Abstract
Background
Maternal mortality is high in sub-Saharan Africa, and most deaths occur around childbirth. In Ethiopia, most births happen at home without skilled delivery attendants, and particularly, the least utilization of skilled delivery is recorded in Afar Region. The factors that influence this utilization are not well documented in the region where utilization has been low. The aim of this study was to determine the prevalence of utilization of institutional delivery and associated factors.
Methods
A cross-section study with pretested structural questionnaire was conducted from August 5 to September 27, 2015, among women who gave birth within 24 months preceding the survey. A multivariable logistic regression analysis was done to identify factors associated with utilization of institutional delivery.
Results
Out of the total 1842 women, only 339(18.4%) of mothers reported having delivered their youngest child at a health facility. Home delivery was preferred due to cultural norms, low-risk perception, and distance from a health facility. The odds of delivering in a health facility were higher for mothers who attended at least four antenatal visits during the index pregnancy (AOR=3.08,95%CI=1.91–4.96), those whose husbands were educated to secondary school (AOR= 1.86, 95% CI=1.34–2.60), and those that had at least secondary school level education themselves (AOR=1.52, 95% CI=1.03–2.23).
Conclusion
Utilization of institution delivery among Afar communities is very low, and less educated mothers are lagging behind. Women's education and full attendance to antenatal care can help increase utilization of skilled delivery services. Qualitative studies to identify socio-cultural barriers are also essential.
Introduction
Maternal and still births are intolerably high in sub-Saharan Africa mostly due to lack of access to maternal healthcare during pregnancy and delivery(1, 2). It is known that approximately 15% of all deliveries could involve potentially life-threatening complications(3). Ensuring utilization of institutional delivery services by skilled birth attendants is essential to prevent unnecessary maternal and newborn deaths(4, 5). The presence of skilled birth attendants, early recognition of complications, timely provision of care and referral when necessary can significantly reduce birth complications and reulting deaths(3, 6). However, a large number of deliveries in developing countries still occur at home without the assistance of skilled birth attendants(7, 8).
According to studies conducted in developing countries, better maternal education, better socioeconomic status, residence close to the nearest health service, urban residence and access to information are the common factors associated with increased utilization of skilled birth(9–11). Many African countries have made substantial efforts to expand the number of health facilities and reduced distance from home. Educational opportunities even for rural populations have been improved.
In Ethiopia, most deliveries take place at home assisted by untrained birth attendants; countrywide only 26.2 % of births occur in health facilities(12). The institutional delivery coverage is lowest in pastoralist communities of the country which consist of more than 10% of the total population(13). For example, in Afar Region, which is one of the pastoralist dominated regions of the country, utilization of institutional delivery services is significantly lower in comparison to the rural settled communities in neighboring states(5, 12, 13). According to the Ethiopian demographic health survey, institutional delivery in Afar Region was 14.7% while it was 56.93% in the neighboring predominantly agrarian region of Tigray(12).
Poor health facilities, inadequate staff, frequent mobility in search of grazing land, and cultural and traditional practices contribute to the low utilization of institutional delivery services in the pastoralist community, have been substantiated with few reports in the literature (14, 15). Therefore, it is imperative to investigate the factors associated with utilization of institutional delivery services in the Afar Region in order to design strategies to overcome barriers hindering predominately pastoralist women from giving birth in health facilities. Therefore, this study determined the prevalence of utilization of institutional delivery service and investigated the factors associated with utilization of the service among mothers in the predominantly pastoralist region of Afar in Ethiopia.
Methods
This study was conducted in Afar Regional State, one of the nine regions in Ethiopia. The study was carried out in 6 of the 32 districts: Mille, Dubti, Gawane, Amebra, Golina and Ewa districts. The majority of the population are pastoralists and Muslims. The study area has one regional hospital, three zonal hospitals, 14 health centers and 69 health posts. Health centers are the primary access point for delivery services. Health centers are equipped with basic delivery facilities and staffed with skilled delivery attendants. a total of 235 health workers in the facilities at the time of the study and cite 2016 Afar regional health bureau report.
A community-based cross-sectional study was conducted from August 5 to September 27, 2015. The study participants were all women who had resided in the study area for the past six months and gave birth in the last 24 months preceding the study.
The sample size for the study was calculated using single population proportion formula, which assumed institutional delivery service utilization of 6.8%(5), 95% confidence level, margin error of 2%, design effect of 3, and 10% non-response rate. Accordingly, the calculated sample size was 2009. A multistage sampling method was used to enroll study subjects. In the first stage, three out of five zones were selected randomly. Secondly, two districts per zone were randomly selected. Then, three kebeles per district (one urban and two rural) were randomly selected. Then, a census was conducted to identify eligible mothers. Those eligible mothers were proportionally allocated to each kebeles. Mothers were selected using simple random sampling methods based on the list obtained during the census.
Data were collected through face-to-face interviews using structured questionnaire adapted from the Ethiopian Demographic and Health Survey and other published literature. Initially, the questionnaire was prepared in English and then translated into Afar-afa (local language). The questionnaire consists of socio-demographic characteristics of respondents such as age of the mother, place of residence, ethnicity, religion, level of education, occupation of the mother and that of the husband and family size. It also consists of obstetrics history such as service utilization, number of antenatal visits, place for delivery, gravidity, parity, pervious history of obstructed labor and history of abortion, kind of assistance received during childbirth and information on distance between home and the nearby health facility, reasons for preferring place of delivery and decision making about the place for childbirth. The questionnaire was pretested in Awash District, not selected for the survey. Following the pretest, a debriefing session was conducted with field supervisors and data collectors to make the necessary fine-tuning of the questionnaire.
Data were collected by female nurses and health extension workers drawn from areas not included in the study. All data collectors were capable of conducting interviews in the local language (Afar-afa). Data collectors and supervisors were trained for three days by the principal investigator with emphasis on proper conduct of interviews, research ethics and data handling.
In some villages, interviews were conducted either during the morning or late afternoon hours in order to capture eligible pastoralist mothers while they were at their residence. In such areas, the survey team members had to stay overnight in the study villages in order to conduct interviews. The principal investigator and two supervisors checked the completeness of questionnaires on a daily basis.
Data entry and cleaning were done using EPI Data 3.1. Cleaned data were transferred onto SPSS version 20.0 for analysis. Both bivariate and multivariate logistic regression analyse were run to see the association of the independent variables with the outcome variable. Those variables with p-value < 0.05 in COR were included in the multivariate analysis. The crude and adjusted odds ratios were presented with their 95% confidence intervals. Ethical clearance for the study was obtained from the College of Health Sciences Ethical Review Committee at Mekelle University. Letters of permission to conduct the fieldwork was obtained from the Afar Regional Health Bureau and the local administration office in the study districts. Voluntary informed verbal consent was obtained from each study participant.
Results
A total of 1842 eligible women were successfully interviewed yielding a response rate of 91.7%. The majority of the respondents were rural residents [1244(67.5%)], Muslims [1734(94.1%)], married [1773(96.3%)], housewives [1493(81.1%)], illiterate [1143(62.1%)], pastoralist by occupation [1351(76.2%)] and Afar in ethnicity [1520(82.5%)]. The mean age of the mothers was 26.6 with SD ±5.5, range 15–48 years (Table 1).
Table 1.
Socio-Demographic characteristics of women and husband in six districts, Afar region stat, North East Ethiopia, August-September 2015, (n=1842)
| Characteristics | Frequency | % |
| Residence | ||
| Urban | 598 | 32.5 |
| Rural | 1244 | 67.5 |
| Current age of Mother's | ||
| 15–19 | 149 | 8.1 |
| 20–24 | 511 | 27.7 |
| 25–29 | 611 | 33.2 |
| 30–34 | 368 | 20.0 |
| 35–39 | 159 | 8.6 |
| >=40 | 44 | 2.4 |
| Mean±SD | 26.6 | (±5.5) |
| Marital status currently | ||
| Married | 1773 | 96.3 |
| Widowed | 28 | 1.5 |
| Divorced | 26 | 1.4 |
| Single | 15 | 0.8 |
| Ethnicity | ||
| Afar | 1520 | 82.5 |
| Amhara | 213 | 11.6 |
| Oromo | 47 | 2.6 |
| Tigre | 26 | 1.4 |
| Others(specify) | 36 | 2.0 |
| Religion | ||
| Muslim | 1734 | 94.1 |
| Orthodox | 81 | 4.4 |
| Others | 27 | 1.5 |
| Educational level of mothers | ||
| Not attend school | 1143 | 62.1 |
| Primary | 434 | 23.6 |
| Secondary | 244 | 13.2 |
| More than secondary | 21 | 1.1 |
| Educational level of Husbands=(1773) | ||
| Not attended school | 949 | 53.3 |
| Primary | 403 | 22.7 |
| Secondary | 218 | 12.3 |
| More than secondary | 203 | 11.4 |
| Occupation of Mothers | ||
| House wife | 1493 | 81.1 |
| Pastoralist | 182 | 9.9 |
| Gov employee | 82 | 4.5 |
| Others | 85 | 4.6 |
| Occupation of Husbands=(1773) | ||
| Pastoralist | 1351 | 76.2 |
| Merchant | 128 | 7.2 |
| Gov employee | 155 | 8.7 |
| Others | 139 | 7.8 |
Of the 1,842 mothers, 41.4% reported parity of 1–2, and 21.1% had 5 or more births. The majority of the study participants (72.1%) had 5 or more family members. Moreover, a substantial number of women (34.6%) did not attend ANC at all while only 17.5% of them attended the recommended four ANC during their last pregnancy. History of abortion was reported by 440(23.9%), and 371(20.1%) mothers reported history of obstructed labor (Table 2).
Table 2.
Obstetric characteristics of women in six districts, Afar region, Northeast Ethiopia August–September 2015 (n=1842)
| Characteristics | Frequency | Percent |
| Number of alive birth (parity) | ||
| 1–2 | 762 | 41.1 |
| 3–4 | 692 | 37.6 |
| >=5 | 388 | 21.1 |
| Family size | ||
| 1–2 | 94 | 5.1 |
| 3–4 | 419 | 22.7 |
| 5+ | 1329 | 72.1 |
| Obstructed labor history | ||
| No | 1471 | 79.9 |
| Yes | 371 | 20.1 |
| History of terminated pregnancy | ||
| No | 1402 | 76.1 |
| Yes | 440 | 23.9 |
| ANC visit during last pregnancy | ||
| No visit | 637 | 34.6 |
| 1st –3rd | 883 | 47..9 |
| 4th & above | 322 | 17.5 |
| Advice during ANC where to delivery | ||
| No | 710 | 58.9 |
| Yes | 495 | 41.1 |
| Place of last birth | ||
| At home | 1503 | 81.6 |
| Health facilities | 339 | 18.4 |
| Assistant During Delivery At Home (N=1503) | ||
| TBA | 1276 | 84.9 |
| Mothers | 163 | 10.8 |
| HEW | 40 | 2.7 |
| Neighbor | 24 (1.6) | 1.6 |
| preferred to attended for delivery | ||
| Male | 65 | 3.5 |
| Female | 1399 | 76.0 |
| Both male and female | 378 | 20.5 |
| Time taken to nearly delivery facility | ||
| <=30 mints | 1009 | 54.8 |
| >30 mints | 833 | 45.2 |
| Health facility provide delivery service at Kebeles (sub-district) | ||
| No | 756 | 41 |
| Yes | 1086 | 59 |
| Transportation to reach the health facility | ||
| Public Transpiration | 882 | 47.9 |
| Ambulance | 674 | 36.6 |
| Others | 286 | 15.5 |
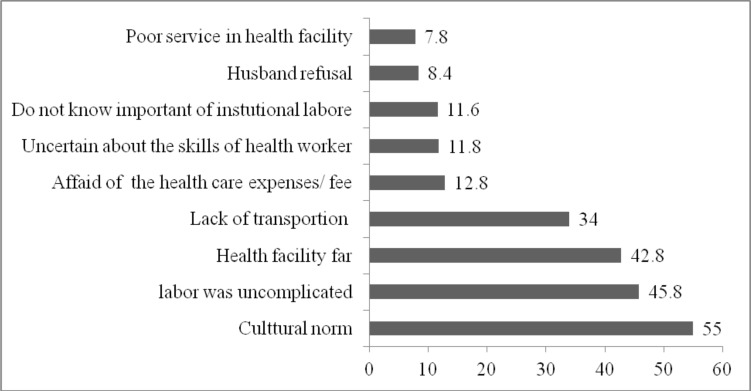
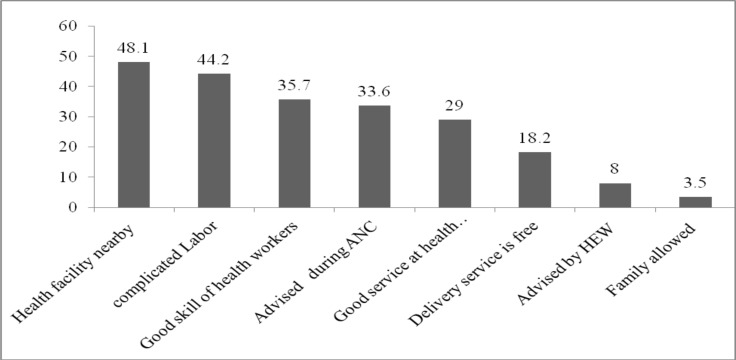
Among the reasons given for attending ANC services, 717(38.9%) wanted to know their health status, 390(32.4%) visited due to sickness, and 279(15.1%) attended to know the health status of their fetus (Figure 1). Overall, 339(18.4%, 95% CI: 16.5–20.1) mothers reported institutional delivery for the last birth. The major reasons for not utilizing delivery services included cultural norms, uncomplicated labor, long distance to health facility from home and lack of transportation (Figure 2).
Figure 1.
Reasons for attanding ANC among mother who gave birth at home in Afar region, NorthEast Ethiopia, 201 (The total is above 100% because of Multiple response).
Figure 2.
Reasons for home delivery among mother who gave birth at home in Afar region, NorthEast Ethiopia, 2015 (The total is above 100% because of Multiple response)
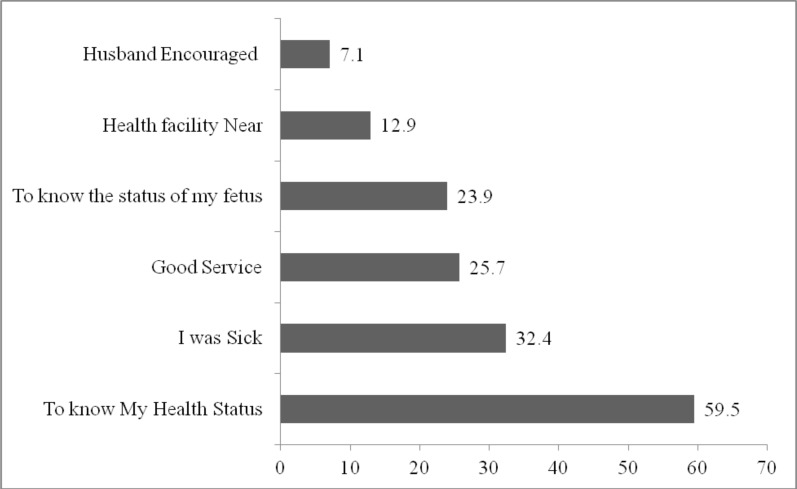
The major reasons for utilizing delivery services at the health facilities included the proximity of health facility, facing complicated labor, presence of reputable health workers, advice during ANC visit to deliver in a health facility and positive perception of services in the health facility (Figure 3).
Figure 3.
Reasons for health facility delivery among mother who gave birth in health facilities in Afar Region, Northeast Ethiopia, 2015 (The total is above 100% because of Multiple response).
The odds of institutional delivery was significantly higher among mothers who had secondary or above education as compared to mothers with no education (AOR =1.52; 95% CI= 1.03–2.23); mothers whose husbands attended primary school compared to those whose husbands had no formal education (AOR = 1.72, 95% CI = 1.23–2.41); mothers whose husbands attended secondary or above compared to those whose husbands had no formal education (AOR = 1.86, 95% CI =1.33–2.60). Likewise, mothers who were living within 30 minutes walking distance or less from a health facility compared to those who lived more than 30 minute distance were higher odds(AOR = 1.39, 95% CI= 1.05–1.84).Concerning to ANC visits, mothers who attended 4 or more ANC visits compared to those who did not have ANC visit during the pregnancy had higher odds (AOR = 3.08, 95% CI = 1.95–4.96). Regarding the sex preference, mothers who had no sex preference of service providers compared with those who prefer to be attended only by female service providers were higher odds (AOR = 1.76, 95% CI = 1.30–2.39). (Table 3)
Table 3.
Socio-Demographic and Obstetric factors affecting place of delivery among mothers having a child in the last 24 Months in Afar region, Northeast Ethiopia, 2015 (n=1842)
| Variable | Place of delivery | COR 95% CI | AOR 95% CI | |
| Health Facility N (%) |
Home N (%) |
|||
| Residence | ||||
| Urban | 141(23.6) | 457(76.4) | 1 | 1 |
| Rural | 198(15.9) | 1046(84.1) | 0.61(0.48–0.78)* | 1.26(0.92–1.74) |
| Currant age of Mother | ||||
| 15–19 | 41(27.5) | 108(72.5) | 2.11(1.25–3.56) * | 1.16(0.59–2.27) |
| 20–24 | 85(16.6) | 426(83.4) | 1.11(0.71–1.73) | 0.59(0.33–1.03) |
| 25–29 | 120(19.6) | 491(80.4) | 1.36(0.88–2.09) | 0.94(0.56–1.56) |
| 30–34 | 62(16.8) | 306(83.2) | 1.12(0.70–1.80) | 0.97(0.58–1.63) |
| >=35 | 31(15.3) | 172(84.1) | 1 | 1 |
| Ethnicity | ||||
| Afar ethnic | 252(16.6) | 1268(83.4) | 1 | 1 |
| Others | 87(27) | 235(73) | 1.86(1.41–2.47)* | 0.73(0.49–1.09) |
| Religion | ||||
| Muslim | 298(17.2) | 1436(82.6) | 0.34 (0.23–0.51) * | 0.50(0.30–0.83)* |
| Others Christian | 41(38) | 67(62) | 1 | 1 |
| Educational level of mothers | ||||
| Not attended | 150(13.1) | 993(86.9) | 1 | 1 |
| Primary | 104(24) | 330(76) | 2.09(1.58–2.76) * | 1.35(0.98–1.87) |
| Secondary and more | 85(32.1) | 180(67.9) | 3.13(2.29–4.26) * | 1.52(1.03–2.24)* |
| Occupation of Mothers | ||||
| House wife | 263(17.6) | 1230(82.4) | 0.77(0.58–1.02) | |
| Others | 76(21.8) | 273(78.2) | 1 | |
| Educational level of husband (n=1773) | ||||
| Not attended | 111(11.7) | 838(88.3) | 1 | 1 |
| Primary | 100(24.8) | 303(75.2) | 2.49(1.85–3.37) * | 1.72(1.23–2.41) * |
| Secondary and more | 118(28.0) | 303(72.0) | 2.94(2.20–3.93) * | 1.87(1.33–2.60) * |
| Occupation of Husbands (n=1773) | ||||
| Pastoralist | 229(17) | 1122(83) | 0.67(0.51–0.87)* | 1.02(0.75–1.38) |
| Others | 99(23.5) | 323(76.5) | 1 | 1 |
| Parity | ||||
| 1 | 605(79.4) | 157(20.6) | 1.68 (1.19–2.36)* | 1.02(0.61–1.69) |
| 2–4 | 562(81.2) | 130(18.8) | 1.50(1.05–2.12)* | 1.22(0.81–1.83) |
| ≥5 | 336(86.6) | 52(13.4) | 1 | 1 |
| Family size | ||||
| 1–2 | 11(11.7) | 83(88.3) | 0.64 (0.33–1.21) | 0.80(0.37–1.77) |
| 3–4 | 99(23.6 | 320(76.4) | 1.49(1.14–1.94) * | 1.22(.82–1.80) |
| 5+ | 229(17.2) | 1100(82.8) | 1 | 1 |
| Obstructed labor history | ||||
| No | 285(19.4) | 1186(80.6) | 1 | 1 |
| Yes | 54(19.4) | 317(85.4) | 0.71(0.52–0.97)* | 0.71(0.51–1.00) |
| Abortion/terminated pregnancy | ||||
| No | 277(19.8) | 1125(80.2) | 1 | 1 |
| Yes | 62(14.1) | 378(85.9) | 0.69(0.49–0.91)* | 0.83 (0.59–1.15) |
| Advices in ANC where to delivery | ||||
| No | 183(14.9) | 1045(85.1) | 1 | 1 |
| Yes | 156(25.4) | 458(74.6) | 1.95(1.53–2.47)* | 1.11(.83–1.49) |
| ANC visit during last pregnancy | ||||
| No visit | 46(7.2) | 591(92.8) | 1 | 1 |
| 1st–3rd | 196(22.2) | 687(77.8) | 3.67(2.61–5.15)* | 2.84(1.87–4.32)* |
| 4th & above | 97(30.1) | 225(69.9) | 5.54(3.78–8.12) * | 3.08(1.92–4.97)* |
| HF give delivery service at Kebele | ||||
| No | 92(12.2) | 664(87.8) | 1 | 1 |
| yes | 247(22.7) | 839(77.3) | 2.13(1.64–2.76)* | 1.03 (0.74–1.43) |
| Distance of HF for delivery | ||||
| <=30 minute | 224(22.2) | 785(77.8) | 1.78 (1.39–2.28)* | 1.39 (1.05–1.84)* |
| >30 minute | 115(13.8) | 718(13.8) | 1 | 1 |
| Preference for gender delivery | ||||
| Female | 209(14.9) | 1190(85.1) | 1 | 1 |
| Male | 16(24.6) | 49(75.4) | 1.86(1.04–3.33)* | 1.38(0.71–2.63) |
| Male and female | 114(30.2) | 264(69.8) | 2.46(1.89–3.20)* | 1.76(1.30–2.39)* |
HI=Health institute COR=Crude odds ratio AOR=Adjusted odds ratio ANC=Antenatal care HF=Health facility
Discussion
This community-based study revealed that only 18.4% of the mothers delivered at health facilities while the great majority (81.6 %) of them delivered at home. Educational status of the mother and husband, ANC visits during last pregnancy and distance from the nearest health facility were significantly associated with institutional delivery service utilization.
Although the rate of utilization of institutional delivery services we found was better than what was recorded five years back, it is still very low when compared to other areas in Ethiopia and other developing countries(12, 16–18). These large differences in utilization might be due to the differences in the context of studies as well as social and cultural variations. The observed association between ANC attendance and better chance of utilization of institutional delivery is in agreement with previous studies(12, 19, 20). Mothers with frequent ANC visits may have had better information on where to give birth which could have influenced their decision to give birth in health facilities.
Educational status of the husband is an important factor to allow women to utilize delivery service(19, 21). Women who have husbands with at least primary level education were more likely to give birth in health institutions. In addition, women's education is reported to have a positive effect on the use delivery services particularly if they attend secondary and above education(19, 22). The relationship between education and institutional delivery has been consistently reported in other similar studies conducted in Ethiopia (19, 21, 23, 24) and in other countries(24, 25). Thus, access to formal education would be important in improving the utilization of institutional delivery.
The Long distance between residence and health facilities was the most common reason for choosing home for delivery. This finding is in line with the finding of other similar studies conducted in Ethiopia and other developing countries(25–27). We observed that women who had to travel long distance were less likely to give birth at health facility. Thus, making health institution accessible would increase the chance of using the health facility delivery services.
In the study area, laboring women are not comfortable exposing their private parts to others especially to male health workers. As a result, 76% of respondents in this study preferred to attend the services by a female health worker. In the efforts to increase institutional delivery, due consideration needs to be given to socio-cultural issues. Assigning more female health workers in the delivery units can help increase the utilization of delivery service(28).
Due to cultural pressure, we expected that some women may not be comfortable responding to questions related to birthing events. To minimize that limitation and associated bias, data collectors were trained to conduct all interviews in privacy and to keep completed questionnaire in a strictly confidential manner. Thus, we believe the bias related to respondents' reluctance was minimal. Moreover, to minimize recall bias, we restricted questions only to the most recent birth. Despite these limitations, this study is one of the few large scale studies conducted in pastoralist communities.
It can be concluded that utilization of institutional delivery service is very low in the study setting. Attending the recommended number of ANC visits and education were significantly associated with institutional delivery. Proper dissemination of information regarding the availability of delivery services and removal of social and cultural barriers can help increase the utilization of delivery service by pastoralist women. Furthermore, conducting qualitative studies is necessary to explore the influence of culture, belief, traditional practices and seasonal mobility on the utilization of institutional delivery services.
References
- 1.World Health Organization, Unicef, author. Trends in maternal mortality: 1990–2015: estimates from WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: WHO; 2015. [Google Scholar]
- 2.Kinney MV, Kerber KJ, Black RE, et al. Sub-Saharan Africa's mothers, newborns, and children: where and why do they die? PLoS Med. 2010;7(6):e1000294. doi: 10.1371/journal.pmed.1000294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO, UNFPA, Unicef, AMDD, author. Monitoring emergency obstetric care: a handbook. Geneva: WHO; 2009. p. 152. [Google Scholar]
- 4.Prata N, Passano P, Rowen T, Bell S, Walsh J, Potts M. Where there are (few) skilled birth attendants. J Health Popul Nutr. 2011;29(2):81. doi: 10.3329/jhpn.v29i2.7812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CSA-Ethiopia, ICF, author. International: Ethiopia Demographic and Health Survey 2011. Ethiopia and Calverton, Maryland, USA: Central Statistical Agency of Ethiopia and ICF International Addis Ababa; 2012. [Google Scholar]
- 6.Lucas AO, Stoll BJ, Bale JR. Improving birth outcomes: meeting the challenge in the developing world. Washington (DC): National Academies Press; 2003. [PubMed] [Google Scholar]
- 7.United Nations, author. Millennium Development Goals Indicators Report. New Work: 2010. www.un.org/millenniumgoals/…/MDG%20Report%202010%20En%20r15%20-low. [Google Scholar]
- 8.Montagu D, Yamey G, Visconti A, Harding A, Yoong J. Where do poor women in developing countries give birth? A multi-country analysis of demographic and health survey data. PloS one. 2011;6(2):e17155. doi: 10.1371/journal.pone.0017155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baral YR, Lyons K, Skinner J, Van Teijlingen ER. Determinants of skilled birth attendants for delivery in Nepal. Kathmandu Univ Med J. 2010;8(31):325–332. doi: 10.3126/kumj.v8i3.6223. [DOI] [PubMed] [Google Scholar]
- 10.Bohren MA, Hunter EC, Munthe-Kaas HM, Souza JP, Vogel JP, Gülmezoglu AM. Facilitators and barriers to facility-based delivery in low-and middle-income countries: a qualitative evidencesynthesis. Reproductive health. 2014;11(1):71. doi: 10.1186/1742-4755-11-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yebyo H, Alemayehu M, Kahsay A. Why do women deliver at home? Multilevel modeling of Ethiopian National Demographic and Health Survey data. PLoS One. 2015;10(4):e0124718. doi: 10.1371/journal.pone.0124718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.CSA, ICF Demographic, ICF Ethiopia, author. Health Survey 2016: key Indicators Report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: 2016. [Google Scholar]
- 13.Federal Democratic Republic of Ethiopia Ministry of Health, author. Health Sector Development Program IV. 2010/11–2014/15.2010. www.nationalplanningcycles.org/…/ethiopia_2015.pdf.
- 14.Dubale T, Mariam DH. Determinants of conventional health service utilization among pastoralists in northeast Ethiopia. Ethiopian J Health Dev. 2007;21(2):142–147. [Google Scholar]
- 15.El Shiekh B, van der Kwaak A. Factors influencing the utilization of maternal health care services by nomads in Sudan. Pastoralism: Research, Policy and Practice. 2015;5:23. [Google Scholar]
- 16.Odo D, Shifti D. Institutional delivery service utilization and associated factors among child bearing age women in Goba Woreda, Ethiopia. J Gynecol Obstet. 2014;2(4):63–70. [Google Scholar]
- 17.Mpembeni RN, Killewo JZ, Leshabari MT, et al. Use pattern of maternal health services and determinants of skilled care during delivery in Southern Tanzania: implications for achievement of MDG-5 targets. BMC Pregnancy Childbirth. 2007;7:29. doi: 10.1186/1471-2393-7-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hazemba AN, Siziya S. Choice of place for childbirth: prevalence and correlates of utilization of health facilities in Chongwe district, Zambia. Medical journal of Zambia. 2008;35(2):53–57. [Google Scholar]
- 19.Teferra AS, Alemu FM, Woldeyohannes SM. Institutional delivery service utilization and associated factors among mothers who gave birth in the last 12 months in Sekela District, North West of Ethiopia: A community-based cross sectional study. BMC Pregnancy Childbirth. 2012;12:74. doi: 10.1186/1471-2393-12-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Choulagai B, Onta S, Subedi N, et al. Barriers to using skilled birth attendants' services in mid-and far-western Nepal: a cross-sectional study. BMC international health and human rights. 2013;13:49. doi: 10.1186/1472-698X-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Amano A, Gebeyehu A, Birhanu Z. Institutional delivery service utilization in Munisa Woreda, South East Ethiopia: a community based cross-sectional study. BMC pregnancy childbirth. 2012;12:105. doi: 10.1186/1471-2393-12-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abera M, Belachew T. Predictors of safe delivery service utilization in Arsi Zone, South-East Ethiopia. Ethiopian J Health Sci. 2011;21(3):95–106. [PMC free article] [PubMed] [Google Scholar]
- 23.Worku A, Jemal M, Gedefaw A. Institutional delivery service utilization in Woldia, Ethiopia. Science journal of public health. 2013;1(1):18–23. [Google Scholar]
- 24.Lwelamira J, Safari J. Choice of place for childbirth: prevalence and determinants of health facility delivery among women in Bahi District,Central Tanzania. Asian J Med Sci. 2012;4(3):105–112. [Google Scholar]
- 25.Jat TR, Ng N, San Sebastian M. Factors affecting the use of maternal health services in Madhya Pradesh state of India: a multilevel analysis. International journal for equity in health. 2011;10(1):59. doi: 10.1186/1475-9276-10-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Warren C. Care seeking for maternal health: challenges remain for poor women. Ethiopia J Health Dev. 2010;24(1):100–104. [Google Scholar]
- 27.Yousuf J, Ayalew M, Seid F. Maternal health beliefs, attitudes and practices among Ethiopian Afar. Exchange. 2011;1:12–13. [Google Scholar]
- 28.Nakambale A, Nzala S, Hazemba A. Factors Affecting Utilization of Skilled Birth Attendants by Women in Northern Zambia. Medical Journal of Zambia. 2014;41(2):86–94. [Google Scholar]