Abstract
A 26-year-old gravida 2, para 2-0-0-2 woman with a recent uncomplicated vaginal delivery 10 weeks prior presented to our hospital with 5 weeks of abdominal swelling and discomfort. Four weeks after delivery, the patient began having right upper quadrant pain and was found to have cholelithiasis. She underwent an elective laparoscopic cholecystectomy 6 weeks prior to admission, but started to develop worsening abdominal swelling 1 week postoperatively. Abdominal distension and shifting dullness were present on examination. CT of the abdomen and pelvis was remarkable for moderate-volume ascites and mild enhancement of the pelvic peritoneum. Paracentesis removed 2.46 L of ascites fluid with 76% lymphocytic predominance. Results for Chlamydia trachomatis were positive in urine, cervical swab and ascitic fluid. Doxycycline was prescribed for a diagnosis of pelvic inflammatory disease exudative ascites. Since discharge, she has completed her antibiotic course and reports resolution of all symptoms without recurrence of ascites.
Keywords: infection (gastroenterology), general practice / family medicine, infectious diseases, obstetrics and gynaecology
Background
Chlamydia trachomatis is the most frequently reported bacterial infection in the USA.1 In 2016, approximately 1.5 million cases were reported to the Centers for Disease Control.1 Given its prevalence, C. trachomatis is also one of the most important bacterial infections clinicians treat in both an inpatient and outpatient setting. It is especially prevalent in young women (ages 15–29) and in the African American population where the rate of Chlamydia is 5.7 times higher in black women than their white counterparts.2 Thus, it is key for clinicians to understand the clinical manifestations of this disease and to be more vigilant in testing for and making the diagnosis of Chlamydia in high-risk patients. Chlamydia, if symptomatic, has a myriad of clinical manifestations including conjunctivitis, pharyngitis, cervicitis, urethritis, proctitis, perihepatitis and pelvic inflammatory disease (PID). Untreated PID can lead to chronic pelvic pain syndrome, infertility and ectopic pregnancy. C. trachomatis has been noted to be the predominant pathogen in patients with Fitz-Hugh-Curtis syndrome with rates as high as 73%–82% in those with liver infection.3 4 Much less frequently seen is C. trachomatis infection causing ascites without the presence of PID or Neisseria gonorrhoeae coinfection. Here, we present a case of a postpartum woman with recent cholecystectomy presenting with ascites secondary to chlamydial infection.
Case presentation
A 26-year-old G2P2002 woman with a recent uncomplicated pregnancy and vaginal delivery of a term infant 10 weeks prior to admission presented to our hospital with 5 weeks of abdominal swelling and discomfort. Four weeks after delivery, the patient began having right upper quadrant pain and was found to have cholelithiasis on ultrasound performed at an outside hospital. She also had mild dysuria and was found to have uncomplicated cystitis on urinalysis and treated with a 10-day course of antibiotics. She underwent elective laparoscopic cholecystectomy 6 weeks prior to admission, but started to develop abdominal swelling 1 week postoperatively, which continued to worsen over the following 5 weeks preceding admission to our institution. One week prior to admission, she was referred to a gastroenterologist as an outpatient for the abdominal problems who ordered a CT of the abdomen and pelvis, which was remarkable for moderate-volume ascites with a non-cirrhotic appearing liver, scattered arterially enhancing lesions in the liver, mild enhancement of the pelvic peritoneum and tubular appearance of the left adnexa (figure 1).
Figure 1.
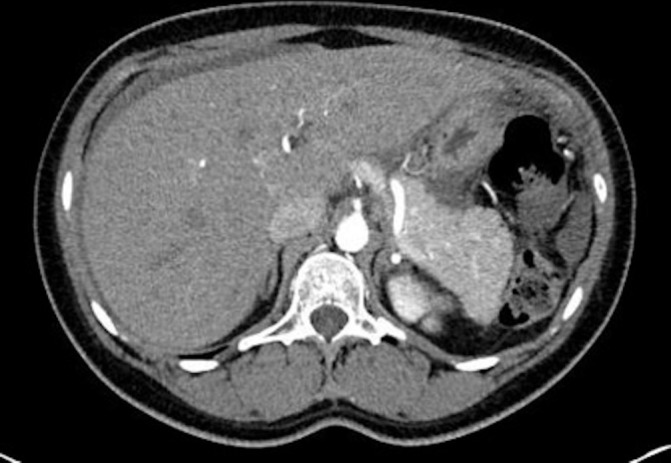
CT abdomen and pelvis with contrast demonstrating a non-cirrhotic liver and moderate ascites.
She also underwent a paracentesis with removal of 2.46 L of cloudy ascitic fluid. The patient was referred to the emergency department by her gastroenterologist after reviewing the results of the ascitic analysis, which demonstrated 6123 nucleated cells with a lymphocytic predominance (76% lymphocytes) and a serum-ascites albumin gradient (SAAG) <1.1 g/dL. The cytology of the fluid revealed reactive mesothelial cells and chronic inflammation, but no malignant cells.
On admission, the patient endorsed mild abdominal distension and discomfort as well as difficulty passing gas. She reported substantial yellowish vaginal discharge, which had been present during her pregnancy, but decreased somewhat since delivery. She denied a history of sexually transmitted infections (STIs) and reported receiving routine prenatal care, treated only with intrapartum antibiotics for group B Streptococcus. She denied any complication of neonatal infection, and reported routine paediatric follow-up of her infant since delivery. She had not been sexually active since delivery and reported being in a mutually monogamous relationship with her husband. She denied any subjective fever, chills, weight loss, dyspnoea, chest pain, nausea, vomiting, diarrhoea, constipation, joint pains, skin changes, vaginal itching or burning. Review of systems was positive for night sweats since her cholecystectomy. She denied any risk factors for tuberculosis.
Investigations
On examination, the patient was afebrile with normal vital signs. Her examination was remarkable only for a moderately distended abdomen with mild non-focal tenderness, shifting dullness and a positive fluid wave. Her labs were largely unremarkable with normal complete blood count, lipid panel and chemistries, including liver enzymes and liver function tests. Urinalysis showed moderate leucocyte esterase without proteinuria and leucocytes. Chest radiograph was negative for any cardiopulmonary abnormalities.
She was seen by infectious disease and gynaecology. A pelvic examination revealed mild tenderness on bimanual examination, but no true cervical motion tenderness and no adnexal masses. A transvaginal ultrasound was unremarkable. HIV, rapid plasma reagin (RPR) and viral hepatitis panel were negative. Although the suspicion for PID was relatively low, urine and endocervical swabs were sent for gonorrhoea and Chlamydia nucleic acid amplification tests (NAATs).
Given the lymphocytic predominance on ascitic fluid analysis and peritoneal enhancement on CT, tuberculous peritonitis and peritoneal carcinomatosis diagnoses were entertained and blood cultures for acid fast bacilli (AFB) were ordered. She underwent a repeat paracentesis with fluid analysis for Chlamydia NAAT, AFB stain and culture, adenosine deaminase and Mycobacterium tuberculosis DNA. A total of 1.3 L of fluid was removed and revealed a persistently elevated polymorphonuclear neutrophils (PMN) count of 9400 (55% lymphocytes) with no bacterial or fungal growth, and no malignant cells on cytology.
The patient remained afebrile without leucocytosis and felt well throughout the duration of her admission. Workup for tuberculous peritonitis and peritoneal carcinomatosis was negative; peritoneal biopsy was not pursued. On hospital day 4, results for C. trachomatis were positive in urine, cervical swab and ascitic fluid.
Differential diagnosis
Peritoneal tuberculosis.
Operative lymphatic tear.
Peritoneal carcinomatosis.
Advanced endometriosis.
Lymphangioleiomyomatosis.
Peritoneal serositis in systemic lupus erythematosus (SLE).
Lymphoma.
Chlamydial peritonitis.
Treatment
She was discharged on doxycycline 100 mg two times a day for 14 days with a diagnosis of presumed exudative ascites, likely secondary to PID, and instructed to follow-up as an outpatient with her gynaecologist.
Outcome and follow-up
Since discharge, she completed her antibiotic course and reported completed resolution of all symptoms without recurrence of ascites. Her partner was actively deployed in the military beginning in the latter part of her pregnancy through her admission to our institution, but she was counselled that she would need to inform her partner of her result and that he would need to be tested as well. She was in agreement with this plan.
Discussion
Tuberculous peritonitis, peritoneal carcinomatosis and pancreatic disease are the most common causes of exudative (total protein ≥2.5 g/dL) ascites with a low SAAG <1.1 g/dL. PID is an unusual cause of exudative, lymphocytic-predominant ascites with a low SAAG and is rarely described in the literature.5 6 Our case describes a young woman with an exudative, lymphocytic-predominant ascites with low SAAG and mild peritoneal enhancement on imaging who had a negative workup for malignancy, tuberculosis and all other infectious aetiologies except for Chlamydia. Interestingly, our patient had an unrevealing gynaecological examination, normal pelvic ultrasound and no other findings on imaging that suggested PID.
There are many clinical manifestations of initial chlamydial infection and it is not uncommon for patients to present without frankly purulent vaginal discharge, uterine, adnexal or cervical motion tenderness.3 While the patient described a yellowish discharge that had been present during her pregnancy, she was not noted to have abnormal vaginal discharge on pelvic examination performed by the consulting gynaecology team. Additionally, she reported receiving routine prenatal care, during which she presumably completed the recommended prenatal labs including STI testing. However, we were unable to review her outside records. If no such prenatal testing was done, this case reinforces the necessity of early and uniform STI testing and treatment in pregnant women.
The timing of our patient’s cholecystectomy is of interest in this case. The patient had already experienced subjective changes in her vaginal discharge at the time of cholecystectomy and then began developing abdominal swelling only 1 week postoperatively. It is possible that the cholecystectomy could have contributed to the development of peritonitis and ascites as a retrospective analysis of laparoscopic complications demonstrated a 0.21% incidence of postoperative peritonitis with cholecystectomy.7 Similarly, studies in animal models have shown an increase in proinflammatory cytokines and incidence of bacteraemia and systemic inflammation following laparoscopic surgery.8 9 Additionally, there is a relative immunosuppression following any form of surgery.10 While these risks are higher for laparotomy compared with laparoscopy, the recent surgical procedure could have theoretically precipitated her chlamydial induced peritonitis due to local inflammation, bacterial translocation and immunosuppression.
There are a few case reports that describe PID-induced ascites that initially mimicked either tuberculous peritonitis or peritoneal carcinomatosis, with elevated adenosine deaminase levels in the ascitic fluid, postinflammatory peritoneal nodularity on imaging, or pelvic cystic masses on imaging.5 11 Although our patient did have mild peritoneal enhancement on imaging, there were no cysts on imaging, the ascitic fluid adenosine deaminase level was normal with negative ascitic and blood tests for tuberculosis, and no malignant cells were seen on cytology.
The diagnosis of PID-induced ascites was ultimately made with a positive RNA test for C. trachomatis and the exclusion of other causes. The majority of patients with PID-induced ascites, as in our patient, reported as about 8 out of 9 in one study, had resolution of ascites after treatment with a tetracycline, although it has been suggested that some cases may be self-limiting without antibiotic administration.12 In conclusion, this case demonstrates the challenge of considering multiple aetiologies for the patient’s clinical picture and balancing this with the risk of superfluous testing. It also highlights the importance of a thorough sexual history for all patients and consideration for STIs such as Chlamydia and gonorrhoea in addition to the standard diagnostic workup of any young sexually active woman who presents with abdominal discomfort and ascites.
Learning points.
Chlamydia trachomatis is the most common bacterial infection reported in the USA, and the disease is especially concentrated in sexually active young African-American women.
Consider chlamydial infection in the young sexually active woman with unexplained ascites with low serum-ascites albumin gradient (SAAG) and lymphocytic predominance.
Low SAAG ascites should be considered its own symptom when considering diagnostic criteria for C. trachomatis infection.
C. trachomatis plays a significant role in peritoneal inflammation without Neisseria gonorrhoeae coinfection.
Given the prevalence of C. trachomatis in Fitz-Hugh-Curtis syndrome and ascites, C. trachomatis may play a greater role in intra-abdominal pathology than previously thought.
Footnotes
Contributors: All authors contributed to the care of the patient and writing the case report. BH reviewed, revised and submitted the case report and serves as the corresponding author.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Centers for Disease Control and Prevention. 2016 Sexually Transmitted Diseases Surveillance. Sexually Transmitted Diseases 2017:1–9 https://www.cdc.gov/std/stats16/CDC_2016_STDS_Report-for508WebSep21_2017_1644.pdf (accessed 18 Sep 2018).27930501 [Google Scholar]
- 2.Centers for Disease Control and Prevention. Health Disparities in HIV/AIDS, Viral Hepatitis, STDs and TB. https://www.cdc.gov/nchhstp/healthdisparities/africanamericans.html (accessed 18 Sep 2018).
- 3.Mackay G, et al. Sexually Transmitted Diseases & Pelvic Infections : DeCherney AH, Nathan L, Laufer N, Roman AS, CURRENT Diagnosis & Treatment: Obstetrics & Gynecology. New York, NY: McGraw-Hill, 2013. https://accessmedicine.mhmedical.com/content.aspx?sectionid=41008635&bookid=498&guestAccessKey=1ca19c9a-f63f-40b3-abe7-4834ed29d8cf (accessed 18 Sep 2018). [Google Scholar]
- 4.Woo SY, Kim JI, Cheung DY, et al. Clinical outcome of Fitz-Hugh-Curtis syndrome mimicking acute biliary disease. World J Gastroenterol 2008;14:6975–80. 10.3748/wjg.14.6975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kang HM, Oh TH, Kang GH, et al. [A case of Chlamydia trachomatis peritonitis mimicking tuberculous peritonitis]. Korean J Gastroenterol 2011;58:111–6. 10.4166/kjg.2011.58.2.111 [DOI] [PubMed] [Google Scholar]
- 6.Gregora MG, McNamara T. Ascites–an unusual association with pelvic inflammatory disease. Aust N Z J Obstet Gynaecol 1997;37:477–9. 10.1111/j.1479-828X.1997.tb02467.x [DOI] [PubMed] [Google Scholar]
- 7.Drăghici L, Drăghici I, Ungureanu A, et al. Laparoscopic surgery complications: postoperative peritonitis. J Med Life 2012;5:288–96. [PMC free article] [PubMed] [Google Scholar]
- 8.Jacobi CA, Ordemann J, Zieren HU, et al. Increased systemic inflammation after laparotomy vs laparoscopy in an animal model of peritonitis. Arch Surg 1998;133:258–62. 10.1001/archsurg.133.3.258 [DOI] [PubMed] [Google Scholar]
- 9.Shan CX, Ni C, Qiu M, et al. Influence of laparoscopy vs. laparotomy on bacterial translocation and systemic inflammatory responses in a porcine model with peritonitis. J Invest Surg 2014;27:73–80. 10.3109/08941939.2013.837564 [DOI] [PubMed] [Google Scholar]
- 10.Novitsky YW, Litwin DE, Callery MP. The net immunologic advantage of laparoscopic surgery. Surg Endosc 2004;18:1411–9. 10.1007/s00464-003-8275-x [DOI] [PubMed] [Google Scholar]
- 11.Gojayev A, English DP, Macer M, et al. Chlamydia peritonitis and ascites mimicking ovarian cancer. Case Rep Obstet Gynecol 2016;2016:1–4. 10.1155/2016/8547173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yanagisawa N, Tomiyasu H, Hada T, et al. Chlamydia trachomatis peritonitis: report of a patient presenting spontaneous regression of ascites. Intern Med 1992;31:835–9. 10.2169/internalmedicine.31.835 [DOI] [PubMed] [Google Scholar]


