Abstract
A healthy 31-year-old man presenting with back pain was found to have multiple spinal enhancing lesions on MRI. An incidental asymptomatic large pleural effusion was identified on investigations for the back pain and pleural and pulmonary tuberculosis (TB) was subsequently diagnosed. The radiographical features on MRI spine were not typical of spinal TB and a Ga68 DOTATATE Positron Emission Tomography (PET)/CT confirmed metastatic paraganglioma with multiple bone metastases. Although metastatic paraganglioma is rare, this case highlights that even in young patients dual pathology needs to be considered. Most importantly, it is a reminder to physicians managing TB of the clues that help distinguish spinal TB from important alternative causes, including metastatic malignancy.
Keywords: head and neck cancer, tuberculosis, endocrine cancer
Background
The spectrum of disease and presentations with tuberculosis (TB) can be broad. In countries with a low incidence of TB, it is not uncommon for the diagnosis to be missed or delayed.1 In this case report, we highlight the less common issue of identifying a second diagnosis in a patient with known TB, who presented with symptomatic spinal lesions that were initially suspected as being due to the same pathology (ie, disseminated TB with spinal involvement). Metastatic malignancy was ultimately confirmed as the cause of the spinal lesions, and this case is a reminder of the importance of clinician’s being aware of the classical radiographical features of spinal TB, differentiating these from other important alternative causes and knowing when further investigations are warranted. The case also highlights a non-invasive diagnostic technique that was helpful in confirming the diagnosis of metastatic paraganglioma.
Case presentation
A previously healthy 31-year-old Thai man presented to his general practitioner (GP) with 3 weeks of progressive lumbar back pain. He had a history of a resected locally invasive paraganglioma from his right carotid body 5 years prior without any subsequent follow-up. He had no history of TB or known TB contact and had previously had a normal immigration chest X-ray when arriving in Australia 6 years ago.
The back pain had started after an episode of heavy lifting at work. The patient had no neurological deficit at the time of initial review; however, he reported intermittent paresthesia in the right L4/5 dermatome distribution. There was no history of weight loss or cough but the patient reported intermittent subjective fevers over the previous 3 weeks. Following imaging performed at the request of his GP, the patient was referred to a specialist public TB service on the presumption that the patient likely had spinal and pulmonary TB.
Investigations
An MRI spine was performed which showed multiple enhancing lesions throughout the spine with extension of the L4 lesion into the epidural space (figure 1). The scout imaging performed during the MRI incidentally identified a large right pleural effusion with associated collapse and consolidation within the right lung and this was subsequently confirmed on a CT chest (figure 2).
Figure 1.

MRI lumbar spine (T1 postcontrast sagittal and T2 sagittal images) showing multiple ring-enhancing lesions throughout the lumbar spine with a large L4 lesion extending into the epidural space.
Figure 2.

CT chest (axial plane) showing a large right pleural effusion.
On initial assessment, a malignancy was thought to be the most likely unifying diagnosis given the radiological findings on MRI spine. TB was included in the differential diagnosis. A thoracoscopy with drainage of the pleural effusion and pleural biopsies was performed. Pleural biopsies showed necrotising granulomatous inflammation and acid-fast bacilli were seen. An Xpert MTB/RIF assay was performed on pleural tissue which detected Mycobacterium tuberculosis DNA without evidence of rifampicin resistance. M. tuberculosis was cultured from sputum and pleural biopsies and this was subsequently confirmed to be fully sensitive on drug susceptibility testing. The patient was thought to have disseminated TB with pleuropulmonary and spinal involvement and commenced on standard TB treatment with isoniazid, rifampicin, pyrazinamide and ethambutol, with the addition of prednisolone given the neurological symptoms and obvious epidural extension at the L4 level (figure 1).
Once the diagnosis of TB was confirmed and the patient was established on treatment, the MRI spine was discussed and reviewed by a radiologist. The MRI spine showed a number of features which were atypical for spinal TB. First, there was no evidence of a paraspinal collection which typically forms subligamentously, beneath the anterior longitudinal ligament, within the psoas muscles and within the epidural space. Second, there was no evidence of significant involvement of the vertebral body end plates or disc spaces with no evidence of collapse. Third, TB tends to involve the spinal canal but there was no evidence of dural enhancement or thickening. There were multifocal small ring-enhancing vertebral body lesions. In addition, a larger marginated L4 vertebral body lesion was present which was slightly expansile, distorting the basivertebral veins and distorting the posterior aspect of the vertebral body. Within the L4 lesion, there was subtle involvement of the posterior elements and enhancing epidural extension with internal flow voids consistent with a relatively vascular lesion. These features were more suggestive of a neoplastic process.
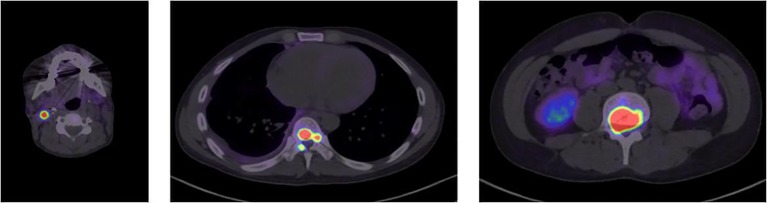
The final clue which increased the suspicion of underlying metastatic paraganglioma was a CT head and neck scan which showed an increased amount of soft tissue within the right carotid space at the site of previous tumour resection. Given the atypical features for extrapulmonary TB on the MRI spine and the patient’s history of a resected carotid body tumour a whole body Ga68 DOTATATE Positron Emission Tomography (PET)/CT scan was performed 5 weeks after commencing TB therapy. This showed well-defined foci of DOTATATE avidity within the right carotid space at the site of the previous tumour resection and innumerable DOTATATE avid osseous lesions throughout the spine and axial skeleton (figures 3 and 4). There was no DOTATATE avidity within the lung parenchyma or pleura at the site of the known pleuropulmonary tuberculous infection.
Figure 3.
Ga68 DOTATATE PET/CT showing well-defined foci of DOTATATE avidity at the right carotid space consistent with residual tumour from previous carotid body resection. Multiple DOTATATE avid lesions within the thoracic and lumbar vertebra, especially L4 vertebra.
Figure 4.
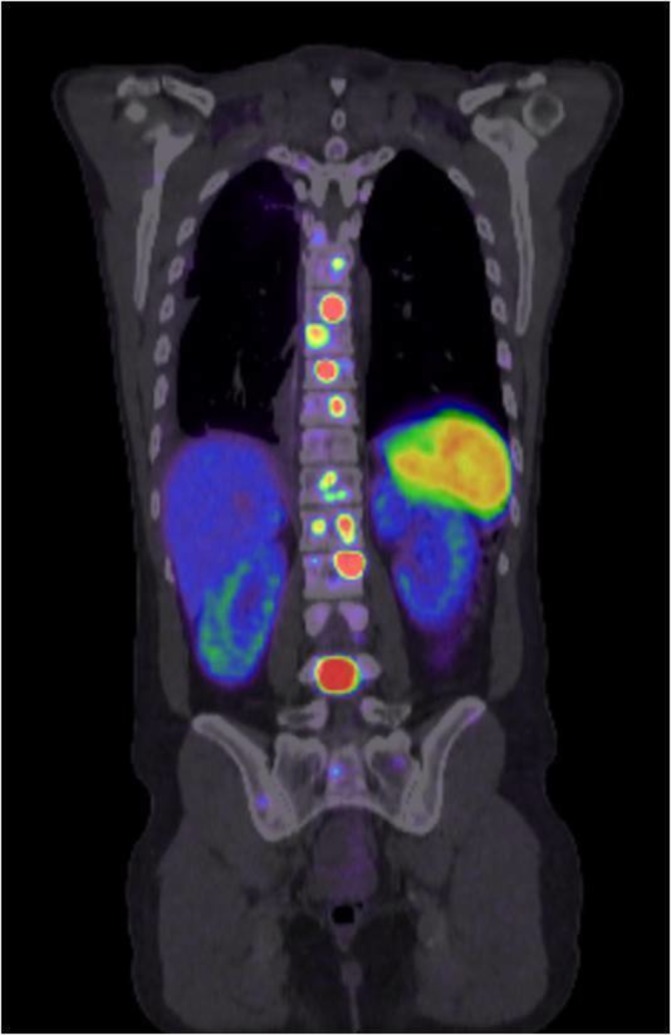
Ga68 DOTATATE PET/CT showing multiple DOTATATE avid osseous lesions throughout the thoracic and lumbar spine.
The Ga68 DOTATATE PET/CT scan confirmed that the patient had metastatic paraganglioma accounting for the spinal lesions and excluded disseminated TB. On reviewing the histopathology from the previously resected carotid body tumour, atypical features which have been described in both benign and malignant paragangliomas were noted. These features included irregular extension of the paraganglioma into adjacent fibrous tissue and striated muscle, mitotic activity (at least 2–3 per 10 high power fields (HPF)), vascular invasion and perineural invasion. Tumour cells were also present immediately adjacent to the surgical margin in a number of areas. Two lymph nodes were resected without any tumour involvement. The case was discussed at the head and neck multidisciplinary team meeting and given the high specificity of Ga68 DOTATATE PET for paragangliomas, the previous histological diagnosis and the vascular appearance of the spinal lesions, a biopsy was not required.
Treatment
The patient was given a total of 9 months of TB treatment for fully sensitive pulmonary and pleural TB. Six months of treatment is likely to have been adequate, however treatment was extended to 9 months as a small persistent pleural effusion remained at the end of 6 months of therapy and the patient was tolerating treatment well. The patient received 8 weeks of prednisolone and this was weaned once spinal TB was excluded. Prior to the exclusion of disseminated TB, the planned treatment duration was for 12 months, given the neurological symptoms and epidural involvement at L4.
There has been a good response to TB treatment with a radiological improvement and culture conversion.
For the metastatic paraganglioma, the patient has received palliative radiotherapy to C5–C7 and L2–L5 with 20Gy/5 fractions over 1 week. His back pain improved and neurological symptoms resolved. Systemic chemotherapy was deemed to have no role at this stage.
Outcome and follow-up
At the time of writing, the patient was planned to undergo post-treatment surveillance for TB; however, given the good response to treatment, the risk of relapse was thought to be low.
Further ongoing surveillance from the oncology team was also planned. Plasma metanephrines and 3-methoxytyramine have been within normal limits. The patient had no known family history of phaeochromocytoma, paraganglioma or related tumours. A familial cancer panel for paragangliomas/phaeochromocytomas did not detect any mutations. The familial cancer-related genes tested included EPAS1, FH, IDH1, KIF1B, MAX, MDH2, NF1, NF2, RET, SDHA, SDHAF2, SDHB, SDHC, SDHD, TMEN127 and VHL. The patient may be a candidate for peptide receptor radionuclide therapy in the future; however, given the clinical course of metastatic, paraganglioma is highly variable and the patient had a symptomatic response following radiotherapy, a decision was made to observe initially with serial imaging.
Discussion
In this case, once pulmonary and pleural TB was diagnosed, it was initially thought that this patient had disseminated TB with spinal involvement to explain the enhancing lesions on MRI spine. However, the radiological appearance of the spinal lesions was not typical for TB and this, in combination with the history of paraganglioma prompted the referral for the Ga68 DOTATATE CT/PET scan which helped to confirm the ultimate diagnosis. This case highlights the importance of physicians being aware of the classical radiological feature of spinal TB to diagnose this when present, but as importantly, to distinguish it from alternative diagnoses that may mimic this appearance on imaging.
Although spinal TB is rare, it is the most frequent site of musculoskeletal TB.2 Table 1 shows the classical features of spinal TB although the presentations of spinal TB can vary significantly and can often mimic pyogenic spondylitis and malignancy leading to delays in diagnosis and morbidity.3
Table 1.
Typical radiographic features of tuberculosis (TB) spondylitis, pyogenic spondylitis and spinal metastases3–6
| Features | Tuberculous spondylitis | Pyogenic spondylitis | Spinal metastases |
| Vertebrae involvement | Subligamentous spread to≥3 vertebrae | Involves 1 spinal segment with≤2 vertebral bodies | Can be solitary or multiple |
| Most common site of disease | Thoracic spine | Lumbar spine | Skip lesions/non-consecutive multifocal involvement |
| Vertebral bone destruction | Usually anterior and severe | Mild-moderate with loss of definition of the vertebral end plate and vertebral bodies (T1-weighted MRI) | Variable |
| Intervertebral disc involvement | Narrowing of the disc space (more preserved than in pyogenic spondylitis) | Moderate to complete disc destruction | Disc is spared |
| Abscess formation | Para-spinal abscess±calcification | Para-spinal abscess (less common than in TB spondylitis) | Soft tissue mass |
Most commonly, spinal TB involves the thoracic followed by the lumbar segments of the spine with involvement of two or more continuous vertebral bodies and the intervening discs. However, infection can also occur at single or multiple vertebrae without disc involvement.3 4
In most cases, spinal TB occurs via haematogenous spread. The vertebral body corners adjacent to the end plates are most commonly involved first due to their rich arterial supply. The infection then spreads throughout the vertebral body, to the disc space, the vertebral arch and beneath the anterior or posterior longitudinal ligaments. This eventually leads to the infection involving multiple adjacent or separate vertebrae.4
The typical radiological features for spinal TB include vertebral body destruction (usually anterior), loss of disc height, erosion of end plates, bone sequestration, sclerosis and paravertebral masses. The presence of calcification in paraspinal masses is especially indicative of TB.4
MRI is considered to be highly sensitive for the diagnosis of TB as it can identify early signal changes. However, MRI findings are generally not specific and a biopsy is still necessary to differentiate TB from other infections and malignancy. Key features which appear more commonly in spinal TB compared with other pyogenic spondylitis include well-defined paraspinal abnormal signal, thin and smooth abscess wall, intraosseous abscess, subligamentous spread to >2 vertebral levels, involvement of multiple vertebral bodies, thoracic spine localization and hyperintense signals on T2-weighted imaging.5 6
As previously discussed in the case presented, the MRI spine showed multiple features not consistent with TB. Given the history of a resected carotid body tumour, a Ga68 DOTATATE CT/PET scan was performed to investigate for metastatic paraganglioma.
Paragangliomas are neuroendocrine tumours associated with neurons of the autonomic nervous system. They can arise anywhere along the paravertebral axis.7 The majority of paragangliomas are benign; however, metastasis can occur and are often associated with hereditary forms.8 A combination of molecular and anatomic imaging is used to stage paragangliomas. PET/CT with Ga68 DOTATATE-coupled peptides have been showed to have a high sensitivity and specificity for staging and diagnosing the disease.9 10 In the case presented, the Ga68 DOTATATE PET/CT was diagnostic for metastatic paraganglioma, given the patient’s previous histological diagnosis from the carotid body tumour. Therefore, a biopsy of the highly vascular spinal lesions was not undertaken.
Immunosuppression is a well-known risk factor for reactivation of TB. This patient was not known to be immunosuppressed at the time of diagnosis of TB; however, metastatic malignancy may have caused a degree of immunosuppression and been a contributor to developing active TB infection.
This case report is a reminder that although spinal TB can have a broad range of radiological features, there are other processes including malignancy and other infections that need to be considered. If the radiological features on MRI spine are not typical for TB spondylitis in a patient with known TB, then further investigations may still be warranted.
Learning points.
This case is a reminder that patients can have dual pathologies, especially noting the complex interplay between tuberculosis (TB), malignancy and the immune system.
The radiological features of spinal TB are varied and can mimic pyogenic spondylitis and malignancy.
It is important for physicians to be aware of the typical radiological features of spinal TB and if they are not present, further investigations are warranted even when culture and drug susceptibility information is available from another anatomical site, most commonly culture of sputum.
A new imaging modality (Ga68 DOTATATE PET/CT) for a rare neuroendocrine tumour has enabled a non-invasive diagnosis of metastatic disease which otherwise may have been delayed on the assumption that the spinal disease was TB or resulted in significant morbidity due to invasive sampling of highly vascular spinal tissue.
Footnotes
Patient consent for publication: Obtained.
Contributors: All authors have made an individual contribution to this case report. JG, CC and GE were involved in the management of this patient as well as planning of the case report and background research. JG has written the majority of this manuscript and JC has provided the interpretation of the radiology images. All authors have contributed to the manuscript editing.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Miller AC, Polgreen LA, Cavanaugh JE, et al. Missed opportunities to diagnose tuberculosis are common among hospitalized patients and patients seen in emergency departments. Open Forum Infect Dis 2015;2:171 10.1093/ofid/ofv171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garg RK, Somvanshi DS. Spinal tuberculosis: a review. J Spinal Cord Med 2011;34:440–54. 10.1179/2045772311Y.0000000023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hong SH, Choi J-Y, Lee JW, et al. MR imaging assessment of the spine: infection or an imitation? Radiographics 2009;29:599–612. 10.1148/rg.292085137 [DOI] [PubMed] [Google Scholar]
- 4.Rivas-Garcia A, Sarria-Estrada S, Torrents-Odin C, et al. Imaging findings of pott’s disease. Eur Spine J 2013;22 Suppl 4:567–78. 10.1007/s00586-012-2333-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jung NY, Jee WH, Ha KY, et al. Discrimination of tuberculous spondylitis from pyogenic spondylitis on MRI. AJR Am J Roentgenol 2004;182:1405–10. 10.2214/ajr.182.6.1821405 [DOI] [PubMed] [Google Scholar]
- 6.Lee KY. Comparison of pyogenic spondylitis and tuberculous spondylitis. Asian Spine J 2014;8:216–23. 10.4184/asj.2014.8.2.216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang CA, Pattison DA, Tothill RW, et al. (68)Ga-DOTATATE and (18)F-FDG PET/CT in Paraganglioma and Pheochromocytoma: utility, patterns and heterogeneity. Cancer Imaging 2016;16:22 10.1186/s40644-016-0084-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kantorovich V, King KS, Pacak K. SDH-related pheochromocytoma and paraganglioma. Best Pract Res Clin Endocrinol Metab 2010;24:415–24. 10.1016/j.beem.2010.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Janssen I, Blanchet EM, Adams K, et al. Superiority of [68Ga]-DOTATATE PET/CT to other functional imaging modalities in the localization of sdhb-associated metastatic pheochromocytoma and paraganglioma. Clin Cancer Res 2015;21:3888–95. 10.1158/1078-0432.CCR-14-2751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haug AR, Cindea-Drimus R, Auernhammer CJ, et al. The role of 68Ga-DOTATATE PET/CT in suspected neuroendocrine tumors. J Nucl Med 2012;53:1686–92. 10.2967/jnumed.111.101675 [DOI] [PubMed] [Google Scholar]