Abstract
Objective
To assess the factors contributing to longer total ischemic times in ST elevation myocardial infarction (STEMI) patients undergoing primary percutaneous coronary intervention (PPCI).
Methods
Three hundred forty-six patients who underwent PPCI from July 2016 to June 2017 were studied. From time for the patient to recognize the symptoms, time was divided into 11 stages, any reason for delay was observed.
Results
Mean window period was 6.7 ± 9.8 hours. Mean time to recognize the symptoms, reach first medical contact and prehospital management were 150.2 ± 140.5 min, 58.5 ± 57.0 min and 36.3 ± 38.0 min, respectively. Mean time for the patients brought in ambulance was 82.4 ± 59.8 min whereas for those transported in other vehicles was 130.4 ± 59.7 min (p = < 0.0001). Mean door to electrocardiogram (ECG) time, decision for PPCI, consent time and STEMI team activation time were 6.2 ± 3.1 min, 8.3 ± 4.5 min, 12.6 ± 16.2 min and 10.7 ± 8.2 min, respectively. Mean time for financial process and mean sheath to balloon time were 9.1 ± 6.9 min and 21.8 ± 11.7 min, respectively. Door to balloon time (DTB) was <90 min in 81% of the patients, mean DTB was 72.0 ± 33.0 min. Mean DTB for cases performed during night was 72.6 ± 32.9 min, whereas for those performed during day was 60.3 ± 30.2 min (p < 0.05). Total 30 day mortality was 2.9%. Mortality among DTB <90 min was 1.4%, mortality among DTB > 90 min was 9% (p < 0.05).
Conclusions
The main contributor for longer total ischemic time was the time taken for the patient to recognize the symptoms. DTB of <90 min can be achieved with effective hospital strategies.
Keywords: Time intervals, Total ischemic time, Primary percutaneous coronary intervention, Door to balloon time
1. Introduction
Globally, coronary artery disease (CAD) has reached epidemic proportions. While mortality from CAD is declining in developed countries, it is rapidly increasing in developing countries like India. There has been a 4-fold increase of CAD prevalence in India during the past 40 years. According to few national studies, the prevalence of CAD in India varies from 7%–13% in urban and 2%–7% in rural populations.1 According to the Create Registry, the incidence of STEMI is higher (60.6%) and the mortality is more (8.6%) in Indian population than that of developed countries.2 The above statistics necessitate urgent measures to restrain the risk factors and put forth effective treatment strategies in the management of CAD.
The current guidelines, based on multiple randomized clinical trials, recommend primary percutaneous coronary intervention (PPCI) as the preferred reperfusion strategy over thrombolysis in patients with ST elevation myocardial infarction (STEMI), provided it can be performed within 120 min from STEMI diagnosis.3 Patients undergoing PPCI were shown to have lower rates of nonfatal re-infarction, stroke, and short-term mortality than thrombolytic recipients.4 Outcomes after STEMI mainly depend on the early reperfusion of the infarct related coronary artery. Longer ischemic times are associated with increase in microvascular obstruction, which further increases the infarct size. The total ischemic time, measured from symptom onset to the provision of reperfusion therapy is thus of significant importance for the outcomes of patients with STEMI.5 There are fewer studies which assessed the factors that cause longer total ischemic time.6 We evaluated various determinants of total ischemic time and its significance on clinical outcomes in patients with STEMI treated with PPCI.
2. Objectives
To evaluate the various time intervals of total ischemic time.
To assess the factors which contribute to longer total ischemic time.
To determine whether longer total ischemic times is associated with adverse outcomes (mortality at 30 days).
3. Methods
This is a prospective, observational study involving patients who underwent PPCI in Department of Cardiology, Sri Venkateswara Institute of Medical Sciences, Tirupati, Andhra Pradesh, India, a tertiary cardiac centre, which has round the clock PPCI facility.7 The hospital has two state of the art cardiac catheterization laboratories and performed a total of 4433 catheterization procedures in 2016, out of which 1317 were PCIs.
3.1. Study population
The study included consecutive patients who underwent PPCI in our institute from July 2016 to June 2017.
3.2. Inclusion criteria
Patients presenting with STEMI within a window period of 12 hours and willing to undergo PPCI were included in the study.
3.3. Exclusion criteria
Patients who opted for thrombolysis were excluded.
The ethics committee of the institute cleared the study.
3.4. Study protocol
The data was documented by Intensive coronary care unit (ICCU) team who was blinded to the study objectives.
Total ischemic time was assumed to be sum of window period and door to balloon (DTB) time.
Window period was divided into
-
1
Time from the onset of chest pain to recognition of symptoms
-
2
Time to obtain first medical contact
-
3
Time for diagnosis and prehospital management
-
4
Time for transportation (Ambulance/Others)
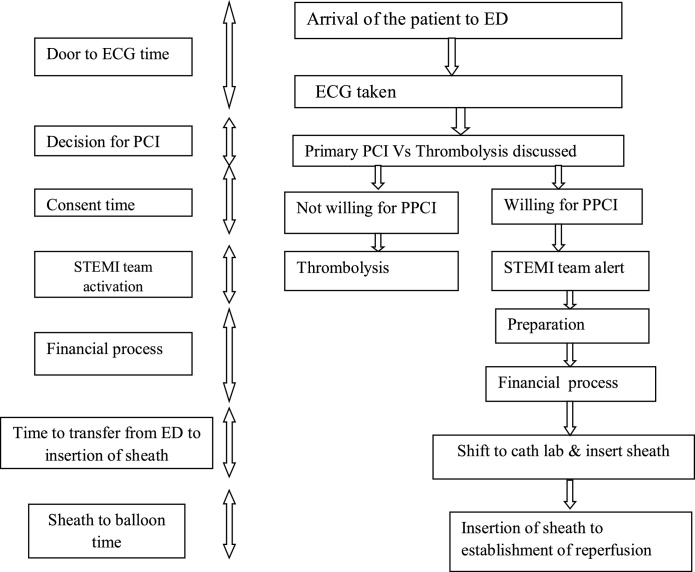
DTB time was divided into (Chart 1)
-
1
Door to electrocardiogram (ECG) time
-
2
Time for decision of PCI
-
3
Consent time
-
4
Time for STEMI team activation
-
5
Time for financial process
-
6
Time to transfer from emergency department to insertion of sheath
-
7
Time from sheath to balloon
Chart 1.
Depicting division of window period and door to ECG time.
First medical contact; ED: Emergency Department; ECG: Electrocardiogram; PPCI: Primary percutaneous coronary intervention; STEMI: ST elevation myocardial infarction.
Any delay and the reason for it were studied. PPCIs performed during day (8AM to 8PM) were included in subgroup A (Table 2) and compared with those (subgroup B) performed during night (8PM to 8AM). Total ischemic time was correlated with adverse outcomes (mortality at 30 days).
Table 2.
Subgroup analysis of the study group.
| Characteristic | Subgroup A (PPCI performed in day) | Subgroup B (PPCI performed in night) | p value |
|---|---|---|---|
| Age in years | 56.4 ± 13.1 | 54.2 ± 11.4 | 0.12 |
| EF% | 42.7 ± 8.6 | 44.4 ± 9.4 | 0.09 |
| Diabetes mellitus | 21% | 18% | 0.52 |
| Hypertension | 24% | 18% | 0.20 |
EF: Ejection fraction; PPCI: Primary percutaneous coronary intervention.
The institute has a tertiary cardiac centre with well-trained PPCI personnel and dedicated ICCU team round the clock. When the patient with symptoms suggestive of STEMI presented to emergency room, the time of arrival and the time variables of window period were noted by the duty team. As soon as the patient arrived, ECG technician was called and the door to ECG time was noted. The ECG was assessed by the cardiologist. After a quick clinical examination, decision for PPCI was made and the time taken for decision was recorded. Benefits and risks of PPCI were explained to the patient’s relatives and consent was taken. Time to consent was recorded. Meanwhile the STEMI team was alerted and catheterization laboratory made ready. Most of the patients undergoing PPCI were included in Government insurance scheme and time taken for the financial process to be completed was noted. Time taken to shift the patient from emergency to catheterization laboratory was noted. After the onset of procedure, the time taken for the establishment of reperfusion was noted. The causes for any delay were documented.
Post PPCI, patients were monitored in ICCU and were discharged on dual antiplatelet therapy on day 5 post PPCI. Patients were followed up at 30 days and any adverse events including mortality were documented.
4. Definitions
4.1. STEMI
Angina or angina equivalent with at least 2 contiguous leads showing ST elevation ≥2.5 mm in men < 40 years, ≥2 mm in men ≥ 40 years or ≥1.5 mm in women in leads V2-V3 and/or ≥1 mm in the other leads (in the absence of left ventricular hypertrophy or left bundle branch block. ST segment elevation ≥0.5 mm in leads V7-V9 was considered as means to identify posterior MI.3
4.2. Window period
Time from the onset of chest pain to the arrival at PPCI facilitated centre.
4.3. Door to balloon time
Time from first hospital arrival to the establishment of reperfusion.
4.4. Total ischemic time
Time from symptom onset to the provision of reperfusion therapy.
4.5. Systemic hypertension
Systolic blood pressure >140 mmHg and or diastolic pressure >90 mmHg, or on treatment.
4.6. Diabetes mellitus
Fasting blood sugar of ≥126 mg/dl or random blood sugar of ≥200 mg/dl or HbA1C of ≥6.5% or on treatment.
4.7. Dyslipidemia
Fasting cholesterol >200 mg/dl or on treatment.
5. Statistical analysis
All the statistical analyses were performed on Microsoft-excel spread sheets and Statistical Package for Social Science Software (SPSS) for Microsoft Windows, version 20.0, (IBM Corp., Armonk, NY, USA) MedCalc V.12.7.1.0. [MedCalc Software, Mariakerke, Belgium. Mean and standard deviation were calculated for all continuous variables. Percentages were calculated for all categorical variables. Unpaired student’s ‘t’ test was utilized to find out the difference between means and to calculate the significance level and p-value. A p value of <0.05 was considered statistically significant.
6. Results
A total of 346 patients underwent PPCI during study period. Table 1, Table 2 show baseline clinical and demographic characteristics and subgroup analysis of the study population respectively.
Table 1.
Baseline demographic and clinical characteristics of the study group.
| Characteristic | Number (%) |
|---|---|
| Age (Mean ± SD) in years | 55.3 ± 12.1 |
| Male gender | 277 (80%) |
| BMI (Mean ± SD) in kg/m2 | 25.7 ± 3.4 |
| EF% (Mean ± SD) | 43.6 ± 7.3 |
| Hypertension | 42% |
| Diabetes mellitus | 39% |
| Smoking | 32% |
| Family H/O CAD | 18% |
| Dyslipidemia | 30% |
| AWMI | 201 (56%) |
| IWMI | 145 (44%) |
| PPCIs performed during day (sub group A) | 230 (66%) |
SD: Standard deviation; BMI: Body mass index; EF: Ejection fraction; CAD: Coronary artery disease; AWMI: Anterior wall myocardial infarction; IWMI: Inferior wall myocardial infarction; PPCI: Primary percutaneous coronary intervention.
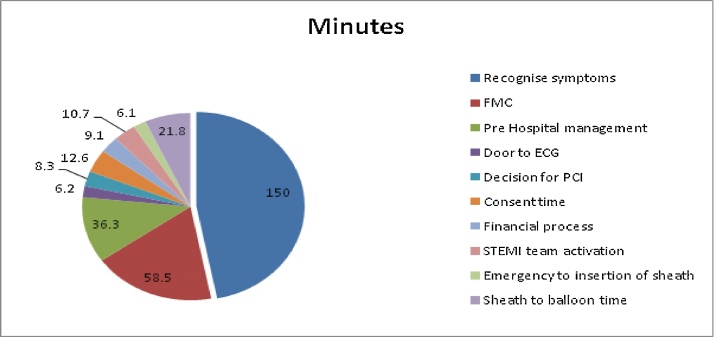
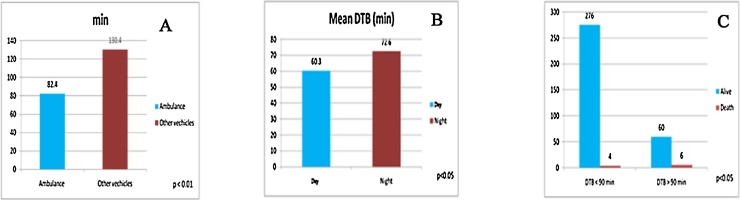
Mean window period was 6.7 ± 9.8 hours. Mean time to recognize the symptoms, reach first medical contact and prehospital management were 150.2 ± 140.5 min, 58.5 ± 57.0 min and 36.3 ± 38.0 min respectively (Fig. 1). Ambulance (108 & private) was the mode of transport in 60% of the patients and the mean time was 82.4 ± 59.8 min (Fig. 2a). Mean time for the patients transported in other vehicles was 130.4 ± 59.7 min (p = < 0.05). Mean door to ECG time, decision for PCI, consent time and STEMI team activation time were 6.2 ± 3.1 min, 8.3 ± 4.5 min, 12.6 ± 16.2 min and 10.7 ± 8.2 min, respectively. Mean time for financial processes, mean time taken to transfer the patient from emergency to insertion of sheath and mean sheath to balloon time were 9.1 ± 6.9 min, 6.1 ± 5.1 min and 21.8 ± 11.7 min, respectively.
Fig. 1.
Pie diagram depicting various time intervals of total ischemic time. FMC: First medical contact; ECG; Electrocardiogram; PCI: Percutaneous coronary intervention; STEMI: ST elevation myocardial infarction.
Fig. 2.
(a) Bar diagram showing transportation time in ambulance and other vehicles. Mean transportation time was less and statistically significant (p < .01) for those transported in ambulance. (b). Bar diagram comparing door to balloon time among cases those performed in the day and night. (c). Bar diagram comparing mortality among patients with door to balloon time of less than and more than 90 min. DTB: Door to balloon time; min: Minutes.
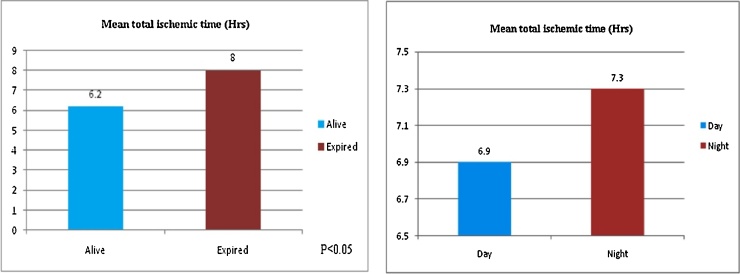
DTB time was <90 min in 81% of the patients, mean DTB was 72.0 ± 33.0 min, median time was 70 min and range was from 25 to 200 min. Mean DTB for cases performed during night was 72.6 ± 32.9 min (Fig. 2b), whereas for those performed during day was 60.3 ± 30.2 min (p < 0.05). Mortality at 30 days among <90 min was 1.4%, (Fig. 2c) mortality among >90 min was 9% (p < 0.05). Mean total ischemic time was 7.1 ± 3.2 hours. Mean total ischemic time for cases performed during day was 6.9 ± 3.0 hours (Fig. 3a) whereas for those performed during night was 7.3 ± 3.5 hours (p = 0.25). Total 30-day mortality was 2.9%. Mean total ischemic time among expired patients was 8.0 ± 3.6 h (Fig. 3b) whereas that among alive patients was 6.2 ± 2.8 hours (p < 0.05).
Fig. 3.
(a) Bar diagram showing subgroup analysis of mean total ischemic time. (b) Bar diagram showing mean total ischemic time in alive and dead patients. Hrs: Hours.
7. Discussion
In this prospective study, we found that the mortality rates were higher with longer DTB and total ischemic times. Several studies have established the fact that by achieving lesser DTB and total ischemic times, the mortality rates in patients undergoing PPCI can be decreased.8, 9, 10 Our findings support the current guideline-based recommendations for rapid PCI.
In our study most of the study population was from rural India and mean age was 55.3 years and 80% were males. Hypertension was the most common risk factor (40%) in our study unlike in other studies where Diabetes mellitus was found to be most common.6,11 Other traditional risk factors like smoking, dyslipidemia, family history were also prevalent in our study.
Mean window period was 6.7 hours which is longer than that in Create Registry2 (5 hours) and the main delay was time taken for the patient to recognize the symptoms (150 min). The Kerala ACS Registry12 also states that STEMI patients were more likely to present 6 hours after symptom onset. This delay was mainly due to lack of knowledge about the symptoms of ischemia among rural population. The ambulance was the mode of transport in only 60% of study population and is higher when compared to that in Create Registry (5.5%),2 but very low when compared to that in Western countries. Though some studies suggest that delays in the delivery of PPCI are important only within the first 2 or 3 hours after the onset of symptoms,13 in a rural setup of India achieving this is very challenging due to lack of adequate infrastructure and trained manpower. Based on these results, a strong emphasis should be made to initiate spoke and hub model, which could hold potential for middle- and low-income countries where treatment for and survival from STEMI are suboptimal. This experimental model initiated in Tamil Nadu in 2013, was successful in increasing the percentage of patients by three times who underwent PPCI and improved mortality at 1 year in a rural, impoverished region.14
Mean DTB was 72 min, which is at par with several other studies and also well within the international recommendations. DTB was <90 min in 81% of the patients. Mean DTB was significantly lower for the cases performed during day than during night. Delay in STEMI team activation was found to be the major factor prolonging DTB for the cases performed during night. Mean time taken for financial process was less in our study when compared to other studies and this is mainly due to Government insurance scheme, which was availed by most of our study population. Mean total ischemic time was 7.1 hours, which is high when compared to other Indian studies.11,15 Mean total ischemic time was significantly higher in expired patients, which is similar to the study conducted by Terkelsen CJ et al.16 Mean total ischemic time did not significantly vary among two subgroups. Despite achieving DTB of <90 min in 81% of the study population, longer window period was the major factor for longer total ischemic time. Mortality at 30 days was 2.9% which is far less when compared to other Indian studies.2, 11, 12 Mortality was significantly higher in patients who had DTB of >90 min. This again emphasizes the fact that longer intervals between the onset of symptoms and balloon time correlate with poorer outcomes.
More effective strategies like creating awareness among population regarding identification of ischemic symptoms and gaining of immediate access to health services, introduction of spoke and hub model, increasing use of prehospital ECGs, direct activation of the STEMI team by emergency medicine physicians without routine cardiology consultation, establishment of a single-call system for activating the entire STEMI team, establishment of time fixation for STEMI team members such that they will be available to receive the patient within 20–30 min, quick clearance of elective cases during routine work hours, allocation of dedicated night STEMI team on rotation would minimize the time intervals and help in improving the mortality rates.
8. Limitations
This is a single centre observational study conducted in a tertiary care hospital with limited applicability to the rest of the country. Follow up would have been for longer duration for better assessment of outcomes. Few patients were treated with DTB times greater than guideline recommendations.
9. Conclusion
Time taken for the patient to recognize symptoms and transportation time were the major factors for longer total ischemic time, which is in turn associated with higher mortality rates. Public awareness, establishment of proper infrastructure, efficient health schemes along with effective hospital strategies are utmost important factors in cutting down total ischemic time and thus help in achieving lesser mortality rates among patients undergoing PPCI for STEMI.
Source of funding
None
Conflict of interest
None
Acknowledgement
None
Contributor Information
Sreenivasa Reddy Doddipalli, Email: drsreenivasadoddipalli@gmail.com.
D. Rajasekhar, Email: cardiologysvims@gmail.com.
V. Vanajakshamma, Email: vvanaja1966@yahoo.in.
K. Sreedhar Naik, Email: sreedhar.k98@gmail.com.
References
- 1.Krishnan M.N. Coronary heart disease and risk factors in India – on the brink of an epidemic. Indian Heart J. 2012;64:364–367. doi: 10.1016/j.ihj.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xavier D., Pais P., Devereaux P.J. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371(9622) doi: 10.1016/S0140-6736(08)60623-6. [1435e1442] [DOI] [PubMed] [Google Scholar]
- 3.Ibanez B., James S., Agewall S. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2017;(August) [Google Scholar]
- 4.Mullasari A. Strategy of in ambulance thrombolysis followed by routine PCI in acute myocardial infarction. Indian Heart J. 2009;61:448e453. [PubMed] [Google Scholar]
- 5.Fokkema M.L., Wieringa W.G., van der Horst I.C., Boersma E., Zijlstra F., de Smet B.J. Quantitative analysis of the impact of total ischemic time on myocardial perfusion and clinicaloutcome in patients with ST-elevation myocardial infarction. Am J Cardiol. 2011;108:1536–1541. doi: 10.1016/j.amjcard.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 6.Victor S.M., Gnanaraj A., Pattabiram S.V., Mullasari A.S. Door-to-balloon: where do we lose time: single centre experience in India. Indian Heart J. 2012;64:582–587. doi: 10.1016/j.ihj.2012.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rajasekhar D., Vanajakshamma V., Vamsidhar A., Babu M.B., Latheef K. Experience of primary percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction at a referral healthcare centre in India. Natl Med J India. 2015;28(6 (November–December)):276–279. [PubMed] [Google Scholar]
- 8.McNamara R.L., Wang Y., Herrin J. Effect of door-to balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006;47:2180–2186. doi: 10.1016/j.jacc.2005.12.072. [DOI] [PubMed] [Google Scholar]
- 9.Rathore S.S., Curtis J.P., Chen J. Association of door-to balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: national cohort study. BMJ. 2009;338:b1807. doi: 10.1136/bmj.b1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berger P.B., Ellis S.G., Holmes D.R., Jr Relationship between delay in performing direct coronary angioplasty and early clinical outcome in patients with acute myocardial infarction: results from the Global Use of Strategies to Open Occluded Arteries in Acute Coronary Syndromes (GUSTO-IIb) Trial. Circulation. 1999;100:14e20. doi: 10.1161/01.cir.100.1.14. [DOI] [PubMed] [Google Scholar]
- 11.Subban V., Lakshmanan A., Victor S.M. Outcome of primary PCI – an Indian tertiary care center experience. Indian Heart J. 2014;66:25–30. doi: 10.1016/j.ihj.2013.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mohanan P.P., Mathew R., Harikrishnan S. Presentation, management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS Registry. Eur Heart J. 2013;34:121–129. doi: 10.1093/eurheartj/ehs219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nallamothu B.K., Bradley E.H., Krumholz H.M. Time to treatment in primary percutaneous coronary intervention. N Engl J Med. 2007;357:1631–1638. doi: 10.1056/NEJMra065985. [DOI] [PubMed] [Google Scholar]
- 14.Alexander T., Mullasari A.S., Joseph G. A system of care for patients with ST-Segment elevation myocardial infarction in India: the tamil nadu-ST-Segment elevation myocardial infarction program. JAMA Cardiol. 2017;2:498–505. doi: 10.1001/jamacardio.2016.5977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dubey G., Verma S.K., Bahl V.K. Primary percutaneous coronary intervention for acute ST elevation myocardial infarction: outcomes and determinants of outcomes: a tertiary care center study from North India. Indian Heart J. 2017;69:294–298. doi: 10.1016/j.ihj.2016.11.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Terkelsen C.J., Sørensen J.T., Maeng M. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304:763–771. doi: 10.1001/jama.2010.1139. [DOI] [PubMed] [Google Scholar]