Abstract
Background
Information is needed on bleeding risk factors specific for patients with atrial fibrillation (AF) treated with non-vitamin K oral anticoagulants (NOACs). We aimed to identify risk factors in a large real-world cohort and to derive a bleeding risk score for patients with AF treated with NOACs.
Methods
From nationwide registries (the Norwegian Patient Registry and the Norwegian Prescription Database), we identified patients with AF with a first prescription of a NOAC between January 2013 and June 2015. Cox proportional-hazards analysis was used to identify the strongest risk factors for major or clinically relevant non-major (CRNM) bleeding. Based on these, a risk prediction score was derived. Discrimination was assessed with Harrel’s C-index. C-indexes for the modified Hypertension, Age, Stroke, Bleeding tendency/predisposition, Labile international normalised ratios, Elderly age, Drugs or alcohol excess (HAS-BLED), the Anticoagulation and Risk Factors in Atrial Fibrillation (ATRIA) and the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT) scores were also calculated from the same cohort.
Results
Among 21 248 NOAC-treated patients with a median follow-up time of 183 days, 1257 (5.9%) patients experienced a major or CRNM bleeding. Ten independent risk factors for bleeding were identified, which when included in a risk prediction model achieved a C-index of 0.68 (95% CI 0.66 to 0.70). A simplified score comprising three variables; age, history of bleeding and non-bleeding related hospitalisation within the last 12 months, yielded a c-index of 0.66 (95% CI 0.65 to 0.68). In the same cohort, the modified HAS-BLED, ATRIA and ORBIT scores achieved c-indexes of 0.62 (95% CI 0.60 to 0.63), 0.66 (95% CI 0.64 to 0.67) and 0.66 (95% CI 0.64 to 0.67), respectively.
Conclusions
Our proposed simplified bleeding score could be a useful clinical tool for quick estimation of risk of bleeding in patients with AF treated with NOACs.
Keywords: cardiac arrhythmias, atrial fibrillation, epidemiology, haemorrhage, anticoagulants
Key messages.
What is already known about this subject?
Oral anticoagulation (OAC) is highly effective in preventing stroke and reducing mortality in patients with atrial fibrillation.
Non-vitamin K oral anticoagulants (NOACs) have gradually replaced vitamin K antagonists as drugs of choice. Before prescribing OAC, the doctors should determine the patients’ risk of bleeding.
What does this study add?
Several risk scores for bleeding have previously been published, but none have been derived from real-world cohorts consisting solely of patients using NOACs.
In a large real-world cohort of patients using NOACs, we have identified strong predictors of bleeding and subsequently derived a simple risk score for bleeding, requiring no laboratory or radiological tests, and therefore being available for use by physicians anywhere.
How might this impact on clinical practice?
This study sheds light on predictors of bleeding specific for patients using NOACs and offers the physician a tool for rapidly identifying individuals at increased risk for bleeding, being in need of closer follow-up.
Introduction
Atrial fibrillation (AF) is associated with an overall fivefold increase in the risk of embolic stroke and a twofold increase in the risk of death.1 2 Numerous trials and meta-analyses have concluded that oral anticoagulation (OAC) is highly effective in preventing stroke and reducing mortality in patients with AF.3 Historically, dose-adjusted vitamin K antagonism (warfarin) has been the only available option, but in recent years, four non-vitamin K oral anticoagulants (NOACs) have been approved for stroke prevention in non-valvular AF (dabigatran, rivaroxaban, apixaban and edoxaban). NOACs are gradually replacing warfarin as the drugs of choice for anticoagulation in patients with AF.4 5
A major concern with the use of anticoagulants is the associated bleeding risk. According to a recent registry-based study of 54 321 patients with AF on OAC, 4.5% experienced a major bleeding event during an average follow-up period of 403 days.6 In the Effective Anticoagulation With Factor Xa Next Generation in Atrial Fibrillation–Thrombolysis In Myocardial Infarction (ENGAGE AF–TIMI 48) trial, 579 (1.22%) of 21 105 patients developed major gastrointestinal bleedings per year.7 It is likely that a substantial number of these bleeding events could be prevented, if patients at high risk of bleeding were identified, and preventive measures were taken prior to initiation of, or during treatment with OAC. The tools available to estimate the risk of bleeding associated with use of NOACs are limited, as most of the existing bleeding risk scores were developed in the pre-NOAC era.8–10 Furthermore, most risk scores were developed using data from randomised trials and/or selected registries rather than from real-life cohorts. The aim of this cohort study was to identify risk factors for bleeding in a nationwide cohort of patients with AF being treated with NOACs and to derive a bleeding risk-score for patients with AF treated with NOACs.
Methods
Data sources
The nationwide cohort used in this study has already been investigated in a previous study.11 The cohort is based on data from two nationwide registries: the Norwegian Patient Registry (NPR) and the Norwegian Prescription Database (NorPD). The NPR was established in 2008 and holds information on all patient visits from all hospitals in Norway (emergency, inpatient and outpatient consultations), including relevant diagnoses, procedures performed and duration of stay.12 Diagnoses are coded according to the International Classification of Diseases, 10th revision (ICD10). Medical and surgical procedures are coded according to the Nordic Medico-Statistical Committee (NOMESCO) coding system. Both primary and secondary codes related to each admission were taken into account in the analyses.
The NorPD is a registry containing information on all prescriptions dispensed at pharmacies nationwide (drugs are coded according to the Anatomical Therapeutic Chemical system, ATC).13 The Norwegian system of general reimbursement of medicine expenses for treatment of serious and prolonged chronic illnesses requires the prescribing physician to state the relevant underlying disease for each drug. The NorPD also contains information about date of dispensation, quantity and strength of drugs dispensed and time of all-cause death.
Cohort creation and study design
All patients≥18 years diagnosed with non-valvular AF in the study period were identified from the NPR, and this dataset was then linked to the NorPD to identify all patients with AF with at least one NOAC dispensation in the study period (1 January 2013 to 30 June 2015). Non-valvular AF was defined in accordance with the 2016 European Society of Cardiology guidelines as AF in the absence of rheumatic valvular disease or mechanical heart valves.14 Only doses recommended for stroke prevention in AF were included: apixaban 2.5 mg or 5 mg; rivaroxaban 15 mg or 20 mg or dabigatran 110 mg or 150 mg. Edoxaban was still not approved for stroke prevention in AF in the study period and thus not included in this study. Index date was defined as the first dispensation of a NOAC in the study period. To establish an OAC naïve cohort, patients were excluded if they had been exposed to OACs in the 180 days before index date, diagnosed with deep venous thrombosis during the last 180 days before index date or having had knee-replacement or hip-replacement surgery performed within the last 35 days before the index date. For this specific study, we selected all patients from this cohort being treated with a NOAC.11 A cohort creation chart is presented in figure 1, and the study design is presented in figure 2.
Figure 1.

Cohort creation flowchart. NorPD, Norwegian Prescription Database; NPR, Norwegian Patient Registry; NVAF, non-valvular atrial fibrillation; OAC, oral anticoagulant; VTE, venous thromboembolism.
Figure 2.

Study design. NOAC index date was the date of the first OAC dispensation (warfarin, apixaban, rivaroxaban, dabigatran) in the study period (January 2013–June 2015). Each patient was followed from the index date to the date of discontinuation orswitching of OAC therapy, date of death, or end of the study period. OAC, oralanticoagulant.
Comorbidity and medication history
The diagnoses for all hospital consultations including procedures performed were extracted from the NPR. From a prespecified list, a medication history during the preindex period, including the relevant diagnosis-specific reimbursement codes, was completed from the NorPD (see online supplementary table S1).
openhrt-2018-000931supp001.pdf (184.3KB, pdf)
Oral anticoagulant supply
For each dispensation, length of OAC supply was computed using information on date of dispensation, the number of packages and the pack-size dispensed. As NOACs are prescribed in fixed doses, the number of days of supply strictly corresponds to amount dispensed. The NorPD contains information on tablet strength, pack-size and number of packages dispensed, and we assumed, according to the labelling, two times per day dosing for apixaban and dabigatran and once daily dosing for rivaroxaban. To estimate the end of OAC supply date, we accounted for incomplete adherence by allowing a gap period of 30 days after the calculated end of OAC supply. Patients were censored on discontinuation or switching of OAC, death or end of follow-up, whichever occurred first.
Bleeding complications
Bleeding episodes were identified through search for prespecified ICD10-codes in the NPR between index date and 30 days after the calculated end of OAC supply. Bleeding events were categorised as major or clinically relevant non-major (CRNM) bleeding. Major bleeding was defined as any bleeding event which occurred in a critical area or organ or any bleeding event that was accompanied by blood transfusion ≤10 days after hospital admission date (see online supplementary table S2). This is a slight modification of the classification according to the International Society on Thrombosis and Haemostasis (ISTH) because no information was available in our data set on haemoglobin levels.15 A CRNM bleeding was defined in accordance with the ISTH classification as any bleeding requiring medical intervention by a healthcare professional or leading to hospitalisation or increased level of care or prompting a face-to-face evaluation, which did not fit the criteria for major bleeding.16 In this study, major and CRNM bleeding were analysed together.
Ethics
Registration of information in NPR and NorPD is mandatory in Norway and legally exempt from obtainment of patient consent. All people resident in Norway are given a Norwegian national identification number, which allows for linkage of the two databases on an individual level.
Statistical analysis
Categorical variables are reported by numbers and percent, continuous variables by mean±SD or median (25th–75th percentiles). To develop the risk prediction model, general principles from the Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD) statement were followed.17 Cox proportional-hazards regression was used to analyse the time to the first bleeding episode taking censoring into account. Cases with missing data were handled by listwise deletion. After resolving issues of multicollinearity by excluding affected variables, the proportional hazard assumption was checked using Schoenfeld residuals and by comparing the log-log transformation of the Kaplan Meier survival curves for each variable.18 A gender-stratified saturated Cox proportional-hazards model was fitted. Age was included as the only continuous variable. From the saturated model, an alpha level of 0.1 was used as a threshold to enter a variable predictor into a backwards elimination model.
Discrimination was assessed by Harrell’s C-statistic and by comparing Kaplan-Meier curves and HRs.19 Each model was internally validated by bootstrapping using 300 samples. A risk prediction score was derived from the Cox model by adding rounded HRs.
Annualised Kaplan-Meier event rates using person-time of follow-up were calculated according to an increase in integer score and then categorised into four categories: low risk (0–2 points), low intermediate risk (3–4 points), high intermediate risk (5–6 points) and high risk (7–12 points).
The full model was reduced to a three-variable model, based on the variables’ predictive abilities, reliability and simplicity. The performance of the simplified model was assessed by Harrell’s C-statistic. In a manner similar to that described for the full model, an integer risk score was created, annualised Kaplan-Meier event-rates calculated according to an incremental increase in integer score and then categorised into three categories: low risk (0–1 points), intermediate risk (2–3 points) and high risk (4–5 points). The simple model was internally validated by bootstrapping using 300 samples.
For comparison, the C-indexes for three previously published scores were calculated on the same cohort: the Hypertension, Age, Stroke, Bleeding tendency/predisposition, Labile international normalised ratios, Elderly age, Drugs or alcohol excess (HAS-BLED) score,8 the Anticoagulation and Risk Factors in Atrial Fibrillation (ATRIA) score10 and the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT) score.9
As some of the variables in these three scores were unavailable to us (elevated liver enzymes, drug abuse and labile INR in the HAS-BLED score; renal failure with eGFR <30 mL/min in the ATRIA score), they were modified to include the variables available. For the modified ATRIA score, patients with chronic kidney disease (CKD) stages 3 and 4 (ICD10 code N183 and N184) were included, and the definitions used for the construction of the modified HAS-BLED score are listed in online supplementary table S7.
Statistical analyses were performed using SAS V.9.4 (SAS Institute) and STATA V.15 (STATA). Level of significance was set to 5%; all CIs are 95%.
Results
The cohort included 21 248 patients, of whom 12 205 (57%) were men and the mean age was 73 years. Due to missing data, 186 (0.9%) patients were removed by listwise deletion. Table 1 shows the baseline characteristics. A total of 7925 (37.3%) patients were treated with dabigatran, 6817 (32.1%) with rivaroxaban and 6506 (30.6%) with apixaban. Hypertension was the most common comorbidity, affecting 13 431 (63.2%) of the patients and one quarter had ischaemic heart disease. The mean CHA2DS2-VASc score was 2.76. During a median follow-up time of 183 days (91-358), and 14 155 person-years, 1257 (5.9%) patients experienced a major or CRNM bleeding, corresponding to 8.9 bleeding events/100 person years.
Table 1.
Baseline characteristics of the study population (n=21 248)
| Male sex | 12 205 (57.4) |
| Age, years | |
| Mean (SE) | 73 (11.2) |
| Median (25th–75th percentile) | 73 (66–82) |
| ≥75 years | 9786 (46.1) |
| Type NOAC used | |
| Dabigatran | 7925 (37.3) |
| Rivaroxaban | 6817 (32.1) |
| Apixaban | 6506 (30.6) |
| Medical history | |
| Hypertension | 13 431 (63.2) |
| Chronic kidney disease | 1046 (4.9) |
| Chronic heart failure | 3979 (18.7) |
| Ischaemic heart disease | 5230 (24.6) |
| History of stroke/TIA | 2746 (12.9) |
| COPD | 1665 (7.8) |
| Diabetes | 2413 (11.4) |
| Dementia | 369 (1.7) |
| Anaemia (last year) | 559 (2.6) |
| Active cancer (last year) | 1776 (8.4) |
| Previous bleeding hospitalisation | 2881 (13.6) |
| Non-bleeding related hospitalisation (last year) |
13 294 (62.6) |
| Medication before index date | |
| Previous use of OAC (>180 days prior to index) | 2175 (10.2) |
| Antiplatelet therapy | 11 217 (52.8) |
| Low-dose aspirin (last year) | 10 612 (49.9) |
| Non-aspirin platelet inhibitor | 605 (2.8) |
| NSAIDs (last year) | 5018 (23.6) |
| Risk scores | |
| Modified HAS-BLED score ≥3 | 9169 (43.2) |
| CHA2DS2-VASc score | |
| Mean | 2.76 |
| ≥2 | 16 905 (79.6) |
| Comorbidity score ≥1 | 11 891 (56.0) |
| Reduced NOAC dose at index date | 6303 (29.7) |
Values are numbers (percentages) unless otherwise stated.
COPD, chronic obstructive pulmonary disease; NOAC, non-vitamin K oral anticoagulant; NSAIDs, non-steroidal anti-inflammatory drugs; OAC, oral anticoagulant; TIA, transient ischaemic attack.
The strongest predictors of bleeding were: age, history of bleeding (major or CRNM), CKD, chronic obstructive pulmonary disease (COPD), previous stroke/transient ischaemic attack (TIA), male sex, anaemia diagnosed during the last 12 months, heart failure, hypertension and non-bleeding related hospital admission during the last 12 months (table 2). We constructed an integer risk score based on these 10 variables. For the purpose of clarification of the cumulative hazards-illustration (figure 3), the age variable was divided into three groups;<65 years, 65–75 years and >75 years. The model showed a Harrel’s C-index of 0.68 (95% CI 0.66 to 0.70). Table 3 shows distribution of patients within the risk score and the 1 year cumulative bleeding risks.
Table 2.
Individual predictors of bleeding in full model
| Risk factor | HR (95% CI) | P value | Score |
| Male sex | 1.242 (1.106 to 1.394) | <0.001 | 1 |
| Age (continuous) | 1.036 (1.029 to 1.043) | <0.001 | |
| Age (categorical) | |||
| <65 years | 1.00 (reference) | 1 for age 65–75 | |
| 65–75 years | 1.637 (1.291 to 1.043) | ||
| >75 years | 2.544 (2.047 to 3.147) | 2 for age >75 | |
| Hypertension | 1.197 (1.061 to 1.351) | 0.003 | 1 |
| Chronic kidney disease | 1.257 (1.028 to 1.584) | 0.041 | 1 |
| Chronic heart failure | 1.260 (1.114 to 1.426) | <0.001 | 1 |
| Stroke/TIA in history | 1.250 (1.100 to 1.421) | 0.001 | 1 |
| COPD | 1.276 (1.0579 to 1.538) | 0.011 | 1 |
| Anaemia diagnosed last 12 months | 1.400 (1.052 to 1.865) | 0.021 | 1 |
| Bleeding in history | 1.996 (1.743 to 2.284) | <0.001 | 2 |
| Hospitalisation (non-bleeding related), last 12 months |
1.165 (1.013 to 1.339) | 0.032 | 1 |
| SUM | 12 | ||
COPD, chronic obstructive pulmonary disease; TIA, transient ischaemic attack.
Figure 3.
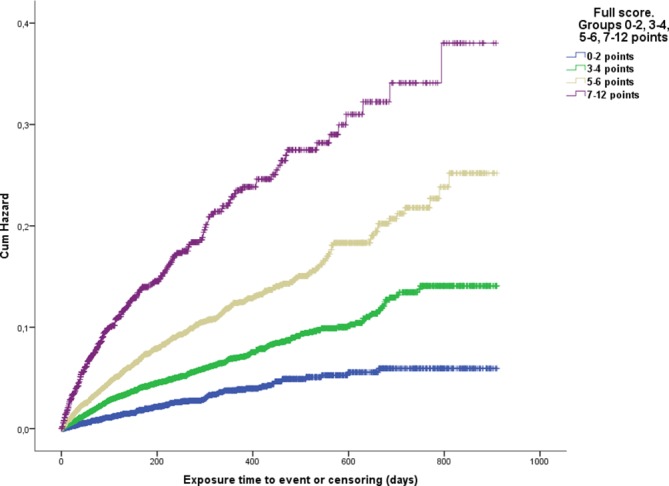
Cumulative hazard of bleeding in relation to score level (full score). Blue line, 0–2 points; green line, 3–4 points; brown line, 5–6 points; purple line 7–12 points.
Table 3.
Distribution of patients within model and cumulative bleeding risk
| Score | Total N | No. of events | 1 year cumulative risk (%) |
| 0 | 206 | 3 | 1.96 |
| 1 | 1734 | 31 | 3.24 |
| 2 | 3139 | 85 | 4.10 |
| 3 | 4625 | 206 | 6.37 |
| 4 | 4601 | 268 | 7.61 |
| 5 | 3330 | 253 | 11.35 |
| 6 | 1820 | 180 | 14.63 |
| 7 | 979 | 130 | 22.23 |
| 8 | 445 | 64 | 24.52 |
| 9 | 149 | 29 | 28.10 |
| 10 | 31 | 7 | 24.45 |
| 11 | 3 | 1 | N/A |
| 12 | 0 | 0 | N/A |
A simplified version of the score was subsequently derived using the following three variables: Age (<65 years, 65–75 years and >75 years), history of Bleeding (major or CRNM) and non-bleeding related Hospitalisation within the last 12 months. The three variables were chosen for their unambiguity and accessibility bedside. This simplified ‘ABH-score’ showed a C-index of 0.66 (95% CI 0.65 to 0.67). Table 4 shows the specific statistics for the simplified score and figure 4 shows the cumulative hazard of bleeding in the different risk groups. The results of internal validation by bootstrapping for the two models are shown in online supplementary tables S4 and S5. Receiver operating characteristic curves comparing the full 10-variable score with the ABH-score are shown in the online supplementary file 1.
Table 4.
ABH-Score
| Risk factor | HR (95% CI) | P value | Score |
| Age groups | |||
| <65 years | 1.00 (reference) | ||
| 65–75 years | 1.666 (1.398 to 1.998) | <0.001 | 1 for age 65–75 |
| 75 years | 2.681 (2.109 to 3.287) | <0.001 | 2 for age >75 |
| History of bleeding | 2.208 (1.914 to 2.447) | <0.001 | 2 |
| Hospitalisation (non-bleeding related) last 12 months | 1.365 (1.215 to 1.486) | <0.001 | 1 |
| Distribution with in score | Total N | No. of events | 1-year cumulative risk (%) |
| 0 | 1948 (9.2) | 28 | 2.34 |
| 1 | 4704 (22.1) | 139 | 4.48 |
| 2 | 6 352 (29.9) | 341 | 7.13 |
| 3 | 5 864 (27.6) | 450 | 11.46 |
| 4 | 946 (4.5) | 116 | 19.35 |
| 5 | 1 434 (6.7) | 183 | 20.29 |
Figure 4.
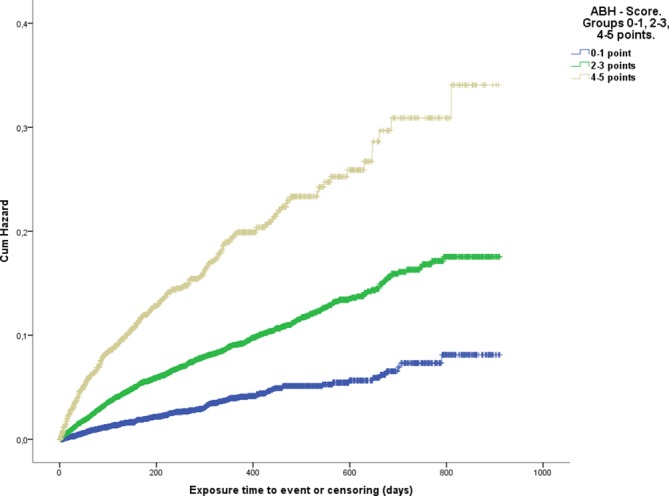
Applied on the same cohort, the modified HAS-BLED score showed a C-index of 0.62 (95% CI 0.60 to 0.63), the modified ATRIA score a C-index of 0.66 (95% CI 0.64 to 0.67) and the ORBIT score a C-index of 0.66 (95% CI 0.64 to 0.67).
Discussion
This study aimed to identify predictors of bleeding in a large real-world population of patients with AF treated with NOACs. We identified 10 independent predictors of bleeding and derived a bleeding risk score which showed a good discriminative ability (C-statistic 0.68 (95% CI 0.66 to 0.70)). Risk prediction scores that involve many predictor variables are often difficult to remember and require detailed knowledge of the patient’s medical history and laboratory parameters. To provide the clinician with a tool that is easily remembered and can be used bedside, we derived a three-variable simplified version of the score that was given the acronym ‘ABH-score’. This simplified score showed comparable predictive ability to previously published scores (C-statistic 0.66 (0.65 to 0.67)).
A recently published Danish study investigated the predictive abilities of the ATRIA, ORBIT and HAS-BLED scores in a very similar cohort of Danish patients with AF treated with NOACs.20 They found C-statistics for ATRIA of 0.59 (95% CI 0.57 to 0.60), HAS-BLED 0.58 (95% CI 0.57 to 0.59) and ORBIT 0.61 (95% CI 0.59 to 0.62). Although they investigated major bleeding only, the C-statistics were modest and in line with our estimates for the three scores based on our cohort.
The HAS-BLED score was derived from the EuroHeart survey AF population on vitamin K antagonist (VKA)8 and has subsequently been validated in patient cohorts taking OAC (VKA and Idraparinux).21 The ATRIA bleeding score was derived from the ATRIA community cohort of VKA users and later validated in the ROCKET-AF trial population.10 The ORBIT score was derived from the ORBIT registry composed mostly of VKA users.9 Despite being validated in patients using NOACs, and also in real-world populations, none of the existing risk scores were initially derived from real-world population cohorts.
Unlike stroke-specific risk scores, there have been no randomised trials that have proven an overall benefit of withholding OAC from patients on the basis of a high bleeding risk score. Although the risk of bleeding is dynamic and repeated bleeding risk assessments have been shown to increase accuracy of risk prediction, there is no bleeding risk threshold above which the beneficial effect of anticoagulation is offset by the risk of serious bleeding.22 Large observational data have shown a clear net clinical benefit from OAC despite very high bleeding risks.23 Also, cessation of OAC leads to increased risk of stroke, cardiovascular events and mortality. Simultaneously, studies have shown that 30%–60% of American patients with AF do not receive anticoagulation when indicated, probably mainly due to fear of bleeding, and that elevated bleeding risk often leads to discontinuation of OAC.24 25 To increase the likelihood of physicians prescribing anticoagulants for patients of AF, it is of utmost importance that they are familiar with the properties of NOACs and that their judgement of risks and benefits are based on solid evidence.
The two risk scores we present in this study seem to perform comparably. The importance of our full score lies in the presentation of distinct risk factors for patients with AF on NOACs. Several of the risk factors are potentially modifiable, such as hypertension, heart failure, CKD and COPD. It is logical to assume that modification of these may reduce the risk of bleeding. Physician awareness of these treatable chronic illnesses is thus especially important. The simplified version of the score has no modifiable risk factors; instead it consists of unambiguous risk factors without any grading or degree of severity, thereby leaving no room for misinterpretation. Also, it can be assessed without need for blood tests or imaging and still has a comparable discriminative ability to the alternative scores. In the simplified ABH-score, the variable ‘non-bleeding related hospitalisation’ serves as a surrogate marker of disease burden, emphasising the importance of considering the patient’s comorbidities as a whole. In general, a high bleeding risk score should not deter the clinician from prescribing OAC, but rather prompt a careful evaluation of each patient’s individual set of risk factors, with subsequent modification whenever possible.26
Concomitant use of antiplatelet drugs, but not non-steroidal anti-inflammatory drugs (NSAIDs), was associated with increased risk of bleeding in the univariate analysis. However, use of antiplatelet drugs was not included in our scores (online supplementary table S3), since it did not achieve statistical significance in the multivariate analysis. Nonetheless, other studies have shown that such a combination of drugs increases the risk of bleeding. Discontinuation of antiplatelet and avoidance of concomitant use of NSAIDs are recommended in all patients treated with NOACs, if these drugs are not strictly indicated. In general, use of risk scores does not imply that well known risk factors not being included in the risk score should be disregarded. The simple risk score could be used as a practical and quick tool for risk estimation, but other risk factors should also be taken into consideration.
Strengths and limitations
The strength of our study is that it retrieved data from mandatory and nationwide registries in a public healthcare system that covers all residents. As a result, the dataset gave us a complete list of all hospital contacts and prescriptions dispensed nationwide for the entire study period. This complete coverage of data eliminates selection bias and recall bias that is an apparent problem using other databases based on selected hospitals, health insurance schemes, self-reported questionnaires or clinical trials where the patients are highly selected and subjected to thorough follow-up which may reduce the risk of bleeding. Our score may be more suitable to assess the risk of bleeding in patients in the routine practice. With the exception of apixaban being granted general reimbursement 6 months after rivaroxaban and dabigatran, the same conditions for OAC prescribing were valid nationwide and throughout the study period.
One limitation of the study was that we did not have access to information on laboratory tests such as thrombocyte and erythrocyte count, estimated glomerular filtration rate, liver enzymes or cardiac markers as well as other important characteristics such as smoking and body weight. One other caveat that influences the external validity of the results is that the AF diagnosis was retrieved from hospital level only, meaning that patients with AF who were solely managed in primary care were not included in the study. However, most of the patients with AF in Norway are referred to the hospital for evaluation and initiation of therapy.
Due to the registry-based nature of this study, bleeding endpoints were not adjudicated. Therefore, some bleeding episodes may have been overlooked. Likewise, bleeding tendencies may be identified earlier in patients enrolled in clinical trials, due do closer follow-up, accordingly, major or fatal bleedings that would have occurred in real life may not be seen in trial cohorts.
The study participants were largely white Europeans. This may limit the generalisability of the results. Due to the relatively small number of patients on each separate NOAC, we did not consider possible differences in bleeding risk factors between the different NOACs. Although all prescribed drugs were included in our data set, use of non-prescription drugs (eg, NSAIDs) would go undetected. Bleeding episodes or other significant comorbidities only revealed in the primary care setting would not be visible in our data set and may thus be under-represented. There is also a risk of misclassification related to coding errors of hospital admissions; however, for serious conditions like bleeding, this is unlikely. No formal validation studies of the AF diagnosis in NPR against health records have been conducted. We studied drug exposure at the level of pharmacy dispensation and have no information on patient’s actual NOAC intake. The full-scale and the simplified scores have so far only been internally validated. The scores’ discriminative abilities were assessed with Harrel’s C-statistic, a measure chosen on account of its widespread use and assumed physician familiarity, but will naturally be restricted by any and all inherent weaknesses of the C-statistic.
Conclusion
In this nationwide cohort study on patients with AF being prescribed NOACs, we have identified strong predictors of bleeding, several of which are potentially modifiable. A simplified, easy to remember bleeding risk score was derived that could allow the clinician to rapidly identify high-risk patients in need of closer attention and follow-up, without the need for laboratory or radiological tests.
Footnotes
Correction notice: This paper has been updated since first published. In Table 4, row 4, column ‘Score’, data has been revised from ‘for age > 75’ to ‘2 for age>75’.
Contributors: WG, CJ and SH contributed in conception and design of the study. CJ, WG and SH contributed with data collection. O-CWR, RH, CJ, WG and SH contributed with data analysis and interpretation. O-CWR drafted the manuscript. CJ, RH, WG and SH critically revised the manuscript and approved the final version to be published.
Funding: The study was funded by the South-Eastern Norway Regional Health Authority. Additional funding was granted by Bristol-Myers Squibb/Pfizer through the European Investigator Initiated Research Program ERISTA (Grant number CV185-619) and Helse Sør-Øst RHF.
Competing interests: O-CWR reports personal fees from Boehringer Ingelheim, Novartis and Pfizer, outside the submitted work. CJ reports personal fees from Pfizer and Bayer, outside the submitted work. WG reports grants and personal fees from Bayer, grants and personal fees from Novartis, personal fees from Amgen, personal fees from Pfizer, outside the submitted work. RH reports no conflicts of interest. SH reports personal fees from Pfizer, Bayer, Boehringer Ingelheim and Bristol-Myers Squibb, outside the submitted work.
Patient consent for publication: Not required.
Ethics approval: Norwegian Regional Ethics Committee (Ref. No. 2015/162/REC Central).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 1991;22:983–8. 10.1161/01.STR.22.8.983 [DOI] [PubMed] [Google Scholar]
- 2.Kamel H, Okin PM, Elkind MSV, et al. . Atrial fibrillation and mechanisms of stroke. Stroke 2016;47:895–900. 10.1161/STROKEAHA.115.012004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hart RG, Benavente O, McBride R, et al. . Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta-analysis. Ann Intern Med 1999;131:492–501. 10.7326/0003-4819-131-7-199910050-00003 [DOI] [PubMed] [Google Scholar]
- 4.Heidbuchel H, Verhamme P, Alings M, et al. . Updated European heart rhythm association practical guide on the use of non-vitamin K antagonist anticoagulants in patients with non-valvular atrial fibrillation. Europace 2015;17:1467–507. 10.1093/europace/euv309 [DOI] [PubMed] [Google Scholar]
- 5.Oktay E. Will NOACs become the new standard of care in anticoagulation therapy? Int J Cardiovasc Acad 2015;1:1–4. 10.1016/j.ijcac.2015.06.007 [DOI] [Google Scholar]
- 6.Lamberts M, Staerk L, Olesen JB, et al. . Major bleeding complications and persistence with oral anticoagulation in non-valvular atrial fibrillation: contemporary findings in real-life danish patients. J Am Heart Assoc 2017;6 10.1161/JAHA.116.004517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aisenberg J, Chatterjee-Murphy P, Friedman Flack K, et al. . Gastrointestinal bleeding with edoxaban versus warfarin: results from the engage af-timi 48 trial (effective anticoagulation with factor xa next generation in atrial fibrillation-thrombolysis in myocardial infarction). Circ Cardiovasc Qual Outcomes 2018;11(5:e003998. [DOI] [PubMed] [Google Scholar]
- 8.Pisters R, Lane D A, Nieuwlaat R, et al. . A novel user-friendly score (HAS-BLED) to Assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro heart survey, 2010. [DOI] [PubMed] [Google Scholar]
- 9.O'Brien EC, Simon DN, Thomas LE, et al. . The ORBIT bleeding score: a simple bedside score to assess bleeding risk in atrial fibrillation. Eur Heart J 2015;36:ehv476–64. 10.1093/eurheartj/ehv476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fang MC, Go AS, Chang Y, et al. . A new risk scheme to predict warfarin-associated hemorrhage: the ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation) Study. J Am Coll Cardiol 2011;58:395–401. 10.1016/j.jacc.2011.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Halvorsen S, Ghanima W, Fride Tvete I, et al. . A nationwide registry study to compare bleeding rates in patients with atrial fibrillation being prescribed oral anticoagulants. Eur Heart J Cardiovasc Pharmacother 2017;3:28–36. 10.1093/ehjcvp/pvw031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bakken IJ NK, Halsteinli V, Kvam UH. The Norwegian patient registry. Norwegian J Epidemiol 2004;14:65–9. [Google Scholar]
- 13.Wettermark B, Zoëga H, Furu K, et al. . The Nordic prescription databases as a resource for pharmacoepidemiological research--a literature review. Pharmacoepidemiol Drug Saf 2013;22:691–9. 10.1002/pds.3457 [DOI] [PubMed] [Google Scholar]
- 14.Kirchhof P, Benussi S, Kotecha D, et al. . 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 2016;37:2893–962. 10.1093/eurheartj/ehw210 [DOI] [PubMed] [Google Scholar]
- 15.Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis . Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 2005;3:692–4. 10.1111/j.1538-7836.2005.01204.x [DOI] [PubMed] [Google Scholar]
- 16.Kaatz S, Ahmad D, Spyropoulos AC, et al. . Definition of clinically relevant non-major bleeding in studies of anticoagulants in atrial fibrillation and venous thromboembolic disease in non-surgical patients: communication from the SSC of the ISTH. J Thromb Haemost 2015;13:2119–26. 10.1111/jth.13140 [DOI] [PubMed] [Google Scholar]
- 17.Collins GS, Reitsma JB, Altman DG, et al. . Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. The TRIPOD group. Circulation 2015;131:211–9. 10.1161/CIRCULATIONAHA.114.014508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hess KR. Graphical methods for assessing violations of the proportional hazards assumption in cox regression. Stat Med 1995;14:1707–23. 10.1002/sim.4780141510 [DOI] [PubMed] [Google Scholar]
- 19.Harrel F. Regression modeling strategies with applications to linear models, logistic and ordinal regression and survival analysis. Springer, 2015: 582. [Google Scholar]
- 20.Lip GYH, Skjøth F, Nielsen PB, et al. . The HAS-BLED, ATRIA, and ORBIT bleeding scores in atrial fibrillation patients using non-vitamin K antagonist oral anticoagulants. Am J Med 2018;131:574–27. 10.1016/j.amjmed.2017.11.046 [DOI] [PubMed] [Google Scholar]
- 21.Apostolakis S, Lane DA, Guo Y, et al. . Performance of the HEMORR 2 HAGES, ATRIA, and HAS-BLED bleeding risk-prediction scores in nonwarfarin anticoagulated atrial fibrillation patients. J Am Coll Cardiol 2013;61:386–7. 10.1016/j.jacc.2012.10.010 [DOI] [PubMed] [Google Scholar]
- 22.Chao TF, Lip GYH, Lin YJ, et al. . Incident risk factors and major bleeding in patients with atrial fibrillation treated with oral anticoagulants: a comparison of baseline, follow-up and delta HAS-BLED scores with an approach focused on modifiable bleeding risk factors. Thromb Haemost 2018;118:768–77. 10.1055/s-0038-1636534 [DOI] [PubMed] [Google Scholar]
- 23.Savarese G, Sartipy U, Friberg L, et al. . Reasons for and consequences of oral anticoagulant underuse in atrial fibrillation with heart failure. Heart 2018;104:1093–100. 10.1136/heartjnl-2017-312720 [DOI] [PubMed] [Google Scholar]
- 24.Friberg L, Rosenqvist M, Lip GY. Net clinical benefit of warfarin in patients with atrial fibrillation: a report from the Swedish atrial fibrillation cohort study. Circulation 2012;125:2298–307. 10.1161/CIRCULATIONAHA.111.055079 [DOI] [PubMed] [Google Scholar]
- 25.Rivera-Caravaca JM, Roldán V, Esteve-Pastor MA, et al. . Cessation of oral anticoagulation is an important risk factor for stroke and mortality in atrial fibrillation patients. Thromb Haemost 2017;117:1448–54. 10.1160/TH16-12-0961 [DOI] [PubMed] [Google Scholar]
- 26.Kirchhof P, Benussi S, Kotecha D, et al. . 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 2016;37:2893–962. 10.1093/eurheartj/ehw210 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
openhrt-2018-000931supp001.pdf (184.3KB, pdf)


