Abstract
Osteitis pubis is a common cause of chronic groin pain, especially in athletes. Although a precise etiology is not defined, it seems to be related to muscular imbalance and pelvic instability. Diagnosis is based on detailed history, clinical evaluation, and imaging, which are crucial for a correct diagnosis and proper management. Many different therapeutic approaches have been proposed for osteitis pubis; conservative treatment represents the first-line approach and provides good results in most patients, especially if based on an individualized multimodal rehabilitative management. Different surgical options have been also described, but they should be reserved to recalcitrant cases. In this review, a critical analysis of the literature about athletic osteitis pubis is performed, especially focusing on its diagnostic and therapeutic management.
Keywords: osteitis pubis, pubalgia, groin pain, rehabilitation, review
Introduction
Osteitis pubis is a painful chronic overuse condition affecting the pubic symphysis and surrounding soft tissues. It is characterized by pelvic pain and local tenderness over the pubic symphysis. It commonly affects athletes, especially those who participate in sports that involve kicking, turning, twisting, cutting, pivoting, sprinting, rapid acceleration and deceleration or sudden directional changes.1 Osteitis pubis has been described in athletes who play sports such as soccer, rugby, ice hockey, Australian Rules football and distance running.2
The diagnosis is difficult because of the anatomical complexity of the groin area, the biomechanics of the pubic symphysis region and the large number of potential sources of groin pain. Also, nomenclature is often confusing, resulting in different terms that describe similar clinical conditions.3
We present a review of literature to examine the current knowledge of osteitis pubis, with particular interest in the management of athletes suffering from this condition.
Materials and methods
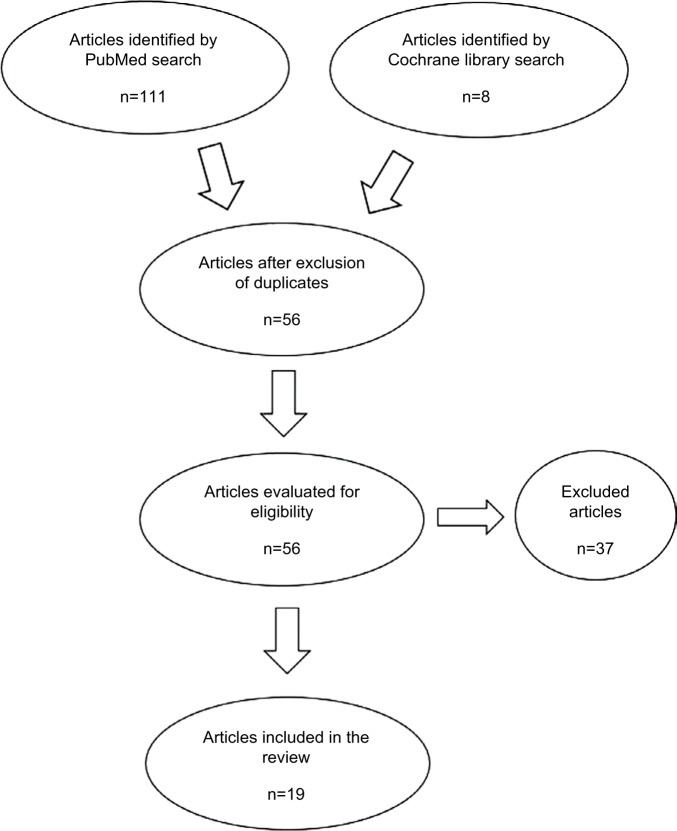
This work represents a descriptive non-systematic review on the management of osteitis pubis in athletes. A search of two databases (PubMed and Cochrane Library) was performed using the terms “osteitis pubis” or “pubalgia” in the title of articles combined with the terms “athlete,” “athletic,” “sport,” “training,” “rehabilitation” and “rehabilitative” as keywords. Search results were limited to articles written in English and published between January 1, 2012 and August 31, 2018. The decision to limit the bibliographic research to the most recent literature is due to the fact that the purpose of this article was to perform a descriptive and not a systematic review of literature. This is certainly a limitation, but it must be also considered that all recent literature is strongly influenced by the previous one. The search with the aforementioned criteria provided a total of 56 articles. As a fundamental criterion for inclusion in the review, the studies had to deal with recent concepts in the diagnosis and therapy of osteitis pubis in athletes. Articles that did not specifically concern osteitis pubis, but dealt generically with groin injuries without distinguishing osteitis pubis from the frequently associated pathologies, were excluded. Articles concerning osteitis pubis in non-athletes were also excluded. To avoid selection bias, all the authors analyzed the search results and disagreement over article inclusion was resolved by consensus. Eventually, 19 articles met the inclusion criteria and 37 articles were excluded (Figure 1). Only one of the selected articles is a prospective double-blinded controlled study (level I), while most of the studies are retrospective case series, case reports or reviews of literature (Table 1). For each article, the level of evidence is defined on the basis of the classification shown in Table 2.4
Figure 1.
Flow chart for search and selection of articles.
Table 1.
Characteristics of selected studies
| Author and year | Study design | Main conclusions | Levels of evidence |
|---|---|---|---|
| Angoules, 20152 | Review | OP is usually self-limiting and responds well to conservative treatment; in chronic recalcitrant cases surgical approach is needed | IV |
| Hegedus et al, 201314 | Review | Following a precise paradigm should lead to a more successful diagnosis and treatment of athletic pubalgia | IV |
| Beatty, 201222 | Review | Treatment includes non-operative measures of rest, rehabilitation, pharmacotherapy and may also include injections or surgery | IV |
| Jardí et al, 201526 | Case series | The protocol presented ensures a safe return for elite athletes, with full recovery longer in football players and increasing with age | IV |
| Cheatham et al, 201530 | Review | There is grade D evidence that a non-operative program is effective in helping athletes return to their pre-injury levels | III |
| Schöberl et al, 201731 | Prospective double-blinded controlled | Non-surgical therapy is successful in treating athletic osteitis pubis. Shock wave therapy reduced pain, thus enabling return to football within 3 months of trauma | I |
| McAleer et al, 201732 | Case series | A non-operative rehabilitative protocol is successful in athletes with osteitis pubis, enabling return to sport within 11 weeks | IV |
| Elattar et al, 201634 | Review | A variety of surgical options have been reported for athletic pubalgia, with successful outcomes and high rates of return to sport | IV |
| Gupta et al, 201542 | Case series | Endoscopic pubic symphysectomy is a safe, minimally invasive treatment for recalcitrant osteitis pubis | IV |
| Matsuda et al, 201543 | Case series | Endoscopic pubic symphysectomy is a minimally invasive procedure that may be useful in treating recalcitrant osteitis pubis | IV |
| Larson, 201446 | Review | An association between FAI and athletic pubalgia has been recognized, with better outcomes reported when both are managed concurrently or in a staged manner | IV |
| Ross et al, 201547 | Review | There is a subset of athletes that presents both athletic pubalgia and intra-articular hip disorders such as FAI | IV |
| Kajetanek et al, 201848 | Retrospective non-controlled | In patients with athletic pubalgia, a la carte surgery confined to the injured structure(s) produces excellent return to play outcomes | IV |
| Masala et al, 201749 | Prospective non-randomized non-controlled | Pulse-dose radio frequency is an effective and safe technique in the management of chronic pubalgia in athletes | IV |
| Scholten et al, 201550 | Case report | Ultrasound-guided needle tenotomy and PRP injection can be a safe and effective option in refractory cases of athletic pubalgia | IV |
| Henning, 201457 | Review | Overuse injuries can usually be managed non-operatively through rest and control of regional muscle imbalances | IV |
| McAleer et al, 201558 | Case report | A nine-point conservative strategy has been successful in an elite football player | IV |
| Rossidis et al, 201559 | Retrospective review | Laparoscopic hernia repair accompanied by an ipsilateral adductor longus tenotomy is a useful surgical technique for athletic pubalgia | IV |
| Ellsworth et al, 201460 | Review | A precise distinction between athletic pubalgia and inguinal disruption allows for an efficient rehabilitative plan of care | IV |
Abbreviations: FAI, femoroacetabular impingement; OP, osteitis pubis; PRP, platelet rich plasma.
Table 2.
Classification of levels of evidence
| Levels of evidence | Criteria for analysis and inclusion |
|---|---|
| I | Meta-analysis and systematic reviews of randomized, controlled trials (RCTs) of high quality, or RCTs with minimum or low risk of bias. Systematic reviews of high quality relative to cohort studies or case–controls. |
| II | Cohort studies or randomized case–controls of high quality with minimal risk of confounding or bias and with high or discrete probability of causation. |
| III | Case–control studies and retrospective comparison of well-conducted studies with reasonable probability of causation. |
| IV | Non-analytic studies as case series or individual cases. |
Epidemiology and pathogenesis
Osteitis pubis is a common source of groin pain in athletes. The incidence in athletes has been reported as 0.5%–8%, with a higher incidence in distance runners and athletes participating in kicking sports, in particular in male soccer players, who account for 10%–18% of injuries per year.5,6
The etiology is not completely clear and is still being debated. Muscle imbalance between the abdominal and hip adductor muscles is currently considered the most important pathogenetic factor in the development of osteitis pubis.7 Abdominal muscles act synergistically with the posterior paravertebral muscles to stabilize the pelvis. They allow a single-leg stance while maintaining balance and contributing to the power and precision of the kicking leg. Stabilization during the single-leg stance also results from gluteus and adductor muscle activity. The adductors are antagonists to the abdominal muscles. Imbalances between abdominal and adductor muscle groups disrupt the equilibrium of forces around the symphysis pubis, predisposing the athlete to a subacute periostitis caused by chronic microtrauma.8 Reduced internal rotation of the hip and instability of the sacroiliac joint could represent other possible predisposing factors as they lead to increased shearing stress in the pelvis.9
Whatever the cause, the biomechanical overload leads to a bony stress response in the parasymphyseal bone and/or degenerative changes in the cartilage of the pubic symphysis, usually in the absence of inflammatory findings.10
Diagnosis
Even though osteitis pubis is considered a self-limiting condition, players with groin pain frequently have to stop sporting activities for many months and long absence from sports is not feasible for high level athletes. For this reason, an early diagnosis and a multimodal therapeutic approach are mandatory. The diagnosis of osteitis pubis starts with recording the history and clinical evaluation. Athletes suffering from osteitis pubis typically present anterior and medial groin pain. Pain may also affect pubic symphysis, adductor musculature, lower abdominal muscles, perineal region, inguinal region or scrotum.11 Pain may be unilateral or bilateral, and it is exacerbated by running, kicking, hip adduction or flexion, and eccentric loads to the rectus abdominis.12
At clinical evaluation, tenderness on palpation of the symphyseal region is common. However, clinical examina tion is not standardized and includes various tests, such as lateral compression and pubic symphysis gap test with isometric adductor contraction.8 Verrall et al13 proposed three provocation tests (i.e., Single Adductor, Squeeze and Bilateral Adductor tests) for the assessment of chronic groin pain in athletes, with bilateral adductor test exhibiting the best metrics.14 Restricted range of hip motion, positive FABER test, sacroiliac joint dysfunction and weakness of abductor or adductor muscles can be associated with clinical findings.6 In addition, some authors suggest that local corticoid and/or anesthetic injections in the pubic symphysis may be helpful diagnostic tools.15,16
Rodriguez et al8 classified athletes with osteitis pubis into four stages, based on clinical examination and diagnostic features (Table 3). However, it is not a validated classification and only empiric in nature since the authors included only a small number of patients.
Table 3.
Stages of osteitis pubis
| Stages | Side of pain | Site of pain | Characteristics of pain |
|---|---|---|---|
| 1 | Unilateral, dominant | Inguinal, with radiation to adductors | Pain alleviation after warm-up, pain exacerbation after training |
| 2 | Bilateral | Inguinal and adductors | Pain exacerbation after training |
| 3 | Bilateral | Groin, adductor region, suprapubic, abdominal | During training, kicking, sprinting, turning. Cannot achieve training goals, forced to withdraw |
| 4 | Generalized | Generalized, radiation to lumbar region | Walking, getting up, straining at stool, simple activities of daily living |
Diagnosis is challenging because of the anatomical complexity of the groin area, the biomechanics of the pubic symphysis region and the large number of potential sources of groin pain (Table 4).6,17 A differential diagnosis is mandatory.
Table 4.
Differential diagnosis of groin pain
| Intra-articular pathologies | Extra-articular pathologies | Non-musculoskeletal disorders |
|---|---|---|
| Femoroacetabular Impingement Syndrome (FAI) | Insertional adductors and rectus abdominis tendinopathy | Genitourinary |
| Acetabular labral tears | Groin pain disruption | Adnexa torsion |
| Chondral lesions | Osteitis pubis | Nephrolithiasis |
| Femoral neck stress fractures | Adductor muscles injuries | Orchitis |
| Osteoarthrosis | Lumbar radiculopathy | Ovarian cystis |
| Transitory synovitis | Pubic ramus stress fracture | Pelvic inflammatory disease |
| Osteonecrosis of the femoral head | Apophyseal avulsion fractures | Urinary tract infections |
| Osteochondritis dissecans | Internal snapping hip syndrome | Endometriosis |
| Legg–Calvè–Perthes disease | Greater trochanter pain syndrome | Prostatitis |
| Epiphysiolysis of the femoral head | Sacroiliac joint disorders | Testicular cancer |
| Septic arthritis | Nerve entrapment | Testicular torsion |
| Oncologic process | Intra-abdominal pathologies | |
| Sports hernia | ||
| Inguinal hernia | ||
| Appendicitis | ||
| Diverticulitis/Diverticulosis | ||
| Lymphadenitis | ||
| Inflammatory bowel disease |
Note: Data from Maffulli et al.6
Imaging is not pathognomonic, but radiographs, triple-phase scintigraphy and MRI can assist physical examination and confirm diagnosis and/or exclude other pathologies and possible sources of groin pain.18
Plain radiographs may demonstrate symphyseal bony sclerosis, erosions and widening or narrowing of the joint, especially in the chronic phase, while radiographic changes may be absent in the early or mild forms of the condition.19
A “flamingo view” (an anterior–posterior view of the pelvis with the patient standing on one leg) can give evidence of pelvic instability (Figure 2), as a vertical subluxation greater than 2 mm or a widening of the symphysis greater than 7 mm are considered pathognomonic.20
Figure 2.
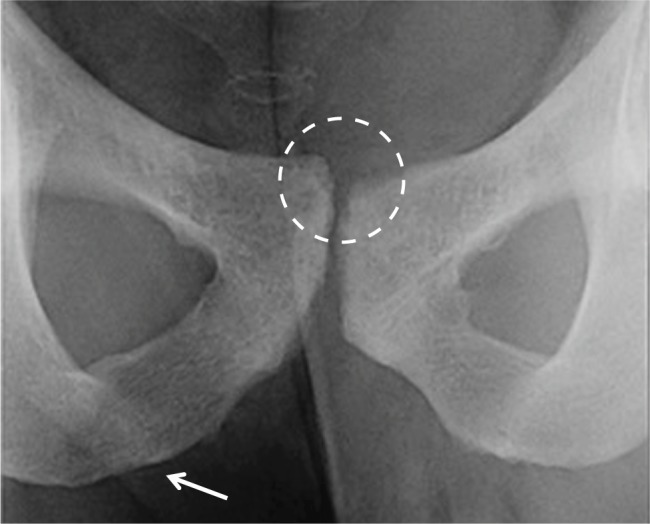
“Flamingo view” radiograph (obtained with the patient bearing weight alternately on each leg) that shows vertical pubic subluxation greater than 2 mm and underlying degenerative changes.
Note: A caudal osteolysis is visible on the right side (arrow).
Bone scintigraphy may reveal increased tracer uptake in the pubic symphysis region and parasymphyseal bone, even though the degree of uptake is poorly correlated with duration and severity of symptoms.21
As a gold standard, MRI provides a more detailed view of the symphysis pubis and surrounding soft tissues as well as the bony pelvis and hips. The most common finding in athletic osteitis pubis of less than 6-month duration is the presence of a hyper-intense signal on T2-weighted images within the symphysis and adjacent parasymphy- seal region (Figure 3); on the other hand, subchondral sclerosis, subchondral resorption with bony irregularity and osteophytosis or pubic beaking are characteristic of chronic phases.7
Figure 3.
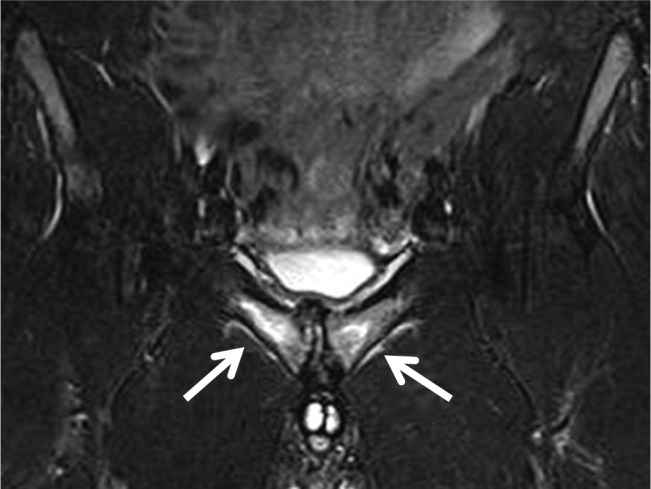
Coronal T2 fat suppression MRI image showing marked bilateral diffuse symphyseal bone marrow edema and parasymphyseal edema (arrows).
Nevertheless, some studies report similar marrow edema in asymptomatic athletes also; so a correlation between MRI and clinical examination is mandatory.22,23
Recently, some authors proposed dynamic ultrasonography as a non-invasive diagnostic tool for evaluating osteitis pubis, but its high operator-dependency and lack of precise methodological criteria seem to determine a poor reproducibility.24
Treatment and return to sport
Osteitis pubis is typically described as a self-limiting condition that improves with rest. However, management of groin pain is sometime difficult and patients can undergo extended periods of rest, which is not feasible for athletes. Different treatments have been proposed, ranging from conservative management to surgical procedures. Unfortunately, few level one studies have been published in the most recent literature and most of the scientific articles are retrospective case series or case reports, making it difficult to draw conclusions about this topic (Table 1).
Conservative treatment
Conservative management includes rest, limited activity, ice and anti-inflammatory drugs, followed by a rehabilitation program. Conservative management aims to correct muscular imbalance around the pubic symphysis, and it usually consists of a progressive exercise program, involving stretching and pelvic musculature strengthening.25 Physical therapy is usually prescribed and a progressive sport-specific program is indicated before a return to sporting activities.25 However, there is a lack of standard rehabilitative protocols, resulting in extremely different rehabilitative programs, with variable outcomes and time to recovery.
Recent studies underline the importance of an individualized progressive multimodal rehabilitation program.26–29 In this program, patients are moved through the protocol stages after they are able to perform exercises without pain and have achieved adequate levels of motion and core stability grading.27,29 The first stage is to focus on pain control and improve lumbo-pelvic stability. Gentle prolonged stretching, except for the adductors and ischiopubic muscles, is started. Cycling on an exercise bike is introduced as cardiovascular training. In the second stage, Swiss balls and other aids are indicated for performing resistance and strengthening exercises of the pelvis, abdominal and gluteal muscles. Abdominal core isometrics targeting the transversus abdominis, abdominal crunches, gluteal bridges with and without resistance bands, Swiss ball exercises for abdominal core, manual hip strengthening and resistance hip strengthening with band are indicated. The third and fourth stages included eccentric hip exercises, side stepping with bands, lunge and squat exercises and progressive sport-specific training. Running is gradually increased, and changes of pace and direction are introduced. To reproduce the sport requirements, athletes start training on the field, performing exercises mimicking their sport. Kicking is allowed only at the end of this stage. Eccentric abdominal wall strengthening exercises are started. Good results have been reported with this progressive rehabilitation program, despite some differences between protocols.26 Most of the athletes return to pre-injury levels within 3 months (from 4 to 14 weeks). Moreover, a successful long-term follow-up was reported between 6 and 48 months for all patients.30
In one of these studies, Jardì et al26 described a specific conservative protocol for the treatment of six elite athletes in three different sports (two football, two basketball, two rugby players) who were diagnosed with osteitis pubis stage III and IV according to Rodriguez classification.8 The average time to start squad training was 2 months, while an average of 3 months was required to return to competition. Basketball players had the shortest recovery, followed by rugby and football players. No recurrences were reported at a follow-up of at least two seasons. However, the results of this study are limited by the small cohort of included patients.
In a recent prospective double-blinded controlled level I study, Schöberl et al31 analyzed amateur football players with osteitis pubis and divided them into three groups. Patients in groups 1 and 2 received an intensive 3-phase rehabilitation program. Group 1 additionally received three weekly sessions of shock wave therapy directly on the pubis, while group 2 was treated with sham shock wave therapy. The control group was treated with rest and stopping of participation in all sporting activities; they did not receive shock wave therapy. Forty-two of the 44 players of groups 1 and 2 returned to football within 4 months, but return-to-sport was significantly earlier in group 1. No recurrences were reported in both groups at 1-year follow-up. On the other hand, time to return-to-play was significantly longer (8 months) in the control group, and players frequently experienced recurrent groin pain during the first year. Physiotherapy seems to have been successful for treatment of osteitis pubis in the athletes, and local shock wave therapy significantly reduced pain, thus enabling return-to-play within 3 months of injury.31 McAleer et al32 described a non-operative rehabilitation program for professional and aspiring professional football players with osteitis pubis. Their rehabilitative protocol was based on a specific nine-point program that included pain control, tone reduction of over-active structures, improved range of motion at hips, pelvis and thorax, adductor strength, functional movement assessment, core stability, lumbo-pelvic control, gym-based strengthening and field-based conditioning/rehabilitation. All players returned to training, without symptoms, within 60 days and, to play, within 72 days. The authors also recommended to patients a daily prophylactic program to be followed after recovery and this may have contributed to the absence of symptom recurrence in all players at a follow-up period ranging from 16 to 33 months.
Local injections
If symptoms fail to improve with conservative measures, local injections can be used. Injections of corticosteroids in the symphyseal region and surrounding tissues have been used in various studies. However, the evidence is low. Some of these articles report resolution of pain at short-term follow-up with corticosteroids injections but a high rate of non-responders.33 Moreover, despite successful return to sport participation, a large percentage of these patients continued to report pain and/or required multiple injections.30 There is not enough evidence regarding the short- and long-term efficacy of corticosteroid injections.33–35
One study reported on prolotherapy (dextrose injections) for the treatment of recalcitrant pubalgia.36 Nevertheless, the literature is very limited and the efficacy and mechanism of action of prolotherapy remain controversial.
Surgical treatment
Surgery is usually performed when conservative treatments fail. It may be indicated after at least 3 months of well-conduced rehabilitation protocol.37 Surgical intervention is required for 5%–10% of patients recalcitrant to conservative approaches.6
Many different open or minimally invasive surgical procedures have been proposed, including open or endoscopic curettage of the symphysis pubis, arthrodesis of the symphysis with or without bone graft and wedge resection.38 All procedures can be associated with the release of the adductor tendons or with adductor enthesis repair.2,39–41 These surgical treatments vary widely in their invasiveness, impact on pelvic biomechanics and recovery time. Even if most authors reported favorable outcomes after surgical procedures, most articles are retrospective case series, and studies are available up today.6 Given the lack of adequate clinical trials, little evidence exists to support one surgical method over another, or indeed the need of surgery itself. Moreover, clinicians should evaluate cost-effectiveness and consider possible side effects of each procedure.
Gupta et al42 described an endoscopic technique for pubic symphysectomy, proposing it as a safe and feasible, minimally invasive procedure for recalcitrant cases. As a complication of surgery, they reported only transient postoperative edema of the scrotum in men and of the labia in women, which resolved within 24 hours in all cases. Similar results have been reported by Matsuda et al.43
Recently, some authors demonstrated the association between osteitis pubis/athletic pubalgia and femoroacetabular impingement (FAI).44,45 In these patients, better results have been reported after treatment of both intra and extra-articular pathologies, with a high rate of return to previous level of activity/sport.46,47
In a retrospective level IV study, Kajetanek et al48 included 27 patients who had failed at least 3 months of appropriate conservative therapy and then underwent surgery for athletic pubalgia with injury to the abdominal wall and/or adductor attachment. Each patient received a la carte surgery, which was confined to the injured structure(s) only on the affected side (abdominal wall, adductor tendon or both), without routine contralateral procedure, with the aim of limiting morbidity and reducing recovery time. The results showed that 25 (92.6%) patients were able to return to their previous sport activity within a mean of 3–4 months and experienced no recurrence during 1-year follow-up. Time to return to play was significantly shorter in the group with abdominal wall injury only as compared to patients with adductor tendon injury only or combined injuries.
Novel approaches
Recently, other treatments have been proposed. Masala et al49 in 2015 reported on pulse-dose radio frequency on 32 patients with chronic pubic pain refractory to conservative therapies. The goals of this percutaneous treatment were to denervate the genital branches of the genitor-femoral, ilioinguinal and iliohypogastric nerves and the obturator nerve. These nerves provide motor and sensory innervation of the groin region, and they can be involved in entrapment or irritation syndromes that cause pubic pain. Twenty-four patients referred a significant pain reduction at final followup (9 months) after one treatment. Six of 7 patients who were treated twice referred significant pain reduction only after the second procedure, while only one patient had no pain relief after two treatments. All patients tolerated the procedure well, with some minimal post-operative discomfort during the first few days, but without complications during the early or late period of follow-up. However, further studies are required.
Scholten et al50 reported a case of distal rectus abdominis ultrasound-guided needle tenotomy and platelet-rich plasma injection, followed by a progressive rehabilitation. The patient was pain free and went back competition 8 weeks after the procedure.
Discussion
Groin pain is well-known among both athletes and physicians. Osteitis pubis is a painful degenerative condition of the pubic symphysis, surrounding soft tissues and tendons. It was first described by Beer in 1924,51 and it is currently considered as one of the most debilitating pain syndromes for athletes. Although the condition is considered self-limiting, it often requires stoppage of sporting activities for several months, representing a significant problem especially for elite athletes. The etiology is still debated, but muscular imbalance and pelvic instability have been identified as the most likely pathogenetic mechanism. However, groin anatomy is complex and pain is often caused by the association of different pathologies. These may include not only intra-articular and extra-articular pathologies around the hip but also lumbar spine conditions, nerve entrapments and intra-abdominal and genitourinary pathologies. Therefore, accurate differential diagnosis is mandatory.
Many different treatment protocols and strategies have been proposed for osteitis pubis, including conservative management and rehabilitation, injections and surgery. Conservative treatment is the first-line therapeutic approach, and it includes rest, limitation of sporting activities, ice and anti-inflammatory drugs. A rehabilitative protocol aimed at correcting muscular imbalances upon pubic symphysis is also indicated.52–54
Despite a lack of standardized rehabilitative protocols, recent literature underlines the importance of progressive individualized rehabilitation, which usually consists of four stages. However, the lack of level 1 studies makes it difficult to compare the outcomes and a gold standard treatment is still not exploitable. Shock wave therapy can be included in the conservative treatment protocol in addition to physical exercise. Few articles are published about injection therapy, with not enough evidence regarding the efficacy of steroid injections and prolotherapy. However, promising results have been reported with the use of dextrose injections.
The relationship between athletic pubalgia and FAI is a growing topic. Although they are considered two distinct pathologies, recent studies suggest that both conditions frequently affect athletes with groin pain.46 Economopoulos et al55 reported that 86% of patients referring groin pain and treated for osteitis pubis and/or sports hernia had a radiographic evidence of FAI. Hammoud et al56 described a consecutive series of 38 professional athletes who had been treated for symptomatic FAI. Twelve patients (32%) had undergone previous surgery for athletic pubalgia or osteitis pubis. All these patients returned to play after treatment of FAI. Furthermore, 39% of patients were diagnosed with osteitis pubis/athletic pubalgia and FAI, and they had complete resolution of pain and returned to play after surgical treatment of FAI alone. Even though the pathogenesis is not fully understood, it is possible that the restricted range of motion of the hip related to FAI may lead to compensatory stresses on the lumbar spine, pubic symphysis, sacroiliac joint and posterior acetabulum in high-performance athletes.55 Excessive biomechanical stress on the groin may lead to secondary injury to the abdominal wall musculature, including the posterior inguinal wall, resulting in symptomatic osteitis pubis or groin pain disruption.55
Surgery should be reserved for a limited subgroup of patients who fail conservative management, after at least 3 months of a well-conduced rehabilitative program. Many different surgical techniques have been described, but the majority of published studies exhibit a low level of evidence with no randomized controlled trials. Recent works reported better results and shorter time to return to sport, especially for patients with concurrent intra-articular pathologies such as FAI or sports hernia. Therefore, it is unclear whether the favorable outcomes are related to the treatment of concomitant pathologies or to the osteitis pubis itself.
Conclusion
Evaluation and treatment of groin pain are challenging, and a correct diagnosis is mandatory for appropriate management. Conservative treatments are indicated to stabilize the pelvis and pubic symphysis. Core stability exercises and muscle stretching and strengthening exercises of the abdominal, adductor, flexor and extensor hip muscles are effective for this purpose. Surgery is indicted for patients who do not respond to conservative management.
Despite these final considerations, it must be emphasized that this study presents some obvious limitations. First of all, the study population is limited. Second, this study is aimed at focusing only on “osteitis pubis,” which, however, is a misnomer for a variety of different pathologies which are frequently associated with osteitis pubis. Third, this review refers only to the latest literature from 2012 to 2018 and does not cover the complete literature about this topic. Therefore, given the gross heterogeneity of the studies available and the abovementioned limitations of this research, no meta-analysis could be conducted.
Nevertheless, this review could provide key directions for future investigations needed to improve our current knowledge about the management of osteitis pubis and to define the most effective therapeutic approaches.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Verrall GM, Hamilton IA, Slavotinek JP, et al. Hip joint range of motion reduction in sports-related chronic groin injury diagnosed as pubic bone stress injury. J Sci Med Sport. 2005;8(1):77–84. doi: 10.1016/s1440-2440(05)80027-1. [DOI] [PubMed] [Google Scholar]
- 2.Angoules AG. Osteitis pubis in elite athletes. World J Orthop. 2015;6(9):672–679. doi: 10.5312/wjo.v6.i9.672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harmon KG. Evaluation of groin pain in athletes. Curr Sports Med Rep. 2007;6(6):354–361. [PubMed] [Google Scholar]
- 4.DeVries JG, Berlet GC. Understanding levels of evidence for scientific communication. Foot Ankle Spec. 2010;3(4):205–209. doi: 10.1177/1938640010375184. [DOI] [PubMed] [Google Scholar]
- 5.Ekstrand J, Hilding J. The incidence and differential diagnosis of acute groin injuries in male soccer players. Scand J Med Sci Sports. 1999;9(2):98–103. doi: 10.1111/j.1600-0838.1999.tb00216.x. [DOI] [PubMed] [Google Scholar]
- 6.Maffulli N, Giai Via A, Oliva F. Groin Pain. In: Volpi P, editor. Football Traumatology: New Trends. Cham: Springer International Publishing; 2015. pp. 303–315. [Google Scholar]
- 7.Omar IM, Zoga AC, Kavanagh EC, et al. Athletic pubalgia and “sports hernia”: optimal MR imaging technique and findings. Radiographics. 2008;28(5):1415–1438. doi: 10.1148/rg.285075217. [DOI] [PubMed] [Google Scholar]
- 8.Rodriguez C, Miguel A, Lima H, Heinrichs K. Osteitis Pubis Syndrome in the Professional Soccer Athlete: A Case Report. J Athl Train. 2001;36(4):437–440. [PMC free article] [PubMed] [Google Scholar]
- 9.Williams JG. Limitation of hip joint movement as a factor in traumatic osteitis pubis. Br J Sports Med. 1978;12(3):129–133. doi: 10.1136/bjsm.12.3.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Verrall GM, Henry L, Fazzalari NL, Slavotinek JP, Oakeshott RD. Bone biopsy of the parasymphyseal pubic bone region in athletes with chronic groin injury demonstrates new woven bone formation consistent with a diagnosis of pubic bone stress injury. Am J Sports Med. 2008;36(12):2425–2431. doi: 10.1177/0363546508324690. [DOI] [PubMed] [Google Scholar]
- 11.Fricker PA, Taunton JE, Ammann W. Osteitis pubis in athletes: infection. inflammation or injury? Sports Med. 1991;12(4):266–279. doi: 10.2165/00007256-199112040-00005. [DOI] [PubMed] [Google Scholar]
- 12.Braun P, Jensen S. Hip pain – a focus on the sporting population. Aust Fam Physician. 2007;36(6):410–413. [PubMed] [Google Scholar]
- 13.Verrall GM, Slavotinek JP, Barnes PG, Fon GT. Description of pain provocation tests used for the diagnosis of sports-related chronic groin pain: relationship of tests to defined clinical (pain and tenderness) and MRI (pubic bone marrow oedema) criteria. Scand J Med Sci Sports. 2005;15(1):36–42. doi: 10.1111/j.1600-0838.2004.00380.x. [DOI] [PubMed] [Google Scholar]
- 14.Hegedus EJ, Stern B, Reiman MP, Tarara D, Wright AA. A suggested model for physical examination and conservative treatment of athletic pubalgia. Phys Ther Sport. 2013;14(1):3–16. doi: 10.1016/j.ptsp.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 15.Murar J, Birmingham P. Osteitis Pubis Hip Arthroscopy and Hip Joint Preservation Surgery. New York: Springer; 2014. pp. 737–749. [Google Scholar]
- 16.Hopp S, Ojodu I, Jain A, Fritz T, Pohlemann T, Kelm J. Novel patho-morphologic classification of capsulo-articular lesions of the pubic symphysis in athletes to predict treatment and outcome. Arch Orthop Trauma Surg. 2018;138(5):687–697. doi: 10.1007/s00402-018-2893-1. [DOI] [PubMed] [Google Scholar]
- 17.Bisciotti GN, Auci A, Di Marzo F, et al. Groin pain syndrome: an association of different pathologies and a case presentation. Muscles Ligaments Tendons J. 2015;5(3):214–222. doi: 10.11138/mltj/2015.5.3.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zoga AC, Kavanagh EC, Omar IM, et al. Athletic pubalgia and the “sports hernia”: MR imaging findings. Radiology. 2008;247(3):797–807. doi: 10.1148/radiol.2473070049. [DOI] [PubMed] [Google Scholar]
- 19.Harris NH, Murray RO. Lesions of the symphysis in athletes. Br Med J. 1974;4(5938):211–214. doi: 10.1136/bmj.4.5938.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Williams PR, Thomas DP, Downes EM. Osteitis pubis and instability of the pubic symphysis. When nonoperative measures fail. Am J Sports Med. 2000;28(3):350–355. doi: 10.1177/03635465000280031101. [DOI] [PubMed] [Google Scholar]
- 21.Verrall GM, Slavotinek JP, Fon GT. Incidence of pubic bone marrow oedema in Australian rules football players: relation to groin pain. Br J Sports Med. 2001;35(1):28–33. doi: 10.1136/bjsm.35.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beatty T. Osteitis pubis in athletes. Curr Sports Med Rep. 2012;11(2):96–98. doi: 10.1249/JSR.0b013e318249c32b. [DOI] [PubMed] [Google Scholar]
- 23.Lovell G, Galloway H, Hopkins W, Harvey A. Osteitis pubis and assessment of bone marrow edema at the pubic symphysis with MRI in an elite junior male soccer squad. Clin J Sport Med. 2006;16(2):117–122. doi: 10.1097/00042752-200603000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Orchard JW, Read JW, Neophyton J, Garlick D. Groin pain associated with ultrasound finding of inguinal canal posterior wall deficiency in Australian Rules footballers. Br J Sports Med. 1998;32(2):134–139. doi: 10.1136/bjsm.32.2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Frizziero A, Vittadini F, Pignataro A, et al. Conservative management of tendinopathies around hip. Muscles Ligaments Tendons J. 2016;6(3):281–292. doi: 10.11138/mltj/2016.6.3.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jardí J, Rodas G, Pedret C, et al. Osteitis pubis: can early return to elite competition be contemplated? Transl Med UniSa. 2014;10:52–58. [PMC free article] [PubMed] [Google Scholar]
- 27.Jarosz BS. Individualized multi-modal management of osteitis pubis in an Australian Rules footballer. J Chiropr Med. 2011;10(2):105–110. doi: 10.1016/j.jcm.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sudarshan A. Physical therapy management of osteitis pubis in a 10-year-old cricket fast bowler. Physiother Theory Pract. 2013;29(6):476–486. doi: 10.3109/09593985.2012.753650. [DOI] [PubMed] [Google Scholar]
- 29.Vijayakumar P, Nagarajan M, Ramli A. Multimodal physiotherapeutic management for stage-IV osteitis pubis in a 15-year old soccer athlete: a case report. J Back Musculoskelet Rehabil. 2012;25(4):225–230. doi: 10.3233/BMR-2012-0337. [DOI] [PubMed] [Google Scholar]
- 30.Cheatham S, Kolber MJ, Shimamura KK. The effectiveness of nonoperative rehabilitation programs for athletes diagnosed with osteitis pubis. J Sport Rehabil. 2015;25(4):399–403. doi: 10.1123/jsr.2015-0016. [DOI] [PubMed] [Google Scholar]
- 31.Schöberl M, Prantl L, Loose O, et al. Non-surgical treatment of pubic overload and groin pain in amateur football players: a prospective double-blinded randomised controlled study. Knee Surg Sports Traumatol Arthrosc. 2017;25(6):1958–1966. doi: 10.1007/s00167-017-4423-z. [DOI] [PubMed] [Google Scholar]
- 32.McAleer S, Lippie E, Norman D, Riepenhof H. Management of osteitis pubis/pubic bone stress in professional soccer players using a nonoperative rehabilitation protocol with clinical and functional progression criteria. J Orthop Sports Phys Ther. 2017;47(9):683–690. doi: 10.2519/jospt.2017.7314. [DOI] [PubMed] [Google Scholar]
- 33.Choi H, McCartney M, Best TM. Treatment of osteitis pubis and osteomyelitis of the pubic symphysis in athletes: a systematic review. Br J Sports Med. 2011;45(1):57–64. doi: 10.1136/bjsm.2008.050989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Elattar O, Choi H, Dills VD, Busconi B. Groin Injuries (Athletic Pubalgia) and Return to Play. Sports Health. 2016;8(4):313–323. doi: 10.1177/1941738116653711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kelm J, Ludwig O, André J, Maas S, Hopp S. What do we know about osteitis pubis in athletes? Sportverletz Sportschaden. 2018 Feb 8; doi: 10.1055/s-0043-122763. Epub. [DOI] [PubMed] [Google Scholar]
- 36.Topol GA, Reeves KD. Regenerative injection of elite athletes with career-altering chronic groin pain who fail conservative treatment: a consecutive case series. Am J Phys Med Rehabil. 2008;87(11):890–902. doi: 10.1097/PHM.0b013e31818377b6. [DOI] [PubMed] [Google Scholar]
- 37.Valent A, Frizziero A, Bressan S, Zanella E, Giannotti E, Masiero S. Insertional tendinopathy of the adductors and rectus abdominis in athletes: a review. Muscles Ligaments Tendons J. 2012;2(2):142–148. [PMC free article] [PubMed] [Google Scholar]
- 38.Williams PR, Thomas DP, Downes EM. Osteitis pubis and instability of the pubic symphysis. When nonoperative measures fail. Am J Sports Med. 2000;28(3):350–355. doi: 10.1177/03635465000280031101. [DOI] [PubMed] [Google Scholar]
- 39.Maffulli N, Loppini M, Longo UG, Denaro V. Bilateral mini-invasive adductor tenotomy for the management of chronic unilateral adductor longus tendinopathy in athletes. Am J Sports Med. 2012;40(8):1880–1886. doi: 10.1177/0363546512448364. [DOI] [PubMed] [Google Scholar]
- 40.Hopp SJ, Culemann U, Kelm J, Pohlemann T, Pizanis A. Osteitis pubis and adductor tendinopathy in athletes: a novel arthroscopic pubic symphysis curettage and adductor reattachment. Arch Orthop Trauma Surg. 2013;133(7):1003–1009. doi: 10.1007/s00402-013-1777-7. [DOI] [PubMed] [Google Scholar]
- 41.Hopp S, Tumin M, Wilhelm P, Pohlemann T, Kelm J. Arthroscopic pubic symphysis debridement and adductor enthesis repair in athletes with athletic pubalgia: technical note and video illustration. Arch Orthop Trauma Surg. 2014;134(11):1595–1599. doi: 10.1007/s00402-014-2065-x. [DOI] [PubMed] [Google Scholar]
- 42.Gupta A, Redmond JM, Hammarstedt JE, et al. Endoscopic Pubic Symphysectomy for Recalcitrant Osteitis Pubis. Arthrosc Tech. 2015;4(2):e115–e117. doi: 10.1016/j.eats.2014.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Matsuda DK, Sehgal B, Matsuda NA. Endoscopic Pubic Symphysectomy for Athletic Osteitis Pubis. Arthrosc Tech. 2015;4(3):e251–e254. doi: 10.1016/j.eats.2015.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Strosberg DS, Ellis TJ, Renton DB. The role of femoroacetabular impingement in core muscle injury/athletic pubalgia: diagnosis and management. Front Surg. 2016;3:6. doi: 10.3389/fsurg.2016.00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rambani R, Hackney R. Loss of range of motion of the hip joint: a hypothesis for etiology of sports hernia. Muscles Ligaments Tendons J. 2015;5(1):29–32. [PMC free article] [PubMed] [Google Scholar]
- 46.Larson CM. Sports hernia/athletic pubalgia: evaluation and management. Sports Health. 2014;6(2):139–144. doi: 10.1177/1941738114523557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ross JR, Stone RM, Larson CM. Core muscle injury/sports hernia/athletic pubalgia, and femoroacetabular impingement. Sports Med Arthrosc Rev. 2015;23(4):213–220. doi: 10.1097/JSA.0000000000000083. [DOI] [PubMed] [Google Scholar]
- 48.Kajetanek C, Benoît O, Granger B, et al. Athletic pubalgia: Return to play after targeted surgery. Orthop Traumatol Surg Res. 2018;104(4):469–472. doi: 10.1016/j.otsr.2018.01.012. [DOI] [PubMed] [Google Scholar]
- 49.Masala S, Fiori R, Raguso M, et al. Pulse-dose radiofrequency in athletic pubalgia: preliminary results. J Sport Rehabil. 2017;26(3):227–233. doi: 10.1123/jsr.2015-0149. [DOI] [PubMed] [Google Scholar]
- 50.Scholten PM, Massimi S, Dahmen N, Diamond J, Wyss J. Successful treatment of athletic pubalgia in a lacrosse player with ultrasound-guided needle tenotomy and platelet-rich plasma injection: a case report. PM R. 2015;7(1):79–83. doi: 10.1016/j.pmrj.2014.08.943. [DOI] [PubMed] [Google Scholar]
- 51.Schnute WJ. Osteitis pubis. Clin Orthop. 1961;20:187–192. [PubMed] [Google Scholar]
- 52.Frizziero A, Trainito S, Oliva F, Nicoli Aldini N, Masiero S, Maffulli N. The role of eccentric exercise in sport injuries rehabilitation. Br Med Bull. 2014;110(1):47–75. doi: 10.1093/bmb/ldu006. [DOI] [PubMed] [Google Scholar]
- 53.Dello Iacono A, Maffulli N, Laver L, Padulo J. Successful treatment of groin pain syndrome in a pole-vault athlete with core stability exercise. J Sports Med Phys Fitness. 2017;57(12):1650–1659. doi: 10.23736/S0022-4707.16.06735-9. [DOI] [PubMed] [Google Scholar]
- 54.Hölmich P, Uhrskou P, Ulnits L, et al. Effectiveness of active physical training as treatment for long-standing adductor-related groin pain in athletes: randomised trial. Lancet. 1999;353(9151):439–443. doi: 10.1016/S0140-6736(98)03340-6. [DOI] [PubMed] [Google Scholar]
- 55.Economopoulos KJ, Milewski MD, Hanks JB, Hart JM, Diduch DR. Radiographic evidence of femoroacetabular impingement in athletes with athletic pubalgia. Sports Health. 2014;6(2):171–177. doi: 10.1177/1941738113510857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hammoud S, Bedi A, Magennis E, Meyers WC, Kelly BT. High incidence of athletic pubalgia symptoms in professional athletes with symptomatic femoroacetabular impingement. Arthroscopy. 2012;28(10):1388–1395. doi: 10.1016/j.arthro.2012.02.024. [DOI] [PubMed] [Google Scholar]
- 57.Henning PT. The running athlete: stress fractures, osteitis pubis, and snapping hips. Sports Health. 2014;6(2):122–127. doi: 10.1177/1941738114523381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McAleer SS, Gille J, Bark S, Riepenhof H. Management of chronic recurrent osteitis pubis/pubic bone stress in a Premier League footballer: Evaluating the evidence base and application of a nine-point management strategy. Phys Ther Sport. 2015;16(3):285–299. doi: 10.1016/j.ptsp.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 59.Rossidis G, Perry A, Abbas H, et al. Laparoscopic hernia repair with adductor tenotomy for athletic pubalgia: an established procedure for an obscure entity. Surg Endosc. 2015;29(2):381–386. doi: 10.1007/s00464-014-3679-3. [DOI] [PubMed] [Google Scholar]
- 60.Ellsworth AA, Zoland MP, Tyler TF. Athletic pubalgia and associated rehabilitation. Int J Sports Phys Ther. 2014;9(6):774–784. [PMC free article] [PubMed] [Google Scholar]