Abstract
Objective:
A small body of work has started developing cannabis use “typologies” for use in treatment and prevention. Two potentially relevant dimensions for classifying cannabis use typologies are medical versus recreational cannabis use and the co-use of cannabis and alcohol. Here we compare alcohol use and related problems between cannabis users with and without medical cannabis recommendations.
Method:
Data come from a larger general population study in Washington State conducted between January 2014 and October 2016. All participants in the analytic sample (n = 991) reported using both alcohol and cannabis in the past 12 months. The primary exposure was having a medical recommendation for cannabis. Outcomes were past-30-day drinking (drinks/day, frequency of 5+ drinks, and maximum number of drinks in a day) and past-12-month Alcohol Use Disorders Identification Test (AUDIT) scores.
Results:
Compared with those without medical cannabis recommendations, cannabis users with medical cannabis recommendations had 0.59 times fewer drinks/day, 0.44 times fewer occasions drinking 5+, and 0.78 times the average maximum number of drinks in one day (all ps < .05). Those with a recommendation also had 0.87 times lower AUDIT total scores (p < .05) and 0.57 times lower AUDIT problem scores (p < .01).
Conclusions:
Cannabis users with medical cannabis recommendations drink less and have fewer alcoholrelated problems than those without recommendations, even after adjusting for health status. Future studies should examine nonhealth reasons regarding how medical and nonmedical users use cannabis differently.
The liberalization of recreational and medical cannabis laws has inherently increased the prevalence of legal cannabis use. In light of these movements, a small body of work has started developing cannabis use “typologies” to classify cannabis users into distinct groups and assess differential risks for use in prevention and intervention strategies. For example, a cluster analysis of cannabis users recruited from Dutch coffee shops distinguished three groups: “strongest high,” “consistent high,” and “steady quantity.” These groups were characterized by different ages at onset, monthly frequencies, motivations for use, and differential risks of problems, with the “strongest high” group having the highest risk (Korf et al., 2007). Similarly, latent class analyses of the Canadian Addiction Survey (N = 1,003) showed four distinct classes based on use patterns (Fischer et al., 2010). Again, classes were mainly distinguished by age at onset and frequency of cannabis use. In this study, the class featuring earliest onset and highest frequency of use (onset at or under age 15, daily or near-daily use; 22% of the sample) had substantially higher rates of harms, including other illicit drug use, physical and mental health problems, cannabis use and driving, and cannabis use problems (Fischer et al., 2010). Half of the highest frequency class also reported medical cannabis use. Interestingly, the prevalence of alcohol use was high in all classes, with no significant differences between classes.
The distinction between medical and nonmedical “recreational” cannabis use and the co-use of cannabis and alcohol are two additional dimensions of cannabis use relevant for classifying cannabis use typologies and assessing differential risks. An internet survey of cannabis users showed that while the degree of overlap between medical and recreational cannabis users was high (86%), medical users reported higher quantities consumed and money spent per month (Pacula et al., 2016). Medical users were also more likely to vaporize and to consume edibles than recreational users (Pacula et al., 2016). In this sample, 20% of recreational users and 3% of medical users reported using cannabis and alcohol simultaneously. Studies have shown that individuals who use both cannabis and alcohol form heterogeneous groups that experience different likelihoods of consequences relative to their co-use patterns (Subbaraman & Kerr, 2015). Furthermore, the simultaneous use of cannabis and alcohol in one occasion has been shown to be the most detrimental co-use pattern, with increased odds of alcohol-related problems compared to the separate use of alcohol and cannabis shown in both laboratory and epidemiologic studies (Midanik et al., 2007; Ronen et al., 2010; Subbaraman & Kerr, 2015).
Still, few studies have compared alcohol use and related problems between medical and recreational cannabis users, which may be important for informing strategies to prevent alcohol-related problems. Several studies have shown that medical cannabis users substitute cannabis for alcohol, thus reducing both alcohol use and related problems (Lucas & Walsh, 2017; Lucas et al., 2013; Reiman, 2009; Subbaraman, 2014); however, these studies are limited to medical users without recreational cannabis comparison groups, and consequently suffer from selection bias. Among studies that directly compare medical to recreational cannabis users, a study of primary care patients found that medical cannabis users have significantly fewer problems with alcohol and lower alcohol and drug problem severity but significantly more health problems (e.g., pain, reduced mobility, disability status) than recreational users (Roy-Byrne et al., 2015). Medical users also had significantly higher frequency of cannabis use in the past 30 days but were less likely to combine cannabis and alcohol than recreational users (Roy-Byrne et al., 2015). Similarly, in the internet sample of cannabis users, individuals who reported using cannabis solely for recreation were significantly more likely to use cannabis simultaneously with alcohol than those who only use cannabis for medical purposes (Pacula et al., 2016). Thus, if recreational cannabis users are more likely to use cannabis simultaneously with alcohol, then recreational users probably have more alcoholrelated problems than medical cannabis users; however, no study to date has compared alcohol-related problems between medical and recreational cannabis users. Furthermore, studies that show substitution of cannabis for alcohol and thus fewer alcohol-related problems among medical cannabis patients may be biased by health status because poorer health could lead to both obtaining a medical cannabis recommendation and decreased alcohol consumption (e.g., people with serious health conditions might be medically advised to stop drinking).
Rationale for current study
Although the evidence suggests that cannabis users with medical cannabis recommendations use less alcohol than cannabis users without medical cannabis recommendations, prior studies have not (a) examined differences in alcoholrelated problems between those with and without medical cannabis recommendations or (b) adjusted for health status, a potential confounder that is known to be related to both having a medical cannabis recommendation and alcohol use. The primary aim of this study is to compare alcohol use and related problems between cannabis users with and without medical cannabis recommendations while accounting for health status.
Method
Data
Data come from a larger general population study evaluating the policy changes of spirits privatization and cannabis legalization in Washington State (N = 5,492). List-assisted dual-frame random digit dial procedures were used for recruitment, with more than 40% from cell phones. All participants were Washington residents age 18 and older at the time of data collection. Data were collected in six separate cross-sectional samples across six time points (every 6 months) between January 2014 and October 2016. The American Association for Public Opinion Research cooperation rates were 50.8% (landline) and 59.5% (cell phone) for T1 (n = 1,202); 45.8% (landline) and 62.4% (cell) for T2 (n = 804); 43.7% (landline) and 61.5% (cell) for T3 (n = 823); 41.7% (landline) and 59.6% (cell) for T4 (n = 823); 49.4% (landline) and 60.9% (cell) for T5 (n = 610); and 45.3% (landline) and 63.0% (cell) for T6 (n = 1,391); the American Association for Public Opinion Research (2000) has detailed formulas for cooperation rates that can be found on its website (www.aapor.org). Our analytic subsample consists of the 991 participants who reported using both cannabis and alcohol in the past 12 months. The Public Health Institute’s institutional review board approved this study, and informed consent was obtained from all participants.
Measures
Our primary independent variable was derived from the question, “Do you have a medical recommendation from a health care professional for marijuana or cannabis?” Drinking outcomes were past-30-day average number of drinks/ day (open ended, range: 0–70), past-30-day frequency of five or more drinks (open ended, range: 0–30), and past-30-day maximum number of drinks in one day (open ended, range: 0–48). In terms of alcohol-related problem outcomes, we used both the total Alcohol Use Disorders Identification Test (AUDIT) and AUDIT problem subscale. The 10-item total AUDIT is scored out of 40 points, with a cutoff of 8 indicating hazardous or harmful alcohol use; it has 92% sensitivity and 94% specificity for patients with heavy drinking patterns and/or active AUD (Saunders et al., 1993). The AUDIT problem subscale is the score for the seven AUDIT problem items (e.g., needing a morning drink, feeling guilt or remorse after drinking, blacking out), and ranges from 0 to 28. The AUDIT has shown strong validity and reliability in more than 45 studies of diverse health and community settings (De Meneses-Gaya et al., 2009).
Covariates
Multivariable regressions adjusted for health status based on the question, “Would you say your health in general is excellent, very good, good, fair, or poor?” and for simultaneous versus concurrent use based on the question, “[In the past 12 months] how often did you use alcohol and marijuana at the same time? Was it usually, sometimes, or never?” Participants were classified as concurrent users if they never used cannabis and alcohol together or as simultaneous users if they usually/sometimes used cannabis and alcohol together. Covariates also included past-12-month cannabis use frequency (less than monthly, monthly, more than monthly but less than weekly, weekly, daily/almost daily); age (18–29, 30–49, ≥50); race/ethnicity (African American, Hispanic, other, White); education (less than high school, high school diploma or more); employment (full/part-time employed, unemployed); and relationship status (married/ cohabiting, not married/cohabiting). Although we analyzed drinking variables as outcomes (past-30-day average number of drinks/day, past-30-day frequency of five or more drinks, and past-30-day maximum number of drinks in one day), these three variables were also included as covariates in the multivariable regressions on AUDIT scores.
Statistical analyses
First, bivariate t tests and chi-squared tests were used to examine differences between those with medical recommendations for cannabis and those without. Next, multivariable negative binomial regressions were used to model past-30day drinking outcomes and past-12-month AUDIT scores; negative binomial regressions were used because the dependent variables are all counts with distributions in which the variances are greater than the means (i.e., overdispersed). All analyses adjusted for probability of selection due to the sampling design through survey weights and were performed in Stata Version 14.2 (StataCorp LP, College Station, TX). Sampling weights accounted for differential probability of response between landline and cell phone samples, and incorporated post-stratification weights for age, gender, race/ ethnicity, and educational attainment based on the Washington 2010 Census.
Results
Bivariate results
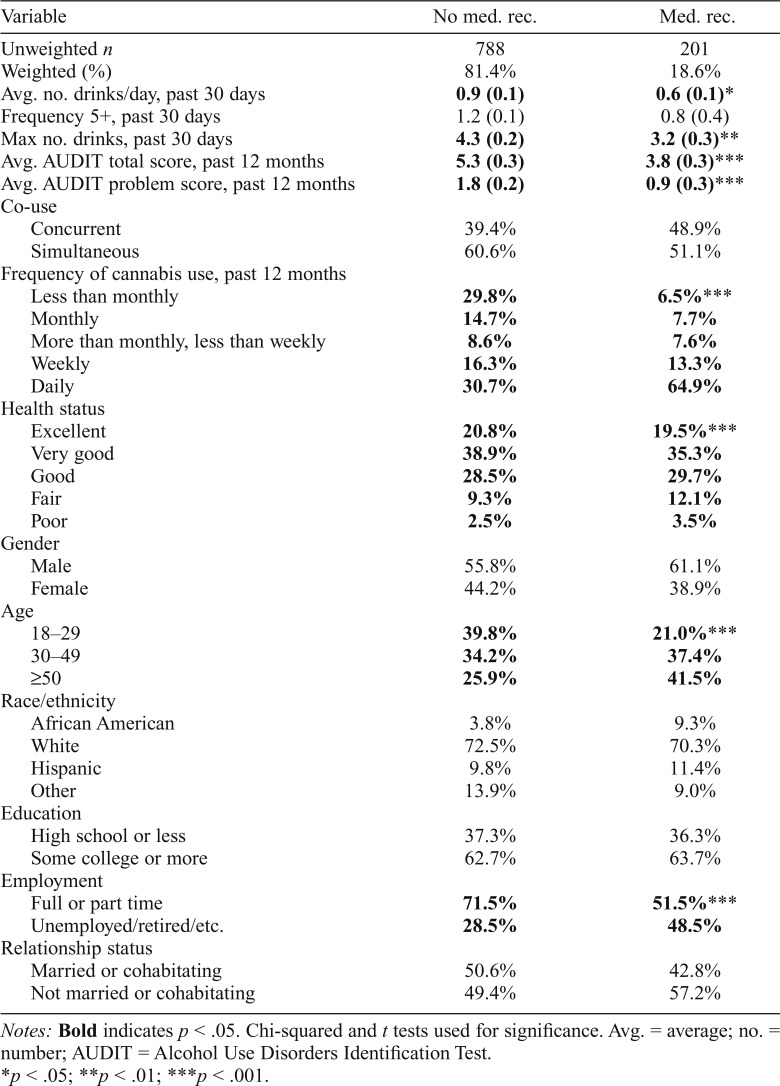
As shown in Table 1, those with medical cannabis recommendations were more often older; not employed full or part time; and with fewer drinks/day, lower maximum number of drinks, and lower AUDIT total and problem subscale scores compared with those without medical cannabis recommendations. Those with medical cannabis recommendations were also more likely to be in fair or poor health and more likely to use cannabis daily than those without medical cannabis recommendations.
Table 1.
Comparisons of demographics, substance use between those without versus with medical recommendation among co-users (n = 991)
| Variable | No med. rec. | Med. rec. |
| Unweighted n | 788 | 201 |
| Weighted (%) | 81.4% | 18.6% |
| Avg. no. drinks/day, past 30 days | 0.9 (0.1) | 0.6 (0.1)* |
| Frequency 5+, past 30 days | 1.2 (0.1) | 0.8 (0.4) |
| Max no. drinks, past 30 days | 4.3 (0.2) | 3.2 (0.3)** |
| Avg. AUDIT total score, past 12 months | 5.3 (0.3) | 3.8 (0.3)*** |
| Avg. AUDIT problem score, past 12 months | 1.8 (0.2) | 0.9 (0.3)*** |
| Co-use | ||
| Concurrent | 39.4% | 48.9% |
| Simultaneous | 60.6% | 51.1% |
| Frequency of cannabis use, past 12 months | ||
| Less than monthly | 29.8% | 6.5%*** |
| Monthly | 14.7% | 7.7% |
| More than monthly, less than weekly | 8.6% | 7.6% |
| Weekly | 16.3% | 13.3% |
| Daily | 30.7% | 64.9% |
| Health status | ||
| Excellent | 20.8% | 19.5%*** |
| Very good | 38.9% | 35.3% |
| Good | 28.5% | 29.7% |
| Fair | 9.3% | 12.1% |
| Poor | 2.5% | 3.5% |
| Gender | ||
| Male | 55.8% | 61.1% |
| Female | 44.2% | 38.9% |
| Age | ||
| 18–29 | 39.8% | 21.0%*** |
| 30–49 | 34.2% | 37.4% |
| ≥50 | 25.9% | 41.5% |
| Race/ethnicity | ||
| African American | 3.8% | 9.3% |
| White | 72.5% | 70.3% |
| Hispanic | 9.8% | 11.4% |
| Other | 13.9% | 9.0% |
| Education | ||
| High school or less | 37.3% | 36.3% |
| Some college or more | 62.7% | 63.7% |
| Employment | ||
| Full or part time | 71.5% | 51.5%*** |
| Unemployed/retired/etc. | 28.5% | 48.5% |
| Relationship status | ||
| Married or cohabitating | 50.6% | 42.8% |
| Not married or cohabitating | 49.4% | 57.2% |
Notes: Bold indicates p < .05. Chi-squared and t tests used for significance. Avg. = average; no. = number; AUDIT = Alcohol Use Disorders Identification Test.
p < .05;
p < .01;
p < .001.
Multivariable regression results: Drinking outcomes
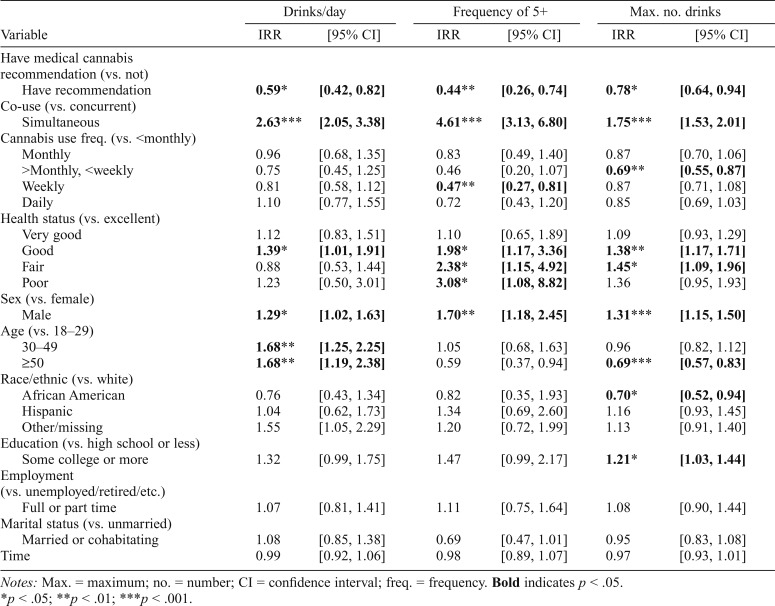
Table 2 displays results from negative binomial regressions on past-30-day drinking outcomes; the incidence rate ratio (IRR) is interpreted as the factor by which the dependent variable changes for a unit change in the independent variable. First, those with medical cannabis recommendations had 0.59 times fewer drinks/day (p < .05), 0.44 times fewer occasions drinking 5+ drinks (p < .01), and 0.78 times as many maximum number of drinks (p < .01) in the past 30 days compared with those without medical cannabis recommendations. Simultaneous users had 2.63 times more drinks/ day (p < .001), 4.61 times more 5+ occasions (p < .001), and 1.75 times higher maximum drinks number of drinks (p < .001) in the past 30 days compared with concurrent users. Cannabis use frequency generally was not related to alcohol use, although compared with less than monthly cannabis users, the more than monthly/less than weekly users did have a lower maximum number of drinks (IRR = 0.69, p < .01) and weekly users had a lower frequency of 5+ drink occasions (IRR = 0.47, p < .01).
Table 2.
Adjusted incidence rate ratios (IRRs) between medical cannabis use and drinking outcomes (n = 991)
| Drinks/day |
Frequency of 5+ |
Max. no. drinks |
||||
| Variable | IRR | [95% CI] | IRR | [95% CI] | IRR | [95% CI] |
| Have medical cannabis recommendation (vs. not) | ||||||
| Have recommendation | 0.59* | [0.42, 0.82] | 0.44** | [0.26, 0.74] | 0.78* | [0.64, 0.94] |
| Co-use (vs. concurrent) | ||||||
| Simultaneous | 2.63*** | [2.05, 3.38] | 4.61*** | [3.13, 6.80] | 1.75*** | [1.53, 2.01] |
| Cannabis use freq. (vs. <monthly) | ||||||
| Monthly | 0.96 | [0.68, 1.35] | 0.83 | [0.49, 1.40] | 0.87 | [0.70, 1.06] |
| >Monthly, <weekly | 0.75 | [0.45, 1.25] | 0.46 | [0.20, 1.07] | 0.69** | [0.55, 0.87] |
| Weekly | 0.81 | [0.58, 1.12] | 0.47** | [0.27, 0.81] | 0.87 | [0.71, 1.08] |
| Daily | 1.10 | [0.77, 1.55] | 0.72 | [0.43, 1.20] | 0.85 | [0.69, 1.03] |
| Health status (vs. excellent) | ||||||
| Very good | 1.12 | [0.83, 1.51] | 1.10 | [0.65, 1.89] | 1.09 | [0.93, 1.29] |
| Good | 1.39* | [1.01, 1.91] | 1.98* | [1.17, 3.36] | 1.38** | [1.17, 1.71] |
| Fair | 0.88 | [0.53, 1.44] | 2.38* | [1.15, 4.92] | 1.45* | [1.09, 1.96] |
| Poor | 1.23 | [0.50, 3.01] | 3.08* | [1.08, 8.82] | 1.36 | [0.95, 1.93] |
| Sex (vs. female) | ||||||
| Male | 1.29* | [1.02, 1.63] | 1.70** | [1.18, 2.45] | 1.31*** | [1.15, 1.50] |
| Age (vs. 18–29) | ||||||
| 30–49 | 1.68** | [1.25, 2.25] | 1.05 | [0.68, 1.63] | 0.96 | [0.82, 1.12] |
| ≥50 | 1.68** | [1.19, 2.38] | 0.59 | [0.37, 0.94] | 0.69*** | [0.57, 0.83] |
| Race/ethnic (vs. white) | ||||||
| African American | 0.76 | [0.43, 1.34] | 0.82 | [0.35, 1.93] | 0.70* | [0.52, 0.94] |
| Hispanic | 1.04 | [0.62, 1.73] | 1.34 | [0.69, 2.60] | 1.16 | [0.93, 1.45] |
| Other/missing | 1.55 | [1.05, 2.29] | 1.20 | [0.72, 1.99] | 1.13 | [0.91, 1.40] |
| Education (vs. high school or less) | ||||||
| Some college or more | 1.32 | [0.99, 1.75] | 1.47 | [0.99, 2.17] | 1.21* | [1.03, 1.44] |
| Employment (vs. unemployed/retired/etc.) | ||||||
| Full or part time | 1.07 | [0.81, 1.41] | 1.11 | [0.75, 1.64] | 1.08 | [0.90, 1.44] |
| Marital status (vs. unmarried) | ||||||
| Married or cohabitating | 1.08 | [0.85, 1.38] | 0.69 | [0.47, 1.01] | 0.95 | [0.83, 1.08] |
| Time | 0.99 | [0.92, 1.06] | 0.98 | [0.89, 1.07] | 0.97 | [0.93, 1.01] |
Notes: Max. = maximum; no. = number; CI = confidence interval; freq. = frequency. Bold indicates p < .05.
p < .05;
p < .01;
p < .001.
Compared with those reporting excellent health, those reporting good health drank 1.39 more drinks/day (p < .05), had 1.98 times more 5+ occasions (p < .01), and had 1.38 times more maximum number of drinks (p < .01); those reporting fair health had 2.38 times more 5+ occasions (p < .05) and 1.45 times more maximum number of drinks (p < .05); and those reporting poor health had 3.08 times as many 5+ occasions (p < .05). Men drank more drinks/day, binged more often, and had a higher maximum number of drinks in the past 30 days compared with women. Those ages 50 and older had a lower maximum number of drinks compared with those ages 18–29, as did African Americans compared with Whites.
Multivariable regression results: Alcohol-related problem outcomes
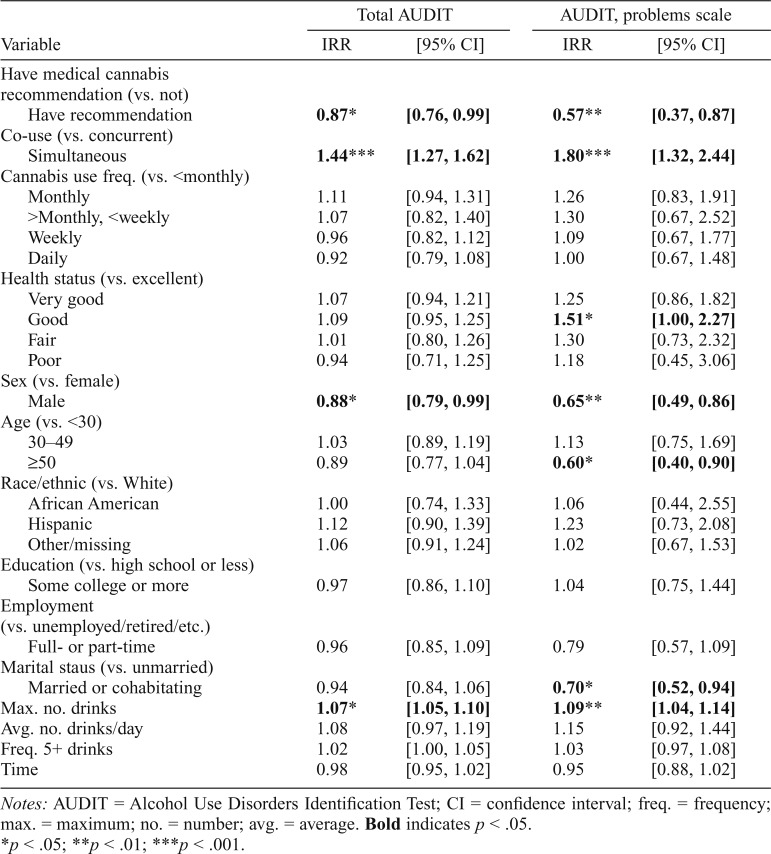
Table 3 shows results from negative binomial regressions on past-12-month AUDIT scores. Those with medical cannabis recommendations had significantly lower total AUDIT (IRR = 0.87, p < .05) and AUDIT problem scale (IRR = 0.57, p < .01) scores compared with those without medical cannabis recommendations. Compared with concurrent use, simultaneous use was related to 1.44 times higher total AUDIT scores and 1.80 times higher AUDIT problem scale scores (ps < .001). Neither cannabis use frequency nor health status was significantly related to total AUDIT scores.
Table 3.
Adjusted incidence rate ratios (IRRs) between medical cannabis use and alcohol-related problems (n = 991)
| Total AUDIT |
AUDIT, problems scale |
|||
| Variable | IRR | [95% CI] | IRR | [95% CI] |
| Have medical cannabis recommendation (vs. not) | ||||
| Have recommendation | 0.87* | [0.76, 0.99] | 0.57** | [0.37, 0.87] |
| Co-use (vs. concurrent) | ||||
| Simultaneous | 1.44*** | [1.27, 1.62] | 1.80*** | [1.32, 2.44] |
| Cannabis use freq. (vs. <monthly) | ||||
| Monthly | 1.11 | [0.94, 1.31] | 1.26 | [0.83, 1.91] |
| >Monthly, <weekly | 1.07 | [0.82, 1.40] | 1.30 | [0.67, 2.52] |
| Weekly | 0.96 | [0.82, 1.12] | 1.09 | [0.67, 1.77] |
| Daily | 0.92 | [0.79, 1.08] | 1.00 | [0.67, 1.48] |
| Health status (vs. excellent) | ||||
| Very good | 1.07 | [0.94, 1.21] | 1.25 | [0.86, 1.82] |
| Good | 1.09 | [0.95, 1.25] | 1.51* | [1.00, 2.27] |
| Fair | 1.01 | [0.80, 1.26] | 1.30 | [0.73, 2.32] |
| Poor | 0.94 | [0.71, 1.25] | 1.18 | [0.45, 3.06] |
| Sex (vs. female) | ||||
| Male | 0.88* | [0.79, 0.99] | 0.65** | [0.49, 0.86] |
| Age (vs. <30) | ||||
| 30–49 | 1.03 | [0.89, 1.19] | 1.13 | [0.75, 1.69] |
| ≥50 | 0.89 | [0.77, 1.04] | 0.60* | [0.40, 0.90] |
| Race/ethnic (vs. White) | ||||
| African American | 1.00 | [0.74, 1.33] | 1.06 | [0.44, 2.55] |
| Hispanic | 1.12 | [0.90, 1.39] | 1.23 | [0.73, 2.08] |
| Other/missing | 1.06 | [0.91, 1.24] | 1.02 | [0.67, 1.53] |
| Education (vs. high school or less) | ||||
| Some college or more | 0.97 | [0.86, 1.10] | 1.04 | [0.75, 1.44] |
| Employment (vs. unemployed/retired/etc.) | ||||
| Full- or part-time | 0.96 | [0.85, 1.09] | 0.79 | [0.57, 1.09] |
| Marital staus (vs. unmarried) | ||||
| Married or cohabitating | 0.94 | [0.84, 1.06] | 0.70* | [0.52, 0.94] |
| Max. no. drinks | 1.07* | [1.05, 1.10] | 1.09** | [1.04, 1.14] |
| Avg. no. drinks/day | 1.08 | [0.97, 1.19] | 1.15 | [0.92, 1.44] |
| Freq. 5+ drinks | 1.02 | [1.00, 1.05] | 1.03 | [0.97, 1.08] |
| Time | 0.98 | [0.95, 1.02] | 0.95 | [0.88, 1.02] |
Notes: AUDIT = Alcohol Use Disorders Identification Test; CI = confidence interval; freq. = frequency; max. = maximum; no. = number; avg. = average. Bold indicates p < .05.
p < .05;
p < .01;
p < .001.
Men had significantly lower total AUDIT and AUDIT problem scale scores compared with women. Those age 50 and older had significantly lower AUDIT problem scores compared with those ages 18–29, those married/cohabiting had significantly lower AUDIT problem scores than those not married/cohabiting, and increasing maximum number of drinks was significantly related to increased AUDIT scores.
Discussion
Summary of results
In a general population sample of alcohol and cannabis users from the state of Washington, we find that those with medical cannabis recommendations drank less and had lower AUDIT total and AUDIT problem scores compared with those without medical cannabis recommendations. The lesser amounts of alcohol consumed and lower frequency of binge drinking is in line with what studies of medical cannabis users have found in the past (Lucas et al., 2013; Reiman, 2009); however, we hesitate to make conclusions about substitution without longitudinal data. Those with medical cannabis recommendations also had lower AUDIT problem scores than those without medication cannabis recommendations, which may be attributable to their lesser drinking. Those with medical cannabis recommendations may have different motives for substance use, i.e., they are using cannabis as medicine and not for intoxication. Medical users may also have higher tolerance to cannabis because of their increased frequency of cannabis use; however, having a medical cannabis recommendation was still significantly associated with lower AUDIT problem scores even after adjusting for cannabis use frequency, suggesting an association beyond tolerance. We also found that compared with those reporting excellent health, those reporting good, fair, or poor health all had significantly more 5+ occasions; this pattern conflicts with the “sick quitter” hypothesis that people reduce or even completely stop drinking as they age and become unwell (Fillmore et al., 2006, 2007). However, only those reporting good health drank significantly more drinks per day, had a higher maximum number of drinks, and had higher AUDIT scores than those reporting excellent health. We speculate that the lack of significant differences in these latter outcomes between those reporting fair or poor versus excellent health is attributable to small cell sizes, whereas the lack of significant differences between those reporting very good versus excellent health reflects generally similar drinking patterns between the two groups.
The distinction between medical and nonmedical, or “recreational,” cannabis use is a gray area, and a single individual could use cannabis for a variety of both health- and non–health-related reasons (Pacula et al., 2016). Of note, data come from Washington, a state that has had legalized cannabis use for adults 21 or older throughout our entire study duration, although retail stores only opened after we began data collection. Still, the legal environment means that having a medical recommendation to obtain cannabis legally was not necessary, even if the motivation for use is medical. This further supports that those with medical cannabis recommendations may be intrinsically different from those without, regardless of health status, which is a finding that merits further research. As of November 2017, adults 18 and older can obtain “medical marijuana authorization” from a licensed healthcare practitioner in Washington for conditions severe enough to hinder daily life activities and functions that can also be objectively assessed. These conditions include cancer, intractable pain, glaucoma, traumatic brain injury, and a range of others. Mental health conditions do not qualify. Advantages to having authorization include not having to pay sales or use taxes, being able to purchase three times the retail limit, and possession of plants, which currently remains illegal for recreational users; these are all possible motivations for continuing to obtain medical authorization in a legal cannabis environment. However, none of these reasons explain why medical cannabis users use less alcohol and have fewer alcohol-related problems than nonusers, which warrants future research.
We also found that compared with concurrent or separate use of alcohol and cannabis, simultaneous use is associated with significantly more drinking, as well as significantly higher AUDIT total and AUDIT problem scores. These results corroborate what has been found in prior general population studies (Midanik et al., 2007; Subbaraman & Kerr, 2015), as well as laboratory studies showing that combined use of alcohol and cannabis leads to greater impairment than the use of each substance alone (Downey et al., 2013; Ramaekers et al., 2000, 2001; Ronen et al., 2010). Future research regarding cannabis and alcohol co-use should continue to account for whether individuals use the two substances concurrently or simultaneously.
Taken together, the set of results demonstrates how various dimensions of cannabis use (i.e., medical use, couse with alcohol) are associated with alcohol use and related problems, and could be important dimensions of cannabis use typologies. Some have argued that a typology of cannabis users may be more objective and neutral than the concepts of abuse, dependency, and substance use disorder because typologies can account for life centrality and use intensity (Korf et al., 2007). For example, this may be relevant for high frequency “steady quantity” users because these are users with long cannabis careers that may fit the profile for dependence even though their use is not particularly problematic and they have little reason to quit (Korf et al., 2007). Similarly, we found that the medical use of cannabis is associated with high frequency of cannabis use (that could be seen as problematic or even dependent) but lower risks of alcohol-related problems. Still, how the dimensions of medical cannabis use and the co-use of cannabis and alcohol would augment existing typologies remains to be seen and merits further research. Creating a cannabis user typology that integrates all of these variables could be immensely useful in both prevention and clinical settings.
Our findings may have other public health implications as well. For example, whether cannabis can be used therapeutically to help mitigate alcohol-related problems, especially among those with alcohol use disorder, remains a hot topic (Subbaraman, 2014). A review of studies regarding the effects of cannabinoids on alcohol consumption found that cannabinoid antagonists can alleviate alcohol withdrawal symptoms and lead to a significant reduction in alcohol use (Kleczkowska et al., 2016). Furthermore, a number of studies have found that medical cannabis users can substitute cannabis for alcohol successfully and reduce both alcohol use and related problems (Lucas & Walsh, 2017; Lucas et al., 2013; Reiman, 2009; Subbaraman, 2014). Although the current data are not suited for testing substitution hypotheses directly, the findings support that in the general population, medical cannabis users drink less than recreational users for reasons beyond health status. Therefore, if motivations for cannabis use are medical rather than recreational, cannabis potentially could be used to improve alcohol-related problems. In terms of clinical implications, alcohol treatment programs might reconsider the zero-tolerance practice of expelling patients who test positive for any drug, or specifically for cannabis. The findings also indicate that cannabis users should be treated as a heterogeneous group for research purposes. For example, the motivations or circumstances for medical versus recreational cannabis use could be an important confounder or mediating factor for future research to consider.
Limitations
Those without medical cannabis recommendations may still be using cannabis for medical reasons; however, reclassifying these individuals as medical users would likely strengthen the current findings. Future studies should ask more detailed questions regarding medical cannabis use, as well as motivations for use. Although simultaneous use was related to increased risks, it may not be solely responsible for increased alcohol use and related problems, and may act as an indicator of other characteristics associated with increased use such as risk taking or impulsivity. Data were collected cross-sectionally and may be affected by reporting biases, such as the social acceptability of cannabis use and/ or alcohol-related problems, or by changes in the characteristics of nonresponse. Furthermore, data regarding nonresponders were not available, and it is possible that there are clinically important subpopulations not represented in the study population (e.g., those with severe alcohol problems and dependence). Last, Washington’s population may have characteristics that limit generalizability to other states and countries.
Conclusions and future directions
Those with medical cannabis recommendations had fewer problems than those without medical cannabis recommendations, even after accounting for quantity and frequency of alcohol use, and health status. On the other hand, simultaneous users were at higher odds of a wide variety of problems. These findings have direct public health and clinical implications; for example, alcohol treatment programs might reconsider zero-tolerance policies that expel patients for testing positive for cannabis, and individuals who use both alcohol and cannabis should avoid using them at the same time in order to minimize risk. Detailed, longitudinal studies regarding contexts, motivations, and patterns of co-use are needed to better understand why medical cannabis appears protective for alcohol problems, even at high levels of cannabis use.
Footnotes
This research was supported by National Institute on Alcohol Abuse and Alcoholism Grant R01 AA021742. The authors have no conflicts of interest, financial or otherwise, to declare.
References
- American Association for Public Opinion Research. Standard definitions. Final dispositions of case codes and outcome rates for surveys 2000 [Google Scholar]
- De Meneses-Gaya C., Zuardi A. W., Loureiro S. R., Crippa J. A. S. Alcohol Use Disorders Identification Test (AUDIT): An updated systematic review of psychometric properties. Psychology & Neuroscience. 2009;2:83–97. doi:10.3922/j.psns.2009.1.12. [Google Scholar]
- Downey L. A., King R., Papafotiou K., Swann P., Ogden E., Boorman M., Stough C. The effects of cannabis and alcohol on simulated driving: Influences of dose and experience. Accident Analysis and Prevention. 2013;50:879–886. doi: 10.1016/j.aap.2012.07.016. doi:10.1016/j.aap.2012.07.016. [DOI] [PubMed] [Google Scholar]
- Fillmore K. M., Kerr W. C., Stockwell T., Chikritzhs T., Bostrom A. Moderate alcohol use and reduced mortality risk: Systematic error in prospective studies. Addiction Research and Theory. 2006;14:101–132. doi: 10.1016/j.annepidem.2007.01.005. doi:10.1080/16066350500497983. [DOI] [PubMed] [Google Scholar]
- Fillmore K. M., Stockwell T., Chikritzhs T., Bostrom A., Kerr W. Moderate alcohol use and reduced mortality risk: Systematic error in prospective studies and new hypotheses. Annals of Epidemiology. 2007:S16–S23. doi: 10.1016/j.annepidem.2007.01.005. doi:10.1016/j.annepidem.2007.01.005. [DOI] [PubMed] [Google Scholar]
- Fischer B., Rehm J., Irving H., Ialomiteanu A., Fallu J.-S., Patra J. Typologies of cannabis users and associated characteristics relevant for public health: A latent class analysis of data from a nationally representative Canadian adult survey. International Journal of Methods in Psychiatric Research. 2010;19:110–124. doi: 10.1002/mpr.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleczkowska P., Smaga I., Filip M., Bujalska-Zadrozny M. Cannabinoid ligands and alcohol addiction: A promising therapeutic tool or a humbug? Neurotoxicity Research. 2016;29:173–196. doi: 10.1007/s12640-015-9555-7. doi:10.1007/ s12640-015-9555-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korf D. J., Benschop A., Wouters M. Differential responses to cannabis potency: A typology of users based on self-reported consumption behaviour. International Journal on Drug Policy. 2007;18:168–176. doi: 10.1016/j.drugpo.2006.08.002. doi:10.1016/j.drugpo.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Lucas P., Reiman A., Earleywine M., McGowan S. K., Oleson M., Coward M. P., Thomas B. Cannabis as a substitute for alcohol and other drugs: A dispensary-based survey of substitution effect in Canadian medical cannabis patients. Addiction Research and Theory. 2013;21:435–442. doi:10.3109/16066359.2012.733465. [Google Scholar]
- Lucas P., Walsh Z. Medical cannabis access, use, and substitution for prescription opioids and other substances: A survey of authorized medical cannabis patients. International Journal on Drug Policy. 2017;42:30–35. doi: 10.1016/j.drugpo.2017.01.011. doi:10.1016/j.drugpo.2017.01.011. [DOI] [PubMed] [Google Scholar]
- Midanik L. T., Tam T. W., Weisner C. Concurrent and simultaneous drug and alcohol use: Results of the 2000 National Alcohol Survey. Drug and Alcohol Dependence. 2007;90:72–80. doi: 10.1016/j.drugalcdep.2007.02.024. doi:10.1016/j. drugalcdep.2007.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula R. L., Jacobson M., Maksabedian E. J. In the weeds: A baseline view of cannabis use among legalizing states and their neighbours. Addiction. 2016;111:973–980. doi: 10.1111/add.13282. doi:10.1111/add.13282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaekers J. G., Robbe H. W. J., O’Hanlon J. F. Marijuana, alcohol and actual driving performance. Human Psychopharmacology. 2000;15:551–558. doi: 10.1002/1099-1077(200010)15:7<551::AID-HUP236>3.0.CO;2-P. doi:10.1002/1099-1077(200010)15:7 <551::AID-HUP236>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- Ramaekers J. G., Theunissen E. L., de Brouwer M., Toennes S. W., Moeller M. R., Kauert G. Tolerance and cross-tolerance to neurocognitive effects of THC and alcohol in heavy cannabis users. Psychopharmacology. 2011;214:391–401. doi: 10.1007/s00213-010-2042-1. doi:10.1007/s00213-010-2042-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiman A. Cannabis as a substitute for alcohol and other drugs. Harm Reduction Journal. 2009;6:35. doi: 10.1186/1477-7517-6-35. doi:10.1186/1477-7517-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronen A., Chassidim H. S., Gershon P., Parmet Y., Rabinovich A., Bar-Hamburger R., Shinar D. The effect of alcohol, THC and their combination on perceived effects, willingness to drive and performance of driving and non-driving tasks. Accident Analysis and Prevention. 2010;42:1855–1865. doi: 10.1016/j.aap.2010.05.006. doi:10.1016/j.aap.2010.05.006. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne P., Maynard C., Bumgardner K., Krupski A., Dunn C., West I. I., Ries R. Are medical marijuana users different from recreational users? The view from primary care. American Journal on Addictions. 2015;24:599–606. doi: 10.1111/ajad.12270. doi:10.1111/ajad.12270. [DOI] [PubMed] [Google Scholar]
- Saunders J. B., Aasland O. G., Babor T. F., De La Fuente J. R., Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. doi:10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Subbaraman M. S. Can cannabis be considered a substitute medication for alcohol? Alcohol and Alcoholism. 2014;49:292–298. doi: 10.1093/alcalc/agt182. doi:10.1093/ alcalc/agt182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaraman M. S., Kerr W. C. Simultaneous versus concurrent use of alcohol and cannabis in the National Alcohol Survey. Alcoholism: Clinical and Experimental Research. 2015;39:872–879. doi: 10.1111/acer.12698. doi:10.1111/ acer.12698. [DOI] [PMC free article] [PubMed] [Google Scholar]