Abstract
Global Burden of Disease study has reported that cardiovascular and ischemic heart disease (IHD) mortality has increased by 34% in last 25 years in India. It has also been reported that despite having lower coronary risk factors compared to developed countries, incident cardiovascular mortality, cardiovascular events and case-fatality are greater in India. Reasons for the increasing trends and high mortality have not been studied. There is evidence that social determinants of IHD risk factors are widely prevalent and increasing. Epidemiological studies have reported low control rates of hypertension, hypercholesterolemia, diabetes and smoking/tobacco. Registries have reported greater mortality of acute coronary syndrome in India compared to developed countries. Secondary prevention therapies have significant gaps. Low quality cardiovascular care is an important risk factor in India. Package of interventions focusing on fiscal, intersectoral and public health measures, improvement of health services at community, primary and secondary healthcare levels and appropriate referral systems to specialized hospitals is urgently required.
Keywords: Coronary heart disease, India, Quality, Preventive cardiology
1. Introduction
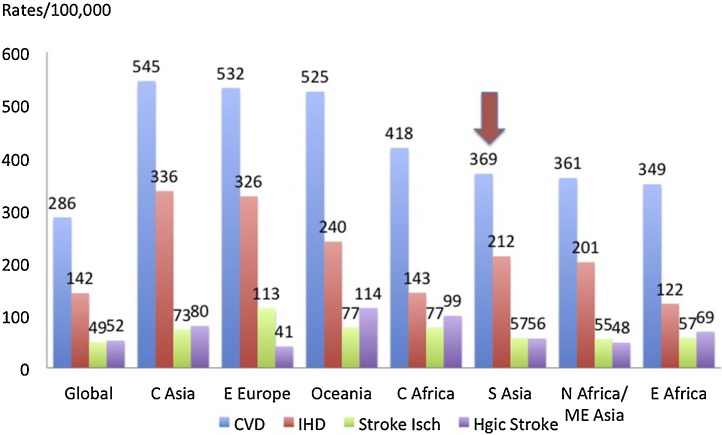
Global Burden of Disease (GBD) reports by the World Health Organization (WHO)1 and Institute of Health Metrics and Evaluation (IHME)2 have highlighted high cardiovascular disease (CVD) and ischemic heart disease (IHD) mortality rates in India and other South Asian countries.3, 4 According to GBD 2015 Study, high CVD mortality in India is driven by IHD in contrast to the East Asian countries where stroke is the predominant cause.5 GBD 2015 study reported that cardiovascular mortality rate in South Asian region was 369/100,0005 and although this was lower than in Central Asia (545), Eastern Europe (532), Oceania (525) and Sub-Saharan Central Africa (418), it is substantially greater than in North Africa and Middle-East (361), Sub-Saharan Eastern Africa (361), Southeast Asia (321) and Eastern Asia (295) (Fig. 1).5 GBD Study 2015 also reported that IHD mortality rates in India were more than twice the rates in North America and Western Europe.5
Fig. 1.
Cardiovascular disease (CVD) and ischemic heart disease (IHD) mortality rates (per 100,000) in high mortality low- and lower-middle income regions of the world compared to global average (Global Burden of Disease 2015 Study).5 (C central, E eastern, S south, N north, ME middle-east).
The GBD 2016 study reported years of life lost (YLL) as a measure of premature mortality.4 The estimated YLL rate for IHD in India was 2971/100,000 in the year 2015 and was 32.7% higher than 1990 rate of 2239/100,000.4 These rates were also significantly greater than high-income countries. For example, in USA, YLL declined from 3776/100,000 in 1990 to 2325/100,000 in 2015 (-62.4%) with a greater decline in European high-income countries (-72.2%).4 Premature IHD in form of low age of presentation of first myocardial infarction (MI) compared to other countries of the world was reported in the INTERHEART study.6 Young age of first MI has also been reported in recent acute coronary syndrome (ACS) registries from India.7, 8, 9, 10
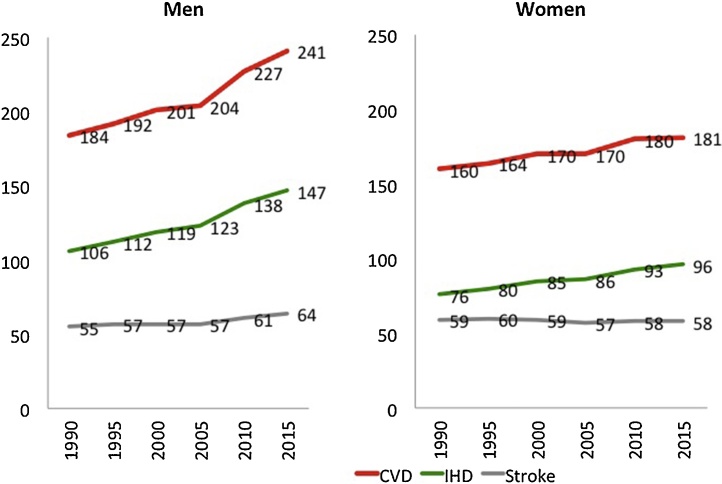
Serial mortality data from Registrar General of India has reported increasing CVD death rates in India.11, 12 In the years 2001–2003,11 the top three causes of deaths as percent of total mortality in men and women, respectively were, CVD (20.3 and 16.9%), respiratory diseases (9.3 and 8.0%) and diarrheal diseases (6.7 and 9.9%). In the years 2010–2013,12 the top three causes of deaths in men and women, respectively were, CVD (25.1 and 20.8%), respiratory diseases (7.8 and 7.5%) and cancer (5.8 and 6.6%). GBD 2016 study also reported increase in cardiovascular, IHD and stroke mortality among men and women in India (Fig. 2).4 In men, the age-adjusted cardiovascular mortality (per 100,000) was 184 in 1990 which increased to 241 in 2015 (+31%) while IHD mortality rate increased from 106 to 147 (+39%). During the same duration, among women cardiovascular mortality increased from 160 to 181 (+13%) and IHD mortality from 76 to 96 (+26%). This is in contrast to most high income and upper middle-income countries where both cardiovascular and IHD mortality rates have declined by more than 60% during this period.5 Increasing prevalence of IHD in India has been reported in previous reviews.13, 14, 15, 16, 17 GBD 2016 study also reported that the disease burden due to CVD and IHD measured by disability adjusted life years (DALYs) was increasing in India. DALYs from IHD doubled from 19.77 million/year in 1990 to 39.68 million in 2015 (+100.7%) and DALYs/100,000 increased from 2289 in 1990 to 3047 in 2015 (+33.1%).4
Fig. 2.
Age-adjusted cardiovascular, IHD and stroke mortality in men and women in India according to the Global Burden of Diseases study 2016.
There could be multiple reasons for the increase in CVD and IHD mortality and morbidity in India. Multiple hypotheses have been postulated. These include rapid increase in social determinants, “the causes of causes”, of cardiovascular health,16, 17, 18, 19 increasing standard coronary risk factors,16, 17, 18, 19 and genomic factors including gene-environment interaction and adverse epigenetic influences.20, 21 In the present review we have briefly reviewed available data on social determinants of health, standard and emerging coronary risk factors and emerging genetic and epigenetic factors relevant to India. We have also evaluated studies that report quality of primary prevention and gaps in acute and chronic IHD management. We argue that poor quality of preventive and clinical care is widespread in India and is an important modifiable risk factor that is responsible for increasing IHD mortality in India.
2. Methods
The present narrative review is based on a number of previous studies and publications on epidemiology of IHD and its risk factors from India. In addition to data from previous reviews of IHD epidemiology in India,13, 14, 15, 16, 17 we evaluated newer publications from the Registrar General of India.11, 12 We also obtained data from electronic databases of WHO3 and GBD Study 20164 to estimate absolute number of deaths and adjusted rates/100,000 from CVD and IHD in India. We obtained data on social determinants of IHD and risk factor data for India from previous reviews15, 16, 17, 18 and literature search using PubMed. Genetic risk factors including influence of epigenetic factors have been summarized in some of the recent reviews.20, 21 South Asian specific genes that predispose to IHD were obtained using PubMed search. Registries and reviews highlighting gaps in preventive and curative treatment of IHD were also obtained using PubMed. Descriptive statistics are presented.
3. Group 1: epidemiological transition and social determinants
Social determinants of chronic diseases such as IHD have been poorly studied in India. Increase in almost all the major IHD risk factors is rooted in epidemiological transition.18 This transition involves many socio-demographic factors.22 Adverse transition in India is associated with increase in cardiometabolic risk factors.17, 18 Relevant for India are migration, urbanization, education, poverty, human development index (HDI), and individual socioeconomic factors.18, 19, 23, 24 India is still on the increasing curve of epidemiological transition and it has been argued that stabilization in risk factor prevalence and their decline, as observed in developed countries, shall take time.18 These socioeconomic changes have been collectively called political, social and economic determinants of health.25
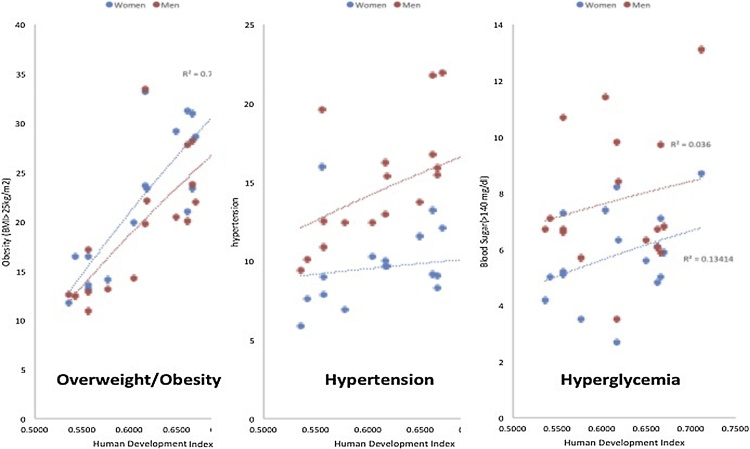
We obtained state-level data on major IHD risk factors- hypertension and overweight from Fourth National Family Health Survey (NFHS-4).26 We also obtained data on state-level social parameters such as HDI, urbanization and educational status.26 Correlational analysis demonstrated that states with greater HDI have greater prevalence of overweight (body mass index- BMI ≥25 kg/m2), hypertension and hyperglycemia (random blood glucose >140 mg/dl) both in men and women (Fig. 3).
Fig. 3.
Association of Human Development Index (HDI) with prevalence of overweight/obesity, hypertension and hyperglycemia among men (red markers) and women (blue markers) in larger states of India. Data. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Source: 4th National Family Health Survey (NFHS-4).26
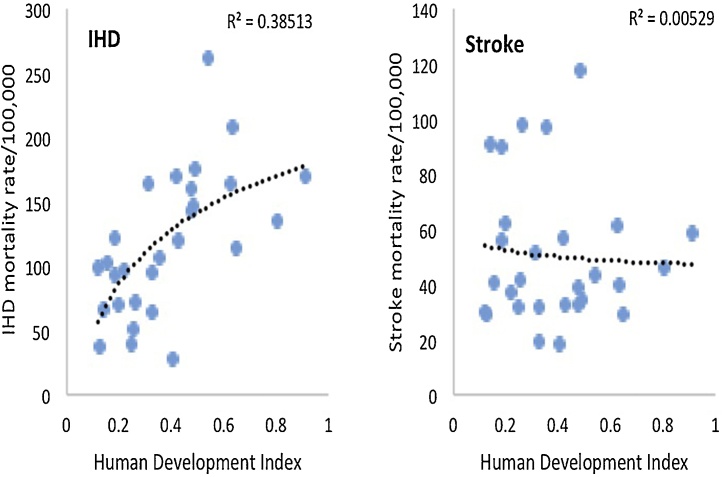
We also performed association analysis of district level prevalence of overweight and hypertension with urbanization and HDI in states with high, moderate and low HDI (Table 1). The analysis suggests varying level of epidemiological transition in different states in India and explains the varying IHD mortality in these states. Similar results have been reported in a state specific reports from Rajasthan,27 NFHS-4,26 and India GBD Alliance.19 Household level data from the Indian Census shows a rapid increase in social services such as water supply, electric supply and construction of pucca houses and regular roads.28 This is coupled with exponential increase in ownership of labor saving devices such as 2- and 4-wheeler transport vehicles, cell phones, televisions and telephone connections. All these macrolevel and microlevel distal determinants of cardiovascular health have led to a significant decline in physical activity and changes in dietary habits and led to increase in cardiometabolic risk factors and IHD. There is a significant positive correlation of state-level HDI with IHD mortality and null association with stroke mortality suggesting evolving epidemiological transition in the country (Fig. 4). The mortality data have been obtained from India GBD Alliance report.19
Table 1.
Examples of association of district level urbanization and human development index (HDI) with prevalence of overweight, hypertension and hyperglycemia (random blood glucose ≥140 mg/dl) among 15–49 years old women and 15–54 year old men in NFHS-4 in Indian states at high (Kerala, Tamil Nadu), middle (Rajasthan, Madhya Pradesh) and low (Uttar Pradesh, Bihar) levels of HDI (Spearman’s correlation coefficient).
| States (HDI) | Overweight/Obesity |
Hypertension |
Hyperglycemia |
||||
|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | ||
| Kerala (0.712) | Urbanization | −0.235 | 0.095 | −0.138 | −0.128 | −0.367 | −0.534* |
| HDI | 0.279 | 0.464 | 0.068 | 0.282 | 0.187 | −0.044 | |
| Tamil Nadu (0.666) | Urbanization | 0.302 | 0.660** | 0.062 | 0.371* | −0.016 | 0.069 |
| HDI | 0.091 | 0.758* | 0.248 | 0.225 | 0.316 | 0.212 | |
| Rajasthan (0.577) | Urbanization | 0.484** | 0.591** | 0.306* | 0.294 | 0.139 | 0.045 |
| HDI | 0.592** | 0.625** | 0.494** | 0.294 | 0.144 | 0.052 | |
| Madhya Pradesh (0.557) | Urbanization | 0.319* | 0.634** | 0.167 | −0.007 | 0.112 | 0.095 |
| HDI | 0.558** | 0.573** | 0.159 | 0.001 | −0.008 | 0.008 | |
| Uttar Pradesh (0.542) | Urbanization | 0.368** | 0.588** | −0.231 | −0.332** | 0.096 | −0.004 |
| HDI | 0.381** | 0.417** | −0.131 | −0.357** | −0.164 | −0.269* | |
| Bihar (0.536) | Urbanization | 0.190 | 0.268 | 0.004 | 0.087 | 0.040 | 0.179 |
| HDI | −0.100 | 0.116 | 0.313 | −0.085 | −0.036 | −0.116 | |
HDI Human development index.
p < 0.05.
p < 0.01.
Fig. 4.
Association of state-level Human Development Index (HDI) with ischemic heart disease (IHD) and stroke mortality in India. A significant positive correlation is observed with IHD mortality (logarithmic R2 = 0.385) and no correlation is observed with stroke (logarithmic R2 = 0.005).
4. Group 2: changes in standard & emerging coronary risk factors
There are no large prospective studies from India that have evaluated association of risk factors with IHD outcomes. INTERHEART, a case-control study of acute coronary events had a large representation from India and other South Asian countries.29 In this study it was reported that IHD risk factors were not dissimilar among South Asians as compared to populations from other parts of the world.6 Nine common risk factors were identified as important: high ApoB/ApoA1 ratio (dyslipidemia), smoking, known hypertension, known diabetes, abdominal obesity, psychosocial stress, unhealthy diet, low physical activity and alcohol. However, the population attributable risks among South Asians were greater for dyslipidemia, abdominal obesity, smoking, physical inactivity, unhealthy diet and alcohol intake.6 Similar findings have been reported in the INTERSTROKE case-control study.30 All the above mentioned nine IHD risk factors have been identified as important in South Asians with ischemic and hemorrhagic strokes.30
Epidemiological studies have reported that all the common risk factors are increasing in India.17, 31 Systematic reviews and other studies have reported significant increase in obesity,32 abdominal obesity,33 hypertension,34, 35 diabetes,36 metabolic syndrome37 and dyslipidemias (hypercholesterolemia and hypertriglyceridemia)38 in India, both in urban and rural populations. It has been suggested that this increase in cardiometabolic risk factors is fueling the IHD epidemic in India.39
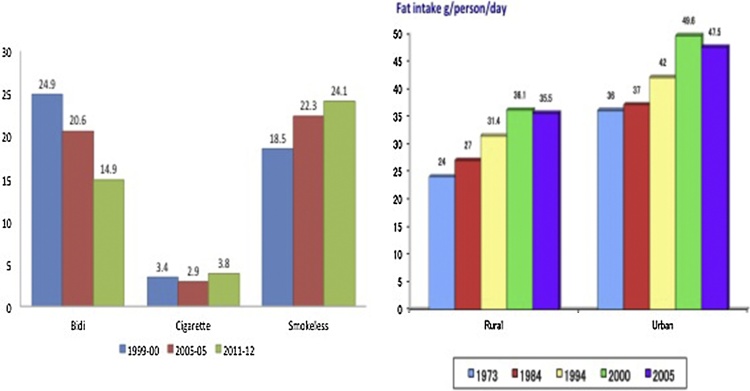
These changes are also due to adverse effects of globalization that influence social construct, social movements, occupational exposures, technologies, physical activity, food preferences and consumption, smoking and tobacco consumption.40 Trends in lifestyle factors demonstrate variable change. For smoking and tobacco use, Bhan et al41 analyzed data from National Sample Survey Organization (NSSO) Reports, 1999–2012 (Fig. 5). The study showed a decline in smoking rates among men with an increase among women. Smokeless tobacco consumption increased during this period. Similar results were reported by Mishra et al,42 who reported smoking and non-smoked tobacco-use from the Special Fertility and Mortality Survey (SFMS 1998) and Global Adult Tobacco Survey (GATS 2010).42 In this report the finding of increased smoking among younger men and women was a cause of concern. Changes in dietary consumptions are difficult to analyze. Serial studies by National Nutrition Monitoring Bureau (NNMB) and NSSO have reported increasing trends in consumption of calories and fats among rural and urban populations.43, 44 The per-capita consumption of saturated fats, trans-fats as well as refined sugars and carbohydrates is increasing.43 Although the per capita consumption of fruits and vegetables has increased but remains suboptimal.44 Trends in consumption of other cardioprotective micronutrients has not been reported.
Fig. 5.
Time-trends in prevalence of smoking, smokeless tobacco-use in men and women and dietary fat consumption (in National Sample Survey Organization studies).
Data on other lifestyle factors that influence cardiovascular health are sparse in India. Alcohol intake has been reported in NFHS studies and appears to be increasing.26 A study from Kerala reported that percentage of those consuming alcohol under 21 years from years 1986 to 2014 increased from 2% to 20% while age of initiation decreased from 19 to 13.5 years.45 NFHS-3 reported that about 32% men in India use alcohol.26 The National Mental Health Survey of India 2015–2016, found that prevalence of alcohol use disorders (dependence and harmful use) in males was 9% and in females was 0.5%.46 It was the third most common mental disorder after tobacco use disorder and depression. Globally, alcohol has become the most common risk factor for death and disability in the age group of 15–49 years.4 A similar situation is emerging in India. Excessive alcohol consumption is related to greater hypertension prevalence and sudden death. INTERHEART study reported that in South Asians, harmful use of alcohol such as binge drinking is common and does not offer any cardiovascular protection.6
Some of the newer and emerging risk factors may be important in Indian patients with IHD (Table 2).16 In a case-control study involving young survivors of ACS <50 years, Panwar et al. reported that smoking, hyperhomocysteinemia, hypertension and abdominal obesity were important risk factors.47 Another study of coronary risk factors in young Indians (CADY) reported that psychosocial stress and family history were important risk factors.48 However, the trends in these and other risk factors (Table 2) have not been studied in India and it shall be difficult to associate them with increasing IHD in Indians.
Table 2.
Important and unique coronary risk factors in Indians.
| Standard major risk factors | Emerging risk factors |
|---|---|
|
|
5. Group 3: genetic risk factors
Genetic factors have been hypothesized to explain the greater risk of IHD in Indians for a long time.49 Studies among South Asian families show that cardiovascular risk factors and coronary artery disease are heritable.50 Initial studies among emigrant Indians in Southeast Asia, Oceania and UK suggested that standard risk factors do not explain greater incidence and it was speculated that some genetic factors were involved.50 Subsequent studies reported that higher insulin resistance and diabetes in these populations explained this greater risk.51, 52
Multiple low-power genetic studies have been performed in India and have reported associations with many single nucleotide polymorphisms (SNPs).53, 54 All these studies are underpowered. Genetic analyses using genome-wide association studies (GWAS) have failed to replicate the results of most of these studies.55 GWAS have identified a number of SNPs as important coronary atherosclerosis at different pathways (Table 3).21 This list keeps on growing with more information being available rapidly including genes important in South Asians.56 These individual variants have a modest effect size with odds ratios of 1.05 to 1.30 per risk allele copy and in aggregate account for only a small proportion of the total predicted genetic variance. However, these findings do not exclude a role for genetic factors since the GWAS approach is not well designed to identify either low frequency or rare variants.57 Moreover, the South Asian genome, although similar to Caucasian populations, in certain extents is unique56, 57 and more research is required in this direction.
Table 3.
Genes identified for atherosclerosis and its pathways.
| LDL cholesterol and lipoprotein(a) | Triglyceride rich lipoproteins | Inflammation | Cellular proliferation and vascular remodeling | Vascular tone and nitric oxide signaling |
|---|---|---|---|---|
| SORT1 | LPL | IL6R | COL4A1-COL4A2 | CUCY1A3 |
| PCSK9 | TRIB1 | CXCL12 | MIA3 | EDNRA |
| APOB | APOA5 | REST-NOA1 | NOS3 | |
| ABCG5-ABCG8 | APOA4 | ZC3HC1 | ||
| LPA | APOC4 | 9p21 | ||
| LIPA | APOA1 | PDGFD | ||
| LDLR | ANGPTL4 | AWAP70 | ||
| APOE | KSR2 | |||
| ADAMTS7 | ||||
| BCAS3 | ||||
| FLT1 | ||||
| SMAD3 |
IHD and vascular atherosclerosis is a multifactorial disease. Research on of individual genetic factors on IHD incidence that used SNPs were found inferior to classical cardiovascular risk factors in risk prediction. Therefore, recent focus has shifted from SNP model to gene risk score models.21 The initial reports combined 11 SNPs for risk prediction.58 As knowledge has evolved more and more SNPs have been added to create various polygenic risk scores using SNPs involved in not only inflammatory and thrombogenic pathways but also pathways involved in various major cardiovascular risk factors- hypertension, dyslipidemias and diabetes. These polygenic risk scores have been created using 50–100 SNPs.59, 60, 61 Complex trait diseases such as IHD may have omnigenic rather than polygenic pathways.62 Recent reports suggest that an omnigenic gene risk prediction model with incorporation of 50K–100 K SNPs is more reliable and better predictive than classical cardiovascular risk scores mentioned above.63 Indeed there has been a progressive increase in the number of SNPs in each risk score (Table 4) and current genome-wide polygenic risk scores are based on millions of genes that are being investigated to identify a monogenic-risk equivalence for coronary artery disease using advanced mathematic techniques.64
Table 4.
Evolution of coronary gene risk scores from 50’s to include millions of SNPs.
| Polygenic score | Derivation strategy | N variants | Area under the curve | Odds ratio (per SD increment) |
|---|---|---|---|---|
| Tada et al. | Variants that achieved genome-wide statistical significance in prior GWAS (p < 5 × 108) | 50 | 0.59 | 1.38 |
| Abraham et al. | Linkage-equilibrium based thinning of variants from prior GWAS | 49,310 | 0.59 | 1.38 |
| Pruning strategy (pruning & truncation) | Pruning based on statistical significance (p < 0.05) and linkage disequilibrium (r2 < 0.8) of variants from prior GWAS | 116,859 | 0.62 | 1.54 |
| Pruning strategy (GWAS) | LDPred computational algorithm to assign weights to all available variants from prior GWAS via explicit modeling of linkage disequilibrium | 6,630,150 | 0.64 | 1.67 |
Presently, there are no studies that have specifically identified genomic risk factors in South Asians or Indians using GWAS, whole genome studies (WGS), whole exome sequencing (WES) or next generation sequencing (NGS). GWAS study among the PROMIS cohort in Pakistan did not report any unique SNP associations with multiple IHD risk factors.65, 66 Large GWAS based studies in UK have identified a few SNPs that may be important for IHD and stroke in South Asians.55 More studies are needed as detailed study of the South Asian genome has revealed evidence for selective pressure on genes involved in skin biology, metabolism, infection and immunity- all important in processes of atherosclerosis.57
The genetic structure of human populations does not change in a few decades and it would be more important to study gene functions as well as gene–gene and gene-environment interaction.21 Very limited information exists on these areas of research especially in Indians and South Asians. Study of gut microbiome and its influence on atherosclerosis is important in this regard.67 Also required is study of epigenetic factors that are known to alter the gene function but are not the result of changes in the DNA sequence. Gene-environment interactions can lead to adverse epigenetic influences that can promote atherosclerosis. For example, physical inactivity and harmful nutrients are known to promote atherosclerosis via epigenetic changes and both these risk factors are rapidly increasing in India. Ambient air pollution and use of industrial and agricultural toxins are also increasing in India. Both may affect the epigenetic factors responsible for IHD and explain the increased coronary epidemic in India.
6. Group 4: quality of preventative, acute and chronic coronary care
Cardiovascular risk factors such as hypertension, hypercholesterolemia, diabetes and smoking need lifelong control to achieve decline in CVD mortality.68 Once IHD manifests, it also needs lifelong secondary preventative treatment. Poor quality cardiovascular care is associated with increased cardiovascular mortality. There are significant gaps in primary prevention, acute IHD management, as well as secondary prevention in India as highlighted by the Prospective Urban Rural Epidemiology (PURE) study.69, 70 We argue that this is an important coronary risk factor.
The PURE study is the first prospective study that has systematically identified gaps in care as an important cardiovascular risk factor in lower and middle income countries including India.69 In this study 156,424 adults 35–70 years of age were recruited from 3 high, 10 middle income and 4 low income countries (India was a low income country when recruitment started in 2003). Participants from low-income countries (India, Pakistan, Bangladesh and Zimbabwe) had the lowest prevalence of cardiovascular risk factors as estimated by a low mean INTERHEART risk score (8.3, 95% confidence interval 7.6-9.1) compared to middle-income (10.5, 10.1-10.8) and high-income countries (12.9, 12.8-13.0). These people were followed for a mean of 4.1 years. At this time it was observed that CVD mortality, case-fatality as well major event rates (acute MI, stroke or heart failure) were significantly greater in low-income countries compared to middle- and high-income countries. This paradox of “low risk factor, high cardiovascular mortality” is best explained by poor quality of care, low quality primary prevention, inferior acute IHD management and secondary prevention.70 Indeed, studies from India have reported significant gaps in policies for population level primordial prevention; primary prevention involving treatment and control of risk factors such as hypertension, diabetes, hypercholesterolemia and smoking; hospital based acute coronary disease management; as well as long term secondary prevention and cardiac rehabilitation. Significant gaps also exist in cardiovascular care quality parameters (Table 5) in India.71
Table 5.
Cardiovascular care quality parameters.
| Primary preventive care | Disease management and secondary care |
|---|---|
|
|
6.1. Risk factor control and primary prevention
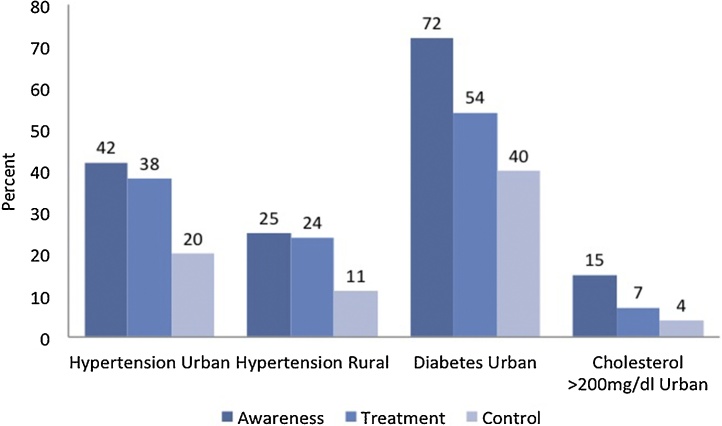
Population based studies from India have consistently reported low awareness, treatment and control of hypertension and other cardiovascular risk factors (Fig. 6). Anchala et al34 and Devi et al72 reviewed all the hypertension epidemiology studies from India and reported very low rates of hypertension awareness (30–50%), treatment (20–40%) and control (5–20%) in different regions of India. The PURE study reported that hypertension treatment and control was the lowest in low and lower-middle income countries (including India) as compared to participants from high and upper-middle income countries.73
Fig. 6.
Awareness, treatment and control of major coronary risk factors in India. Data from hypertension urban and rural are from a meta-analysis by Anchala R, et al.34 Data on diabetes urban (Gupta A, et al)75 and hypercholesterolemia (Gupta R, et al)35 are from multisite India Heart Watch study.
Dyslipidemias are the most important risk factor in India.6 These dyslipidemias include high levels of total cholesterol, LDL cholesterol, triglycerides and apolipoprotein-B and low levels of apolipoprotein-A and HDL choleserol.16 Hypercholesterolemia is the most important form of dyslipidemia amenable to therapy. Awareness and treatment of hypercholesterolemia is very low in India.38 Diabetes is a very important risk factor in Indians and it also has low rates of awareness, treatment and control.36, 74, 75 Smoking quit rates among adults are less than 5% as compared to 25–30% in developed countries.41
The PURE study has also reported that physical activity levels are low in India (and other low and lower-middle income countries)76 and food is high in unhealthy nutrients and low in fruits.77, 78 Situation appears to be improving, though. For example, serial studies from an Indian urban location has reported that over a 25-year period, hypertension awareness, treatment and control status has improved.79 This increase is slow and projections of trends report that India is unlikely to achieve the expected levels of hypertension control as envisaged for the year 2030 as defined by UN Sustainable Development Goals.79
There are multiple reasons for the low quality primary preventive care in India including costs, culture and attitudes- more research is required for their careful characterization.80 Low focus on preventive care and lack of clear national policies for promotion of smoking cessation, improving physical activity and promotion of healthy food are hampering the cardiovascular prevention effort in India.81 High quality primary prevention also depends on government policies and public health spending on primary care; both are low priority areas in India. Disease Control Priorities Project has recommended a number of fiscal, intersectoral, public health and personal health services interventions at levels of community, primary health centre, first-level hospitals, referral hospitals and specialized hospitals for control of CVD in low and middle income countries.82 Because India is a very populous and diverse country with states at different stages of epidemiological transition, it is important to contextually modify these guidelines which focus mainly on tobacco taxation, bans on trans fats and reduction in salt content of manufactured foods. Policy change and health services interventions are also suggested which focus mainly on promotion of universal health coverage.83
A number of studies are ongoing in India that have focused on multifactorial interventions for risk factor control, especially focusing on better hypertension management and control. Most of these studies have used either a health-care worker based intervention or technology-enabled intervention. Results are awaited.
6.2. Management of acute coronary events
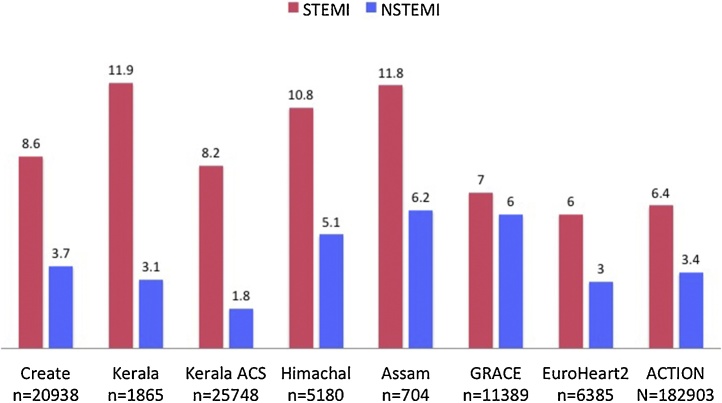
Significant gaps in quality of acute coronary care in Indian patients was initially highlighted by the Organization to Assess Strategies for Ischemic Syndromes (OASIS) and Treatment and Outcomes of Acute Coronary Syndromes in India (CREATE) registries.7, 8 OASIS-2 registry reported a high 2-year mortality rates in patients with non-ST elevation myocardial infarction (NSTEMI) which was almost double than participants from countries in Europe and North America.7 CREATE registry recruited 20,468 patients from 89 hospitals across the country.8 A 30-day mortality rate of 8.6% in ST-elevation MI (STEMI) patients and 3.7% in NSTEMI was reported (Fig. 7). It was also reported that the unadjusted 30-day morality rates among the rich, upper middle, lower middle and poor socioeconomic strata were 5.5, 5.9, 6.5% and 8.2%, respectively (p < 0.001) These significant differences did not change with adjustment of risk factors but were attenuated on adjustment for types of treatments; adjusted mortality rates were 7.2%, 6.9%, 6.4 and 6.6%, respectively (p = 0.97). This study, thus, highlighted disparities in quality of treatments in ACS patients in different socioeconomic groups in India and strongly (or clearly) suggested that quality of care was an important coronary mortality risk factor.8
Fig. 7.
Short term mortality in acute coronary syndrome (ACS) patients with STEMI and NSTEMI. Data are from contemporary ACS registries in India and have been compared with large European and US registries.
High coronary mortality rates have been reported from recent registries in Kerala,84, 85 Himachal Pradesh9, 86 and Assam.10 Kerala ACS registry was conducted in the most developed and epidemiologically evolved state of Kerala (shown in Table 1) and recruited 25,748 participants with STEMI and NSTEMI.85 The 30-day mortality rate in STEMI was greater than CREATE registry (11.9 vs 8.6%) while NSTEMI mortality rates were similar (3.1 vs 3.7%). It was also reported that use of various evidence based treatments were sub-optimal. For example, the use of primary coronary intervention in both CREATE and Kerala-ACS registries was less than 10%.
Lower rates of in-hospital, 30-day or 6-month mortality have been reported in recent acute coronary syndrome registries among metropolitan hospitals in India. In-hospital mortality rates of less than 3% has been reported in multisite Detection and Management of Coronary Heart Disease patients (DEMAT),87 Indian Council of Medical Research- Management of Acute Coronary Event (ICMR-MACE),88 and other some single-hospital registries from Chennai89 and Delhi.90 This could be due to multiple factors including case selection bias, event reporting bias and better quality of treatment. Use of coronary interventions in these studies was greater than the previous studies and better use of evidence-based therapies could also be a factor. The SPREAD study reported a high use of primary coronary intervention (60%) and evidence based therapies- dual antiplatelets, beta blockers, renin-angiotensin system (RAS) blockers and statins, of >90% in 14 tertiary care hospitals.91 Large registries from Europe (GRACE92 and EuroHeart-293) and USA (ACTION94) have reported a much lower in-hospital mortality rates in ACS (Fig. 7). Studies that evaluated secular trends have reported a decline in in-hospital and short term mortality following ACS in developed countries. The American College of Cardiology multicenter acute coronary syndrome registry (ACTION) reported a constant improvement in quality of care associated with declining in-hospital and short-term mortality in ACS patients.94 A decline in the in-hospital ACS mortality has also been reported in nationwide registries from Sweden95 and France.96
In India, systemic nationwide studies are required to identify importance of health systems, patient characteristics and treatments that are important in influencing outcomes. Some of quality improvement methods are described by Disease Control Priorities project.82 Quality improvement studies for ACS management are also required. Acute Coronary Syndrome Quality Improvement in Kerala (ACS-QUIK) study97 was conducted at multiple hospital sites in Kerala. In this cluster-randomized trial with a step wedged design, a multifactorial educational program, which was focused on physicians, reduced door-to-needle and door-to-balloon times and increased use of various evidence based therapies. Use of in-hospital evidence based therapies also increased. However, there was no difference in 30-day major cardiovascular end points in the studies (intervention 5.8%, vs. intervention 6.0%, p = not significant) with multivariate adjusted difference −0.09% (CI −1.32, 1.14%) as well as adjusted odds ratio 0.98 (CI 0.80–1.21). The major cardiovascular events were significantly greater in women as compared to men (odds ratio 1.86, CI 1.65–2.09) with no influence of intervention in either sex.97 Similar and larger multifaceted efforts along with better training to physicians and residents are required.
6.3. Secondary prevention
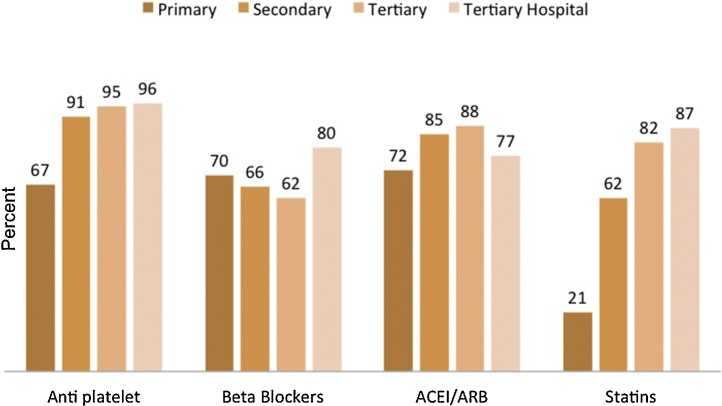
Quality of secondary prevention is also sub-optimal in India.16 In WHO study on Prevention of REcurrences of Myocardial Infarction and StrokE (WHO-PREMISE) study, use of various cardiovascular evidence based medicines (aspirin, beta-blockers, ACE inhibitors and statins) in stable patients with cardiovascular disease (IHD or stroke) was reported in 9 low and middle-income countries, including India.98 A low use of various evidence based medicines especially renin angiotensin system (RAS) blockers and lipid-lowering drugs was reported. In a prescription audit based study in Rajasthan (western India) it was reported that prescription of the four classes of evidence based therapies, mentioned above, was high at tertiary care centers but was significantly lower at secondary and primary care level (Fig. 8).99 Similar findings have been reported at a few other studies in primary care including a study from rural Andhra Pradesh and other parts of the country.100, 101
Fig. 8.
Prescription of various cardiovascular evidence-based therapies at tertiary care hospital, tertiary care clinics, secondary care clinics and primary care clinics in patients with established IHD in India.104.
Community based studies in South Asia and India among rural and urban participants a few years after a CVD event (AMI or strokes) in the Prospective Urban Rural Epidemiology (PURE) study102 reported drastically low community level use of these four classes of drugs. The use of the four evidence-based medications was hugely different in high, compared to low-income countries. The use of anti-platelets (62 vs 9%), beta-blockers (40 vs 8%), ACE inhibitors or angiotensin receptor blockers (50 vs 5%) and statins (67% vs 3%) were significantly different (p < 0.0001). Multiple factors could be involved in these patients involving administrative and health system level factors, clinician health services level factors and patients level factors.99 In the PURE study participants from India, we identified poverty and low educational status of patients as important.103 Many other factors could be involved and require further research.
Systemic effort is required to improve secondary prevention for coronary heart disease in India. This is a “low-hanging” fruit of cardiovascular prevention. It has been estimated that proper use of these therapies can reduce mortality by 20–30% among patients with established disease. SPREAD study was a multisite study conducted at 14 tertiary care hospitals across the country.91 In this study, survivors of ACS were randomized to either usual care or a trained community-health worker based educational intervention for improving knowledge and practice of secondary prevention strategies, every two months for one year. It was reported that after 12 months of follow-up participants in the intervention arm had better adherence to evidence based drug therapies, had lower smoking prevalence, blood pressure, body weight and cholesterol levels. The study was not powered to assess outcomes. A large outcome study based on yoga-lifestyle intervention is currently ongoing.104 Secondary prevention practices can be improved as has been demonstrated in the European Action on Secondary Prevention through Intervention to Reduce Events (EUROASPIRE) program in Europe.105 Participation in a formal cardiac rehabilitation is also important and would lead to reduced coronary events.106
7. Epilogue
Increasing cardiovascular and IHD mortality in India has been reported by WHO and GBD studies.1, 2 PURE study reported that in Indian participants had lower prevalence of major cardiovascular risk factors (INTERHEART risk score) as compared to high and middle-income countries but high cardiovascular mortality.69 This indicated lower quality preventive and therapeutic cardiovascular care in India. Studies have reported that almost all cardiovascular risk factors (social determinants, harmful lifestyles, anthropometric and biochemical factors) are increasing in India.16, 17 We argue that low-quality promotive, preventive and clinical coronary care is a major cardiovascular risk factor. Epidemiological studies have reported low levels of smoking quit rates, and low risk factor (hypertension, diabetes and hypercholesterolemia) awareness, treatment and control rates, high cardiovascular and IHD mortality and case-fatality following acute coronary events, and low quality of long-term secondary preventive care. These gaps are particularly prevalent at primary and secondary care levels.
There is need to improve political and bureaucratic focus on improving cardiovascular and coronary care. Disease Control Priorities Project has identified a number of useful interventions.82 Policy level and fiscal interventions to increase taxes on tobacco and sugar sweetened beverages, improvements in the built environments to encourage physical activity, school based programs to improve nutrition and encourage physical activity, regulation on advertising and labeling of tobacco products, actions to reduce salt content in manufactured foods and bans on trans-fatty acids are crucial. Public health interventions should focus on nutritional supplementation for women of reproductive age and mass-media must be used to propagate harms of specific unhealthy foods and tobacco products. Improvement in quality of personal health services is important.71, 80, 82 Community based interventions include training of community health workers for cardiovascular risk screening using non-lab based tools for risk assessment, to improve adherence, and referral to primary health centers for continued medical management. Primary health centers should perform opportunistic screening for hypertension for all adults, screening for diabetes in high-risk individuals and provide combination therapy for multiple risk factor reduction. These centers should also provide facilities for long term management of IHD patients with evidence based medicines-aspirin, beta blockers, RAS blockers and statins when indicated, and should be trained to use aspirin in all cases of suspected myocardial infarction. First level hospitals should have facilities for tobacco cessation counseling and primary management of acute coronary events with unfractionated heparin, aspirin and generic thrombolytics. Referral hospitals should be equipped with high quality coronary care units and primary coronary interventions should be promoted when appropriate.106 Quality improvement programs at community levels, especially in rural areas, for risk factor prevention, identification and improving adherence to basic therapies are few107, 108 and ongoing.109, 110, 111 ACS-QUIK study has shown that quality of ACS management can be improved.97 Tamil Nadu-STEMI program has reported that coordinated care for STEMI using a public-private partnership model is feasible.112 The SPREAD study has demonstrated usefulness of community health workers in promoting secondary prevention following acute coronary event.91 Global action is required on social determinants of cardiovascular health.113 Innovative methods of healthcare financing using public and private insurances have been evaluated and are available in some states of the country.114 The initiatives are still evolving.115 Although more such studies are required, especially in resource-constrained health systems in different locations, implementation of existing knowledge should lead to improvement in quality of primary and secondary preventative care. Modification of this important risk factor through health system interventions would save hundreds of thousands of lives in India and reduce morbidity in millions. Urgent and focused action is needed from multiple stakeholders.
References
- 1.World Health Organization . World Health Organization; Geneva: 2014. Global Status Report on Non-Communicable Diseases 2014. [Google Scholar]
- 2.GBD 2016 Mortality and Causes of Deaths Collaborators. Global, regional and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . 2018. Country Level Mortality Data. Available at: http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html. Accessed 15 January 2018. [Google Scholar]
- 4.Global Burden of Disease Study . 2015. Health Data. Available at: http://ghdx.healthdata.org/gbd-data-tool. Accessed 15 January 2018. [Google Scholar]
- 5.Roth G.A., Johnson C., Abajobir A. Global, regional, and national cardiovascular disease prevalence, mortality, and disability-adjusted life-years for 10 causes of cardiovascular mortality, 1990 to 2015: A systematic analysis for the Global Burden of Disease Study. J Am Coll Cardiol. 2017;70:1–25. doi: 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joshi P.P., Islam S., Pais P. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297:286–294. doi: 10.1001/jama.297.3.286. [DOI] [PubMed] [Google Scholar]
- 7.Prabhakaran D., Yusuf S., Mehta S. Two-year outcomes in patients admitted with non-ST elevation acute coronary syndrome: results of the OASIS Registry 1 and 2. Indian Heart J. 2005;57:217–225. [PubMed] [Google Scholar]
- 8.Xavier D., Pais P., Devereaux P.J. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371:1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 9.Negi P.C., Merwaha R., Panday D., Chauhan V., Guleri R. Multicenter Himachal Pradesh ACS Registry. Indian Heart J. 2016;68:118–127. doi: 10.1016/j.ihj.2015.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iqbal F., Barkataki J.C. Spectrum of acute coronary syndrome in North Eastern India: a study from a major center. Indian Heart J. 2016;68:128–131. doi: 10.1016/j.ihj.2015.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Registrar General of India . Registrar General of India, Ministry of Home Affairs; New Delhi: 2009. Report on Causes of Deaths in India 2001–2003. [Google Scholar]
- 12.Registrar General of India, Centre for Global Health Research . 2013. Causes of Death Statistics 2010–2013. Available at: http://www.cghr.org/wordpress/wp-content/uploads/COD-India-Report-2010-2013-Dec-19-2015.pdf. Accessed 31 August 2017. [Google Scholar]
- 13.Gupta R., Gupta V.P. Meta-analysis of coronary heart disease prevalence in India. Indian Heart J. 1996;48:241–245. [PubMed] [Google Scholar]
- 14.Krishnaswami S. Prevalence of coronary artery disease in India. Indian Heart J. 2002;54:103. [PubMed] [Google Scholar]
- 15.Gupta R., Joshi P.P., Mohan V., Reddy K.S., Yusuf S. Epidemiology and causation of coronary heart disease and stroke in India. Heart. 2008;94:16–26. doi: 10.1136/hrt.2007.132951. [DOI] [PubMed] [Google Scholar]
- 16.Prabhakaran D., Jeemon P., Roy A. Cardiovascular diseases in India: cuurent epidemiology and future directions. Circulation. 2016;133:1605–1620. doi: 10.1161/CIRCULATIONAHA.114.008729. [DOI] [PubMed] [Google Scholar]
- 17.Gupta R., Mohan I., Narula J. Trends in coronary heart disease epidemiology in India. Ann Glob Health. 2016;82:307–315. doi: 10.1016/j.aogh.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 18.Gupta R., Gupta K.D. Coronary heart disease in low socioeconomic status subjects in India: an evolving epidemic. Indian Heart J. 2009;61:358–367. [PubMed] [Google Scholar]
- 19.India State-Level Disease Burden Collaborators Nations within a nation: variations in epidemiological transition across the states in India 1990–2016, in the Global Burden of Disease Study. Lancet. 2017;390:2437–2460. doi: 10.1016/S0140-6736(17)32804-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jayashree S., Arindam M., Vijay K.V. Genetic epidemiology of coronary artery disease: an Asian Indian perspective. J Genetics. 2015;94:539–549. doi: 10.1007/s12041-015-0547-4. [DOI] [PubMed] [Google Scholar]
- 21.Khera A.V., Kathiresan S. Genetics of coronary artery disease: discovery, biology and clinical translation. Nat Rev Genet. 2017;18:331–344. doi: 10.1038/nrg.2016.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kuate Defo N. Beyond the transition frameworks: the cross-continuum of health, disease and mortality framework. Glob Health Action. 2014;7:1–16. doi: 10.3402/gha.v7.24804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reddy K.S., Yusuf S. Emerging epidemic of cardiovascular disease in developing countries. Circulation. 1998;97:596–601. doi: 10.1161/01.cir.97.6.596. [DOI] [PubMed] [Google Scholar]
- 24.Yusuf S., Reddy K.S., Ounpuu S., Anand S. Global burden of cardiovascular diseases: part I: general considerations, the epidemiologic transition, and impact of urbanization. Circulation. 2001;104:2746–2753. doi: 10.1161/hc4601.099487. [DOI] [PubMed] [Google Scholar]
- 25.Marmot M. Bloomsbury Publishing; London: 2015. The Health Gap: The Challenge of an Unequal World. [DOI] [PubMed] [Google Scholar]
- 26.National Family Health Survey. Available at: http://rchiips.org/nfhs/abt.html. Accessed 2 November 2017.
- 27.Gaur K., Mohan I., Gupta R. Syndemic of obesity, hypertension and hyperglycemia among 15–49 year olds in Rajasthan: district-level data from National Family Health Survey-4. RUHS J Health Sci. 2017;2:54–64. [Google Scholar]
- 28.Bhagat R.B. Conditions of SC/ST households: story of unequal improvement. Econ Pol Weekly. 2013;48:62–66. [Google Scholar]
- 29.Yusuf S., Hawken S., Oonpuu S. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 30.O’Donnell M.J., Chin S.L., Rangarajan S. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016;388:761–775. doi: 10.1016/S0140-6736(16)30506-2. [DOI] [PubMed] [Google Scholar]
- 31.Gupta R., Guptha S., Sharma K.K., Gupta A., Deedwania P.C. Regional variations in cardiovascular risk factors in India: india Heart Watch. World J Cardiol. 2012;4:112–120. doi: 10.4330/wjc.v4.i4.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang Y., Chen H.J., Shaikh S., Mathur P. Is obesity becoming a public health problem in India? Examine the shift form under- to overnutrition problems over time. Obes Rev. 2009;10:456–474. doi: 10.1111/j.1467-789X.2009.00568.x. [DOI] [PubMed] [Google Scholar]
- 33.Gupta R., Guptha S., Gupta V.P., Agrawal A., Gaur K., Deedwania P.C. Twenty year trends in cardiovascular risk factors in India and the influence of educational status. Eur J Prev Cardiol. 2012;19:1258–1271. doi: 10.1177/1741826711424567. [DOI] [PubMed] [Google Scholar]
- 34.Anchala R., Kannuri N.K., Pant H. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32:1170–1177. doi: 10.1097/HJH.0000000000000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gupta R. Recent trends in hypertension epidemiology in India. In: Deb P.K., editor. CSI Textbook of Cardiology. Cardiological Society of India; Kolkata: 2017. [Google Scholar]
- 36.Unnikrishnan R., Anjana R.M., Mohan V. Diabetes mellitus and its complications in India. Nat Rev Endocrinol. 2016;12:357–370. doi: 10.1038/nrendo.2016.53. [DOI] [PubMed] [Google Scholar]
- 37.Ranasinghe P., Mathangasinghe Y., Jayawardena R., Hills A.P., Misra A. Prevalence and trends of metabolic syndrome among adults in the Asia-Pacific region: a systemic review. BMC Public Health. 2017;17:101. doi: 10.1186/s12889-017-4041-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gupta R., Rao R.S., Misra A., Sharma S.K. Recent trends in epidemiology of dyslipidemias in India. Indian Heart J. 2017;69:382–392. doi: 10.1016/j.ihj.2017.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yusuf S., Joseph P. The epidemic of cardiovascular disease in South Asians: time for action. Am Heart J. 2017;185:150–153. doi: 10.1016/j.ahj.2016.11.009. [DOI] [PubMed] [Google Scholar]
- 40.Ebrahim S., Pearce N., Smeeth L., Casas J.P., Jaffar S., Piot P. Tackling non-communicable diseases in low- and middle-income countries: is the evidence from high-income countries all we need? PLoS Med. 2013;10:e1001377. doi: 10.1371/journal.pmed.1001377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bhan N., Karan A., Srivastava S., Selvaraj S., Subramanian S.V., Millet C. Have socioeconomic inequalities in tobacco use in India increased over time? Trends from the National Sample Surveys (2000–2012) Nicotine Tob Res. 2016;18:1711–1718. doi: 10.1093/ntr/ntw092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mishra S., Joseph R.A., Gupta P.C. Trends in bidi and cigarette smoking in India from 1998 to 2015 by age, gender and education. BMJ Glob Health. 2016;1:e000005. doi: 10.1136/bmjgh-2015-000005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gulati S., Misra A., Sharma M. Dietary fats and oils in India. Curr Diabetes Rev. 2017;13:438–443. doi: 10.2174/1573399812666160811165712. [DOI] [PubMed] [Google Scholar]
- 44.National Nutrition Monitoring Bureau . National Institute of Nutrition; Hyderabad: 2017. Diet and Nutritional Status of Urban Population in India and Prevalence of Obesity, Hypertension and Diabetes in Urban Men and Women. NNMB Brief Report on Nutrition. [Google Scholar]
- 45.Edayaranmula J.J. Alcohol and Drug Information Centre; Kerala: 2014. Alcohol Atlas of Kerala. [Google Scholar]
- 46.Gururaj G., Varghese M., Benegal V. National Institute of Mental Health and Neuro Sciences; Bengaluru: 2016. National Mental Health Survey of India, 2015-16: Summary NIMHANS Publication No. 128. [Google Scholar]
- 47.Panwar R.B., Gupta R., Gupta B.K. Atherothrombotic risk factors and premature coronary heart disease in India: a case-control study. Indian J Med Res. 2011;134:26–32. [PMC free article] [PubMed] [Google Scholar]
- 48.Iyengar S.S., Gupta R., Ravi S. Premature coronary artery disease in India: coronary artery disease in the young (CADY) registry. Indian Heart J. 2017;69:211–216. doi: 10.1016/j.ihj.2016.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sapru R.P. An overview of cardiovascular diseases in India. In: Wasir H.S., editor. Preventive Cardiology: An Introduction. Vikas Publishing House; New Delhi: 1991. pp. 69–86. [Google Scholar]
- 50.McKeigue P.M., Miller G.J., Marmot M.G. Coronary heart disease in south Asians overseas. J Clin Epidemiol. 1989;42:597–609. doi: 10.1016/0895-4356(89)90002-4. [DOI] [PubMed] [Google Scholar]
- 51.Zabaneh D., Chambers J.C., Elliott P., Scott J., Balding D.J., Kooner J.S. Heritability and genetic correlations of insulin resistance and component phenotypes in Asian Indian families using a multivariate analysis. Diabetologia. 2009;52:2585–2589. doi: 10.1007/s00125-009-1504-7. [DOI] [PubMed] [Google Scholar]
- 52.Tillin T., Hughes A.D., Mayet J. The relationship between metabolic risk factors and incident cardiovascular disease in Europeans, South Asians and African Caribbean: SABRE (Southall and Brent Revisited): a prospective population based study. J Am Coll Cardiol. 2013;61:1777–1786. doi: 10.1016/j.jacc.2012.12.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tan S.T., Scott W., Panoulas V. Coronary heart disease in Indian Asians. Global Cardiol Sci Pract. 2014;2014:4. doi: 10.5339/gcsp.2014.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jeemon P., Pettigrew K., Sainsbury C., Prabhakaran D., Padmanabhan S. Implications of discoveries from genome-wide association studies in current cardiovascular practice. World J Cardiol. 2011;3:230–247. doi: 10.4330/wjc.v3.i7.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Coronary Artery Disease (C4D) Genetics Consortium A genome wide association study in Europeans and South Asians identifies five new loci for coronary artery disease. Nat Genet. 2011;43:339–344. doi: 10.1038/ng.782. [DOI] [PubMed] [Google Scholar]
- 56.Chambers J.C., Abbott J., Zhang W. The south Asian genome. PLoS One. 2014;9:e102645. doi: 10.1371/journal.pone.0102645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nakatsuka N., Moorjani P., Rai N. The promise of discovering population specific disease associated genes in South Asia. Nat Genetics. 2017;49:1403–1407. doi: 10.1038/ng.3917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Reilly M.P., Li M., He J. Identification of ADAMTS7 as a novel locus for coronary atherosclerosis and association of ABO with myocardial infarction in the presence of coronary atherosclerosis: two genome wide association studies. Lancet. 2011;377:383–392. doi: 10.1016/S0140-6736(10)61996-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Khera A.V., Emdin C.A., Drake I. Genetic risk, adherence to a healthy lifestyle, and coronary disease. N Engl J Med. 2016;375:2349–2358. doi: 10.1056/NEJMoa1605086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Natarajan P., Young R., Stitziel N.O. Polygenic risk score identifies subgroup with higher burden of atherosclerosis and greater relative benefit from statin therapy in the primary prevention setting. Circulation. 2017;135:2091–2101. doi: 10.1161/CIRCULATIONAHA.116.024436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tada H., Melander O., Louie J.Z. Risk prediction by genetic risk scores for coronary heart disease is independent of family history. Eur Heart J. 2016;37:561–567. doi: 10.1093/eurheartj/ehv462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Boyle E.A., Li Y.I., Pritchard J.K. An expanded view of complex traits: from polygenic to omnigenic. Cell. 2017;169:1177–1186. doi: 10.1016/j.cell.2017.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Abraham G., Havulinna A.S., Bhalala O.G. Genomic prediction of coronary heart disease. Eur Heart J. 2016;37:3267–3278. doi: 10.1093/eurheartj/ehw450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Khera AV, Chaffin M, Aragam KG, Emdin CA, Klarin D, Haas ME, et al, Genome wide polygenic score to identify a monogenic risk-equivalent for coronary disease. bioRxiv. 2017. 10.1101/218388. [DOI]
- 65.Globus J.R., Stitziel N.O., Zhao W. Common and rare variants in CCR2, CCR5 or CX3CR1 and risk of atherosclerotic coronary heart disease ands glucometabolic traits. Circ Cardiovasc Genet. 2016;9:250–258. doi: 10.1161/CIRCGENETICS.115.001374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Salaheen D., Haycock P.C., Zhao W. Apolipoproein(a) isoform size, lipoprotein(a) concentration and coronary artery disease: a mendelian randomization analysis. Lancet Diabetes Endocrinol. 2017;5:524–533. doi: 10.1016/S2213-8587(17)30088-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jonsson A.L., Backhed F. Role of gut microbiota in atherosclerosis. Nature Rev Cardiol. 2017;14:79–87. doi: 10.1038/nrcardio.2016.183. [DOI] [PubMed] [Google Scholar]
- 68.O’Flaherty M., Buchan I., Capewell S. Contributions of treatment and lifestyle to declining CVD mortality: why have CVD mortality rates declined so much since the 1960’s. Heart. 2013;99:159–162. doi: 10.1136/heartjnl-2012-302300. [DOI] [PubMed] [Google Scholar]
- 69.Yusuf S., Rangarajan S., Teo K. Cardiovascular risk and events in 17 low-, middle- and high-income countries. N Engl J Med. 2014;371:818–827. doi: 10.1056/NEJMoa1311890. [DOI] [PubMed] [Google Scholar]
- 70.Spencer S. Lessons from the PURE study. Global Cardiol Sci Pract. 2014;4:e52. doi: 10.5339/gcsp.2014.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gupta R., Guptha S., Joshi R., Xavier D. Translating evidence into policy for cardiovascular disease control in India. Health Res Policy Syst. 2011;9:8. doi: 10.1186/1478-4505-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Devi P., Rao M., Sigamani A. Prevalence, risk factors, awareness, treatments, control and outcomes of hypertension in Asian Indians: a systematic review. J Human Hypertens. 2013;27:281–287. doi: 10.1038/jhh.2012.33. [DOI] [PubMed] [Google Scholar]
- 73.Chow C.K., Teo K.K., Rangarajan S. Prevalence, awareness, treatment and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310:959–968. doi: 10.1001/jama.2013.184182. [DOI] [PubMed] [Google Scholar]
- 74.Joshi S.R. Diabetes care in India. Ann Glob Health. 2015;81:830–838. doi: 10.1016/j.aogh.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 75.Gupta A., Gupta R., Sharma K.K. Prevalence of diabetes and cardiovascular risk factors in middle-class urban populations in India. BMJ Open Diab Res Care. 2014;2:e000048. doi: 10.1136/bmjdrc-2014-000048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lear S., Hu W., Rangarajan S. The effect of physical activity on mortality and cardiovascular disease in 130,000 people from 17 high-income, middle-income and low-income countries: the PURE Study. Lancet. 2017;390:2643–2654. doi: 10.1016/S0140-6736(17)31634-3. [DOI] [PubMed] [Google Scholar]
- 77.Dehgan M., Mente A., Zhang X. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet. 2017;390:2050–2062. doi: 10.1016/S0140-6736(17)32252-3. [DOI] [PubMed] [Google Scholar]
- 78.Miller V., Mente A., Dehghan M. Fruit, vegetable, and legume intake, and cardiovascular disease and deaths in 18 countries (PURE): a prospective cohort study. Lancet. 2017;390:2037–2049. doi: 10.1016/S0140-6736(17)32253-5. [DOI] [PubMed] [Google Scholar]
- 79.Gupta R., Gupta V.P., Agrawal A., Sharma K.K., Prakash H., Deedwania P.C. 25-year trends in hypertension prevalence, awareness, treatment and control in an urban population in India. Indian Heart J. 2017 doi: 10.1016/j.ihj.2017.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gupta R., Deedwania P.C. Interventions for cardiovascular disease prevention. Cardiol Clin. 2011;29:15–34. doi: 10.1016/j.ccl.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 81.Editorial. India: a tale of many countries but stories of many states. Lancet. 2017;390:2413. doi: 10.1016/S0140-6736(17)32867-2. [DOI] [PubMed] [Google Scholar]
- 82.Prabhakaran D., Anand S., Watkins D. Cardiovascular, respiratory, and related disorders: key messages from Disease Control Priorities, 3rd edition. Lancet. 2017 doi: 10.1016/S0140-6736(17)32471-6. pii: S0140-6736(17)32471-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Jamison D.T., Alwan A., Mock C.N. Universal health coverage and inter-sectoral action for health: key messages from Disease Control Priorities, 3rd edition. Lancet. 2017 doi: 10.1016/S0140-6736(17)32906-9. pii: S0140-6736(17)32906-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Misriya K.J., Sudhayakumar N., Khadar S.A., George R., Jayaprakash V.L., Pappachan J.M. The clinical spectrum of acute coronary syndromes: experience from a major centre in Kerala. J Assoc Phys India. 2009;57:377–383. [PubMed] [Google Scholar]
- 85.Mohanan P.P., Mathew R., Harikrishnan S. Presentation, management and outcomes of 25748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS Registry. Eur Heart J. 2013;34:121–129. doi: 10.1093/eurheartj/ehs219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Negi P.C., Merwaha R., Pandey D., Chauhan V., Guleri R. Multicenter himachal pradesh ACS registry. Indian Heart J. 2016;68:118–127. doi: 10.1016/j.ihj.2015.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pagidapatti N., Huffman M., Jeemon P. Association between gender, process of care measures, and outcomes in ACS in India: results from the detection and management of coronary heart disease (DEMAT) registry. PLoS One. 2013;8:e062061. doi: 10.1371/journal.pone.0062061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Sharma M., Bharani A., Chadha D.S. Rationale, design and feasibility of a nationwide prospective registry of management of acute coronary events (MACE) in India. Abstract. Am J Med. 2016;11(Suppl):e103. [Google Scholar]
- 89.Isezuo S., Subban V., Krishnamoorthy J. Characteristics, treatment and one-year outcomes of patients with acute coronary syndrome in a tertiary hospital in India. Indian Heart J. 2014;66:156–163. doi: 10.1016/j.ihj.2013.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Kaul U., Seth A., Arambam P. Safety of prasugrel in Indian patients: multicentric registry of 1000 cases. Indian Heart J. 2014;66:598–601. doi: 10.1016/j.ihj.2014.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Xavier D., Gupta R., Sigamani A. Community health worker based intervention for adherence to medications and lifestyle modifications after acute coronary syndrome: a randomized controlled trial. Lancet Diab Endocrinol. 2016;4:244–253. doi: 10.1016/S2213-8587(15)00480-5. [DOI] [PubMed] [Google Scholar]
- 92.Fox K.A., Goodman S.G., Anderson F.A. From guidelines to clinical practice: the impact of hospital and geographic characteristics on temporal trends in the management of acute coronary syndromes. The Global Registry of Acute Coronary Events (GRACE) Eur Heart J. 2003;24:1414–1424. doi: 10.1016/s0195-668x(03)00315-4. [DOI] [PubMed] [Google Scholar]
- 93.Hasdal D., Behar S., Wallentin L. A prospective survey of the characteristics, treatments and outcomes of patients with acute coronary syndromes in Europe and the Mediterranean basin: the Euro Heart Survey of Acute Coronary Syndromes (EuroHeart Survey ACS) Eur Heart J. 2002;23:1190–1201. doi: 10.1053/euhj.2002.3193. [DOI] [PubMed] [Google Scholar]
- 94.Masoudi F.A., Ponirakis A., de Lemos J.A. Trends in US cardiovascular care: 2016 report from 4 ACC national cardiovascular data registries. J Am Coll Cardiol. 2017;69:1427–1450. doi: 10.1016/j.jacc.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 95.Szummer K., Wallentin L., Lindhagen L. Improved outcomes in patients with ST elevation myocardial infarction during the last 20 years are related to implementation of evidence based treatments: experiences from the SWEDEHEART registry 1995–2014. Eur Heart J. 2017;38:3056–3065. doi: 10.1093/eurheartj/ehx515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Puymirat E., Simon T., Cayla G. French ACS Registry. Acute myocardial infarction: changes in patient characteristics, management and 6-month outcomes over a period of 20 years in he FAST-AMI Program (French Registry of Acute ST-Elevation of Non-ST Elevation Myocardial Infarction) 1995–2015. Circulation. 2017;136:1908–1919. doi: 10.1161/CIRCULATIONAHA.117.030798. [DOI] [PubMed] [Google Scholar]
- 97.Huffman M., Mohanan P.P., Devarajan R. Acute coronary syndrome quality improvement in Kerala (ACS QUIK) Investigators. Effect of a quality Improvement Intervention on clinical outcomes in patients in India with acute myocardial infarction: the ACS QUIK randomized clinical trial. JAMA. 2018;319:567–578. doi: 10.1001/jama.2017.21906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mendis S., Abegunde D., Yusuf S. WHO study on prevention of recurrences of myocardial infarction and stroke (WHO-PREMISE) Bull WHO. 2005;83:820–829. [PMC free article] [PubMed] [Google Scholar]
- 99.Sharma K.K., Gupta R., Agrawal A. Low use of statins and other coronary secondary prevention therapies in primary and secondary care in India. Vasc Health Risk Manag. 2009;5:1007–1014. doi: 10.2147/vhrm.s8017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Joshi R., Chow C.K., Raju P.K. Fatal and nonfatal cardiovascular diedase and the use of therapies for secondary prevention in a rural region of India. Circulation. 2009;119:1950–1955. doi: 10.1161/CIRCULATIONAHA.108.819201. [DOI] [PubMed] [Google Scholar]
- 101.Kaul U., Natarajan S., Dalal J., Saran R.K. Prevalence and control of cardiovasculsr risk fac tors in stable coronary artery outpatients in India compared with the rest of the world: an analysis from international CLARIFY registry. Indian Heart J. 2017;69:447–452. doi: 10.1016/j.ihj.2017.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Yusuf S., Islam S., Chow C.K. Low use of secondary prevention medications for cardiovascular disease in the community in 17 high, middle and low income countries (The PURE Study) Lancet. 2011;378:1231–1243. doi: 10.1016/S0140-6736(11)61215-4. [DOI] [PubMed] [Google Scholar]
- 103.Gupta R., Mony P., Shankar K. Socioeconomic status and cardiovascular secondary prevention therapies in South Asia: the PURE Study. Eur J Prev Cardiol. 2015;22:1261–1271. doi: 10.1177/2047487314540386. [DOI] [PubMed] [Google Scholar]
- 104.Chattopadhyay K., Prabhakaran D., Manchanda S., Praveen P.A., Kinra S. Development process of a yoga-based cardiac rehabilitation programme (YOGACARE) Altern Integr Med. 2013;2:10. [Google Scholar]
- 105.Kotseva K., De Bacquer D., Jennings C. Time trends in lifestyle, risk factor control, and use of evidence baed medications in patients with coronary heart disease in Europe: results from 3 EUROASPIRE surveys, 1999–2013. Glob Heart. 2017;12:315–322. doi: 10.1016/j.gheart.2015.11.003. [DOI] [PubMed] [Google Scholar]
- 106.Madan K., Babu A.S., Contractor A.A., Sawhney J.P.S., Prabhakaran D., Gupta R. Cardiac rehabilitation in India. Progr Cardiovasc Dis. 2014;57:543–550. doi: 10.1016/j.pcad.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 107.Shah P., Misra A., Gupta N. Improvement in nutrition related knowledge and behaviour of urban Asian school children: findings from the Medical education for children/adolescents for realistic prevention of obesity and diabetes and for healthy aging (MARG) intervention study. Br J Nutr. 2010;104:427–436. doi: 10.1017/S0007114510000681. [DOI] [PubMed] [Google Scholar]
- 108.Pandey R.M., Agrawal A., Misra A. Population-based intervention for cardiovascular disease related knowledge and behaviours in Asian Indian women. Indian Heart J. 2013;65:40–47. doi: 10.1016/j.ihj.2012.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Fathima F.N., Joshi R., Agrawal T. Rationale and design of the primary prevention strategies at the community level to promote adherence of treatments to prevent cardiovascular diseases (PREPARE) trial. Am Heart J. 2013;166:4–12. doi: 10.1016/j.ahj.2013.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Jeemon P., Narayanan G., Kondal D. Task shifting of frontline community hearth workers for cardiovascular risk reduction: design and rationale of a cluster randomised controlled trial (DISHA study) in India. BMC Public Health. 2016;16:264. doi: 10.1186/s12889-016-2891-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ali M.K., Singh K., Kondal D. Effectiveness of a multicomponent quality improvmrnt strategy to improve achievement of diabetes care goals: a randomised controlled trial. Ann Intern Med. 2016;165:399–408. doi: 10.7326/M15-2807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Raja D.C., Subban V., Victor S.M. The impact of systems-of-care on pharmacoinvasive management with streptokinase: the subgroup analysis of the TN-STEMI programme. Indian Heart J. 2017;69:573–579. doi: 10.1016/j.ihj.2017.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Donkin A., Goldblatt P., Allen J., Nathanson V., Marmot M. Global action on the social determinants of health. BMJ Glob Health. 2018;3(Suppl 1):000603. doi: 10.1136/bmjgh-2017-000603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kumar A.K., Chen L.C., Choudhury M. Financing health care for all: challenges and opportunities. Lancet. 2011;377:668–679. doi: 10.1016/S0140-6736(10)61884-3. [DOI] [PubMed] [Google Scholar]
- 115.Gupta I., Chowdhury S. Public financing for health coverage in India: who spends, who benefits and at what cost? Econ Pol Weekly. 2014;35:30. [Google Scholar]