Abstract
Patients value effective pain relief. Complications of inadequate pain control include increased risk of infection, decreased patient comfort and progression to chronic pain, all of which have significant socioeconomic consequence. Accessibility to analgesia is vital to effective administration. This improvement project aimed to improve the consistency and adequacy of analgesia prescribing for trauma inpatients over a 12-month period. Four PDSA (‘plan, do, study, act’) cycles resulted in sustained and significant improvements in analgesia prescription. The interventions included senior encouragement, teaching sessions, targeted inductions and implementation of a novel e-prescribing protocol. Prospective data and real-time discussion from stakeholder medical and management teams enabled iterative change to practice. Drug charts were reviewed for all trauma inpatients (n=276) over a 10-month period, recording all analgesia prescribed within 24 hours of admission. Each prescription was scored (maximum of 10 points) according to parameters agreed by the acute pain specialty leaders. An improving trend was observed in the analgesia score over the study period. Each intervention was associated with improved practice. Based on observed improvements, a novel electronic prescribing protocol was developed in conjunction with the information technology department, resulting in maximum scores for prescribing which were sustained over the final 3 months of the study. This was subsequently adopted as standard practice within the department. One year following completion of the project, a further 3 weeks of data were collected to assess long-term sustainability—scores remained 10 out of 10. Addressing the prescribing habits of junior doctors improved accessibility to analgesia for trauma patients. The electronic prescribing tool made prescribing straightforward and faster, and was the most successful intervention. Doctor satisfaction using this time-saving tool was high. Identifying a stakeholder within the information technology department proved pivotal to transferring the project aims into clinical practice.
Keywords: continuous quality improvement; decision support, computerised; hospital medicine; pain; pdsa
Problem
Excluding neck of femur fractures, between 5 and 15 adult patients are admitted to the Great Western Hospital (GWH) Trauma and Orthopaedic department each week. The GWH is a district general hospital, representative of many in the UK, accepting patients to all major specialties. The GWH uses electronic prescribing (e-prescribing). For each trauma patient, the clerking doctor should complete an electronic drug chart as soon as possible after admission. For all significant trauma, this should include regular and as-required analgesics. Incomplete drug charts with insufficient analgesia led to delays in the availability of analgesia and inappropriate referrals to the specialist pain team. Doctors were often contacted out of hours to prescribe analgesia, which should have been prescribed on admission. In addition to regular analgesia, it was also noted other medications commonly required for analgesia side effects such as nausea, constipation and opiate toxicity were often missing.
The SMART1 goal for this project was to improve the analgesia prescription score within 24 hours of admission for every patient, to 10 out of 10 over within 12 months.
A 10 out of 10 score (described below) also included as-required medications such as antiemetics, laxatives and naloxone.
Background
Patients value highly their pain being well controlled.2 Studies have shown up to two-thirds of patients can wait up to 1 hour for pain relief in accident and emergency departments in the UK and many receive analgesia which is inappropriate for their severity of pain.3 There are many short-term and long-term consequences of inadequately treated acute pain, making it pivotal to patient care. These consequences include increased infection risk, decreased patient comfort and progression to chronic pain.4 Chronic pain also creates significant long-term economic consequences.5
A literature search has identified efforts in multiple disciplines where pain control has been improved for trauma inpatients. Multiple modes of analgesia have been shown to improve acute pain control6 and targeting prescriber education has been demonstrated to improve practice.7
Clear pain treatment protocols have been shown to provide superior pain control with enhanced patient satisfaction.8 In addition, a protocol can help to minimise the length of inpatient stays and limit the progression to chronic pain.9 Effective pain management depends on timely prescription and administration,10 which has also been shown to improve with protocol-based care.8 Prescription of regular and as-required medication is essential to ensuring availability of patient analgesia when needed.
Embracing a multidisciplinary approach has been shown to enhance care provision when optimising pain control,11 which was pivotal to developing and analysing the interventions during this project.
Measurement
Drug charts for all patients admitted under the care of the trauma and orthopaedic department were prospectively reviewed between August 2016 and May 2017. Paediatric and polytrauma patients were excluded as alternative analgesia prescription is often appropriate. Admissions due to neck of femur fracture were also excluded due to having their own specific care pathway. Over the data collection period, a total of 276 patients were admitted, between 3 and 13 per week. All 276 drug charts were analysed for adequacy of analgesia and common side-effect medications.
An ‘ideal trauma admission prescription’ was devised in conjunction with the GWH Pain Team lead consultant, based on the WHO analgesic ladder.12 Commonly used in clinical practice, the ladder method advises building strength of analgesia in a stepwise fashion to avoid unnecessary use of strong opioids. Step 1 medications include paracetamol and ibuprofen. Weak opioids, such as codeine or tramadol, comprise step 2, and stronger opioids, such as morphine, in step 3. Patients with significant pain stimuli from trauma require regular step 1 and 2 analgesics to reduce the need for stronger alternatives.13 Trauma inpatients are at high risk for developing common side effects of opiate analgesia such as nausea, constipation or toxicity.12 Accessibility to analgesia has been demonstrated to impact patient satisfaction and pain control.10 The score used in this study reflected adequacy of analgesia prescription and was recorded within 24 hours of the patient’s admission to reflect accessibility.
A system was created to enable scoring of every drug chart (see table 1).
Table 1 Drug chart scoring system.
| Prescription | Score |
| Regular step 1 (WHO ladder) | 3 |
| Regular step 2 (WHO ladder) | 2 |
| As-required step 3 (WHO ladder) | 2 |
| As-required antiemetic | 1 |
| As-required laxative | 1 |
| As-required naloxone | 1 |
| Total | 10 |
The electronic drug chart of each patient was reviewed and scored between 0 and 10, for medications prescribed within 24 hours of admission. Doses were not specified as this may vary according to patient weight and medical history.
An initial 3-week baseline data set was recorded in August 2016. Fifty-four per cent of trauma patients were prescribed a regular step 1 analgesic, such as paracetamol. Prescribing of ‘as required’ morphine (step 3) was very high (89%). For the baseline period, the median analgesia score was 5/10.
Data collection was continuous following the initial baseline period. All prescriptions were reviewed and a median weekly analgesia score for the department was transferred onto the project run chart (see Results section).
In order to assess long-term sustainability of the project, a further 3 weeks of data were collected in June 2018, 12 months after project completion.
Design
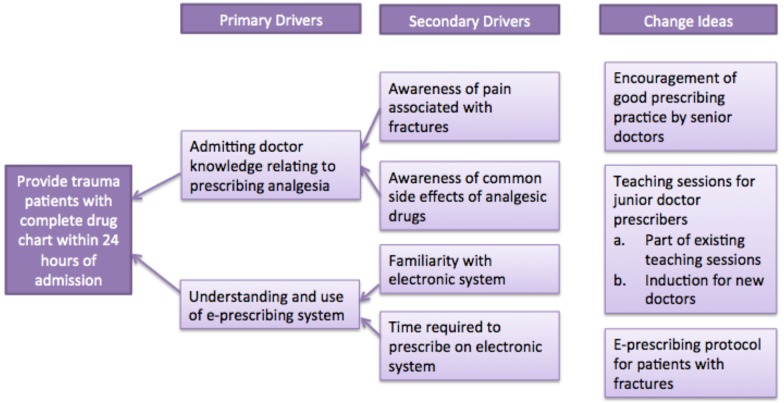
A driver diagram (see figure 1) was used to develop change ideas to improve prescribing. The ‘plan, do, study, act’ (PDSA) model for improvement was used over four cycles.
Figure 1.
Driver diagram depicting the development of intervention ideas.
The authors considered possible reasons for incomplete admission drug charts prior to developing interventions. These included prescriber factors and system factors. Prescribers may not be aware of the benefits of regular analgesia or appreciate the importance of accessibility. Furthermore, prescribers may not be aware of side effects associated with common analgesic medications. With regard to system factors, the e-prescribing system was new to some prescribers and time pressures while clerking patients may have had a negative impact on the quality of prescribing
Four interventions were developed to address drivers: senior encouragement via emails, teaching sessions for junior doctor prescribers, targeted induction for new doctors and implementation of an e-prescribing protocol.
Strategy
The quality improvement team comprised four junior doctors and one consultant (authors). All interventions were developed by the authors after discussion with doctor colleagues and meetings with the pain team specialist nurses, pharmacy and IT representatives.
PDSA 1
After devising an ‘ideal prescription’ and associated scoring system with the specialist pain team, the first intervention was to increase awareness and educate admitting doctors with an email memorandum. Inconsistent prescribing noted during baseline data collection suggested a lack of understanding of effective pain control. Two separate emails were sent, 1 month apart, one from the clinical lead for Orthopaedics and one from the clinical lead for pain. The impact of this intervention was measured via data collection and also discussed among the team of doctors.
The data demonstrated a brief improvement in the weeks following the emails. Subsequent to this, scores decreased towards baseline. Discussion with the team of doctors enabled us to study this intervention. Not all doctors acknowledged the email and those who did, while agreeing with the concept, admitted to ‘forgetting’ or being ‘pushed for time’ while on call.
PDSA 2
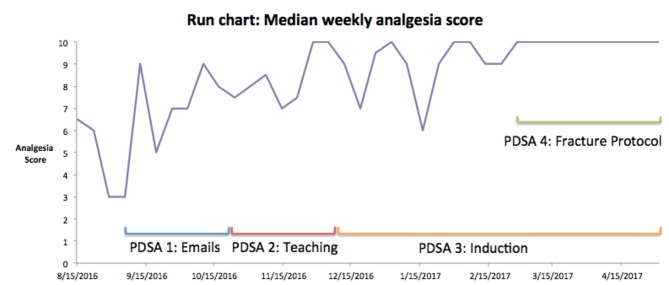
Teaching sessions were given to all doctors in the department with collaboration from the acute pain team. This intervention was designed to address all doctors, including those who had not read the emails. These sessions also allowed feedback from all prescribers regarding their opinions and difficulties in achieving the study aim. The sessions triggered an unsustained improvement in practice (see figure 2). The reasons given by the prescribers for the disappointing progress were time pressures and difficulty with the e-prescribing system.
Figure 2.
Run chart showing continuous data over the study period with timing of each ‘plan, do, study, act’ (PDSA) cycle shown.
PDSA 3
In response to the comments from the previous cohort, induction sessions were developed to show prescribers how to use the e-prescribing system efficiently and as a way to encourage new doctors in the department to form good habits with regards to admission prescribing. Median scores improved with the new cohort of doctors as they were more familiar with the e-prescribing system, but the improvements were inconsistent, with ‘time pressures’ being described as the main obstruction to change.
PDSA 4
In response to time pressures, the authors worked with the IT department to create a prescribing template for trauma patients. A template prescription based on pain consultant advice, in accordance with a 10 out of 10 score, was developed. This template included analgesia and as required medication for analgesia side effects. Within certain safety parameters, mainly regarding opiate prescription, an admitting doctor could efficiently complete an appropriate prescription. The template is adjusted for each individual patient using drop down menus and responses to key prompts. The time saved using the novel e-prescribing template was over 3 min and meant a prescription could safely be completed within seconds. This was well received by the team of prescribing doctors.
Following a further teaching session, and incorporation of the new template into the departmental inductions, analgesia scores increased to 10 and were sustained for the remaining 3 months of the study. PDSA cycles 3 and 4 overlapped as the induction for new doctors became a permanent change within the department and all new doctors experienced PDSA cycle 3 change.
Results
The improvement in median analgesia scores is illustrated in figure 2. Although scores improved with senior encouragement and teaching interventions, this did not achieve the aim of reaching a sustained 10 out of 10 weekly median score. Immediately following the first email, the weekly score increased from 3 to 9; however, this fluctuated between 5 and 9 in the weeks following. Immediately following the teaching session, the median weekly score was 10/10; however, this was not sustained.
Introducing the e-prescribing protocol was the most successful intervention and sustained the improvement in scores from the date of introduction to the end of the study period, compared with baseline. Prescribing was compared between the baseline 3 weeks (n=25) and 3 weeks post protocol introduction (n=23). Fifty-four per cent were prescribed regular step 1 analgesia initially and this increased to 96% post protocol. At baseline, 27% of patients were prescribed ‘as required’ laxatives. This increased to 91%.
We calculate a 26-hour time saving in admission clerking per annum, based on an average of 10 patient admissions per week. In order to estimate time savings, we recorded the time taken for one doctor (not an author) to prescribe a typical drug chart using the standard and protocol methods. The time saved was 3 min and 2 s.
Long-term sustainability was confirmed following further data collection, 1 year following completion of the project. During three successive weeks in June 2018, median weekly analgesia score remained 10 out of 10.
Lessons and limitations
Completing four PDSA cycles with continuous data collection enabled the authors to gain useful insight into successive interventions. Teaching alone was inadequate and despite inductions, the nature of rotating cohorts of doctors challenges sustainability. Introducing a system change that saves time and effort for doctors, rather than increasing it, was well received and highly successful. This was only achievable through engagement with clinicians and liaison with IT services. Combining the e-prescribing protocol (PDSA 4) with the induction sessions (PDSA 3) enabled increased awareness and understanding of the new system.
Baseline data showed prescribing was inconsistent and often incomplete on handwritten drug charts. The department employed rotating FY1, FY2, core-trainee doctors, and overseas trained, trust grade clinicians. No pattern of prescribing error was observed between these groups, and all clinicians identified time pressures while on call as responsible for prescribing omissions. Emails and teaching sessions did have some effect suggesting education played a role. The impact of these interventions was not sustained and the authors feel workload pressures were primarily responsible for lower scores. This was manifest by the time-saving advent of electronic prescribing showing most, and sustained effect. On reflection, a more detailed needs assessment in the planning phase of the project may have highlighted this issue earlier and reduced the number of interventions tested.
Completing this project has also highlighted the importance of stakeholder recognition and involvement. The doctor prescribers were vital to the success of this project and listening to their concerns and feedback was a vital component to studying each intervention. In addition, expertise from senior orthopaedic and pain team staff was essential for delivery of safe, and appropriate, service changes. Finally, involving the nursing and pharmacy staff in project and prescription design was important to understand the practicalities of medicine administration and the potential impact on patients.
This project is transferrable to all adult trauma settings where electronic prescribing is used. The success of this project was based on the acceptance and adaptation of e-prescribing, and while this would be possible with handwritten systems, the interventions described in this study may not be directly applicable to more traditional models of care. The use of the prescribing template does require medical understanding with regard to comorbidities such as renal impairment, cachexia and specific head and chest injuries; however, this pharmacological knowledge should be expected for entry-level doctors and can be covered during induction. There were no prescribing errors as a result of the new template and no adverse incidents were reported to the authors.
This project demonstrated sustained system-based improvements. Analgesia and side-effect medication became readily available to all trauma inpatients, but a direct assessment of patient pain levels was not undertaken.
Conclusion
Addressing initial prescribing habits of junior doctors improved accessibility to analgesia for trauma inpatients at GWH. The introduction of a novel e-prescribing protocol significantly improved analgesia prescription and resulted in sustainable improvements, long after the completion of the project, despite changing cohorts of doctors and the authors leaving the department. Working as a team with doctors, nurses and pain specialists, and liaising with IT representatives, produced a successful initiative which saved time, reduced workloads and improved care.
Acknowledgments
Many thanks to the acute pain service and IT department at the Great Western Hospital for support in completing this project.
Footnotes
Patient consent for publication: Not required.
Contributors: SS was involved in project design and planning, data collection, data analysis, intervention implementation and write-up. CH and RW were involved in data collection and intervention implementation. MD was involved in project design and planning, supervision and review of write-up. AT was involved in project supervision and review of write-up.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Doran GT. There’s a S.M.A.R.T. way to write managements’ goals and objectives. Management Review 1981;70:35–6. [Google Scholar]
- 2. American college of emergency physicians. Patient Satisfaction 2011. https://www.acep.org/patientsatisfaction/#sm.0001eiagv1aahfcfqup1lv4kyfqbn (accessed 4 Apr 2018).
- 3. Awolola AM, Campbell L, Ross A. Pain management in patients with long-bone fractures in a district hospital in KwaZulu-Natal, South Africa. Afr J Prim Health Care Fam Med 2015;7:818 10.4102/phcfm.v7i1.818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Reardon DP, Anger KE, Szumita PM. Pathophysiology, assessment, and management of pain in critically ill adults. Am J Health Syst Pharm 2015;72:1531–43. 10.2146/ajhp140541 [DOI] [PubMed] [Google Scholar]
- 5. Fine PG, Perry G, Fine MD. Long-term consequences of chronic pain: mounting evidence for pain as a neurological disease and parallels with other chronic disease states. Pain Med 2011;12:996–1004. 10.1111/j.1526-4637.2011.01187.x [DOI] [PubMed] [Google Scholar]
- 6. Polomano RC, Fillman M, Giordano NA, et al. . Multimodal analgesia for acute postoperative and trauma-related pain. Am J Nurs 2017;117:S12–S26. 10.1097/01.NAJ.0000513527.71934.73 [DOI] [PubMed] [Google Scholar]
- 7. Oyler D, Bernard AC, VanHoose JD, et al. . Minimizing opioid use after acute major trauma. Am J Health Syst Pharm 2018;75:105–10. 10.2146/ajhp161021 [DOI] [PubMed] [Google Scholar]
- 8. Patil A, Srinivasarangan M, Ravindra P, et al. . Studying protocol-based pain management in the emergency department. J Emerg Trauma Shock 2017;10:180–8. 10.4103/JETS.JETS_83_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ossendorp R, Forouzanfar T, Ashton-James CE, et al. . Protocols for treating the postoperative pain of fractures in Dutch hospitals. J Pain Res 2013;6:635–9. 10.2147/JPR.S43729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Macintyre E, Stephan A, Schug A. Acute pain management: a practical guide. 4th Edition 2014. [Google Scholar]
- 11. Carrie C, Stecken L, Cayrol E. Bundle of care for blunt chest trauma patients improves analgesia but increases rates of intensive care unit admission: a retrospective case–control study Anaesth Crit Care Pain Med. 2018;37:211–5. [DOI] [PubMed] [Google Scholar]
- 12. Miller E. The World Health Organization analgesic ladder. J Midwifery Womens Health 2004;49:542–5. 10.1016/j.jmwh.2004.08.021 [DOI] [PubMed] [Google Scholar]
- 13. Wardhan R, Chelly J. Recent advances in acute pain management: understanding the mechanisms of acute pain, the prescription of opioids, and the role of multimodal pain therapy. F1000Res 2017;6:6 10.12688/f1000research.12286.1 [DOI] [PMC free article] [PubMed] [Google Scholar]