Abstract
Objective:
Several epidemiological studies have reported that veterans and nonveterans have comparable substance use disorder (SUD) prevalence and SUD treatment rates for SUD and treatments of several types. No studies have compared functioning among veterans with SUD to veterans without SUD or to nonveterans.
Method:
We investigated the prevalence of past-year and lifetime SUD (based on criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition), overall and by substance, and estimated the association with physical and mental health functioning and treatment utilization and need among veterans and nonveterans in a nationally representative sample.
Results:
Predicted prevalence of any past-year SUD, with and without tobacco use disorder (TUD), among veterans was 32.9% and 17.1%, and prevalence of any lifetime SUD, with and without TUD, was 52.5 and 38.7%, respectively. Veterans had higher prevalence of past-year and lifetime SUD for some substances (e.g., tobacco, alcohol) but not others (e.g., cannabis, opioid). Lower physical and mental health functioning was found among veterans, relative to nonveterans, and participants with SUD, relative to those without SUD, and veterans with SUD reported the lowest functioning across all domains. More veterans than nonveterans received any SUD treatment and SUD treatment in specific domains (e.g., self-help). About 70% of veterans with past-year SUD did not receive treatment, but only 5.4% reported needing and not receiving treatment.
Conclusions:
Relative to nonveterans, veterans have higher prevalence of past-year TUD and lifetime alcohol use disorder or TUD and lower physical or mental health functioning. A minority of veterans receive SUD treatment, and few report unmet need for treatment.
U.S. armed forces personnel are presented with a unique set of experiences, challenges, and stressors, some of which may increase the likelihood that they will experience ongoing mental symptoms and conditions throughout their lives. Substances such as alcohol and tobacco may be used to cope with past and current stressors, negative affect, and challenging life circumstances, and to obtain and increase pleasure (Cooper et al., 1992, 1995; Mohr et al., 2018). Ongoing excessive or risky use may contribute to development of a substance use disorder (SUD). Four epidemiological studies have compared the prevalence of a limited number of past-year SUD between veterans and nonveterans (Evans et al., 2018; Golub et al., 2013; Hoggatt et al., 2017; Wagner et al., 2007). Few studies have compared veteran and nonveteran SUD treatment need and utilization (Golub et al., 2013; Wagner et al., 2007), and none have compared the mental or physical functioning of veterans with SUD to veterans without SUD and to nonveterans. To support proactive treatment planning and resource allocation, we compared the prevalence of past-year and lifetime SUD (based on criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition; DSM-5; American Psychiatric Association, 2013), overall and by specific substance, between veterans and nonveterans in a large, nationally representative sample. We also assessed the association of veteran status with functioning and SUD treatment need and utilization.
Hoggatt and colleagues (2017), Golub and colleagues (2013), and Wagner and colleagues (2007) compared prevalence of past-year SUD between veterans and nonveterans using National Survey on Drug Use and Health (NSDUH) data over varying time frames from 2000 to 2012, weighted and adjusted in various ways. Evans and colleagues (2018) used data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC-III; Grant, 2014). Hoggatt and colleagues (2017) found that relative to nonveteran women, veteran women did not significantly differ in prevalence of past-year SUDs examined (alcohol use disorder [AUD], drug use disorder [DUD] excluding tobacco use disorder [TUD], combined SUD excluding TUD) for any age group or for unadjusted or age-adjusted overall prevalence. Relative to nonveteran men, veteran men had significantly higher prevalences in two age-specific analyses (AUD and combined SUD among men 18–25 years of age); significantly lower unadjusted (by age) prevalence of AUD, DUD, and combined SUD; and similar age-adjusted prevalence. Golub and colleagues (2013) found, relative to a standardized nonveteran population, veterans age 21–34 did not significantly differ in the prevalence of past-year SUDs examined (AUD, DUD excluding TUD, combined SUD excluding TUD, cannabis, “pain killers,” “any psychotherapeutic”). Similarly, Wagner and colleagues (2007) found that veterans and a sample of comparable nonveterans matched in terms of age, gender, and region did not significantly differ in prevalence of past-year SUDs examined (AUD, DUD excluding TUD, combined SUD excluding TUD).
Several studies with different foci than ours used the same NESARC-III data we use (Dickerson et al., 2009; Evans et al., 2018; Smith et al., 2016). Although a comparison of AUD and DUD prevalence between veterans and nonveterans was included in Evans and colleagues (2018), unlike the current analysis, comparisons were done separately for men and women and by category of childhood adversity.
Studies of functioning among veterans with mental health issues have typically focused on disorders such as posttraumatic stress disorder (PTSD; Dobie et al., 2004; Grubaugh et al., 2005; Magruder et al., 2004). The few studies examining functioning among veterans with SUD (Calsyn et al., 2004; Ouimette et al., 1997, 1999) have not included comparisons to veterans without SUD or nonveterans with or without SUD. In fact, we are aware of few studies that have directly compared functioning between any population of veterans and nonveterans.
Two epidemiological studies have compared veteran and nonveteran SUD treatment utilization and need using NSDUH data (Golub et al., 2013; Wagner et al., 2007). Wagner and colleagues (2007) found that only 2.8% of veterans and 2.9% of nonveterans were estimated as having an unmet treatment need using federally defined treatment gap (i.e., meeting criteria for substance dependence and not receiving specialty treatment). Yet, a very low but statistically significantly higher percentage of veterans versus comparable nonveterans (0.8% vs. 0.5%) reported receiving any prior-year specialty SUD treatment (alcohol or illicit drug counseling or treatment through inpatient hospitalization or inpatient/outpatient rehabilitation facility, mental health center). Among younger veterans (ages 21–34 years), Golub and colleagues (2013) found estimated unmet treatment need (15.9%) to be higher than self-reported unmet treatment need (1.4%), with both rates comparable to the rates for nonveterans. Similarly, rates of estimated treatment receipt were comparable for veterans and nonveterans (1.8% and 1.7%, respectively).
In this analysis, we used an independent data set to replicate prior analyses of SUD prevalence and treatment utilization among veterans (Golub et al., 2013; Hoggatt et al., 2017; Wagner et al., 2007). We expanded on these previous studies by exploring (a) numerous substance-specific disorders, which is important given that veterans suffer from high rates of chronic pain, and physical and mental disorders (e.g., PTSD; Beckham et al., 1997a) for which they are prescribed medications with a high potential for abuse (e.g., opioids, benzodiazepines; Seal et al., 2012); (b) lifetime SUD, which is important as lifetime SUD is associated with negative outcomes (Compton et al., 2007), and even those who have stopped using substances have a high risk of relapse (Dawson et al., 2007; Moos & Moos, 2006); and (c) past-year treatment utilization across several modalities. We further extended the literature by exploring whether veterans reported lower functioning across multiple physical and mental domains and whether any deficits in functioning would be compounded by the presence of any past-year SUD, such that veterans with SUD would report the lowest functioning. We adjusted for a broad range of sociodemographic characteristics, which is important given substantial differences in composition between the veteran and nonveteran populations (see Wagner et al., 2007). In addition, we conducted analyses without adjustment, given noted problems with covariate adjustment of independent variables (Lynam et al., 2006; Miller & Chapman, 2001; also see Simmons et al., 2011).
Method
Participants and procedure
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) collected NESARC-III data from 36,309 United States civilian, noninstitutionalized adults (over 18 years) from April 2012 through June 2013 (Grant et al., 2015a). All participants included in the current study provided data regarding veteran status (N = 36,301).
Eligible adults from addresses/dwellings (tertiary unit) within census-defined blocks/block groups (secondary unit) within individual counties (primary unit) were randomly sampled through a multistage stratified procedure (Grant, 2014; Grant et al., 2015a). The total NESARC-III response rate was comparable to recent surveys (screener level = 72.0%, person level = 84.0%, total = 60.1%; Grant et al., 2015a). To represent the U.S. civilian population, data were adjusted (for nonresponse at person and screener levels and oversampling of Hispanic, Black, and Asian respondents) and weighted (through poststratification analysis). Differences were minimal in weighted distribution of characteristics between participants and the total eligible sample (Grant et al., 2015a).
Participants provided oral consent, were assessed through structured interviews via telephone, and were compensated with $90.00. Multifaceted training and ongoing supervision were provided to participant interviewers. Random callbacks were used to verify data. Institutional review boards of contractor Westat and The National Institutes of Health approved all protocols.
Measures
Veteran status.
Veteran status was assessed with a single item asking if participants ever served on active duty in the U.S. armed forces, reserves, or National Guard (but were no longer on active duty). In total, 3,119 participants (9.6% of the weighted total sample) identified as serving in active duty in the armed forces (rather than the reserves or National Guard), although this may have included participants who had been other-than-honorably discharged and/or not completed their service.
Substance use disorders.
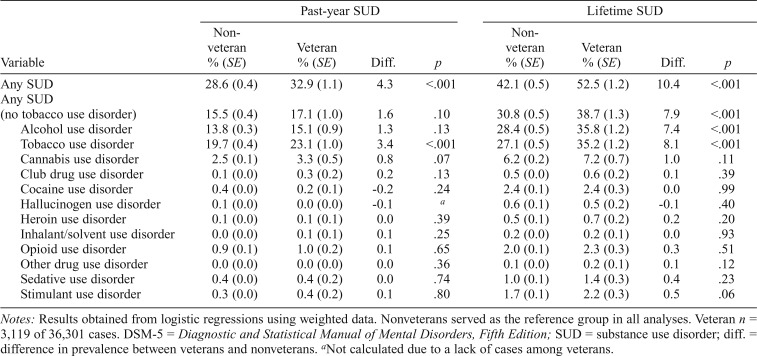
The Alcohol Use Disorder and Associated Disabilities Interview Schedule 5 (AUDADIS-5) was used to assess 12-month (i.e., past-year) and lifetime DSM-5 SUD (Grant et al., 2011). Dichotomous variables represented whether the participant met criteria required by DSM-5 for a given diagnosis (e.g., 2 of 11 alcohol dependence criteria) within (a) 12 months before the interview for past-year diagnoses, and (b) the past-year or any 1-year period before the past year for lifetime diagnoses. SUD indicator variables (with and without TUD) were created to represent the presence of one or more SUD listed in Table 2. Test–retest reliability of dichotomous SUD classification was fair to excellent, as was concordance between AUDADIS-5 and blind clinical reassessment using a second instrument (Psychiatric Research Interview for Substance Use and Mental Disorders, DSM-5; Grant et al., 2015b).
Table 2.
Predicted DSM-5 past-year and lifetime SUD prevalence between nonveterans and veterans, adjusted for sociodemographic variables
| Past-year SUD |
Lifetime SUD |
|||||||
| Variable | Nonveteran % (SE) | Veteran % (SE) | Diff. | p | Nonveteran % (SE) | Veteran % (SE) | Diff. | p |
| Any SUD | 28.6 (0.4) | 32.9 (1.1) | 4.3 | <.001 | 42.1 (0.5) | 52.5 (1.2) | 10.4 | <.001 |
| Any SUD (no tobacco use disorder) | 15.5 (0.4) | 17.1 (1.0) | 1.6 | .10 | 30.8 (0.5) | 38.7 (1.3) | 7.9 | <.001 |
| Alcohol use disorder | 13.8 (0.3) | 15.1 (0.9) | 1.3 | .13 | 28.4 (0.5) | 35.8 (1.2) | 7.4 | <.001 |
| Tobacco use disorder | 19.7 (0.4) | 23.1 (1.0) | 3.4 | <.001 | 27.1 (0.5) | 35.2 (1.2) | 8.1 | <.001 |
| Cannabis use disorder | 2.5 (0.1) | 3.3 (0.5) | 0.8 | .07 | 6.2 (0.2) | 7.2 (0.7) | 1.0 | .11 |
| Club drug use disorder | 0.1 (0.0) | 0.3 (0.2) | 0.2 | .13 | 0.5 (0.0) | 0.6 (0.2) | 0.1 | .39 |
| Cocaine use disorder | 0.4 (0.0) | 0.2 (0.1) | -0.2 | .24 | 2.4 (0.1) | 2.4 (0.3) | 0.0 | .99 |
| Hallucinogen use disorder | 0.1 (0.0) | 0.0 (0.0) | -0.1 | a | 0.6 (0.1) | 0.5 (0.2) | -0.1 | .40 |
| Heroin use disorder | 0.1 (0.0) | 0.1 (0.1) | 0.0 | .39 | 0.5 (0.1) | 0.7 (0.2) | 0.2 | .20 |
| Inhalant/solvent use disorder | 0.0 (0.0) | 0.1 (0.1) | 0.1 | .25 | 0.2 (0.0) | 0.2 (0.1) | 0.0 | .93 |
| Opioid use disorder | 0.9 (0.1) | 1.0 (0.2) | 0.1 | .65 | 2.0 (0.1) | 2.3 (0.3) | 0.3 | .51 |
| Other drug use disorder | 0.0 (0.0) | 0.0 (0.0) | 0.0 | .36 | 0.1 (0.0) | 0.2 (0.1) | 0.1 | .12 |
| Sedative use disorder | 0.4 (0.0) | 0.4 (0.2) | 0.0 | .74 | 1.0 (0.1) | 1.4 (0.3) | 0.4 | .23 |
| Stimulant use disorder | 0.3 (0.0) | 0.4 (0.2) | 0.1 | .80 | 1.7 (0.1) | 2.2 (0.3) | 0.5 | .06 |
Notes: Results obtained from logistic regressions using weighted data. Nonveterans served as the reference group in all analyses. Veteran n = 3,119 of 36,301 cases. DSM-5 = Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition; SUD = substance use disorder; diff. = difference in prevalence between veterans and nonveterans.
Not calculated due to a lack of cases among veterans.
Functioning.
The Short Form Health Survey, Version 2 (SF-12v2) includes 12 items that assess prior 4-week functioning in physical disability, role-physical, bodily pain, general health, vitality, social disability, role-emotional, and mental health domains (Ware et al., 1996). The Physical Health Composite comprises the first four scales, and the Mental Health Composite comprises the last four scales. Scale scores varied from 0 to 100 (M = 50, SD = 10), with lower scores associated with lower functioning. Prior research has demonstrated the reliability and validity of the SF-12v2 (Ware et al., 1996).
Treatment utilization.
The AUDADIS-5 assessed SUD treatment utilization in the prior 12 months. Respondents first answered whether they had ever sought help because of drinking, medication/drugs, or tobacco or nicotine. Additional questions assessed receipt of specific types of treatment, which were categorized into the following domains: (a) self-help (support group), (b) service from a professional (private physician, other professional), (c) outpatient (social service agency, outpatient clinic, crisis center, employee assistance program, counseling, other agency), (d) inpatient (detox ward/clinic, inpatient ward, drug/alcohol rehabilitation program, emergency room, halfway house, therapeutic community), and (e) other (methadone maintenance, religious affiliate [clergy, priest, etc.], medicine, drug [nicotine patches, gum], e-cigarettes/e-liquid, acupuncture, acupressure, meditation, any other methods). Additional questions assessed whether the patient thought they needed but did not seek treatment at any time in the prior 12 months. We defined dichotomous variables to indicate whether participants received any treatment in a given domain for any SUD or whether they needed but did not receive treatment. A composite variable was formed to represent the receipt of any type of treatment in the above-listed domains.
Statistical analysis
To account for the complex survey design of NESARC-III, all analyses incorporated survey weights using the Survey package in R (Lumley, 2016). We first investigated associations between veteran status and past-year and lifetime SUD. We fit a series of logistic regression models for each type of SUD that included an indicator of veteran status and sociodemographic variables (sex, race/ethnicity, age, marital status, education level, annual family income, urbanicity, region) as covariates. Using the fitted model, we calculated predicted SUD prevalence for veterans and nonveterans using the method of Graubard and Korn (1999), which accounts for covariate differences between populations. To investigate associations between functioning and any past-year SUD, we fit two sets of linear regressions with each domain of functioning serving as a dependent variable and sociodemographic variables included as covariates in both sets. In the first set, dummy-coded veteran status and dummy-coded presence of an SUD served as predictors, allowing us to separately examine the association between functioning and veteran status and presence of an SUD. To investigate whether veterans with SUD had lower functioning than other groups, in the second set we included dummy-coded variables to compare veterans with SUD to veterans without SUD and nonveterans with and without SUD. Analyses were restricted to any past-year SUD to be consistent with the time frame of the SF-12v2. We calculated predicted mean scores for each SF-12v2 domain. We also investigated associations between veteran status and receipt of SUD treatment or self-reported treatment need in the prior 12 months. We fit two sets of logistic regressions for SUD treatment as a function of veteran status and sociodemographic variables and calculated the predicted prevalence of SUD treatment in each domain (e.g., self-help). In the first set, we included the total sample of participants to compare rates with Wagner and colleagues (2007) and Golub and colleagues (2013), who based their rates on self-reported receipt of treatment among all veterans included in their samples. In the second set, we included only participants with SUD. Last, we repeated all analysis without adjustment for sociodemographic characteristics.
Results
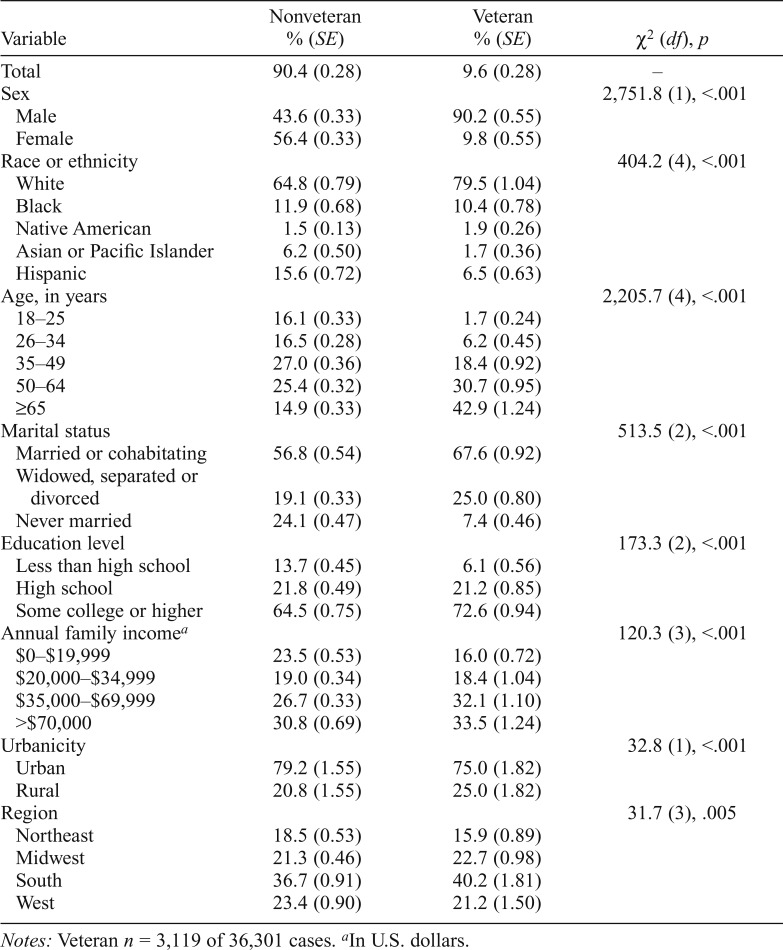
As shown in Table 1, veterans were disproportionality male, White, older, married or cohabitating, college educated, members of families with incomes over $35,000 per year (in U.S. dollars), and from urban areas and the southern United States. All sociodemographic variables differed between veterans and nonveterans.
Table 1.
Distribution of sociodemographic characteristics separately for veterans and nonveterans based on weighted data
| Nonveteran |
Veteran |
||
| Variable | % (SE) | % (SE) | χ2 (df), p |
| Total | 90.4 (0.28) | 9.6 (0.28) | – |
| Sex | 2,751.8 (1), <.001 | ||
| Male | 43.6 (0.33) | 90.2 (0.55) | |
| Female | 56.4 (0.33) | 9.8 (0.55) | |
| Race or ethnicity | 404.2 (4), <.001 | ||
| White | 64.8 (0.79) | 79.5 (1.04) | |
| Black | 11.9 (0.68) | 10.4 (0.78) | |
| Native American | 1.5 (0.13) | 1.9 (0.26) | |
| Asian or Pacific Islander | 6.2 (0.50) | 1.7 (0.36) | |
| Hispanic | 15.6 (0.72) | 6.5 (0.63) | |
| Age, in years | 2,205.7 (4), <.001 | ||
| 18–25 | 16.1 (0.33) | 1.7 (0.24) | |
| 26–34 | 16.5 (0.28) | 6.2 (0.45) | |
| 35–49 | 27.0 (0.36) | 18.4 (0.92) | |
| 50–64 | 25.4 (0.32) | 30.7 (0.95) | |
| ≥65 | 14.9 (0.33) | 42.9 (1.24) | |
| Marital status | 513.5 (2), <.001 | ||
| Married or cohabitating | 56.8 (0.54) | 67.6 (0.92) | |
| Widowed, separated or divorced | 19.1 (0.33) | 25.0 (0.80) | |
| Never married | 24.1 (0.47) | 7.4 (0.46) | |
| Education level | 173.3 (2), <.001 | ||
| Less than high school | 13.7 (0.45) | 6.1 (0.56) | |
| High school | 21.8 (0.49) | 21.2 (0.85) | |
| Some college or higher | 64.5 (0.75) | 72.6 (0.94) | |
| Annual family incomea | 120.3 (3), <.001 | ||
| $0–$19,999 | 23.5 (0.53) | 16.0 (0.72) | |
| $20,000–$34,999 | 19.0 (0.34) | 18.4 (1.04) | |
| $35,000–$69,999 | 26.7 (0.33) | 32.1 (1.10) | |
| >$70,000 | 30.8 (0.69) | 33.5 (1.24) | |
| Urbanicity | 32.8 (1), <.001 | ||
| Urban | 79.2 (1.55) | 75.0 (1.82) | |
| Rural | 20.8 (1.55) | 25.0 (1.82) | |
| Region | 31.7 (3), .005 | ||
| Northeast | 18.5 (0.53) | 15.9 (0.89) | |
| Midwest | 21.3 (0.46) | 22.7 (0.98) | |
| South | 36.7 (0.91) | 40.2 (1.81) | |
| West | 23.4 (0.90) | 21.2 (1.50) |
Notes: Veteran n = 3,119 of 36,301 cases.
In U.S. dollars.
When adjusting for sociodemographic variables, veterans’ predicted prevalence of any past-year SUD with and without TUD was 32.9% and 17.1%, respectively, and any lifetime SUD with and without TUD was 52.5% and 38.7%, respectively (Tables 2 & online-only Appendix A1). Prevalence was higher for veterans than nonveterans, except for any past-year SUD without TUD. Yet, differences in past-year SUD appeared to be attributable almost entirely to differences in TUD, as veterans had higher prevalence of past-year TUD (p < .001) but no other SUD relative to nonveterans. Differences in lifetime SUD appeared to be attributable almost entirely to differences in AUD and TUD, as veterans had significantly higher prevalence of lifetime AUD and TUD relative to nonveterans. Prevalence was similar for veterans and nonveterans for past-year and lifetime cannabis, club drug, cocaine, hallucinogen, heroin, inhalant/solvent, opioid, other drug, sedative, and stimulant use disorders (ranging from 0.0% to 7.2% among veterans and 0.0% to 6.2% among nonveterans).
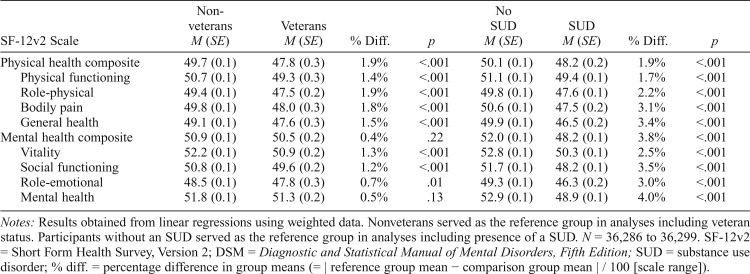
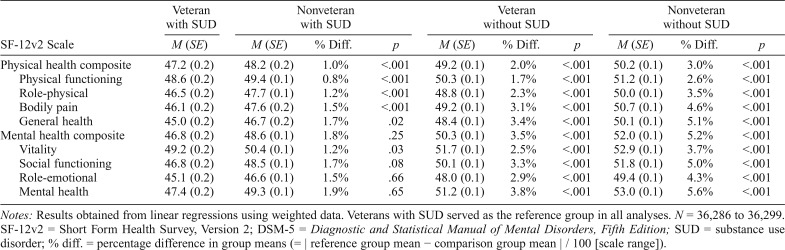
When we adjusted for sociodemographic variables, (a) relative to nonveterans, veterans reported significantly lower functioning in all physical and mental health domains except for Mental Health Composite and Mental Health (for which the point estimates were smaller for veterans, but the difference was not statistically significant), and (b) participants with versus without SUD reported significantly lower functioning in all physical and mental health domains (Tables 3 & A2). When we compared veterans and nonveterans with and without SUD, veterans with SUD reported the lowest functioning in all physical and mental health domains (Table 4 & A3). Functioning for veterans with SUD was significantly lower than veterans and nonveterans without SUD in all domains, and nonveterans with SUD in all physical health domains, and in a single mental health domain (i.e., vitality) when adjusting for sociodemographic variables.
Table 3.
Predicted mean norm-based scores for SF-12v2 composite scales for nonveterans and veterans and participants without any DSM-5 past-year SUD, separately, adjusted for sociodemographic variables
| SF-12v2 Scale | Nonveterans M (SE) | Veterans M (SE) | % Diff. | p | No SUD M (SE) | SUD M (SE) | % Diff. | p |
| Physical health composite | 49.7 (0.1) | 47.8 (0.3) | 1.9% | <.001 | 50.1 (0.1) | 48.2 (0.2) | 1.9% | <.001 |
| Physical functioning | 50.7 (0.1) | 49.3 (0.3) | 1.4% | <.001 | 51.1 (0.1) | 49.4 (0.1) | 1.7% | <.001 |
| Role-physical | 49.4 (0.1) | 47.5 (0.2) | 1.9% | <.001 | 49.8 (0.1) | 47.6 (0.1) | 2.2% | <.001 |
| Bodily pain | 49.8 (0.1) | 48.0 (0.3) | 1.8% | <.001 | 50.6 (0.1) | 47.5 (0.2) | 3.1% | <.001 |
| General health | 49.1 (0.1) | 47.6 (0.3) | 1.5% | <.001 | 49.9 (0.1) | 46.5 (0.2) | 3.4% | <.001 |
| Mental health composite | 50.9 (0.1) | 50.5 (0.2) | 0.4% | .22 | 52.0 (0.1) | 48.2 (0.1) | 3.8% | <.001 |
| Vitality | 52.2 (0.1) | 50.9 (0.2) | 1.3% | <.001 | 52.8 (0.1) | 50.3 (0.1) | 2.5% | <.001 |
| Social functioning | 50.8 (0.1) | 49.6 (0.2) | 1.2% | <.001 | 51.7 (0.1) | 48.2 (0.1) | 3.5% | <.001 |
| Role-emotional | 48.5 (0.1) | 47.8 (0.3) | 0.7% | .01 | 49.3 (0.1) | 46.3 (0.2) | 3.0% | <.001 |
| Mental health | 51.8 (0.1) | 51.3 (0.2) | 0.5% | .13 | 52.9 (0.1) | 48.9 (0.1) | 4.0% | <.001 |
Notes: Results obtained from linear regressions using weighted data. Nonveterans served as the reference group in analyses including veteran status. Participants without an SUD served as the reference group in analyses including presence of a SUD. N = 36,286 to 36,299. SF-12v2 = Short Form Health Survey, Version 2; DSM = Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition; SUD = substance use disorder; % diff. = percentage difference in group means (= | reference group mean − comparison group mean | / 100 [scale range]).
Table 4.
Predicted mean norm-based scores for SF-12v2 composite scales for nonveterans and veterans with and without any DSM-5 past-year SUD, adjusted for sociodemographic variables
| Veteran with SUD |
Nonveteran with SUD |
Veteran without SUD |
Nonveteran without SUD |
|||||||
| SF-12v2 Scale | M (SE) | M (SE) | % Diff. | p | M (SE) | % Diff. | p | M (SE) | % Diff. | p |
| Physical health composite | 47.2 (0.2) | 48.2 (0.2) | 1.0% | <.001 | 49.2 (0.1) | 2.0% | <.001 | 50.2 (0.1) | 3.0% | <.001 |
| Physical functioning | 48.6 (0.2) | 49.4 (0.1) | 0.8% | <.001 | 50.3 (0.1) | 1.7% | <.001 | 51.2 (0.1) | 2.6% | <.001 |
| Role-physical | 46.5 (0.2) | 47.7 (0.1) | 1.2% | <.001 | 48.8 (0.1) | 2.3% | <.001 | 50.0 (0.1) | 3.5% | <.001 |
| Bodily pain | 46.1 (0.2) | 47.6 (0.2) | 1.5% | <.001 | 49.2 (0.1) | 3.1% | <.001 | 50.7 (0.1) | 4.6% | <.001 |
| General health | 45.0 (0.2) | 46.7 (0.2) | 1.7% | .02 | 48.4 (0.1) | 3.4% | <.001 | 50.1 (0.1) | 5.1% | <.001 |
| Mental health composite | 46.8 (0.2) | 48.6 (0.1) | 1.8% | .25 | 50.3 (0.1) | 3.5% | <.001 | 52.0 (0.1) | 5.2% | <.001 |
| Vitality | 49.2 (0.2) | 50.4 (0.1) | 1.2% | .03 | 51.7 (0.1) | 2.5% | <.001 | 52.9 (0.1) | 3.7% | <.001 |
| Social functioning | 46.8 (0.2) | 48.5 (0.1) | 1.7% | .08 | 50.1 (0.1) | 3.3% | <.001 | 51.8 (0.1) | 5.0% | <.001 |
| Role-emotional | 45.1 (0.2) | 46.6 (0.1) | 1.5% | .66 | 48.0 (0.1) | 2.9% | <.001 | 49.4 (0.1) | 4.3% | <.001 |
| Mental health | 47.4 (0.2) | 49.3 (0.1) | 1.9% | .65 | 51.2 (0.1) | 3.8% | <.001 | 53.0 (0.1) | 5.6% | <.001 |
Notes: Results obtained from linear regressions using weighted data. Veterans with SUD served as the reference group in all analyses. N = 36,286 to 36,299. SF-12v2 = Short Form Health Survey, Version 2; DSM-5 = Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition; SUD = substance use disorder; % diff. = percentage difference in group means (= | reference group mean − comparison group mean | / 100 [scale range]).
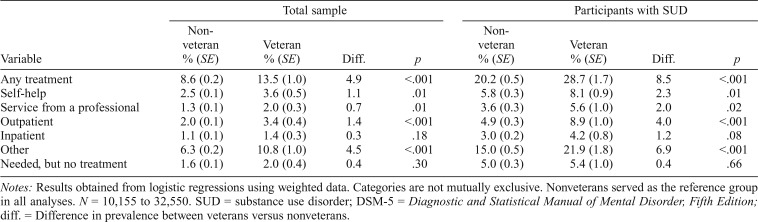
A total of 13.5% of veterans among the total sample, and 28.7% of veterans with a past-year SUD, received any treatment for any past-year SUD, which was 4.9 and 8.5 percentage points higher than for nonveterans (Tables 5 & A4). In both the total sample and among participants with SUD, veterans used specific treatment modalities (self-help, service from a professional, outpatient, other) more than nonveterans even after adjusting for sociodemographic variables. Prevalence of inpatient treatment and self-identified treatment need without receipt of treatment was similar between veterans and nonveterans.
Table 5.
Predicted prevalence of SUD treatment in the prior 12 months for any DSM-5 past year SUD among the full sample and among participants with SUD, adjusted for sociodemographic variables
| Total sample |
Participants with SUD |
|||||||
| Variable | Nonveteran % (SE) | veteran % (SE) | Diff. | p | Nonveteran % (SE) | veteran % (SE) | Diff. | p |
| Any treatment | 8.6 (0.2) | 13.5 (1.0) | 4.9 | <.001 | 20.2 (0.5) | 28.7 (1.7) | 8.5 | <.001 |
| Self-help | 2.5 (0.1) | 3.6 (0.5) | 1.1 | .01 | 5.8 (0.3) | 8.1 (0.9) | 2.3 | .01 |
| Service from a professional | 1.3 (0.1) | 2.0 (0.3) | 0.7 | .01 | 3.6 (0.3) | 5.6 (1.0) | 2.0 | .02 |
| Outpatient | 2.0 (0.1) | 3.4 (0.4) | 1.4 | <.001 | 4.9 (0.3) | 8.9 (1.0) | 4.0 | <.001 |
| Inpatient | 1.1 (0.1) | 1.4 (0.3) | 0.3 | .18 | 3.0 (0.2) | 4.2 (0.8) | 1.2 | .08 |
| Other | 6.3 (0.2) | 10.8 (1.0) | 4.5 | <.001 | 15.0 (0.5) | 21.9 (1.8) | 6.9 | <.001 |
| Needed, but no treatment | 1.6 (0.1) | 2.0 (0.4) | 0.4 | .30 | 5.0 (0.3) | 5.4 (1.0) | 0.4 | .66 |
Notes: Results obtained from logistic regressions using weighted data. Categories are not mutually exclusive. Nonveterans served as the reference group in all analyses. N = 10,155 to 32,550. SUD = substance use disorder; DSM-5 = Diagnostic and Statistical Manual of Mental Disorder, Fifth Edition; diff. = Difference in prevalence between veterans versus nonveterans.
Most analyses that did not account for sociodemographic variables yielded similar results to adjusted analyses (Tables A5–A8) with a few notable exceptions. Namely, differences between veterans and nonveterans in any past-year SUD with TUD and in TUD were not significant (at p < .05), whereas nonveterans had significantly higher prevalence of any past-year SUD without TUD, and alcohol, cannabis, and cocaine use disorders (Table A9). In addition, nonveterans with SUD reported significantly lower functioning on the mental health composite than veterans with SUD (Table A10).
Discussion
This study adds to the epidemiological literature comparing SUD prevalence between veterans and nonveterans. Thus, we provide needed data to inform treatment planning and resource allocation. In an independent sample, we generally replicate findings of no significant differences in past-year alcohol, other drug, or combined substance use disorders after accounting for differences in age and other covariates (Golub et al., 2013; Hoggatt et al., 2017; Wagner et al., 2007). We note, though, that Hoggatt and colleagues (2017) reported important heterogeneity by age, highlighting the importance of accounting for demographic differences in veteran-civilian comparisons. In our analysis, veterans’ higher prevalence of past-year SUD including TUD was primarily attributable to a higher prevalence of TUD. We extended prior research by examining prevalence of lifetime SUD and substance-specific disorders (e.g., tobacco, cannabis, opioids), notably finding higher prevalence of AUD and TUD among veterans. We also filled a research gap by examining functioning among veterans and nonveterans with and without past-year SUD, finding that veterans with SUD reported the lowest levels of functioning across multiple domains. Together, our results regarding functioning suggest that although SUD negatively affects veterans and nonveterans alike, veterans seem to suffer more harm, especially in physical functioning domains. We also found that more veterans receive SUD treatment than (a) nonveterans with SUD in the current study and (b) either veterans and nonveterans in prior studies (Golub et al., 2013; Wagner et al., 2007). Yet, although a minority of veterans with past-year SUD receive SUD treatment, most do not perceive themselves as needing treatment.
Past-year prevalence for any SUD (without TUD) and AUD, adjusted for a broad range of sociodemographic variables, was higher than Hoggatt and colleagues’ (2017) sample of veteran men or women and Wagner and colleagues (2007) veteran sample, and similar to Golub and colleagues (2013) 21- to 34-year-old veteran sample. Together, epidemiological research suggests that at least 1 out of 10 veterans meet criteria for any past-year SUD (without TUD). Although past-year prevalence of any SUD (without TUD) and AUD was similar among veterans and nonveterans, lifetime prevalence of these disorders was substantially higher among veterans versus nonveterans. More than a third of all veterans met criteria for any lifetime SUD (without TUD) and AUD. Veterans appear to be at greater risk for past-year and lifetime TUD, and lifetime AUD and TUD, which may be attributable to alcohol and tobacco both being legal, and historically, highly available while serving in the military.
Veterans do not currently appear to be at greater risk for opioid, sedative, or cannabis use disorders, although risk might increase as prescription and nonprescription access and use increase (Cerdá et al., 2012; Han et al., 2015; Hasin et al., 2015; also see Hadlandsmyth et al., 2018) and as veteran demographics shift to represent younger age groups in which cannabis use, in particular, is more common.
Our study extends research demonstrating increased prevalence of tobacco use among veterans versus nonveterans (Hoggatt et al., 2017; Wagner et al., 2007; also see Beckham et al., 1997b). Predicted prevalence of past-year and lifetime TUD was higher than 20%, although past-year TUD is comparable to prevalence of daily smoking/cigarette use found in prior studies (Hoggatt et al., 2017; Wagner et al., 2007). Our results support continued Veterans Health Administration (VHA) efforts to assess and treat TUD (Hamlett-Berry et al., 2009; Jonk et al., 2005). Importantly, we found that veterans (vs. nonveterans) did not have higher apparent prevalence of opioid or sedative use disorders despite commonly experiencing conditions for which these medications are regularly prescribed (e.g., pain, PTSD). Although prevalence of lifetime and past-year cannabis use disorder was elevated among veterans versus nonveterans, these differences were not statistically significant when adjusting for sociodemographic characteristics. These findings are notable given increasing self-administration of cannabis to treat disorders that veterans suffer from at disproportionate levels (e.g., PTSD; Boden et al., 2013). These conclusions should be interpreted in light of possible intentional or inadvertent under-reporting of SUD symptoms, by both veterans and civilians, or failure to detect symptoms of SUD among individuals using prescription medication (because prescription medications were excluded from the SUD assessment).
Extending prior research (Calsyn et al., 2004; Dobie et al., 2004; Grubaugh et al., 2005; Magruder et al., 2004; Ouimette et al., 1997, 1999), our study is the first to report lower functioning across multiple domains for veterans versus nonveterans, overall and among individuals with SUD. The harmful impact of SUD among veterans and nonveterans alike was evident in both physical and mental functioning domains and is generally enhanced among veterans for physical functioning. The finding of lower functioning among veterans may have been unduly influenced by veterans who were other-than-honorably discharged and/or did not complete their service (e.g., because of a medical condition), who may have been more likely to report poor functioning. Allaying potential concerns regarding the reliability of a single item to assess veteran status are the (a) high face validity of the item, (b) likely ease with which respondents can access the knowledge and memories required to answer this item, and (c) our use of self-reported dates of service as a reliability check. Regardless, accurate characterization of the veteran sample is important, as outreach or treatment may vary depending on whether veterans were honorably discharged and/or completed their service (e.g., veterans can use VHA benefits and services). Furthermore, statistically significant differences may be very small in magnitude for studies such as ours with large sample sizes, and future research is needed to establish the clinical significance of observed differences on the SF-12 (as has been done, for example, in establishing clinically significant changes in clinical trials [Ferguson et al., 2002]). Military service, which includes rigorous, intense, and potentially damaging physical activity, may increase risk of later physical ailments. The use of substance in a manner indicative of an SUD (e.g., to cope with ailments resulting from the veteran experience) is associated with physical limitations (e.g., Whiteford et al., 2013). Future research using prospective and longitudinal designs will be useful in determining whether SUD has a causal effect on poor functioning, as we suspect, along with identifying specific mechanisms that contribute to poor functioning among veterans, especially those with SUD.
Our results regarding treatment utilization and need were somewhat inconsistent with prior research using NSDUH data (Golub et al., 2013; Wagner et al., 2007). We found that more veterans (and nonveterans) reported receiving past-year SUD treatment than did Golub and colleagues (1.8%) and Wagner and colleagues (0.8%), regardless of whether we examined the total sample or participants with SUD only. Potentially accounting for this difference, the latter two studies did not include TUD treatment in their treatment-related variables, whereas we did so in our “any treatment” category (with specific types primarily included in the “other” category). Although more veterans than nonveterans with an SUD received any past-year SUD treatment, almost 70% of all veterans with an SUD did not receive SUD treatment. Like other studies, we found that veterans do not readily perceive themselves as needing SUD treatment, even those with an SUD: Only 5.3% of veterans with a past-year SUD reported needing but not receiving treatment. SUD treatment has been shown to be effective for various SUD (Dutra et al., 2008; Magill & Ray, 2009), and although veterans have higher apparent treatment rates, perhaps because of access to VHA (VHA, 2012), it is imperative that we increase access to and understanding of the benefits of SUD treatment (for veterans and nonveterans) and persuade veterans to use the treatment options at their disposal (VHA, 2012).
Further research is needed to understand the factors that increase SUD risk among veterans, in particular, and the mechanisms through which risky substance use proceeds to SUD and low physical and mental functioning. Prospective and longitudinal studies in which high-risk cohorts of veterans and nonveterans are recruited and followed over time may be especially useful in this regard. Such research can address longitudinal hypotheses, which we were unable to do because of the cross-sectional nature of our study and several additional limitations to our study (i.e., limited reliability of some SUD diagnoses, lack of data from some population segments).
In addition, results that were inconsistent when adjusting versus not adjusting for sociodemographic variables should be considered with some caution because of problems inherent to adjustment of independent variables (e.g., Lynam et al., 2006; Miller & Chapman, 2001). Veteran and nonveteran samples may no longer represent the veteran and nonveteran populations from which they were sampled when removing variance shared with sociodemographic variables from the veteran status variable. In unadjusted analyses, nonveterans had significantly higher unadjusted prevalence for multiple disorders, which may have reflected nonveterans being younger and younger persons having higher prevalence of SUD (Hoggatt et al., 2017). Undoubtedly, there remains much research to be done to identify and treat SUD in at-risk populations, such as veterans, with the use of large, nationally representative samples.
Footnotes
Katherine J. Hoggatt’s effort was funded through a VA HSR&D QUERI Career DevelopmentAward (Project #IIR 15-436; VA HSR&D, Washington, DC) at the VA Greater Los Angeles Healthcare System. The National Institute of Alcohol Abuse and Alcoholism (NIAAA) provided the data but did not review or approve the analyses, content and conclusions presented herein. Declarations of conflict of interest: none.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: Author; 2013. [Google Scholar]
- Beckham J. C., Crawford A. L., Feldman M. E., Kirby A. C., Hertzberg M. A., Davidson J. R. T., Moore S. D. Chronic posttraumatic stress disorder and chronic pain in Vietnam combat veterans. Journal of Psychosomatic Research. 1997a;43:379–389. doi: 10.1016/s0022-3999(97)00129-3. doi:10.1016/S0022-3999(97)00129-3. [DOI] [PubMed] [Google Scholar]
- Beckham J. C., Kirby A. C., Feldman M. E., Hertzberg M. A., Moore S. D., Crawford A. L., Fairbank J. A. Prevalence and correlates of heavy smoking in Vietnam veterans with chronic posttraumatic stress disorder. Addictive Behaviors. 1997b;22:637–647. doi: 10.1016/s0306-4603(96)00071-8. doi:10.1016/S0306-4603(96)00071-8. [DOI] [PubMed] [Google Scholar]
- Boden M. T., Babson K. A., Vujanovic A. A., Short N. A., Bonn-Miller M. O. Posttraumatic stress disorder and cannabis use characteristics among military veterans with cannabis dependence. American Journal on Addictions. 2013;22:277–284. doi: 10.1111/j.1521-0391.2012.12018.x. doi:10.1111/j.1521-0391.2012.12018.x. [DOI] [PubMed] [Google Scholar]
- Bouza C., Angeles M., Muñoz A., Amate J. M. Efficacy and safety of naltrexone and acamprosate in the treatment of alcohol dependence: A systematic review. Addiction. 2004;99:811–828. doi: 10.1111/j.1360-0443.2004.00763.x. doi:10.1111/j.1360-0443.2004.00763.x. [DOI] [PubMed] [Google Scholar]
- Calsyn D. A., Saxon A. J., Bush K. R., Howell D. N., Baer J. S., Sloan K. L., Kivlahan D. R. The Addiction Severity Index medical and psychiatric composite scores measure similar domains as the SF-36 in substance-dependent veterans: Concurrent and discriminant validity. Drug and Alcohol Dependence. 2004;76:165–171. doi: 10.1016/j.drugalcdep.2004.04.018. doi:10.1016/j.drugalcdep.2004.04.018. [DOI] [PubMed] [Google Scholar]
- Cerdá M., Wall M., Keyes K. M., Galea S., Hasin D. Medical marijuana laws in 50 states: Investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug and Alcohol Dependence. 2012;120:22–27. doi: 10.1016/j.drugalcdep.2011.06.011. doi:10.1016/j.drugalcdep.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton W. M., Thomas Y. F., Stinson F. S., Grant B. F. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. doi:10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Cooper M. L., Frone M. R., Russell M., Mudar P. Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology. 1995;69:990–1005. doi: 10.1037//0022-3514.69.5.990. doi:10.1037/0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Cooper M. L., Russell M., Skinner J. B., Windle M. Development and validation of a three-dimensional measure of drinking motives. Psychological Assessment. 1992;4:123–132. doi:10.1037/1040-3590.4.2.123. [Google Scholar]
- Dawson D. A., Goldstein R. B., Grant B. F. Rates and correlates of relapse among individuals in remission from DSM-IV alcohol dependence: a 3-year follow-up. Alcoholism: Clinical and Experimental Research. 2007;31:2036–2045. doi: 10.1111/j.1530-0277.2007.00536.x. doi:10.1111/j.1530-0277.2007.00536.x. [DOI] [PubMed] [Google Scholar]
- Dickerson D. L., O’Malley S. S., Canive J., Thuras P., Westermeyer J. Nicotine dependence and psychiatric and substance use comorbidities in a sample of American Indian male veterans. Drug and Alcohol Dependence. 2009;99:169–175. doi: 10.1016/j.drugalcdep.2008.07.014. doi:10.1016/j.drugalcdep.2008.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobie D. J., Kivlahan D. R., Maynard C., Bush K. R., Davis T. M., Bradley K. A. Posttraumatic stress disorder in female veterans: Association with self-reported health problems and functional impairment. Archives of Internal Medicine. 2004;164:394–400. doi: 10.1001/archinte.164.4.394. doi:10.1001/archinte.164.4.394. [DOI] [PubMed] [Google Scholar]
- Dutra L., Stathopoulou G., Basden S. L., Leyro T. M., Powers M. B., Otto M. W. A meta-analytic review of psychosocial interventions for substance use disorders. American Journal of Psychiatry. 2008;165:179–187. doi: 10.1176/appi.ajp.2007.06111851. doi:10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- Evans E. A., Upchurch D. M., Simpson T., Hamilton A. B., Hoggatt K. J. Differences by Veteran/civilian status and sex in associations between childhood adversity and alcohol and drug use disorders. Social Psychiatry and Psychiatric Epidemiology. 2018;53:421–435. doi: 10.1007/s00127-017-1463-0. doi:10.1007/s00127-017-1463-0. [DOI] [PubMed] [Google Scholar]
- Ferguson R. J., Robinson A. B., Splaine M. Use of the reliable change index to evaluate clinical significance in SF-36 outcomes. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation. 2002;11:509–516. doi: 10.1023/a:1016350431190. doi:10.1023/A:1016350431190. [DOI] [PubMed] [Google Scholar]
- Grant B. F. Source and accuracy statement: National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III) Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2014. [Google Scholar]
- Grant B. F., Goldstein R. B., Saha T. D., Chou S. P., Jung J., Zhang H., Hasin D. S. Epidemiology of DSM-5 Alcohol Use Disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015a;72:757–766. doi: 10.1001/jamapsychiatry.2015.0584. doi:10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant B. F., Goldstein R. B., Chou S. P., et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition Version (AUDADIS-5) Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2011. [Google Scholar]
- Grant B. F., Goldstein R. B., Smith S. M., Jung J., Zhang H., Chou S. P., Hasin D. S. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): Reliability of substance use and psychiatric disorder modules in a general population sample. Drug and Alcohol Dependence. 2015b;148:27–33. doi: 10.1016/j.drugalcdep.2014.11.026. doi:10.1016/j.drugalcdep.2014.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grubaugh A. L., Magruder K. M., Waldrop A. E., Elhai J. D., Knapp R. G., Frueh B. C. Subthreshold PTSD in primary care: Prevalence, psychiatric disorders, healthcare use, and functional status. Journal of Nervous and Mental Disease. 2005;193:658–664. doi: 10.1097/01.nmd.0000180740.02644.ab. doi:10.1097/01.nmd.0000180740.02644.ab. [DOI] [PubMed] [Google Scholar]
- Golub A., Vazan P., Bennett A. S., Liberty H. J. Unmet need for treatment of substance use disorders and serious psychological distress among veterans: A nationwide analysis using the NSDUH. Military Medicine. 2013;178:107–114. doi: 10.7205/milmed-d-12-00131. doi:10.7205/MILMED-D-12-00131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graubard B. I., Korn E. L. Predictive margins with survey data. Biometrics. 1999;55:652–659. doi: 10.1111/j.0006-341x.1999.00652.x. doi:10.1111/j.0006-341X.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- Hadlandsmyth K., Mosher H., Vander Weg M. W., Lund B. C. Decline in prescription opioids attributable to decreases in long-term use: A retrospective study in the Veterans Health Administration 2010–2016. Journal of General Internal Medicine. 2018;33:818–824. doi: 10.1007/s11606-017-4283-8. doi:10.1007/s11606-017-4283-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamlett-Berry K., Davison J., Kivlahan D. R., Matthews M. H., Hendrickson J. E., Almenoff P. L. Evidence-based national initiatives to address tobacco use as a public health priority in the Veterans Health Administration. Military Medicine. 2009;174:29–34. doi: 10.7205/milmed-d-00-3108. doi:10.7205/MILMED-D-00-3108. [DOI] [PubMed] [Google Scholar]
- Han B., Compton W. M., Jones C. M., Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003-2013. JAMA. 2015;314:1468–1478. doi: 10.1001/jama.2015.11859. doi:10.1001/jama.2015.11859. [DOI] [PubMed] [Google Scholar]
- Hasin D. S., Saha T. D., Kerridge B. T., Goldstein R. B., Chou S. P., Zhang H., Grant B. F. Prevalence of marijuana use disorders in the United States between 2001-2002 and 2012-2013. JAMA Psychiatry. 2015;72:1235–1242. doi: 10.1001/jamapsychiatry.2015.1858. doi:10.1001/jamapsychiatry.2015.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoggatt K. J., Lehavot K., Krenek M., Schweizer C. A., Simpson T. Prevalence of substance misuse among US veterans in the general population. American Journal on Addictions. 2017;26:357–365. doi: 10.1111/ajad.12534. doi:10.1111/ajad.12534. [DOI] [PubMed] [Google Scholar]
- Jonk Y. C., Sherman S. E., Fu S. S., Hamlett-Berry K. W., Geraci M. C., Joseph A. M. National trends in the provision of smoking cessation aids within the Veterans Health Administration. American Journal of Managed Care. 2005;11:77–85. [PubMed] [Google Scholar]
- Lynam D. R., Hoyle R. H., Newman J. P. The perils of partialling: Cautionary tales from aggression and psychopathy. Assessment. 2006;13:328–341. doi: 10.1177/1073191106290562. doi:10.1177/1073191106290562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill M., Ray L. A. Cognitive-behavioral treatment with adult alcohol and illicit drug users: A meta-analysis of randomized controlled trials. Journal of Studies on Alcohol and Drugs. 2009;70:516–527. doi: 10.15288/jsad.2009.70.516. doi:10.15288/jsad.2009.70.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magruder K. M., Frueh B. C., Knapp R. G., Johnson M. R., Vaughan J. A., III, Carson T. C., Hebert R. PTSD symptoms, demographic characteristics, and functional status among veterans treated in VA primary care clinics. Journal of Traumatic Stress. 2004;17:293–301. doi: 10.1023/B:JOTS.0000038477.47249.c8. doi:10.1023/B:JOTS.0000038477.47249.c8. [DOI] [PubMed] [Google Scholar]
- Miller G. A., Chapman J. P. Misunderstanding analysis of covariance. Journal of Abnormal Psychology. 2001;110:40–48. doi: 10.1037//0021-843x.110.1.40. doi:10.1037/0021-843X.110.1.40. [DOI] [PubMed] [Google Scholar]
- Mohr C. D., McCabe C. T., Haverly S. N., Hammer L. B., Carlson K. F. Drinking motives and alcohol use: The SERVe Study of U.S. current and former service members. Journal of Studies on Alcohol and Drugs. 2018;79:79–87. doi: 10.15288/jsad.2018.79.79. doi:10.15288/jsad.2018.79.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos R. H., Moos B. S. Rates and predictors of relapse after natural and treated remission from alcohol use disorders. Addiction. 2006;101:212–222. doi: 10.1111/j.1360-0443.2006.01310.x. doi:10.1111/j.1360-0443.2006.01310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouimette P. C., Ahrens C., Moos R. H., Finney J. W. Posttraumatic stress disorder in substance abuse patients: Relationship to 1-year posttreatment outcomes. Psychology of Addictive Behaviors. 1997;11:34–47. doi:10.1037/0893-164X.11.1.34. [Google Scholar]
- Ouimette P. C., Finney J. W., Moos R. H. Two-year posttreatment functioning and coping of substance abuse patients with posttraumatic stress disorder. Psychology of Addictive Behaviors. 1999;13:105–114. doi:10.1037/0893-164X.13.2.105. [Google Scholar]
- Seal K. H., Shi Y., Cohen G., Cohen B. E., Maguen S., Krebs E. E., Neylan T. C. Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan. JAMA. 2012;307:940–947. doi: 10.1001/jama.2012.234. doi:10.1001/jama.2012.234. [DOI] [PubMed] [Google Scholar]
- Simmons J. P., Nelson L. D., Simonsohn U. False-positive psychology: Undisclosed flexibility in data collection and analysis allows presenting anything as significant. Psychological Science. 2011;22:1359–1366. doi: 10.1177/0956797611417632. doi:10.1177/0956797611417632. [DOI] [PubMed] [Google Scholar]
- Smith S. M., Goldstein R. B., Grant B. F. The association between post-traumatic stress disorder and lifetime DSM-5 psychiatric disorders among veterans: Data from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III) Journal of Psychiatric Research. 2016;82:16–22. doi: 10.1016/j.jpsychires.2016.06.022. doi:10.1016/j.jpsychires.2016.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. The NSDUH report: Substance use, dependence and treatment among veterans. Rockville, MD: Author; 2005. [Google Scholar]
- Veterans Health Administration. Local implementation of evidence-based psychotherapies for mental and behavioral health conditions. Washington, D.C.: Author; 2012. [Google Scholar]
- Wagner T. H., Harris K. M., Federman B., Dai L., Luna Y., Humphreys K. Prevalence of substance use disorders among veterans and comparable nonveterans from the National Survey on Drug Use and Health. Psychological Services. 2007;4:149–157. doi:10.1037/1541-1559.4.3.149. [Google Scholar]
- Ware J., Jr, Kosinski M., Keller S. D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. doi:10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Whiteford H. A., Degenhardt L., Rehm J., Baxter A. J., Ferrari A. J., Erskine H. E., Vos T. Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. The Lancet. 2013;382:1575–1586. doi: 10.1016/S0140-6736(13)61611-6. doi:10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]