Abstract
Background
Early diagnosis and risk-stratification among infective endocarditis (IE) patients are limited by poor microbiological yield and inadequate characterization of vegetations. A simple tool that can predict adverse outcomes in the early phase of management is required.
Aim
To study the prognostic value of C-reactive protein (CRP) levels at admission and its role in predicting various clinical outcomes.
Methods
In a prospective study of consecutive IE patients diagnosed by modified Duke’s criteria, we measured the peak levels of CRP and erythrocyte sedimentation rate (ESR) in the first 3 days of admission and correlated it with in-hospital mortality, six-month mortality, embolic phenomena and the need for urgent surgery. Predefined laboratory-microbiological sampling protocols and antibiotic-initiation protocols were followed. Receiver-operating-characteristics curves were generated to identify a reliable cut-off for CRP in predicting various outcomes.
Results
Out of 101 patients who were treated, 85 patients had ‘definite’ IE. Blood cultures were positive in 55% (n = 39); and Staphylococcus species was the most common organism. Major complications occurred in 74.1% (n = 63) and in-hospital mortality was 32.9% (n = 28). Mean ESR and CRP levels were 102 ± 31 mm/h and 51 ± 20 mg/l, respectively. In multivariable analysis, high CRP levels were independently predictive of mortality, major complications, embolic events and need for urgent surgery. A CRP >40 mg/l predicted adverse outcomes with a sensitivity of 73% and specificity of 99%.
Conclusion
The study shows that baseline CRP level in the first 3 days of admission is a strong predictor of short term adverse outcomes in IE patients, and a useful marker for early risk stratification.
Keywords: Infective endocarditis, C-reactive protein, Prognostication, Valvular heart disease, Biomarker
1. Introduction
Infective endocarditis (IE) is a life-threatening infection of the cardiac valves or endocardium, with an incidence of 1.6–11.6 per 100,000 person-years varying from country to country.1 Despite the discernment of pathophysiology, refinement in diagnostic algorithms and advent of powerful antimicrobial and surgical therapies, the morbidity remains high.2, 3, 4 Data from developed5, 6, 7, 8, 9 as well as developing nations10, 11, 12, 13, 14 reveals that mortality rates of IE range from 15%-30% and complication rates exceed 70%. In the current era of rapid progress in structural interventional cardiology, such as transcatheter aortic and mitral valve prosthetic implantations, early IE detection and treatment are vital.15 Lack of a reliable clinical tool that helps in early risk-stratification may contribute to poor treatment outcomes.
Several clinico-laboratory characteristics that predict outcomes in IE have been identified. These include vegetation size greater than 10 mm, Staphylococcus aureus bacteremia, presentation with organ dysfunction or heart failure, prosthetic valve endocarditis and structural cardiac complications.5, 7, 16, 17, 18, 19, 20 The role of inflammatory biomarkers in prognosticating various cardiovascular illnesses has been an active research agenda in the last decade. Leukocytosis and hypoalbuminemia were previously identified as early predictors of in-hospital mortality in IE.7 In a retrospective study among 50 patients, Cornelissen et al.21 found leukocytosis, elevated C-reactive protein (CRP) levels and elevated procalcitonin as independent predictors of complications. Other predictors that have been studied and found useful include brain-type natriuretic peptide (BNP) levels,22 neutrophil-to-lymphocyte ratio,23 D-dimer levels24 and mean platelet volumes.25 Although serial monitoring of CRP levels is proven to have a role in predicting treatment outcomes, the value of CRP level at admission has been scantily studied.26, 27, 28 A biomarker that can help in early risk-stratification may guide decisions on treatment-aggressiveness.29 The aim of the study was to examine whether estimation of serum CRP levels at admission, serves as a predictor of averse outcomes in IE.
2. Methods
2.1. Patient selection
We conducted a prospective single-centre study to look into the role of baseline CRP level and other laboratory markers as independent predictors of outcomes in IE. All patients admitted with suspected IE to our tertiary-care centre, (which provides medical care to around 9.4 million people in North Kerala) from April 2012 to January 2015 were included. All episodes were personally overviewed by the authors and stratified as ‘definite’ and ‘possible’ IE according to the modified Duke criteria.30 Re-infection in the same patient was included only if the first episode was successfully and completely treated. Only patients with ‘definite’ IE were selected for the final statistical analysis. The study was approved by the institutional ethics committee. The conduct was in accordance with the Declaration of Helsinki and informed consent was taken from all patients.
2.2. Data collection
Demographic, clinical and laboratory data were prospectively collected by following a pre-defined protocol. All samples sent in the first week of admission were protocol-based, and changes were made only when indicated. A complete set of blood culture was taken at admission, on the fifth day and subsequently when deemed necessary. The antibiotic treatment-protocol was predefined and a five-day period of antibiotic-withhold was practised for stable patients with an intention to maximize microbiological yield. Stable patients were defined as those who were hemodynamically stable, absence of continuous fever >101 °F for three or more days, non-prosthetic valve endocarditis, no evidence of clinical heart failure (NYHA I/II only), absence of embolic phenomena, aortic root abscess or vegetation size greater than 10 mm at presentation. All other patients were considered unstable and were started on empirical antibiotics immediately after the first set of blood cultures. Details on sampling and antibiotic initiation protocols are provided in the Supplementary file. Indications for urgent cardiac surgery were progressive heart failure, cardiac abscess, high degree AV block, prosthetic valve dysfunction and progressively increasing vegetation size.17
The laboratory markers that were studied were total leukocyte count, erythrocyte sedimentation rate (ESR), CRP and serum albumin. These were sampled on the first day and the third day of admission. The average value was taken for analysis. In case of a gross discrepancy in values between the first two samples, a third sample was sent and the odd value excluded. ESR was estimated by the Westergren’s method (Na citrate anticoagulated specimen). CRP was measured using a commercially available latex-enhanced immuno-turbidimetric assay (BIOLIS 24i system, Agappe diagnostics, Tokyo-bioki, Japan). The normal value was <3 mg/l. Other parameters that were studied included rheumatoid factor, serum creatinine, anemia, albumin levels, serum sodium levels, presence of diabetes mellitus, history of smoking/alcohol/drug addiction, fever duration and staphylococcal infection. These parameters were adjusted for in the final analysis. All measurements were charted by a duty-staff who had no knowledge of the microbiological yield, vegetation characteristics and further patient outcome.
2.3. Echocardiography
A comprehensive transthoracic echocardiography (TTE) was done on the first day of admission in all patients. Transesophageal echocardiography(TEE) was proposed for all patients. Standard definitions put forward by prior observational studies were used for documenting new-onset significant regurgitation, prosthetic valve dysfunction, vegetation dimensions and cardiac abscess formation.7, 16 Semi-quantitative analysis was done to identify moderate and severe valvular regurgitation.
2.4. Clinical outcome
Primary outcomes included in-hospital mortality and the composite of major complications. Major complications included acute kidney injury (excluding antibiotic related transient rise in serum creatinine), neuro-embolic events (cerebral abscess and septic embolic infarcts), non-cerebral embolic phenomena (septic pulmonary emboli, limb ischemia, visceral organ and cutaneous emboli) and cardiac complications (heart failure, abscess, serious new-onset arrhythmia or pericardial tamponade). Patients were followed up through six months with two-monthly outpatient visits or by telephonic interview. Secondary outcomes included the composite of embolic events, need for urgent surgery and six-month mortality.
2.5. Data analysis
Only patients with ‘definite’ IE were considered for the final analysis. Continuous data were summarized as mean along with its standard deviation. Influence of baseline parameters on mortality were assessed by using the chi-square test for categorical variables and the Student’s t-test for continuous variables. The relative risk and its 95% confidence interval were calculated for predictors of complications and in-hospital mortality. To identify reliable cut-offs for CRP we constructed a receiver-operating-characteristics (ROC) curve and determined the area under the curve (AUC). Baseline parameters that were significantly associated with the primary outcome in the univariate analysis were included in a multivariable logistic regression model to identify independent predictors. Kaplan-Meier survival curves were generated to determine the impact of CRP cut-off level on mortality. All statistical tests were 2-tailed; p value < 0.05 was considered as significant. We used SPSS 16.0 software for all statistical analyses.
3. Results
3.1. Epidemiology and presentation
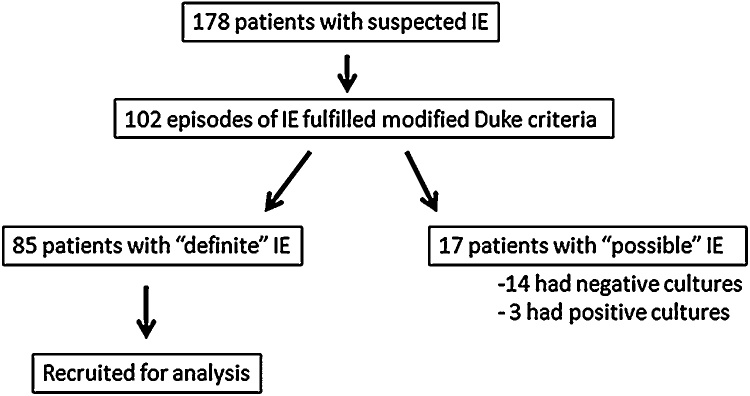
From April 2012 to January 2015, 178 patients were admitted with a suspicion of IE. There were 102 episodes of clinically confirmed IE among 101 patients, of which 85 were ‘definite’ IE and 17 were ‘possible’ IE (Fig. 1). The mean age of the population was 43.4 ± 16.7 years. Males comprised 70 out of the 101 patients (69.3%). The median duration of fever was 21 days (range 7–180 days). 46 patients had fever duration less than 4 weeks (acute presentation). NYHA class III symptoms were reported at presentation for 41 patients (40.2%). The baseline laboratory characteristics are listed in Table 1. A definite vegetation was identified in 87.2% (n = 88) IE episodes. Seven patients were diagnosed with cardiac abscess and one patient had a fistula to right atrium. Progressive or new onset significant valvar regurgitation was found in 58 patients.
Fig. 1.
Flowchart depicting recruitment of infective endocarditis patients prospectively.
Table 1.
Baseline laboratory parameters among patients with infective endocarditis.
| Laboratory parameter | Frequency, n (%)/Mean (SD) |
|---|---|
| Haemoglobin (g/dl), mean(SD) | 10 (2.1) |
| Total leukocyte count (/μl), mean (SD) | 14,139 (6144.9) |
| Erythrocyte sedimentation ratio (mm/h), mean (SD) | 100.5 (28) |
| C- reactive protein (mg/dl), mean (SD) | 47.3 (32) |
| Serum creatinine (mg/dl), mean (SD) | 0.9 (0.4, 4.4) |
| Serum albumin (mg/dl), mean (SD) | 3.34 (0.57) |
| Serum sodium (meq/l), mean (SD) | 133.3 (6.1) |
| Urinary casts, n (%) | 21 (20.6%) |
| Rheumatoid factor (N = 78), n (%) | 16 (20.5%) |
The empirical regimen that was followed was parenteral Ceftriaxone and Gentamicin. Vancomycin was used when Staphylococcus. aureus was suspected. Rifampicin was added for all prosthetic valve endocarditis. Once the culture sensitivities were obtained, antibiotics were modified accordingly. Broad spectrum antibiotics such as Meropenem, Piperacillin-Tazobactam, Colistin and antifungals were added for refractory sepsis and non-response to the initially planned empirical regimen.
3.2. Predisposing heart disease and risk factors
Rheumatic heart disease (RHD) was the most common diagnosis in 38.2% patients (n = 39). The rest were mitral valve prolapse (18.6%), bicuspid aortic valve (2.9%), tetralogy of Fallot (3.9%), patent ductus arteriosus (1.9%), ventricular septal defect (2.9%), degenerative aortic stenosis (1.9%), coronary-cameral fistula (0.9%), Ebstein’s anomaly (0.9%), ischemic heart disease, dilated cardiomyopathy, hypertrophic obstructive cardiomyopathy and Marfan’s syndrome. In 21.6% of patients (n = 22), there was no underlying structural heart disease. Out of all cases, 81.4% (n = 83) cases involved native heart valves and 18.6% (n = 19) were prosthetic valve endocarditis (PVE). Among the latter, 3 patients had significant prosthetic valve dysfunction. The mitral position was involved in 49% (n = 50), followed by the aortic in 27.4% (n = 28). The rest were tricuspid (n = 5), pulmonary (n = 9) and other endocardial sites (n = 4).
A history of chronic smoking was present for 26 patients (25.5%) and 13 patients (12.7%) were chronic alcoholics. Other associations were diabetes mellitus in 10.8% (n = 11), chronic kidney disease in 4.9% (n = 5), coronary artery disease in 1.9% (n = 2), drug-induced immuno-suppression in 1.9% (n = 2) and intravenous drug abuse in 1.9% (n = 2).
3.3. Microbiology
The sampling protocol was successfully followed for all patients. Causative organisms were isolated in 54 episodes (52.9%). Staphylococcus aureus was the most common isolate (in 28 patients). Among these, 14 patients had methicillin-resistant Staphylococcus aureus (MRSA) infection. Other isolates included group viridans Streptococci (20.4%), coagulase-negative staphylococci (11.3%), beta-hemolytic streptococci (2 patients), Acinetobacter species (2 patients), Pseudomonas species (1 patient), Enterococcus faecalis (2 patients) and Enterobacter species (2 patients).
3.4. Major complications, mortality and in-hospital course
Eighty-five patients with ‘definite’ IE were analyzed to identify predictors of treatment outcomes. The percentages of various categorical variables that were considered for the univariable analysis are listed in Table 2. The descriptive characteristics that were considered for univariable analysis are provided in Table 3.
Table 2.
Frequencies of various categorical variables among 85 episodes of definite infective endocarditis.a
| Baseline parameter | Frequency, n (%) |
|---|---|
| Thrombocytopeniab | 12 (14.1%) |
| Hypoalbuminemiab (N = 83) | 52 (62.7%) |
| Hyponatremiab | 54 (63.5%) |
| Diabetes mellitus | 10 (11.8%) |
| Smokerc | 22 (25.9%) |
| Vegetation size >10 mm | 58 (73.4%) |
| Aortic valve involvement | 27 (34.2%) |
| Mitral valve involvement | 46 (57.5%) |
| New-onset significant valvular dysfunctiond | 60 (70.6%) |
| Cardiac abscess | 8 (9.4%) |
| Blood culture positive | 51 (60%) |
| Prosthetic valve involvement | 16 (18.8%) |
| Staphylococcus aureus infection (N = 54) | 26 (48.1%) |
| NYHA class I/II | 47 (55.3%) |
| NYHA class III/IV | 38 (44.7%) |
Categorical variables are expressed as number (percentage) and the total sample size is N = 85. For hypoalbuminemia data is available for 83 patients. The percentage of S. aureus infection is calculated out of 54 episodes with a positive blood culture.
Thrombocytopenia is defined as a platelet count less than 1,00,000/μl; Hyponatremia is defined as S. sodium <135 meq/l; hypoalbuminemia is defined as S. albumin <3.5 mg/dl.
A smoker is defined as a person with a lifetime history of smoking >100 cigarettes.
New-onset significant valvular dysfunction is defined as a any new detection of moderate or more valvular regurgitation or any form of prosthetic valve dysfunction.
Table 3.
Mean and standard deviations of descriptive variables among 85 episodes of definite infective endocarditis.
| Baseline parameter | Mean (SD) |
|---|---|
| Age (years) | 43.7 (16.3) |
| Fever duration (days) | 34.3 (33.5) |
| Haemoglobin (g/dl) | 9.8 (2.2) |
| Total leukocyte count (per μl) | 14,219.4 (5890) |
| Erythrocyte sedimentation ratio (mm/h) | 99.7 (29.1) |
| C-reactive protein (mg/l) | 47.5 (30.3) |
| Serum creatinine (mg/dl) | 1.4 (1.6) |
| Serum albumin (mg/dl) | 3.2 (0.6) |
| Serum sodium (meq/l) | 132 (5.9) |
Major complications occurred in 63 patients (74.1%). These included cardiac complications in 37 patients (43.5%), renal failure in 21 patients (24.7%), neuro-embolic complications in 26 (30.6%) and peripheral embolic complications in 39 patients (45.9%). Cerebral abscess was seen in 10 patients, while 16 patients had septic infarcts without abscess formation. The composite of embolic phenomena (neurological and peripheral) occurred in 46 patients (54.1%). The in-hospital mortality was 32.9% (n = 28) and 6-month mortality was 36.5% (n = 31). Urgent cardiac surgery was indicated in 36 patients (42.4%), but was done in only 14 cases. The most common reasons cited for deferring surgery in the others were hemodynamic instability, severe sepsis and lack of consent.
3.5. Predictors of the composite of major complications
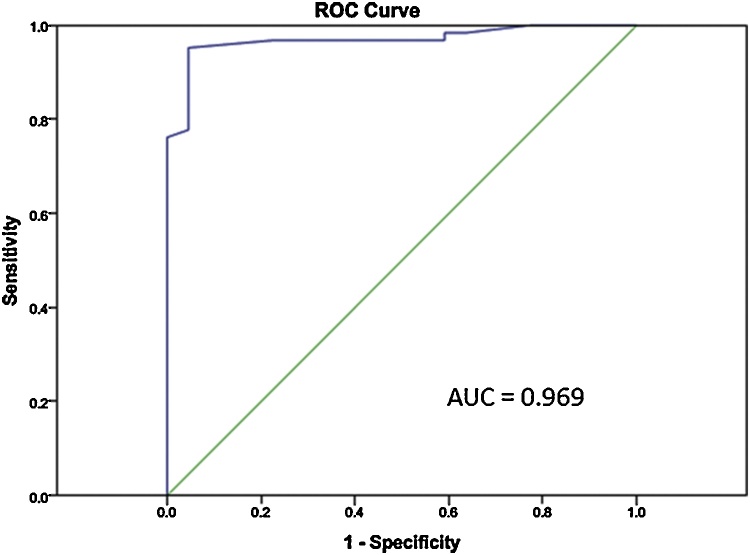
In the univariable analysis; high CRP (p < 0.001), higher leukocyte counts (p = 0.031), lower serum albumin (p = 0.032), lower serum sodium (p = 0.002), NYHA class III or IV (p = 0.016), hyponatremia (p < 0.001), vegetation >10 mm (p = 0.018), leukocytosis (p = 0.022), and serum creatinine >1.4 mg/dl (p = 0.014) were statistically significant predictors of adverse outcomes. ROC curves were generated for CRP levels, and a cut-off of 40 mg/l was found to have a sensitivity of 76% and specificity of 99% with an AUC of 0.969 ± 0.018 (p < 0.001) (Fig. 2). CRP >40 mg/l was significantly predictive of major complications (p < 0.001) (Table 4). The mean ESR among patients who had an adverse event (100 ± 31 mm/h) did not differ significantly from those without events (96.7 ± 25 mm/h; p value = 0.61).
Fig. 2.
Receiver operating characteristics curve generated for C-reactive protein against the composite of major complications among 85 patients with IE.
Table 4.
Association of baseline patient characteristics with the composite of major complications by univariable analysis.a
| Parameter | Major complications (N = 63) | No complications (N = 22) | Relative risk | 95% confidence interval | P value |
|---|---|---|---|---|---|
| Age >40 years | 37 (58.7%) | 15 (68.2%) | 0.90 | 0.70–1.16 | 0.434 |
| NYHA III/IV | 33 (52.4%) | 5 (22.7%) | 1.36 | 1.06–1.74 | 0.016 |
| Thrombocytopeniab | 8 (12.7%) | 4 (18.2%) | 0.89 | 0.58–1.35 | 0.525 |
| Hypoalbuminemiab | 42 (66.7%) | 10 (45.5%) | 1.25 | 0.93–1.68 | 0.099 |
| Hyponatremiab | 47 (74.6%) | 7 (31.8%) | 1.69 | 1.18–2.41 | <0.001 |
| Diabetes mellitus | 8 (12.7%) | 2 (9.1%) | 1.09 | 0.78–1.53 | 0.651 |
| Smokerc | 17 (27%) | 5 (22.7%) | 1.06 | 0.81–1.39 | 0.695 |
| Vegetation >10 mm | 46 (73.1%) | 12 (54.5%) | 1.51 | 0.99–2.32 | 0.018 |
| Aortic valve involvement | 22 (34.9%) | 5 (22.7%) | 1.21 | 0.93–1.57 | 0.183 |
| Mitral valve involvement | 30 (47.6%) | 16 (72.7%) | 0.79 | 0.61–1.03 | 0.090 |
| Significant valve dysfunctiond | 44 (69.8%) | 16 (72.7%) | 0.96 | 0.74–1.26 | 0.798 |
| Prosthetic valve IE | 12 (19.1%) | 4 (18.2%) | 1.01 | 0.74–1.39 | 0.929 |
| S. aureus infection | 18 (28.6%) | 8 (36.4%) | 0.91 | 0.68–1.22 | 0.495 |
| Moderate or severe anemiac | 37 (58.7%) | 11 (50%) | 1.10 | 0.85–1.42 | 0.477 |
| Leukocytosis | 48 (76.2%) | 11 (50%) | 1.41 | 0.99–2.0 | 0.022 |
| Serum creatinine >1.4 mg/dl | 18 (28.6%) | 1 (4.5%) | 1.39 | 1.14–1.69 | 0.020 |
| C-reactive protein >40 mg/l | 49 (77.8%) | 1 (4.5%) | 2.45 | 1.63–3.68 | <0.001 |
Statistical analysis was done using the chi square test.
Thrombocytopenia is defined as a platelet count less than 1,00,000/μl; Hyponatremia is defined as S. sodium <135 meq/l; hypoalbuminemia is defined as S. albumin <3.5 mg/dl; moderate to severe anemia is defined as Hb <10 g/dl.
A smoker is defined as a person with a lifetime history of smoking >100 cigarettes.
New-onset significant valvular dysfunction is defined as any new detection of moderate or more valvular regurgitation or any form of prosthetic valve dysfunction.
In multivariable analysis CRP >40 mg/l, with an odds ratio of 9.62 (95% CI 2.44–37.88, p = 0.001), came out as the single independent predictor of major complications (Table 5).
Table 5.
Multivariable analysis for various baseline parameters that predict the composite of major complications among 85 infective endocarditis patients.
| Baseline characteristic | Odds ratio | 95% confidence interval | P value |
|---|---|---|---|
| NYHA III/IV | 0.39 | 0.1–1.53 | 0.174 |
| Leukocytosis | 2.02 | 0.50–8.11 | 0.322 |
| Hypoalbuminemia | 1.00 | 0.25–4.02 | 0.995 |
| Hyponatremia | 0.97 | 0.26–3.60 | 0.961 |
| Vegetation size >10 mm | 3.98 | 0.87–18.09 | 0.074 |
| Aortic valve involvement | 0.30 | 0.07–1.33 | 0.112 |
| Serum creatinine >1.4 mg/dl | 2.1 | 0.32–6.78 | 0.356 |
| C-reactive protein >40 mg/l | 9.62 | 2.44–37.88 | 0.001 |
3.6. Predictors of in-hospital mortality
In the univariable analysis; age >40 years (p = 0.02), hypoalbuminemia (p = 0.014), moderate to severe anemia (p = 0.004), hyponatremia (p = 0.018), NYHA class III/IV (p < 0.001) and CRP >40 mg/l (p < 0.001) predicted mortality. Multivariable analysis identified NYHA class III/IV (p = 0.033), hemoglobin <10 g/dl (p = 0.027), CRP >40 mg/l (p = 0.021) and age >40 years (p = 0.029) as independently predictors of in-hospital mortality (Table 6).
Table 6.
Multivariable analysis for various baseline parameters that predict in-hospital mortality.
| Baseline characteristic | Odds ratio | 95% confidence interval | P value |
|---|---|---|---|
| Age >40years | 6.28 | 1.20–32.93 | 0.030 |
| NYHA III/IV | 5.82 | 1.15–29.72 | 0.033 |
| Hypoalbuminemia | 2.73 | 0.44–17.19 | 0.285 |
| Hyponatremia | 1.50 | 0.26–8.69 | 0.652 |
| Vegetation size >10 mm | 0.71 | 0.09–5.85 | 0.747 |
| Aortic valve involvement | 2.38 | 0.43–13.07 | 0.317 |
| Moderate or severe anemia | 7.61 | 1.26–46.14 | 0.027 |
| Serum creatinine >1.4 mg/dl | 0.91 | 0.15–5.69 | 0.924 |
| C-reactive protein >40 mg/l | 8.29 | 1.39–49.41 | 0.021 |
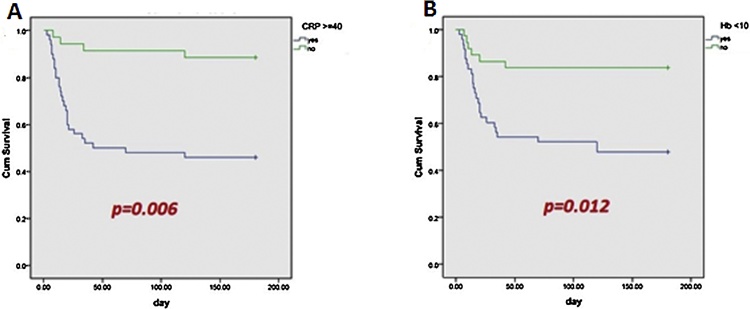
3.7. Predictors of 6-month mortality
In the multivariable analysis NYHA class III/IV (odds ratio- 4.60; 95% CI 1.57–13.50, p = 0.006), hemoglobin <10 mg/l (odds ratio- 4.2; 95% CI 1.37–12.86, p = 0.012) and CRP >40 mg/l (odds ratio- 5.55; 95% CI 1.65–18.72, p = 0.006) were the only independent predictors of six-month mortality (Fig. 3).
Fig. 3.
Kaplan-Meier survival curve analysis showing C-reactive protein >40 mg/l and hemoglobin <10 g/dl as predictors for six-month mortality.
3.8. Predictors of embolic phenomena and need for urgent surgery
The composite of embolic phenomena (neurological and peripheral) occurred in 46 patients (54.1%). In the multivariable analysis, CRP >40 mg/l (odd risk- 7.42; 95% CI 2.06–26.72, p = 0.002) was the single independent predictor of embolic phenomena. Vegetation size >10 mm (p = 0.09) and the presence of aortic valve vegetation (p = 0.07) showed a trend towards statistical significance.
CRP >40 mg/l was the only independent predictor (odds ratio- 3.61; 95% CI 1.11–11.81, p = 0.033) of the need for urgent surgery (n = 36).
4. Discussion
Our study is the largest single-centre prospective analysis in Asia, which examined the prognostic value of baseline inflammatory markers among patients with IE. The study showed that CRP level at admission was the most powerful predictor of poor outcomes, and this was independent of the age, culture-yield, clinical presentation, other laboratory markers or valvular involvement. These results are particularly relevant in developing nations where there is a high prevalence of culture-negative endocarditis (50–60%) and where routine transesophageal echocardiographic (TEE) imaging is often unavailable for adequate characterization of vegetations; and there-by affecting prognostication. Baseline risk-stratification among IE patients has hence been a matter of constant dilemma.11, 13, 34 This often adversely affects decision-making regarding early referral, surgical management and in turn treatment outcomes.
In the present study, CRP independently predicted in-hospital mortality, composite of major complications, embolic phenomena and the need for urgent surgery. In a previous prospective analysis, Heiro et al. had evaluated the prognostic role of monitoring CRP levels during hospitalization among 134 IE patients and found it to be useful.28 In another retrospective analysis of a Finnish population, the value of high CRP levels in predicting short term and one-year mortality was noted.35 In the present study, the prognostic value of baseline CRP even superseded vegetation size and NYHA class. A CRP level greater than 40 mg/l predicted a nearly ten times higher risk of a major complication and nearly eight times higher risk of in-hospital mortality. ESR, on the other hand, was of no prognostic significance and this had been shown repeatedly in previous studies also.21, 26, 28 The non-specific variations of ESR associated with anemia, renal failure and elderly may be the reason why it is often a poor guide to treatment. Anemia (hemoglobin <10 g/dl) was noted to be another early predictor of higher in-hospital and 6-month mortality. Hyponatremia, hypoalbuminemia, leukocytosis, raised serum creatinine levels and vegetation size >10 mm at admission showed only a trend for predicting adverse events; probably explained by the small sample size.
In-hospital complication rates and mortality of IE remain high (around 74% and 33%, respectively), despite protocol-based management. This echoes the event-rates of previous studies conducted in developing nations.10, 11, 36, 37, 38 Our centre being a tertiary-care centre catering to a large population, selection bias of a sicker cohort may have come into play. Previous studies have shown that adjudication towards an early surgical strategy significantly improved outcomes.33 Data from the ICE-PCS also showed that patients with heart failure for whom surgery was indicated had a mortality of 45% when treated medically, versus 21% with early surgery.17 In this study, even though almost 40% had an indication, less than 19% underwent urgent surgery (mostly because of the reluctance from the surgical team to operate on unstable patients and lack of consent). It was noted that patients who underwent surgery survived more than those for whom surgery was not done; which however could be due to the selection bias involved. Interestingly, our study showed that a baseline CRP >40 mg/l significantly predicted the need for urgent surgery. A previous analysis had however reported CRP to have no value in predicting need for urgent cardiac surgery at any point during hospitalization.28 This is an area for further research and a prospective analysis looking into the role of CRP-guided allotment to early surgery may be warranted.
As seen in prior studies from endemic nations, RHD is still the most common etiology for IE. This justifies a separate analysis of various inflammatory markers in this background. However, a ‘western’ shift in epidemiology is noted in the form of high prevalence of mitral valve prolapse and patients with no previous structural heart disease. The mean age of the population at risk has also increased in comparison to previous epidemiological studies from India. Still, the heterogeneous background of risk factors among various tertiary centres make such comparisons difficult.11, 20
The study exposes the limitations in diagnosis and early risk-stratification of patients in the developing countries. Despite following strict protocol-based microbiological techniques, the culture-yield was only around 53%. This concurs with previous data from developing nations. The most important reason identified was partial outpatient antibiotic treatment without appropriate evaluation. Among the 102 episodes, despite all patients having clinically definite IE by consensus, the modified Duke criteria identified only 85 ‘definite’ IE. Previously also it has been reported that further modifications of the Duke criteria, like the St Thomas’ modification (which includes CRP), may be necessary to improve sensitivity, especially in countries with a high incidence of culture-negative endocarditis.31, 32
5. Limitations
The study has a few limitations. The small sample size and the inherent selection bias may have skewed the outcome to represent a population at high risk. This fact cannot however be confirmed as most prospective studies on IE are feasible only in high-volume referral centres. In our study, serial measurements of CRP were not analyzed. The role of changing levels of CRP as a guide to favorable outcomes had already been proven in several previous studies. The focus of the present analysis was the prognostic value of baseline CRP levels. We did not use routine serological testing for culture-negative endocarditis. However, these are rarely tested in the real-world scenario in developing countries, and hence may not have significant implications.
6. Conclusion
IE management accounts for one of the most challenging critical-care decisions faced by physicians and cardiologists. Limited sensitivity of the Duke criteria, culture-negative endocarditis and difficult characterization of vegetations are major obstacles in early risk-stratification. In this study, baseline CRP in the first 3 days of admission was identified as an independent and strong predictor of complications, in-hospital mortality and six-month mortality. A CRP >40 mg/l showed a sensitivity of 73% and specificity of 99% for predicting a major complication. Large-scale multi-centre prospective studies are needed, to further define the prognostic role of CRP and help its integration into diagnostic as well as risk-stratification algorithms for IE.
Key Questions of the Study
1) What is already known about this subject?
IE is a life-threatening infection of the cardiac valves and/or endocardium with high morbidity and mortality rates. Early risk-stratification is vital to decide on management strategies.
2) What does this study add?
The study confirms and emphasizes the role of baseline CRP levels after admission as a strong predictor of adverse outcomes. In endemic countries like India, this finding can help guide early risk-stratification.
3) How might this impact on clinical practice?
Developing countries like India face limitations of poor culture yield and lack of wide access to advanced imaging. A cheap and widely available biomarker like CRP, will be valuable in adjudicating patients for early aggressive management (such as urgent cardiac surgery) versus standard care.
Sampling Protocol for Diagnosis of Infective Endocarditis (MCH, Calicut)
-
1.
2 sets of blood cultures should be taken (1 set includes 3 * 10 ml of blood in at least 2, and preferably 3, BACTEC bottles)
-
2.
BACTEC bottles are issued from the microbiology department
-
3.
1st set (includes 3 bottles) should be taken immediately/earliest possible after admission- each bottle with 10 ml sample preferably 30 min apart by the “standard technique” mentioned below.
-
4.
All ‘stable’ patients (as defined in methodology) must be observed in-hospital by 6-hourly fever charting for the 1st 4 days.
-
5.
The 2nd set should be sent on the 5th day using the same technique and then empirical antibiotics maybe started (provided clinical diagnosis has been established).
-
6.
If even after the 1st week of microbiological analysis, the patient is being treated as BCN-IE, repeat cultures maybe sent in the 2nd or 3rd week.
-
7.
In unstable patients (as in methodology/as deemed by Unit Chief), blood cultures should be taken immediately after admission by the duty cardiologist and empirical antibiotics started.
-
8.
STANDARD TECHNIQUE: Proper explanation and informed consent should be taken first. Prior to the procedure the exterior of the BACTEC culture bottle is wiped with a spirit swab thoroughly. Following strict aseptic precautions (hand washing, sterile gloves etc.) the patient’s cubital fossa is prepared with chlorhexidine solution. The bottle cap is then opened and the rubber top is cleaned with a spirit swab. After allowing sufficient time for the spirit from local skin site and rubber top to vaporize, the sample is withdrawn in a 10 ml syringe and transferred to the BACTEC bottle (without forceful injection). Subsequent 2 samples should be taken in a similar manner through separate punctures.
Conflict of interest
None.
Contributor Information
Sandeep Mohanan, Email: stg222@gmail.com.
Rajesh Gopalan Nair, Email: drrajeshgnair@gmail.com.
Haridasan Vellani, Email: haridasanv@yahoo.com.
Sajeev C G, Email: sajeev.cg@gmail.com.
Biju George, Email: bijugeorge1@gmail.com.
Krishnan M N, Email: drmnkrishnan@gmail.com.
References
- 1.Bin Abdulhak A.A., Baddour L.M., Erwin P.J. Global and regional burden of infective endocarditis, 1990–2010: a systematic review of the literature. Glob Heart. 2014;9:131–143. doi: 10.1016/j.gheart.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Dayer M.J., Jones S., Prendergast B. Incidence of infective endocarditis in England, 2000–13: a secular trend, interrupted time-series analysis. Lancet. 2015;385(9974):1219–1228. doi: 10.1016/S0140-6736(14)62007-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moges T., Gedlu E., Isaakidis P. Infective endocarditis in Ethiopian children: a hospital based review of cases in Addis Ababa. Pan Afr Med J. 2015;20:75. doi: 10.11604/pamj.2015.20.75.4696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fedeli U., Schievano E., Buonfrate D. Increasing incidence and mortality of infective endocarditis: a population-based study through a record-linkage system. BMC Infect Dis. 2011;11:48. doi: 10.1186/1471-2334-11-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Netzer R.O., Zollinger E., Seiler C. Infective endocarditis: clinical spectrum, presentation and outcome: an analysis of 212 cases 1980–1995. Heart. 2000;84:25–30. doi: 10.1136/heart.84.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mansur A.J., Grinberg M., Cardoso R.H. Determinants of prognosis in 300 episodes of infective endocarditis. Thorac Cardiovasc Surg. 1996;44:2–10. doi: 10.1055/s-2007-1011974. [DOI] [PubMed] [Google Scholar]
- 7.Wallace S.M., Walton B.I., Kharbanda R.K. Mortality from infective endocarditis: clinical predictors of outcome. Heart. 2002;88:53–60. doi: 10.1136/heart.88.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chu V.H., Cabell C.H., Benjamin D.K., Jr Early predictors of in-hospital death in infective endocarditis. Circulation. 2004;109:1745–1749. doi: 10.1161/01.CIR.0000124719.61827.7F. [DOI] [PubMed] [Google Scholar]
- 9.Mirabel M., André R., Barsoum Mikhaïl P. Infective endocarditis in the Pacific: clinical characteristics, treatment and long-term outcomes. Open Heart. 2015;2:e000183. doi: 10.1136/openhrt-2014-000183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garg N., Kandpal B., Garg N. Characteristics of infective endocarditis in a developing country – clinical profile and outcome in 192 Indian patients, 1992–2001. Int J Cardiol. 2005;98:253–260. doi: 10.1016/j.ijcard.2003.10.043. [DOI] [PubMed] [Google Scholar]
- 11.Math R.S., Sharma G., Kothari S.S. Prospective study of infective endocarditis from a developing country. Am Heart J. 2011;162:633–638. doi: 10.1016/j.ahj.2011.07.014. [DOI] [PubMed] [Google Scholar]
- 12.Jain S.R., Prajapati J.S., Phasalkar M.A. Clinical spectrum of infective endocarditis in a tertiary care centre in western India: a prospective study. Int J Clin Med. 2014;5:177–187. [Google Scholar]
- 13.Watt G., Pachirat O., Baggett H.C. Infective endocarditis in northeastern Thailand. Emerg Infect Dis. 2014;20:473–476. doi: 10.3201/eid2003.131059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koegelenberg C.F.N., Doubell A.F., Orth H. Infective endocarditis in the Western Cape Province of South Africa: a three-year prospective study. QJM Mar. 2003;96:217–225. doi: 10.1093/qjmed/hcg028. [DOI] [PubMed] [Google Scholar]
- 15.Regueiro A., Linke A., Latib A. Association between transcatheter aortic valve replacement and subsequent infective endocarditis and in-hospital death. JAMA. 2016;316:1083–1092. doi: 10.1001/jama.2016.12347. [DOI] [PubMed] [Google Scholar]
- 16.Thuny F., Di Salvo G., Belliard O. Risk of embolism and death in infective endocarditis: prognostic value of echocardiography: a prospective multicenter study. Circulation. 2005;112:69–75. doi: 10.1161/CIRCULATIONAHA.104.493155. [DOI] [PubMed] [Google Scholar]
- 17.Murdoch D.R., Corey G.R., Hoen B. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009;169:463–473. doi: 10.1001/archinternmed.2008.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fowler V.G., Jr., Sanders L.L., Kong L.K. Infective endocarditis due to Staphylococcus aureus: 59 prospectively identified cases with follow-up. Clin Infect Dis. 1999;28:106–114. doi: 10.1086/515076. [DOI] [PubMed] [Google Scholar]
- 19.Hill E.E., Herijgers P., Claus P. Infective endocarditis: changing epidemiology and predictors of 6-month mortality: a prospective cohort study. Eur Heart J. 2007;28:196–203. doi: 10.1093/eurheartj/ehl427. [DOI] [PubMed] [Google Scholar]
- 20.Gupta K., Jagadeesan N., Agrawal N. Clinical, echocardiographic and microbiological study, and analysis of outcomes of infective endocarditis in tropical countries: a prospective analysis from India. J Heart Valve Dis. 2014;23:624–632. [PubMed] [Google Scholar]
- 21.Cornelissen C.G., Frechen D.A., Schreiner K. Inflammatory parameters and prediction of prognosis in infective endocarditis. BMC Infect Dis. 2013;13:272. doi: 10.1186/1471-2334-13-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Siciliano R.F., Gualandro D.M., Mueller C. Incremental value of B-type natriuretic peptide for early risk prediction of infective endocarditis. Int J Infect Dis. 2014;29:120–124. doi: 10.1016/j.ijid.2014.08.017. [DOI] [PubMed] [Google Scholar]
- 23.Turak O., Özcan F., Işleyen A. Usefulness of neutrophil-to-lymphocyte ratio to predict in-hospital outcomes in infective endocarditis. Can J Cardiol. 2013;29:1672–1678. doi: 10.1016/j.cjca.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 24.Turak O., Canpolat U., Ozcan F. D-dimer level predicts in-hospital mortality in patients with infective endocarditis: a prospective single-centre study. Thromb Res. 2014;134:587–592. doi: 10.1016/j.thromres.2014.06.015. [DOI] [PubMed] [Google Scholar]
- 25.Icli A., Tayyar S., Varol E. Mean platelet volume is increased in infective endocarditis and decreases after treatment. Med Princ Pract. 2013;22:270–273. doi: 10.1159/000345393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Olaison L., Hogevik H., Alestig K. Fever, C-reactive protein, and other acute-phase reactants during treatment of infective endocarditis. Arch Intern Med. 1997;157:885–892. [PubMed] [Google Scholar]
- 27.Verhagen D.W., Hermanides J., Korevaar J.C. Prognostic value of serial C-reactive protein measurements in left-sided native valve endocarditis. Arch Intern Med. 2008;168:302–307. doi: 10.1001/archinternmed.2007.73. [DOI] [PubMed] [Google Scholar]
- 28.Heiro M., Helenius H., Sundell J. Utility of serum C-reactive protein in assessing the outcome of infective endocarditis. Eur Heart J. 2005;26:1873–1881. doi: 10.1093/eurheartj/ehi277. [DOI] [PubMed] [Google Scholar]
- 29.Ostrowski S., Marcinkiewicz A., Nowak D. Comparison of the clinical application of reactive oxygen species and inflammatory markers in patients with endocarditis. Arch Med Sci. 2012;8:244–249. doi: 10.5114/aoms.2012.28551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li J.S., Sexton D.J., Mick N. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis. 2000;30:633–638. doi: 10.1086/313753. [DOI] [PubMed] [Google Scholar]
- 31.Naber C.K., Erbel R. Diagnosis of culture negative endocarditis: novel strategies to prove the suspect guilty. Heart. 2003;89:241–243. doi: 10.1136/heart.89.3.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lamas C.C., Eyken S.J. Suggested modifications to the Duke criteria for the diagnosis of native valve and prosthetic valve endocarditis: analysis of 118 pathologically proven cases. Clin Infect Dis. 1997;25:713–719. doi: 10.1086/513765. [DOI] [PubMed] [Google Scholar]
- 33.Nishimura R.A., Otto C.M., Bonow R.O. AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;2014(129):2440–2492. doi: 10.1161/CIR.0000000000000029. [DOI] [PubMed] [Google Scholar]
- 34.Tariq M., Alam M., Munir G. Infective endocarditis: a five year experience at a tertiary care hospital in Pakistan. Int J Infect Dis. 2004;8:163–170. doi: 10.1016/j.ijid.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 35.Heiro M., Helenius H., Hurme S. Short-term and one-year outcome of infective endocarditis in adult patients treated in a Finnish teaching hospital during 1980–2004. BMC Infect Dis. 2007;7:78. doi: 10.1186/1471-2334-7-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Al-Mogheer B., Ammar W., Bakoum S. Predictors of in-hospital mortality in patients with infective endocarditis. Egypt Heart J. 2013;65:159–162. [Google Scholar]
- 37.Arshad S., Awan S., Bokhari S.S. Clinical predictors of mortality in hospitalized patients with infective endocarditis at a tertiary care center in Pakistan. J Pak Med Assoc. 2015;65:3–8. [PubMed] [Google Scholar]
- 38.Abegaz T.M., Bahagavathula A.S., Gebreyohannes E.A. Short- and long-term outcomes in infective endocarditis patients: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2017;17:291. doi: 10.1186/s12872-017-0729-5. [DOI] [PMC free article] [PubMed] [Google Scholar]