Abstract
Objective:
Gay, bisexual, and other men who have sex with men (GBMSM) remain at high risk of HIV infection via condomless anal sex. Sexually explicit media (SEM) likely influences GBMSM’s sexual behavior and has been associated with condomless anal sex. SEM messages may be especially potent during formative developmental periods.
Methods:
We examined the association between age of first SEM exposure and condomless anal sex in a sample of adult GBMSM (N = 1,114) recruited using the internet.
Results:
Every one-year delay in age of first SEM exposure resulted in a 3% decrease in the odds of engaging in condomless anal sex as an adult (OR=.97, [.95, .99], p=.01). This association remained significant in three separate multivariable models that controlled for age of sexual debut, age of anal sex debut, and current age, respectively. This association was moderated by ethnicity such that the effect was stronger among Latino men.
Conclusions:
GBMSM who were exposed to SEM earlier in their lives report more sexual risk behavior as adults. SEM exposure in GBMSM is an important sexual development milestone deserving further research.
Keywords: sexually explicit media, men who have sex with men, sexual debut, sexual development, condomless sex
Gay, bisexual, and other men who have sex with men (GBMSM) come of age with relatively few models or resources to guide the development of safe, healthy sexual behavior (e.g., Mustanski, Newcomb, DuBois, & Garcia, 2011). Because (a) early sexual experiences influence later sexual behaviors and (b) GBMSM remain disproportionately impacted by HIV in the United States (CDC, 2016a), increased knowledge of how early sexual experiences shape adult sexual behavior among GBMSM can inform and improve HIV prevention efforts.
One of the few sexual “resources” available to young GBMSM is sexually explicit media (SEM; i.e., pornography). GBMSM use SEM to become comfortable with their sexuality and to learn about social-sexual norms and expectations (Nelson, Leickly, Yang, Pereira, & Simoni, 2014). Viewing SEM that portrays condomless anal sex undermines safer sex intentions (Jonas, Hawk, Vastenburg, & de Groot, 2014) and suggests that condomless anal sex is normative (e.g., Nelson et al., 2014; Scrimshaw, Antebi-Gruszka, & Downing, 2016).
SEM exposure may be especially potent when received during a formative developmental period. Using a heterosexual sample, Sinkovic, Stulhofer, and Bozic (2013) found that earlier exposure to SEM was associated with greater sexual risk-taking later in life. As research has also documented associations between early sexual development and adult sexual risk behavior among GBMSM (e.g., Outlaw et al., 2011), early exposure to SEM may be related to later sexual risk behaviors in this population.
The current study investigated associations between early SEM exposure and condomless sexual behavior among adult GBMSM. Our analyses controlled for other markers of sexual behavior development (e.g., age of sexual debut, age of anal sex debut, current age) and, given the racial disparities in the HIV epidemic (CDC, 2016a), we also explored differences by race/ethnicity and HIV status. We hypothesized that (a) early SEM exposure would be associated with adult sexual risk behavior, and that (b) this effect would remain after controlling for other sexual milestones and current age (i.e., an indicator of the sociopolitical climate in which participants came of age). We had no a priori hypotheses regarding differences in the associations across HIV-status or race/ethnicity.
Methods
Procedures
This cross-sectional study enrolled GBMSM online in 2012 (see Nelson et al., 2014 for recruitment procedures). Participants were recruited via GBMSM websites (e.g., Men4Now.com, Recon.com, BGCLive.com, BearCentral.com, BearNation.us, Craigslist) and Facebook. Eligibility criteria included (a) being ≥ 18 years old, (b) identifying as male, and (c) in the past year, having had sex with another male, accessed a GBMSM website, and used online SEM. Participants completed a 30-minute survey and were offered entrance into a drawing for fifteen $50 gift certificates. Study procedures were approved by the Institutional Review Board at the University of Washington.
Participants
For the current analyses, men were excluded if they reported their age of sexual debut as < 8 (n=53; one standard deviation below the average age of puberty among U.S. males, Herman-Giddens et al., 2012) or reported first exposure to SEM prior to age three (n=3; the age at which infants develop clear memories, CDC, 2016b). Men who were excluded were more likely to be HIV-positive (40% vs. 16%, p<.05), identify as Black (21% vs. 12%, p<.05), or identify as other (i.e., non-Black, non-White) race (12% vs. 5%, p<.05). There were no differences in age, income, or education (all ps>.05). The final sample included 1,114 GBMSM (see Table 1 for participant characteristics).
Table 1.
Summary statistics for study variables among adult gay, bisexual, and other men who have sex with men (N=1,114)
| M (SD) | Range | |
|---|---|---|
| Age | 37 (14) | 18-84 |
| Sexually explicit media exposure age | 15 (6) | 5-71 |
| Sexual debut age | 17 (6) | 8-60 |
| Anal sexual debut age | 20 (7) | 8-68 |
| n (%) | ||
| HIV-positive | 159 (14) | -- |
| White | 825 (74) | -- |
| Black/African-American | 138 (12) | -- |
| Other race | 77 (7) | |
| Multiracial | 66 (6) | -- |
| Latino | 98 (9) | -- |
| Condomless anal sex | 617 (56) | -- |
Other race = Asian, Native Hawaiian or other Pacific Islander, American Indian/Alaskan Native, or “other” racial identity
Measures
Demographics and HIV status.
Men reported their current age, race (i.e., White, Black/African-American, other race, or multiracial), ethnicity (i.e., Hispanic/Latino), and HIV status. Each racial and ethnic identity was categorized with dummy codes (e.g., 1 ‘Hispanic/Latino’, 0 ‘non-Hispanic/Latino). HIV status was coded as 1 ‘positive’ and 0 ‘negative/unknown’.
Age of first SEM exposure, sexual debut, and sexual behavior.
Men reported the age they first viewed SEM, age of voluntary general sexual debut, and age of voluntary anal sexual debut. Men reported the percentage of time they had used a condom during insertive or receptive anal sex over the past three months (none (0%), a little (1–24%), less than half (25–49%), half (50%), more than half (51–74%), most (75–99%), all (100%)).
Analytic Plan
The association between age of SEM exposure and recent condomless anal sex was assessed using a bivariate logistic regression model. The dependent variable was dichotomized (any condomless anal sex = 1; 100% condom use = 0) due to its distribution being bimodal (Hershberger, Fisher, & Reynolds, 2005). Due to high collinearity between covariates (VIF for covariates ranged from 9.86–22.01), it was not feasible to test a model with all covariates included. Three separate multivariable models controlled for: (1) age of general sexual debut, (2) age of anal sexual debut, and (3) current age. Secondary models tested whether race/ethnicity or HIV status moderated the association between age of SEM exposure and condomless anal sex. Analyses were conducted using Stata v. 14.
Results
Over half the sample (56%) reported recent condomless anal sex. The average age of first exposure to SEM was 15 (SD=6, range: 5–71), general sexual debut was 17 (SD = 6, range: 8–60), and anal sexual debut was 20 (SD = 7, range: 8–68). Age of SEM exposure was correlated with general sexual debut (r=.30, p<.05), anal sexual debut (r=.34, p<.05), current age (r=.40, p<.05), and recent condomless anal sex (r=−.08, p<.05).
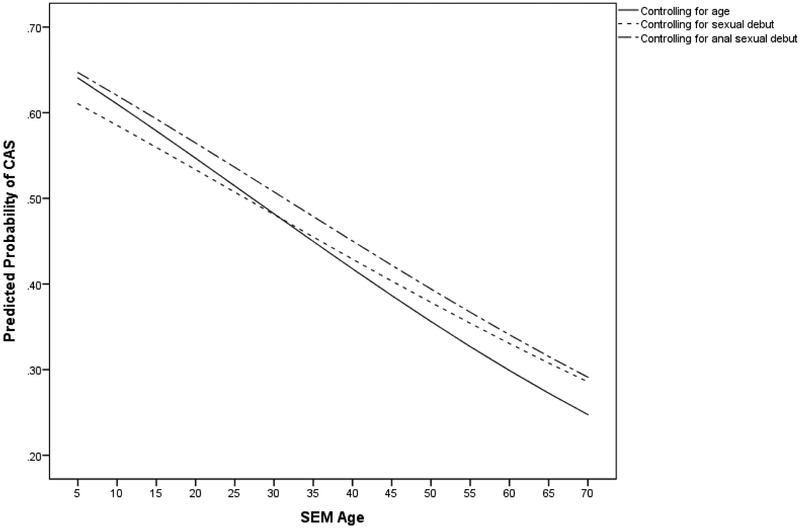
Every one-year delay in age at first SEM exposure resulted in a 3% decrease in the odds of engaging in recent condomless sex (OR=.97, [.95, .99], p=.01). This association remained significant when controlling for age of general sexual debut (AOR = .98 [.96, 1.0], p=.05), age of anal sex debut (AOR = .98, [.96, 1.0], p=0.03), and current age (AOR= .97, [.95, .99], p=.02) (see Figure 1).
Figure 1.
Graph of predicted probability of engaging in condomless anal sex by age of SEM exposure controlling for covariates
Note: Each line represents the association between CAS and SEM exposure when controlling for a covariate (i.e., current age, age of general sexual debut, age of anal sexual debut)
CAS = condomless anal sex; SEM = sexually explicit media
There were no significant differences in the association between age of SEM exposure and condomless anal sex by HIV status (p=.70) or race (ps>.06). There was a significant interaction with Latino ethnicity, such that the association between age of SEM exposure and adult sexual risk was stronger among Latino men (OR = .76, [.63, .90], p<.05) than among non-Latino men (OR = .98, [.96, 1.0], p<.05).
Exploratory Analyses
To explore potential explanations for why age of SEM exposure was related to adult sexual behavior, we tested whether results would change when controlling for frequency of recent SEM use or number of sexual partners. The association of SEM with condomless sex did not change in either model (controlling for recent SEM use: AOR=.97 [.95, .99]; controlling for number of recent sex partners: AOR = .97 [.95, .99]).
Discussion
In the current sample of GBMSM, age of SEM exposure was negatively associated with engagement in sexual risk behavior as an adult. Put another way, the younger an individual was when first exposed to SEM, the more likely they were to engage in sexual risk as an adult. The effect of SEM exposure persisted after controlling for other sexual milestones (i.e., general sexual debut, anal sex debut) known to be associated with later sexual risk behavior. Further, earlier age of SEM exposure was associated with earlier age of other sexual behavior debuts and preceded these other sexual milestones. Overall, these patterns suggest that early SEM exposure is important to the development of GBMSM sexuality and points to the possibility that first exposure to SEM may be a distinct sexual milestone for GBMSM.
We also observed a stronger association between age of SEM exposure and adult sexual behavior among Latino compared to non-Latino men. It is possible that cultural factors are relevant to this association given that differences in SEM use have been shown for other racial/ethnic minority populations. For example, research has documented racialized advertising on adult websites, as well as specific SEM content preferences among Black GBMSM (Nelson, Eaton, & Gamarel, 2016; White, Dunham, Rowley, Reisner, & Mimiaga, 2015). Similar research examining cultural beliefs that may influence SEM exposure and use among Latino GBMSM is needed to better understand the association found in this study.
Our findings suggest several directions for research on early sexual development among GBMSM. Almost all GBMSM report SEM use (e.g., Downing, Schrimshaw, Scheinmann, Antebi-Gruszka, & Hirshfield, 2016) and our results suggest that SEM exposure may be a sexual milestone. Thus, it will be important for future research to assess the optimal timing of SEM exposure for GBMSM and how to best prepare young males for their seemingly inevitable exposure. In addition, understanding how early sexual behaviors, including SEM exposure, interact with other sexual development processes (e.g., cognitive, biological) could further explicate the link between SEM exposure and sexual behavior in adulthood. This would valuably inform future sexual health interventions among GBMSM youth.
Results should be considered in the context of study limitations. First, the cross-sectional design precludes inferences regarding causality. Longitudinal designs capturing younger GBMSM prior to exposure are needed. Second, our SEM measure did not assess the context or content of that first exposure, which may affect relations with adult behavior. Third, all men in the study were required to have viewed SEM in the past year. Finally, because data were collected before widespread availability of pre-exposure prophylaxis (PrEP) for HIV prevention, our results focus on only one prevention behavior (i.e., condom use).
Overall, our results indicate that, for many GBMSM, early exposure to SEM may have an enduring effect on adult sexual behavior. Specifically, early SEM exposure is associated with condomless anal sex among adult GBMSM. Further, age of first SEM exposure precedes and is related to other sexual debut behaviors among GBMSM. Given these findings, SEM exposure may be a unique sexual developmental milestone among GBMSM and one with implications for later sexual health. Moving forward, researchers should work to understand where SEM use fits within the complex process of sexual development for young GBMSM in order to best support their sexual health.
References
- Centers for Disease Control and Prevention. HIV Surveillance Report, 2015; vol. 27 https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2015-vol-27.pdf Published November 2016a. Accessed September 25, 2017. [Google Scholar]
- Centers for Disease Control and Prevention. Developmental Milestones. https://www.cdc.gov/ncbddd/actearly/about.html. Published August 2016b. Accessed September 30, 2017.
- Downing MJ, Schrimshaw EW, Scheinmann R, Antebi-Gruszka N, & Hirshfield S (2016). Sexually explicit media use by sexual identity: A comparative analysis of gay, bisexual, and heterosexual men in the United States. Archives of Sexual Behavior, 1–14. [DOI] [PubMed] [Google Scholar]
- Herman-Giddens ME. ., Steffes J, Harris D, Slora E, Hussey M, Dowshen SA, Wasserman R, Serwint JR, Smitherman L, & Reiter EO (2012). Secondary sexual characteristics in boys: data from the pediatric research in office settings network. Pediatrics, 130, e1058–68. [DOI] [PubMed] [Google Scholar]
- Hershberger SL, Fisher DG, & Reynolds GL (2005). Modeling censored-in-the-middle condom use data. AIDS Care, 17 610–622. [DOI] [PubMed] [Google Scholar]
- Jonas KJ, Hawk ST, Vastenburg D, & de Groot P (2014). “Bareback” pornography consumption and safe-sex intentions of men having sex with men. Archives of Sexual Behavior, 43, 745–753. [DOI] [PubMed] [Google Scholar]
- Mustanski BS, Newcomb ME, Du Bois SN, Garcia SC, & Grov C (2011). HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. Journal of Sex Research, 48, 218–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson KM, Eaton LA, & Gamarel KE (2016). Preferences for condomless sex in sexually explicit media among Black/African American men who have sex with men: Implications for HIV prevention. Archives of Sexual Behavior, 46, 977–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson KM, Leickly E, Yang JP, Pereira A, & Simoni JM (2014). The influence of sexually explicit online media on sex: do men who have sex with men believe they “do what they see”? AIDS Care, 26, 931–934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson KM, Simoni JM, Morrison DM, George WH, Leickly E, Lengua LJ, & Hawes SE (2014). Sexually explicit online media and sexual risk among men who have sex with men in the United States. Archives of Sexual Behavior, 43, 833–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Outlaw AY, Phillips G, Hightow-Weidman LB, Fields SD, Hidalgo J, Halpern-Felsher B, & Green-Jones, and The Young MSM of Color SPNS Initiative Study Group. (2011). Age of MSM sexual debut and risk factors: results from a multisite study of racial/ethnic minority YMSM living with HIV. AIDS Patient Care and STDs, 25, S23–S29. [DOI] [PubMed] [Google Scholar]
- Scrimshaw EW, Antebi-Gruszka N, & Downing MJ Jr. (2016). Viewing of Internet-based sexually explicit media as a risk factor for condomless anal sex among men who have sex with men in four US cities. PloS One, 11(4), e0154439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinković M, Štulhofer A, & Božić J (2013). Revisiting the association between pornography use and risky sexual behaviors: The role of early exposure to pornography and sexual sensation seeking. Journal of Sex Research, 50, 633–641. [DOI] [PubMed] [Google Scholar]
- White JM, Dunham E, Rowley B, Reisner SL, & Mimiaga MJ (2015). Sexually explicit racialised media targeting men who have sex with men online: A content analysis of high-risk behaviour depicted in online advertisements. Culture, Health & Sexuality, 17, 1021–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]