Abstract
Pheochromocytomas (PCCs) are rare neuroendocrine tumors that originate from chromaffin cells of the adrenal medulla, and paragangliomas (PGLs) are extra-adrenal pheochromocytomas. These can be mainly found in clinical syndromes including multiple endocrine neoplasia (MEN), von Hippel–Lindau (VHL) syndrome, neurofibromatosis-1 (NF-1) and familial paraganglioma (FPGL). PCCs and PGLs are thought to have the highest degree of heritability among human tumors, and it has been estimated that 60% of the patients have genetic abnormalities. This review provides an overview of the clinical syndrome and the genetic screening strategies of PCCs and PGLs. Comprehensive screening principles and strategies, along with specific screening based on clinical symptoms, biochemical tests and immunohistochemistry, are discussed.
Keywords: multiple endocrine neoplasia, von Hippel–Lindau syndrome, neurofibromatosis-1, pheochromocytoma, paraganglioma
Introduction
Pheochromocytomas (PCCs) and paragangliomas (PGLs), with an incidence of 2–8 per million population per year (1, 2), are rare neuroendocrine tumors that originate from chromaffin cells within or outside the adrenal medulla. With the recent recognition of the metastatic potential of PCC and PGL, risk stratification incorporating the metastatic potential, rather than just differentiation of benign or malignant, is recommended (3). PCC and PGL are thought to have the highest heritability among human tumors (4). Up to 40% of PCC and PGL are attributed to germline mutations, and overall, germline and somatic mutations can be present in 60% of PCC and PGL (5). Hereditary PCC and PGL (HPCC/PGL) are usually associated with neoplasm syndromes including multiple endocrine neoplasia (MEN 1 and MEN 2), von Hippel–Lindau (VHL), neurofibromatosis-1 (NF-1), and familial paraganglioma (FPGL). Apart from these, some catecholamine-secreting syndromes such as Sturge–Weber syndrome, tuberous sclerosis complex, ataxia-telangiectasia syndrome, and Carney Trilogy can be related to PCC and PGL (6). To date, there are 29 genes known to be related to PCC and PGL and the exploration of new genes is far from over (7). Genetic screening is useful to identify carriers of the pathogenic mutations of PCC and PGL. With the development of high-throughput screening technologies and comprehensive screening strategies, significant progress has been made in the field. This review provides an overview of the clinical syndromes and genetic screening strategies for PCC and PGL.
Clinical Syndromes of PCC/PGL
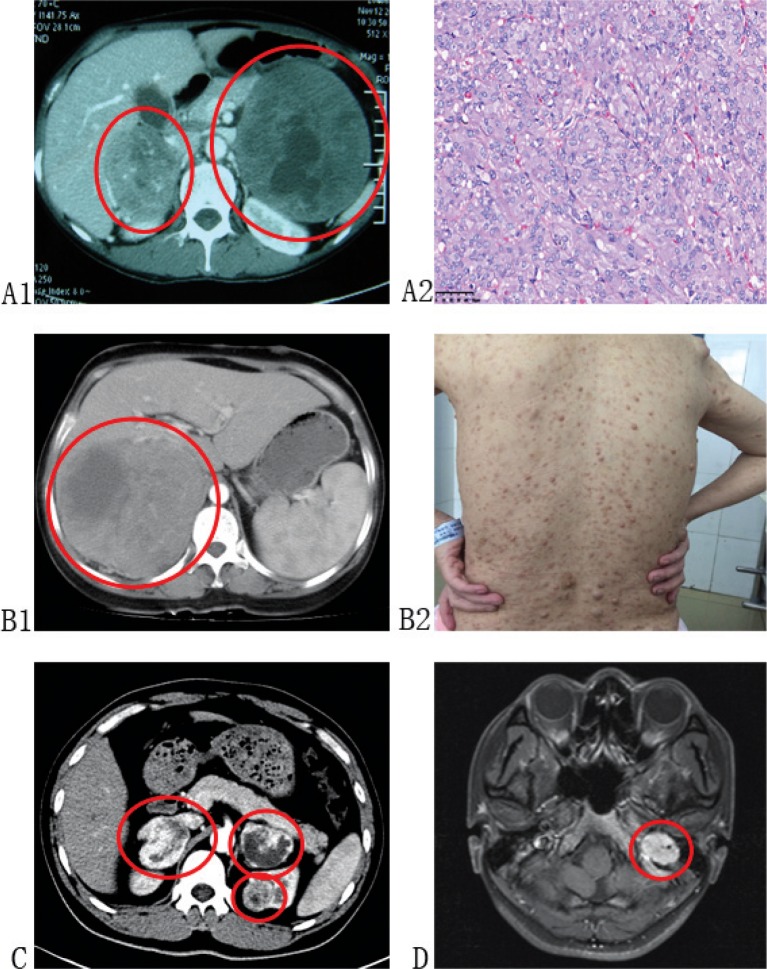
PCC and PGL are considered to be part of clinical syndromes when it comes to hereditary form. An understanding of these syndromes may help to raise awareness of PCC and PGL systematically. The PCC/PGL-related syndromes are summarized in Table 1, and the clinical presentations of PCC/PGL-related syndromes are depicted in Figure 1.
Table 1.
PCC/PGL-related syndromes
| Clinical syndrome | Subtype | Main manifestations | Mutation gene | Genetic nature |
|---|---|---|---|---|
| MEN 1 | PHPT, gastrinomas, benign insulinomas, anterior pituitary tumors, and PCC | MEN 1 | Tumor suppressor | |
| MEN 2 | MEN 2A | MTC, PCC, hyperthyroidism, and amyloidosis of the skin | RET | Proto oncogene |
| MEN 2B | MTC, PCC, hyperthyroidism, multiple mucosal neuromas, and Marfan-like syndrome | RET | Proto oncogene | |
| FMTC | HMTC | RET | Proto oncogene | |
| VHL | Type 1A | Hemangioblastoma in retina and central nervous system, multiple abdominal neoplasms and cysts, ccRCC, and no PCC | VHL | Tumor suppressor |
| Type 1B | Hemangioblastoma in retina and central nervous system, multiple abdominal neoplasms and cysts, and no ccRCC or PCC | VHL | Tumor suppressor | |
| Type 2A | PCC, hemangioblastoma in retina or central nervous system, and no ccRCC | VHL | Tumor suppressor | |
| Type 2B | PCC, hemangioblastoma in retina or central nervous system, ccRCC, endocrine neoplasia, and pancreatic cyst | VHL | Tumor suppressor | |
| Type 2C | Only PCC | VHL | Tumor suppressor | |
| NF-1 | Caft-au-lait macules, neurofibromas, freckling in the axillary or inguinal region, optic glioma, lisch nodules, osseous lesion, and PCC | NF-1 | Tumor suppressor | |
| FPGL | FPGL-1 | Multiple head and neck PGLs | SDHD | Tumor suppressor |
| FPGL-2 | Head and neck PGLs | SDHAF2 | Tumor suppressor | |
| FPGL-3 | Solitary head and neck PGLs | SDHC | Tumor suppressor | |
| FPGL-4 | The abdomen, pelvis, and mediastinum PGLs | SDHB | Tumor suppressor | |
| FPGL-5 | Leigh’s syndrome | SDHA | Tumor suppressor | |
| TMEM127 | PCC and rare renal cancers | TMEM127 | Tumor suppressor | |
| MAX | PCC/PGL | MAX | Tumor suppressor | |
| FH | Cutaneous and uterine leiomyomas, type 2 papillary renal carcinoma, and rare PCC/PGL | FH | Tumor suppressor |
PHPT, primary hyperparathyroidism; PCC, pheochromocytoma; MTC, medullary thyroid carcinoma; HMTC, hereditary medullary thyroid carcinoma; ccRCC, clear-cell renal cell carcinoma; PGL, paraganglioma.
Figure 1.
Clinical presentations of PCC/PGL-related syndromes. (A1 and A2): Patient diagnosed with MEN-2 presented with bilateral PCC and MTC. (B1 and B2): Patient diagnosed with NF-1 presented with PCC of right adrenal and multiple neurofibromas on her body. (C): Patient diagnosed with VHL presented with bilateral PCC and left ccRCC. (D): Patient diagnosed with FPGL presented with PGL in her left foramina jugulare, and genetic testing identified germline SDHB mutation of her and her families.
Multiple Endocrine Neoplasia 2
MEN 2 is an autosomal-dominant inheritance syndrome characterized by the presence of diseases such as medullary thyroid carcinoma (MTC), PCC, and hyperthyroidism (8). MEN 2 has three subtypes: MEN 2A, MEN 2B, and familial MTC (FMTC). Mutations of the proto-oncogene RET, located at chromosome 10q11.2, are responsible for the pathogenesis, and nearly 90% of MEN 2 is caused by single point mutation. The RET gene encodes tyrosine kinase receptor (TK receptor), which binds to the glial cell line-derived neurotrophic factor (GDNF) and modulates the targets downstream. There are 21 exons in the RET gene, and mutations in exons 10, 11, 13, 14, and 15 are responsible for the pathogenesis of MEN 2A (9, 10). According to Tang et al. (11), the incidence rate of MEN 2A is 1/25,000 and FMTC is 1.54/1,000,000; MEN 2B is the rarest form afflicting approximately 5% of the MEN 2 patients. All MEN 2 patients will suffer from MTC at an average age of 20 (10–30 years), about 50% cases of MEN 2 will contract PCC/PGL and 20–30% cases will develop parathyroid tumors (12). However, PCC caused by the mutation of RET has a relative low risk of becoming a malignant tumor, and the characteristic clinical manifestation is pathogenesis in both adrenal glands, which easily relapse. MTC typically occurs in MEN 2A patients during adulthood, in MEN 2B patients in childhood, and in FMTC patients in midlife. Some MEN 2A patients will develop amyloidosis of the skin. The clinical manifestations of MEN 2B are similar to MEN 2A with some considerably various characteristics such as multiple mucosal neuromas and Marfan-like syndrome (13).
Multiple Endocrine Neoplasia 1
MEN 1 is also an autosomal-dominant disease caused by inactivating mutation of MEN 1 tumor suppressor gene that is located on chromosome 11q13. This gene consists of 10 exons that encode a 610-amino acid suppressor protein, menin, whose main function is maintaining DNA stability and gene regulation. The prevalence of MEN1 is approximately 1/30,000 (14). Neuroendocrine tumors of parathyroid gland, pancreas, and pituitary gland are more common in MEN1, with occasional tumors of the adrenal, thymus, and bronchi (15). Therefore, when these lesions appear on the parathyroid gland, pancreas, and pituitary gland, MEN 1 should be considered. Biochemical tests for parathyroid hormone (PTH), calcium concentrations, glucagonomas, prolactin (PRL), and growth hormone (GH) can assist in the diagnosis of MEN 1. The most common clinical manifestation of MEN 1 is primary hyperparathyroidism (PHPT), which can occur in 90% of patients. The prevalence of MEN 1 patients who exhibit gastro-entero-pancreatic (GEP) tract lesions, such as gastrinomas and benign insulinomas, varies from 30% to 70% (16). The occurrence of anterior pituitary tumors in MEN 1 ranges between 10% and 60% (16).
Von Hippel–Lindau Syndrome
VHL is an autosomal-dominant inheritance syndrome caused by the germline mutations of VHL tumor suppressor gene. The VHL gene, which has three exons, is located in chromosome 3p25. The clinical manifestations of VHL syndrome include hemangioblastomas of retina and central nervous system, multiple neoplasms (clear cell carcinoma, multiple endocrine neoplasia, and pheochromocytoma), and cysts (multiple cysts in kidney and pancreas) (17). VHL contains a significant variation in phenotype and an age-related penetrance (18). The incidence rate of VHL is 1/36,000 (19), and there is an extremely high penetrance which reaches 95% before 60 years old. Although there has been a significant development in the recognition of molecular biology of VHL and advances in management strategies, the average survival age of VHL patients is mere 49 years. According to the possibility of suffering from PCC, VHL can be separated into two types: type 1 and type 2 (20). Type 1 VHL can also be separated into two subtypes: type 1A and type 1B, based on the probability of developing renal cell carcinoma. Type 1A patients will develop ccRCC without suffering from PCC. Therefore, VHL patients who suffer from PCC are recognized as Type 2. Type 2 VHL syndrome can also be classified into type 2A (hemangioblastoma, PCC, no ccRCC), type 2B (hemangioblastoma, PCC, and ccRCC), and type 2C (the only clinical manifestation is PCC). The VHL gene encodes the VHL protein (pVHL), which has a wide range of functions (21), the most important being the degradation of hypoxia inducible factors (HIFs). Without degradation, HIFs can be translocated to the nucleus and initiate transcription of multiple target genes, which can promote cell proliferation, angiogenesis, erythropoiesis, and anaerobe metabolism (22, 23).
Neurofibromatosis-1
NF-1 is also an autosomal-dominant disorder caused by mutation of the NF-1 gene that is located at chromosome 17q11.2, whose main function is to inhibit cell proliferation by converting RAS protein into its inactive form (6). Mutation can cause tumors to grow out of control, most commonly on peripheral nerves. NF-1 has a variety of clinical manifestations: caft-au-lait macules, neurofibromas, freckling in the axillary or inguinal region, optic glioma, lisch nodules, osseous lesion, and PCC. The diagnosis of NF-1 is usually based on its clinical presentations. The National Institutes of Health (NIH) suggest that if two or more of the above manifestations are found in someone, NF-1 should be considered by the clinician, and several examination measures may help the diagnosis, for example, CT or MRI for the detection of optic gliomas and plexiform neurofibromas, and biopsy for histologic confirmation. It is important to choose different examination measures to detect different clinical manifestations. There are also several variants of NF-1: segmental neurofibromatosis in which the lesions are confined to one or more well-circumscribed regions; spinal neurofibromatosis in which the tumors are mostly on the spinal nerve roots; NF-Noonan syndrome that is characterized by microsomia, webbed neck, and congenital heart disease; and Watson syndrome that is characterized by pulmonic stenosis, caft-au-lait macules, and decreased IQ (6, 24).
Other Catecholamine-Secreting Syndromes
Catecholamine-secreting tumors, although rare, can be found in patients with other neurocutaneous syndromes such as Sturge–Weber syndrome (encephalotrigeminal angiomatosis—a congenital neurological and skin disorder), tuberous sclerosis complex (a multisystem genetic disease), ataxia-telangiectasia syndrome (a neurodegenerative, autosomal recessive disease causing severe disability), and Carney–Trilogy (gastrointestinal stromal tumor, pulmonary chondroma, and extra-adrenal paraganglioma) (25).
SDH Mutations and Familial Paragangliomas
Mutations in the succinate dehydrogenase (SDH, mitochondrial complex II) and its subunit genes (SDHA, SDHB, SDHC, SDHD, and SDHAF2) can lead to FPGLs. The SDH is a part of both the electron transport chain and the tricarboxylic acid (TCA) cycle (26). It is worth noting that mutation in SDHB is possibly related to malignancy and poor prognosis (27). Mutations in SDHD and SDHAF2 are frequently found in head and neck PGLs in the paternal branch. SDHA-, SDHAF2-, and SDHC-related PGLs are infrequent.
FPGL-1
Mutations in SDHD are responsible for FPGL-1 (23–25), which are inherited in an autosomal-dominant fashion with a parent of origin effect. The gene is located on chromosome 11q23. Piccini et al. reported that SDHD was the most mutated gene among the genes coding for the SDHX complex (28). Usually, the clinical characteristics of the PGL-1 are multiple head and neck PGLs in patients with an age range of 28–31 years (29). Other tumors such as rare renal cancers and gastric stromal tumors have also been found in these patients (5).
FPGL-2
The germline loss-of-function mutations in the SDHAF2 (SDH5) gene, which is located on chromosome 11q13.1, lead to FPGL-2 (30). This syndrome is transmitted in an autosomal-dominant pattern with a parent of origin effect, similar to SDHD. FPGL-2 is commonly associated with parasympathetic PGL at the skull base and neck, and there has been no record of metastases. The average age of initial diagnosis is 33 years, with a range of 22–47 years (31).
FPGL-3
The gene for FPGL-3 is identified as SDHC, which is mapped to chromosome 1q23.3. FPGL-3 is an autosomal-dominant syndrome, which is unlikely to be PCC (32). Most patients develop solitary head and neck FPGLs. Tumors with SDHC mutations do not tend to be malignant or multifocal. The mean age of onset for patients with FPGL-3 is 38 years (33).
FPGL-4
FPGL-4 is caused by inactivating mutations in the tumor suppressor gene SDHB, located on chromosome 1p35-36, with an autosomal-dominant inheritance endowing the tumor susceptibility. Clinically, this syndrome is characterized by PGLs in the abdomen, pelvis, and mediastinum (34). The mean age at diagnosis of these tumors is 25–30 years (35). Furthermore, there is an increased risk of malignant PGL associated with this gene mutation (36).
FPGL-5
The SDHA gene mutations that map to chromosome 5p15 can result in FPGL-5. Biallelic mutations in SDHA are associated with Leigh’s syndrome (37). SDHA germline mutations have been identified in patients with PCC/PGL (38).
Other mutations
Apart from the typical mutations mentioned above, mutations in TMEM127 (locus of 2q11.2), MAX (14q23.3), FH (11q42.1), SPAS1/HIF2A (2P21), EGN1 (1q42.1), and KIF1β (1p36.22) have also been proved to be associated with PCC/PGL development (39, 40).
Genetic Screening Strategies of PCC/PGL
As PCC/PGL accounts for the highest proportion of hereditary-related tumors, it is recommended that all patients with PCC/PGL should be tested for genetic mutations for the following reasons: (i) up to 40% patients carry disease-causing germline mutations (41); (ii) even for sporadic patients, the overall frequency of germline mutation is higher than 10% (42); (iii) specific genetic mutations are related to malignant PCC/PGL; (iv) positive genetic test may lead to an accurate pre-surgery diagnosis; (v) germline mutation in genes may cause other syndromic morbidity; and (vi) positive genetic mutation of the proband may result in an earlier diagnosis of their relatives. To date, approximately 30 different genes have been reported to be related with the morbidity of PCC/PGL and the number is rising with the use of next-generation sequencing (NGS) (6). Thus, using NGS to test the germline mutation of patients with PCC/PGL may be a suitable process. These techniques include whole-genome sequencing (WGS), whole-exome sequencing (WES), and targeted NGS.
Whole-Genome Sequencing
WGS is a method of sequencing the whole human genome or determining the complete nucleotide sequence of an entire DNA sample (43, 44). It involves sequencing of all the coding and non-coding regions, making it one of the most comprehensive methods (45, 46). With sufficient read depth and fast sequencing time, it has been successfully used to detect chromosomal aberrations in circulating cancer cells (47). WGS has several disadvantages. In order to extract useful data with regard to known disease-causing mutations from enormous data that WGS generate, extensive filtering is usually needed (44). Ethical issues may also be raised when pathogenic mutations are identified in patients who have no known connections to the disease for which the genetic diagnosis was originally requested (44). WGS has been performed to characterize 179 cases of PCC/PGL in order to figure out genomic alterations in PCC/PGL (45, 46). However, high cost and complex data analysis have prevented WGS from being used as a routine diagnostic tool in PCC/PGL (48).
Whole-Exome Sequencing
Unlike WGS, which analyzes almost all nucleotides of the genome, WES only sequences coding regions of DNA (7). WES allows analysis of all potential disease-causing genes including known disease genes and genes unrelated to a disease (44). WES can also identify new disease genes or mutations that have not yet been associated with certain clinical phenotypes. Compared with WGS, WES can achieve higher read depths at a lower cost. However, regions such as promoters, enhancers, and transcription factor binding sites, which adjoin the exons, are often missed when WES is performed (7). Another limitation of WES is its incomplete representation due to the fact that exons are not included in the manufacturer’s capture design and coverage of base-pair reads in certain exons are relatively low (44). Due to the fact that about 85% of disease-causing mutations are expected to occur within the exome, WES has gained popularity in analysis of PCC/PGL (49). However, when WES is applied in PCC/PGL, the individual exon coverage of PCC/PGL genes and sequence depth are not easily achieved upon the completion of the analysis (7). Also, unsolicited pathogenic mutations are concerns when WES is applied in clinical diagnostic for monogenetic disorders just like WGS.
Targeted NGS
In targeted NGS method, only the coding regions of genes are enriched to target a specific disease (50). By restricting the mutation detection to a limited gene sets, targeted NGS can achieve better quality of representation and a much higher read depth than WGS or WES. Moreover, as the analysis is targeted at known disease genes, turn-around times for test results are significantly reduced due to simpler procedures in analyzing datasets and interpreting variants (51). In addition, unlike WGS and WES, targeted NGS minimizes the problem of unsolicited findings and thereby increases the willingness of patients in taking part in NGS method (52). In the diagnosis of PCC/PGL, three types of targeted NGS gene panels have been recommended. The first one, the basic panel, includes the PCC/PGL genes mutated at the germline level and is associated with familial disease (7). Second, the extended panel consists of the basic panel genes and candidate genes that have been proven to be functionally relevant in the pathogenesis of PCC/PGL (7). Third, the comprehensive panel includes all the extended panel genes, genes mutated at the germline or somatic level, and the genes found to be exclusively mutated at the somatic level (7, 45, 46). A high degree of diagnostic agreement with targeted NGS and conventional Sanger sequencing method in the analysis of PCC/PGL has been reported in several studies (50, 53). However, the application of targeted NGS is limited by problems like difficulty in adding new genes to existing panels and instruments-based errors.
Genetic screening according to clinical features and syndromic presentations
NGS is not feasible for all patients because of the high cost. In addition, patients with specific clinical features indicate different germline mutations. Therefore, establishing the priorities for genetic testing with a clinical feature-driven diagnostic algorithm can be a cost-saving and effective screening approach for PCC/PGL patients. Probands or their relatives presented with other syndromic morbidity (Table 1) may be directed for targeted germline mutation testing.
Genetic screening for patients with bilateral PCC
The presence of bilateral PCC means a relatively high probability of a germline mutation. For such patients, genetic screening of VHL and RET should be the priority as about 50% of these patients present with VHL/RET mutations. In addition, in bilateral PCC, TMEM127 is mutated in 39.1% of patients and MAX is mutated in 66.7% of patients (40, 54). These genes should also be tested for patients without VHL or RET mutation. Germline mutation of KIF1Bβ has also been reported to cause bilateral PCC (55), but it is not recommended for routine test as only a few patients with KIF1Bβ mutation have been reported. Although 14.1% of patients with NF1 germline mutation suffer bilateral PCC (40), the diagnosis of NF1 can be invariably established by clinical findings alone. Thus, genetic screening for these patients may base on syndromic presentations.
Genetic screening for patients with metastatic PCC/PGL
Because no single histological feature or immunohistochemical profile is able to predict metastatic potential independently, malignancy is established only by the presence of distant metastases in a site where paraganglia are not normally located (56, 57). However, to the modern understanding, PCC/PGL were granted to be malignant as all tumors have metastatic potential. Thus, PCC/PGL should be defined as metastatic or non-metastatic instead of malignant or benign (3). Metastatic disease was reported to occur in 10–20% of PCCs and in 15–35% of abdominal PGLs, and the potential varies depending on the genetic background (58–60). For patients with metastatic disease, SDHB should be tested first as more than 40% of this mutation is related to metastatic PCC/PGL and 5.5% of PCC/PGL patients carried SDHB germline mutation (27, 40). Further, SDHD, RET, VHL, and MAX should be tested if the result of SDHB mutation is negative given that 21.4% of PCC/PGL patients carry these germline mutations and those genes were reported to cause metastatic PCC/PGL with a relatively considerable rate (40). Although germline mutation in FH, KMT2D, and MEN1 had been reported to cause metastatic PCC/PGL, the proportion of PCC/PGL patients with these mutations is very low (61–63). Therefore, it is not recommended to be a routine test. Although the diagnosis of NF1 can be established by clinical findings, it is reported that 9.3% of patients with PCC/PGL caused by NF1 germline mutation suffer metastatic disease (40). Thus, genetic screening should be done among PCC/PGL patients clinically diagnosed with NF1 and their relatives for precise and early diagnosis.
Genetic screening according to the location of the tumor
Although PCC and PGL are both neuroendocrine tumors arising from chromaffin cells and regarded as the same disease, their location and hereditary background are different. Tumors that originate from the adrenal medulla are defined as PCCs, which are thought to be caused by the mutation of RET, VHL, MAX, NF1, and TMEM127; while tumors located in extra-adrenal positions are called paragangliomas, which were more likely to be caused by the mutation of SDHx, MDH2, and HIF2A (54). Therefore, genetic screening should also be done according to the location of the tumor.
Genetic screening according to the genotype–biochemical phenotype relationships
PCC and PGL are neuroendocrine tumors known to generally produce and secrete catecholamines and their metabolites which can be divided into three major phenotypes determined by the underlying molecular pathways of the tumor: (i) noradrenergic phenotype characterized by a (pseudo) hypoxic signature caused by mutations of VHL, SDHx, FH, MDH, and EPAS1; (ii) adrenergic phenotype characterized by activation of kinase signaling pathways caused by mutations of RET, NF1, TMEM127, and MAX; and (iii) dopaminergic phenotype, which is usually seen in patients with metastatic disease caused by SDHB and SDHD mutations. In addition, there are still tumors that do not exhibit elevations in either catecholamines or metanephrines, which is extremely rare, and are called the silent subgroup (64). Given all these, genetic screening could also be performed according to the genotype–biochemical phenotype relationships.
Genetic screening according to the immunohistochemical features
SDHB immunohistochemistry is negative in tumors mutated on all SDHx genes (2). Studies by Papathomas et al. showed that immunohistochemistry for SDHB was a reliable surrogate marker of SDHx mutation despite that the SDHB-immunonegative subset of VHL- and NF1-mutated paraganglionic tumors may influence the specificity (65). However, NF1 immunohistochemistry alone does not predict NF1 gene mutation status in PCCs (66). It is also reported that SDHA is negative only in SDHA-mutated tumors, and negative SDHB and SDHA immunohistochemistry on paraffin-embedded tumors can be associated with the presence of SDHA mutation. Generally, SDHD immunohistochemistry is positive in tumors mutated on SDHx genes. SDHB negative immunostaining is sometimes difficult to interpret because of background staining. So, the addition of SDHD immunohistochemistry will be very useful to predict SDHx gene variants in PGL/PCC (67). In addition, study by Korpershoek et al proved high predictive value of negative FH immunohistochemistry for patients with germline FH mutations (68, 69). Given these, SDHx should be tested for patients with negative SDHB immunohistochemistry, and test of VHL and NF1 should be performed if the test of SDHx were negative. SDHA should be tested for patients with negative SDHA immunohistochemistry. FH should be tested for patients with negative FH immunohistochemistry.
Conclusion
Genetic screening can be of great importance for all patients with PCC/PGL, and their relatives, especially for those with syndromic manifestation, multiple tumors, metastatic disease, or a young age of onset. Although traditional approach to genetic testing is likely be replaced in the future because of the development of NGS methods, it takes time. Currently, NGS is still unaffordable for many patients with PCC/PGL, and targeted sequencing is more convenient and precise. Given these, preliminary targeted genetic screening can be performed based on clinical features of the patients.
Acknowledgment
This work was supported by the National Natural Science Foundation of China (No. 81400773), Natural Science Foundation of China Hunan Province (No.14JJ6002), Funds for the Shenghua Yuying talents program of Central South University, and the Fundamental Research Funds for the Graduate Students of Central South University (No. 2017zzts901).
Footnotes
These authors contributed equally to this chapter.
Conflict of interest
The authors declare no potential conflict of interest with respect to research, authorship, and/or publication of this manuscript.
References
- 1.Bjorklund P, Pacak K, Crona J. Precision medicine in pheochromocytoma and paraganglioma: Current and future concepts. J Int Med. 2016;280(6):559–73. 10.1111/joim.12507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pai R, Manipadam MT, Singh P, Ebenazer A, Samuel P, Rajaratnam S. Usefulness of Succinate dehydrogenase B (SDHB) immunohistochemistry in guiding mutational screening among patients with pheochromocytoma-paraganglioma syndromes. APMIS. 2014;122(11):1130–5. 10.1111/apm.12269 [DOI] [PubMed] [Google Scholar]
- 3.Turchini J, Cheung VKY, Tischler AS, De Krijger RR, Gill AJ. Pathology and genetics of phaeochromocytoma and paraganglioma. Histopathology. 2018;72(1):97–105. 10.1111/his.13402 [DOI] [PubMed] [Google Scholar]
- 4.Dahia PL. Pheochromocytoma and paraganglioma pathogenesis: Learning from genetic heterogeneity. Nat Rev Canc. 2014;14(2):108–19. 10.1038/nrc3648 [DOI] [PubMed] [Google Scholar]
- 5.Favier J, Amar L, Gimenez-Roqueplo AP. Paraganglioma and phaeochromocytoma: From genetics to personalized medicine. Nat Rev Endocrinol. 2015;11(2):101–11. 10.1038/nrendo.2014.188 [DOI] [PubMed] [Google Scholar]
- 6.Pillai S, Gopalan V, Smith RA, Lam AK. Updates on the genetics and the clinical impacts on phaeochromocytoma and paraganglioma in the new era. Crit Rev Oncol Hematol. 2016;100:190–208. 10.1016/j.critrevonc.2016.01.022 [DOI] [PubMed] [Google Scholar]
- 7.Pillai S, Gopalan V, Lam AK. Review of sequencing platforms and their applications in phaeochromocytoma and paragangliomas. Crit Rev Oncol Hematol. 2017;116:58–67. 10.1016/j.critrevonc.2017.05.005 [DOI] [PubMed] [Google Scholar]
- 8.Lebeault M, Pinson S, Guillaud-Bataille M, Gimenez-Roqueplo AP, Carrie A, Barbu V, et al. . Nationwide French study of RET variants detected from 2003 to 2013 suggests a possible influence of polymorphisms as modifiers. Thyroid. 2017;27(12):1511–22. 10.1089/thy.2016.0399 [DOI] [PubMed] [Google Scholar]
- 9.Qi XP, Chen XL, Ma JM, Du ZF, Fei J, Yang CP, et al. . RET proto-oncogene genetic screening of families with multiple endocrine neoplasia type 2 optimizes diagnostic and clinical management in China. Thyroid. 2012;22(12):1257–65. 10.1089/thy.2012.0134 [DOI] [PubMed] [Google Scholar]
- 10.Plaza-Menacho I. Structure and function of RET in multiple endocrine neoplasia type 2. Endocr Relat Canc. 2018;25(2):T79–90. 10.1530/ERC-17-0354 [DOI] [PubMed] [Google Scholar]
- 11.Tang KL, Lin Y, Li LM. Diagnosis and surgical treatment of multiple endocrine neoplasia type 2A. World J Surg Oncol. 2014;12:8 10.1186/1477-7819-12-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Castinetti F, Maia AL, Peczkowska M, Barontini M, Hasse-Lazar K, Links TP, et al. . The penetrance of MEN2 pheochromocytoma is not only determined by RET mutations. Endocr Relat Canc. 2017;24(8):L63–7. 10.1530/ERC-17-0189 [DOI] [PubMed] [Google Scholar]
- 13.Wells SA., Jr Advances in the management of MEN2: From improved surgical and medical treatment to novel kinase inhibitors. Endocr Relat Canc. 2018;25(2):T1–13. 10.1530/ERC-17-0325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsirlin A, Oo Y, Sharma R, Kansara A, Gliwa A, Banerji MA. Pheochromocytoma: A review. Maturitas. 2014;77(3):229–38. 10.1016/j.maturitas.2013.12.009 [DOI] [PubMed] [Google Scholar]
- 15.Manoharan J, Raue F, Lopez CL, Albers MB, Bollmann C, Fendrich V, et al. . Is routine screening of young asymptomatic MEN1 patients necessary? World J Surg. 2017;41(8):2026–32. 10.1007/s00268-017-3992-9 [DOI] [PubMed] [Google Scholar]
- 16.Falchetti A, Marini F, Luzi E, Tonelli F, Brandi ML. Multiple endocrine neoplasms. Best Pract Res Clin Rheumatol. 2008;22(1):149–63. 10.1016/j.berh.2007.11.010 [DOI] [PubMed] [Google Scholar]
- 17.Bouhamdani N, Joy A, Barnett D, Cormier K, Leger D, Chute IC, et al. . Quantitative proteomics to study a small molecule targeting the loss of von Hippel-Lindau in renal cell carcinomas. Int J Canc. 2017;141(4):778–90. 10.1002/ijc.30774 [DOI] [PubMed] [Google Scholar]
- 18.Butz JJ, Yan Q, McKenzie TJ, Weingarten TN, Cavalcante AN, Bancos I, et al. . Perioperative outcomes of syndromic paraganglioma and pheochromocytoma resection in patients with von Hippel-Lindau disease, multiple endocrine neoplasia type 2, or neurofibromatosis type 1. Surgery. 2017;162(6):1259–69. 10.1016/j.surg.2017.08.002 [DOI] [PubMed] [Google Scholar]
- 19.Santos P, Pimenta T, Taveira-Gomes A. Hereditary pheochromocytoma. Int J Surg Pathol. 2014;22(5):393–400. 10.1177/1066896914537683 [DOI] [PubMed] [Google Scholar]
- 20.Crespigio J, Berbel LCL, Dias MA, Berbel RF, Pereira SS, Pignatelli D, et al. . Von Hippel-Lindau disease: A single gene, several hereditary tumors. J Endocrinol Investig. 2018;41(1):21–31. 10.1007/s40618-017-0683-1 [DOI] [PubMed] [Google Scholar]
- 21.Binderup MLM. von Hippel-Lindau disease: Diagnosis and factors influencing disease outcome. Danish Med J. 2018;65(3):1–29. [PubMed] [Google Scholar]
- 22.Gossage L, Eisen T, Maher ER. VHL, the story of a tumour suppressor gene. Nat Rev Canc. 2015;15(1):55–64. 10.1038/nrc3844 [DOI] [PubMed] [Google Scholar]
- 23.Nordstrom-O'Brien M, van der Luijt RB, van Rooijen E, van den Ouweland AM, Majoor-Krakauer DF, Lolkema MP, et al. . Genetic analysis of von Hippel-Lindau disease. Hum Mutat. 2010;31(5):521–37. 10.1002/humu.21219 [DOI] [PubMed] [Google Scholar]
- 24.Radtke HB, Sebold CD, Allison C, Haidle JL, Schneider G. Neurofibromatosis type 1 in genetic counseling practice: Recommendations of the National Society of Genetic Counselors. J Genet Counsel. 2007;16(4):387–407. 10.1007/s10897-007-9101-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hes FJ, Hoppener JW, Lips CJ. Clinical review 155: Pheochromocytoma in Von Hippel-Lindau disease. J Clin Endocrinol Metabol. 2003;88(3):969–74. 10.1210/jc.2002-021466 [DOI] [PubMed] [Google Scholar]
- 26.Rustin P, Rotig A. Inborn errors of complex II--unusual human mitochondrial diseases. Biochim Biophys Acta. 2002;1553(1–2):117–22. 10.1016/S0005-2728(01)00228-6 [DOI] [PubMed] [Google Scholar]
- 27.Amar L, Baudin E, Burnichon N, Peyrard S, Silvera S, Bertherat J, et al. . Succinate dehydrogenase B gene mutations predict survival in patients with malignant pheochromocytomas or paragangliomas. J Clin Endocrinol Metabol. 2007;92(10):3822–8. 10.1210/jc.2007-0709 [DOI] [PubMed] [Google Scholar]
- 28.Piccini V, Rapizzi E, Bacca A, Di Trapani G, Pulli R, Giache V, et al. . Head and neck paragangliomas: Genetic spectrum and clinical variability in 79 consecutive patients. Endocr Relat Canc. 2012;19(2):149–55. 10.1530/ERC-11-0369 [DOI] [PubMed] [Google Scholar]
- 29.Astuti D, Douglas F, Lennard TW, Aligianis IA, Woodward ER, Evans DG, et al. . Germline SDHD mutation in familial phaeochromocytoma. Lancet. 2001;357(9263):1181–2. 10.1016/S0140-6736(00)04378-6 [DOI] [PubMed] [Google Scholar]
- 30.Hao HX, Khalimonchuk O, Schraders M, Dephoure N, Bayley JP, Kunst H, et al. . SDH5, a gene required for flavination of succinate dehydrogenase, is mutated in paraganglioma. Science. 2009;325(5944):1139–42. 10.1126/science.1175689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kunst HP, Rutten MH, de Monnink JP, Hoefsloot LH, Timmers HJ, Marres HA, et al. . SDHAF2 (PGL2-SDH5) and hereditary head and neck paraganglioma. Clin Canc Res. 2011;17(2):247–54. 10.1158/1078-0432.CCR-10-0420 [DOI] [PubMed] [Google Scholar]
- 32.Schiavi F, Boedeker CC, Bausch B, Peczkowska M, Gomez CF, Strassburg T, et al. . Predictors and prevalence of paraganglioma syndrome associated with mutations of the SDHC gene. JAMA. 2005;294(16):2057–63. 10.1001/jama.294.16.2057 [DOI] [PubMed] [Google Scholar]
- 33.Jafri M, Maher ER. The genetics of phaeochromocytoma: Using clinical features to guide genetic testing. Eur J Endocrinol. 2012;166(2):151–8. 10.1530/EJE-11-0497 [DOI] [PubMed] [Google Scholar]
- 34.Neumann HP, Pawlu C, Peczkowska M, Bausch B, McWhinney SR, Muresan M, et al. . Distinct clinical features of paraganglioma syndromes associated with SDHB and SDHD gene mutations. JAMA. 2004;292(8):943–51. 10.1001/jama.292.8.943 [DOI] [PubMed] [Google Scholar]
- 35.Gimenez-Roqueplo AP, Dahia PL, Robledo M. An update on the genetics of paraganglioma, pheochromocytoma, and associated hereditary syndromes. Horm Metab Res. 2012;44(5):328–33. 10.1055/s-0031-1301302 [DOI] [PubMed] [Google Scholar]
- 36.Ricketts CJ, Forman JR, Rattenberry E, Bradshaw N, Lalloo F, Izatt L, et al. . Tumor risks and genotype-phenotype-proteotype analysis in 358 patients with germline mutations in SDHB and SDHD. Hum Mutat. 2010;31(1):41–51. 10.1002/humu.21136 [DOI] [PubMed] [Google Scholar]
- 37.Horvath R, Abicht A, Holinski-Feder E, Laner A, Gempel K, Prokisch H, et al. . Leigh syndrome caused by mutations in the flavoprotein (Fp) subunit of succinate dehydrogenase (SDHA). J Neurol Neurosurg Psychiatr. 2006;77(1):74–6. 10.1136/jnnp.2005.067041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Parfait B, Chretien D, Rotig A, Marsac C, Munnich A, Rustin P. Compound heterozygous mutations in the flavoprotein gene of the respiratory chain complex II in a patient with Leigh syndrome. Hum Genet. 2000;106(2):236–43. 10.1007/s004390051033 [DOI] [PubMed] [Google Scholar]
- 39.Mercado-Asis LB, Wolf KI, Jochmanova I, Taieb D. Pheochromocytoma: A genetic and diagnostic update. Endocrine Pract. 2018;24(1):78–90. 10.4158/EP-2017-0057 [DOI] [PubMed] [Google Scholar]
- 40.Welander J, Soderkvist P, Gimm O. Genetics and clinical characteristics of hereditary pheochromocytomas and paragangliomas. Endocr Relat Canc. 2011;18(6):R253–76. 10.1530/ERC-11-0170 [DOI] [PubMed] [Google Scholar]
- 41.Fishbein L, Merrill S, Fraker DL, Cohen DL, Nathanson KL. Inherited mutations in pheochromocytoma and paraganglioma: Why all patients should be offered genetic testing. Ann Surg Oncol. 2013;20(5):1444–50. 10.1245/s10434-013-2942-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brito JP, Asi N, Bancos I, Gionfriddo MR, Zeballos-Palacios CL, Leppin AL, et al. . Testing for germline mutations in sporadic pheochromocytoma/paraganglioma: A systematic review. Clin Endocrinol. 2015;82(3):338–45. 10.1111/cen.12530 [DOI] [PubMed] [Google Scholar]
- 43.van El CG, Cornel MC, Borry P, Hastings RJ, Fellmann F, Hodgson SV, et al. . Whole-genome sequencing in health care: Recommendations of the European Society of Human Genetics. Eur J Hum Genet. 2013;21(6):580–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.de Koning TJ, Jongbloed JD, Sikkema-Raddatz B, Sinke RJ. Targeted next-generation sequencing panels for monogenetic disorders in clinical diagnostics: The opportunities and challenges. Expert Rev Mol Diagn. 2015;15(1):61–70. 10.1586/14737159.2015.976555 [DOI] [PubMed] [Google Scholar]
- 45.Toledo RA, Qin Y, Cheng ZM, Gao Q, Iwata S, Silva GM, et al. . Recurrent mutations of chromatin-remodeling genes and kinase receptors in pheochromocytomas and paragangliomas. Clin Canc Res. 2016;22(9):2301–10. 10.1158/1078-0432.CCR-15-1841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Toledo RA, Burnichon N, Cascon A, Benn DE, Bayley JP, Welander J, et al. . Consensus statement on next-generation-sequencing-based diagnostic testing of hereditary phaeochromocytomas and paragangliomas. Nat Rev Endocrinol. 2017;13(4):233–47. 10.1038/nrendo.2016.185 [DOI] [PubMed] [Google Scholar]
- 47.Leary RJ, Sausen M, Kinde I, Papadopoulos N, Carpten JD, Craig D, et al. . Detection of chromosomal alterations in the circulation of cancer patients with whole-genome sequencing. Science Translat Med. 2012;4(162):162ra54 10.1126/scitranslmed.3004742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mardis ER. Sequencing the AML genome, transcriptome, and epigenome. Seminars in hematology. 2014;51(4):250–8. 10.1053/j.seminhematol.2014.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bainbridge MN, Wang M, Burgess DL, Kovar C, Rodesch MJ, D'Ascenzo M, et al. . Whole exome capture in solution with 3 Gbp of data. Genome Biol. 2010;11(6):R62 10.1186/gb-2010-11-6-r62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Welander J, Andreasson A, Juhlin CC, Wiseman RW, Backdahl M, Hoog A, et al. . Rare germline mutations identified by targeted next-generation sequencing of susceptibility genes in pheochromocytoma and paraganglioma. J Clin Endocrinol Metabol. 2014;99(7):E1352–60. 10.1210/jc.2013-4375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sikkema-Raddatz B, Johansson LF, de Boer EN, Almomani R, Boven LG, van den Berg MP, et al. . Targeted next-generation sequencing can replace Sanger sequencing in clinical diagnostics. Hum Mutat. 2013;34(7):1035–42. 10.1002/humu.22332 [DOI] [PubMed] [Google Scholar]
- 52.Neveling K, Feenstra I, Gilissen C, Hoefsloot LH, Kamsteeg EJ, Mensenkamp AR, et al. . A post-hoc comparison of the utility of sanger sequencing and exome sequencing for the diagnosis of heterogeneous diseases. Hum Mutat. 2013;34(12):1721–6. [DOI] [PubMed] [Google Scholar]
- 53.Rattenberry E, Vialard L, Yeung A, Bair H, McKay K, Jafri M, et al. . A comprehensive next generation sequencing-based genetic testing strategy to improve diagnosis of inherited pheochromocytoma and paraganglioma. J Clin Endocrinol Metabol. 2013;98(7):E1248–56. 10.1210/jc.2013-1319 [DOI] [PubMed] [Google Scholar]
- 54.Lalloo F. Diagnosis and management of hereditary phaeochromocytoma and paraganglioma. Recent Results Cancer Res. 2016;205:105–24. 10.1007/978-3-319-29998-3_7 [DOI] [PubMed] [Google Scholar]
- 55.Yeh IT, Lenci RE, Qin Y, Buddavarapu K, Ligon AH, Leteurtre E, et al. . A germline mutation of the KIF1B beta gene on 1p36 in a family with neural and nonneural tumors. Hum Genet. 2008;124(3):279–85. 10.1007/s00439-008-0553-1 [DOI] [PubMed] [Google Scholar]
- 56.Linnoila RI, Keiser HR, Steinberg SM, Lack EE. Histopathology of benign versus malignant sympathoadrenal paragangliomas: Clinicopathologic study of 120 cases including unusual histologic features. Hum Pathol. 1990;21(11):1168–80. 10.1016/0046-8177(90)90155-X [DOI] [PubMed] [Google Scholar]
- 57.Tischler AS. Pheochromocytoma and extra-adrenal paraganglioma: Updates. Arch Pathol Lab Med. 2008;132(8):1272–84. [DOI] [PubMed] [Google Scholar]
- 58.O'Riordain DS, Young WF Jr., Grant CS, Carney JA, van Heerden JA. Clinical spectrum and outcome of functional extraadrenal paraganglioma. World J Surg. 1996;20(7):916–21; discussion 22 10.1007/s002689900139 [DOI] [PubMed] [Google Scholar]
- 59.Amar L, Bertherat J, Baudin E, Ajzenberg C, Bressac-de Paillerets B, Chabre O, et al. . Genetic testing in pheochromocytoma or functional paraganglioma. J Clin Oncol. 2005;23(34):8812–8. 10.1200/JCO.2005.03.1484 [DOI] [PubMed] [Google Scholar]
- 60.King KS, Prodanov T, Kantorovich V, Fojo T, Hewitt JK, Zacharin M, et al. . Metastatic pheochromocytoma/paraganglioma related to primary tumor development in childhood or adolescence: Significant link to SDHB mutations. J Clin Oncol. 2011;29(31):4137–42. 10.1200/JCO.2011.34.6353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Castro-Vega LJ, Buffet A, De Cubas AA, Cascon A, Menara M, Khalifa E, et al. . Germline mutations in FH confer predisposition to malignant pheochromocytomas and paragangliomas. Hum Mol Genet. 2014;23(9):2440–6. 10.1093/hmg/ddt639 [DOI] [PubMed] [Google Scholar]
- 62.Schussheim DH, Skarulis MC, Agarwal SK, Simonds WF, Burns AL, Spiegel AM, et al. . Multiple endocrine neoplasia type 1: New clinical and basic findings. J Trends Endocrinol Metabol. 2001;12(4):173–8. 10.1016/S1043-2760(00)00372-6 [DOI] [PubMed] [Google Scholar]
- 63.Juhlin CC, Stenman A, Haglund F, Clark VE, Brown TC, Baranoski J, et al. . Whole-exome sequencing defines the mutational landscape of pheochromocytoma and identifies KMT2D as a recurrently mutated gene. J Gene Chromosome Canc. 2015;54(9):542-54. 10.1002/gcc.22267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gupta G, Pacak K. Precision medicine: An update on genotype/biochemical phenotype relationships in pheochromocytoma/paraganglioma patients. Endocr Pract. 2017;23(6):690–704. 10.4158/EP161718.RA [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Papathomas TG, Oudijk L, Persu A, Gill AJ, van Nederveen F, Tischler AS, et al. . SDHB/SDHA immunohistochemistry in pheochromocytomas and paragangliomas: A multicenter interobserver variation analysis using virtual microscopy: A Multinational Study of the European Network for the Study of Adrenal Tumors (ENS@T). Modern Pathol. 2015;28(6):807–21. 10.1038/modpathol.2015.41 [DOI] [PubMed] [Google Scholar]
- 66.Stenman A, Svahn F, Welander J, Gustavson B, Soderkvist P, Gimm O, et al. . Immunohistochemical NF1 analysis does not predict NF1 gene mutation status in pheochromocytoma. Endocrine Pathol. 2015;26(1):9–14. 10.1007/s12022-014-9348-1 [DOI] [PubMed] [Google Scholar]
- 67.Menara M, Oudijk L, Badoual C, Bertherat J, Lepoutre-Lussey C, Amar L, et al. . SDHD immunohistochemistry: A new tool to validate SDHx mutations in pheochromocytoma/paraganglioma. J Clin Endocrinol Metabol. 2015;100(2):E287–91. 10.1210/jc.2014-1870 [DOI] [PubMed] [Google Scholar]
- 68.Korpershoek E, Favier J, Gaal J, Burnichon N, van Gessel B, Oudijk L, et al. . SDHA immunohistochemistry detects germline SDHA gene mutations in apparently sporadic paragangliomas and pheochromocytomas. J Clin Endocrinol Metabol. 2011;96(9):E1472–6. 10.1210/jc.2011-1043 [DOI] [PubMed] [Google Scholar]
- 69.Udager AM, Magers MJ, Goerke DM, Vinco ML, Siddiqui J, Cao X, et al. . The utility of SDHB and FH immunohistochemistry in patients evaluated for hereditary paraganglioma-pheochromocytoma syndromes. Hum Pathol. 2018;71:47–54. 10.1016/j.humpath.2017.10.013 [DOI] [PubMed] [Google Scholar]