CASE PRESENTATION
A 72-year-old man presented with sudden-onset chest pain with odynophagia and hematemesis that developed when he was having a meal at a restaurant. His history was significant for coronary artery disease (inferior wall myocardial infarction) and diabetes mellitus, and he was on aspirin, atorvastatin, and metformin. On examination, the patient was in pain and had tachycardia (110 beats/min) and his blood pressure was 100/60 mmHg. The other vitals were normal. The abdominal examination and cardiovascular examination were otherwise unremarkable. Liver function test, renal function test, and the coagulation profile were normal, as were the electrocardiogram, cardiac enzymes, and chest roentgenogram.
In view of the patient’s history of hematemesis and odynophagia, we performed endoscopic evaluation to exclude any esophagogastric ulcer, which was possible considering his history of diabetes and aspirin intake. Interestingly, the endoscopy revealed a bluish bulge starting at the cervical esophagus and reaching up to the gastroesophageal junction, and the bulge was compromising the lumen of the esophagus (Figure 1). Computed tomography, performed after endoscopy, revealed diffuse thickening of the esophagus (Figure 2).
Figure 1.
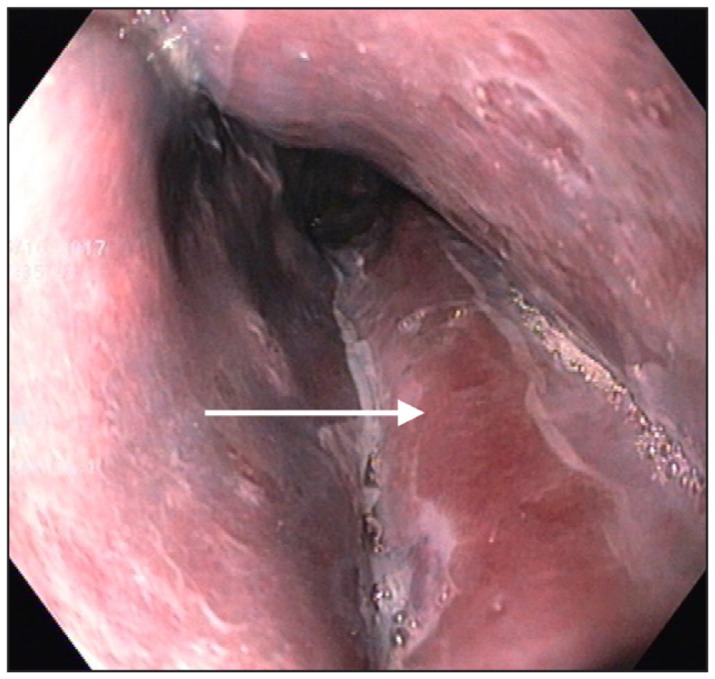
Endoscopic image of the patient’s esophagus. The white arrow indicates the esophageal intramural hematoma.
Figure 2.
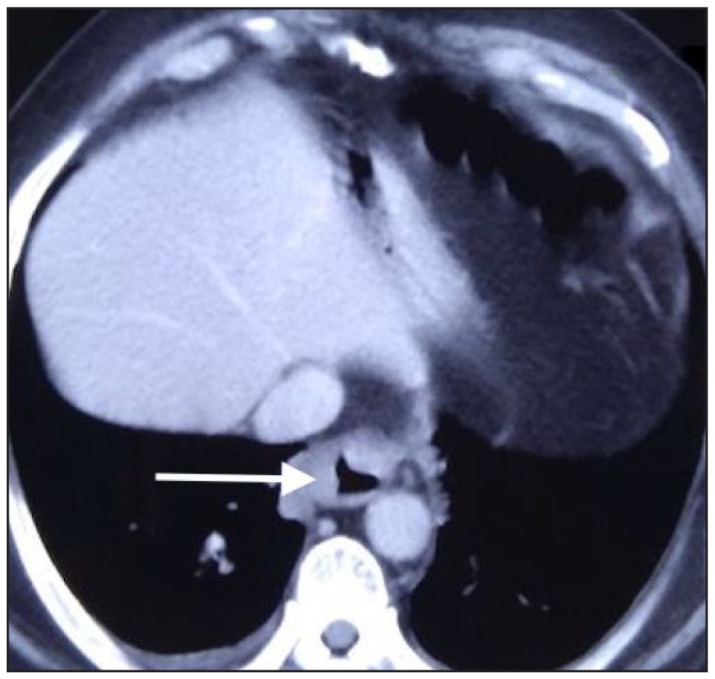
Computed tomography image showing the mural thickening of the esophagus (white arrow).
On the basis of these findings, we made the diagnosis of esophageal intramural hematoma (EIH). The patient was kept nil per os and was given intravenous proton pump inhibitors, fluids, and antibiotics, and he also received a blood transfusion. Gradually, during a week’s time, his dysphagia improved, and he was able to take a semisolid diet. Our patient was discharged from the hospital 7 days after his initial presentation. A week later, his symptoms had resolved completely and a repeat endoscopy showed disappearance of the hematoma and a long, linear ulcer possibly caused by pressure necrosis from the hematoma (Figure 3). The patient provided informed consent for inclusion in this report.
Figure 3.
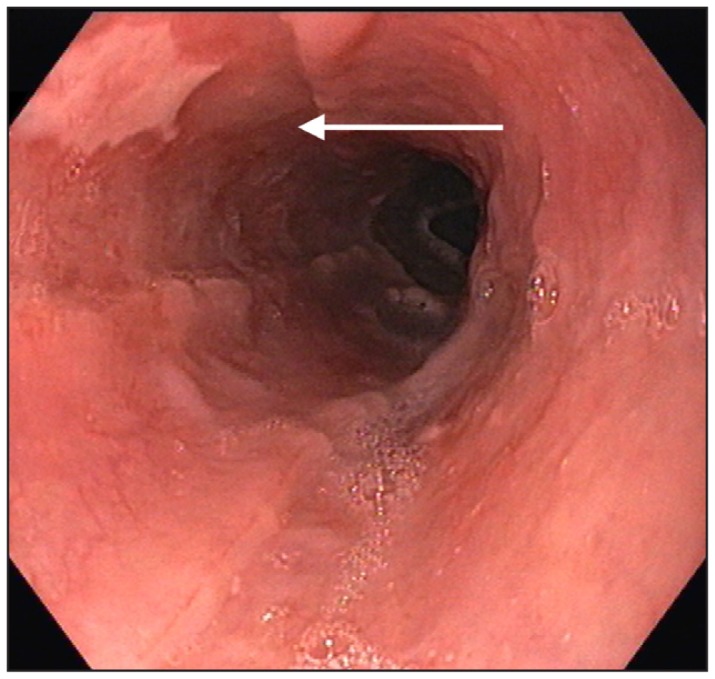
Repeat endoscopy of the patient’s esophagus. The white arrow indicates resolution of the hematoma and the linear ulcer.
DISCUSSION
EIH is a benign, uncommon entity that is part of the spectrum of disorders involving esophageal tears that vary from superficial mucosal tears (Mallory-Weiss syndrome) to transmural laceration (Boerhaave syndrome). However, the spontaneous occurrence of a hematoma does not fit in the spectrum of the above-mentioned disorders because these disorders usually have a trigger in the form of emesis, whereas an esophageal hematoma does not have a similar trigger. EIH could also be secondary to trauma, instrumentation, foreign body ingestion, aortoesophageal fistula and coagulopathy, or it could occur spontaneously.1,2 In our patient, the 2 possible factors responsible for EIH could be the ongoing aspirin intake and the intake of food, to which the event was temporally related.
Other terms used for describing EIH include esophageal apoplexy and esophageal dissection. Given the rarity, exact epidemiologic data are not available, but it has been reported that this condition occurs most frequently in women in their 50s. Underlying coagulopathy could be present in about a fifth of cases.3 Because EIH is an uncommon form of esophageal injury, it is rarely suspected initially and needs to be differentiated from life-threatening situations like aortic dissection and esophageal perforation; computed tomography usually helps in differentiating these conditions. Our patient’s history of heart disease and his presentation with chest pain made it necessary to exclude an acute ischemic event or aortic dissection. However, dysphagia was a clue to the esophageal origin of his symptoms.
The usual location of the hematoma is in the distal esophagus, which lacks supporting structures as well as the striated muscle. EIH could also extend and involve the whole length of the esophagus, as in our case. Typical appearance on computed tomography scan is a symmetric or asymmetric mural thickening with a well-defined, nonenhancing, high-attenuating intramural mass that extends along the wall of the esophagus and may show fluid-fluid level or air-fluid level when there is mucosal tear or infection.4,5 The clinical triad of retrosternal chest pain, dysphagia, and vomiting is seen in a third of patients whereas 2 of these 3 features could occur in two-thirds of patients.6
The diagnosis of EIH should be considered in the presence of any of the symptoms of the clinical triad when presenting with a predisposing factor. However, because EIH is rare, other differential diagnoses of chest pain need exclusion. It is unclear if patients with EIH should be admitted, but patients with underlying conditions that must be corrected (like coagulopathy or rarely aortoesophageal communication) and those who cannot maintain oral intake do need admission. The majority of patients improve with conservative management after 1 to 3 weeks, as was the case in our patient.7
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- 1.Beumer JD, Devitt PG, Thompson SK. Intramural oesophageal dissection. ANZ J Surg. 2010 Jan;80(1–2):91–5. doi: 10.1111/j.1445-2197.2009.05179.x. . [DOI] [PubMed] [Google Scholar]
- 2.Lu MS, Liu YH, Liu HP, Wu YC, Chu Y, Chu JJ. Spontaneous intramural esophageal hematoma. Ann Thorac Surg. 2004 Jul;78(1):343–5. doi: 10.1016/s0003-4975(03)01280-3. [DOI] [PubMed] [Google Scholar]
- 3.Nagai T, Torishima R, Nakashima H, et al. Spontaneous esophageal submucosal hematoma in which the course could be observed endoscopically. Intern Med. 2004 Jun;43(6):461–7. doi: 10.2169/internalmedicine.43.461. . [DOI] [PubMed] [Google Scholar]
- 4.Katabathina VS, Restrepo CS, Martinez-Jimenez S, Riascos RF. Nonvascular, nontraumatic mediastinal emergencies in adults: A comprehensive review of imaging findings. Radiographics. 2011 Jul-Aug;31(4):1141–60. doi: 10.1148/rg.314105177. [DOI] [PubMed] [Google Scholar]
- 5.Abbey P, Sharma R, Garg PK. Spontaneous intramural haematoma of the oesophagus: Complete resolution on follow-up magnetic resonance imaging. Singapore Med J. 2009 Sep;50(9):e318–20. [PubMed] [Google Scholar]
- 6.Xenodemetropoulos T, Khan KJ, Bercik P. Spontaneous intramural esophageal hematoma in association with idiopathic thrombocytopenic purpura: A cause of non-cardiac chest pain. Clin Gastroenterol Hepatol. 2010 Jul;8(7):e73–4. doi: 10.1016/j.cgh.2010.02.015. . [DOI] [PubMed] [Google Scholar]
- 7.Tay YK, Tay JY, Dandie L, Gribbin J. Intramural hematoma of the esophagus mimicking hemorrhaging esophageal cancer. Ann Gastroenterol. 2013;26(1):74–6. [PMC free article] [PubMed] [Google Scholar]


