Abstract
Objectives:
Current cardiovascular disease (CVD) nutrition guidelines do not take into account Chinese medicine (CM) principles. We created a heart healthy integrative nutritional counseling (H2INC) curriculum consistent with CM principles and current nutrition guidelines.
Methods:
We conducted three phases of semi-structured interviews with key stakeholders (CM and biomedical providers and Chinese Americans (CAs) patients with CVD) followed by iterative development of H2INC. First, we interviewed licensed CM providers (n=9) and laypeople with CM foods expertise (n=1). Second, we interviewed biomedical providers (n=11) and licensed CM providers (n=3). Third, we conducted four focus groups with CAs (n=20) with CVD.
Results:
Stakeholders emphasized different principles for creating H2INC. Phase one emphasized alignment of CM diagnoses to biomedical CVD conditions. Phase two overlaid CM concepts like the nature of foods and constitution (hot/neutral/cool) with heart healthy nutrition recommendations such MyPlate, and avoiding excess salt, fat, and sugars. Phase three demonstrated patient acceptability.
Conclusion:
By integrating CM foods principles with biomedical nutrition, this integrative approach yields culturally relevant health education for an underserved population.
Practice Implications:
Integrative nutritional counseling shows promise for CAs and can support biomedical providers with little knowledge about patients’ use of CM for CVD.
Keywords: nutrition, integrative medicine, cardiovascular health, cardiovascular disease, health education, dietary guidelines, Chinese medicine, prevention, Chinese Americans
1. Introduction
Asian Americans constitute the fastest growing racial/ethnic group in the U.S. [1] and the largest subgroup is the Chinese [2]. Between 20–36% of all Chinese Americans (CAs) report not speaking English well or at all [3]. In California, 56.2% of older CAs report limited English proficiency [4], which is associated with barriers to receiving optimal healthcare [5]. In California, the prevalence of hypertension in Chinese patients age 60+ was an estimated 53.6% [4]. Despite reductions in cardiovascular disease (CVD) mortality rates among non-Hispanic Whites, parallel patterns have not been observed in Asian American subgroups [6]. This suggests that interventions promoting prevention and management of CVD are not effectively targeting or made accessible to these populations [6].
Chinese immigrants are less likely to be familiar with U.S. dietary guidelines or food labels and more likely to rely on friends and Chinese newspapers for dietary information [7]. Some see Chinese medicine (CM) as a resource and means of practicing self-efficacy while maintaining a connection with their cultural roots [8]. Others prefer CM because they perceive it as more natural, non-toxic, and affordable [9]. CAs have used a hot/cold balance and traditional foods knowledge in their everyday approach to health and wellbeing [10]. CAs with CVD use traditional CM foods by eating tonic soups for managing their cardiovascular health [11, 12]. In one randomized controlled trial among hypertensive Chinese patients, patients that received CM diet with anti-hypertensive medications and brief health education had a reduction in the number of anti-hypertensive medications compared to patients that received anti-hypertensive medication and brief health education [13]. In other words, there are important practice implications for attending to cultural understandings of foods and health as an entry-point for preventative CVD health. Furthermore, Asian Americans who use complementary medicines disclose that usage to their biomedical providers at much lower rates than White patients [14]. Even when disclosure happens, providers may not know how to advise patients applying both a biomedical and integrative approach because few resources are available that integrate CM and biomedicine for nutrition [15].
To address cardiovascular health disparities among Chinese-speaking patients, linguistically and culturally accessible interventions based in CAs’ actual eating practices and food and health beliefs are needed [10, 16]. Herein, we describe the process of creating a heart healthy integrative nutritional counseling (H2INC) guide that integrates CM principles like balancing hot and cold with western biomedical principles of reducing calories, fat, and salt intake for preventative and early stage cardiovascular health. We incorporate foods commonly eaten in Chinese diets and use both Chinese and English to meet the varied linguistic needs of patients, families/caregivers, and healthcare providers. We describe our multi-disciplinary, iterative approach to create H2INC aimed to support culturally relevant care for CAs with CVD.
2. Methods
This formative, qualitative study was conducted in three phases designed to obtain stakeholder input on philosophical approaches to integration, iteratively create and refine a nutritional guide, and present our findings back to stakeholders. Because there is little guidance for integrating CM foods principles with biomedical nutritional guidelines [17], we adapted methods from grounded theory [18] and a Delphi-like method for achieving consensus [19]. We iteratively solicited expertise and feedback from key stakeholders, CM and biomedical providers and CA patients with CVD, to reach consensus for how to integrate two philosophically different nutritional systems [20]. We successfully used a similar approach to create an integrative nutritional counseling guide for type 2 diabetes [15, 21]. Grounded theory methods are especially useful in areas with little pre-existing research/theorizing.
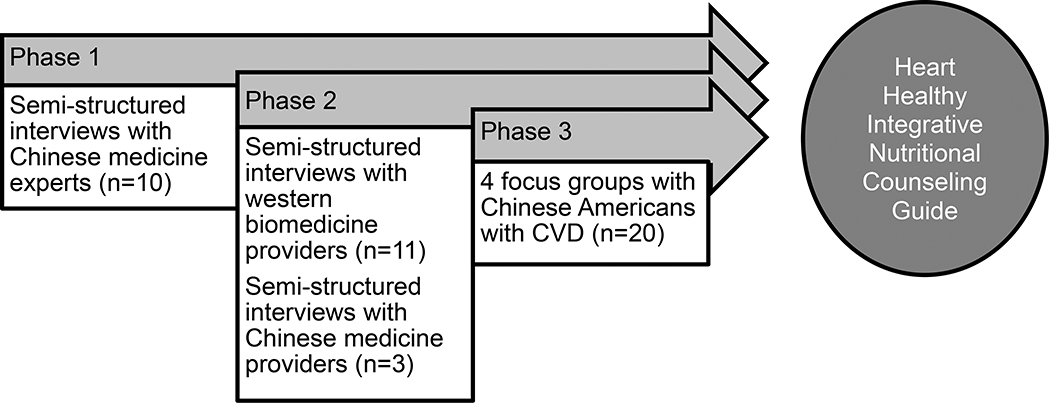
We purposively sampled relevant stakeholder populations in three phases to develop working standards towards integration of CM and biomedical nutritional recommendations to iteratively create H2INC within and between each phase (see Figure 1). Phase 1 consisted of semi-structured interviews with licensed and lay CM experts to learn about CM principles in heart health and nutrition. Phase 2 solicited feedback on the initial H2INC framework through semi-structured interviews with biomedical providers (e.g. primary care and specialist clinicians, dietitians) who care for CA patients followed by interviews with licensed CM experts not interviewed in Phase 1 to ensure we stayed consistent with CM nutritional principles. Phase 3 involved CAs with CVD who already incorporated CM principles or medicinal foods in their eating to elicit their suggestions and feedback on the content and design of H2INC. Although a true Delphi method solicits rank-ordered feedback from the same group of experts over multiple phases, variations have been used in previous research to solicit consensus of CM [22, 23]. During and after each phase of data collection, we iteratively analyzed data. This interim analysis provided a modified consensus-forming procedure, described in more detail below. All procedures were approved by the University of California, San Francisco (UCSF) and the University of San Francisco Institutional Review Boards.
Figure 1.
Iterative heart healthy integrative nutritional counseling guide development
2.1. Phase 1
In Phase 1, we conducted individual semi-structured interviews with CM experts (n=10) including licensed CM providers (LAc), physicians with a medical degree, a currently non-practicing CM professor, and a layperson with self-described expertise and family knowledge in the San Francisco Bay area. We purposively sampled this group because licensing in the U.S. does not require medicinal foods knowledge and many Chinese lay people pass this knowledge through families [8]. Participants with some expertise in using CM or medicinal foods for CVD conditions were recruited from CM schools and clinics and through snowball sampling. Nine interviews were conducted primarily in English with some Mandarin by the first author and one was conducted in Mandarin by a trained bicultural, bilingual research assistant (RA) who also transcribed and translated the interview. This interview was double-checked for accuracy by two other trained bicultural, bilingual RAs. After each interview, the first author open coded the transcripts to generate a spreadsheet of which CM diagnoses matched with which western medicine CVD conditions. An RA checked the list for accuracy based on interview transcripts. At the end of Phase 1, the research team (2 general internists, 1 licensed acupuncturist, 1 registered dietitian, 2 integrative CM researchers, and 1 Chinese language/community researcher reviewed the spreadsheet and culled the list of suggestions into a set of integrative principles. Suggestions were included if they met the criteria of being either acceptable or non-antithetical to: a) CM; b) biomedicine; c) nutrition; d) Chinese cultural practice. This integration was the most difficult part of this project, which will be fully presented in the results section.
2.2. Phase 2
We conducted a second phase of interviews to bring preliminary ideas to biomedical providers. We purposively sampled a variety of biomedically-trained providers who work with CA patients (primary care clinicians, CVD-related specialists, and dietitians). We presented the ideas generated from Phase 1 (such as hot/cold and seasonal eating) formed into our draft H2INC. In doing so, we asked if the information was accurate according to their medical opinions, if it would be suitable for their CA patients with CVD, and whether they had other suggestions. Because these interviews focused on collecting providers’ feedback as opposed to the generative nature of Phase 1 interviews, after each interview, two independent RAs open coded the transcripts to generate a list of suggestions for integration. The lists were compared and consolidated by a third RA, checked by the first author, and formed the basis for refining H2INC. The research team discussed the list of suggestions and decided what should be in/excluded. In Phase 2, we also solicited feedback from additional licensed CM providers that were not interviewed in Phase 1 to ensure that H2INC aligned with CM principles. We reached group consensus regarding content, then designed an initial draft in English and Chinese for patient stakeholder review.
2.3. Phase 3
During Phase 3, we recruited CAs patients from UCSF General Medicine clinic, which serves >25,000 patients including 21% of Asian ethnicity. We used the electronic health record to identify patients that had >1 clinic visit in the past year, indicated Cantonese or Mandarin as their preferred language and had ≥1 of the following CVD-related conditions: hypertension, dyslipidemia, coronary artery disease, cerebrovascular disease, or congestive heart failure. We randomly selected 200 potentially eligible Cantonese-speaking and 75 potentially eligible Mandarin-speaking patients and mailed recruitment letters in three mailings inviting participation in focus groups to learn about combining CM and western medicine for CVD nutrition guidelines. Interested patients contacted us by phone. Bilingual, bicultural RAs screened for eligibility of: (1) ≥1 self-reported CVD-related condition; 2) read Chinese; 3) used some form of CM or medicinal foods in the last 12 months. Four focus groups (three Cantonese-speaking and one Mandarin-speaking) with 3–9 participants each lasting 90-minutes were audio-recorded and conducted by bilingual, bicultural RAs between December 2017 and April 2018.
In each FG, participants completed a short socio-demographic survey and were shown preliminary pages of H2INC to elicit their feedback. Between each of the first three focus groups, we followed the same process of open coding and consolidation presented in Phase 2 and our research team discussed revisions to the H2INC draft guide and additional interview questions to ask in the next focus group.
2.4. Data Analysis
For qualitative data, in all phases of data collection, English-language interviews were professionally transcribed verbatim immediately after, checked for accuracy by the interviewer, and analyzed while ongoing data collection occurred. Chinese-language interviews were conducted and afterward simultaneously transcribed and translated into English by bicultural, bilingual RAs and double-checked by another RA. To describe the basic socio-demographics of study participants, we calculated means for continuous variables and proportions for categorical measures using Microsoft Excel.
3. Results
3.1. Participants
Phases 1 and 2 participant demographics are in Table 1. From Phase 1, 70% of CM experts were ethnically Chinese. Half were between 41 and 60 years old (M=49.38, ±14.79), and the nine who are licensed and/or trained in CM were relatively experienced (M=15.75 years practiced, ±10.69). Phase 2 providers (biomedical and CM) were also fairly experienced (M=16.08 years practiced, ±10.33). Because of our purposive sampling, we oversampled ethnically Chinese providers, and most also spoke Mandarin or Cantonese (n=11, 78.6%). Phase 3 patient participants (Table 2) were older (M=76.75 years old, ±7.15), female (70%), and all except one spoke English poorly or very poorly despite being in the U.S. for over two decades on average (M = 23.60 years, ±10.52). Most participants self-reported fair health status. The most common reported usage of CM was eating/preparing Chinese medicinal/herbal soups (n=12, 60%).
Table 1.
Phase 1 (n=10) & Phase 2 (n=14) Participant Demographics
| Phase 1 N (%) or mean ± SD | Phase 2 N (%) or mean ± SD | |
|---|---|---|
| Profession | ||
| Trained, Licensed Chinese medicine provider (MD or LAc)a | 8 (80) | 3 (21) |
| Trained, Non-licensed Chinese medicine educator | 1 (10) | 0 (0) |
| Lay Chinese medicine expert | 1 (10) | 4 (29) |
| Primary Care Clinicians (MD, NP, RN) | 0 (0) | 4 (29) |
| Medical specialist (MD) | 0 (0) | 3 (21) |
| Registered Dietician | ||
| Years in Practice, meanb | 15.75 ± 10.69 | 16.08 ± 10.33 |
| Chinese Languages Spokend | ||
| Cantonese | 3 (30) | 8 (57) |
| Mandarin | 6 (60) | 9 (64) |
| Toisan | 2 (20) | 0 (0) |
| Shanghainese | 0 (0) | 1 (7) |
| Gender | ||
| Female | 7 (70) | 6 (43) |
| Male | 3 (30) | 8 (57) |
| Age, years | 49.55 ± 13.57 e | 46.35 ± 16.30 |
| Ethnicity | ||
| Chinese | 7 (70) | 11 (79) |
| Taiwanese | 0 (0) | 1 (7) |
| Other Asian | 0 (0) | 2 (14) |
| Non-Asian | 3 (30) | 1 (7) |
Medical Doctors (MD) with acupuncture training can legally practice acupuncture similar to licensed acupuncturists (LAc)
Years in practice based on data from 8 participants in Phase 1 (missing n=1, not applicable for layperson n=1) and 13 participants in Phase 2 (missing n=1)
Some participants reported more than one answer, therefore the total is greater than the number of participants
Based on 9 participants, missing n=1
SD = standard deviation
NP = nurse practitioner
RN = registered nurse
Table 2.
Phase 3 Focus Group Participant Demographics (n=20)
| Participants N (%) or mean ±SD | |
|---|---|
| Gender | |
| Male | 6 (30) |
| Female | 14 (70) |
| Age, years | 76.75 ±7.15 |
| Languages spokena | |
| Cantonese | 11 (55) |
| Mandarin | 10 (50) |
| English (Limited) | 1 (5) |
| Chinese medicine usage within the last yeara | |
| Herbal soups/Chinese medicinal diet | 12 (60) |
| Herbs | 5 (25) |
| Acupuncture | 2 (10) |
| Other (phone app, books, cold treatment) | 2 (10) |
| Duration in the US, years | 23.60 ±10.52 |
| English proficiency | |
| Very well/Well | 1 (5) |
| Not well | 9 (45) |
| Not at all | 8 (40) |
| Don’t Know/not sure | 2 (10) |
| Self-reported health statusb | |
| Excellent/very good | 0 (0) |
| Good | 3 (16) |
| Fair | 13 (68) |
| Poor | 3 (16) |
| Cardiovascular disease diagnosesa | |
| Hypertension | 14 (70) |
| Dyslipidemia | 11 (55) |
| Heart arrhythmias | 5 (25) |
| Coronary artery disease | 3 (15) |
| Congestive heart failure | 1 (5) |
| Angina | 1(5) |
| Medicationsa | |
| Daily aspirin | 8 (40) |
| Statin medication | 14 (70) |
| Anti-hypertensive medication | 12 (60) |
| Non CVD-related medication | 9 (45) |
| Chinese medicinal herb capsule | 1 (5) |
Some participants reported more than one answer, therefore the total is greater than the number of participants and percentages may be greater than 100%.
Based on 19 participants, missing n=1
SD = standard deviation
3.2. Phase 1
An important challenge was how to align CM diagnoses to biomedical CVD conditions. In Phase 1, many participants expressed that CM does not have an equivalent to the western CVD conditions. The CM professor, explained:
“Because high cholesterol is just a lab result… it can be many different situations by Chinese medicine perspective. It depends on the individual… Maybe the person has no sickness based on Chinese medicine diagnosis.”
This disconnect between CM and western diagnosis was made more explicit speaking about the function of the heart, stating:
“In Chinese medicine, the heart is the ruler of the body.… Each organ system has a season that it correlates with. For the heart it’s the summer…. Heart houses the spirit. When there is phlegm blocking the heart, that’s going to change one’s mind and thinking.”
The heart, like all the other major organs is affiliated with a season, taste, color and direction. (see [24] for more information). Unlike in western medicine, the heart in CM does more than just pump blood.
While difficult to reconcile, each interviewee in Phase 1 was asked to try to align CM diagnoses with various CVD conditions (see Table 3). Participants aligned their diagnostic categories with dyslipidemia, hypertension, and cerebrovascular disease (Table 3) while acknowledging that CM does not fit exactly onto CVD conditions. To standardize across these suggestions, we collapsed these divisions into a broader set of CM diagnostic divisions of excess, deficiency, and dampness. Dampness was a special case because it and its related condition of “phlegm” align well with dyslipidemia and was mentioned by 7 out of 8 of the licensed acupuncturists. In CM, dampness suggests avoiding sweet, cold (e.g., ice cream), heavy or rich foods, and eating more warm (e.g., cooked not raw) vegetables and lean proteins, which align well with biomedical suggestions for dyslipidemia.
Table 3.
Integration of Chinese Medicine and Biomedical Conditions
| Chinese Medicine Conditiona | CM Simplification for Integration | Some Associated Biomedical Conditions or Symptoms | Final Integration |
|---|---|---|---|
| Heart yang deficiency | Yang deficiency | Cardiac failure, blood clots, | Deficiency |
| Heart yin deficiency | Yin deficiency | Hypertension, stroke, dyslipidemia, insomnia | Deficiency |
| Heart qi deficiency | Qi/blood deficiency | Palpitations, shortness of breath | Deficiency |
| Heart blood deficiency | Qi/blood deficiency | Palpitations, cardiac failure, dizziness, insomnia | Deficiency |
| Heart qi stagnation | Qi/blood stagnation | Heart attack | Excess |
| Blood stasis | Qi/blood stagnation | Angina, hypertension | Excess |
| Heart fire | Excess/heat | Palpitations | Excess |
| Yang rising | Excess/heat | Hypertension | Excess |
| Damp, spleen | Dampness/phlegm | Stroke, dyslipidemia, nodules, epilepsy, | Dampness |
| Damp/cold | Dampness/phlegm | Dyslipidemia | Dampness |
Not all Chinese medicine conditions are listed on this Table. The full list had over 100 conditions.
3.2.1. Iterative Development of H2INC after Phase 1
After Phase 1, the research team reduced the divisions into excess (e.g., too active/stressful, too much phlegm/weight) and those who are more deficient (e.g., too weak/frail either physically/mentally/emotionally). Because many CAs use hot/cold in making food decisions, which the layperson interviewee also mentioned (e.g., drink warming mustard green soup in the fall to cleanse the system), we decided the notion of hot/cold (proxy for excess/deficiency) and seasonal eating an acceptable lay vocabulary for discussing more complex CM components. Similar to biomedical heart healthy diets recommending whole foods and avoiding saturated fats and sugars, the variety of other suggestions listed aligned well with biomedical suggestions of eating lean meats, fruits, vegetables, whole grains, and legumes.
The first iteration of H2INC focused on hot/cold (excess/deficiency), dampness aligned with dyslipidemia, and seasonal eating. To take into account current heart healthy nutrition suggestions, we used a modified MyPlate (www.choosemyplate.gov) to show a good balance of vegetables, fruits, proteins, and carbohydrates, adding emphasis on reducing salt, fat, and processed foods. To assess the effect of dietary changes, we included a self-assessment about digestion, which was suggested by an interviewee. Finally, we choose a prevention focus with attention to hypertension (less salt) and dyslipidemia (less CM-determined “cold”/rich foods).
3.2. Phase 2
Because H2INC is designed for use in a western medicine clinical setting, Phase 2 interviews were useful for understanding biomedical provider engagement with CAs with CVD. We interviewed primary care clinicians, specialists and dietitians, and received feedback not just about integrating CM with western medicine, but also about how best to cook and shop for food, lifestyle and exercise recommendations, and suggestions for fat and salt intake.
Suggestions that cut across western medicine provider types included food and shopping suggestions across socioeconomic statuses; lowering the literacy level, and being aware of other factors affecting diet such as family structure and concurrent diseases such as diabetes. Similar to Phase 1, interviewees also talked about the importance of avoiding particularly unhealthy foods as one nephrologist explained, “it’s an enormous amount of energy to burn to counteract a doughnut and ice cream.” On the other hand, this idea of energy used to burn food, especially cold temperature and “sticky” foods like ice cream, was expanded upon by a nurse practitioner also going to acupuncture school. She stated, “if your body tends to feel more cold and then you already lack energy, then now you use more and more energy [to burn the cold food]… you’re going to run out of fuel.” In other words while there were similarities in the foods providers suggested that patients avoid, the explanation for why those should be avoided differed depending on what perspective (CM or western) the provider was using.
Providers also emphasized that CA’s frequency and intensity of exercise was often suboptimal. A nephrologist suggested:
“Really, we want to try to decrease people’s stress, increase people’s sleep, and then increase their movement. Getting them to sweat or be out of breath and then set a goal of working out up to five times a week, and maybe all of that will help you lose weight too… I think for my Chinese patients, especially older ones, I just tell them to walk just because I feel like in the older generation the concept of working out or going to gym is not so prevalent, and some of them have limited means anyways.”
Other providers had very patient-friendly suggestions to increase movement including walking up the steep hills of San Francisco or walking in shopping malls/stores.
Providers also raised the importance of possible drug-food interactions. The most commonly mentioned were black fungus and leafy green vegetables and their contraindications with blood thinning drugs such as warfarin. Their suggestions were to “tell your doctor” and “eat a consistent amount” so drug dosages could be accurately prescribed. Participants also suggested including other health education information like recognizing the signs of a stroke and warnings about how uncontrolled hypertension and dyslipidemia may lead to more serious CVD such as coronary artery disease and congestive heart failure.
Regarding some of the CM specific suggestions, participants were not opposed to seasonal eating and, in fact, a few mentioned that this could also be an easy way to get people to eat more whole and fresh foods. There was some skepticism considering that participants believed the most affordable food are often processed foods.
A digestion self-assessment included a checklist of signs of good and bad digestion according to CM. The most controversial aspects of the bad digestion column included such everyday experiences like gas, bloating, belching and bad breath. From a CM perspective, these are small signs that digestion is suboptimal. From our Phase 2 western providers, they wanted to add a note that these could actually be signs of something more serious than just digestion. While some providers were very skeptical, referring to this as “like the humors” and “simplistic,” others spoke about its utility for CA patients specifically. While participants did not fully support all of our suggestions, we also asked providers to determine which of our suggestions they could not professionally condone. When couched in the language of opposition, there were fewer concerns. As one neurologist said, “4000 years of history can’t be completely wrong… the only time I’d be really against it if it’s something we know, under western science that is not good.” It is in this area of non-opposition that much of our integration occurred.
To end Phase 2 interviews, we solicited feedback from three licensed CM providers. While one provider was particularly adamant about the need for CM to have individualized diagnoses (not our simplified ideas), the other providers were mostly supportive and emphasized the importance of CM’s idea of yin/yang and hot/neutral/cold over seasons especially in San Francisco, which has relatively mild seasonal change. One licensed acupuncturist provided a list of hot/neutral/cool foods and suggested we develop an additional self-assessment tool for patients to determine if patients are constitutionally cooler or warmer.
3.2.1. Iterative Development of H2INC after Phase 2
After Phase 2 consolidation and open coding, we decided on the following changes to H2INC. We added additional sections on lifestyle (e.g. managing stress and increasing sleep and exercise), a section on shopping and cooking tips directed to caregivers and families, and nutritional information focused on fat and salt intake. We developed a self-assessment tool for determining CM constitution and provided food lists of hot/neutral/cool foods. In preparation for the Phase 3 focus group interviews, we also took pictures of popularly-eaten Chinese foods and designed a cartoon figure of an older Chinese woman who appears throughout the guide.
3.3. Phase 3
The four focus groups elicited patient suggestions and demonstrated patient acceptance of H2INC. All participants were very interested in the prospect of having this resource. They reported this information a) was somewhat familiar to them; b) would help them make better health decisions; c) confirmed or expanded information they believed was relevant to their health.
Participants appreciated the hot/cold self-assessment tool we created. As one participant reacted:
“For me personally to say, I am more yin. I myself don’t have much expertise but I feel that I am more yin. So, for my children, sometimes they grow their own goji berry for me to eat, or make soup, if I eat a lot, my stomach will feel uncomfortable, like there is a lot of wind. Yes. So, I will remind myself to eat less.”
The participants spent quite a bit of time discussing their agreement or disagreement with various foods. For example, two participants said that egg is neutral though we had listed it as cold, and there were other disagreements over particular foods.
Surprisingly, even though participants acknowledged eating from bowls, they thought MyPlate was easier to visualize and understand than our adaptation using bowls. We had previously used bowls in a type 2 diabetes guide which was well-received by patients [15].
Finally, participants wanted to learn more about common food-drug and food-food interactions from a CM perspective, which we added. Other suggestions included clarity regarding some of the Chinese translations we had used and whether we were trying to develop a nutrition guide or a cooking guide. We stopped conducting focus groups because we reached a level of saturation in the suggestions and comments. Most comments from participants in the last two focus groups had more to do with whether certain foods were categorized correctly as hot or cold than they did in offering additional substantive suggestions for improvement.
3.3.1. Iterative Development of H2INC after Phase 3
After all three Phases of data collection and serial research team consensus-building meetings, we created the final H2INC guide. See Table 4 for a list of sections included or www.INCguide.org for the full guide.
Table 4.
H2INC Guide Topics
| 1. Introduction describing the integration of western and Chinese medicine |
| 2. Sample MyPlate-balanced meals and snacks for each season |
| 3. Description of yin-yang/hot-cold constitutional balance and self-assessment |
| 4. Picture lists of hot/neutral/cool foods |
| 5. MyPlate adaptation (vegetables ½ of your plate, proteins ¼ of plate, carbohydrates ¼ of plate and fruits instead of dairy on the side or as a snack) |
| 6. Suggestions for eating out |
| 7. Hypertension specific page of nutrition recommendations |
| 8. Dyslipidemia specific page of nutrition recommendations |
| 9. Tips for nutrition label reading, eating/drinking, cooking |
| 10. Lifestyle recommendations including guidance on stress, sleep, weight, physical activity including a TaiQi and QiGong movement |
| 11. Health warnings including signs of stroke and drug/food interactions |
| 12. Online resources in English and Chinese including seasonal lists of foods |
4. Discussion and Conclusion
4.1. Discussion
Through an iterative multi-disciplinary process involving CM and biomedical providers and CA patient stakeholders, we have created H2INC in English and Chinese languages, blending CM dietary principles and biomedical nutritional guidelines. H2INC may be a health education resource for both CA patients and healthcare providers and help support patient-provider communication about the use of CM/medicinal foods within the context of CVD care in healthcare settings. There are limited existing interventions that address the cultural and linguistic needs of CAs with CVD, particularly those that use CM. H2INC is a novel patient-centered contribution to address this gap.
As our results demonstrate, creating H2INC is neither simple nor straightforward. This whole process has taken nearly 24 months. However, we believe the time taken to reach out to important stakeholders has led to a better and more acceptable guide. Similar to previous research attempting to integrate CM with western medicine, a major challenge is in trying to standardize an individualized therapy such as CM [21]. Many areas of disagreement were resolved in consensus-building facilitated by shared values within our interdisciplinary research team to improve the health of CAs.
While the guide may not be fully CM, it does provide an important resource for CA patients who are hungry for more medically-validated advice about CM [25]. This research also demonstrates that biomedical providers are also interested in having integrative resources available to share with their CA patients.
Limitations of our work include a convenience sample and small sample sizes of CM and biomedical providers and CA patients with CVD from one geographic region. Furthermore, given the lack of systematic guidance on how to integrate CM and biomedical nutrition principles, the process by which we developed H2INC was more a subjective than objective process, largely guided by local expert opinion and shared desire to achieve consensus. Lastly, the H2INC guide may not be fully generalizable to the broad CA population in the U.S. as there is regional variation of immigration patterns and cultural practices from Chinese-speaking countries. Strengths of our work include a multi-disciplinary, iterative approach to develop H2INC, involvement of CM and biomedical providers as well as CA patients with CVD, and a novel bilingual education resource that is relevant to both patients and providers.
4.2. Conclusion
We have presented the process involved in creating H2INC taking input from key stakeholders including CM experts, biomedical providers, and CA patients. What remains to be studied is the dissemination of H2INC (in person, paper copies, online) and acceptability of H2INC within the clinical and community settings and among non-CA populations. Future research will test the feasibility, acceptability and potential impact of H2INC in clinical and community settings.
4.3. Practice Implications
CAs experience a substantial burden of CVD. Current nutritional guidelines are generally not language appropriate and not routinely inclusive of culturally-relevant practices such as CM. H2INC is a bilingual (English/Chinese) health education resource, developed with the involvement of CM experts, biomedical providers, and CA patients, that holds promise as a potentially high value patient-centered and culturally-sensitive health education material for both CA patients and providers that care for this underserved population. Future work is needed to understand optimal approaches to implement and disseminate H2INC in clinical and community settings, to explore how patient-provider interaction about diet, CVD and CM is impacted by H2INC and how it may impact attainment of CVD health parameters.
Acknowledgments:
We would like to thank the research participants for sharing their time and knowledge with us and the following research assistants: Stephanie Wong, Annalise Stromsta, Ryan Qiu and Ashley Liu and graphic designers Ashley Lin, Ema Matsumura, Yvonne Chow, and Antony Nguyen. This work was supported by funding from the Mount Zion Health Fund (grant number 20160995), the USF Faculty Development Fund, and the National Center for Advancing Translational Sciences of the NIH (award number KL2TR001870). The funding sources had no role or involvement in the design and conduct of the study; the collection, management, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript. Contents are solely the responsibility of the authors and do not necessarily represent the official views of the funders.
Footnotes
Conflicts of interest: There are no conflicts of interest.
Research Ethics: We confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- [1].U.S. Census Bureau News, Facts for Features Asian/Pacific American Heritage Month: May 2013, 2013. http://www.census.gov/newsroom/releases/archives/facts_for_features_special_editions/cb13-ff09.html. (Accessed June 4 2013).
- [2].U.S. Census Bureau News, Facts for Features Asian/Pacific American Heritage Month: May 2017, 2017 https://www.census.gov/newsroom/facts-for-features/2017/cb17-ff07.html. (Accessed March 1 2018).
- [3].Cooc N, Leung G, Who are ‘Chinese’ speakers in the United States?: Examining differences in socioeconomic outcomes and language identities, AAPI Nexus. 15 (2017). [Google Scholar]
- [4].Kim G, Chiriboga DA, Jang Y, Lee S, Huang CH, Parmelee P, Health status of older Asian Americans in California, J Amer Geriatr Soc. 58 (2010) 2003–8. [DOI] [PubMed] [Google Scholar]
- [5].Sentell T, Braun KL, Low health literacy, limited English proficiency, and health status in Asians, Latinos, and other racial/ethnic groups in California, J Health Commun. 17 (2012) 82–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Jose PO, Frank AT, Kapphahn KI, Goldstein BA, Eggleston K, Hastings KG, Cullen MR, Palaniappan LP, Cardiovascular disease mortality in Asian Americans, J Amer Coll of Cardiol. 64 (2014) 2486–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Satia JA, Patterson RE, Taylor VM, Cheney CL, Shiu-Thornton S, Chitnarong K, Kristal AR, Use of qualitative methods to study diet, acculturation, and health in Chinese-American women, J Amer Diet Assoc. 100 (2000) 934–40. [DOI] [PubMed] [Google Scholar]
- [8].Kong H, Hsieh E, The social meanings of traditional Chinese medicine: elderly Chinese immigrants’ health practice in the United States, J Immigr Minor Health. 14 (2012) 841–9. [DOI] [PubMed] [Google Scholar]
- [9].Guo XY, Liu J, Li HJ, Qi Y, Qin LP, Wang M, Zhao D, Use of traditional Chinese medicine in Chinese patients with coronary heart disease, Biomed Environ Sci. 26 (2013) 303–10. [DOI] [PubMed] [Google Scholar]
- [10].Jiang S, Quave CL, A comparison of traditional food and health strategies among Taiwanese and Chinese immigrants in Atlanta, Georgia, USA, J Ethnobiol Ethnomed. 9 (2013) 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Jiang RS, Wu SM, Che HL, Yeh MY, Cultural implications of managing chronic illness: treating elderly Chinese patients with heart failure, Geriatr Nurs. 34 (2013) 199–203. [DOI] [PubMed] [Google Scholar]
- [12].Rong X, Peng Y, Yu HP, Li D, Cultural factors influencing dietary and fluid restriction behaviour: perceptions of older Chinese patients with heart failure, J Clin Nurs. 26 (2017) 717–26. [DOI] [PubMed] [Google Scholar]
- [13].Shen C, Pang SM-C, Kwong EW-Y, Cheng Z, The effect of Chinese food therapy on community dwelling Chinese hypertensive patients with Yin-deficiency, J Clin Nurs. 19 (2010) 1008–20. [DOI] [PubMed] [Google Scholar]
- [14].Chao MT, Wade C, Kronenberg F, Disclosure of complementary and alternative medicine to conventional medical providers: variation by race/ethnicity and type of CAM, J Natl Med Assoc. 100 (2008) 1341–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Ho EY, Leung G, Pritzker S, Chi H-L, Hsieh E, Chan D, Ting I, Chen Y, Huang S, Ruan QN, Seligman HK, Creating and pilot testing an integrative Chinese medicine diet for Chinese Americans with type 2 diabetes [Abstract], Diabet. 64 (2015) A623. [Google Scholar]
- [16].Chesla CA, Chun KM, Kwan CM, Cultural and family challenges to managing type 2 diabetes in immigrant Chinese Americans, Diabet Care. 32 (2009) 1812–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Ho EY, Tran H, Chesla CA, Assessing the cultural in culturally sensitive printed patient-education materials for Chinese Americans with type 2 diabetes, Health Commun. 30 (2015) 39–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Strauss A, Corbin J, Basics of qualitative research: Techniques and procedures for developing grounded theory, 2nd ed., Sage, Thousand Oaks, CA, 1998. [Google Scholar]
- [19].Jones J, Hunter D, Consensus methods for medical and health services research, Brit Med J. 311 (1995) 376–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Ward T, Multiple enactments of Chinese medicine, in: Scheid V, MacPherson H (Eds.), Integrating East Asian Medicine Into Contemporary Healthcare, Churchill Livingstone Elsevier, Edinburgh, Scotland, 2012, pp. 55–74. [Google Scholar]
- [21].Ho EY, Lalancette C, Leung G, ‘Using Chinese medicine in a Western way’: Negotiating integrative Chinese medicine treatment for Type 2 Diabetes, Commun Med. 12 (2015) 41–54. [DOI] [PubMed] [Google Scholar]
- [22].Lai L, Flower A, Moore M, Lewith G, Developing clinical practice guidelines for Chinese herbal treatment of polycystic ovary syndrome: A mixed-methods modified Delphi study, Complement Ther Med. 23 (2015) 430–8. [DOI] [PubMed] [Google Scholar]
- [23].Schnyer RN, Conboy LA, Jacobson E, McKnight P, Goddard T, Moscatelli F, Legedza AT, Kerr C, Kaptchuk TJ, Wayne PM, Development of a Chinese medicine assessment measure: an interdisciplinary approach using the delphi method, J Altern Complement Med. 11 (2005) 1005–13. [DOI] [PubMed] [Google Scholar]
- [24].Kaptchuk TJ, The web that has no weaver, 2nd ed., Congdon & Weed, New York, 2000. [Google Scholar]
- [25].Kwan CML, Chun KM, Huang P, Chesla CA, Concerns about professional Chinese medicine among Chinese immigrants with type 2 diabetes, Diabet Spectr. 26 (2013) 247–53. [Google Scholar]