterectomy (Group 1) and vaginal hysterectomy (Group 2). Anal manometry and all the other examinations of the patients were performed at the Department of General Surgery Endoscopy Unit of Ankara University, Faculty of Medicine.
Results
When the quality of life of the patients was assessed before the operation and on the 12th post-operative month via the SF-36 form; it can be seen that body pain parameters of the patients in Group 1 had significantly improved and there is no statistical difference in other parameters. When the effect of hysterectomy on the quality of life of the patients was evaluated by the “Cleveland Clinic Global Quality of Life” form, the statistically significant improvement in the quality of life of the patients in Group 2 was observed.
Conclusion
If the type of operation (vaginal or abdominal) is performed due to benign causes, it does not affect the urinary and anorectal functions of the patients. Depending on the decrease of complaints of the patients, it has a positive effect on the quality of life.
Keywords: Hysterecetomy, anorectal functions, life quality
Introduction
Hysterectomy is the most commonly performed major gynecological operation for both benign and malign gynecologic conditions1. Despite its low post-operative morbidity, the surgical dissection within the pelvis may disrupt the local nerve supply and anatomic integrity of pelvic organs that results in negative implications for social life, sexuality, and psychological condition of the patient2,3. Nonetheless, the effects of hysterectomy on pelvic organ functions are controversial. After hysterectomy, although some investigations have declared an increased incidence of urinary and anorectal dysfunction, some others could not show any connection2,4,5. Therefore, we conducted this prospective study in order to investigate the effects of abdominal and vaginal hysterectomy on urinary and anorectal functions while evaluating the perception of the patients for their quality of life.
Methods
The voluntary patients who had undergone abdominal or vaginal hysterectomy operations were included in the scope of the study after they filled out the informed consent form before operation. The patients were divided in two groups as abdominal hysterectomy (Group 1) and vaginal hysterectomy (Group 2).
Patients who had been operated on the anorectal region for any reason before or after the operation, who had anal incontinence or neurological impairment before the operation, patients who had an operation other than hysterectomy which may cause urinary or anal incontinence after the operation, or who had illness, were excluded from the study. During the course of our study, 19 out of 61 patients with hysterectomy indications were excluded from the study due to previous anorectal operation or urinary incontinence. The remaining 4 patients did not agree to participate in the study.
Apart from the exclusion criteria, twenty patients who underwent abdominal hysterectomy (Group 1) and 18 patients, who underwent vaginal hysterectomy (Group 2), were enrolled in this study. Twenty patients in Group 1 were diagnosed as myoma uteri and 5 patients were diagnosed as having an ovarian cyst in addition to myoma uteri. Total abdominal hysterectomy was applied to 10 patients and total abdominal hysterectomy+bilateral salpingoopherectomy was applied to other 10 patients in Group 1. In Group 2; 6 patients were diagnosed as myoma uteri, and diagnosis of the other 12 patients was uterine prolapsus. Vaginal hysterectomy operation was applied to all the patients in this group.
In order to assess the anorectal functions and pressures, anal manometry was applied to the patients before the operation and on the post-operative 12th month. At the same time, the patients' quality of life were measured by “SF 36 quality of life scale” and ‘Cleveland Clinic Global Quality of Life’ form. As part of the Medical Outcomes Study, a multi-year, multi-site study to explain variations in patient outcomes, RAND developed the 36-Item Short Form Health Survey (SF-36). SF-36 is a set of generic, coherent, and easily administered quality-of-life measures. These measures rely upon patient self-reporting and are now widely utilized by managed care organizations and by Medicare for routine monitoring and assessment of care outcomes in adult patients. The Cleveland Global Quality of Life (CGQL) is a patient-rated score that was developed by the senior author (Victor W. Fazio) and has been used at this institution since 1986 as a measurement of QOL. It has previously been validated in patients with colitis undergoing stapled restorative proctocolectomy in this institution. Changes in urinary function of the patients and their intestinal functions, whether any gas or fecal incontinence developed or not were assessed by the “Anorectal and urinary functions assessment form” that is prepared by us. Also, the development of constipation after hysterectomy was measured by the Constipation Scoring System Rome-II criteria6. The Rome II criterias have been made by “Functional GI Disorders Coordinating Committee”. The patient should also have at least one of the following symptoms: Abnormal stool frequency, abnormal stool form, abnormal stool passage, passage of mucus and bloating or feeling of abdominal distension, on at least a quarter of occasions or days.
In constipation scoring system, over 15 points was accepted as constipation. Number of parity, abortus and whether they received hormone replacement therapy after hysterectomy or not were recorded in the “Anorectal and urinary functions assessment form”.
For the anal manometry measurements; 11-channel, microcapillary aero infusion vectorial manometry system (Stationary GI manometry UPS-2020, Medical Measurement Systems, Enschede, The Netherlands)consisting of 8 channels pressure+2 channels swallowing, and respiration and channel EMG motility system was used. In this computer-controlled system, measurements were taken by the mechanism that retracted the catheter with a fixed speed of 1 mm/second.
Before anal manometry, a soft enema was applied to the patients 1 or 2 hours. Then the patients were laid in left lateral position and anal manometry was applied. During the test, the initial volume felt by the patients, the volume causing the need for defecation, the volume giving rise to the need for emergency defecation and the maximum volumetric volume, rectoanal inhibitor reflex, anal resting pressures, anal squeeze pressures and high-pressure zone lengths were recorded. The pre-operative and post-operative values of anal manometry results were compared both between the groups and within each group.
‘Quality of Life Scale’, ‘Cleveland Clinic Global Quality of Life’ form and ‘Clinical Assessment form’ were graded and pre-operative and post-operative grades were compared both between the groups and also within each group. Research Ethics Committee approved the study (No: 51-1249). Statistical analysis was performed by the ‘SPSS (Statistical Package for Social Science) 11.5 for Windows package program. The sf-36 results of the groups were analyzed by Wilcoxon Signed Ranks Test. The difference in physical function and vitality between the two groups was assessed with Mann Whitney U test. The results were assessed by Chi-Square, Mann Whitney U test, Student T test, Wilcoxon Signed Ranks test and matched sample test and the p values less than 0.05 were accepted as statistically significant.
Results
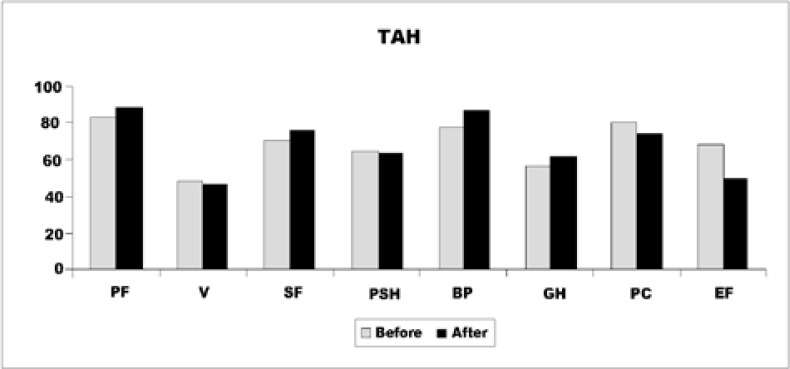
While the average age of the patients in Group 1 was 46.95±3.6 years, average age of the patients in Group 2 was 55.05±10.3 years. Total follow-up term was mean 15.7±4.4 months for Group 1 and 12.3±3.7 months (p>0.05) for Group 2. When the patients' quality of life were assessed before the operation and on the 12th postoperative month via the SF-36 form; it can be seen that body pain parameters of the patients in Group 1 had significantly improved and there was no statistical difference in other parameters also (Figure 1).
Figure 1.
SF-36 results of Group 1. (PF=physical function, V=vitality, SF=social function, PSH=psycological health, BP=body pain, GH=general health, PC=physical condition)
In Group 1, the gravidity was 4.35 +/− 2.52, parity 2.75 +/− 1.33, abortus 1.6 +/− 1.6, while in Group 2 the graviditiy was 6.72 +/− 2.37, parity 3.83 +/− 1.15, abortus 2.66 +/− 2.11. In group 2, both gravidity and parity ratios were found higher.
In Group 1, 17 (85%) patients did not receive hormone replacement therapy. In group 2, only 3 (16.7%) received HRT treatment. As a result, the use of HRT treatment did not affect our outcome and was analyzed by the Chi-Square test with a value of p> 0.05.
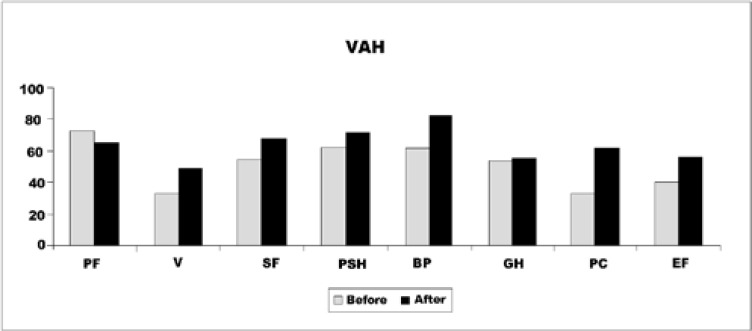
In Group 2, it was determined that vitality, mood, body pain and physical condition had significantly amended after the operation (p<0.05) and there was no statistical difference in other parameters of quality of life form. As can be seen generally in Figure 2, that the patients' quality of life had improved.
Figure 2.
SF-36 results of Group 2. (PF=physical function, V=vitality, SF=social function, PSH=psycological health, BP=body pain, GH=general health, PC=physical condition)
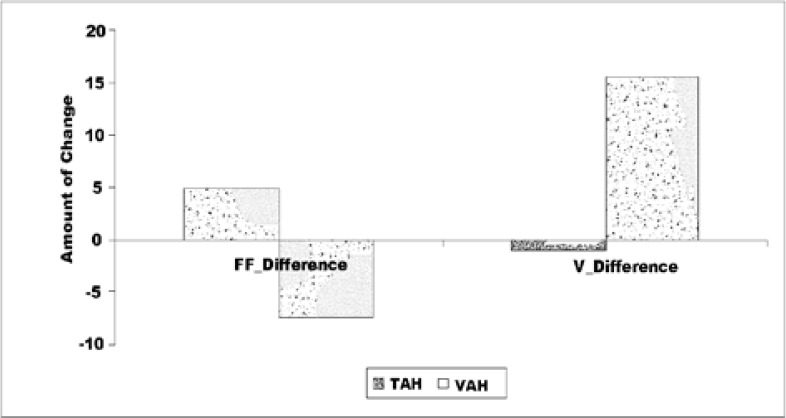
When the difference in the sub-scale scores of the SF 36 form was compared between the groups, while an improvement in physical function was observed in Group 1, vitality was increased in Group 2 (Figure 3). However, when evaluated in general, no significant difference was found between the two groups.
Figure 3.
The difference of physical function and vitality between the groups.
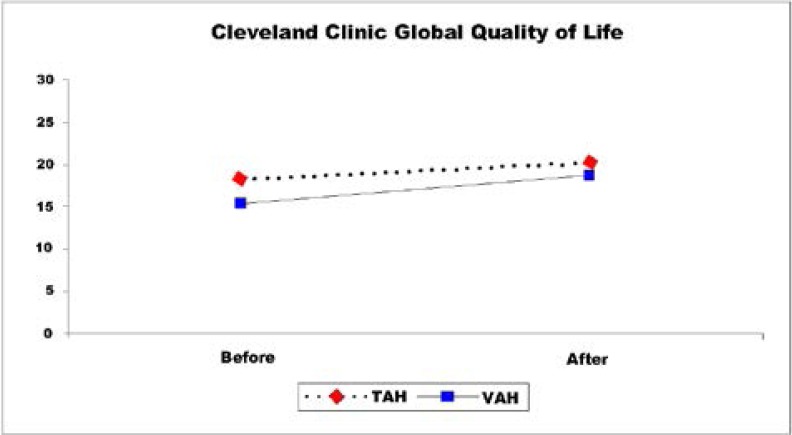
When the effect of the hysterectomy on the quality of life of the patients was evaluated by the “Cleveland Clinic Global Quality of Life” form, the statistically significant improvement in the quality of life of the patients in Group 2 was observed as shown in Figure 4 (p=0.018).
Figure 4.
Comparison of ‘Cleveland Clinic Global Quality of Life’ test results before and after the operation (Mann-Whitney U test).
In Table 1, anal incontinence assessment results of the patients before and after the operation are given. There was no difference in the gas incontinence complaints and its frequency in AI1 (Anal incontinence assessment question 1) in both groups (Table 2).
Table 1.
Comparison of pre-operative and post-operative levels of anal incontinence assessment questions within and between groups (The frequencies of the YES responders to the anal incontinence questions were taken into account.) The Wilcoxon Signed Ranks test was used for pre-operative and post-operative values. The Mann-Whitney U test was used for comparison within the groups
| TAH (n=20) | VAH (n=18) | |||||||
| Frequency | % | p† | Frequency | % | p† | p‡ | ||
| AI1 | Before | 7 | 35.0 | 1.00 | 11 | 61.1 | 1.00 | 0.107 |
| After | 6 | 30.0 | 10 | 55.6 | 0.188 | |||
| AI2 | Before | 1 | 5.0 | * | 0 | 0 | * | 1,00 |
| After | 0 | 0 | 0 | 0 | * | |||
| AI3 | Before | 1 | 5.0 | * | 0 | 0 | * | 1.00 |
| After | 0 | 0 | 0 | 0 | * | |||
| AI4 | Before | 5 | 25.0 | 0.219 | 3 | 16.7 | 0.625 | 0.697 |
| After | 1 | 5.0 | 1 | 5.6 | 1.00 | |||
| AI5 | Before | 0 | 0 | * | 2 | 11.1 | * | 0,218 |
| After | 0 | 0 | 0 | 0 | * | |||
Comparison in groups
Comparison within groups;
No comparison)
Table 2.
Comparison of pre-operative and post operation levels of gas souling and gaita incontinence frequency in groups. Wilcoxon Signed Ranks test was used. (AI=Anal Incontinence)
| TAH (n=20) | VAH (n=18) | ||||||
| Average | Standart Deviation |
p | Average | Standart Deviation |
p | ||
| AIGAS | Before | 0.8 | 1.37 | 0.641 | 2.0 | 2.21 | 0.719 |
| After | 1.1 | 1.93 | 2.1 | 2.27 | |||
| AIGAITA | Before | 0.5 | 0.83 | 0.037* | 0.37 | 0,37 | 0.317 |
| After | 0.1 | 0.22 | 0.24 | 0.24 | |||
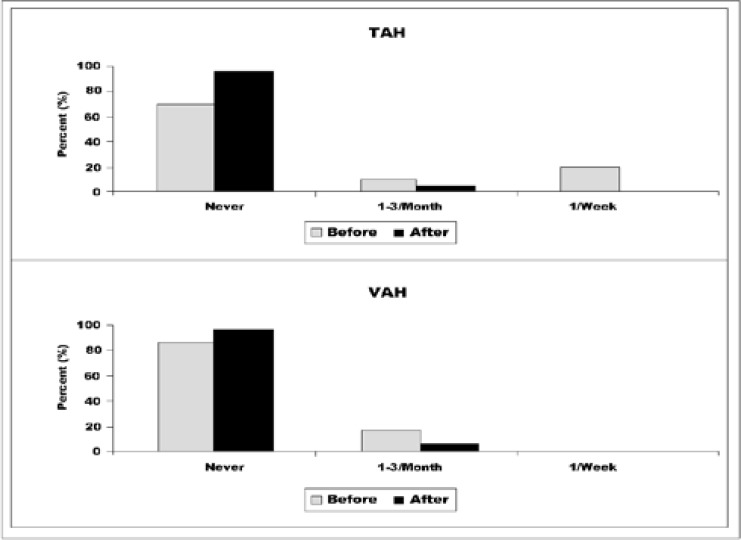
On the other hand, a significant decrease was observed in the frequency in Group 1 for AI2 (Anal incontinence assessment question 2), while there was no difference in fecal incontinence (p=0,037) (Figure 5). No difference was observed in Group 2.
Figure 5.
Anal incontinence frequencies of Group 1 and 2.
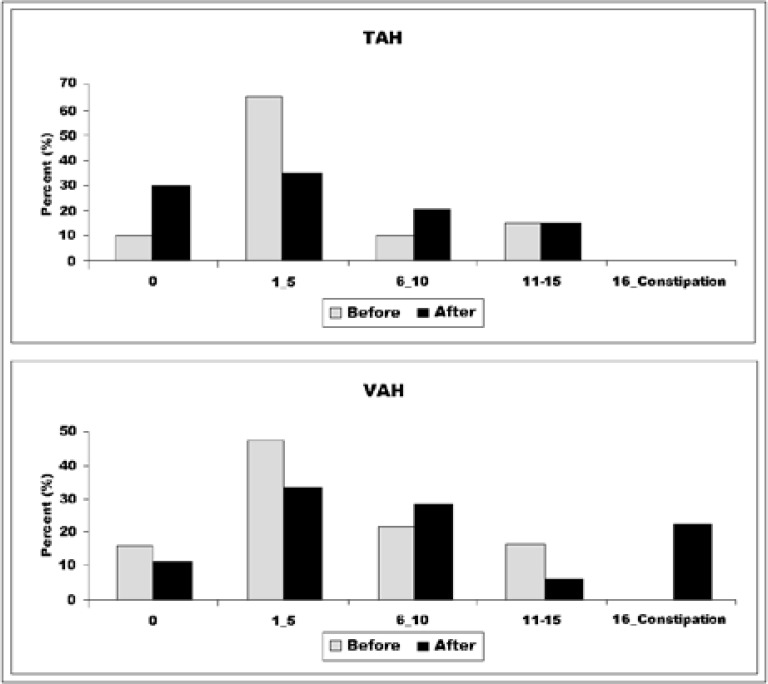
In Table 3, pre-operative and post-operative values of the patients according to ‘Constipation Scoring System’ (CSS) are seen. While there was no difference before and after the operation in patients in Group 1, it was observed that constipation scoring of the patients in Group 2 had statistically increased (p<0,021) (Figure 6). In addition, no statistically significant differences were observed in the bowel habits of the patients before and after operation in both groups.
Table 3.
Comparison of preoperative and postoperative values of CSS levels within groups. The Wilcoxon Signed Ranks test was used. (p<0,05)
| TAH (n=20) | VAH (n=18) | ||||||||||
| Average | Standart Deviation |
Min. | Max. | p | Average | Standart Deviation |
Min. | Max. | p | ||
| CSS | Before | 1.3 | 0.86 | 0 | 3 | 0.480 | 1.4 | 0.96 | 0 | 3 | 0.021* |
| After | 1.2 | 1.06 | 0 | 3 | 1.9 | 1.35 | 0 | 4 | |||
Figure 6.
Distribution of patients according to CSS
It was seen that there was no difference in the results of anal manometry performed before and after the operation. The differences between the initial sensation (IS), defecation sensation (DS), maximum sensation (MS), anal canal resting mean pressure (ARP), anal canal outflow mean pressure (AOP) and high-pressure zone length of the patients were not found statistically significant (p> 0.05). Rectoanal inhibitor reflex (RAIR) was detected preoperatively and post-operatively in all patients. In Table 4, it can be seen that no statistically significant difference was found in the comparison of the manometry results between the groups.
Discussion
In this prospective study, it was revealed that hysterectomy due to benign disorders does not affect the urinary and anorectal functions of the patients, whether it is done via abdominal or vaginal route. In addition, it was found that the complaints of the patients were ameliorated, therefore resulting in a favorable effect on their quality of life.
Hysterectomy is performed in 90% of cases due to benign causes (leiomyoma, endometriosis / adenomyosis, dysfunctional uterine bleeding and chronic pelvic pain). After the indication of hysterectomy is established, the question is how the surgery will be performed. The effects of hysterectomy on quality of life, anorectal and urinary functions are still controversial. Myoma uteri, endometriosis, pelvic pain, dysfunctional uterine bleeding are common causes of hysterectomy which often reduce the quality of life of patients besides threatening their lives. According to the World Health Organization (WHO), quality of life consists of six essential principles. These can be sequenced as physical condition, psychological status, level of independence, social relations, harmony with the environment, personal, spiritual and religious beliefs7. It is shown that women with chronic pelvic pain and conditions that are associated with other gynecological disorders report worse health-related quality of life8. After hysterectomy is performed, it is shown that the patients' quality of life may get worse, reach normal levels or even increase9. In our work, we have reported that body pain parameters of the patients in Group 1 were significantly improved. Also in Group 2 patients, vitality, mood, body pain and physical condition were significantly amended after hysterectomy.
During hysterectomy, dissection of bladder from the uterus is required. This may change the innervation of the bladder resulting in urinary disorders, however previous studies performed give conflicting results10. The first publication in this regard was reported by Hanley in 1969, and reported that total abdominal hysterectomy (TAH) caused an increase in incontinence, dysuria and urinary frequency11. In some prospective studies examining the effects of hysterectomy, it is shown that surgery has significant effects on bladder function11,2. When we examined our results, we found that there was no difference between the pre-operative and post-operative values in urologic function results between Group 1 and Group 2 and within the groups.
Many studies have evaluated the correlation between hysterectomy and post-operative intestinal disorder. In a previous retrospective study, negative effects of hysterectomy operation (regardless of its type) on the intestinal functions are shown11. Daniel Altman et al. reported in their prospective study that patients undergoing abdominal hysterectomy may run an increased risk for developing mild to moderate anal incontinence post-operatively. Besides, their findings do not correlate hysterectomy with de novo or deteriorating constipation12. However, there are conflicting results on bowel function in more recent prospective studies. In one of them, Lakeman et. al. considered that although defecation symptoms are also more common after vaginal hysterectomy, the difference was not statistically significant10. In addition to this study, Humalajarvi et.al. have showed that hysterectomy reduces pelvic floor symptoms in one-year follow-up, whether the patients have accompanying pelvic organ prolapsus or not13. On the other hand, in a recent longitudinal study, it was shown that hysterectomy for benign gynecologic disorders have significant detrimental effects on pelvic floor functions2. When the intestinal habits were examined in our study, it was seen that there is no difference in the patients in Group 1 and in Group 2 during the postoperative 12 months. Also, it seemed that, abdominal or vaginal hysterectomy has no effect on bowel functions.
Formerly, Sood et.al. observed in their study that resting and squeeze sphincter pressures, volume of saline infused at first leak, total volume retained, and threshold volume for maximum tolerable volume are all decreased significantly after hysterectomy for cervical cancer14. However, in more recent work of Loizzi et.al., it was found that maximal and mean anal resting and squeezing pressures were unaffected by the surgical procedure, rectoanal inhibitory reflex and length of the high anal pressure zone did not change when a nerve sparing technique was used15. In our study, there was no statistically significant difference between the groups both in abdominal hysterectomy group and in vaginal hysterectomy group in terms of the manometry results before and after the operation. Also, there was no difference between the groups. The limitation of our study was a small number of subjects and there is a need for work to be done with wider series.
Conclusion
If the type of operation (vaginal or abdominal) is performed due to benign reasons, it can be said that it does not affect the urinary and anorectal functions of the patients, and also it has a positive effect on the quality of life depending on the decrease of complaints of the patients. However, although constipation does not fully develop in the patients who have undergone vaginal hysterectomy, it is also important to consider that there is an increase in constipation complaints.
Conflict of interest
There is no conflict of interest between the authors.
References
- 1.Basket TF. Hysterectomy: Evolution and trends. Best Pract Res Clin Obstet Gynecol. 2005;19:295–305. doi: 10.1016/j.bpobgyn.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 2.Kocaay AF, Oztuna D, Su FA, Elhan AH, Kuzu MA. Effects of Hysterectomy on Pelvic Floor Disorders: A Longitudinal Study. Dis Colon Rectum. 2017;60:303–310. doi: 10.1097/DCR.0000000000000786. PubMed. [DOI] [PubMed] [Google Scholar]
- 3.Selcuk S, Cam C, Asoglu MR, Kucukbas M, Arinkan A, Cikman MS, Karateke A. Effect of simple and radical hysterectomy on quality of life - analysis of all aspects of pelvic floor dysfunction. Eur J Obstet Gynecol Reprod Biol. 2016;198:84–88. doi: 10.1016/j.ejogrb.2016.01.008. [DOI] [PubMed] [Google Scholar]
- 4.Engh MA, Otterlind L, Stjerndahl JH, Löfgren M. Hysterectomy and incontinence: a study from the Swedish national register for gynecological surgery. Acta Obstet Gynecol Scand. 2006;85:614–618. doi: 10.1080/00016340600555942. [DOI] [PubMed] [Google Scholar]
- 5.Van Hoboken EA, Timmermans FG, van der Veek PP, Weyenborg PT, Masclee AA. Colorectal motor and sensory function after hysterectomy. Int J Colorectal Dis. 2014;29:505–510. doi: 10.1007/s00384-013-1823-5. PubMed. [DOI] [PubMed] [Google Scholar]
- 6.Hillila MT, Farkkila MA. Prevalence of irritable bowel syndrome according to different diagnostic criteria in a non-selected adult population. Aliment Pharmacol Ther. 2004;20:339–345. doi: 10.1111/j.1365-2036.2004.02034.x. [DOI] [PubMed] [Google Scholar]
- 7.Rannestad T. Hysterectomy: effects on quality of life and psychological aspects. Best Pract Res Clin Obstet Gynaecol. 2005;19:419–430. doi: 10.1016/j.bpobgyn.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 8.Jones GL, Kennedy SH, Jenkinson C. Health-related quality of life measurement in women with common benign gynecologic conditions: a systematic review. Am J Obstet Gynecol. 2002;187:501–511. doi: 10.1067/mob.2002.124940. PubMed. [DOI] [PubMed] [Google Scholar]
- 9.Rannestad T, Eikeland O-J, Helland H, Qvamström U. The quality of life in women suffering from gynecological disorders is improved by means of hysterectomy. Acta Obstet Gynecol Scand. 2001;80:46–51. doi: 10.1034/j.1600-0412.2001.800109.x. [DOI] [PubMed] [Google Scholar]
- 10.Lakeman MM, van der Vaart CH, Roovers JP. A longterm prospective study to compare the effects of vaginal and abdominal hysterectomy on micturition and defecation. BJOG. 2011;118:1511–1517. doi: 10.1111/j.1471-0528.2011.03080.x. [DOI] [PubMed] [Google Scholar]
- 11.Hanley HG. The late urological complications of total hysterectomy. Br J Urol. 1969;41:682–684. doi: 10.1111/j.1464-410x.1969.tb09977.x. [DOI] [PubMed] [Google Scholar]
- 12.Altman D, Zetterström J, Lopez A, Pollack J, Nordenstram J, Mellgren A. Effect of hysterectomy on bowel function. Dis Colon Rectum. 2004;47:502–509. doi: 10.1007/s10350-003-0087-5. PubMed. [DOI] [PubMed] [Google Scholar]
- 13.Humalajärvi N, Aukee P, Kairaluoma MV, Stach-Lempinen B, Sintonen H, Valpas A, Heinonen PK. Quality of life and pelvic floor dysfunction symptoms after hysterectomy with or without pelvic organ prolapse. Eur J Obstet Gynecol Reprod Biol. 2014;182:16–21. doi: 10.1016/j.ejogrb.2014.08.032. [DOI] [PubMed] [Google Scholar]
- 14.Sood AK, Nygaard I, Shahin MS, Sorosky JI, Lutgendorf SK, Rao SS. Anorectal dysfunction after surgical treatment for cervical cancer. J Am Coll Surg. 2002;195:513–519. doi: 10.1016/s1072-7515(02)01311-x. [DOI] [PubMed] [Google Scholar]
- 15.Loizzi V, Cormio G, Lobascio PL, Marino F, De Fazio M, Falagario M, Leone L, et al. Bowel dysfunction following nerve-sparing radical hysterectomy for cervical cancer: a prospective study. Oncology. 2014;86:239–243. doi: 10.1159/000362213. PubMed. [DOI] [PubMed] [Google Scholar]